Abstract
Acute Respiratory Distress Syndrome (ARDS) is a form of respiratory failure in human. The number of deaths caused by SARS-CoV-2 infection inducing this severe pneumonia (ARDS) is relatively high. In fact, COVID-19 might get worsen in ARDS and provoke respiratory failure. A better understood of ARDS key features and the pathophysiological injuries of the pulmonary parenchyma are linked to lessons learned from previous severe diseases associated previous coronaviruses outbreaks (especially SARS-CoV and MERS-CoV) and more the ongoing SARS-CoV-2. The ARDS mechanism includes a diffuse alveolar damage associated disruption of alveolar capillary membrane, pulmonary edema, damaged endothelium and increased permeability. A diffuse inflammation, with acute onset, on the lung tissue accompanied by release of biochemical signal and inflammatory mediators (TNFα, IL-1 and IL-6) leading to hypoxemia, low PaO2/FiO2 ratio and the chest radiological expression of bilateral infiltrates in ARDS. The ongoing outbreak could lead to a better understood of ARDS pathophysiology and prognostic. An overview is also highlighted about the seven coronaviruses proved to infect human especially those having ability to cause severe disease SARS-CoV, MERS-CoV and SARS-CoV-2. In this review, we focused on the major pathological mechanisms leading to the ARDS development as a result of viral infection, severe COVID-19 worsening.
Communicated by Ramaswamy H. Sarma
Keywords: SARS-CoV-2, ARDS, COVID-19, coronavirus, pathophysiology, ACE2
1. Introduction
A cluster of novel pneumonia cases has emerged in Wuhan-China on December 2019 and by the end of the 1st week in January, the Chinese authorities reported its association with a novel coronavirus. The novel coronavirus, finally named as Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) by the International Committee on Taxonomy of Viruses, and it’s inducing Coronavirus Disease 2019 (COVID-19) (Gorbalenya et al., 2020; Khailany et al., 2020). The world health organization (WHO) confirmed the transmissibility of the novel coronavirus from human to human. Similarly, to SARS-CoV and MERS-CoV, the ongoing coronavirus (SARS-CoV-2) could cause disease with severe symptoms. SARS-CoV-2 has been, already, considered to be as a sister virus to SARS-CoV based on similarities to their hole genome sequences (Su et al., 2016; Khailany et al., 2020). The major common symptoms include fever, cough, difficult (short and rapid) breathing and myalgia or muscular fatigue. While SARS-CoV-2 induces mild symptoms in several infected patients (low pathogenic), it can also be associated with a fast onset of widespread infection in the lungs worsened in an acute respiratory distress syndrome (ARDS) (Chen et al., 2020).
2. Coronaviruses and SARS-CoV-2 infection inducing COVID-19
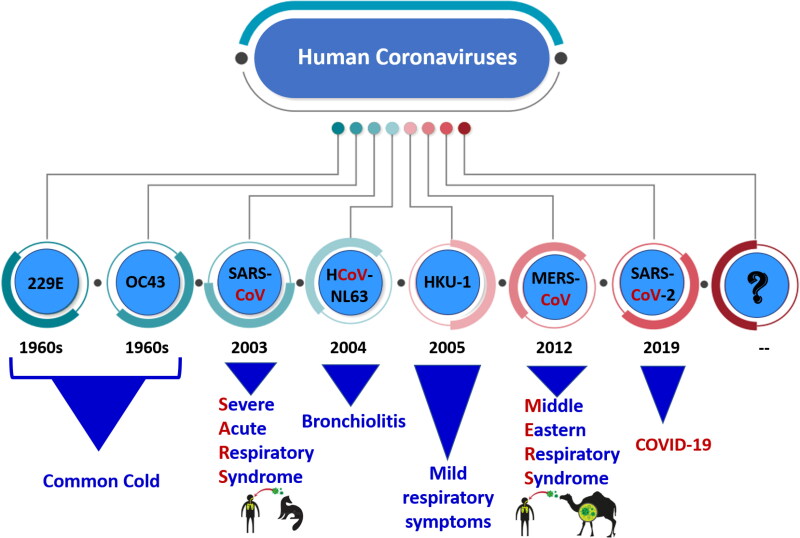
Coronaviruses is a large family (Coronaviridae) of viruses for which the transmission from human to human is possible. This family of viruses has a simple-strand RNA genome of 26 to 32 kb (Lu et al., 2020). Coronaviruses were identified in different animal including birds and mammals such as cat, dogs, bats, camels. They were first identified in humans in mid 1960s and get the name of coronaviruses due to the crown-like spikes on their surfaces. COVID-19 is a disease caused by the seventh confirmed coronavirus (SARS-CoV-2) to infect the human being. It has been preceded by six known human coronaviruses HCoV-229E, HCoV-OC43, SARS-CoV, HCoV-NL63, HCoV-HKU-1 and MERS-CoV (shown in Figure 1) (Tao et al., 2017; Zhou et al., 2018). Overall, these viruses are mainly targeting the respiratory system and causing health problems ranging from symptoms of mild upper respiratory tract to severe respiratory syndrome and even death. Coronaviruses can provoke diseases in different and multiple organ systems in animals and target mainly the respiratory system in humans. While HCoV-229E, HCoV-OC43, HCoV-NL63 and HCoV-HKU-1 induce upper respiratory disease associated with mild symptoms, SARS-CoV, MERS-CoV and SARS-CoV-2 are categorized as highly pathogenic that could cause critical and serious diseases in humans (Cui et al., 2019; Corman et al., 2018; Lu et al., 2020; Yin & Wunderink, 2018). The COVID-19 infected people commonly exhibit fever (83–98.6%), nonproductive/dry cough (59.4–82%), fatigue/muscle pain (11–70%) and breathing difficulties (Chen et al., 2020; Wang et al., 2020).
Figure 1.
The seven confirmed coronavirus to infect the human being. Note that SARS-CoV-2 has been preceded by six known human coronaviruses HCoV-229E, HCoV-OC43, SARS-CoV, HCoV-NL63, HCoV-HKU-1 and MERS-CoV. Note also that these viruses are mainly targeting the respiratory system and causing health problems ranging from symptoms of mild upper respiratory tract (such as HCoV-229E, HCoV-OC43, HCoV-NL63 and HCoV-HKU-1) to severe respiratory syndrome that can even lead to death (such as SARS-CoV, MERS-CoV and SARS-CoV-2).
As shown in Table 1, SARS-CoV was detected in Guangdong in China in 2002 and was responsible for 774 deaths among 8422 confirmed infections. Its mortality rate was estimated 10%. The infection reached 37 countries. Both SARS-CoV and MERS shared the same potential natural reservoir which is bats and the possible intermediate hosts are civets and dromedary camels respectively. MERS-CoV was first detected in Saudi Arabia in 2012 then spread in in 28 countries. MERS-CoV resulted in 2494 reported infections and 858 death and a mortality rate of 35% (Cui et al., 2019; Tao et al., 2017; Zhou et al., 2018). SARS-CoV-2 was first detected in December 2019 in Wuhan-China and is still an ongoing pandemic that infected 213 countries and resulted in more deaths and infected cases. The potential natural reservoir for SARS-CoV-2 is still not known and further investigations are needed to determine the exact zoonotic source. However, it has been proposed that the potential natural reservoir are probably bats and the possible intermediate hosts seems to be Pangolin (Zheng, 2020).
Table 1.
Comparison table of SARS-CoV-2 inducing COVID-19 with two other coronaviruses associated with severe symptoms including acute respiratory distress syndrome (ARDS).
| No. of infected | No. of deaths | Mortality | Period | No. of Countries | Origin | Vectors | |
|---|---|---|---|---|---|---|---|
| SARS-CoV-2 | 15,673,511 (on 24 July, 2020) (a) | 636,848 (a) | 3.4–6 % (b) | December 2019– | 213 (c) | The exact zoonotic source is still unknown (probably bats (Zheng, 2020)) | Still unknown (possibly Pangolin (Zheng, 2020)) |
| MERS-CoV | 2,494 | 858 | 35% | 2012 | 28 (Middle East + PRC) | Bats | Dromedary camels |
| SARS-CoV | 8,422 | 774 | 10% | 2002–2003 | 37 | Bats | Civet cats |
(a) Additional infections and deaths cases might occur in the upcoming infected people and those who are still hospitalized.
