Abstract
Adolescent girls are at heightened risk of depression, and because adolescent depression may initiate a negative developmental cascade, intervention early in adolescence has potential for altering a negative developmental trajectory. Identifying risk factors that impact response to intervention may inform decisions about the type of treatment to provide for adolescent girls with depression. Understanding moderators of outcomes in evidence-based treatment is critical to the delivery of timely and effective interventions. Matching patients effectively with optimal intervention will not only expedite the alleviation of patients’ distress, but will also reduce unnecessary time and resources spent on less advantageous interventions. The current investigation examines the efficacy of Interpersonal Psychotherapy for Depressed Adolescents (IPT-A) in a racially and ethnically diverse sample of 120 low-income adolescent girls age 13–15 with and without histories of child maltreatment. Adolescent and parent report of depressive symptoms were assessed at the beginning and end of treatment and a diagnosis of subsyndromal symptoms of depression or depression were required for purposes of inclusion. Results indicated that among adolescent girls who had experienced two or more subtypes of maltreatment, IPT-A was found to be more efficacious than Enhanced Community Standard (ECS) treatment. Importantly, when the subtype of maltreatment experienced was further probed, among girls with a history of sexual abuse, we found preliminary evidence that IPT-A was significantly more effective than ECS in reducing depressive symptoms, and the effect size was large. Thus, if a history of maltreatment is present, especially including sexual abuse, specifically addressing the interpersonal context associated with depressive symptoms may be necessary.
Keywords: Depression, adolescence, child maltreatment, intervention, developmental psychopathology, Interpersonal Psychotherapy
Adolescence is a time of considerable stress, even for teens who reside in relatively normative environments. It is a developmental period in which investigations guided by a developmental psychopathology perspective can be particularly compelling (Cicchetti & Rogosch, 2002; Cicchetti & Toth, 2016). Neurobiological, psychological, and social systems all undergo marked developmental changes during adolescence (Cicchetti & Toth, 2007; Masten, 2004; Steinberg et al., 2006). When the developmental challenges associated with transitioning from childhood into adulthood are exacerbated by co-occurring risk factors such as poverty, family stress, and trauma, the probability of the emergence of psychopathology is heightened. Because adolescent depression may initiate a negative developmental cascade, the identification of efficacious treatments is particularly important for mitigating against the emergence of depressive processes across the life course.
The prevalence of depression increases during adolescence (Angold & Costello, 2006), particularly for adolescent girls. Socioeconomic disadvantage is also associated with heightened risk for a number of mental health outcomes, including depression (e.g., Yoshikawa, Aber, Beardslee, 2012). Therefore, the provision and evaluation of interventions for adolescent girls who reside in low-income families are particularly important. In addition, when girls have experienced maltreatment during childhood, the risk for the emergence of depression is further heightened (Widom, DuMont, & Czaja, 2007). The current investigation examines the efficacy of Interpersonal Psychotherapy for Depressed Adolescents (IPT-A; Mufson, Dorta, Moreau, & Weissman 2004) in a racially and ethnically diverse sample of low-income adolescent girls with and without histories of child maltreatment.
Depression in Adolescence
Epidemiological estimates suggest that as many as 1 in 5 adolescents will experience a depressive disorder (Rushton et al., 2002), and there is evidence that rates of depression during adolescence are increasing (Collins & Dozois, 2008; Hammen & Rudolph, 2003). Increases in depressive symptoms during adolescence disproportionately affect more girls than boys between the ages of 13 and 15, with prevalence rates doubling for girls who are 15–18 years of age (Weisz & Hawley, 2002; Wichstrom, 1999). Increased rates of depressive symptoms also have been associated with residence in lower-income families, as well as in under-represented minority groups (Rushton et al., 2002). Because it is likely that depression during adolescence will persist into adulthood (Avenevoli, Knight, Kessler, & Merikangas, 2008; Kim-Cohen et al., 2003), the provision of intervention during adolescence is particularly important.
Child Maltreatment and Adolescent Depression
In addition to an increased prevalence of depression in low-income racially and ethnically diverse adolescent girls, risks for depression increase substantially when child maltreatment has occurred (Alloy et al., 1999; Cicchetti & Toth, 2009; Widom et al., 2007). Although the prevalence of depression in the United States is estimated at 7%, the rate of depression in individuals with histories of child maltreatment is significantly greater (Brown, Cohen, Johnson, & Smailes, 1999). Individuals with histories of maltreatment are likely to experience difficulties in relationships with parents, peers, teachers, and romantic partners (Cicchetti & Valentino, 2006; Kim & Cicchetti, 2003). In turn, these relational difficulties may increase the risk for the emergence of depression during adolescence, a developmental period when relationships outside of the home become particularly salient. Research also has demonstrated that children who have experienced multiple subtypes of maltreatment (e.g., physical abuse, neglect, sexual abuse, etc.) are even more likely to develop depressive symptoms (Widom et al., 2007). Additionally, adolescents with trauma histories have been shown to exhibit greater stress reactivity to life events that are of lower severity when compared with teens who do not have histories of maltreatment (Harkness et al., 2006). Severe sexual abuse also has been associated with dysregulation of stress response systems and future reactivity to lower levels of stress (Kendler et al., 2001; Post, 1992; Shenk, Noll, Putnam, & Trickett, 2010). Some research has shown blunted or asymmetrical physiological responses for sexually abused girls that predicted increased depressive symptoms (Shenk et al., 2010). It is therefore clear that a history of maltreatment sets in motion a negative cascade that adversely affects interpersonal relationships, contributes to the emergence of depressive symptoms, and heightens the likelihood that major depressive episodes will occur across the life course. Moreover, it is evident that sexual abuse may represent an especially potent risk factor.
Subtypes of Child Maltreatment and Depression.
Although a history of maltreatment has consistently been associated with increased risk for psychopathology, including depression (Norman, Byambaa, Butchart, & Scott, 2012), a paucity of investigations have focused on how various subtypes of maltreatment may be differentially related to the emergence of depression. While some studies have suggested that certain subtypes of maltreatment may result in specific mental health outcomes (see Cicchetti & Toth, 2016), others have found that various forms of maltreatment may have nonspecific, wide ranging effects on mental health (Vachon, Krueger, Rogosch, & Cicchetti, 2015). Lumley and Harkness (2007) reported both physical abuse and emotional maltreatment, but not sexual abuse, were correlated with depressed mood. In a longitudinal study examining different subtypes of maltreatment, both emotional abuse and neglect predicted depressed mood (Cohen, McNeil, Shorey, & Temple, 2018). Somewhat surprisingly, neither physical nor sexual abuse predicted depressive symptoms over and above the effects of emotional abuse and neglect. In efforts to clarify discrepant findings, Vachon et al. (2015) assessed a sample of over 2,000 racially and ethnically diverse school age children. A multi-informant, multi-method design found that different subtypes of child maltreatment result in similar psychiatric and behavioral outcomes, including anxiety and depression. Additionally, comparable consequences were found for boys and girls of different races. These investigators conclude that mixed findings with respect to sexual abuse may be a function of the overall low base rate in conjunction with the fact that sexual abuse frequently co-occurs with other forms of maltreatment, making its possibly unique effects difficult to parse out (Vachon et al., 2015). Furthermore, results of person-centered analyses of maltreatment parameters suggest substantial co-occurrence of subtypes such that the majority of maltreated children experience multiple forms of maltreatment (Warmingham, Handley, Rogosch, Manly & Cicchetti, 2019). Efforts to understand possible unique consequences of various subtypes of maltreatment become even more challenging when evaluating intervention outcomes.
Interventions for Adolescent Depression
Currently, an array of interventions are available to treat adolescent depression, including psychodynamic and cognitive behavioral approaches, as well as family and group therapies and pharmacotherapy. Given concerns associated with medication for depression during adolescence, including the possibility of an increased risk of suicide (Goodman, Murphy, & Storch, 2007), the provision of alternate modes of treatment is particularly important. The most prevalent evidence-based non-pharmacological interventions include cognitive behavioral therapy (CBT) and interpersonal psychotherapy for depressed adolescents (IPT-A) (Mufson et al., 2004; Maalouf & Brent, 2012; Weersing et al., 2017). Recently released guidelines for the treatment of depression concluded that CBT and IPT-A are the treatments with the most evidence for use with depressed adolescents (American Psychological Association, 2019; Zhou et al., 2015). Concerningly, however, even these efficacious interventions are not effective for all treated individuals, and maltreated individuals may be at elevated risk for poor treatment outcomes (Nanni, Uher, & Danese, 2012). Additionally, when transported to real world clinical settings, efficacious interventions are found to be even less effective (Weisz et al., 2017). Therefore, efforts to ascertain what characteristics of an individual may make them more likely to benefit from a specific type of treatment are of paramount importance. Moreover, because interpersonal relationships become increasingly important during adolescence, interventions that focus on the relational world and its influence on depression may be especially valuable.
Interpersonal Psychotherapy for Depressed Adolescents (IPT-A).
