Abstract
Purpose:
The objective of the study is to investigate trajectories of stress and depressive symptoms of spousal and intimate partner caregivers in the context of cancer. We also examined the patient related predictors of caregiver stress and depression.
Design:
This is a longitudinal cohort study.
Participants:
Patients diagnosed with cancers affecting the hepatobiliary and pancreatic system and their spousal or intimate partner caregivers were recruited at a large tertiary cancer center.
Methods:
The patients and caregivers were assessed for their level of stress, depressive symptoms, relationship quality, and quality of life at the time of the patients’ diagnosis, every 2 months for 12 months and then at 18 months.
Findings:
One hundred and seventy-nine caregivers were included in the trajectory analyses. Amongst the 179 caregivers, 120 patient and caregiver dyads had complete data at baseline to 6-months. The majority of the spousal caregivers were female (84%) and the mean age was 57 years. 25% of caregivers reported high levels of chronic depressive symptoms. However, significant reductions were observed at 6 months. High and moderate levels of caregiver stress were also reported in 21% and 36% of caregivers, respectively. The caregivers who reported moderate levels of stress had a decrease in stress over time while those in the high stress group reported stable levels of stress over time. Caregivers’ stress is predicted by the cancer patients’ depressive symptoms but not patients’ quality of life.
Conclusions:
Caregivers who reported high levels of stress and depressive symptoms at patients’ cancer diagnosis remain high even after the initial adjustment. A bidirectional relationship between the caregivers’ stress and the patients’ depressive symptoms was observed.
Implications:
The development of dyadic interventions focusing on the patients’ and caregivers’ distress is warranted to decrease psychological morbidities of the dyad.
Keywords: cancer caregiver, depression, stress, dyadic functioning, quality of life
Introduction
Cancer is the second leading cause of death in the United States, exceeded only by heart disease, and accounts for nearly one in every four deaths.1 A report from National Alliance for Caregiving in 2015 stated that there are approximately 3 million Americans who care for someone with cancer at home and one in ten provides care for a spouse/partner.2 Caregiving has been shown to be associated with increased morbidity and increased risk of CVD and mortality.3–5 Therefore, understanding the predictors of the consequences of cancer caregiving will allow researchers to develop targeted and effective interventions to reduce psychological and physical morbidity and mortality for intimate partner caregivers.
Spousal caregivers have been linked to poor quality of life and an increased risk of cardiovascular disease (CVD) and mortality.6–8 Lee and colleagues found that caring for an ill spouse or parent was associated with increased risk of coronary heart disease.8 Specific to cancer spousal caregivers, Ji and colleagues found in a large epidemiological study that those caring for advanced cancer patients had the highest risk of CVD and mortality when compared to caregivers of spouses with earlier stage cancers and non-caregiving matched controls.6 The association of stress and depression with CVD has been recognized in caregivers in prior research. In the general population, a diagnosis of depression has been associated with a greater risk of developing metabolic syndrome and CVD.9 Kim and colleagues’ concluded that the stress of spousal caregivers of cancer patients was linked to heart disease independent of age, sex, education, and income. Stressed spousal caregivers were also more likely than other caregivers to develop arthritis and chronic back pain several, which commonly cause disability, years after the initial caregiving experience.7
Caregivers often report higher rates of depression when compared to the general population.10–12 Estimates are that between 40%−70% of caregivers caring for spouses with a variety of chronic diseases, have clinically significant symptoms of depression. Between 25%−50% of these caregivers meet the diagnostic criteria for Major Depression.13,14 Evidence of the high prevalence of depression among cancer caregivers has also been documented.15,16,17A recent prospective longitudinal study of 416 cancer caregivers has found 40% of current caregivers and 50% for bereaved caregivers have depressive symptoms severe enough to be viewed as clinically meaningful (CES-D score ≥16).17,18 Geng and colleagues’ systematic review and meta-analysis reported a 42.3% of prevalence of depression among 21,149 cancer caregivers. Caring for a spouse or parent was also found to be more stressful for caregivers than caring for another relative (35%) or non-relative (18%).2 It is well documented that perceived stress is associated with an increased risk of coronary heart disease. While much work examined stress has been conducted on the elderly and dementia patients’ caregivers,19 relatively little work to date exists on cancer caregiver.
Different from dementia caregivers, cancer caregivers usually provide care for a short and more intense periods with the same amount of effort per week.20 Based upon the literature, the acute and intensive cancer caregiving experience and patterns of depressive symptom changes before and after bereavement suggests that findings in different types of caregiving research might not generalize to cancer caregivers and research of trajectories of stress and depressive symptoms is warranted to understand this unique caregiving course. Few studies have examined the stress and depressive trajectories of spousal caregivers of cancer patients. A study examining depressive symptoms of caregivers providing end-of-life care found a curvilinear model of spousal caregivers’ depressive symptom trajectory.21 The authors concluded that caregivers are more vulnerable when first transitioning to caregiving role and the symptoms ease over time but go up again before patients’ last month of life. One study focused on male spousal caregivers of breast cancer patients found the caregivers had a persistently high level of depressive symptoms and it slowly decreases over the course of a year.22 No study has been identified assessing stress trajectories among cancer caregivers.
Predictors of cancer caregivers’ stress and depressive symptoms started receiving attention in recent years. Caregiving stress, sleep problems, perceived care burden and lack of social support are widely recognized as important predictors of cancer caregiver’s depressive symptoms.18,23,24 Sociodemographic factors such as gender, caregiving demands, feelings of exhaustion and role entrapment are also well documented as the predictors of caregiver’s stress.25, 26 How cancer patients’ outcomes predict their caregiver’s stress and depressive symptoms has not yet been fully investigated. A rich body of research has provided empirical support for the influences of patient’s depression on their caregivers’ depression. But it is unknown if patient’s depression has the similar impacts on caregiver’s stress and how it developed over time.27,28 Patients’ health related quality of life is also playing a significant role of determining their spousal caregivers’ stress and depression.29,30 Steel and colleagues found that the reduction of the care recipients’ cancer-related symptoms reduced the caregivers’ level of stress and depression.31 In addition to traditionally studied predictors of stress and depression, few studies have longitudinally explored the predictors of spousal caregivers’ stress and depressive symptoms.
Given the facts that there is a significant number of intimate partner cancer caregivers in the US and high prevalence and high prevalence of depressive symptoms and caregiving stress observed, the purpose of this study is to address the gap in the current spousal cancer caregiver literature by analyzing trajectories of stress and depressive symptoms and examining the patient-related predictor of caregivers’ stress and depressive symptoms over time.
