Abstract
Iliopsoas bursitis is characterized by distension of the iliopsoas muscle bursa due to synovial fluid and/or hypertrophic synovium. Hip disease is usually associated with it, however, isolated bursitis is also present. Clinically Diagnosing iliopsoas bursitis can be difficult, and imaging is usually required to differentiate iliopsoas bursitis from other inguinal masses such as lymphadenopathy, hernias, and tumors. We present the case of a 45-year-old athletic patient who underwent diagnostic examination for recurrent right hip pain and a recent development (last 3 months) of a bulky right inguinal mass.
Keywords: CT, US, Bursitis, Echo-guided aspiration, Interventional musculoskeletal radiology, Synovitis
Introduction
The iliopsoas (or iliopectineal) bursa is the largest synovial bursa in the body, and is present and bilateral in 98% of adults [1], [2]. It is located between the iliopsoas muscle and the anterior capsule of the hip, this structure is collapsed. The bursa is placed in front of the hip joint, it is adjacent to the thinnest and most vulnerable portion of the anterior capsule and reduces tendon friction over the hip joint during muscle activation and joint movement [3], [4]. Iliopsoas bursitis is characterized by distension of the iliopsoas muscle bursa due to synovial fluid and / or hypertrophic synovium [5], [6]. Hip disease is usually associated with it, however isolated bursitis is also present. In some cases iliopsoas bursitis looks like a mass in the groin or inguinal region [4], [5], [6]. Diagnosing iliopsoas bursitis clinically can be difficult, and imaging is usually required to differentiate iliopsoas bursitis from other inguinal masses such as lymphadenopathy, hernias and tumors. They have been published several articles from the beginning of the middle 1900 describing iliopsoas bursitis [1], [2], [3], [4], [5], [6], [7]. We present the case of a 45-year-old athletic patient who underwent diagnostic examination for recurrent right hip pain and a recent development (last 3 months) of right inguinal masses.
Case
A 45-year-old man performed diagnostic tests at our clinic for recurrent right hip pain prevalent at rest for about 12 months and a recent development (last 3 months) of right inguinal masses. The patient is a semiprofessional runner and he had no other diseases. We performed a clinical examination that showed pain on palpation and active and passive hip movements and confirmed a voluminous left inguinal mass. The joint was not swollen, erythematous without increase in temperature compared to the contralateral hip. The other axile and appendicular joints showed no signs of inflammation. The patient had no fever or other symptoms. Blood pressure was 115/80 mmHg. The complet blood count, liver, kidney, and thyroid function were normal. The inflammation indices (V.E.S. and PCR) had increased. There were normal serum values of uric acid, parathyroid hormone, calcium, phosphate, and magnesium. Tumor markers, ANA, and Rheumatoid Factor were negative. The CT examination performed without contrast medium showed the presence of voluminous hypodense lesion, the size of 34 × 27 × 30 mm (d.t. x d.a.p. x d.l.), which was located between the iliopsoas muscle and the left coxo femoral joint capsule. The CT exam didn't show joint bone injury or intra-articular effusion.
The lesion was inhomogeneously hypodense regarding the corpuscular fluid content with evidence of periferal solid nodules and septa. The iliopsoas muscle was located forward but there were no lesions or alterations to the trophism. CT excluded the presence of lymphadenopathies, tumors, thrombosis, or hernias. The finding was suspicious due to distension of the iliopsoas bursa and synovial thickening, in relation to a chronic bursitis of overuse but an ultrasound examination was useful (Fig. 1a–1b). The high frequency ultrasound examination (12 mHz) confirmed the presence of the voluminose fluid-corpuscular distension of the bursa, thickening and proliferation of the synovium, hyperecoic punctiform deposits in the synovial membrane. The P. Doppler examination showed a significant increase in the vascular signal of the synovium. Tendons and muscles in the region examined were normal. The diagnosis was perfected with the withdrawal of the synovial fluid. It was subjected to microbiological, cytological and chemical-physical examination with an increase in leukocytes in accordance with the suspicion of bursitis. The patient was subsequently treated with ice, functional rest and oral corticosteroids without success. Therefore it was subjected to 6 ultrasound-guided intra-articular aspiration and infiltrative therapy of corticosteroids and physiotherapy with excellent results on the symptoms. He is currently in good condition and he performs 6-monthly clinical and ultrasound follow-up (Fig. 2–4).