Interpersonal Psychotherapy (IPT) was first developed as a short-term treatment for depression in adult outpatients (Klerman, Weissman, & Rounsaville, 1984). The foundation for IPT is drawn from theoretical frameworks proffered by Adolf Meyer (Meyer, 1957), Harry Stack Sullivan (Sullivan, 1953), and John Bowlby (Bowlby, 1978, 1988). Although not discounting the role of biological and genetic factors, a central premise of IPT is that challenges encountered in the interpersonal context contribute to the onset and course of depression. The initial phase of IPT focuses on identifying central relationships in the individual’s life and then addressing 1 or 2 problem areas, including role disputes, role transitions, grief, and interpersonal deficits (Klerman et al., 1984). IPT-A differs from the adult version with respect to shortening treatment duration, including parents during the course of treatment, and serving as a liaison between families and schools (Klomek & Mufson, 2006). IPT-A presents the limited “sick role” to both the adolescent and the parent as a means to educate them about the effects of depression on the daily activities of a teenager. Throughout treatment, the purpose of providing the limited sick role is to allow the teen some relief from the pressures of performing their usual social roles (e.g. attending school, getting good grades, doing chores around the house) at the same level and in the same way as prior to being depressed, and to receive some support from their parents for the efforts they put in to these activities (Mufson et al, 2004). The overarching goal of IPT-A is to consider the role of salient developmental tasks such as individuation from parents, increased peer involvement/pressure, the formation of romantic relationships, and initial losses through death of loved ones. Although prior experiences, including early trauma, may have contributed to depression, IPT-A focuses on how these earlier experiences are affecting current interpersonal functioning.
There is clear evidence for the efficacy of IPT-A in treating adolescent depression (Mufson et al., 2004; Mychailyszyn & Elson, 2018; Pu et al., 2017; Young, Mufson, & Davies, 2006). A recent meta-analysis found that adolescents who received IPT-A experienced improvement in depressive symptoms, interpersonal difficulties, and general functioning that were medium to very large in effect size (Duffy, Sharpe, & Schwannauer, 2019). Moreover, IPT-A demonstrated superiority to non-CBT active control interventions, and showed equivalent efficacy to CBT (Duffy et al., 2019). However, whether individual characteristics moderate the efficacy of IPT-A is largely understudied.
Given the prevalence of child maltreatment and its relevance to the development of depression, understanding an individual’s history of child maltreatment may be critical to evaluating treatment efficacy. Furthermore, given prior research showing the particularly harmful effects of sexual abuse on the stress response system and development of depression (e.g., Shenk et al., 2010), identifying efficacious interventions for this especially vulnerable group is paramount. Prior research on predictors and moderators of treatment efficacy for adolescent depression have focused on CBT. Results show differential responses to treatment for youth with and without a trauma history (see Weersing et al., 2015; Weersing et al., 2017 for reviews). Within the adult literature, evidence is emerging for IPT as an efficacious intervention for trauma-exposed adults (e.g., Markowitz et al., 2015; Rafaeli et al., 2011; Toth et al., 2013). However, to date no studies have examined child maltreatment as a moderator of IPT-A efficacy.
Hypotheses
The investigation was guided by the following hypotheses:
IPT-A would be more efficacious in reducing depressive symptoms than would Enhanced Community Standard (ECS).
A history of child maltreatment will moderate the efficacy of IPT-A such that girls with a history of maltreatment will evidence greater benefits from IPT-A compared to ECS.
Specific hypotheses on how maltreatment subtype would affect treatment response were not made given the lack of prior studies in this area. However, a primary aim was to ascertain possible differential treatment response based on the occurrence of sexual abuse.
Method
Participants
Participants for this investigation included 120 racially and ethnically diverse low-income adolescent girls (aged 13–15; mean age =13.96, SD=.84; 65.0% African-American, 20.8% Caucasian, 14.2% identified as “other race,” and 14.2% Latinx ethnicity). The majority of adolescents lived with single mothers (80.0%) and 33.3% of adolescents lived with a parent with less than a high school diploma. Regarding family income within the sample, the mean total family income was $27, 900 (SD=12,380, min=5,000, max=70,000). Inclusion criteria included low-income adolescents between ages 13–15 years residing in the county in which the study was conducted. All girls were diagnosed with subsyndromal symptoms of depression or with major depressive disorder, dysthymia, or depressive diagnosis not otherwise specified. By design, approximately half of the participants had documented child maltreatment prior to enrollment, whereas the other half had no documented or self- or parent-reported maltreatment histories. Girls were excluded if there was evidence of compromised cognitive ability (i.e., WISC-IV IQ < 70) or if a pervasive developmental disorder, physical disability or major physical or neurological disorder (based on parent/guardian report or direct observation) prevented participation in clinical or research activities. Girls living in foster care were not recruited, although changes in custody could have occurred during the course of participation. Girls who were actively suicidal, diagnosed with a severe major mental disorder, (including bipolar disorder or a psychotic spectrum disorder) abusing alcohol or drugs, taking antidepressants or prescription medications for anxiety, or who were in any mental health treatment were excluded to minimize confounds. Families who did not have sufficient English proficiency to complete research procedures also were excluded.
Procedures
Informed consent and assent were obtained from parents and adolescents, respectively. Ethics approval of the study was provided by the University of Rochester. All families struggled financially and were eligible for Temporary Assistance to Needy Families (TANF). Adolescents were recruited by a Department of Human Services (DHS) liaison and through adolescent-serving organizations. The DHS liaison contacted potentially eligible families (those receiving public assistance with children in the age range) and explained the study. Fliers, brochures, and requests for referrals were distributed to organizations such as schools, recreational centers, youth bureaus, and medical providers. Interested parents provided signed permission for their contact information to be shared with project staff. Eligible adolescent girls who met criteria for subsyndromal (34.2%) or clinical depression (65.8%) at enrollment as assessed by the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children—Present and Lifetime (K-SADS-PL; Kaufman et al, 1997) were eligible. Subsyndromal depression was defined as meeting K-SADS criteria for Depression/Irritability or Anhedonia (at threshold and/or sub-threshold) plus one additional symptom (at threshold and/or sub-threshold). Because of possible variations in reading ability and literacy, all self-report measures were read to participants while they followed along and indicated their responses. Parents and adolescents were interviewed simultaneously in separate rooms.
Assessments were conducted at baseline and post-intervention between 2011 and 2016 by trained interviewers who were unaware of group conditions or study hypotheses. Following confirmation of eligibility, adolescents who met criteria for current subsyndromal or clinical depression were randomly assigned to the IPT-A (n=68; 56.7%) or to the ECS (n=52; 43.3%). Group assignment was not revealed until completion of the baseline research assessments, at which time participants were informed of their group assignment by the recruitment coordinator. In both conditions, we aimed to complete the 14 treatment sessions within 4–5 months. Families were contacted by research staff to schedule their post-intervention assessment immediately following their 14th treatment session. Please see Figure 1 for a CONSORT Flow Diagram.
Figure 1.
