Highlights
-
•
Pneumatosis cystoides intestinalis is a rare condition with a broad spectrum of clinical symptoms.
-
•
Images are typically striking, which can confuse the medical team and lead to unnecessary procedures.
-
•
Close follow up is needed as complications can lead to a troublesome outcome.
Keywords: Pneumatosis cystoides intestinalis, Pneumoperitoneum, Laparoscopy
Abstract
Background
Pneumatosis cystoides intestinalis (PCI) is a rare condition characterized by gas infiltration into the intestine wall. When gas is seen in the intestinal wall, it is usually a sign of bowel wall infarction and a surgical emergency; therefore, an adequate differentiation of benign and urgent conditions of pneumatosis intestinalis is necessary to prevent misdiagnosis and inadequate therapies.
Case presentation
We present the case of a 79-year-old male with past medical history of Alzheimer’s, cholecystectomy, and umbilical hernia. PCI was identified, and conservative therapy was started. Since the patient's pain persisted, a complication was suspected, and surgery was decided. After successful treatment, the patient completely recovered.
Conclusion
There are many benign and life-threatening causes of pneumatosis intestinalis, the imaging appearance of both may look very similar. Therefore, clinical history, physical examination, and laboratory test results are the best indicators of whether it is due to a benign or life-threatening cause. PCI must be managed with a multidisciplinary team of clinicians, radiologists, and surgeons to achieve better results for our patients.
1. Introduction
Intestinal Pneumatosis (IP) is a pathological condition characterized by the presence of gas within the intestinal wall that is usually seen on computed tomography (CT) [1,2]. This finding in adults has been considered indicative of advanced intestinal infarction; However, this same sign can be seen in a rare condition called Pneumatosis cystoides intestinalis (PCI), unlike other pathologies, this condition is treated with conservative and supportive therapies. Surgery is required if complications appear so close follow up and monitoring is vital [2,3].
We present the case of a 79-year-old male with PCI. Conservative therapy was started, yet as the patient's pain persisted, a complication was suspected, and surgery was decided. After successful treatment, the patient completely recovered.
This work has been reported in line with the SCARE criteria [12].
2. Case report