Methods
Design
The study is prospective in design. Cancer patients and intimate partner caregivers were assessed at baseline (at diagnosis), every 2 months for 12 months and then at 18 months.
Participants and procedures
The study was approved by the University of Pittsburgh Institutional Review Board (IRB) before commencement of the study. Patients diagnosed with advanced cancers affecting the hepatobiliary and pancreatic system at a large tertiary cancer center and their caregivers were referred by their attending physician and enrolled between January 2008 and September 2012. One hundred and seventy-nine caregivers were recruited at the time of patient’s diagnosis in this study. Amongst 179 caregivers, 120 patient and caregiver dyads completed the questionnaires from baseline to 6-month follow up. Inclusion criteria for the patients were: (1) biopsy, radiological and/or biological evidence of cancer, (2) age 21 years or older, and (3) fluency in English. Exclusion criteria for patients included current suicidal or homicidal ideation, or current psychosis or thought disorder. Inclusion criteria for the caregivers were (1) spouse or intimate partner of the cancer patient, (2) caregiver of the cancer patient, (3) age 21 years or older. Exclusion criteria for caregivers included psychiatric symptoms including psychosis, thought disorder, current suicidal ideation. The exclusion criteria for caregivers is severe mental illness (e.g., psychosis, thought disorder, current suicidal ideation). The patient and caregiver provided written informed consent. Patients and family caregivers were interviewed by phone separately. The interviewers were blinded and used a structured clinical interview based on the questionnaires described below.
Instruments
Sociodemographic, disease, and treatment specific factors
Sociodemographic data including patients and caregivers’ age, gender, race, ethnicity, educational level, income (reported by range) and basic needs were collected on a self-reported questionnaire designed specifically for this study. Disease-specific and treatment-related information including diagnosis, number of lesions, size of lesions, and treatment was gathered from the patients’ electronic medical record.
Caregiver Stress
The Caregiver Quality of Life Index-Cancer Scale (CQOLC)32 is a 35-item, 5-point Likert-type scale designed to measure caregiver stress. The total possible score is the summed score of 35 items ranging from 0 to 140. The CQOLC was reversed scored to reflect high levels of stress rather than high levels of quality of life. The items of the CQOLC reflect caregiving related stressors. The CQOLC is a measure of the effect of a loved one’s illnesses on a family caregiver’s physical, emotional, social and other areas of function. The internal consistency of the instrument has been reported to be excellent–the Cronbach alpha is 0.91.32 Significant differences have been shown between CQOLC ratings in cancer caregivers and hospice caregiver; with evidence the instrument can make discernments between reports of caregiver stress at different stages of patient treatment.33 This is the only instrument solely for caregivers in the study. All the other instruments are for both cancer patients and their intimate partner caregivers.
Depressive Symptoms
The Center for Epidemiologic Studies-Depression (CES-D)34 is a 20-item, self-report questionnaire that provides an index for the presence of depressive symptoms over the previous seven days. Patients and caregivers responded to items on a four-point Likert scale (0 = rarely or none of the time; 1 = some or a little of the time; 2 = occasionally or a moderate amount of time; and 3 = most or all of the time). The CES-D has a range of 0–60 for the summed item scores. The established clinical cutoff is a score of 16 or higher scores, which was used to signify clinical levels of depression.34 The CES-D has demonstrated adequate construct validity and was found to be reliable in studies including patients with breast cancer as well as caregivers of cancer patients.35
Health Related Quality of Life
The Functional Assessment of Cancer Therapy (FACT)-Hepatobiliary36 was used to assess quality of life of the cancer patient. The FACT-Hep includes both the FACT-General (FACT-G) and a module specific to hepatobiliary disease (HepCS). The FACT-G is a 27-item instrument with four subscales for physical (PWB), social and family (SFWB), emotional (EWB), and functional well-being (FWB). The HepCS includes 18 items that pertain to symptoms of the disease as well as side effects of treatment. All FACT items are rated on 5-point scales ranging from 0 = not at all to 4 = very much. The FACT-G and HepCS score are summed to form the FACT-Hep total score, which ranged from 0–180. Higher scores on all scales of the FACT-Hep reflect better quality of life or fewer symptoms. The FACT is one of the most widely utilized quality of life questionnaires in clinical trials for new cancer treatments.37 Both the FACT-G and the FACT-Hep have been demonstrated to be valid and reliable instruments.38
Statistical Analyses
Preliminary analyses to examine descriptive statistics and to verify characteristics and distributions of variables were performed using SPSS (v. 26, IBM), while primary analyses were performed using SAS software. To examine caregiver stress and depressive symptoms over time, multiple trajectory polynomial censored regression analyses with maximum likelihood estimation were performed using a group-based semi-parametric technique in SAS PROC TRAJ.39 The group-based semi-parametric method, which was well-suited for categorical data, assumed that the population defined by outcome variables were composed of a mixture of multiple underlying trajectory groups. A different number of multiple trajectories using first-order (linear) and second-order (quadratic) polynomials were estimated for caregivers’ stress and depressive symptoms. A comprehensive examination of all model fit indices, including the Akaike’s Information Criterion, Bayesian Information Criterion, classification quality, and likelihood ratio tests, was used to determine the best fit of trajectories.
Cross-lagged panel analyses were performed to examine predictors of caregiver depressive symptoms over time. Prior to the analyses, simple linear regressions were performed to examine associations between demographic characteristics (age, gender, marital status, education level), predictors (caregiver stress, quality of life), and caregiver depressive symptoms. In the panel analyses, three types of relationships were examined: 1) autoregressive (e.g., relationship between depressive symptoms at time 1 and depressive symptoms at time 2; 2) contemporaneous (e.g., relationship between depressive symptoms and predictors at same time points); and 3) cross-lagged (predictive relationship between depressive symptoms and predictors at subsequent time points).
Results
Consistent with the characteristics of diagnoses of this sample (e.g., hepatocellular carcinomas) a 2:1 male to female ratio (70.8% males) was observed, and the mean age was 61.6 with a range of 36–91 years. The majority of patients were diagnosed with hepatocellular carcinoma (73.3%). The majority of caregivers were female (84%) and mean age was 57 years with a range of 25–83 years. Disease specific factors of the patient and demographic characteristics of the patient and caregiver can be found in Tables 1 and Table 2.