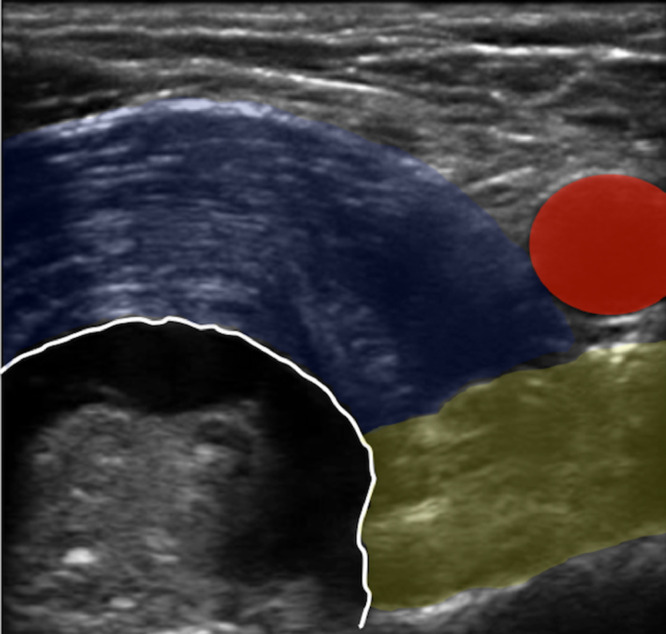
Fig. 3.
US axial plane show bursa with synovial ipertrophy and iliopsoas muscle (blue), pectineal muscle (yellow) and femoral common artery (red).
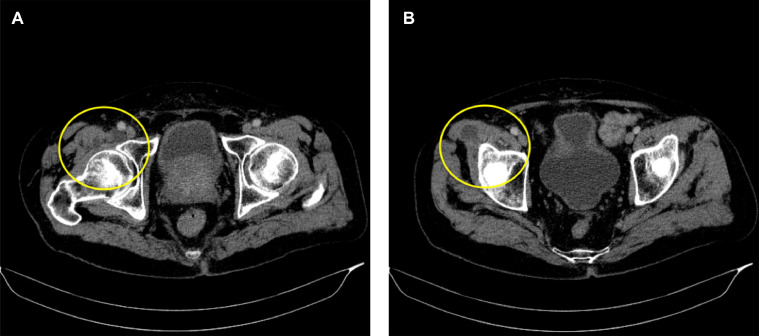
Fig. 1a-1b.
CT exam performed without contrast medium. Axial plane shows the voluminous fluid relaxation of the right iliopsoas bursa (circle).
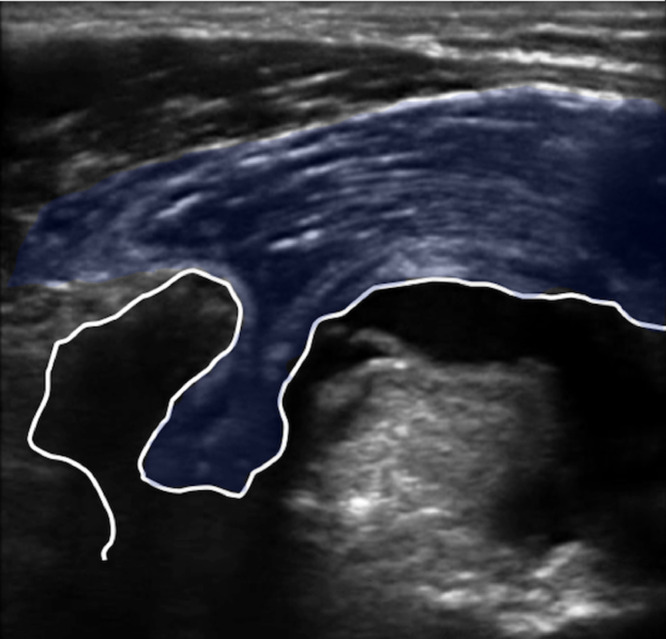
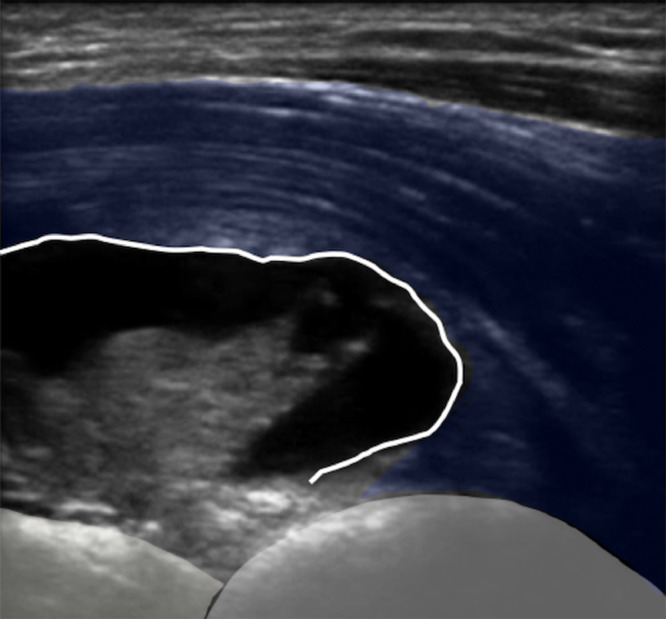
Fig. 2-4.