(b) It is early to give a real percentage. Because both numbers of deaths and cases are not final and continue to escalate. The given values is regarding the updated data from WHO and published reports.
(c) This number is by July 24, 2020 and it does not include the Holland America’s MS Zaandam and Diamond Princess Cruise ships, two international conveyances, hosted in USA and Japan respectively. The number of countries is still increasing and might reach the entire world’s countries and territories in the next few days.
SARS-CoV-2 started in Huanan Seafood Wholesale Market in Wuhan-China, and it has subsequently spread worldwide. The outbreak of infection with SARS-CoV-2 causing COVID-19, which was confirmed as new by sequencing all its genome, has rapidly met the criteria for public health emergency of international concern (PHEIC, at 30th January 2020) and had been declared pandemic by the WHO on March 11, 2020. As of July 24, 2020, more than 15,67 million cases of infection with COVID-19 have been confirmed in 213 countries and 636,848 death cases. The case fatality rate of SARS-CoV-2 is estimated to be 3.5 based on notified cases. Unlike SARS-CoV transmission of COVID-19 could occur before symptoms development.
Common symptoms in COVID-19 include fever, cough and feeling tired/muscle pain…
It has been outlined, by several authors from different centers, that COVID-19 is more likely to be fatal in elderly people with comorbidities (mainly cardiovascular and cerebrovascular diseases and diabetes), as a consequence of less rigorous immune system, in a similar way to MERS-CoV (Badawi & Ryoo, 2016; Channappanavar et al., 2017; Chen et al., 2020). Additionally, it and can be associated with fatal respiratory disease such as ARDS.
3. Angiotensin-Converting enzyme II (ACE2) receptor and susceptibility to SARS-CoV-2
Membrane receptor of host cells play a key role in the entry of coronaviruses into the host cells as well as their pathogenesis. Coronavirus recognizes and bind to its host receptor via its envelope-anchored spike (S) protein, then enters into the cell by fusing of host and viral membranes (Bosch et al., 2003; Gallagher & Buchmeier, 2001). Comparisons of genome sequences of SARS-CoV-2 with other coronaviruses showed 79.5% sequence identity with SARS-CoV (Lu et al., 2020; Zhou et al., 2020). Coronavirus genome annotations revealed four major structural proteins so called (1) the spike (S) protein, (2) nucleocapsid (N) protein, (3) membrane (M) protein and (4) the envelope (E) protein (Schoeman & Fielding, 2019). Two functional subunits of spike protein S1 and S2 have been proved to be responsible for receptor binding and fusion of viral and cellular membranes, respectively (He et al., 2004). The angiotensin-converting enzyme 2 (ACE2) has previously been reported as a receptor for both the SARS-coronavirus (SARS-CoV) and the human respiratory coronavirus NL63 (Li et al., 2003). While sequence comparisons of S proteins of SARS-CoV-2 with SARS-CoV showed only 75% sequence identity, most amino acid residues essential for receptor binding in the receptor binding domain (RBD) in the S protein were conserved between SARS-CoV and SARS-CoV-2 (Lu et al., 2020; Zhou et al., 2020). Recent studies have uncovered that SARS-CoV-2 mediates ACE2 as a host cell receptor for cellular entry and a serine protease TMPRSS2 for S protein priming (Hoffmann et al., 2020; Lu et al., 2020; Wang et al., 2020; Xu et al., 2020; Zhou et al., 2020). A strong interaction has been found between RBD domain of the SARS-CoV-2 S-protein with human ACE2 molecules (Xu et al., 2020). ACE2, an enzyme playing a key role in the Renin-Angiotensin System (RAS), is an integral membrane protein and a zinc metalloprotease of the ACE family, mainly expressed in vascular endothelial cells, the renal tubular epithelium, Leydig, lung, kidney, and gastrointestinal tract (Harmer et al., 2002; Ksiazek et al., 2003; Leung et al., 2003).
ACE2-expressing cells may become susceptible and accordingly become targets to SARS-CoV-2. Previous studies have demonstrated a positive correlation of SARS-CoV-2 with high ACE2 expressing cells in various organs (Chai et al., 2020; Zhao et al., 2020; Zou et al., 2020). Therefore, both expression level and pattern of ACE2 in different human tissues might be involved in the susceptibility, symptoms and consequently the outcome of COVID-19. ACE2 expression in lung tissues from Asian and Caucasian populations, based on the single-cell RNA seq analysis, suggested higher ACE2 expression in the Asian donors than white and African-American donors (Zhao et al., 2020). On the other hand, no significant difference has been found between Asian and Caucasians in ACE2 expression from lung tissues of controls using the RNA-seq and microarray datasets. A recent study investigated the mechanism of SARS-CoV-2 infection by studying ACE2 expression in various human tissues (Li et al., 2020). They have proposed that SARS-CoV-2 may also infect more tissues relatively with the higher level of ACE2 expression other than lungs. Since there were no significant differences in ACE2 expression levels between different sexes, ages and races. It was concluded they all are equally prone to be infected by SARS-CoV-2, but have different immune responses due to differences in their ACE expression level and immune signature in the lungs. These findings may partially elucidate differences in COVID-19 severity between male and female and young and old persons.
Another important issue in infection and progression of coronavirus disease is an interaction between viral spike protein and ACE2 receptors of host cells. This host-pathogen interaction of coronaviruses is critically important since it is likely that more could evolve in the future because of their high mutation rate. Therefore, a substantial effort has been spent on viral genetic variants known to be related with COVID-19 progression. On the other hand, only few studies have published on the genetics basis of risk factors that might have an effect on the susceptibility in human. Earlier studies on the ACE2 poymorphism in human populations have been carried out in order to determine their associations with several diseases such as hypertention, cardiovascular diseases, diabetes, kidney diseases and more recently COVID-19 (Delanghe et al., 2020; Luo et al., 2019; Ramachandran et al., 2008; Reich et al., 2008; Yang et al., 2015; Zhou & Yang, 2009). In fact, this gene is a peptidase that regulates the renin-angiotensin-aldosterone system.
Previous studies on a group 2 coronavirus, a mouse hepatitis virus, showed an association between allelic variants of viral receptor and binding activity of virus (Ohtsuka & Taguchi, 1997). Hence, it was proposed that genetic variants of ACE2 may ease the symptoms of SARS-CoV-2 infection. Although a previous study (Chiu et al., 2004) has proposed that ACE2 gene polymorphisms do not support an association between its common genetic variants and SARS susceptibility or outcome, there is no evidence if this is true for SARS-CoV-2 infection. Cao et al. (2020) have investigated the candidate functional coding variants in ACE2 and the allele frequency (AF) differences between populations. They have found the differences in distribution and AFs of QTLs in different populations indicating diversity of ACE2 expression in populations. Their findings showed differences in distribution and AFs of eQTLs for ACE2 in different populations (much higher in the East Asian populations) indicating different susceptibility or response to 2019-nCoV/SARS-CoV-2 from different populations under the similar conditions. A recent study investigated the interaction between proteins encoded by different ACE2 variants and SARS-CoV-2 spike protein (Hussain et al., 2020). Data analyses showed that most ACE2 variants displayed a similar binding affinity for SARS-CoV-2 spike protein alike wild-type ACE2. However, intermolecular interaction between ACE2 alleles, rs73635825 (S19P) and rs143936283 (E329G) and viral spike protein showed a considerable variations indicating a potential individual resistance against SARS-CoV-2 infection.