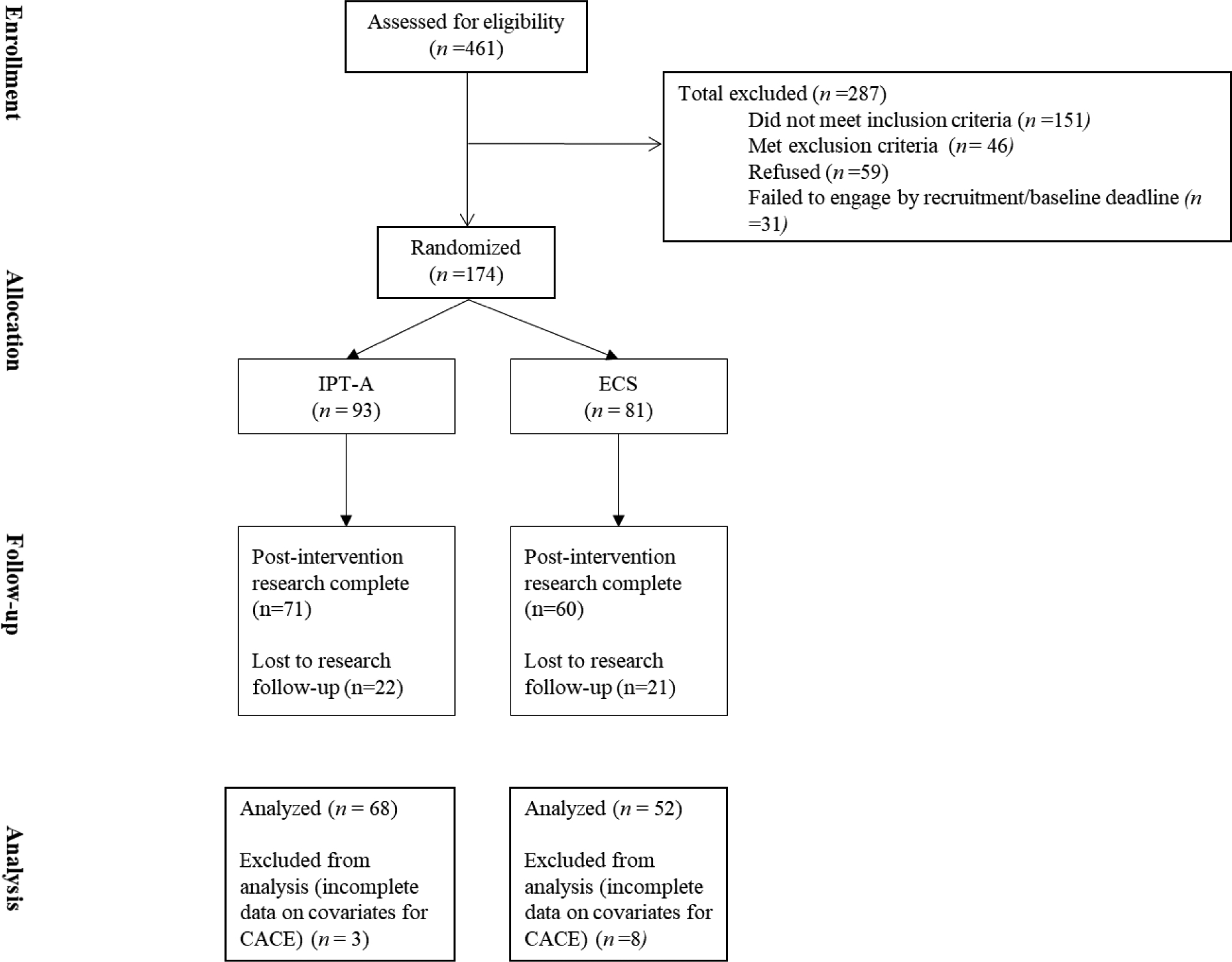
CONSORT Flow Diagram
Despite the presence of depressive symptomatology, the adolescent girls were not in treatment nor were they treatment-seeking. Therefore, a number of girls randomized to the intervention arms chose not to participate in the treatment. The mean number of treatment sessions completed did not significantly differ by intervention arm (MIPT-A = 8.24 (SD=6.43); MECS = 7.38 (SD=5.65); t (118) = −.76, p=n.s.). As described in detail below, complier average causal effect modeling (CACE) was employed to handle the rate of non-compliance within the IPT-A group. We adopted a definition of engagement whereby attending 0–3 sessions was defined as “non-compliance” because of minimal clinical engagement and inability to move beyond the initial assessment phase of treatment. If participants could not be engaged in treatment following multiple outreach efforts or declined all participation, further efforts to engage them were discontinued. However, they were contacted for follow-up research interviews and included in intent-to-treat analyses when possible. For the IPT-A arm, n=25 adolescents (36.7%) were classified as non-compliers with randomization. The rate of non-compliance in the ECS group was 34.6% (n=18). Table 1 presents information on characteristics of compliers and non-compliers for the entire sample. Overall, girls with more maltreatment subtypes were more likely to comply with their assigned randomization (Mnon-complier = .35 subtypes (SD=.48), Mcomplier = .56 subtypes (SD=.50; t (1) = −2.23, p=.03). With regards to service utilization outside of the randomly assigned intervention, 21.2% of girls assigned to ECS also saw a psychiatrist, psychologist, social worker, or counselor between baseline and post-intervention; 16.2% of girls assigned to IPT-A saw one of the above providers between baseline and post-intervention.
Table 1.
Characteristics of overall treatment compliers and non-compliers
| Non-compliers (n=43) | Compliers (n=77) | Statistic Test (df) | |||
|---|---|---|---|---|---|
| N | % | N | % | χ2 | |
| Adolescent race | |||||
| Black | 28 | 65.1 | 50 | 64.9 | |
| White | 7 | 16.3 | 18 | 23.4 | |
| Other | 8 | 18.6 | 9 | 11.7 | 1.60 (2), p=.45 |
| Adolescent ethnicity (% Latinx) | 5 | 11.6 | 12 | 15.6 | .36 (1), p=.79 |
| Parental education (% high school) | 28 | 65.1 | 52 | 67.5 | .07 (1), p=.84 |
| Parental marital status (% single) | 37 | 86.0 | 59 | 76.6 | 1.53 (1), p=.24 |
| Adolescent depressive disorder (KSADs) | |||||
| Major depressive disorder | 5 | 11.6 | 17 | 22.1 | |
| Minor depressive disorder | 14 | 32.6 | 17 | 22.1 | |
| Dysthymia | 2 | 4.7 | 4 | 5.2 | |
| Subsyndromal | 22 | 51.2 | 39 | 50.6 | 2.83 (3), p=.42 |
| Adolescent baseline anxiety diagnosis | 5 | 11.6 | 7 | 9.1 | .20 (1), p=.75 |
| Adolescent history of sexual abuse | 3 | 7.0 | 12 | 15.6 | 1.87 (1), p=.25 |
| Adolescent baseline self-harm | 7 | 20.6 | 18 | 26.5 | .42 (1), p=.63 |
| Adolescent baseline suicide ideation | 16 | 37.2 | 41 | 53.2 | 2.85 (1), p=.13 |
| Adolescent baseline PTSD | 12 | 27.9 | 27 | 35.1 | .64 (1), p=.54 |
| M | SD | M | SD | t-test, t (1, 118) | |
| Adolescent age | 13.88 | .82 | 14.00 | .86 | −.72, p=.47 |
| Family income (in thousands) | 25.74 | 8.49 | 29.13 | 14.02 | −1.44, p=.15 |
| Parental baseline depressive symptoms (BDI-II; sum score) | 17.65 | 10.00 | 15.71 | 11.94 | .90, p=.37 |
| Adolescent baseline depressive symptoms (BDI-Y: sum score) | 12.23 | 11.74 | 15.57 | 9.48 | −1.70, p=.09 |
| Adolescent number of maltreatment subtypes | .35 | .48 | .56 | .50 | −2.23, p=.03 |
Notes: KSADS = Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (Kaufman et al., 1997) BDI-Y = Beck Depression Inventory for Youth (Beck et al., 2005)
Intervention Groups
Interpersonal Psychotherapy for Depressed Adolescents (IPT-A).
IPT-A was delivered in accordance with the treatment manual (Mufson, Dorta, Moreau, & Weissman, 2004) and included the provision of 14 one-hour sessions on a weekly basis. Initiation of services began with a motivational interviewing session to establish a therapeutic alliance and to increase the likelihood of girls entering and remaining in treatment. Flexibility of delivery site (home, schools, community, or clinic) was offered to reduce the possible stigma associated with receiving mental health services for low-income, racially and ethnically diverse participants who were non-treatment seeking and to increase receptivity to services. The decision of where to meet was discussed with the teen and family, and location sometimes varied session by session depending on logistics of scheduling and convenience for participants. Sessions were held individually with adolescents to provide private time to discuss personal concerns, but parents/caregivers were apprised of their daughters’ progress in treatment, and caregivers and families were included to the extent that treatment goals included parent-child communication.
Depression was explained to participants as common feelings that can be associated with life challenges and stressors. At times, language focused more on “feeling overwhelmed, stressed and down” because it was difficult for some teens to acknowledge feeling “depressed.” Therefore, in some instances the psychoeducation about depression that therapists typically provide in the initial phase was provided later in treatment, once therapeutic rapport was established.
Maltreatment history was discussed and explored within the context of the depression timeline during the initial phase of treatment. This was an opportunity for the teens to identify and label their experiences in the past that impacted their mood and contributed to depressive symptomatology and it allowed the client to gain a better understanding of what her depression specifically looks like. The history of maltreatment was then conceptualized within the context of her interpersonal focus areas and explored within the framework of trying to understand and link how that history was impacting current relationships. For example, one common theme that emerged included a lack of trust in relationships that stemmed from a history of maltreatment. This contributed to interpersonal deficits or a lack of supportive social relationships. Regarding interpersonal disputes, teens with a history of maltreatment often found it difficult to express themselves effectively within relationships-- i.e., they either closed themselves off to others and would not express their feelings, or they would become emotionally dysregulated when triggered—which would then lead to difficulties in relating to others and getting their needs met. Identifying that these responses might be coming from their history of abuse was important. Then the focus was on learning new ways of coping, and practicing alternative strategies to express themselves more effectively.
Therapists included master’s- or doctoral-level practitioners who were trained in IPT-A in accord with credentialing recommendations by an International Society for IPT Certified Trainer and Supervisor. Training consisted of a 2-day workshop with a didactic overview of each phase of treatment, and on-going consultation and supervision around 3 training cases before being assigned cases. Consultation for these training cases included the review and discussion of taped sessions in between each session throughout treatment, with a focus on fidelity to the IPT model as well as clinical supervision around the case. Therapists provided therapy as part of their role in the community mental health center, but they had dedicated time devoted to the project. Once training cases were completed, weekly individual and group supervision was provided by supervisors who also met credentialing requirements for the IPT-A supervisory level.
Fidelity was monitored by supervisors through the completion of the IPT-A Supervision Checklist (Mufson, Clougherty, Young, & Verdeli, 2004) at the initial, intermediate, and termination phases of IPT-A. One audio recording from each of the initial (Sessions 1–3), intermediate (Sessions 4–11), and termination (Sessions 12–14) phases of treatment for each client was randomly selected to be reviewed by the supervisor to ensure treatment fidelity. Overall fidelity scores could range from 5 ‘excellent’ to 1 ‘poor.’ Supervisors’ ratings of IPT-A therapists’ fidelity to the IPT-A model averaged 4.44 (SD=.82) for the initial phase, 4.45 for the middle phase (SD=.82), and 4.45 for the termination phase (SD=.83), indicating high fidelity to the model.
Enhanced Community Standard (ECS).