US longitudinal plane show iliopsoas bursa with synovial ipertrophy (fig-2-4), (blue) iliopsoas muscle (fig-2-4) and (grey) femoral head and iliac bone (fig 4).
Discussion
The iliopsoas bursa is normally a potential space. Communication between the iliopsoas bursa and the hip joint is present in 15% of individuals and can be congenital or acquired [4], [5], [6], [7], [8]. Gatc and Green described the connection acquired between bursa and the joint capsule and the presence of hip pathology [1], [2], [3], [4], [5], [6], [7], [8], [9]. One or more pathological mechanisms could contribute to this communication, including increased intra-articular pressure, friction from the overlying iliopsoas tendon, a capsule weakened by inflammation, arthritic degeneration, or osteonecrosis of the hip. Very often it can be associated with snap hip syndrome. It is a sign characterized by a snap sensation during movement and not always associated with pain. In the absence of hip diseases, inflammation and distension of the iliopsoas bursa can be caused by rheumatological diseases, gout, infection, trauma, or overuse injuries. Sometimes both described pathological conditions can be concurrent. Iliopsoas bursitis can be asymptomatic or cause various symptoms related to compression of adjacent vascular and nerve structures: lower limb edema, paresthesias, and thrombosis. Iliopsoas bursitis is an infrequent cause of hip pain. It's important note that often, iliopsoas bursitis and tendinitis are related as the inflammation of one will inevitably lead to inflammation of the other because of their proximity [4], [5], [6]. This condition it is often referred to as iliopsoas syndrome [1], [2], [3], [4], [5], [6], [7], [8], [9]. Although iliopsoas bursitis is a deep anatomical structure, it can sometimes cause swelling of the hip joint and must be placed in differential diagnosis with intraperitoneal hernias content, tumors, aneurysms of the iliac or common femoral vessels, and lymphadenopathy. In both situations, the position of the deep bursa to the iliopsoas muscle often delays the diagnosis [1], [2], [3]. Differential clinical diagnosis is difficult and imaging is indispensable [10], [11], [12] .US is certainly the first level imaging technique utilized due to its inexpensive costs, the wide diffusion of the equipment on the territory, and the scarce contraindications [13], [14], [15]. US examination allows detecting the structural characteristics and the vascular behavior of the bursa. The dimensions, the presence of septa and thickening and proliferation of the synovium, as well as the presence of increased vascularization, are all signs of suspected malignancy. In our case, US allowed to quantify the bursa fluid, the synovial thickening, the structural conditions of tendons, ligaments and muscles. We have excluded the presence of thrombosis, tumors, and lymphadenopathies. The study of P. Doppler allowed identifying the degree of hyperemia of the tissues involved. In addition, ultrasound allows you to perform diagnostic and therapeutic procedures [15], [16]. The CT and MRI examinations evaluate the spatial and dimensional relationships, as well as to characterize of the bursa and the presence of septa or synovial thickenings. The US, CT, and MRI have an increasing role in the detection and diagnosis of iliopsoas bursitis. It is advisable to aspirate echo-guided the synovial fluid and subject it to infectious, cytological and chemical-physical analyzes. For a correct treatment of iliopsoas bursitis it is essential to determine its etiology. As in our case, interventional radiology techniques can be a valid therapeutic choice (Figure 4).
Fig. 4.
Conflict of interest
-
•
We confirm that this work is original and has not been published elsewhere nor is it currently under consideration for publication elsewhere.
-
•
Publication is approved by all authors and by the responsible authorities where the work was carried out.
-
•
Each author has participated sufficiently in any submission to take public responsibility for its content.
-
•
The authors have no conflicts of interest.
-
•
Written informed consent was obtained from all patients, and the study was approved by the ethics committee of the institution.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.radcr.2020.08.036.