Stawiski et al. (2020) have recently investigated ACE2 polymorphisms in a large cohort of human population to predict SARS-Cov-2 susceptibility. They have proposed that while human ACE2 variants S19P, I21V, E23K, K26R, T27A, N64K, T92I, Q102P and H378R are those increasing susceptibility to SARS-Cov-2, K31R, N33I, H34R, E35K, E37K, D38V, Y50F, N51S, M62V, K68E, F72V, Y83H, G326E, G352V, D355N, Q388L and D509Y are putative protective variants decreasing SARS-Cov-2 S protein and ACE2 binding. However, there was no significant difference between ACE2 variant allele frequencies of the studied populations. In addition to the ACE2 gene, the relationship between ACE1 D/I polymorphism associated with alterations in circulating and tissue concentrations of ACE and COVID-19 infections has also been investigated in 25 different European countries with the prevalence and mortality of COVID-19 (Delanghe et al., 2020). Results of this study have showed that prevalence of COVID-19 infections are inversely correlated with ACE1 D allele frequency. Alike, there was a significant correlation between COVID-19 mortality and the prevalence of ACE1 D allele. Furthermore, a meta-analysis study on 48,758 healthy subjects from 30 different countries showed that a significant correlation between ACE1 D/I allele frequency ratio and the prevalence of COVID-19 but no significant difference in the case of death rate (Hatami et al., 2020).
Since human ACE2 gene is X-linked, males will express each allelic variants of ACE2 coding variants separately due to their homozygosity that increase chance to observe phenotypic expression of rare coding variants in males. However, females will express those variants in a mosaic manner because of early X-inactivation. Gibson et al. (2020) have used the gnomAD database (The Genome Aggregation Database: a resource cataloging genetic coding variants) for 141,456 adults and detected 15 missense variants of which rs4646116 ACE2 (thought to encode p.Lys26Arg) predicted to be located at or close to the ACE2 binding site for SSARS-CoV-2 spike protein. This allele 1 in 70 among Ashkenazi Jewish males and 1 in 172 among non-Finnish European males (higher frequency in females) but absent in Korean and Japanese participants. To date no studies have been carried out on the people infected by SARS-CoV-2 with no symptoms, mild symptoms and severe symptoms for determining association between different variants of ACE2 gene and susceptibility to SARS-CoV-2. ACE receptor could play a key role in developing vaccines and therapeutics for COVID-19. Since ACE2 is a gate for entry of SARS-Cov-2, angiotensin-converting enzyme inhibitors (ACEI) and angiotensin II receptor blockers (ARB) that has been proved to upregulate ACE2 expression in some animal models are being hope in treating COVID-19 (Ishiyama et al., 2004: Ferrario et al., 2005). Therefore, regulation of ACE2 may improve outcomes of SARS-Cov-2 infection (Gurwitz, 2020; Kuba et al., 2005). However, it has been proposed that use of ARBs and ACEI in certain high-risk COVID-19 patients may be harmful (Reynolds et al., 2020). In a recent cohort study of 18472 patients showed that there is no correlation between ACEI/ARBs use and testing positive for COVID-19 (Mehta et al., 2020). Despite the lack of sufficient clinical evidence, several professional societies have recommended to continued use of these medications for COVID-19 treatment. Another approach to prevent SARS-Cov-2 infection is to use antibodies to stop the viruses from attaching to ACE2 receptor. An antibody so called ‘decoy’ ACE2 receptor has been developed to block the virus before it reaches to the ACE2 on the cell surfaces and cause infection. A number of antibodies carrying ACE2 have been developed but particularly one, called MDR504, have been more tightly bound to SARS-Cov-2 and effectively neutralize the virus and blocked it from entering the cells (Iwanaga et al., 2020).
4. Acute respiratory distress syndrome: ARDS
ARDS is a form of respiratory failure, for which the first case has been described in 1967 by Ashbaugh and his collaborators (Ashbaugh et al., 1967; Irwin & Rippe, 2003). Wang et al. reported, in 2020, that the average time observed to develop ARDS, if any, is 8 days after the first appeared symptom following COVID-19 infection.
ARDS is considered as a significant life threatening. In fact, the death is estimated to range between 35 and 46% even with the best medical care. It could reach 50% in same cases (Ferguson et al., 2012). These averages are mainly related to the severity of the disease, for which 3 types have been categorized according to the severity of hypoxemia: mild, moderate and severe cases (Ferguson et al., 2012).
Hypoxemia is assessed by the following ratio PaO2/FiO2. PaO2 stands for the pressure of the arterial oxygen and FiO2 stands for the fraction of the inspired oxygen. So far, ARDS is categorized as a mild whenever PaO2/FiO2 is ranging between 200 mmHg and 300 mmHg (or ≤ 40 kPa), moderate if PaO2/FiO2 ranges between 100 mmHg and 200 mmHg (or ≤ 27 kPa), and severe if PaO2/FiO2 is less than 100 mmHg (or ≤ 13.4 kPa) (Brown et al., 2016; Fan et al., 2018; Ferguson et al., 2012). Moreover, ARDS pathogenesis excludes heart related pulmonary edema and should exhibits an acute onset (Matthay et al., 2019). Lung injury in ARDS is described as a fast onset (worsening within a week) of widespread inflammation. X-ray radiographs of the chest exhibit several radiological opacities as a result of bilateral infiltrates (Matthay et al., 2020).
The total average of worldwide death, related to ARDS, is estimated to be 3 million per year (Bellani et al., 2016). In patients, ARDS is resulting into symptomatic features such as difficulty (short and rapid) in breathing and bluish skin coloration due to low oxygen level in the blood.
ARDS has been largely described and several research activities have been done for a better prognostic. However, until nowadays no efficient pharmacological treatment has been described to date. Thus, the mechanical ventilation is still the principal used way and one of the best practices together with the treatment of the underlying cause of the edema. Furthermore, the patients who survive the ARDS would most often have long hospital stay. Physical and neurological morbidity is very common among the surviving patients, even several years after their hospital discharge. However, because treatment of COVID-19 induced- ARDS is an ongoing challenge, it may be a good opportunity for a better understanding of the disease prognostics.
5. Pathophysiology of COVID-19 induced ARDS
Lessons learned from previous severe diseases caused by coronaviruses outbreaks (SARS-CoV and MERS-CoV) and more recently SARS-CoV-2 lead to a better understood of ARDS key features associated COVID-19.
ARDS is categorized as a diffuse alveolar damage inducing pulmonary edema together with damaged lungs endothelia (Kao et al., 2015; Vasudevan et al., 2004). The damaged endothelia show much more permeability to both water and proteins (exudate) and disrupt the alveolar capillary barrier (Kao et al., 2015; Vasudevan et al., 2004).
In ARDS, the viral infection caused with SARS-CoV-2 and others, leads to injury of the entire lung not only a particular area as what is happening in pneumonia (Wujtewicz et al., 2020; Yang et al., 2020).
Once an organism has been infected by SARS-CoV-2, similarly to SARS-CoV, the novel coronavirus uses one of the spikes, particularly the S-protein type, as a key to enter the cells of the body (Li et al., 2003). In fact, the S-protein bind with specific cytoplasmic receptor called ACE2 which is a crucial component of RAS (Cheng et al., 2020, Khailany et al., 2020). While, MERS-CoV bind to CD26, it is believed that SARS-CoV and SARS-CoV-2 bind to ACE2 (Khailany et al., 2020). ACE2 counteracts the RAS activation, protects the tissue injuries and is much more expressed in females than in males. Likewise, it’s also much more expressed in young than in elderly people (Soro-Paavonen et al., 2012). Regardless its activity in most tissues, it is widely active in the lungs but also in several other organs such as the hearts, testis and kidneys (Cheng et al., 2020; Ohtsuki et al., 2010).