Table 1:
Sociodemographic and disease related characteristics of patients, n=120
| Characteristics | N (%) |
|---|---|
| Gender | |
| Male | 85 (70.8) |
| Female | 35 (29.2) |
| Age | |
| Mean (SD) | 62 (12.7) |
| Range | 36 – 92 |
| Diagnosis | |
| Hepatocellular carcinoma | 88 (73) |
| Cholangio carcinoma | 8 (7) |
| Colorectal cancer with liver metastases | 10 (8) |
| Other | 14 (12) |
| Size of Lesions | |
| Mean (SD) | 5.5 (5) |
| Number of Lesions | |
| <2 lesions | 54 (45) |
| >2 lesions | 66 (55) |
| Treatment | |
| No treatment | 11 (9) |
| Transarterial Chemoembolization | 57 (47) |
| 90 Yttrium Radioembolization | 24 (20) |
| Radiofrequency Ablation | 10 (8) |
| Resection | 17 (14) |
Table 2:
Caregiver sociodemographic characteristics, n=120
| Characteristics | N (%) |
|---|---|
| Gender | |
| Male | 101 (84) |
| Female | 19 (16) |
| Age | |
| Mean (SD) | 57 (13) |
| Range | 25 – 83 |
| Ethnicity | |
| Caucasian | 102 (85) |
| African American | 7 (6) |
| Asian American | 10 (8) |
| Hispanic/Latino | 1 (1) |
| Education Completed | |
| High school or GED1 | 102 (85) |
| Vocational/tech/2-year college | 18 (15) |
| 4 years college | 28 (23) |
| Master, Doctorate or professional degree | 12 (10) |
| Annual Household Income in USD | |
| < 20,000 | 9 (7) |
| 20,000–50,000 | 27 (22) |
| 50,001–100,000 | 79 (66) |
| >100,000 | 6 (5) |
| Difficulty Meeting Basic Needs | |
| Not at all | 11 (9) |
| Somewhat | 57 (47) |
| Extremely | 24 (20) |
GED refers to Graduate Equivalency Degree
The mean of the patient CES-D score is 13.2 (SD=10.5) and the mean of caregiver CES-D score is 15.7 (SD=11.6). Caregiver stress has a mean score of 102 (SD=106.6). The mean of patients’ health related quality of life score is 76.3 (SD=19.4).
Trajectories of Caregiver Stress and Depressive Symptoms
Three trajectory groups for caregiver’s stress (linear trend was best fit based on BIC values) were observed. There were 42.7% cases in Group 1 (low stress), 36.0% cases in Group 2 (moderate stress), and 21.3% cases in Group 3 (high stress). The low stress group (M=30.80) experienced a significant reduction in caregiver stress over time (B=−1.46, p<.05), as did the moderate stress group (M=53.76) (B=−2.08,p<.05); however, the high stress group (M=69.34) did not experience a significant decline in caregiver stress over time (B= −0.64, p>.05). See Figure 1.
Figure 1:
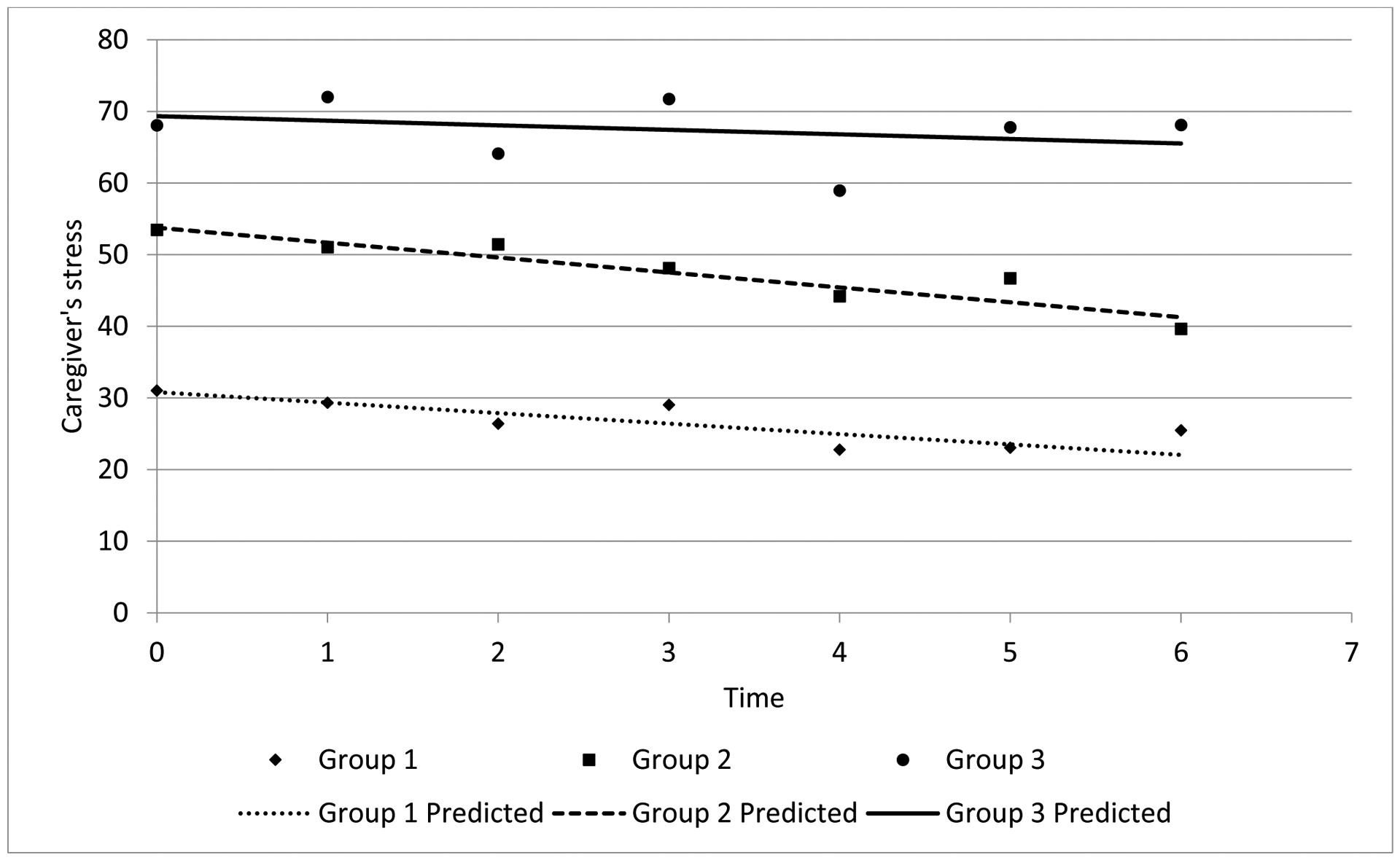
Semi-parametric trajectory analyses of caregivers’ stress, n=179
* The groups are categorized using Caregiver Quality of Life Index-Cancer Scale (total score range, 0 to 140). Higher score represents higher stress.
