Abstract
Introduction:
Special populations, including veterans, pregnant/postpartum women, and adolescents, benefit from opioid use disorder treatment tailored to their specific needs, but access to such services is poorly described. This study identifies the availability of opioid use disorder treatment facilities that use medications and have special programming, and contextualizes facilities amid counties’ opioid-related overdose mortality.
Methods:
Data were compiled on 15,945 U.S. treatment facilities using medications for opioid use disorder listed in the Behavioral Health Services Treatment Locator in 2018. Facilities with programs tailored to special populations (veterans, pregnant/postpartum women, and adolescents) were identified and geocoded. Counties with such facilities were characterized. “Cold spots” (county clusters with poor treatment availability) were identified using Getis–Ord Gi* statistics. Data were extracted in October 2018 and analyzed October 2018–May 2019.
Results:
Of all 3,142 U.S. counties, 1,889 (60.1%) had opioid use disorder treatment facilities. Facilities with tailored programs for veterans, pregnant/postpartum women, and adolescents were located in 701 (22.3%), 918 (29.2%), and 1,062 (33.8%) of counties, respectively. Specific medications provided for opioid use disorder varied, with only a minority of facilities offering methadone (among facilities with tailored programs for veterans, 6.0%; pregnant/postpartum women, 13.2%; adolescents, 1.3%). Many counties reporting opioid-related overdose deaths lacked programs for special populations (veterans, 72.6%; pregnant/postpartum women, 54.8%; adolescents, 30.6%). Cold spots were located throughout the Midwest, U.S. Southeast, and portions of Texas.
Conclusions:
Facilities using medications for opioid use disorder with tailored programs for veterans, pregnant/postpartum women, and adolescents are limited. There is need for improved access to evidence-based programs that address the unique treatment needs of special populations.
INTRODUCTION
To combat the high mortality attributable to opioid use disorder (OUD), ensuring access to evidence-based treatment has become a national priority in the U.S.1 However, there is a well-described treatment gap in which few individuals with OUD receive standard-of-care pharmacotherapy with buprenorphine, naltrexone, or methadone.2 A central reason is that many regions, particularly rural areas, lack OUD treatment facilities that offer or allow pharmacotherapy.3
There are reasons to expect that this gap may be even larger for special populations—namely veterans, pregnant and postpartum women, and adolescents—as these three populations have special considerations when treating OUD. For example, veterans with OUD have an elevated prevalence of post-traumatic stress disorder.4 Although most veterans can attend any OUD treatment facility, they may be more likely to achieve recovery if they receive trauma-informed care.5 Pregnant and postpartum women with OUD require careful monitoring owing to changes in dose requirements for buprenorphine and methadone and also benefit from support in their transition to parenthood.6 Pregnant and postpartum women may therefore be more likely to achieve recovery through specialized programming.6,7 Adolescents with OUD require developmentally appropriate care, particularly in relation to consent and confidentiality.8 Data suggest that young people may have better treatment outcomes when they receive care separate from adults.9
This study of U.S. counties aims to determine the availability of OUD treatment facilities that provide or allow medications for veterans, pregnant and postpartum women, and adolescents, and to contextualize the availability of OUD treatment facilities in relation to local opioid-related overdose mortality.
METHODS
The study was approved by the New York University School of Medicine IRB and followed the STROBE reporting guideline.9 Data were extracted in 2018 and analyzed in 2018–2019.
Study Sample
County-level information on substance use disorder treatment facilities and opioid-related overdoses was linked using data from the Substance Abuse and Mental Health Services Administration Behavioral Health Treatment Locator and the Centers for Disease Control and Prevention, respectively. All U.S. counties and county equivalents (n=3,142) were eligible for inclusion.
Publicly available data on 15,945 public and private treatment facilities were compiled from the Behavioral Health Treatment Locator, a publicly accessible online database.10 Information for this database is sourced from the National Survey of Substance Abuse Treatment Services, an annual census performed by the Substance Abuse and Mental Health Services Administration that compiles data on facilities operated by nonprofit and for-profit organizations, hospital-based programs, group practices, federal agencies (including the Department of Veterans Affairs and Indian Health Services), and local governmental organizations such as health departments. The Treatment Locator is updated at least monthly to incorporate new programs and update addresses. Treatment facilities are otherwise updated annually in March using data from the most recent National Survey of Substance Abuse Treatment Services. Treatment facilities used in analyses completed the 2017 National Survey of Substance Abuse Treatment Services questionnaire or were added in 2018.
Data were extracted October 2018 and included all entries classified as “Substance Use” facilities. For each facility, data were compiled on service location, information on special populations served, medications offered, forms of payment accepted, levels of addiction care provided, and services in Spanish. Each facility was geocoded in ArcGIS to determine its county. The sample was restricted to substance use treatment facilities that treat OUD and provide medications (i.e., buprenorphine, naltrexone, or methadone) or allow medications prescribed by an outside clinician or facility. Facilities were not included if they only provided buprenorphine or methadone for detoxification, as this did not represent longitudinal treatment of OUD. Facilities reporting that they had programs specifically tailored to veterans, pregnant and postpartum women, and adolescents were then identified.
As an indicator of likely need for OUD treatment services, county-level data were extracted on opioid-related overdose deaths in 2014–2016 from the Centers for Disease Control and Prevention and were aggregated to produce stable estimates.11 Using the ICD-10 underlying cause-of-death codes, overdose deaths related to intentional and unintentional underlying causes of death (X40–X44, X60–X64, and Y10–Y14) involving any opioid (T40.0–T40.4 and T40.6) were identified.