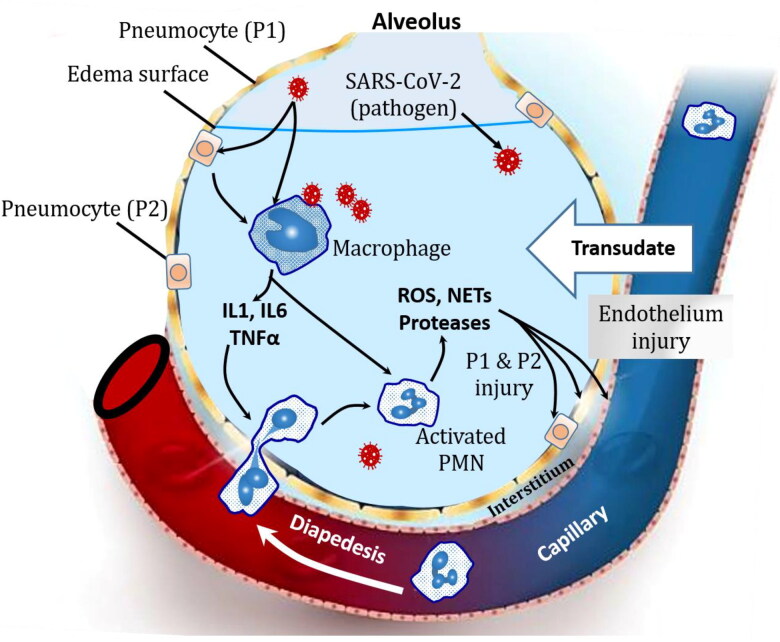
Once the virus enters the body, it is believed that SARS-CoV-2 targets, mainly, the pneumocytes II, and these tension-protective cells will be destroyed. Being infected by COVID-19, the pneumocytes II seem to be largely involved the replication and amplification SARS-CoV-2 before being damaged. Moreover, the infected cells secret a high amount of specific inflammatory mediators that enhance macrophages to release cytokines including Tumor Necrosis Factor alpha (TNFα) and interleukins (IL-1 and IL-6). These cytokines lead to the disruption of the alveolar-capillary membrane integrity, which is associated with vasodilation and increased vascular permeability. The latter is mainly related to the cytokines (TNFα, IL-1 and IL-6) induced endothelial contraction. The disrupted integrity of the alveolar-capillary allow the plasma leakage into the alveoli and the lungs interstitial spaces. A loss of osmotic pressure gradient leads to a leaky barrier and an increased sensitivity to hydrostatic forces are believed to play key role in the diffuse edema formation. The formation of protein rich edema, known as exudate, in the interstitium and alveolar spaces leads to alveolar flooding making it very difficult to breathe and then lead to hypoxemia, which is one of the common symptoms of COVID-19 infection (Matthay et al., 2020). The flooded interstitium itself exert additional pressure on the alveoli that might lead to their contraction; alveolar collapsing enhanced by reduced surfactant level due to the damaged pneumocytes II. Typical lung histopathological micrographs, at this stage, exhibit already diffuse alveolar damage (DAD) and hyaline membrane formation in the alveolar wall.
Furthermore, pulmonary macrophages release much more interleukins (IL-1 and IL-6) and TNFα, which exhibit a chemotaxis towards Polymorpho-nuclear Neutrophils (PMNs) (Zemans & Matthay, 2017). The invading PMNs release especially reactive oxygen species (ROS), neutrophil extracellular traps (NETs) and proteases to the pathogens; SARS-CoV-2 in the case of COVID-19. However, the PMNs of the inflamed tissue amplify the phenomena by damaging the different cells existing in the lung inflammatory microenvironment including endothelial cells and pneumocytes 1 and 2 (shown in Figure 2). Hence, significant decrease in both gaseous exchanges and surfactant production would be outlined together with a consolidation process related to the cellular debris, PMNs, macrophages and edema, which become more and more a protein-rich fluid… The consolidation is also enhancing and worsening the alveolar collapsing.
Figure 2.
Pathophysiology of ARDS in SARS-CoV-2 inducing COVID-19 patients with severe symptoms. Once SARS-CoV-2 gets into the body, it uses its S-spike type, as a key to enter the cells by binding to angiotensin-converting enzyme (ACE2). The virus use the mainly pneumocytes 2 components for its own proliferation. The infected cells secret a high amount of specific inflammatory mediators that enhance macrophages to release cytokines Tumor Necrosis Factor alpha (TNFα) and interleukins (IL-1 and IL-6). These cytokines lead to the disruption of the alveolar-capillary membrane integrity and increased the vascular permeability. The disrupted integrity of the alveolar-capillary allow the plasma leakage into the alveoli and the lungs interstitial spaces. The formation of protein rich edema, known as exudate, in the interstitium and alveolar spaces leads to alveolar flooding making it very difficult to breathe and lead to hypoxemia. Driven by IL-1, IL-6 and TNFα, PMNs invade the alveoli and release reactive oxygen species (ROS), neutrophil extracellular traps (NETs) and proteases that damage the vascular and the alveoli components that exacerbates the hypoxemia, the alveoli collapsing and lead to a worse situation: alveolar consolidation.
In normal physiological conditions, during inhalation the oxygen that reach the alveoli oxygenate the blood which turns back to the heart and then to the different cells of the body. So the exchange of the gases, is facilitated by the alveolar capillary membrane which should be very thin. However, in ARDS, the inflammatory process it widespread not only within the alveoli but also in the intersititium. So instead of having functional little small alveoli able to inflate and deflate during the inhalation and exhalation respectively, the lungs stiff and it becomes very difficult to inflate due to fluid and the inflammation. Finally, a significant increase in the load to breathe occurs in vain leading to the pulmonary failure.
6. Biomarkers of acute respiratory distress syndrome
ARDS is a life threatening associated with fast onset of widespread inflammatory damage. It concerns mainly the alveolar epithelial cells (type 1 and type 2) and the vascular endothelial cells. This damage is associating release of several biochemical signals and inflammatory mediators by local endothelial and pulmonary epithelial cells. In this context, during ARDS worsening, lung epithelial cells might secrete sRAGE, SP, KL-6, CC16 and KGF (for soluble receptor of advanced glycation end-products, surfactant proteins, Krebs von den Lungen protein 6, Clara cell protein and keratinocyte growth factor respectively) (Determann et al., 2010; Koh et al., 2018; Sato et al., 2004). In ARDS, endothelial cells might secrete Ang-1, Ang-2, vWF and VEGF (for angiopoietin-1, angiopoietin-2, von Willebrand factor and vascular endothelial growth factor respectively). These secreted products may be used as biomarkers of ARDS. Pro- inflammatory (IL-1β, IL-6, IL-8, IL-18 and TNFα, for interleukin 1, 6, 8 and 18 and tumor necrosis factor alpha respectively) and anti-inflammatory biomarkers (IL-1RA, IL-10, sTNF-RI and sTNF-RII for interleukin 1 receptor antagonist, interleukin 10 and soluble tumor necrosis factor receptors I and II respectively) are often used to have an idea about neutrophils and their toxic mediators. Plasminogen activator inhibitor-1 (PAI-1) is a useful biomarker indicating the degree of coagulation and fibrinolysis which is a common feature on ARDS (Spadaro et al., 2019). MicroRNA (miRNA) are also good biomarker candidates as their expression varies in early stages of gene expression associated ARDS (Cardinal-Fernández et al., 2016; Ferruelo et al., 2018). Specifically, miRNA-146a and miRNA-155 have been reported to increase significantly in patients with severe sepsis and sepsis induced acute lung injury (Han et al., 2016). Similarly, these non-coding RNA molecules may play important role in ARDS associated COVID-19.
Hence, several biomarkers are used for patient in severe trauma associated ARDS but some biomarkers combinations were reported to be efficient in ARDS prognostic and even to predict the mortality associated to this syndrome (Ware et al., 2013, Ware & Calfee, 2016). Recently, the development of methods for gene expression and sensitive immunoassay is offering a great potential for personalized treatment (Spadaro et al., 2019; Sweeney & Khatri, 2017).Taken together, these biomarkers could certainly have potential relevance for mortality prediction, diagnosis and therapy of ARDS due to SARS-CoV-2 infection.