* Group1=Low Stress; Group 2=Moderate Stress; Group 3=High Stress
* Time Point 0=Diagnosis of Patient; Time Point 1=2 months; Time Point 3=4 months; Time Point 4=6 months; Time Point 5=8 months; Time Point 6=10 months
Two trajectory groups (low level of depressive symptoms and high level of depressive symptoms) for caregivers’ depressive symptoms (linear and quadratic trend) were estimated. There were 77.2% (low level) and 22.8% (high level) of cases in the groups, respectively. There was a significant linear reduction of caregiver’s depressive symptoms over time (B = −2.43, p<.05) for the low-level group. For the high-level group, there were significant linear (p<.05) and quadratic (p<.05) trends over time. See Figure 2.
Figure 2:
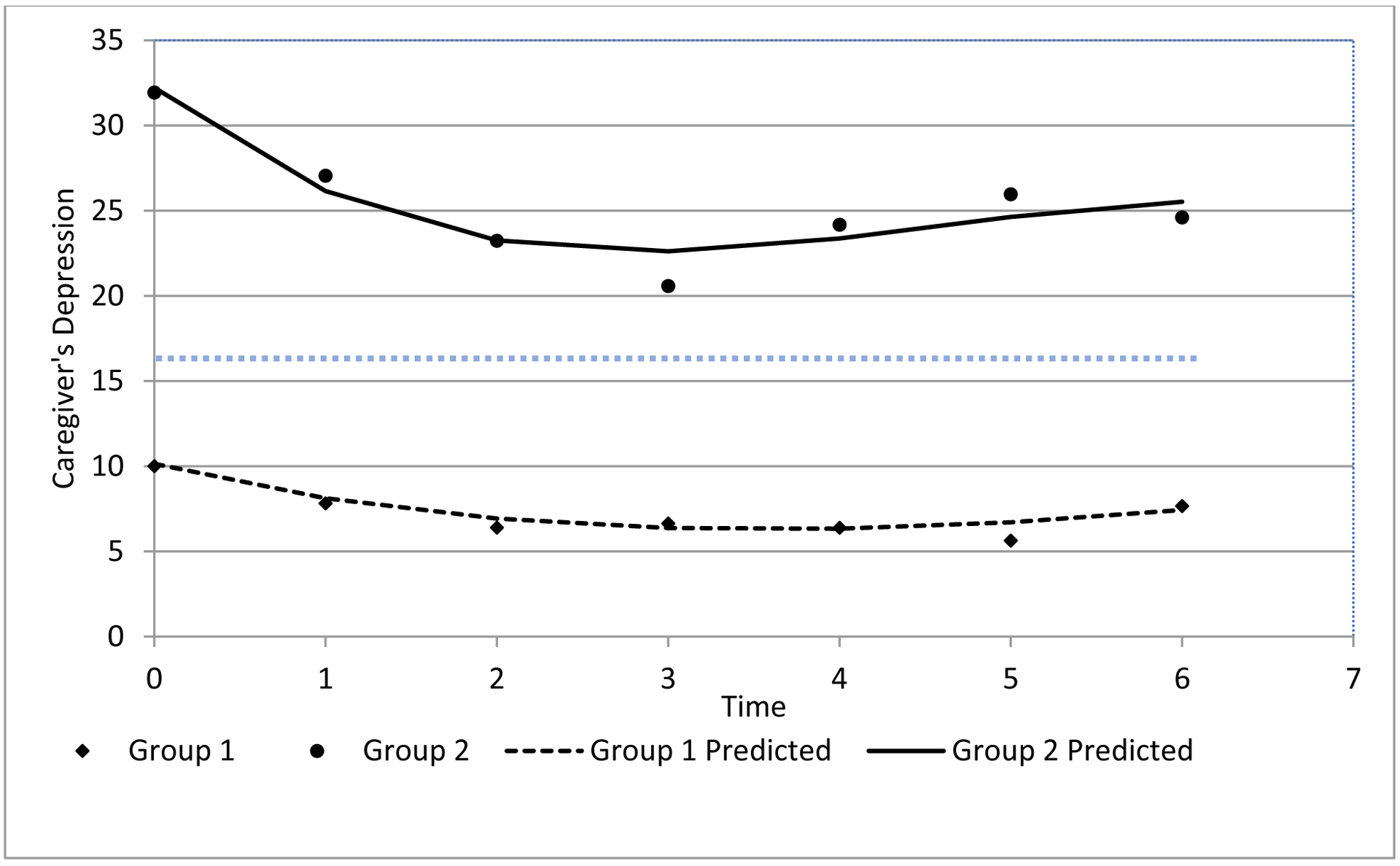
Semi-parametric trajectory analyses of caregivers’ depressive symptoms, n=179
* Group 1=Depressive symptoms below clinical cutoff; Group 2=Depressive symptoms above the clinical cutoff; the blue dotted line represents the clinical cutoff score “16” of the Center for Epidemiologic Studies-Depression.
* Time Point 0=Diagnosis of Patient; Time Point 1=2 months; Time Point 3=4 months; Time Point 4=6 months; Time Point 5=8 months; Time Point 6=10 months
Predictors of Caregiver Stress and Depressive Symptoms
Using simple linear regressions, demographic characteristics such as caregiver age, caregiver gender, patient gender, marital status, and educational level as well as disease specific variables of the patient including diagnosis were not found to be significant predictors of the caregivers’ reported depressive symptoms or levels of stress (p>.05). However, when using cross-lagged panel analyses, the caregivers’ reported stress at 2-months was predicted by the patients’ level of depressive symptoms (β=0.21, p<.01) and the caregiver’s stress predicted the patients’ depressive symptoms at 4-months (p<.05). See Figure 3.