Measures
The primary outcome was number of OUD treatment facilities providing or allowing medications per capita in a given county. The number of facilities offering programs tailored to veterans, pregnant and postpartum women, and adolescents was enumerated. When examining all OUD treatment facilities, the denominator for per capita estimates was the county-level population of all individuals aged ≥11 years. When examining programs for veterans, the denominator was the county population of veterans; for pregnant and postpartum women, all women aged 15–44 years; and for adolescents, all individuals aged 11–17 years.11–13
A ratio was developed for each county as a measure of the availability of OUD treatment facilities in relation to opioid overdose mortality rates. This measure was calculated as the number of facilities per capita divided by the opioid-related overdose mortality rate per 100,000 people. In determining overdose deaths in the entire population, all fatalities involving individuals aged ≥11 years were included; in veterans, all individuals aged ≥18 years; in pregnant and postpartum women, all women aged 15–44 years; and in adolescents, all individuals aged 11–17 years. Counties not reporting any opioid-related overdose deaths overall or for specific populations were excluded from the relevant measure and analyses involving this measure (overall, 405 [12.9%]; veterans, 647 [20.6%]; pregnant and postpartum women, 1,380 [43.9%]; adolescents, 2,554 [81.3%]).
County-level covariates included sociodemographic characteristics (percentage composition according to sex, age, race/ethnicity, unemployment, poverty, any health insurance coverage, and receipt of public health insurance using U.S. Census Bureau American Community Survey 5-year estimates from 2012 to 2016), 2016 opioid prescribing rate from the Centers for Disease Control and Prevention, prior mean opioid-related overdose rate for 2014–2016 per 100,000 people, National Center for Health Statistics rural/urban classification, U.S. Census Bureau division, and designation as a medically underserved area.13–16 In the National Center for Health Statistics classification, large central metro, large fringe metro, medium metro, and small metro counties are considered urban (n=1,167; 37.1% of all counties); and micropolitan and non-core counties are considered rural (n=1,976; 62.9%).13 Medically underserved areas are designated by the Health Resources and Services Administration as areas with insufficient primary care providers, high infant mortality, high poverty, a high percentage of the population that is elderly, or a combination of these.16
Statistical Analysis
Maps were generated with quartiles ranking counties’ total number of facilities per capita, as well as the number of facilities per capita with programs for veterans, pregnant and postpartum women, and adolescents. Descriptive statistics characterized treatment facilities based on forms of payment accepted, levels of addiction care provided, services in Spanish, and medications provided on-site for OUD treatment.
To identify county characteristics associated with OUD treatment facility availability, generalized estimating equations analyses were used with a robust Poisson distribution, exchangeable correlation structure of clusters at the state level, and robust SEs. The dependent variable was the count of all facilities in a given county. County population size was included as an offset variable to estimate the number of facilities per capita. Offset variables are included in Poisson models to divide the count of the outcome by an exposure—in this case, by county population size. This accounted for the fact that counties with larger populations would likely have a higher count of treatment facilities. Models were repeated for the three special populations. The negative binomial likelihood model was used to assess availability of treatment facilities for pregnant and postpartum women and adolescents to address overdispersion of mortality rates. Multivariable models included all study covariates based on their established associations with treatment.2,3,17,18
Variance inflation factors were generated for covariates to identify collinearity. Only the percentages of individuals with any health insurance and receiving public health insurance had variance inflation factors >10, suggestive of collinearity. Both covariates were included because they provided unique information, and sensitivity analyses in which each variable was sequentially removed from final multivariable models did not reveal substantially different effect sizes.
Opioid prescribing rates were available for 2,962 (94.2%) counties. Multiple imputation methods were used to generate prescribing rates for missing counties. Predictive mean matching with a sequential chained equation was used to generate 20 complete data sets of county prescribing rates. All models were then repeated using the 20 complete data sets and pooled results according to Rubin’s rules.19
To examine the distribution of treatment availability in relation to need, additional maps were generated with quartiles ranking counties’ ratios of number of OUD treatment facilities per capita to their opioid overdose mortality rate. Separate maps were generated for the overall population and for veterans, pregnant and postpartum women, and adolescents. To identify global and local clusters of high or low treatment availability among neighboring counties, a first-order queen contiguity spatial weight was used to define the adjacency matrix.20 Global statistics Moran’s I and Getis–Ord General G were used to measure the correlation among neighboring counties using row standardization.21,22 Getis–Ord Gi* statistics were used to locate “cold spots” and “hot spots,”21 which represent clusters of contiguous counties that collectively had ratios of treatment facilities per capita to local overdose mortality that were below and above the national median, respectively. Counties were defined in three categories: (1) below the median ratio of treatment facilities to overdose mortality, (2) above the median ratio of treatment facilities to overdose mortality, or (3) no deaths reported during the study period. Tests were applied using a mean of 9,999 random permutations. Adolescents were omitted from analyses owing to excessive variation in the ratio. The number of counties in Hawaii were insufficient to include in local indicators of spatial association analyses. Alaska was analyzed as a spatially distinct cluster of counties since it is not contiguous with other US states; however, it was compared to national medians to assess how it compared to other states.
Statistical analyses used R Studio, version 3.5 and ArcGIS, version 10.6.1. All tests were two-sided with p<0.05 indicating significance.
RESULTS
Across the U.S. in 2018, there were 9,920 OUD treatment facilities that indicated that they provided or allowed medications. Of these, 5,603 (56.5%) provided medications and 4,317 (43.5%) facilities did not provide medications but allowed patients to be on them if provided by an outside prescriber or facility. Of the 5,603 facilities providing medications, 4,202 (75.0%) offered buprenorphine, 4,054 (72.4%) offered naltrexone, and 1,347 (24.0%) offered methadone.