7. Management and treatment strategies of ARDS associated SARS-CoV-2 infection
The ARDS treatment requires a clear defining of the underlying anatomo-physiological properties of lung tissues being managed. Otherwise, the ARDS treatment would be based mainly on the response likelihood and its adjustment (Dries, 2019; Gattinoni et al., 2018). Even the ventilation management is independently associated with improved survival (Fan et al., 2018). Nevertheless, some new clinical trials sound promising such as the use of higher positive end-expiratory pressure (Dries, 2019). It has also been shown that lung recruitment maneuvers may improve the oxygenation process and shorten the hospital stay period in ARDS (Cui et al., 2020) and avoid the pro-inflammatory processes triggered by mechanical ventilation (Spadaro et al., 2019) . Because in ARDS, the lung injury is accompanied with an acute onset, the recognition and the determination of the respiratory damage threshold would certainly be a key point for a better and efficient ARDS therapy (Dries, 2019). To date, no specific treatment has been proven for SARS-CoV-2 infection and WHO management still focus on preventing the infection, detection and monitoring of cases together with supportive care. However, extracorporeal membrane oxygenation (ECMO) has been reported to be effective in treating ARDS. Similarly, ECMO might be effective in treatment of COVID-19 severe cases (Hong et al., 2020).
8. Conclusion
Development and availability of simple and rapid diagnostic tests for COVID-19 is as important as the development of treatment of its serious ARDS complication. Moreover, there is an important need for early identification of patients with higher ARDS risk following critical SARS-CoV-2 infection. More investigations, about what is highly needed to know about the etiology of COVID-19 associated ARDS, needed to be done by taking into account several linked factors mainly the age of the infected patients and their comorbidities. In this context, mathematical modeling might help both to understand the ARDS outcomes and to predict its severity in the populations at risk. It could also help in the therapeutic processes. Elsewhere, a better understanding of ACE2 receptor (which is playing a key role in cellular entry of coronaviruses including SARS-CoV-2) polymorphisms and susceptibility to SARS-CoV-2 inducing COVID-19 could help in understanding ARDS phenotypes and outcomes. Regarding the key protective role played by ACE2 on several diseases including ARDS, investigation on spike protein-based vaccination and drugs might be promising to enhance ACE2 activity for the treatment of COVID-19 including ARDS. Because the ARDS associated with COVID-19 is an ongoing challenge, the SARS-CoV-2 pandemic period would certainly be helpful for a better understood of the ARDS life threatening, which is associated with several pathogens.
Acknowledgements
The authors have no acknowledgments to declare.
Glossary
Abbreviations
- ACE
Angiotensin-converting enzyme
- Ang
Angiopoietin
- ARDS
Acute Respiratory Distress Syndrome
- CC-16
Clara Cell protein 16
- CoV
Coronavirus
- COVID-19
Coronavirus disease 2019
- DAD
Diffuse Alveolar Damage
- IL
Interleukin
- IL-1RA
IL-1 Receptor Antagonist
- KGF
Keratinocyte Growth Factor
- KL-6
Krebs von den Lungen protein 6
- MERS
Middle Eastern Respiratory Syndrome
- miRNA
MicroRNA
- NETs
Neutrophil Extracellular Traps
- PAI-1
Plasminogen Activator Inhibitor-1
- PaO2/FIO2
Oxygen arterial partial pressure/oxygen inspired fraction ratio
- PMN
Polymorpho-nuclear Neutrophils
- ROS
Reactive Oxygen Species
- SARS
Severe Acute Respiratory Syndrome
- SP
Surfactant Proteins
- sRAGE
soluble Receptor of Advanced Glycation End-products
- sTNF-R
Tumor Necrosis Factor Receptors
- TNFα
Tumor Necrosis Factor-alpha
- VEGF
Vascular Endothelial Growth Factor
- vWF
von Willebrand Factor
Funding Statement
Authors (RB, FB and MMA) received grants from the Scientific Research Deanship at University of Ha’il - Saudi Arabia through project number COVID-1942 and focuses mainly on polymorphism of ACE2 and its susceptibility to the severity of COVID-19.
Disclosure statement
The authors declare no competing financial interest.
Author contributions
RB drafted of the manuscript. Additional content has been provided by MMA, FB an MVE then the critical revision of the final manuscript has been done by all the authors. All authors red and approved the version of manuscript to be submitted.
Ethical approval
The Ethical approval: This article does not contain any studies with human participants or animals performed by any of the authors.
References
- Ashbaugh, D. G., Bigelow, D. B., Petty, T. L., & Levine, B. E. (1967). Acute respiratory distress in adults. The Lancet, 290(7511), 319–323. 10.1016/S0140-6736(67)90168-7 [DOI] [PubMed] [Google Scholar]
- Badawi, A., & Ryoo, S. G. (2016). Prevalence of comorbidities in the Middle East respiratory syndrome coronavirus (MERS-CoV): A systematic review and meta-analysis. International Journal of Infectious Diseases: IJID : Official Publication of the International Society for Infectious Diseases, 49, 129–133. 10.1016/j.ijid.2016.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellani, G., Laffey, J. G., Pham, T., Fan, E., Brochard, L., Esteban, A., Gattinoni, L., van Haren, F., Larsson, A., McAuley, D. F., Ranieri, M., Rubenfeld, G., Thompson, B. T., Wrigge, H., Slutsky, A. S., & Pesenti, A., ESICM Trials Group . (2016). Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA, 315(8), 788–800. 10.1001/jama.2016.0291 [DOI] [PubMed] [Google Scholar]
- Bosch, B. J., van der Zee, R., de Haan, C. A. M., & Rottier, P. J. M. (2003). The coronavirus spike protein is a Class I virus fusion protein: Structural and functional characterization of the fusion Core Complex. Journal of Virology, 77(16), 8801–8811. 10.1128/jvi.77.16.8801-8811.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, S. M., Grissom, C. K., Moss, M., Rice, T. W., Schoenfeld, D., Hou, P. C., Thompson, B. T., & Brower, R. G. (2016). Nonlinear imputation of Pao2/Fio2 from Spo2/Fio2 among patients with acute respiratory distress syndrome. Chest, 150(2), 307–313. 10.1016/j.chest.2016.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao, Y., Li, L., Feng, Z., Wan, S., Huang, P., Sun, X., Wen, F., Huang, X., Ning, G., & Wang, W. (2020). Comparative genetic analysis of the novel coronavirus (2019-nCoV/SARS-CoV-2) receptor ACE2 in different populations. Cell Discovery, 6, 11. 10.1038/s41421-020-0147-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardinal-Fernández, P., Ferruelo, A., Esteban, A., & Lorente, J. A. (2016). Characteristics of microRNAs and their potential relevance for the diagnosis and therapy of the acute respiratory distress syndrome: From bench to bedside. Transl Res, 169, 102–111. 10.1016/j.trsl.2015.11.004 [DOI] [PubMed] [Google Scholar]
- Chai, X., Hu, L., Zhang, Y., Weiyu, H., Lu, Z., & Ke, A. (2020). Specific ACE2 expression in cholangiocytes may cause liver damage after 2019-nCoV infection. bioRxiv Preprint, 10.1101/2020.02.03.931766 [DOI] [Google Scholar]