Figure 3:
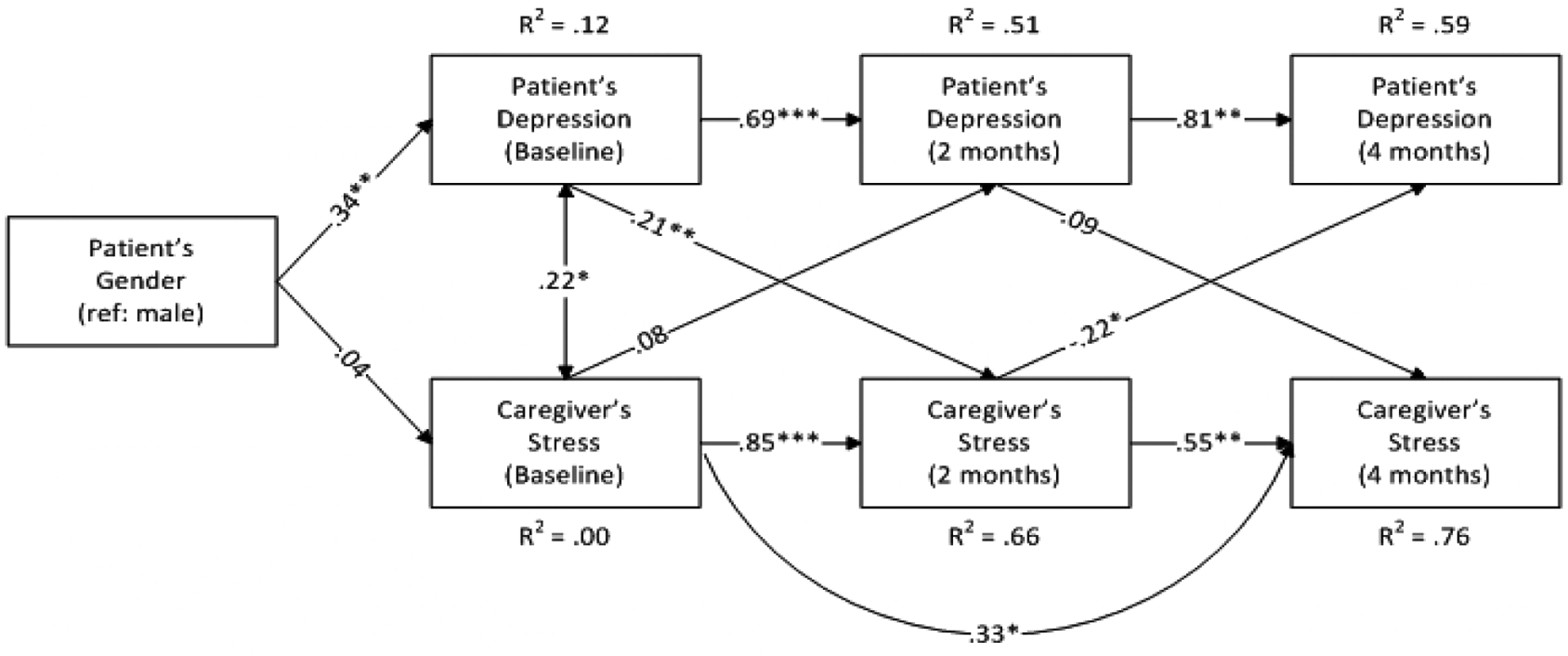
Cross-lagged panel analyses of predictors of caregiver stress, n=120
* p < 0.05, ** p <0.01, *** p < 0.001
The results of simple linear regressions revealed no patient demographic or disease specific characteristics were related to quality of life including gender or diagnosis (p >.05). Caregiver gender, marital status, or educational level were also not significantly associated with quality of life (p>.05). Patients’ quality of life was significantly associated with caregivers’ depression at baseline (p<.01). However, using cross-lagged panel analyses, the patients’ quality of life did not significantly predict the caregivers’ depressive symptoms at any time points. See Figure 4.
Figure 4:
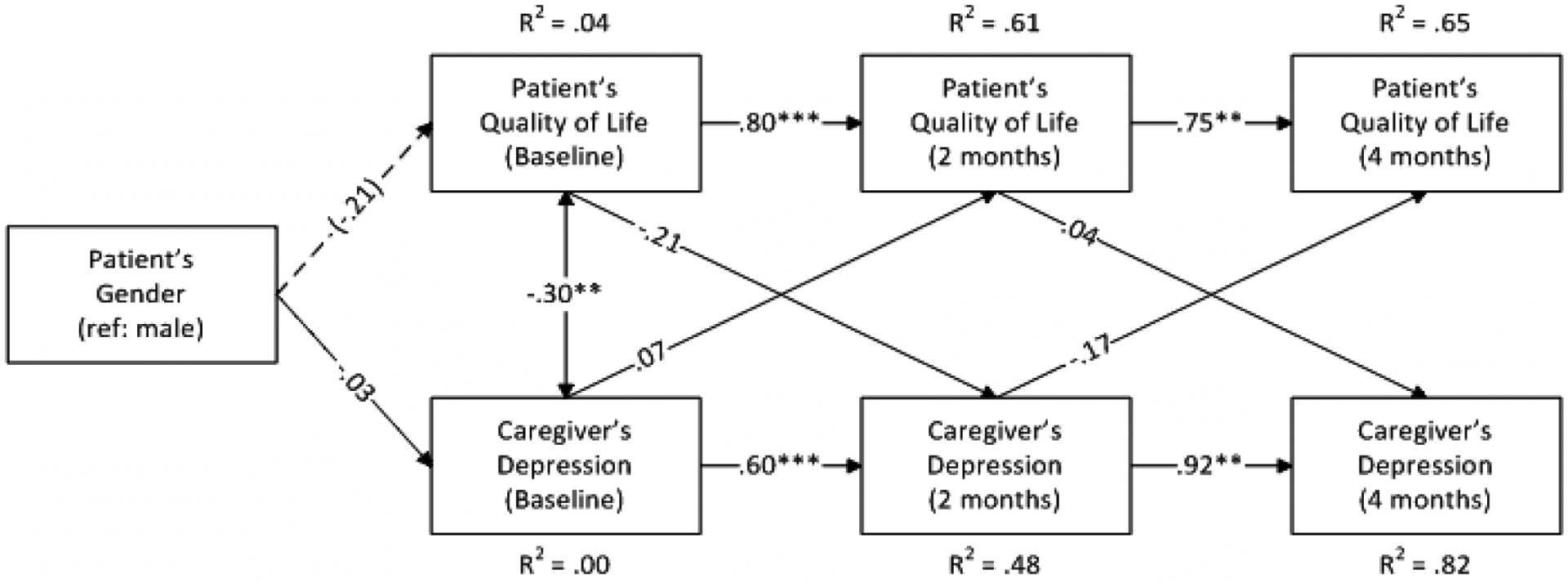
Cross-lagged panel analyses of predictors of caregivers’ depressive Symptoms, n=120
---p<0.10, * p <0 .05, ** p <0.01, *** p < 0.001
The relationship between patient and caregiver’s depression and patient HRQoL and caregiver’s stress were examined but not found to be statistically significant.