Appendix. Supplementary materials
Video 1-2: Voluminous iliopsoas bursa with synovial ipertrophy in US longitudinal plane (video 1) and in axial plane (video 2)
References
- 1.Johnston 1 C.A., Wiley J.P., Lindsay D.M., Wiseman D.A. Iliopsoas bursitis and tendinitis. Sports Med. 1998;25(4):271–283. doi: 10.2165/00007256-199825040-00005. [DOI] [PubMed] [Google Scholar]
- 2.O'Connor Early recognition of iliopectineal bursitis. Surg Gynecol Obstet. 1933;57:674–684. [Google Scholar]
- 3.Bianchi Stefano, Martinoli Carlo, Keller Alain, Bianchi‐Zamorani Maria Pia. Giant iliopsoas bursitis: Sonographic findings with magnetic resonance correlations. J Clin Ultrasound. 2002;30(7):437–441. doi: 10.1002/jcu.10093. [DOI] [PubMed] [Google Scholar]
- 4.Ginesty E., Dromer C., Galy-Fourcade D. Iliopsoas bursopathies. A review of twelve cases. Revue du Rhumatisme English Edition. 1998;65:181. [PubMed] [Google Scholar]
- 5.Pellman E., Kumari S., Greenwald R. Rheumatoid iliopsoas bursitis presenting as unilateral leg edema. J Rheumatol. 1986;13:197. [PubMed] [Google Scholar]
- 6.Janus C., Hermann G. Enlargement of the iliopsoas bursa: unusual cause of cystic mass on pelvic sonogram. J Clin Ultrasound. 1982;10:133. doi: 10.1002/jcu.1870100310. [DOI] [PubMed] [Google Scholar]
- 7.Pec′ina M.M., Bojanic′ I. CRC Press; Boca Raton: 1982. Overuse injuries of the musculoskeletal system; pp. 143–147. [Google Scholar]
- 8.Salmeron I., Cardenas J.L., Ramirez-Escobas M.A. Idiopathic iliopsoas bursitis. Eur Radiol. 1999;9:175. doi: 10.1007/s003300050652. [DOI] [PubMed] [Google Scholar]
- 9.Finder J.G. lliopectineal bursitis. Arch Surg. 1938;36:519–530. [Google Scholar]
- 10.Corvino Antonio, Setola Sergio Venanzio, Sandomenico Fabio, Corvino Fabio, Catalano Orlando. Synchronous tumours detected during cancer patient staging: prevalence and patterns of occurrence in multidetector computed tomography. Pol J Radiol. 2020;85:e261–e270. doi: 10.5114/pjr.2020.95781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Catelli Antonio, Pane Francesco, Liccardo Alessandro, Tafuri Domenico. Giant right-side inguinal hernia: anatomo-clinical and diagnostic considerations of a case. Acta Medica Mediterranea. 2020;36:439. [Google Scholar]
- 12.Corvino Antonio, Caruso Martina, Varelli Carlo, Gennaro Francesca Di, Pignata Saverio, Corvino Fabio. Diagnostic imaging of parotid gland oncocytoma: a pictorial review with emphasis on ultrasound assessment. J Ultrasound. 2020;36:439. doi: 10.1007/s40477-020-00511-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Catelli Antonio, Ponsiglione Andrea, Capaldo Iolanda, Corvino Antonio, Radice Leonardo, Venetucci Pietro. Giant endometriod ovarian cancer: the role of dagnostic imaging and figo staging. Euro Mediterranean Biomedical Journal. 2020;15(22):94–96. [Google Scholar]
- 14.Catelli Antonio, Loiudice Giovanni, Corvino Antonio, Castaldo Anna, Bracale Umberto Marcello, Quarantelli Mario. Amplatzer vascular plug IV in the treatment of high flow renal arteriovenous fistula: case considerations. Radiol Case Rep. 2020;15(9):1442–1445. doi: 10.1016/j.radcr.2020.05.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Corvino A., Catelli A., Trovato P., Pane F., Corvino F. Volar ganglion cyst of the wrist simulating a radial artery pseudoaneurysm: A case report. Euro Mediterranean Biomedical Journal. 2020;(15):90–93. [Google Scholar]
- 16.Corvino A., Catalano O., de Magistris G., Corvino F., Giurazza F., Raffaella N., Vallone G. Usefulness of doppler techniques in the diagnosis of peripheral iatrogenic pseudoaneurysms secondary to minimally invasive interventional and surgical procedures: imaging findings and diagnostic performance study. J Ultrasound. 2020 doi: 10.1007/s40477-020-00475-6. . [Epub Ahead of Print] [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video 1-2: Voluminous iliopsoas bursa with synovial ipertrophy in US longitudinal plane (video 1) and in axial plane (video 2)