Patient is a 79-year-old male with past medical history of Alzheimer's, cholecystectomy, and umbilical hernia. His family brought him to the emergency room with a 48-h history of acute lower abdominal pain and distension. He had experienced this same pain in the past five years. Nonetheless, he didn't seek medical attention as the pain faded away spontaneously. He also reported weight loss (15 kg in the last year) and had recurrent but brief episodes of biliary vomits.
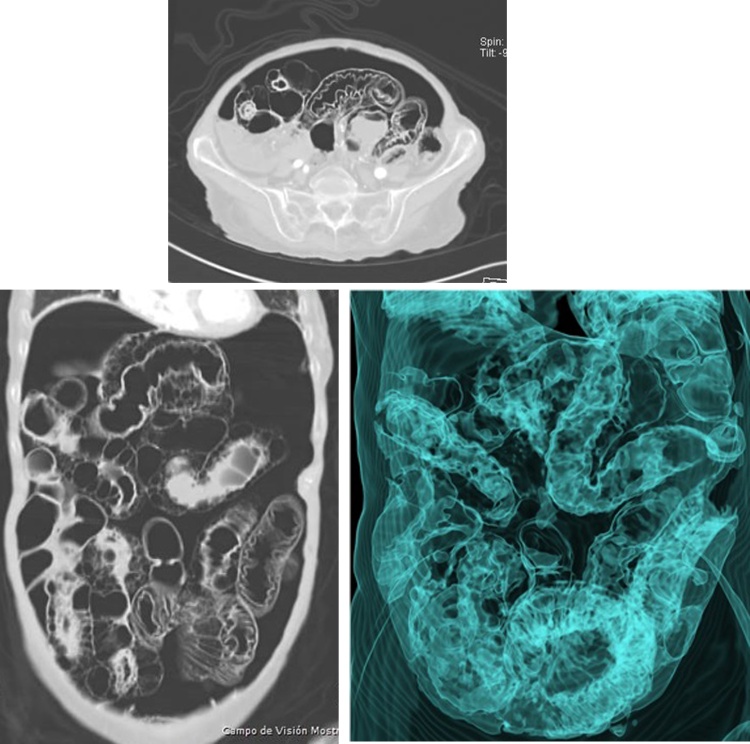
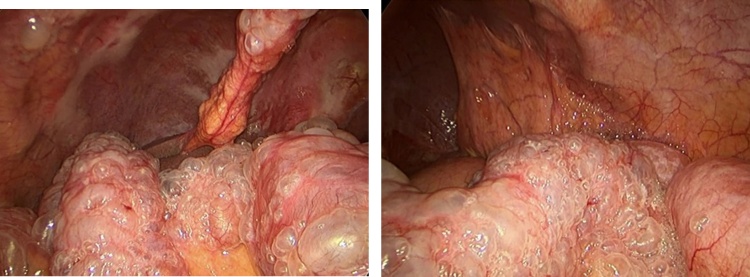
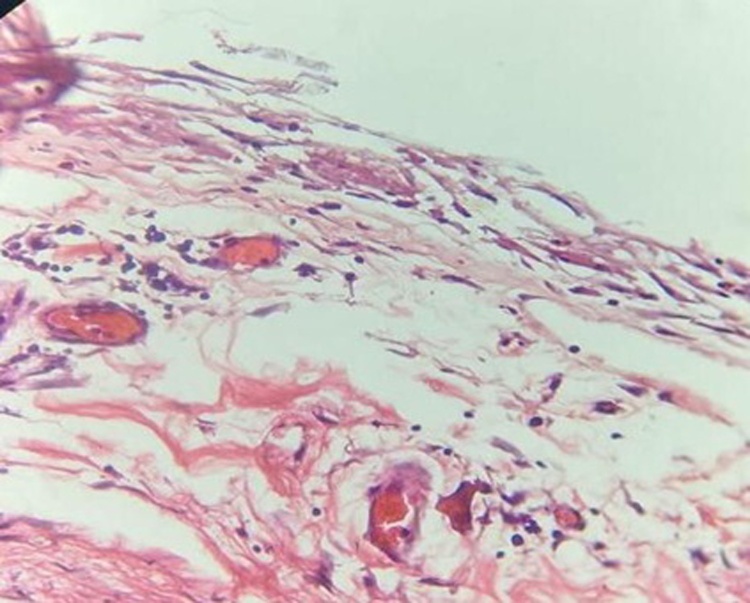
On clinical examination, a malnourished and tachycardic patient was encountered. His abdomen was distended, and he had mild pain on his lower abdomen without tenderness. Complementary exams revealed a normal white blood count (7.810 mm3) with neutrophilia 86.8%, an elevated C-reactive protein (110 mg/dl), no acidosis or hyperlactatemia. Due to this, a contrast-enhanced computed tomography (CT) was requested, revealing a bubbly pattern across the length of the small bowel, multiple cystic round shapes in the wall of the jejunum, and its mesentery, and a large pneumoperitoneum. No signs of pneumobilia, gas in the portal venous system, or free liquid were detected (Fig. 1A–C). Pneumatosis cystoides intestinalis was suspected, and he was admitted for close surveillance, oxygen, and broad-spectrum antibiotics. Despite this, his pain worsened, and a complication was suspected; thus, surgery was decided. At laparoscopy, the whole length of the small bowel was surrounded by multiple 1 × 1 cm gas-filled cystic lesions on its serosa. However, no evidence of perforation was detected. A small biopsy of the small bowel mesentery was taken, and the procedure was completed without complications (Fig. 2A–C). Pathology reported chronic inflammation with fibrosis of the serosa (Fig. 3). Pneumatosis cystoides intestinalis was the final diagnosis. Postoperatively the patient completed a five-day course of intravenous metronidazole and oxygen. On follow-up and six months, post-surgery the patient is doing well without any complications. An upper and lower endoscopy was completed after surgery, which were normal.
Fig. 1.
A: CT, pneumatosis cystoides intestinalis is seen on the bowel wall. B: CT, revealing massive pneumoperitoneum. C: CT reconstruction revealing multiple cysts on the bowel wall.
Fig. 2.
A: Laparoscopy, revealing cystic lesion on the bowel. B: Laparoscopy, lesions on the bowel wall, and falciform ligament.