Discussion
The present study is one of the first to prospectively examine the courses and predictors of stress and depressive symptoms in intimate partner caregivers of advanced cancer patients.
Moderate to high levels of chronic stress were observed in over half of the caregivers. The trajectory of stress showed that there was a reduction in stress among caregivers who reported a low and moderate level of stress, but this trend was not seen among high-stress caregivers. The group of caregivers who reported high levels of stress, that remained stable over time, may be particularly vulnerable to cardiovascular disease.6–8 An emergent research literature on caregiver stress has begun to develop interventions to manage caregiver’s stress. However, most interventions to date have focused on dementia caregivers; there remains a major need for cancer caregiver interventions.43
Caregivers shown a higher level of depressive symptoms compared with their care recipients and the average score is closer to the clinical threshold of depression. High and moderate rates of depressive symptoms were observed in the caregivers with nearly a quarter of cancer caregivers reported high levels of chronic depressive symptoms in the clinical range. These findings are consistent with a study of advanced gastrointestinal and lung cancer patients which found that 38.9% of caregivers and 23% of their care recipients reported symptoms of depression.5 The rates of depression in women with breast cancer and their caregivers was 11% and 12%, respectively.40 Although cancer patients in this study retained greater physical functioning over the course of their illness, their caregivers in this study reported higher rates of depressive symptoms.
The high rate of depression in caregivers may be secondary to the larger number of women in the present study when compared to a study of caregivers for breast cancer which are primarily male and often patients have a better prognosis.3 Prior research provide substantial supports on female caregivers having a higher rate of depression.17 Interestingly, female caregivers of Alzheimer’s patients had high, stable rates of depression while male caregivers’ depression increased over time.41 These findings suggest the importance of examining gender when investigating the interaction between the patients’ and caregivers’ psychological functioning and the need for prospective studies of family caregivers.
A higher proportion of caregivers reported clinical levels of depression when compared to the study by Chen and colleagues which included breast cancer patients’ caregivers.22 We also found a decrease of depressive symptoms with a larger effect size. This finding may be secondary to the longer follow up period that we included in the present study. The trajectories of caregivers’ depressive symptoms in our study showed a similar pattern with the “resilience trajectory” described in the study by Tang and colleagues.21 This resilience trajectory is reflected by the sharp decrease in depressive symptoms followed by stable levels of depressive symptoms. Differed from this trajectory, our findings reveal that caregivers who have high levels of depressive symptoms at baseline continue to have symptoms above clinical threshold over the course of 18 months. One explanation for the difference was the nature of our study participants. The cohort of caregivers in the present study included carers of advanced cancer patients. Thus, they are more likely to show increasing depressive symptoms that may reflect anticipatory grief. This suggests that closely monitoring depressive symptoms among spousal caregivers of cancer patients and constantly providing emotional supports are critical along the way of their caregiving journey. Anticipatory grief shares some symptomatology with depression but may be treated differently.44 Interventions to assist the coping with anticipatory grief have been developed and test for caregivers of dementia patients, but little has been done with cancer caregivers.45”
A large majority of caregiving research that has been conducted was cross-sectional in design and therefore the present prospective study provides important longitudinal findings regarding the predictors of caregivers’ stress and depressive symptoms. Unlike prior research, no sociodemographic or disease specific factors predicted caregiver stress or depression. But we observed a bidirectional relationship between patients’ depressive symptoms and caregiver stress at four months follow up. This suggests that patients’ depressive symptoms at or shortly after the diagnosis predict subsequent caregiver stress. Patients’ depressive symptoms in turn predicted caregivers’ stress. Due to the relatively short follow up, whether the bidirectional relationship will continue across a longer time period is not unknown. Future research may benefit from larger samples of patient-caregiver dyads followed for a longer period of time.
These findings also suggest that dyadic interventions are warranted secondary to the interdependence between patients and caregivers. For decades, psychosocial interventions have attempted to reduce depression, stress, and improve quality of life in patients and caregivers separately.46A study looking at dyadic effects of coping strategies found that when caregivers seek social support, patients feel greater anxiety; conversely, when patients seek for social supports, both the patients and caregivers experience lower anxiety.47 These studies and our findings together suggest that both patients and caregivers should be included in psychosocial programs to better support caregivers while avoiding creating anxiety for patients. Few interventions have been designed and tested to include both patient and caregiver with a focus on the dyad in the context of cancer. A meta-analysis of interventions focused on patient-caregiver dyads concluded that there are small but beneficial effects in improving the quality of life in patients and caregivers.48 More recent studies however, have concluded that interventions with patient-caregiver dyads with a significant decrease in caregiver’s anxiety, depression and burden.49 A recent dyadic psychological intervention in the palliative care setting found consistent results.50 A paradigm shift has begun in which policy makers, stakeholders, and research funding agencies are beginning to recognize the association of cancer patients’ and caregivers’ outcomes and the importance of treating them together. Research will benefit by developing and testing dyadic intervention targeting enhancing relationship quality between cancer patients and their caregivers.
There are limitations of this study including the short term of follow up, the generalizability of caregivers to other cancer types, particularly at earlier stages of the disease, and the relatively small sample size. The sample size of this study may not have the power to detect all significant relationships between variables; therefore, the results should be cautiously interpreted. It is also too small at this time to be able to include all potential covariates.
Conclusion
The rate of stress and depressive symptoms was high among intimate partner caregivers of advanced cancer patients. There was a further improvement in stress for caregivers who reported low and moderate stress and low depressive symptoms at their spouse’s cancer diagnosis. However, those who reported a high level of stress and depressive symptoms remained above the clinical threshold of depression after the adjustment from the diagnosis of the patient. In the cross-lagged panel analyses, we observed a bidirectional relationship between the caregivers’ stress and the patients’ depressive symptoms. Larger multi-center longitudinal studies with a more diverse sample are needed to make definitive conclusions. Future research may want to include a measure of caregivers’ anticipatory grief to explore if this is driving the depressive symptoms after the diagnosis of the patient so as to develop appropriate interventions for caregivers. Dyadic interventions are also warranted to improve cancer patients’ and their caregivers’ quality of life.
Acknowledgments
Support and Financial Disclosure Declaration: NCIK07CA118576
Contributor Information
Qi Chen, University of Pittsburgh School of Medicine, Department of Surgery; University of Texas at Austin, Steven Hicks School of Social Work.