- Channappanavar, R., Fett, C., Mack, M., Ten Eyck, P. P., Meyerholz, D. K., & Perlman, S. (2017). Sex-based differences in susceptibility to severe acute respiratory syndrome coronavirus infection. Journal of Immunology (Baltimore, Maryland: 1950), 198(10), 4046–4053. 10.4049/jimmunol.1601896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, N., Zhou, M., Dong, X., Qu, J., Gong, F., Han, Y., Qiu, Y., Wang, J., Liu, Y., Wei, Y., Xia, J., Yu, T., Zhang, X., & Zhang, L. (2020). Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. The Lancet, 395(10223), 507–513. 10.1016/S0140-6736(20)30211-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng, H., Wang, Y., & Wang, G. Q. (2020). Organ-protective effect of angiotensin-converting enzyme 2 and its effect on the prognosis of COVID-19. Journal of Medical Virology, 92(7), 726–730. 10.1002/jmv.25785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu, R. W. K., Tang, N. L. S., Hui, D. S. C., Chung, G. T. Y., Chim, S. S. C., Chan, K. C. A., Sung, Y-m., Chan, L. Y. S., Tong, Y-k., Lee, W-s., Chan, P. K. S., & Lo, Y. M. D. (2004). ACE2 gene polymorphisms do not affect outcome of severe acute respiratory syndrome. Clinical Chemistry, 50(9), 1683–1686. 10.1373/clinchem.2004.035436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corman, V. M., Muth, D., Niemeyer, D., & Drosten, C. (2018). Hosts and sources of endemic human coronaviruses. Advances in Virus Research, 100, 163–188. 10.1016/bs.aivir.2018.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui, J., Li, F., & Shi, Z. L. (2019). Origin and evolution of pathogenic coronaviruses. Nature Reviews Microbiology, 17(3), 181–192. 10.1038/s41579-018-0118-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui, Y., Cao, R., Wang, Y., & Li, G. (2020). Lung recruitment maneuvers for ARDS patients: A systematic review and meta-analysis. Respiration, 99(3), 264–276. 10.1159/000501045 [DOI] [PubMed] [Google Scholar]
- Delanghe, J. R., Speeckaert, M. M., & De Buyzere, M. L. (2020). COVID-19 infections are also affected by human ACE1 D/I polymorphism. Clinical Chemistry and Laboratory Medicine, 58(7), 1125–1126. 10.1515/cclm-2020-0425 [DOI] [PubMed] [Google Scholar]
- Delanghe, J. R., Speeckaert, M. M., & De Buyzere, M. L. (2020). The host's angiotensin-converting enzyme polymorphism may explain epidemiological findings in COVID-19 infections. Clinica Chimica Acta; International Journal of Clinical Chemistry, 505, 192–193. 10.1016/j.cca.2020.03.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Determann, R. M., Royakkers, A. A. N. M., Haitsma, J. J., Zhang, H., Slutsky, A. S., Ranieri, V. M., & Schultz, M. J. (2010). Plasma levels of surfactant protein D and KL-6 for evaluation of lung injury in critically ill mechanically ventilated patients. BMC Pulmonary Medicine, 10, 6–6. 10.1186/1471-2466-10-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dries, D. J. (2019). ARDS from syndrome to disease-treatment strategies. Air Medical Journal, 38(2), 64–67. 10.1016/j.amj.2018.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan, E., Brodie, D., & Slutsky, A. S. (2018). Acute respiratory distress syndrome: Advances in diagnosis and treatment. JAMA, 319(7), 698–710. 10.1001/jama.2017.21907 [DOI] [PubMed] [Google Scholar]
- Ferguson, N. D., Fan, E., Camporota, L., Antonelli, M., Anzueto, A., Beale, R., Brochard, L., Brower, R., Esteban, A., Gattinoni, L., Rhodes, A., Slutsky, A. S., Vincent, J.-L., Rubenfeld, G. D., Thompson, B. T., & Ranieri, V. M. (2012). The Berlin definition of ARDS: An expanded rationale, justification, and supplementary material. Intensive Care Medicine, 38(10), 1573–1582. 10.1007/s00134-012-2682-1 [DOI] [PubMed] [Google Scholar]
- Ferrario, C. M., Jessup, J., Chappell, M. C., Averill, D. B., Brosnihan, K. B., Tallant, E. A., Diz, D. I., & Gallagher, P. E. (2005). Effect of angiotensin-converting enzyme inhibition and angiotensin II receptor blockers on cardiac angiotensin-converting enzyme 2. Circulation, 111(20), 2605–2610. 10.1161/CIRCULATIONAHA.104.510461 [DOI] [PubMed] [Google Scholar]
- Ferruelo, A., Peñuelas, Ó., & Lorente, J. A. (2018). MicroRNAs as biomarkers of acute lung injury. Annals of Translational Medicine, 6(2), 34. 10.21037/atm.2018.01.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher, T. M., & Buchmeier, M. J. (2001). Coronavirus spike proteins in viral entry and pathogenesis. Virology, 279(2), 371–374. 10.1006/viro.2000.0757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gattinoni, L., Marini, J. J., & Quintel, M. (2018). Time to rethink the approach to treating acute respiratory distress syndrome. JAMA, 319(7), 664–666. 10.1001/jama.2017.21900 [DOI] [PubMed] [Google Scholar]
- Gibson, W. T., Evans, D. M., An, J., & Jones, S. J. M. (2020). ACE 2 coding variants: A potential X-linked risk factor for COVID-19 disease. bioRxiv Preprint. 10.1101/2020.04.05.026633 [DOI] [Google Scholar]
- Gorbalenya, A. E., Baker, S. C., Baric, R. S., de Groot, R. J., Drosten, C., Gulyaeva, A. A., Haagmans, B. L., Lauber, C., Leontovich, A. M., & Neuman, B. W. (2020). Severe acute respiratory syndrome-related coronavirus: Classifying 2019-NCoV and naming it SARS-CoV-2. Nature Microbiology, 2020, 1–9. 10.1038/s41564-020-0695-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurwitz, D. (2020). Angiotensin receptor blockers as tentative SARS-CoV-2 therapeutics. Drug Development Research, 6(2), 1–4. 10.1002/ddr.21656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han, Y., Li, Y., & Jiang, Y. (2016). The prognostic value of plasma MicroRNA-155 and MicroRNA-146a level in severe sepsis and sepsis-induced acute lung injury patients. Clinical Laboratory, 62(12), 2355–2360. 10.7754/Clin.Lab.2016.160511 [DOI] [PubMed] [Google Scholar]
- Harmer, D., Gilbert, M., Borman, R., & Clark, K. L. (2002). Quantitative MRNA expression profiling of ACE 2, a novel homologue of angiotensin converting enzyme. FEBS Letters, 532 (1–2), 107–110. 10.1016/S0014-5793(02)03640-2 [DOI] [PubMed] [Google Scholar]
- Hatami, N., Ahi, S., Sadeghinikoo, A., Foroughian, M., Javdani, F., Kalani, N., Fereydoni, M., Keshavarz, P., & Hosseini, A. (2020). Worldwide ACE (I/D) polymorphism may affect COVID-19 recovery rate: An ecological meta-regression. Endocrine, 68(3), 479–484. 10.1007/s12020-020-02381-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He, Y., Zhou, Y., Liu, S., Kou, Z., Li, W., Farzan, M., & Jiang, S. (2004). Receptor-binding domain of SARS-CoV spike protein induces highly potent neutralizing antibodies: Implication for developing subunit vaccine. Biochemical and Biophysical Research Communications, 324(2), 773–781. 10.1016/j.bbrc.2004.09.106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann, M., Kleine-Weber, H., Schroeder, S., Krüger, N., Herrler, T., Erichsen, S., Schiergens, T. S., Herrler, G., Wu, N.-H., Nitsche, A., Müller, M. A., Drosten, C., & Pöhlmann, S. (2020). SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell, 181(2), 271–280. 10.1016/j.cell.2020.02.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong, X., Xiong, J., Feng, Z., & Shi, Y. (2020). Extracorporeal membrane oxygenation (ECMO): Does it have a role in the treatment of severe COVID-19? International Journal of Infectious Diseases: IJID: Official Publication of the International Society for Infectious Diseases, 94, 78–80. 10.1016/j.ijid.2020.03.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussain, M., Jabeen, N., Raza, F., Shabbir, S., Baig, A. A., Amanullah, A., & Aziz, B. (2020). Structural variations in human ACE2 may influence its binding with SARS‐CoV‐2 spike protein. Journal of Medical Virology. 10.1002/jmv.25832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin, R. S., & Rippe, J. M. (2003). Irwin and rippe’s intensive care medicine (5th ed.). Lippincott Williams & Wilkins. [Google Scholar]