Because it is not ethical to withhold treatment from adolescents who have been identified as depressed, all girls in the ECS condition received an active intervention. The ECS was designed to be comparable with counseling services that may typically be provided in the community as well as with the number of sessions provided in IPT-A (maximum of 14 sessions). These counseling services were “enhanced” by having extensive outreach available, including having services available in homes, community settings, clinic, and schools, to improve accessibility and uptake of services for non-treatment-seeking participants. This flexibility in setting was comparable to that in IPT-A, with location dependent on teen and caregiver choice, scheduling logistics for each session, and convenience for participants. These outreach efforts were comparable to what was available for participants in the IPT-A group, although they are above and beyond what is typically available in a traditional outpatient mental health model. The ECS therapist held a master’s degree in social work and experience in working with urban families, and dedicated time to the project as part of her role in the center. The ECS services focused on providing support for teens dealing with challenging issues that they self-reported, such as school success, making positive life choices, self-identity, and conflicts with peers and family members. The services did not include any specific model of intervention, but were supportive in nature and provided an outlet for teens to discuss stressors in their lives. Parents/caregivers were included in discussions of these issues as deemed clinically appropriate, although individual sessions with girls were the primary modality of treatment.
Measures
Current adolescent depression and anxiety diagnoses.
The presence of current subsyndromal or clinical major depression and anxiety disorders (General Anxiety Disorder, Social Anxiety Disorder, Panic Disorder, and Obsessive-Compulsive Disorder) was determined using the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL; Kaufman et al., 1997), a psychometrically-sound parent-child diagnostic interview of common childhood psychiatric disorders consistent with DSM-IV criteria. The KSADS-PL consists of 82-items to screen for core symptoms specific to 20 disorders, skip-out criteria, and supplemental sections to determine concurrent diagnosis-specific symptoms as well as the timing, duration, and severity of these symptoms (Kaufman et al., 2000). For purposes of this investigation, modules for 10 disorders were administered, including: Depressive Disorders; Mania; Psychosis; Panic Disorder; Social Phobia; Generalized Anxiety Disorder; Obsessive Compulsive Disorder; Oppositional Defiant Disorder; Conduct Disorder; and Alcohol and Substance Use Disorders. Reliably trained clinical interviewers (including research assistants and clinical graduate students supervised by licensed clinical psychologists) administered the KSADS-PL to adolescents and parents individually and in separate rooms. Symptom scores for depression and anxiety disorders were based on a synthesis of both parent and adolescent-report of the adolescent’s depression and anxiety symptomatology in the past 2 months and 6 months, respectively, with symptoms rated on a 1–3 scale (1=absent, 2=subthreshold, 3=threshold). Final diagnostic determination for each disorder was coded as a binary variable (0=no, 1=yes). Comorbid anxiety disorders were controlled for in all subsequent analyses. The K-SADS has evinced good test-retest reliability, concurrent validity (Kaufman et al., 1997) and convergent validity (Lauth et al., 2010). Interrater reliabilities (ICCs) ranged from .75–93 across diagnoses.
Adolescent depressive symptoms.
Adolescents reported on their current depressive symptoms using the Beck Depression Inventory for Youth (BDI-Y; Beck et al., 2005). The BDI-Y is a 20-item self-report instrument measuring severity of depressive symptoms over the past 2 weeks. Adolescents rated their responses on a 0–3 scale (0=Never, 3=Always). A summary score was calculated, with higher scores indicating greater depressive symptom severity. Psychometric properties of the BDI-Y have been demonstrated previously (Stapleton, Sander, & Stark, 2007).
Adolescent posttraumatic stress symptoms.
Posttraumatic stress disorder symptoms were assessed through self-report on the UCLA-PTSD Reaction Index (Steinberg et al., 2013; Steinberg, Brymer, Decker, Pynoos, 2004). The UCLA PTSD Index is a 49 item self-report measure to screen for exposure to traumatic events and for all DSM-IV post-traumatic stress disorder (PTSD) symptoms in adolescents who report traumatic stress experiences. The adolescent version was utilized for this project. The scale has been demonstrated to have good internal consistency (.87), convergent validity, and test-retest reliability (.64-.94) (Steinberg et al., 2013).
Parent depressive symptoms.
Parents reported on their own current depressive symptoms using the Beck Depression Inventory, second edition (BDI-II; Beck et al., 1996). The BDI-II is a 21-item self-report measuring the severity of depressive symptoms over the past 2 weeks. Parents endorsed symptoms on a 0–3 scale (0=not present to 3 = severe). A summary score was calculated, with higher numbers indicating greater depressive symptom severity. The BDI-II has demonstrated good test-retest reliability, internal consistency and concurrent validity (Beck et al., 1996).
Adolescent maltreatment.
The Childhood Trauma Questionnaire CTQ; Bernstein et al., 2003) is a 25-item self-report measure on childhood experiences of maltreatment. Adolescents rated their experience with each item in their lifetime based on a 5-point scale (0=Never True to 5= Very True). Sample items include: “I got hit so hard by someone in my family that I had to see a doctor or go to the hospital,” and “When I was growing up, I didn’t have enough to eat.” Maltreated subtypes include emotional abuse, physical abuse, sexual abuse, emotional neglect, and physical neglect. Items are scored on a scale of 1=never, 2= rarely true, 3=sometimes true, 4=often true, and 5=very often true. Established cut-offs were used to determine the presence of each subtype (Walker et al., 1999). These were calculated by summing items from each subscale and using the following criterion cut-off: sexual abuse ≥ 8, physical abuse ≥ 8, physical neglect ≥ 8, emotional neglect ≥ 15, and emotional abuse ≥ 10. A summary score based on the number of maltreatment subtypes meeting this threshold was then computed (0–5) and used in subsequent analyses. The CTQ has evidenced good internal consistency (α = 0.66 – 0.92; Bernstein & Fink, 1998) and convergent validity with other self-report and interview measures of child maltreatment (Bernstein et al., 2003; Hyman, Garcia, Kemp, Mazure, & Sinha, 2005).
Approximately half of the sample were non-maltreated based on the CTQ (n=62, 51.7%); 29 youth (24.2%) endorsed 1 maltreatment subtype, 12 (10.0%) endorsed 2 maltreatment subtypes, 11 (9.2%) endorsed 3 subtypes, 5 (4.2%) endorsed 4 subtypes, and 1 (0.8%) endorsed all 5 maltreatment subtypes. Regarding sexual abuse, 15 (12.5%) teens in the sample endorsed a history of sexual abuse. Among girls with a history of sexual abuse, 4% did not report any other forms of maltreatment. For other maltreatment subtypes, 23.3% of the teens in this sample endorsed physical abuse, 16.7% endorsed physical neglect, 10.8% endorsed emotional neglect, and 29.2% endorsed emotional abuse.
Analytic Plan
Our data analytic plan consisted of first examining differences between IPT-A and ECS groups on baseline adolescent and family demographic and study-related variables. Intent-to-treat (ITT) analyses were then conducted to examine the effect of randomization to IPT-A versus ECS on adolescent post-intervention depressive symptoms. As-treated analyses were also conducted to investigate differences in post-intervention depressive symptoms across intervention arms for those individuals who completed at least 4 sessions of treatment. Finally, complier average causal effect (CACE) modeling was used to examine treatment effects while incorporating treatment engagement within Mplus Version 8.1 (Muthén & Muthén, 1998– 2018). We conducted two sets of CACE analyses. The first set examined whether the number of maltreatment subtypes experienced by the adolescent moderated treatment efficacy. The second set examined whether a history of sexual abuse moderated treatment efficacy. We used the robust maximum likelihood (MLR; Yuan & Bentler, 2000) estimator in analyses involving a structural equation mixture modeling (SEM) framework (e.g., CACE modeling).
Complier Average Causal Effect Modeling (CACE).
We employed CACE modeling because of the proportion of non-treatment seeking adolescents who were randomly assigned to the IPT-A condition but who failed to reach a sufficient level of treatment engagement (i.e., less than 4 sessions), as is common in Randomized Encouragement Trial designs (Connell, 2009). Other analytic approaches and methods have been used for addressing non-compliance (e.g., per protocol analysis, as-treated analysis, intent-to-treat (ITT) analysis); however, each may lead to bias in treatment effect estimates relative to the true causal effect of receiving treatment would have been in the population (Jo, 2002). ITT analyses evaluate the effect of the treatment by comparing individuals assigned to the treatment group to individuals assigned to the control group, regardless of their actual compliance, or participation in the treatment. Ignoring compliance with the treatment can lead to an underestimate of treatment effects. Accordingly, the treatment effect estimate in ITT analyses is referred to as the “average causal effect of treatment as treatment was assigned” but not as treatment was actually received (Jo, 2002, p.180). CACE estimation is an analytic approach for randomized trials that considers treatment engagement in the analysis of the treatment effect and it has been utilized in other RCTs with non-treatment seeking populations (Toth et al., 2013). In CACE modeling, engagement is considered a moderator of the effect of random assignment on the outcomes. Model fit is assessed using entropy, which represents the probability of membership in the most-likely class for each individual (IPT-A complier or noncomplier). Entropy values range from 0 to 1.0 and higher values indicate better classification (Muthen & Muthen, 1998–2018).