Lauren Terhorst, University of Pittsburgh, Department of Occupational Therapy
David A. Geller, University of Pittsburgh School of Medicine, Department of Surgery
Wallis Marsh, University of Pittsburgh School of Medicine, Department of Surgery
Michael Antoni, University of Miami, Department of Psychology
Mary Amanda Dew, University of Pittsburgh, Department of Psychiatry, Psychology, Epidemiology, and Biostatistics
Michelle Biala, University of Pittsburgh, Department of Psychology.
Josh Weinstein, University of Pittsburgh, Department of Surgery
Allan M.D. Tsung, University of Pittsburgh School of Medicine, Department of Surgery
Jennifer Steel, University of Pittsburgh School of Medicine, Department of Surgery, Psychiatry, and Psychology
Reference
- 1.Miller KD, Siegel RL, Lin CC, et al. Cancer treatment and survivorship statistics, 2016. 2016;66:271–89. [DOI] [PubMed] [Google Scholar]
- 2.AARP NAfCa. Caregiving in the U.S 2015. Retrieved from: http://www.aarp.org/content/dam/aarp/ppi/2015/caregiving-in-the-united-states-2015-report-revised.pdf.2015.
- 3.Grunfeld E, Coyle D, Whelan T, et al. Family caregiver burden: results of a longitudinal study of breast cancer patients and their principal caregivers. Canadian Medical Association Journal 2004;170:1795–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O’Reilly D, Connolly S, Rosato M, et al. Is caring associated with an increased risk of mortality? A longitudinal study. Social Science & Medicine 2008;67:1282–90. [DOI] [PubMed] [Google Scholar]
- 5.Braun M, Mikulincer M, Rydall A, Walsh A, Rodin G. Hidden morbidity in cancer: spouse caregivers. Journal of Clinical Oncology 2007;25:4829–34. [DOI] [PubMed] [Google Scholar]
- 6.Ji J, Zöller B, Sundquist K, Sundquist J. Increased Risks of Coronary Heart Disease and Stroke Among Spousal Caregivers of Cancer PatientsClinical Perspective. Circulation 2012;125:1742–7. [DOI] [PubMed] [Google Scholar]
- 7.Kim Y, Carver CS, Shaffer KM, Gansler T, Cannady RS. Cancer caregiving predicts physical impairments: roles of earlier caregiving stress and being a spousal caregiver. Cancer 2015;121:302–10. [DOI] [PubMed] [Google Scholar]
- 8.Lee S, Colditz GA, Berkman LF, Kawachi I. Caregiving and risk of coronary heart disease in US women: a prospective study. American Journal of Preventive Medicine 2003;24:113–9. [DOI] [PubMed] [Google Scholar]
- 9.Busch LY1PP, Valentine JC1. Meta-analyses of cardiovascular reactivity to rumination: A possible mechanism linking depression and hostility to cardiovascular disease. Psychological Bulletin 2017;143:1378–94. [DOI] [PubMed] [Google Scholar]
- 10.Pinquart M, Sörensen S. Differences between caregivers and noncaregivers in psychological health and physical health: a meta-analysis. Psychology and aging 2003;18:250. [DOI] [PubMed] [Google Scholar]
- 11.Kim Y, Duberstein PR, Sörensen S, Larson MR. Levels of depressive symptoms in spouses of people with lung cancer: effects of personality, social support, and caregiving burden. Psychosomatics 2005;46:123–30. [DOI] [PubMed] [Google Scholar]
- 12.Kurtz ME, Kurtz J, Given CW, Given B. Relationship of caregiver reactions and depression to cancer patients’ symptoms, functional states and depression—a longitudinal view. Social Science & Medicine 1995;40:837–46. [DOI] [PubMed] [Google Scholar]
- 13.Drinka TJ, Smith JC, Drinka PJ. Correlates of depression and burden for informal caregivers of patients in a geriatrics referral clinic. Journal of the American Geriatrics Society 1987;35:522–5. [DOI] [PubMed] [Google Scholar]
- 14.Gallagher D, Rose J, Rivera P, Lovett S, Thompson LW. Prevalence of depression in family caregivers. The Gerontologist 1989;29:449–56. [DOI] [PubMed] [Google Scholar]
- 15.Mystakidou K, Tsilika E, Parpa E, Galanos A, Vlahos L. Caregivers of advanced cancer patients: feelings of hopelessness and depression. Cancer Nursing 2007;30:412–8. [DOI] [PubMed] [Google Scholar]
- 16.Nijboer C, Tempelaar R, Triemstra M, van den Bos GA, Sanderman R. The role of social and psychologic resources in caregiving of cancer patients. Cancer 2001;91:1029–39. [PubMed] [Google Scholar]
- 17.Geng HM1CD, Yang F1, Yang Y1, Liu WM1, Liu LH3, Tian HM3. Prevalence and determinants of depression in caregivers of cancer patients: A systematic reviewand meta-analysis. Medicine 2018;87:e11863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim Y, Shaffer KM, Carver CS, Cannady RSJJoc, psychology c. Prevalence and predictors of depressive symptoms among cancer caregivers 5 years after the relative’s cancer diagnosis. Journal of Consulting and Clinical Psychology. 2014;82:1. [DOI] [PubMed] [Google Scholar]
- 19.Son J, Erno A, Shea DG, et al. The caregiver stress process and health outcomes. Journal of Aging and Health 2007;19:871–87. [DOI] [PubMed] [Google Scholar]
- 20.Kim Y, Schulz RJJoA, Health. Family caregivers’ strains: comparative analysis of cancer caregiving with dementia, diabetes, and frail elderly caregiving. Journal of Aging and Health 2008;20:483–503. [DOI] [PubMed] [Google Scholar]
- 21.Tang ST, Huang GH, Wei YC, Chang WC, Chen JS, & Chou WC Trajectories of caregiver depressive symptoms while providing end‐of‐life care. Psycho‐Oncology, 2013;22:2702–10. [DOI] [PubMed] [Google Scholar]
- 22.Rottmann N, Hansen DG Hagedoorn M, Larsen PV, Nicolaisen A, Bidstrup PE,… & Johansen C Depressive symptom trajectories in women affected by breast cancer and their male partners: a nationwide prospective cohort study. Journal of Cancer Survivorship 2016;10:915–26. [DOI] [PubMed] [Google Scholar]
- 23.Price MA, Butow PN, Costa DS, et al. Prevalence and predictors of anxiety and depression in women with invasive ovarian cancer and their caregivers. Medical Journal of Australia 2010;193:S52. [DOI] [PubMed] [Google Scholar]
- 24.Carter PA, Chang BLJCn. Sleep and depression in cancer caregivers. Cancer Nursing 2000;23:410–5. [DOI] [PubMed] [Google Scholar]