The OUD treatment facilities were located in 1,889 (60.1%) of 3,142 U.S. counties or county equivalents (Appendix Figure 1). Among the 9,920 facilities, 1,894 (19.1%) had programs tailored for veterans, 2,577 (26.0%) for pregnant and postpartum women, and 2,285 (23.0%), for adolescents.
Facilities with tailored programs for veterans, pregnant and postpartum women, and adolescents were located in 701 (22.3%), 918 (29.2%), and 1,062 (33.8%) of counties, respectively (Table 1). Buprenorphine, naltrexone, and methadone were available through facilities in 29.3%, 34.5%, and 17.5% of counties, respectively, and 36.5% of counties only had facilities that only allowed clients to be on medications if prescribed elsewhere. For veterans and adolescents, the most commonly available medication across counties was naltrexone (13.5% and 16.3%, respectively). However, for adolescents, it was more common to require receipt of medications from an outside prescriber or facility (23.6% of counties). For pregnant and postpartum women, the most commonly available medication was buprenorphine (17.0%). For all three special populations, methadone was the least available medication across counties (veterans, 6.0%; pregnant and postpartum women, 13.2%; adolescents, 1.3%). Overall, a majority of counties with OUD treatment facilities had programs that accepted Medicaid (55.9%), private health insurance (55.6%), or cash or self-payment (59.3%). Less than half of counties had facilities that accepted other state-financed health insurance or TRICARE for veterans (49.6%), or offered assistive or sliding scale payments (45.6%). A majority of counties had facilities offering outpatient treatment (59.0%); less than half had facilities providing opioid detoxification (23.3%), inpatient care (10.2%), or residential care (23.8%). Overall, 18.6% of counties had facilities with services in Spanish, and counties with the greatest share of services were located in coastal census divisions and large central metropolitan regions (Appendix Table 1).
Table 1.
Characteristics of Counties With Opioid Use Disorder Treatment Programs That Provide or Allow Medications (n=3,142)
| Percentage of counties with program | ||||
|---|---|---|---|---|
| Characteristics | Any program | Programs for veterans | Programs for pregnant and postpartum women | Programs for adolescents |
| % (n) | % (n) | % (n) | % (n) | |
| Total | 60.1 (1,889) | 22.3 (701) | 29.2 (918) | 33.8 (1,062) |
| Medications provided on-site | ||||
| Buprenorphinea | 29.3 (920) | 12.2 (382) | 17.0 (534) | 11.8 (371) |
| Naltrexone | 34.5 (1,083) | 13.5 (423) | 16.0 (504) | 16.3 (512) |
| Methadonea | 17.5 (550) | 6.0 (188) | 13.2 (415) | 1.3 (40) |
| Allows medications but must be provided by outside prescriber/facility | 36.5 (1,147) | 12.7 (399) | 15.9 (499) | 23.6 (742) |
| Payments accepted | ||||
| Medicaid | 55.9 (1,755) | 17.5 (550) | 25.3 (795) | 31.3 (985) |
| Other state-financed insurance or TRICARE for veterans | 49.6 (1,557) | 14.5 (455) | 21.1 (662) | 26.7 (839) |
| Private health insurance | 55.6 (1,747) | 19.4 (609) | 24.7 (775) | 31.0 (974) |
| Cash/Self-payment | 59.3 (1,864) | 21.2 (666) | 28.8 (904) | 33.1 (1,039) |
| Sliding scale available | 45.6 (1,432) | 14.2 (445) | 19.5 (613) | 25.0 (784) |
| Levels of addiction care | ||||
| Opioid detoxification | 23.3 (733) | 9.8 (307) | 12.0 (378) | 7.2 (225) |
| Inpatient | 10.2 (321) | 3.8 (118) | 2.5 (77) | 2.5 (80) |
| Residential | 23.8 (748) | 9.3 (292) | 10.5 (331) | 5.4 (170) |
| Outpatient | 59.0 (1,855) | 20.6 (648) | 27.6 (868) | 33.4 (1,048) |
| Treatment in Spanish | 18.6 (585) | 8.0 (252) | 10.6 (333) | 11.0 (347) |
Excludes buprenorphine or methadone used only in detoxification.
In multivariable analyses, relative to counties in New England, counties in the Middle Atlantic, East North Central, South Atlantic, East South Central, West South Central, and Pacific census divisions were significantly less likely to have any OUD treatment facility (Table 2; univariate results in Appendix Table 2). Availability of facilities with programs tailored to veterans, and pregnant and postpartum women varied significantly, with all census divisions exhibiting significantly poorer availability of facilities than New England. Availability of facilities with programs tailored to adolescents were significantly more common in the Middle Atlantic and Mountain census divisions than in New England. Availability of facilities with programs tailored for adolescents were also significantly more common in large fringe metro, medium metro, small metro, micropolitan, and non-core counties relative to large central metro counties.
Table 2.