Results
Table 2 presents the results of the comparison between the IPT-A and ECS groups at baseline on demographic and study variables. Results indicated that groups did not differ on demographic characteristics including adolescent age, race, parental educational attainment, total family income, baseline parental depressive symptoms, baseline adolescent depressive symptoms, baseline adolescent co-occurring anxiety disorder, and number of maltreatment subtypes or history of sexual abuse. Adolescents randomly assigned to IPT-A were significantly more likely to be Latinx (20.6%) compared to those randomly assigned to ECS (5.8%, χ2 (1) = 5.32, p<.05).
Table 2.
Between group differences in baseline and demographic variables for entire sample
| Assigned to IPT- A (n=68) | Assigned to ECS (n=52) | Statistic Test (df) | |||
|---|---|---|---|---|---|
| N | % | N | % | χ2 | |
| Adolescent race | |||||
| Black | 40 | 58.8 | 38 | 73.1 | |
| White | 17 | 25.0 | 8 | 15.4 | |
| Other | 11 | 16.2 | 6 | 11.5 | 2.68 (2), p=.27 |
| Adolescent ethnicity (% Latinx) | 14 | 20.6 | 3 | 5.8 | 5.32 (1), p=.03 |
| Parental education (% high school) | 45 | 66.2 | 35 | 67.3 | .02 (1), p=.1.00 |
| Parental marital status (% single) | 52 | 76.5 | 44 | 84.6 | .27 (1), p=.36 |
| Adolescent depressive disorder (KSADs) | |||||
| Major depressive disorder | 10 | 14.7 | 12 | 23.1 | |
| Minor depressive disorder | 22 | 32.4 | 9 | 17.3 | |
| Dysthymia | 2 | 2.9 | 4 | 7.7 | |
| Subsyndromal | 34 | 50.0 | 27 | 51.9 | 5.06 (3), p=.17 |
| Adolescent baseline anxiety diagnosis | 6 | 8.8 | 6 | 11.5 | .62 (1), p=.76 |
| Adolescent history of sexual abuse | 6 | 8.8 | 9 | 17.3 | 1.94 (1), p=.18 |
| Adolescent baseline self-harm | 19 | 29.2 | 13 | 24.1 | .40 (1), p=.54 |
| Adolescent baseline suicide ideation | 30 | 46.9 | 37 | 46.8 | .00 (1), p=.1.00 |
| Adolescent baseline PTSD | 25 | 36.8 | 14 | 26.9 | 1.30 (1), p=.34 |
| M | SD | M | SD | t-test, F (1, 118) | |
| Adolescent age | 13.97 | .86 | 13.94 | .83 | −.18, p=.86 |
| Family income (in thousands) | 28.30 | 12.61 | 27.39 | 12.17 | −.40, p=.69 |
| Parental baseline depressive symptoms (BDI-II; sum score) | 16.79 | 11.84 | 15.90 | 10.60 | −.43, p=.67 |
| Adolescent baseline depressive symptoms (BDI-Y: sum score) | 13.47 | 8.64 | 15.56 | 12.36 | 1.08, p=.28 |
| Adolescent number of maltreatment subtypes | .43 | .50 | .56 | .50 | 1.43, p=.16 |
Notes: Total family income is in thousands. BDI-II = Beck Depression Inventory II (Beck et al., 1996), BDI-Y = Beck Depression Inventory for Youth (Beck et al., 2005)
Intent to treat analyses compared post-intervention depressive symptoms between adolescents randomly assigned to IPT-A and those assigned to ECS. Results of an independent samples t-test indicated that those assigned to IPT-A (M=9.19, SD=6.85) evidenced marginally significantly lower depressive symptoms at post-intervention compared to those assigned to ECS (M=11.92, SD=9.88, F (1) = 3.20, p=.076). An additional ordinary least squares regression was conducted, including intervention arm and baseline depressive symptoms as predictors (F (2) = 10.23, p<.001). Results indicated a significant continuity in depressive symptoms over time (b=.35, p<.001) and a non-significant main effect of intervention status (b=−.13, p=.14).
As-treated analyses were conducted examining differences among the two intervention arms on post-depression symptoms for the subsample of participants who completed at least 4 sessions of the assigned intervention (N=77; NIPT =43, NECS =34; F (2) = 9.35, p<.001). Results indicated a significant continuity in depressive symptoms over time (b=.39, p<.001) and a significant effect of intervention (b=−.23, p=.03) such that those who completed at least 4 sessions of IPT-A reported significantly lower depressive symptoms at post-intervention compared to those who completed at least 4 sessions of ECS.
Complier Average Causal Effect (CACE) Modeling
ITT analyses can underestimate treatment effects due to the lack of consideration of compliance (Jo, 2002). Because the current study was a Randomized Control Trial of non-treatment seeking adolescents, taking into account compliance or engagement with treatment was critical. Therefore, CACE modeling was conducted which allowed for an examination of treatment as received (rather than as assigned which is the case with ITT). CACE modeling differs from “as-treated analyses” because CACE modeling treats engagement as a moderator of the effect of random assignment. Moreover, model fit for CACE is assessed using entropy, which represents the probability of membership in the most-likely class for each individual (IPT-A complier or noncomplier). An initial recommended step in CACE analysis is to define participant “engagement” in treatment (Connell, 2009). We adopted a definition of engagement whereby attending 0–3 sessions was defined as “non-compliance” because of minimal clinical engagement and inability to move beyond the initial assessment phase of treatment. If participants could not be engaged following multiple outreach efforts or declined all participation, further efforts to engage them were discontinued. As a result of this IPT-A treatment compliance definition, IPT-A compliers attended 4 or more sessions (compliers, n=43, 63.2%), and IPT-A non-compliers attended 3 or fewer sessions (non-compliers, n = 25, 36.8%)1.
Treatment Effect Moderation by Number of Maltreatment Subtypes
The compliance rate (adjusted for the covariates including family income, parental educational attainment, marital status, depressive symptoms, and adolescent age race, ethnicity, and co-morbid anxiety disorder) was 57.5% based on the estimated posterior probabilities. With this compliance definition, entropy, a measure of model fit for CACE modeling, was good (0.72). Logistic regression examining predictors of the IPT-A complier class showed that those adolescents from families with higher incomes were marginally significantly more likely to be in the complier class (OR=1.04, SE=.02, p=.07). Other predictors including parental educational attainment, marital status, depressive symptoms, and adolescent age race, ethnicity, and co-morbid anxiety disorder were not significant predictors of IPT-A complier class.
Results of this CACE model showed that adjusted for IPT-A non-compliance and baseline levels of adolescent depressive symptoms, there was not a significant difference between the IPT-A and ECS groups on post-intervention depressive symptoms. Significant stability in depressive symptoms from pre-intervention to post-intervention was also found (b=.29 (SE=.10), p=.004). Moreover, a greater number of maltreatment subtypes was predictive of a higher level of post-intervention depressive symptoms (b=.77 (SE=.14), p<.001). Importantly, the interaction of intervention by number of maltreatment subtypes was statistically significant (b=−.62 (.14), p<.001). See Table 3 for results.
Table 3.
Results of CACE models with maltreatment subtypes predicting post-intervention depressive symptoms among IPT-A compliers
| MODEL 1 | MODEL 2 | |||||
|---|---|---|---|---|---|---|
| Predictor | Number of maltreatment subtype moderator | Sexual abuse moderator | ||||
| B | SE | p | b | SE | p | |
| Intervention (IPT-A vs ECS) | .07 | .13 | .60 | .08 | .12 | .48 |
| Baseline depressive symptoms | .29 | .10 | .004 | .36 | .09 | <.001 |
| Maltreatment moderator | .77 | .14 | <.001 | .69 | .14 | <.001 |
| Maltreatment moderator X intervention | −.62 | .14 | <.001 | −.42 | .15 | .004 |
The significant interaction of intervention and maltreatment subtypes presented above was probed at various levels of number of maltreatment subtypes following guidelines provided by Cohen, Cohen, West, and Aiken (2003) for continuous by binary interaction terms. The maltreatment subtype variable was not treated as a grouping variable, but rather the effect of IPT-A versus ECS was probed at various levels of the continuous variable maltreatment subtypes by re-centering this variable. Results indicated that among adolescents without a maltreatment history (n=62), there was not a significant difference between IPT-A and ECS on post-intervention depressive symptoms (b=.07, p=.59). However, among adolescents who experienced one maltreatment subtype (n=29), IPT-A predicted marginally significantly fewer depressive symptoms at post-intervention (b=−.21, p=.067). Among adolescents who experienced two maltreatment subtypes (n=12), IPT-A predicted significantly fewer depressive symptoms at post-intervention compared to ECS (b=−.50, p<.001). Finally, among adolescents who experienced three maltreatment subtypes (n=11), IPT-A predicted significantly fewer depressive symptoms at post-intervention compared to ECS (b=−.78, p<.001).
An examination of the standardized betas for the simple slopes indicates that the magnitude of the effect of IPT-A versus ECS on post-intervention depressive symptoms is greater at higher levels of maltreatment subtypes. For adolescents who experienced one maltreatment subtype, the effect of IPT-A versus ECS on post-intervention depressive symptoms can be considered small/medium in size. For adolescents who experienced two or more maltreatment subtypes, the effect of IPT-A versus ECS on post-intervention depressive symptoms can be considered large in size (Cohen, 1988). Thus, the difference in the effect of IPT-A versus ECS on depressive symptoms becomes greater at higher levels of maltreatment subtypes.