Fig. 3.
Pathology, the chronic inflammatory reaction is seen with mild inflammatory infiltrate.
(Hematoxylin eosin 40×).
3. Discussion
Pneumatosis cystoides intestinalis (PCI), is a rare disease (0.03% of the adult population) self-limited process, in which the intestinal submucosa and subserosa are filled with gas-filled cysts [1]. DuVernoi et al. first described this condition in 1783, and its pathogenesis remains unclear to this day [2,3]. It is thought that the cysts appear due to chronic inflammation, physical damage to the intestine, nutritional imbalances, dysbacteriosis, gastrointestinal dysmotility, immune dysfunctions, postsurgery, chemotherapy, scleroderma, and pulmonary illness [1,3]. Although not proved, there is the assumption that the gas enters the tissue form a defect in the epithelial layer of the bowel; nevertheless, the areas of gas are generally in areas without any ulcers, other theories involve the lungs or an increase in the aerogenic bacterias [1,4]. PCI usually has a preference for middle age (45.3 ± 15.6 years) male patients (2.4: 1 male to female ratio) [1,2,5]. In our case, the patient was a 79-year-old male with Alzheimer’s, a history of weight loss, and an umbilical hernia.
The cysts can appear anywhere within the gastrointestinal tract, (large intestine 46%, small intestine 27%, stomach 5%, mixed 7%), nonetheless, they are usually located in the terminal ileum but has been found in rare places like the mesentery, omentum, and ligamentum hepatogastricum [1,6]. PCI has a broad spectrum of clinical symptoms, from asymptomatic patients to non-specific gastrointestinal symptoms. (Diarrhea, abdominal distention, weight loss, among others) [6,7]. Our patient had a history of abdominal pain and weight loss; the cysts were discovered all over the bowel wall.
Endoscopy is an invaluable tool that can aid the diagnosis, mainly as biopsies can be obtained and distinguish PCI from other diseases like polyps, carcinoma, lymphoma, liquid cysts, Gardner syndrome, and Cronkhite-Canada syndrome [8]. Nonetheless, CT has a clear advantage since the gas can be seen in the cysts and in the portal venous system or as pneumoperitoneum; thus, it can be of great assistance in revealing possible complications [1,8]. About 3% of the patients with PCI can present with pneumoperitoneum, volvulus, intestinal obstruction, or ischemia, which may alter the usual therapy course [9]. Pathology of usually reveal giant cell arrays and partial or collapsed cysts.
The finding of pneumatosis intestinalis should raise the clinician’s concern about the development of life-threatening conditions [10]. Ominous signs and symptoms include abdominal pain, peritoneal signs, and laboratory abnormalities such as an elevated white blood cell count and acidosis.
Conservative management is usually the treatment of choice [1,6,11]. Oxygen and antibiotics are often sufficient (70% of remission), nonetheless as these cases are rare, misdiagnosis can occur, which can lead to unnecessary procedures; however, surgery must be considered if peritoneal irritation or bowel obstruction appears [1,2].
In our case, the patient had a CT with grape-like cysts all over the bowel wall and pneumoperitoneum. Conservative management was the initial treatment, yet as the pain persisted, a complication was suspected, and surgery was decided, nonetheless as no signs of perforation were identified, a biopsy was taken without complications.
4. Conclusions
Due to its rarity and its broad spectrum of clinical symptoms, PCI can be easily misdiagnosed. Since the radiographic images are usually striking, the medical team must always rely on clinical history, physical examination, laboratory, and imaging tests to formulate life-saving clinical decisions and to prevent troublesome complications. If doubts exist or there is clinical worsening, surgical consultation is mandatory.
Declaration of Competing Interest
The authors declares that there is no conflict of interest regarding the publication of this article.
Sources of funding
The authors have no funding to report.
Ethical approval
The authors declare that we obtained permission from the ethics committee in our institution.
Consent
The authors declare that written consent was obtained from the patient before publication of this case.
Author contribution
Fernando X. Moyon Conceptualization.
Gabriel A. Molina Conceptualization.
Jorge F. Tufiño Conceptualization; Data curation; Formal analysis.
Veronica M. Basantes Conceptualization; Data curation; Formal analysis.