- Ishiyama, Y., Gallagher, P. E., Averill, D. B., Tallant, E. A., Brosnihan, K. B., & Ferrario, C. M. (2004). Upregulation of angiotensin-converting enzyme 2 after myocardial infarction by blockade of angiotensin II receptors. Hypertension (Dallas, Texas: 1979), 43(5), 970–976. 10.1161/01.HYP.0000124667.34652.1a [DOI] [PubMed] [Google Scholar]
- Iwanaga, N., Cooper, L., Rong, L., Beddingfield, B., Crabtree, J., Tripp, R. A., & Kolls, J. K. (2020). Novel ACE2-IgG1 fusions with improved activity against SARS-CoV2. bioRxiv. 10.1101/2020.06.15.152157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kao, K. C., Hu, H. C., Chang, C. H., Hung, C. Y., Chiu, L. C., Li, S. H., Lin, S. W., Chuang, L. P., Wang, C. W., Li, L. F., Chen, N. H., Yang, C. T., Huang, C. C., & Tsai, Y. H. (2015). Diffuse alveolar damage associated mortality in selected acute respiratory distress syndrome patients with open lung biopsy. Critical Care, 19(1), 228. 10.1186/s13054-015-0949-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khailany, R. A., Safdar, M., & Ozaslan, M. (2020). Genomic characterisation of a novel SARS-CoV-2. Gene Reports, 19, 100682. 10.1101/2020.01.24.919183 [DOI] [PMC free article] [PubMed]
- Koh, H., Tasaka, S., Hasegawa, N., Asano, K., Kotani, T., Morisaki, H., Takeda, J., Fujishima, S., Matsuda, T., Hashimoto, S., & Ishizaka, A. (2018). Vascular endothelial growth factor in epithelial lining fluid of patients with acute respiratory distress syndrome. Respirology, 13(2), 281–284. 10.1111/j.1440-1843.2007.01193.x [DOI] [PubMed] [Google Scholar]
- Ksiazek, T. G., Erdman, D., Goldsmith, C. S., Zaki, S. R., Peret, T., Emery, S., Tong, S., Urbani, C., Comer, J. A., Lim, W., Rollin, P. E., Dowell, S. F., Ling, A. E., Humphrey, C. D., Shieh, W. J., Guarner, J., Paddock, C. D., Rota, P., Fields, B., … Anderson, L. J., SARS Working Group . (2003). A novel coronavirus associated with severe acute respiratory syndrome. The New England Journal of Medicine, 348(20), 1953–1966. 10.1056/NEJMoa030781 [DOI] [PubMed] [Google Scholar]
- Kuba, K., Imai, Y., Rao, S., Gao, H., Guo, F., Guan, B., Huan, Y., Yang, P., Zhang, Y., Deng, W., Bao, L., Zhang, B., Liu, G., Wang, Z., Chappell, M., Liu, Y., Zheng, D., Leibbrandt, A., Wada, T., … Penninger, J. M. (2005). A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury. Nature Medicine, 11 (8), 875–879. 10.1038/nm1267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung, W. K., To, K., Chan, P. K. S., Chan, H. L. Y., Wu, A. K. L., Lee, N., Yuen, K. Y., & Sung, J. J. (2003). Enteric involvement of severe acute respiratory syndrome-associated coronavirus infection. Gastroenterology, 125(4), 1011–1017. 10.1016/j.gastro.2003.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, M. Y., Li, L., Zhang, Y., & Wang, X. S. (2020). Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues. Infectious Diseases of Poverty, 9(45), 1-7. 10.1186/s40249-020-00662-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, W., Moore, M. J., Vasilieva, N., Sui, J., Wong, S. K., Berne, M. A., Somasundaran, M., Sullivan, J. L., Luzuriaga, K., Greenough, T. C., Choe, H., & Farzan, M. (2003). Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature, 426(6965), 450–454. 10.1038/nature02145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu, R., Zhao, X., Li, J., Niu, P., Yang, B., Wu, H., Wang, W., Song, H., Huang, B., Zhu, N., Bi, Y., Ma, X., Zhan, F., Wang, L., Hu, T., Zhou, H., Hu, Z., Zhou, W., Zhao, L., … Tan, W. (2020). Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. The Lancet, 395(10224), 565–574. 10.1016/S0140-6736(20)30251-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo, Y., Liu, C., Guan, T., Li, Y., Lai, Y., Li, F., Zhao, H., Maimaiti, T., & Zeyaweiding, A. (2019). Association of ACE2 genetic polymorphisms with hypertension-related target organ damages in south Xinjiang. Hypertension Research: Official Journal of the Japanese Society of Hypertension, 42(5), 681–689. 10.1038/s41440-018-0166-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthay, M. A., Aldrich, J. M., & Gotts, J. E. (2020). Treatment for severe acute respiratory distress syndrome from COVID-19. The Lancet Respiratory Medicine S2213 Medicine, 8(5), 433–434. 10.1016/S2213-2600(20)30127-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthay, M. A., Zemans, R. L., Zimmerman, G. A., Arabi, Y. M., Beitler, J. R., Mercat, A., Herridge, M., Randolph, A. G., & Calfee, C. S. (2019). Acute respiratory distress syndrome. Nature Reviews Disease Primers, 5(1), 18. 10.1038/s41572-019-0069-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta, N., Kalra, A., Nowacki, A. S., Anjewierden, S., Han, Z., & Bhat, P. (2020). Association of use of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers with testing positive for coronavirus disease 2019 (COVID-19). JAMA Cardiology. https://doi.org/ 10.1001/jamacardio.2020.1855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohtsuka, N., & Taguchi, F. (1997). Mouse susceptibility to mouse hepatitis virus infection is linked to viral receptor genotype. Journal of Virology, 71(11), 8860–8863. 10.1128/JVI.71.11.8860-8863.1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohtsuki, M., Morimoto, S-i., Izawa, H., Ismail, T. F., Ishibashi-Ueda, H., Kato, Y., Horii, T., Isomura, T., Suma, H., Nomura, M., Hishida, H., Kurahashi, H., & Ozaki, Y. (2010). Angiotensin converting enzyme 2 gene expression increased compensatory for left ventricular remodeling in patients with end-stage heart failure. International Journal of Cardiology, 145(2), 333–334. 10.1016/j.ijcard.2009.11.057 [DOI] [PubMed] [Google Scholar]
- Ramachandran, V., Ismail, P., Stanslas, J., Shamsudin, N., Moin, S., & Mohd Jas, R. (2008). Association of insertion/deletion polymorphism of angiotensin‐converting enzyme gene with essential hypertension and type 2 diabetes mellitus in Malaysian subjects. Journal of the Renin-Angiotensin-Aldosterone System, 9(4), 208–214. 10.1177/1470320308097499 [DOI] [PubMed] [Google Scholar]
- Reich, H. N., Oudit, G. Y., Penninger, J. M., Scholey, J. W., & Herzenberg, A. M. (2008). Decreased glomerular and tubular expression of ACE2 in patients with type 2 diabetes and kidney disease. Kidney International, 74(12), 1610–1616. 10.1038/ki.2008.497 [DOI] [PubMed] [Google Scholar]
- Reynolds, H. R., Adhikari, S., Pulgarin, C., Troxel, A. B., Iturrate, E., Johnson, S. B., Hausvater, A., Newman, J. D., Berger, J. S., Bangalore, S., Katz, S. D., Fishman, G. I., Kunichoff, D., Chen, Y., Ogedegbe, G., & Hochman, J. S. (2020). Renin-Angiotensin-Aldosterone System Inhibitors and Risk of Covid-19. The New England Journal of Medicine, 382 (25), 2441–2448. 10.1056/NEJMoa2008975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato, H., Callister, M. E. J., Mumby, S., Quinlan, G. J., Welsh, K. I., DuBois, R. M., & Evans, T. W. (2004). KL-6 levels are elevated in plasma from patients with acute respiratory distress syndrome. The European Respiratory Journal, 23(1), 142–145. 10.1183/09031936.03.00070303 [DOI] [PubMed] [Google Scholar]