County-level Characteristics Associated With Availability of Opioid Use Disorder Treatment Facilities That Provide or Allow Medications, Multivariable Analyses (n=3,142)
| Characteristic | Any program | Programs for veterans | Programs for pregnant and postpartum women | Programs that accept adolescents |
|---|---|---|---|---|
| Adjusted RR (95% CI)a | Adjusted RR (95% CI)a | Adjusted RR (95% CI)a | Adjusted RR (95% CI)a | |
| % male | 1.00 (1.00, 1.01)** | 0.99 (0.99, 1.00)* | 0.99 (0.95, 1.04) | 1.01 (0.95, 1.07) |
| Age distribution, years | ||||
| % age 0–19 | ref | ref | ref | ref |
| % age 20–24 | 0.87 (0.79, 0.96)** | 0.89 (0.69, 1.15) | 1.03 (0.90, 1.18) | 1.02 (0.86, 1.22) |
| % age 25–44 | 1.01 (0.99, 1.03) | 1.04 (0.99, 1.08) | 1.01 (0.98, 1.04) | 0.96 (0.94, 0.99)** |
| % age 45–64 | 1.02 (0.98, 1.06) | 1.05 (0.96, 1.15) | 1.03 (0.98, 1.08) | 1.04 (1.00, 1.07)* |
| % age ≥65 | 0.97 (0.94, 0.99)** | 0.98 (0.93, 1.04) | 1.01 (0.96, 1.05) | 0.99 (0.96, 1.03) |
| % non-Hispanic white | 1.00 (1.00, 1.01) | 0.99 (0.98, 1.00)* | 1.00 (0.99, 1.01) | 1.00 (0.99, 1.01) |
| % unemployed | 1.00 (0.98, 1.01) | 1.00 (0.98, 1.02) | 0.99 (0.99, 1.01) | 0.99 (0.98, 1.01) |
| % living in poverty | 1.01 (0.99, 1.02) | 1.03 (1.01, 1.06)** | 1.03 (1.01, 1.05)** | 1.02 (1.01, 1.04)** |
| % uninsured | 0.98 (0.96, 1.01) | 1.00 (0.97, 1.02) | 0.98 (0.96, 1.02) | 0.98 (0.96, 1.01) |
| % with public health insurance | 1.02 (1.00, 1.03) | 1.00 (0.97, 1.02) | 1.02 (1.00, 1.04) | 1.01 (0.99, 1.02) |
| U.S. Census Bureau division | ||||
| New England | ref | ref | ref | ref |
| Middle Atlantic | 0.69 (0.58, 0.83)*** | 0.70 (0.48, 1.01) | 0.57 (0.47, 0.70)*** | 1.52 (1.13, 2.04)** |
| East North Central | 0.57 (0.45, 0.72)*** | 0.36 (0.24, 0.52)*** | 0.36 (0.30, 0.44)*** | 0.91 (0.64, 1.31) |
| West North Central | 0.77 (0.54, 1.11) | 0.56 (0.33, 0.94)* | 0.63 (0.40, 0.99)* | 1.39 (0.90, 2.14) |
| South Atlantic | 0.58 (0.35, 0.96)* | 0.34 (0.18, 0.64)*** | 0.55 (0.36, 0.85)** | 0.84 (0.48, 1.44) |
| East South Central | 0.53 (0.33, 0.84)** | 0.34 (0.16, 0.72)** | 0.41 (0.26, 0.63)*** | 0.86 (0.48, 1.54) |
| West South Central | 0.37 (0.25, 0.55)*** | 0.20 (0.09, 0.42)*** | 0.29 (0.20, 0.43)*** | 0.64 (0.40, 1.02) |
| Mountain | 0.75 (0.48, 1.18) | 0.69 (0.46, 1.03) | 0.60 (0.41, 0.87)** | 1.43 (1.02, 2.00)* |
| Pacific | 0.59 (0.41, 0.84)** | 0.46 (0.35, 0.61)*** | 0.58 (0.46, 0.73)*** | 0.89 (0.51, 1.56) |
| Rural/Urban classification | ||||
| Large central metro | ref | ref | ref | ref |
| Large fringe metro | 0.95 (0.74, 1.21) | 0.84 (0.60, 1.19) | 0.88 (0.73, 1.05) | 1.18 (0.96, 1.45) |
| Medium metro | 1.06 (0.87, 1.28) | 0.93 (0.72, 1.20) | 1.04 (0.88, 1.23) | 1.32 (1.10, 1.59)** |
| Small metro | 1.10 (0.90, 1.34) | 0.93 (0.71, 1.23) | 1.19 (0.96, 1.47) | 1.70 (1.44, 2.00)*** |
| Micropolitan | 1.25 (1.00, 1.56) | 1.02 (0.73, 1.42) | 1.17 (0.94, 1.46) | 2.09 (1.67, 2.62)*** |
| Noncore | 1.24 (0.91, 1.68) | 0.85 (0.61, 1.19) | 1.08 (0.82, 1.43) | 2.13 (1.68, 2.71)*** |
| Medically underserved area | 0.95 (0.81, 1.13) | 0.90 (0.67, 1.22) | 0.88 (0.75, 1.04) | 0.94 (0.69, 1.28) |
| Opioid prescriptions rate per 100b | 1.00 (1.00, 1.01) | 1.00 (1.00, 1.01) | 1.00 (1.00, 1.01) | 1.00 (0.99 1.00) |
| Opioid overdose rate per 100,000c | 1.00 (1.00, 1.00)* | 1.00 (1.00, 1.00)* | 1.00 (1.00, 1.01)*** | 1.00 (0.99, 1.01) |
Boldface indicates statistical significance (*p<0.05; **p<0.01; ***p<0.001). Analyses are adjusted for all variables listed in the table.
180 counties excluded from analyses due to missing data.
Mean rate for the period 2014–2016.
There was substantial heterogeneity in counties’ availability of facilities in relation to opioid-related overdose mortality (Figure 1). Overall, 959 (35.0%) counties reporting opioid-related overdose deaths had no facilities providing or allowing OUD medications, although many were near other counties in which services were available. With regard to programs tailored to veterans, 1,812 (72.6%) counties with opioid-related overdose deaths had no facilities offering such programming; pregnant and postpartum women, 966 (54.8%) counties; and adolescents, 180 (30.6%) counties.
Figure 1. Per capita availability of opioid use disorder treatment facilities in relation to county opioid overdose mortality.