Darwin S. Espin Data curation.
Miguel A. Moyon Data curation.
Jaime M. Cevallos Data curation; Formal analysis.
Néstor Enrique Data curation; Formal analysis.
Ruben Parra Data curation; Formal analysis.
Karla Rosalía Eras Data curation; Formal analysis.
Registration of research studies
The authors declare that the patient gave his consent to publish this case, and as this is a case report not human participants were involved in a study.
Guarantor
Gabriel A. Molina.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Contributor Information
Fernando X. Moyon, Email: xavomcons@hotmail.com.
Gabriel A. Molina, Email: gabomolina32@gmail.com.
Jorge F. Tufiño, Email: jorguetufino@msn.com.
Veronica M. Basantes, Email: veronica_basantes@yahoo.es.
Darwin S. Espin, Email: postgsantiago@hotmail.com.
Miguel A. Moyon, Email: mmoyon.surgeon@gmail.com.
Jaime M. Cevallos, Email: marceloc-71@hotmail.com.
Néstor E. Palacios, Email: ecnestormd@gmail.com.
Ruben A. Parra, Email: rpmontenegro@gmail.com.
Karla R. Eras, Email: karla.1990.eras@gmail.com.
References
- 1.Wang Yjuan, Wang Yming, Zheng Ymin, Jiang Hqing, Zhang J. Pneumatosis cystoides intestinalis: six case reports and a review of the literature. BMC Gastroenterol. 2018;18(1) doi: 10.1186/s12876-018-0794-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Turnure P.R. Gas cysts of the intestine. Ann. Surg. 1913;57(6):811–839. doi: 10.1097/00000658-191306000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ling F., Guo D., Zhu L. Pneumatosis cystoides intestinalis: a case report and literature review. BMC Gastroenterol. 2019;19(1) doi: 10.1186/s12876-019-1087-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tchabo N., Grobmyer S., Jarnagin W., CHI D. Conservative management of pneumatosis intestinalis. Gynecol. Oncol. 2005;99(3):782–784. doi: 10.1016/j.ygyno.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 5.Molina G.A., Fuentes G., Orejuela M.E., Herrera J.M., Jiménez G.E., Pinto J.C., Cobo M.M. Pneumatosis cystoides intestinalis in an elderly patient, better to be safe than sorry. J. Surg. Case Rep. 2020;2020(4) doi: 10.1093/jscr/rjaa053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Keene J.G. Pneumatosis cystoides intestinalis and intramural intestinal gas. J. Emerg. Med. 1989;7(6):645–650. doi: 10.1016/0736-4679(89)90013-9. [DOI] [PubMed] [Google Scholar]
- 7.Chiu C.-C., Siao F.-Y., Yen H.-H. Pneumatosis intestinalis. J. Emerg. Med. 2015;49(4):e137–e138. doi: 10.1016/j.jemermed.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 8.Lassandro F., di Santo Stefano M.L.M., Maria Porto A., Grassi R., Scaglione M., Rotondo A. Intestinal pneumatosis in adults: diagnostic and prognostic value. Emerg. Radiol. 2010;17(5):361–365. doi: 10.1007/s10140-010-0868-9. [DOI] [PubMed] [Google Scholar]
- 9.Ko S., Hong S.S., Hwang J., Kim H., Chang Y.-W., Lee E. Benign versus life-threatening causes of pneumatosis intestinalis: differentiating CT features. Rev. Assoc. Méd. Bras. 2018;64(6):543–548. doi: 10.1590/1806-9282.64.06.543. [DOI] [PubMed] [Google Scholar]
- 10.St. Peter S.D. The spectrum of pneumatosis intestinalis. Arch. Surg. 2003;138(1):68. doi: 10.1001/archsurg.138.1.68. [DOI] [PubMed] [Google Scholar]
- 11.Ho L.M., Paulson E.K., Thompson W.M. Pneumatosis intestinalis in the adult: benign to life-threatening causes. Am. J. Roentgenol. 2007;188(6):1604–1613. doi: 10.2214/ajr.06.1309. [DOI] [PubMed] [Google Scholar]
- 12.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A., Orgill D.P., For the SCARE Group The SCARE 2018 statement: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]