- Schoeman, D., & Fielding, B. C. (2019). Coronavirus envelope protein: Current knowledge. Virology Journal, 16(1), 69. 10.1186/s12985-019-1182-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soro-Paavonen, A., Gordin, D., Forsblom, C., Rosengard-Barlund, M., Waden, J., Thorn, L., Sandholm, N., Thomas, M. C., & Groop, P. H. (2012). Circulating ACE2 activity is increased in patients with type 1 diabetes and vascular complications. Journal of Hypertension, 30, 375–383. 10.1097/HJH.0b013e32834f04b6 [DOI] [PubMed] [Google Scholar]
- Spadaro, S., Park, M., Turrini, C., Tunstall, T., Thwaites, R., Mauri, T., Ragazzi, R., Ruggeri, P., Hansel, T. T., Caramori, G., & Volta, C. A. (2019). Biomarkers for acute respiratory distress syndrome and prospects for personalised medicine. Journal of Inflammation (London), 16(1), 1–11. 10.1186/s12950-018-0202-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stawiski, E. W., Diwanji, D., Suryamohan, K., Gupta, R., Fellouse, F. A., Sathirapongsasuti, F., Liu, J., Jiang, Y. P., Ratan, A., Mis, M., Santhosh, D., Somasekar, S., Mohan, S., Phalke, S., Kuriakose, B., Antony, A., Junutula, J. R., Schuster, S. C., Jura, N., Seshagiri, S. (2020). Human ACE2 receptor polymorphisms predict SARS-CoV-2 susceptibility. bioRxiv. https://www.biorxiv.org/content/10.1101/2020.04.07.024752v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su, S., Wong, G., Shi, W., Liu, J., Lai, A. C. K., Zhou, J., Liu, W., Bi, Y., & Gao, G. F. (2016). Epidemiology, genetic recombination, and pathogenesis of coronaviruses. Trends in Microbiology, 24(6), 490–502. 10.1016/j.tim.2016.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweeney, T. E., & Khatri, P. (2017). Generalizable biomarkers in critical care: Toward precision medicine. Critical Care Medicine, 45(6), 934–939. 10.1097/CCM.0000000000002402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tao, Y., Shi, M., Chommanard, C., Queen, K., Zhang, J., Markotter, W., Kuzmin, I. V., Holmes, E. C., & Tong, S. (2017). Surveillance of bat coronaviruses in Kenya identifies relatives of human coronaviruses NL63 and 229E and their recombination history. Journal of Virology, 91(5), e01953–16. 10.1128/JVI.01953-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasudevan, A., Lodha, R., & Kabra, S. K. (2004). Acute lung injury and acute respiratory distress syndrome. Indian Journal of Pediatrics, 71(8), 743–750. 10.1007/BF02730667 [DOI] [PubMed] [Google Scholar]
- Wang, C., Horby, P. W., Hayden, F. G., & Gao, G. F. (2020). A novel coronavirus outbreak of global health concern. The Lancet, 395(10223), 470–473. 10.1016/S0140-6736(20)30185-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, D., Hu, B., Hu, C., Zhu, F., Liu, X., Zhang, J., Wang, B., Xiang, H., Cheng, Z., Xiong, Y., Zhao, Y., Li, Y., Wang, X., & Peng, Z. (2020). Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA, 323(11), e201585. 10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware, L. B., & Calfee, C. S. (2016). Biomarkers of ARDS: What's new? Intensive Care Medicine, 42(5), 797–799. 10.1007/s00134-015-3973-0 [DOI] [PubMed] [Google Scholar]
- Ware, L. B., Koyama, T., Zhao, Z., Janz, D. R., Wickersham, N., Bernard, G. R., May, A. K., Calfee, C. S., & Matthay, M. A. (2013). Biomarkers of lung epithelial injury and inflammation distinguish severe sepsis patients with acute respiratory distress syndrome. Critical Care (London, England), 17(5), R253. 10.1186/cc13080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, Y., Ho, W., Huang, Y., Jin, D.-Y., Li, S., Liu, S.-L., Liu, X., Qiu, J., Sang, Y., Wang, Q., Yuen, K.-Y., & Zheng, Z.-M. (2020). SARS-CoV-2 is an appropriate name for the new coronavirus. The Lancet, 395(10228), 949–950. 10.1016/S0140-6736(20)30557-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wujtewicz, M., Dylczyk-Sommer, A., Aszkiełowicz, A., Zdanowski, S., Piwowarczyk, S., & Owczuk, R. (2020). COVID-19 - what should anaethesiologists and intensivists know about it?. Anaesthesiol Intensive Ther, 52(1), 34–41. 10.5114/ait.2020.93756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu, X., Chen, P., Wang, J., Feng, J., Zhou, H., Li, X., Zhong, W., & Hao, P. (2020). Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. Science China Life Sciences, 63(3), 457–460. 10.1007/s11427-020-1637-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang, M., Zhao, J., Xing, L., & Shi, L. (2015). The association between angiotensin-converting enzyme 2 polymorphisms and essential hypertension risk: A meta-analysis involving 14,122 patients. Journal of the Renin-Angiotensin-Aldosterone System, 16(4), 1240–1244. 10.1177/1470320314549221 [DOI] [PubMed] [Google Scholar]
- Yang, X., Yu, Y., Xu, J., Shu, H., Xia, J., Liu, H., Wu, Y., Zhang, L., Yu, Z., Fang, M., Yu, T., Wang, Y., Pan, S., Zou, X., Yuan, S., & Shang, Y. (2020). Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. The Lancet Respiratory Medicine, 8(5), 475–481. 10.1016/S2213-2600(20)30079-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin, Y., & Wunderink, R. G. (2018). MERS, SARS and other coronaviruses as causes of pneumonia. Respirology (Carlton, Victoria), 23(2), 130–137. 10.1111/resp.13196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zemans, R. L., & Matthay, M. A. (2017). What drives neutrophils to the alveoli in ARDS?. Thorax, 72(1), 1–3. 10.1136/thoraxjnl-2016-209170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao, Y., Zhao, Z., Wang, Y., Zhou, Y., Ma, Y., & Zuo, W. (2020). Single-cell RNA expression profiling of ACE2, the putative receptor of Wuhan 2019-nCov. bioRxiv. 10.1101/2020.01.26.919985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng, J. (2020). SARS-CoV-2: An emerging coronavirus that causes a global threat. International Journal of Biological Sciences, 16 (10), 1678–1685. 10.7150/ijbs.45053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou, J. B., & Yang, J. K. (2009). Meta-analysis of association of ACE2 G8790A polymorphism with Chinese Han essential hypertension . Journal of the Renin-Angiotensin-Aldosterone System : Jraas, 10(1), 31–34. 10.1177/1470320309103047 [DOI] [PubMed] [Google Scholar]
- Zhou, P., Fan, H., Lan, T., Yang, X.-L., Shi, W.-F., Zhang, W., Zhu, Y., Zhang, Y.-W., Xie, Q.-M., Mani, S., Zheng, X.-S., Li, B., Li, J.-M., Guo, H., Pei, G.-Q., An, X.-P., Chen, J.-W., Zhou, L., Mai, K.-J., … Ma, J.-Y. (2018). Fatal swine acute diarrhoea syndrome caused by an HKU2-related coronavirus of bat origin . Nature, 556(7700), 255–258. 10.1038/s41586-018-0010-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou, P., Yang, X.-L., Wang, X.-G., Hu, B., Zhang, L., Zhang, W., Si, H.-R., Zhu, Y., Li, B., Huang, C.-L., Chen, H.-D., Chen, J., Luo, Y., Guo, H., Jiang, R.-D., Liu, M.-Q., Chen, Y., Shen, X.-R., Wang, X., … Shi, Z.-L. (2020). A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature, 579(7798), 270–273. 10.1038/s41586-020-2012-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou, X., Chen, K., Zou, J., Han, P., Hao, J., & Han, Z. (2020). Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection. Frontiers of Medicine, 14(2), 185–192. 10.1007/s11684-020-0754-0 [DOI] [PMC free article] [PubMed] [Google Scholar]