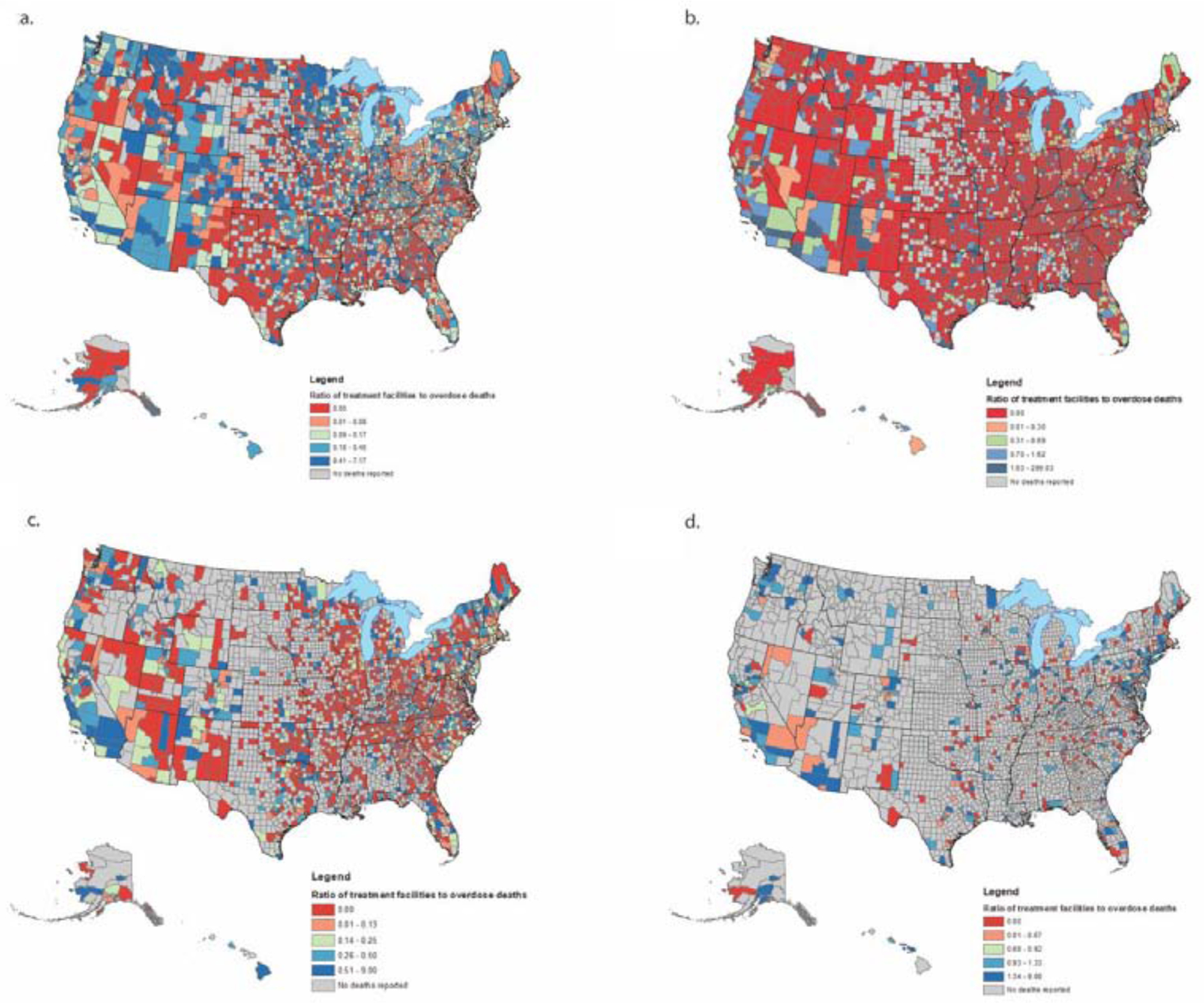
(A) Any facilitya; (B) Facilities offering programs for veteransb; (C) Facilities offering programs for pregnant and postpartum womenc; (D) Facilities offering programs for adolescents or accepting adolescent into other programs.d
aFacilities and mortality rates per 100,000 individuals aged ≥11 years.
bFacilities and mortality rates per 100,000 veterans.
cFacilities and mortality rates per 100,000 women aged 15–44 years.
dFacilities and mortality rates per 100,000 individuals aged 11–17 years.
In considering all treatment facilities, “cold spots” (clusters of counties with poor availability of treatment facilities in relation to overdose mortality) were located throughout the Midwest, U.S. Southeast, and portions of Texas (n=502 counties) (Figure 2). With regard to facilities for veterans, cold spots were observed in the Midwest, portions of Texas, and southern states including Alabama and Louisiana (n=466); hot spots were identified in the West, Northeast, and Florida (n=449). For pregnant and postpartum women, cold spots were located in the Midwest, portions of Texas, and parts of the Southeast (n=620 counties); hot spots were observed in the Northeast, West, North Carolina, and Florida (n=563 counties).
Figure 2. Getis-Ord Gi* cluster detection of ‘cold’ and ‘hot spots’a for treatment availability in relation to county opioid overdose mortality.