Treatment Effect Moderation by Sexual Abuse History
The compliance rate for this CACE model (adjusted for the covariates including family income, parental educational attainment, marital status, depressive symptoms, and adolescent age race, ethnicity, and co-morbid anxiety disorder) was 59.5% based on the estimated posterior probabilities. Entropy for this model was also good (0.72). Logistic regression examining predictors of the IPT-A complier class again showed that those adolescents from families with higher incomes were marginally significantly more likely to be in the complier class (OR=1.04, SE=.02, p=.07). Moreover, in this model, compliers were more likely to be non-African American (OR=.36, SE=.24, p=.006) and not have a co-morbid anxiety diagnosis (OR=.35, SE=.25, p=.01). Adolescents of parents with higher depressive symptoms were more likely to comply with IPT-A (OR=1.05, SE=.02, p=.03). Other predictors of complier class membership were not significant (e.g., parental educational attainment and marital status, adolescent age and ethnicity).
Results of the CACE model examining sexual abuse histories showed that adjusted for IPT-A non-compliance and baseline levels of adolescent depressive symptoms, there was not a significant difference between groups on post-intervention depressive symptoms (b=.08 (SE=.12), p=.48). Significant stability in depressive symptoms from pre-intervention to post-intervention was also found (b=.36 (SE=.09), p<.001). Moreover, a history of sexual abuse predicted higher post-intervention depressive symptoms (b=.69 (SE=.14), p<.001). Importantly, significant treatment effect moderation was again found. In this model, the interaction of sexual abuse by intervention was statistically significant (b=−.42 (SE=.15), p=.004). See Table 3 for results.
Probing the interaction indicated that among adolescents without a sexual abuse history, there were no differences in efficacy of IPT-A and ECS on post-intervention depressive symptoms (b=.08, p=.48). However, among adolescents with a history of sexual abuse, IPT-A was predictive of greater reduction in depressive symptoms at post-intervention compared to ECS (b=−.72, p=.002). Thus, the effect of IPT-A versus ECS on decreased post-intervention depressive symptoms depended on sexual abuse history such that among adolescents with a sexual abuse history, IPT-A was predictive of fewer depressive symptoms at post-intervention. The size of the difference between IPT-A and ECS on post-intervention depressive symptoms among adolescents with a sexual abuse history can be interpreted as large (Cohen, 1988).
Discussion
The current investigation contributes to the growing body of research that supports the efficacy of IPT-A in reducing depressive symptoms. However, our findings extend the extant literature by highlighting the importance of considering how a history of maltreatment might result in differential outcomes among adolescent girls. For girls who did not have a history of maltreatment, IPT-A and ECS were equally effective in reducing depressive symptoms. However, among girls who had experienced maltreatment, IPT-A was shown to be more efficacious than ECS in reducing depressive symptoms. Specifically, when girls had experienced a single subtype of maltreatment, IPT-A was marginally more significant than ECS. Among adolescent girls who had experienced two or more subtypes of maltreatment, IPT-A was found to be significantly more efficacious than ECS. Importantly, when the subtype of maltreatment experienced was further probed, we found preliminary evidence that a history of sexual abuse may be a significant variable to consider. When girls had a history of sexual abuse, IPT-A was significantly more effective than ECS in reducing depressive symptoms and the effect size was large.
Although our finding that girls with a sexual abuse history benefited more from IPT-A than ECS is preliminary given the small number of girls with a sexual abuse history (n=15, 12.5% of the overall sample), it is consistent with the work of Markowitz and colleagues (2017) who showed that among adults with post-traumatic stress disorder (PTSD), sexual trauma moderated the efficacy of IPT. Specifically, IPT demonstrated greater efficacy for sexually traumatized adults compared to both prolonged exposure therapy and relaxation therapy. Similarly, Duberstein and colleagues (2018) found that women with childhood histories of sexual abuse evidenced decreased PTSD symptoms and improvements in social health following the completion of IPT and that these beneficial outcomes persisted for one year following the end of treatment. We extend these findings to show that among a sample of socioeconomically disadvantaged depressed adolescent girls, IPT-A may be a better treatment option for those with a sexual abuse history, than ECS.
These findings possess important implications for considering a history of abuse in making decisions about the type of treatment to provide for adolescent girls with depression. It appears that when maltreatment has not occurred, non-specific therapeutic factors may result in improvement. However, when maltreatment has occurred and, specifically, if prior sexual abuse is present, the relational focus of IPT-A may be particularly important. Interestingly, when comparing IPT-A with the widely utilized model of cognitive behavioral therapy (CBT) both models have been found to be equally effective (Weersing et al., 2017). The current findings raise the possibility that if other moderating factors were considered, then differences between the models might emerge. If a history of maltreatment is present, it is possible that specifically addressing the interpersonal context associated with depressive symptoms might be necessary to reduce depressive symptoms. Such a perspective is consistent with the longstanding call to ascertain “what works best for whom” (Roth & Fonagy, 2005).
According to Kraemer (2013), “emphasis in randomized clinical trials (RCTs) is gradually shifting … to discovery and documentation of moderators of treatment choice on outcome in RCTs, that is, personalized medicine.” Understanding which evidence-based treatment works best for various populations is critical to the delivery of timely and effective interventions. The ability to match patients with their optimal intervention effectively will not only expedite the alleviation of patients’ distress, but will also reduce unnecessary time and resources spent on less optimally matched interventions. Thus, there is a clear need for future research that continues to investigate treatment effect moderators for adolescent depression. Our study compared IPT-A to an enhanced community standard of care, similar to a general community counseling approach. Future studies are necessary to examine whether there are differential treatment effect moderators for IPT-A versus CBT, given that these are the two psychotherapeutic interventions with the strongest evidence base for adolescent depression (Zhou et al., 2015). For example, whether depressed adolescents with a history of child maltreatment may benefit more favorably from IPT-A versus CBT is a critical next question for the field.
It is important to note that this sample included a diverse group of adolescent girls from low-income families. Extensive outreach was utilized to recruit these teens and engage them in treatment. Risk factors and barriers to care included extreme poverty, lack of transportation, familial mental health concerns, including high rates of maternal depression and suicidality, chaotic family lifestyles within single-parent families with multiple children, homelessness, intimate partner violence among parents, parental substance abuse, teen pregnancy, and high rates of community violence in urban neighborhoods. Several of the participants endured extreme traumatic events during the course of the study, including being victims of assaults, losing parents or family members to death, parental incarceration, changes in custody and living arrangements, bullying in school, and dating violence (Adams, Handley, Manly, Cicchetti, & Toth, 2019). Although these girls were not treatment seeking, when depressive symptoms and suicidal ideation were assessed at baseline, they reported very high levels of depression, thoughts of self-harm and suicidal ideation, which in many cases they had not shared with anyone previously. The presence of depressive symptoms and risks of self-harming and suicidal behavior in non-treatment seeking populations underscores the need for outreach, screening, and provision of depression treatment outside of current traditional outpatient mental health settings. Many girls may be suffering from the consequences of maltreatment and trauma and feeling depressed, and they may feel that they have nowhere to turn and no one who can help them. It also is important to note that treatment-seeking populations are typically more responsive to treatment than individuals recruited via community outreach efforts. Therefore, the results of the current investigation are particularly compelling.
Even for families who had been involved with the Child Protective and child welfare systems, referrals for outpatient mental health care may have been unsuccessful because of difficulties with follow-through on connecting with traditional services that are not designed to address all of the barriers to care mentioned above. In our experience, adolescent depression is often under-identified, and youth in the child welfare and juvenile justice systems are likely to have unmet service needs (Bringewatt & Gershoff, 2010) or demonstrate limited improvement even when they do receive mental health services (McCrae, Barth, & Guo, 2010).
Limitations
Because of the challenges in recruiting and engaging non-treatment seeking low-income maltreated teens, the rates of compliance with treatment were not as high as they might have been in a more controlled setting and were lower than in other IPT-A studies. However, the nature of the population, being disenfranchised and living in poverty with limited access to transportation, and with family histories characterized by conflictual and/or negligent parent-child relationships, and with high rates of maternal as well as teen depression, these teens were especially in need of support and highly unlikely to receive it. The size of the sample and the less than optimal compliance with treatment may be considered limitations of the study; however, inclusion of this high-risk population in a treatment evaluation study underscores the importance of evaluating services outside frequently utilized populations of convenience or populations who are more resourced from white middle-class families. Interestingly, girls whose mothers had higher rates of depressive symptoms were more likely to comply with treatment. Although multi-site prevention studies have found that maternal depression adversely affects outcomes in offspring (Weersing, Shamseddeen, Garber, et al., 2016), the current study did not corroborate these findings. It may be that in the current investigation, mothers struggling with their own depression may have been more likely to understand their daughters’ symptoms and support treatment. Additionally, because mothers were able to be involved in treatment, they may have been better able to support their daughters’ treatment. Because of their own depression, without outreach and home- or school-based services, they may not have been able to take their daughters for treatment in more traditional outpatient settings.