- 25.Gaugler JE, Hanna N, Linder J, et al. Cancer caregiving and subjective stress: a multi‐site, multi‐dimensional analysis. Psycho‐Oncology 2005;14:771–85. [DOI] [PubMed] [Google Scholar]
- 26.Bevans M, Sternberg EM. Caregiving burden, stress, and health effects among family caregivers of adult cancer patients. Jama 2012;307:398–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Given B, Wyatt G, Given C, Gift A Sherwood P, DeVoss D, & Rahbar M Burden and depression among caregivers of patients with cancer at the end-of-life. In Oncology nursing forum 2004;31:1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kurtz ME, Kurtz JC, Given CW, Given B. Relationship of caregiver reactions and depression to cancer patients’ symptoms, functional states and depression: A longitudinal view. Social Science & Medicine 1995;40:837–46. [DOI] [PubMed] [Google Scholar]
- 29.Chen ML, Chu L, & Chen HC. Impact of cancer patients’ quality of life on that of spouse caregivers. Supportive Care in Cancer. 2004;12:469–75. [DOI] [PubMed] [Google Scholar]
- 30.Chen ML, Chu L, Chen HC. Impact of cancer patients’ quality of life on that of spouse caregivers. Support Care Cancer. 2004;12:469–75. [DOI] [PubMed] [Google Scholar]
- 31.Steel J, Geller DA, Tsung A, et al. Randomized controlled trial of a collaborative care intervention to manage cancer-related symptoms: lessons learned. Clinical Trials 2011;8:298–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Weitzner MA, Jacobsen P, Wagner H, Friedland J, Cox C. The Caregiver Quality of Life Index–Cancer (CQOLC) scale: development and validation of an instrument to measure quality of life of the family caregiver of patients with cancer. Quality of Life Research 1999;8:55–63. [DOI] [PubMed] [Google Scholar]
- 33.Weitzner MA, McMillan SC, Jacobsen PB. Family caregiver quality of life: differences between curative and palliative cancer treatment settings. J Pain Symptom Manage 1999;17:418–28. [DOI] [PubMed] [Google Scholar]
- 34.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement 1977;1:385–401. [Google Scholar]
- 35.Hann D, Winter K, Jacobsen P. Measurement of depressive symptoms in cancer patients: evaluation of the Center for Epidemiological Studies Depression Scale (CES-D). Journal of Psychosomatic Research 1999;46:437–43. [DOI] [PubMed] [Google Scholar]
- 36.Cella DF, Tulsky DS, Gray G, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. Journal of clinical oncology 1993;11:570–9. [DOI] [PubMed] [Google Scholar]
- 37.Luckett T, King M, Butow P, et al. Choosing between the EORTC QLQ-C30 and FACT-G for measuring health-related quality of life in cancer clinical research: issues, evidence and recommendations. Annals of Oncology 2011;22:2179–90. [DOI] [PubMed] [Google Scholar]
- 38.Cella D, Butt Z, Kindler HL, et al. Validity of the FACT Hepatobiliary (FACT-Hep) questionnaire for assessing disease-related symptoms and health-related quality of life in patients with metastatic pancreatic cancer. Quality of Life Research 2013;22:1105–12. [DOI] [PubMed] [Google Scholar]
- 39.Nagin D, Tremblay RE. Trajectories of boys’ physical aggression, opposition, and hyperactivity on the path to physically violent and nonviolent juvenile delinquency. Child Development 1999;70:1181–96. [DOI] [PubMed] [Google Scholar]
- 40.Giese-Davis J, Hermanson K, Koopman C, Weibel D, Spiegel D. Quality of couples’ relationship and adjustment to metastatic breast cancer. Journal of Family Psychology 2000;14:251. [DOI] [PubMed] [Google Scholar]
- 41.Schulz R, Williamson GM. A 2-year longitudinal study of depression among Alzheimer’s caregivers. Psychology and Aging 1991;6:569. [DOI] [PubMed] [Google Scholar]
- 42.Sherwood PR, Given CW, Given BA, Von Eye A. Caregiver burden and depressive symptoms: Analysis of common outcomes in caregivers of elderly patients. Journal of Aging and Health 2005;17:125–47. [DOI] [PubMed] [Google Scholar]
- 43.Hu C, Kung S, Rummans TA, Clark MM, & Lapid MI. Reducing caregiver stress with internet-based interventions: a systematic review of open-label and randomized controlled trials. Journal of the American Medical Informatics Association 2015;22:e194–e209. [DOI] [PubMed] [Google Scholar]
- 44.Walker RJ, Pomeroy EC. Depression or grief? The experience of caregivers of people with dementia. Health & Social Work 1996;21:247–54. [DOI] [PubMed] [Google Scholar]
- 45.Meichsner F, & Wilz G. Dementia caregivers’ coping with pre-death grief: effects of a CBT-based intervention. Aging & mental health, 2018;22: 218–25. [DOI] [PubMed] [Google Scholar]
- 46.Fu F, Zhao H, Tong F, & Chi I A systematic review of psychosocial interventions to cancer caregivers. Frontiers in Psychology 2017;8:834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lafaye A, Sylvie Petit, Pierre Richaud, Nadine Houédé, Fanny Baguet, & Florence CoussonGeille. Dyadic effects of coping strategies on emotional state and quality of life in prostate cancer patients and their spouses. Psycho-Oncology 2014;23:797–803. [DOI] [PubMed] [Google Scholar]
- 48.Badr H, Krebs P. A systematic review and meta‐analysis of psychosocial interventions for couples coping with cancer. Psycho‐Oncology 2013;22:1688–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Badr H, Smith CB, Goldstein NE, Gomez JE, & Redd WH Dyadic psychosocial intervention for advanced lung cancer patients and their family caregivers: results of a randomized pilot trial. Cancer 2015;121:150–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.von Heymann-Horan A, Bidstrup P, Guldin MB, Sjøgren P, Andersen EAW, von der Maase H, … & , Johansen C Effect of home-based specialised palliative care and dyadic psychological intervention on caregiver anxiety and depression: A randomised controlled trial. British Journal of Cancer, 2018;119:1307. [DOI] [PMC free article] [PubMed] [Google Scholar]