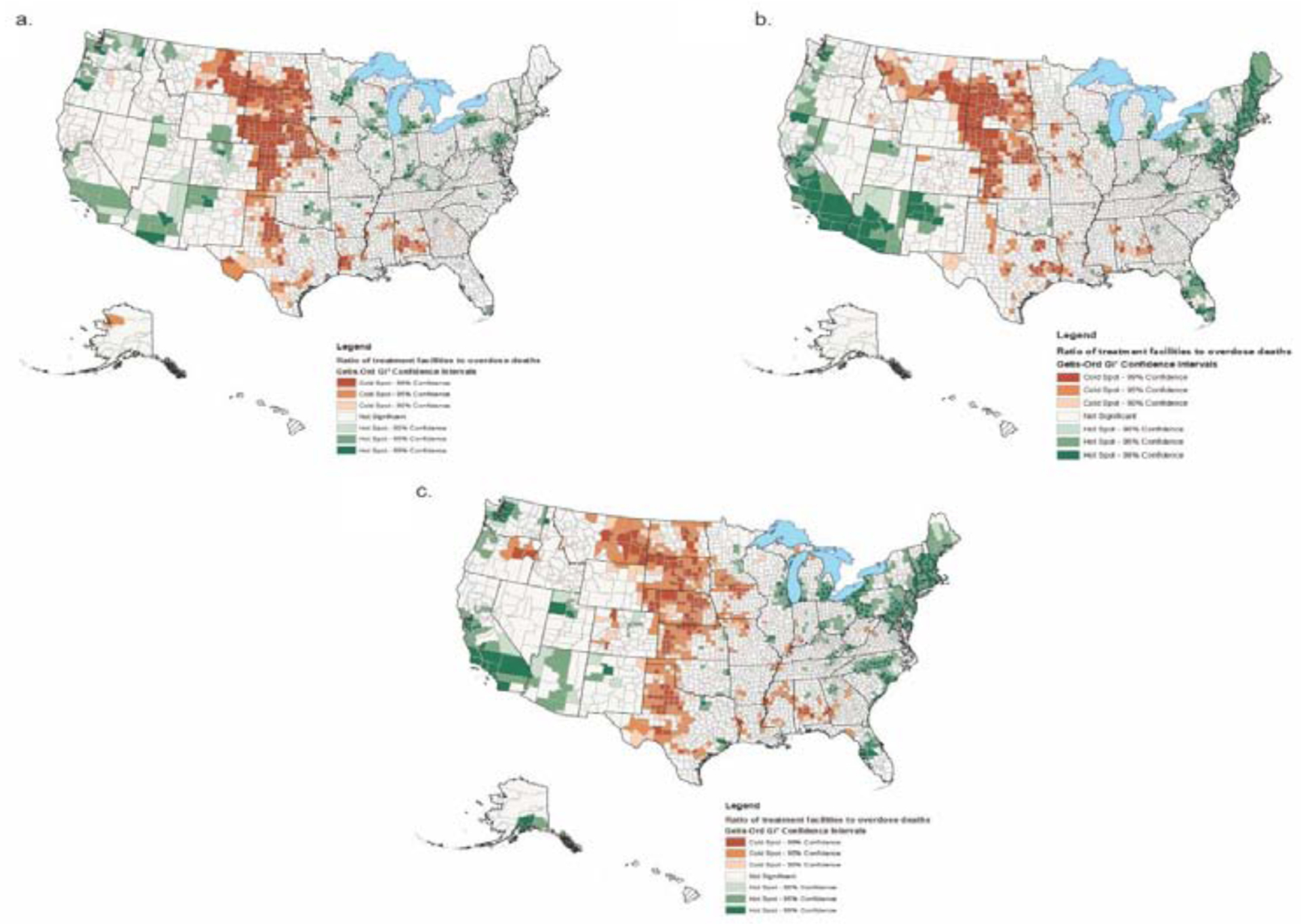
(A) Any facilityb; (B) Facilities offering programs for veteransc; (C) Facilities offering programs for pregnant and postpartum women.d
a’Cold’ and ‘hot spots’ are clusters of contiguous counties that collectively had ratios of treatment facilities per capita to local overdose mortality below and above the national median, respectively.
bFacilities and mortality rates per 100,000 individuals aged ≥11 years.
cFacilities and mortality rates per 100,000 veterans.
dFacilities and mortality rates per 100,000 women aged 15–44 years.
DISCUSSION
In this national study of OUD treatment facilities, only 60% of all counties had facilities that provide or allow buprenorphine, naltrexone, or methadone. Facilities with programs specifically tailored for veterans were available in approximately one in five counties; for pregnant and postpartum women, in under one in three counties; and for adolescents, in approximately one in three counties. Significant “cold spots”—contiguous counties with poor treatment availability in relation to their opioid-related overdose mortality—were identified throughout the U.S.
Although access to OUD treatment for the general population is lacking,2 these findings indicate that special populations may face even greater difficulty in accessing care tailored to their needs. This treatment gap is detrimental, as veterans with OUD frequently require trauma-informed care and management of post-traumatic stress disorder, pregnant and postpartum women have unique medication dosing concerns and should receive support in their transition to parenthood, and adolescents benefit from developmentally appropriate care.5,8,23 This gap suggests that individuals from these special populations may be receiving care in facilities without group-specific expertise, or that they may be traveling large distances for care.