Compliers with IPT-A were also more likely to be non-African-American and without comorbid anxiety diagnoses (as found in our CACE model). Interventions for depression should continue to explore ways of reducing stigma and partnering with African-American families in ways that facilitate engagement and help them feel more comfortable with treatment. Treatment approaches that address co-morbidity are essential given the frequency with which depression and anxiety co-occur. Teens with anxiety symptoms may be reluctant to engage in treatment, and strategies for addressing both anxiety and depression need to be evaluated to determine what approaches are likely to be most successful with these youths.
Despite the presence of some limitations, the results of this treatment evaluation study of IPT-A suggest that the girls who have experienced multiple subtypes of maltreatment, and especially those with sexual abuse histories, may be most likely to benefit from IPT-A treatment. While these teens may need non-traditional approaches to facilitate engagement, reduce stigma, and overcome barriers to treatment, there is hope that, with the provision of evidence-based intervention, these girls can find relief and symptom reduction.
Acknowledgements:
This work was supported by the National Institute of Mental Health (grant number R01MH091070). We thank the research staff for all aspects of data collection, and the adolescents and their families, without whom the project would not have been possible, for their willingness to share their experiences with us.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Disclosure of potential conflicts of interest
The corresponding author certifies that neither she nor any of the contributing authors have any conflict of interest to disclose.
It is worth noting that in the situation of two active intervention arms, such as the current study, the number of potential strata (compliance) increases, making identification of the principal effects very difficult, if not impossible. We selected to model compliance with IPT-A, rather than ECS, given IPT-A’s central importance to the study aims.
References
- Adams TR, Handley ED, Manly JT, Cicchetti D, & Toth SL (2019). Intimate partner violence as a mechanism underlying the intergenerational transmission of maltreatment among economically disadvantaged mothers and their adolescent daughters. Development and Psychopathology, 31, 83–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alloy LB, Abramson LY, Whitehouse WG, Hogan ME, Tashman NA, Steinberg DL, … & Donovan P (1999). Depressogenic cognitive styles: Predictive validity, information processing and personality characteristics, and developmental origins. Behaviour Research and Therapy, 37(6), 503–531. [DOI] [PubMed] [Google Scholar]
- American Psychological Association (2019). Clinical practice guideline for treatment depressive across three age cohorts.. Retrieved from https://www.apa.org/depression-guideline/guideline.pdf.
- Angold A, & Costello EJ (2006). Puberty and depression. Child and Adolescent Psychiatric Clinics, 15(4), 919–937. [DOI] [PubMed] [Google Scholar]
- Avenevoli S, Knight E, Kessler RC, & Merikangas KR (2008). Epidemiology of depression in children and adolescents In Abela JRZ & Hankin BL (Eds.), Handbook of depression in children and adolescents (pp. 6–32). New York, NY: Guilford Press. [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Manual for the Beck Depression Inventory—II. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Bernstein DP, & Fink LA (1998). CTQ: Childhood Trauma Questionnaire: A retrospective self-report. San Antonio, TX: Psychological Corp. [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, … & Zule W (2003). Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect, 27(2), 169–190. [DOI] [PubMed] [Google Scholar]
- Bowlby J (1978). Attachment theory and its therapeutic implications. Adolescent Psychiatry, 6, 5–33. [PubMed] [Google Scholar]
- Bowlby J (1988). A secure base: Parent-Child attachment and healthy human development. New York, NY: Basic Books. [Google Scholar]
- Bringewatt EH & Gershoff ET (2010). Falling through the cracks: Gaps and barriers in the mental health system for America’s disadvantaged children. Children and Youth Services Review, 32, 1291–1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown J, Cohen P, Johnson JG, & Smailes EM (1999). Childhood abuse and neglect: Specificity of effects on adolescent and young adult depression and suicidality. Journal of American Academy of Child & Adolescent Psychiatry, 38(12), 1490–1496. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, & Rogosch FA (2002). A developmental psychopathology perspective on adolescence. Journal of Consulting and Clinical Psychology, 70, (1), 6–20. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, & Toth SL (2016). Child maltreatment and developmental psychopathology: A multilevel perspective Developmental psychopathology: Maladaptation and psychopathology (3rd ed., Vol. 3, pp. 457–512). Hoboken, NJ: Wiley & Sons. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, & Toth SL (2009). A developmental psychopathology perspective on adolescent depression In Nolen-Hoeksema S & Hilt L (Eds.) Handbook of Adolescent Depression (pp. 3–31). New York: Taylor & Francis. [Google Scholar]
- Cicchetti D, & Toth SL (2006). Developmental Psychopathology and Preventive Intervention In Renninger KA, Sigel IE, Damon W, & Lerner RM (Eds.), Handbook of child psychology: Child psychology in practice (Vol. 4, pp. 497–547). Hoboken, NJ: Wiley & Sons. [Google Scholar]
- Cicchetti D, & Valentino K (2006). An ecological-transactional perspective on child maltreatment: Failure of the average expectable environment and its influence on child development In Cicchetti D & Cohen D (Eds.), Developmental psychopathology: Risk, disorder, and adaptation (2nd ed., Vol. 3, pp. 129–201). Hoboken, NJ: Wiley & Sons. [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Erlbaum. [Google Scholar]
- Cohen JR, McNeil SL, Shorey RC, & Temple JR (2018). Maltreatment subtypes, depressed mood, and anhedonia: A longitudinal study with adolescents. Psychological Trauma: Theory, Research, Practice, and Policy, 11(7), 704–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins KA, & Dozois DJ (2008). What are the active ingredients in preventative interventions for depression? Clinical Psychology: Science and Practice, 15(4), 313–330. [Google Scholar]
- Connell AM (2009). Employing complier average causal effect analytic methods to examine effects of randomized encouragement trials. The American Journal of Drug and Alcohol Abuse, 35(4), 253–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duberstein PR, Ward E.aA,, Chaudron LH, He H, Toth SL, Wang W, VarOrden KA, Gamble SA, & Talbot NL (2018). Effectiveness of interpersonal psychotherapy-trauma for depressed women with childhood abuse histories. Journal of Consulting and Clinical Psychology, 86(10), 868–878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffy F, Sharpe H, & Schwannauer M (2019). The effectiveness of interpersonal psychotherapy for adolescents with depression–a systematic review and meta-analysis. Child and Adolescent Mental Health, 24(4), 307–317. [DOI] [PubMed] [Google Scholar]
- Goodman WK, Murphy TK, & Storch EA (2007). Psychopharmacology, 191, 87–96. [DOI] [PubMed] [Google Scholar]
- Hammen C, & Rudolph KD (2003). Childhood mood disorders. Child Psychopathology, 2, 233–278. [Google Scholar]
- Harkness KL, Bruce AE, & Lumley MN (2006). The role of childhood abuse and neglect in the sensitization to stressful life events in adolescent depression. Journal of abnormal psychology, 115(4), 730–741. [DOI] [PubMed] [Google Scholar]
- Hyman SM, Garcia M, Kemp K, Mazure CM, & Sinha R (2005). A gender specific psychometric analysis of the early trauma inventory short form in cocaine dependent adults. Addictive Behaviors, 30(4), 847–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jo B (2002). Estimation of intervention effects with noncompliance: Alternative model specifications. Journal of Educational and Behavioral Statistics, 27(4), 385–409. [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao UMA, Flynn C, Moreci P, … & Ryan N (1997). Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child & Adolescent Psychiatry, 36(7), 980–988. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent DA, Ryan ND, & Rao U (2000). K-SADS-PL. Journal of the American Academy of Child & Adolescent Psychiatry, 39(10), 1208. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Thornton LM, & Prescott CA (2001). Gender differences in the rates of exposure to stressful life events and sensitivity to their depressogenic effects. American Journal of Psychiatry, 158(4), 587–593. [DOI] [PubMed] [Google Scholar]
- Kim J, & Cicchetti D (2003). Social self-efficacy and behavior problems in maltreated and nonmaltreated children. Journal of clinical child and adolescent psychology, 32(1), 106–117. [DOI] [PubMed] [Google Scholar]
- Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, & Poulton R (2003). Prior juvenile diagnoses in adults with mental disorder: developmental follow-back of a prospective-longitudinal cohort. Archives of general psychiatry, 60(7), 709–717. [DOI] [PubMed] [Google Scholar]
- Klerman GL, Weissman MM, Rounsaville B, & Chevron E (1984). Interpersonal therapy of depression (IPT). New York, NY: Basic Books. [Google Scholar]
- Klomek AB, & Mufson L (2006). Interpersonal psychotherapy for depressed adolescents. Child and Adolescent Psychiatric Clinics, 15(4), 959–975. [DOI] [PubMed] [Google Scholar]
- Kraemer HC (2013). Discovering, comparing, and combining moderators of treatment on outcome after randomized clinical trials: A parametric approach. Statistics in Medicine, 32(11), 1964–1973. [DOI] [PubMed] [Google Scholar]
- Lauth B, Arnkelsson GB, Magnusson P, Skarphéðinsson GÁ, Ferrari P, & Petursson H (2010). Validity of K-SADS-PL (Schedule for Affective Disorders and Schizophrenia for School-Age Children—Present and Lifetime Version) depression diagnoses in an adolescent clinical population. Nordic Journal of Psychiatry, 64(6), 409–420. [DOI] [PubMed] [Google Scholar]
- Layne et al. , 2010,
- Lumley MN, & Harkness KL (2007). Specificity in the relations among childhood adversity, early maladaptive schemas, and symptom profiles in adolescent depression. Cognitive Therapy and Research, 31(5), 639–657. [Google Scholar]
- Maalouf FT, & Brent DA (2012). Child and adolescent depression intervention overview: what works, for whom and how well? Child and Adolescent Psychiatric Clinics, 21(2), 299–312. [DOI] [PubMed] [Google Scholar]
- Markowitz JC, Petkova E, Neria Y, Van Meter PE, Zhao Y, Hembree E, … & Marshall RD (2015). Is exposure necessary? A randomized clinical trial of interpersonal psychotherapy for PTSD. American Journal of Psychiatry, 172(5), 430–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markowitz JC, Neria Y, Lovell K, Van Meter PE, & Petkova E (2017). History of sexual trauma moderates psychotherapy outcome for posttraumatic stress disorder. Depression and Anxiety, 34(8), 692–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten AS (2004). Regulatory processes, risk, and resilience in adolescent development. Annals of the New York Academy of Sciences, 1021(1), 310–319. [DOI] [PubMed] [Google Scholar]
- McCrae JS, Barth RP, & Guo S (2010). Changes in maltreatment children’s emotional-behavioral problems following typically provided mental health services. American Journal of Orthopsychiatry, 80 (3), 350–361. [DOI] [PubMed] [Google Scholar]
- Meyer A (1957). Psychobiology: A science of man. Oxford, England: Charles C Thomas. [Google Scholar]
- Mufson L, Clougherty K, Young J, & Verdeli H (2004). IPT-A Supervision Checklist. New York Psychiatric Institute, Columbia University College of Physicians and Surgeons. [Google Scholar]
- Mufson L, Dorta KP, Moreau D, & Weissman MM (2004). Interpersonal Psychotherapy for depressed adolescents. New York, NY: The Guilford Press. [Google Scholar]
- Muthén LK, & Muthén BO (1998–2018). Mplus user’s guide [computer software]. Los Angeles, CA: Author. [Google Scholar]
- Mychailyszyn MP, & Elson DM (2018). Working through the blues: A meta-analysis on Interpersonal Psychotherapy for depressed adolescents (IPT-A). Children and Youth Services Review, 87, 123–129. [Google Scholar]
- Nanni V, Uher R, & Danese A (2012). Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: a meta-analysis. American Journal of Psychiatry, 169(2), 141–151. [DOI] [PubMed] [Google Scholar]
- Norman RE, Byambaa M, De R, Butchart A, Scott J, & Vos T (2012). The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS Medicine, 9(11), e1001349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Post RM (1992). Transduction of psychosocial stress into the neurobiology of recurrent affective disorder. The American Journal of Psychiatry, 149(8), 999–1010. [DOI] [PubMed] [Google Scholar]
- Pu J, Zhou X, Liu L, Zhang Y, Yang L, Yuan S, … & Xie P (2017). Efficacy and acceptability of interpersonal psychotherapy for depression in adolescents: a meta-analysis of randomized controlled trials. Psychiatry Research, 253, 226–232. [DOI] [PubMed] [Google Scholar]
- Rafaeli AK, & Markowitz JC (2011). Interpersonal Psychotherapy (IPT) for PTSD: A case study. American Journal of Psychotherapy, 65(3), 205–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth A, & Fonagy P (2005). What works for whom?: A critical review of psychotherapy research (2nd ed.). New York, NY: Guilford Press. [Google Scholar]
- Rushton JL, Forcier M, & Schectman RM (2002). Epidemiology of depressive symptoms in the National Longitudinal Study of Adolescent Health. Journal of the American Academy of Child & Adolescent Psychiatry, 41(2), 199–205. [DOI] [PubMed] [Google Scholar]
- Shenk CE, Noll JG, Putnam FW, & Trickett PK (2010). A prospective examination of the role of childhood sexual abuse and physiological asymmetry in the development of psychopathology. Child Abuse & Neglect, 34(10), 752–761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stapleton LM, Sander JB, & Stark KD (2007). Psychometric properties of the Beck Depression Inventory for Youth in a sample of girls. Psychological Assessment, 19(2), 230–235. [DOI] [PubMed] [Google Scholar]
- Steinberg AM, Brymer MJ, Kim S, Ghosh C, Ostrowski SA, Gulley K,, Briggs EC, Pynoos RS (2013). Psychometric properties of the UCLA PTSD Reaction Index: Part 1, Journal of Traumatic Stress, 26, 1–9. [DOI] [PubMed] [Google Scholar]
- Steinberg AM, Brymer M, Decker K, & Pynoos RS (2004). The UCLA PTSD Reaction Index. Current Psychiatry Reports, 6, 96–100. [DOI] [PubMed] [Google Scholar]
- Steinberg L, Dahl R, Keating D, Kupfer DJ, Masten AS, & Pine DS (2006). The study of developmental psychopathology in adolescence. Developmental Psychopathology, 2, 710–742. [Google Scholar]
- Sullivan HS (1953). The interpersonal theory of psychiatry. New York, NY: WW Norton. [Google Scholar]
- Toth SL, Manly JT, Asarnow J, & Goldston D (April, 2017). Innovative trauma-informed approaches to depression and suicide prevention National Center for Child Traumatic Stress Network All-Network Conference, Arlington, VA. [Google Scholar]
- Toth SL, Rogosch FA, Oshri A, Gravener-Davis J, Sturm R, & Morgan-López AA (2013). The efficacy of interpersonal psychotherapy for depression among economically disadvantaged mothers. Development and Psychopathology, 25(4pt1), 1065–1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vachon DD, Krueger RF, Rogosch FA, & Cicchetti D (2015). Assessment of the harmful psychiatric and behavioral effects of different forms of child maltreatment. JAMA Psychiatry, 72(11), 1135–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker EA, Unutzer J, Rutter C, Gelfand A, Saunders K, VonKorff M, … & Katon W (1999). Costs of health care use by women HMO members with a history of childhood abuse and neglect. Archives of General Psychiatry, 56(7), 609–613. [DOI] [PubMed] [Google Scholar]
- Warmingham JM, Handley ED, Rogosch FA, Manly JT, & Cicchetti D (2019). Identifying maltreatment subgroups with patterns of maltreatment subtype and chronicity: A latent class analysis approach. Child Abuse & Neglect, 87, 28–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weersing VR, Jeffreys M, Do MCT, Schwartz KT, & Bolano C (2017). Evidence base update of psychosocial treatments for child and adolescent depression. Journal of Clinical Child & Adolescent Psychology, 46(1), 11–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weersing VR, Schwartz KT, & Bolano CARL (2015). Moderators and mediators of treatments for youth with depression In Maric M, Prins PJM, and Ollendick TH (Eds.), Moderators and mediators of youth treatment outcomes (pp. 65–96). New York, NY: Oxford University Press. [Google Scholar]
- Weersing VR, Shamseddeen W, Garber J, Hollon SD, Clarke GN, Beardslee WR, Gladstone TR, Lynch FL, Porta G, Iyengar S, & Brent DA (2016). Prevention of depression in at-risk adolescents: Predictors and moderators of acute effects. Journal of American Academy of Child and Adolescent Psychiatry, 55 (3), 219–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisz JR, & Hawley KM (2002). Developmental factors in the treatment on adolescents. Journal of Consulting and Clinical Psychology, 70(1), 21. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Kuppens S, Ng MY, Eckshtain D, Ugueto AM, Vaughn-Coaxum R, … & Weersing VR (2017). What five decades of research tells us about the effects of youth psychological therapy: a multilevel meta-analysis and implications for science and practice. American Psychologist, 72(2), 79–117. [DOI] [PubMed] [Google Scholar]
- Wichstrøm L (1999). The emergence of gender difference in depressed mood during adolescence: The role of intensified gender socialization. Developmental Psychology, 35(1), 232–245. [PubMed] [Google Scholar]
- Widom CS, DuMont K, & Czaja SJ (2007). A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up. Archives of General Psychiatry, 64(1), 49–56. [DOI] [PubMed] [Google Scholar]
- Yoshikawa H, Aber JL, & Beardslee WR (2012). The effects of poverty on the mental, emotional, and behavioral health of children and youth: Implications for prevention. American Psychologist, 67(4), 272. [DOI] [PubMed] [Google Scholar]
- Young JF, Mufson L, & Davies M (2006). Efficacy of interpersonal psychotherapy-adolescent skills training: An indicated preventive intervention for depression. Journal of Child Psychology and Psychiatry, 47(12), 1254–1262. [DOI] [PubMed] [Google Scholar]
- Yuan KH, & Bentler PM (2000). 5. Three likelihood-based methods for mean and covariance structure analysis with nonnormal missing data. Sociological Methodology, 30(1), 165–200. [Google Scholar]
- Zhou X, Hetrick SE, Cuijpers P, Qin B, Barth J, Whittington CJ, … & Zhang Y (2015). Comparative efficacy and acceptability of psychotherapies for depression in children and adolescents: A systematic review and network meta-analysis. World Psychiatry, 14(2), 207–222. [DOI] [PMC free article] [PubMed] [Google Scholar]