This treatment gap is consistent with that described in other studies. Although this study only examined addiction treatment facilities, data suggest that many of the same counties that lacked services in this study also lack office-based addiction treatment, particularly in rural areas. For example, the “cold spots” the present study identified in the Midwest and Texas also lacked buprenorphine-waivered clinicians in another recent national study.24 Further, although Veterans Health Administration (VHA) facilities are 5.5 times more likely to offer medications for OUD than non-VHA facilities,25 the number of VHA facilities is limited, particularly in rural regions.26 Similarly, pregnant women seeking treatment have limited options: A recent survey of Appalachian OUD treatment programs demonstrated that only half of all buprenorphine providers were willing to accept new patients who were pregnant.7 Adolescents have minimal access to methadone due to federal regulations that prohibit its use unless they have two “failed attempts” at treatment without pharmacotherapy, and very few methadone treatment programs accept adolescents.27,28 Adolescents also have limited access to other forms of specialty addiction treatment and office-based care, with only 26% of all addiction treatment facilities offering programs for adolescents,10 and pediatricians comprising less than 1% of waivered buprenorphine providers.17 Studies have demonstrated that only a quarter of youth with an OUD diagnosis receive medication,29 and even among youth who are able to access treatment, far fewer receive medication compared with adults.30
The number of veterans who receive tailored care could be improved by efforts to better coordinate with non-VHA facilities and extend services to remote regions through hub-and-spoke models and telemedicine.18,31 For pregnant and postpartum women, possible solutions include prioritizing these clients on facilities’ waitlists, additional investment in programming for women, enacting policies that prioritize OUD treatment for pregnant women, and eliminating criminal penalties for prenatal substance use that exist in many states, as this may deter facilities from offering special programming.7,31–33 Adolescents’ access to treatment could be greatly broadened by eliminating “fail-first” methadone requirements and disseminating clinical recommendations that OUD medications be used more routinely.8,34
Limitations
This study has limitations. First, the study did not differentiate among facilities with high and low client volume. Some VHA facilities and certified opioid treatment programs, for example, may be rarer across counties but able to provide services to a large number of individuals. Other facilities might have been under-resourced to provide their stated services. Second, results may have been affected by the modifiable areal unit problem—that is, that the measures included in this study are affected by the geographical boundaries imposed by county lines. Third, associations described in the study are ecological and cannot be fully generalized to individuals within counties. Fourth, treatment occurring in office-based settings outside dedicated addiction treatment facilities was not examined.
CONCLUSIONS
Amid a national addiction treatment gap, these results suggest that access to facilities using OUD medications and offering tailored care for veterans, pregnant and postpartum women, and adolescents is limited. Clear treatment gaps exist across contiguous counties in the U.S., and these findings inform where new treatment facilities may be needed. A national strategy to address overdoses should include expansion of tailored treatment programs that comprehensively address the unique treatment considerations for these special populations.
Supplementary Material
ACKNOWLEDGMENTS
Ms. Jent and Dr. Cerdá had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Dr. Hadland is supported by K23DA045085 (NIH/National Institute on Drug Abuse [NIDA]), L40DA042434 (NIH/NIDA), Early Career Award (Thrasher Research Fund), and Young Investigator Award (Academic Pediatric Association). Dr. Cerdá and Ms. Jent are supported by R01DA039962 (NIH/NIDA) and by funding provided by NYU Langone Health for the NYU Center for Opioid Epidemiology and Policy. Dr. Marshall is supported in part by the National Institute of General Medical Sciences (P20GM125507). Dr. Mauro is supported by K01DA045224 (NIH/NIDA).
SEH, VAJ, RAH, BDLM, and MC designed the study. SEH, VAJ, and MC wrote the protocol. SEH conducted the literature review and wrote the first draft of the manuscript. VAJ and MC undertook data management and statistical analyses with additional input from SEH. All authors contributed to and have approved the final manuscript.
No financial disclosures were reported by the authors of this paper. No funders had any role in the design or analysis of the study, the interpretation of findings, or the decision to publish the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Hedegaard H, Mininño A, Warner M, et al. Drug overdose deaths in the United States, 1999–2017. NCHS Data Brief. 2018;(329):1–8. [PubMed] [Google Scholar]
- 2.Mojtabai R, Mauro C, Wall MM, Barry CL, Olfson M. Medication treatment for opioid use disorders in substance use treatment facilities. Health Aff (Millwood). 2019;38(1):14–23. 10.1377/hlthaff.2018.05162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dick AW, Pacula RL, Gordon AJ, et al. Growth in buprenorphine waivers for physicians increased potential access to opioid agonist treatment, 2002–11. Health Aff (Millwood). 2015;34(6):1028–1034. 10.1377/hlthaff.2014.1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seal KH, Shi Y, Cohen G, et al. Association of mental health disorders with prescription opioids and high-risk opioid use in US veterans of Iraq and Afghanistan. JAMA. 2012;307(9):940–947. 10.1001/jama.2012.234. [DOI] [PubMed] [Google Scholar]
- 5.Fareed A, Eilender P, Haber M, Bremner J, Whitfield N, Drexler K. Comorbid posttraumatic stress disorder and opiate addiction: a literature review. J Addict Dis. 2013;32(2):168–179. 10.1080/10550887.2013.795467. [DOI] [PubMed] [Google Scholar]
- 6.American College of Obstetricians and Gynecologists, American Society of Addiction Medicine. Opioid Use and Opioid Use Disorder in Pregnancy. Washington, DC: American College of Obstetricians and Gynecologists; 2017. [Google Scholar]
- 7.Patrick SW, Buntin MB, Martin PR, et al. Barriers to accessing treatment for pregnant women with opioid use disorder in Appalachian states. Subst Abus. 2019;40(3):356–362. 10.1080/08897077.2018.1488336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Committee on Substance Use and Prevention. Medication-assisted treatment of adolescents with opioid use disorders. Pediatrics. 2016;138(3):e20161893 10.1542/peds.2016-1893. [DOI] [PubMed] [Google Scholar]
- 9.Schuman-Olivier Z, Weiss RD, Hoeppner BB, Borodovsky J, Albanese MJ. Emerging adult age status predicts poor buprenorphine treatment retention. J Subst Abuse Treat. 2016;47(3):202–212. 10.1016/j.jsat.2014.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Substance Abuse and Mental Health Services Administration. SAMHSA Behavioral Health Treatment Services Locator. https://findtreatment.samhsa.gov/. Published 2018. Accessed October 5, 2018.
- 11.CDC. Wide-Ranging Online Data for Epidemiologic Research (WONDER). Atlanta, GA: HHS, CDC, National Center for Health Statistics; 2018. https://wonder.cdc.gov/. Published 2018. Accessed October 5, 2018. [Google Scholar]
- 12.National Center for Veterans Analysis and Statistics. Veteran Population Table. Washington, DC: U.S. Department of Veterans Affairs; 2018. www.va.gov/vetdata/veteran_population.asp. Accessed October 22, 2018. [Google Scholar]
- 13.Social Explorer. US Census Bureau American Community Survey 2012–2016 5-Year Estimates. www.socialexplorer.com. Published 2018. Accessed October 1, 2018. [Google Scholar]
- 14.CDC, National Center for Health Statistics. NCHS Urban-Rural Classification Scheme for Counties. www.cdc.gov/nchs/data_access/urban_rural.htm#2013_Urban-Rural_Classification_Scheme_for_Counties. Published 2017. Accessed October 22, 2018. [Google Scholar]
- 15.CDC, National Center for Injury Prevention and Control. US County Prescribing Rate Maps. www.cdc.gov/drugoverdose/maps/rxrate-maps.html. Published 2018. Accessed October 22, 2018. [Google Scholar]
- 16.Health Resources and Services Administration. Medically Underserved Areas Find. https://data.hrsa.gov/tools/shortage-area/mua-find. Published 2018. Accessed October 2, 2018.
- 17.Rosenblatt RA, Andrilla CHA, Catlin M, Larson EH. Geographic and specialty distribution of US physicians trained to treat opioid use disorder. Ann Fam Med. 2015;13(1):23–26. 10.1370/afm.1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Valenstein-Mah H, Hagedorn H, Kay CL, Christopher ML, Gordon AJ. Underutilization of the current clinical capacity to provide buprenorphine treatment for opioid use disorders within the Veterans Health Administration. Subst Abus. 2018;39(3):286–288. 10.1080/08897077.2018.1509251. [DOI] [PubMed] [Google Scholar]
- 19.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York, NY: John Wiley & Sons, Inc.; 1987. [Google Scholar]
- 20.Zhou X, Lin H. Spatial Weights Matrix In: Shekhar S, Xiong H, eds. Encyclopedia of GIS. Boston, MA: Springer; 2008. [Google Scholar]
- 21.Getis A, Ord JK. The analysis of spatial association by use of distance statistics. Geogr Anal. 1992;24(3):189–206. 10.1111/j.1538-4632.1992.tb00261.x. [DOI] [Google Scholar]
- 22.Moran PAP. The interpretation of statistical maps. J R Stat Soc Ser B. 1948;10(2):243– 251. [Google Scholar]
- 23.Saia KA, Schiff D, Wachman EM, et al. Caring for pregnant women with opioid use disorder in the USA: expanding and improving treatment. Curr Obstet Gynecol Rep. 2016. 10.1007/s13669-016-0168-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Andrilla CHA, Moore TE, Patterson DG, Larson EH. Geographic distribution of providers with a DEA waiver to prescribe buprenorphine for the treatment of opioid use disorder: a 5-year update. J Rural Health. 2019;35(1):108–112. 10.1111/jrh.12307. [DOI] [PubMed] [Google Scholar]
- 25.Wyse JJ, Gordon AJ, Dobscha SK, et al. Medications for opioid use disorder in the Department of Veterans Affairs (VA) health care system: historical perspective, lessons learned, and next steps. Subst Abus. 2018;39(2):139–144. 10.1080/08897077.2018.1452327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cully JA, Jameson JP, Phillips LL, Kunik ME, Fortney JC. Use of psychotherapy by rural and urban veterans. J Rural Health. 2010;26(3):225–233. 10.1111/j.1748-0361.2010.00294.x. [DOI] [PubMed] [Google Scholar]
- 27.Hadland SE, Bagley SM, Rodean J, et al. Receipt of timely addiction treatment and association of early medication treatment with retention in care among youths with opioid use disorder. JAMA Pediatr. 2018;172(11):1029–1037. 10.1001/jamapediatrics.2018.2143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Saloner B, Feder KA, Krawczyk N. Closing the medication-assisted treatment gap for youth with opioid use disorder. JAMA Pediatr. 2017;171(8):729–731. 10.1001/jamapediatrics.2017.1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hadland SE, Wharam JF, Schuster MA, Zhang F, Samet JH, Larochelle MR. Trends in receipt of buprenorphine and naltrexone for opioid use disorder among adolescents and young adults, 2001–2014. JAMA Pediatr. 2017;171(8):747–755. 10.1001/jamapediatrics.2017.0745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Feder KA, Krawczyk N, Saloner B. Medication-assisted treatment for adolescents in specialty treatment for opioid use disorder. J Adolesc Health. 2017;60(6):747–750. 10.1016/j.jadohealth.2016.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jarlenski M, Hogan C, Bogen DL, Chang JC, Bodnar LM, Van Nostrand E. Characterization of U.S. state laws requiring health care provider reporting of perinatal substance use. Womens Health Issues. 2017;27(3):264–270. 10.1016/j.whi.2016.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Angelotta C, Appelbaum PS. Criminal charges for child harm from substance use in pregnancy. J Am Acad Psychiatry Law. 2017;45(2):193–203. [PubMed] [Google Scholar]
- 33.Patrick SW, Schiff DM, Committee on Substance Use and Prevention. A public health response to opioid use in pregnancy. Pediatrics. 2017;139(3):e20164070 10.1542/peds.2016-4070. [DOI] [PubMed] [Google Scholar]
- 34.Hadland SE, Wood E, Levy S. How the paediatric workforce can address the opioid crisis. Lancet. 2016;388(10051):1260–1261. 10.1016/s0140-6736(16)31573-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


