Abstract
Since the outbreak of coronavirus disease 2019 (COVID-19) in December 2019, an epidemic has spread rapidly worldwide. COVID-19 is caused by the highly infectious severe acute respiratory syndrome coronavirus-2. A 42-year-old woman presented to hospital who was suffering from epigastric discomfort and dyspepsia for the past 5 days. Before the onset of symptoms, she was healthy, and had no travel history to Wuhan or contact with laboratory-confirmed COVID-19 cases. An examination showed chronic superficial gastritis with erosion and esophagitis. Enhanced magnetic resonance imaging of the abdomen showed a lesion in the right lower lobe of the lungs. Chest computed tomography showed multiple ground-glass opacity in the lungs. Reverse transcription-polymerase chain reaction was negative for severe acute respiratory syndrome coronavirus-2. There was no improvement after antibiotic treatment. Polymerase chain reaction performed 2 days later was positive and she was diagnosed with COVID-19. After several days of antiviral and symptomatic treatments, her symptoms improved and she was discharged. None of the medical staff were infected. Clinical manifestations of COVID-19 are nonspecific, making differentiating it from other diseases difficult. This case shows the sequence in which symptoms developed in a patient with COVID-19 with gastrointestinal symptoms as initial manifestations.
Keywords: COVID-19, severe acute respiratory syndrome coronavirus-2, gastrointestinal symptoms, angiotensin-converting enzyme 2, lungs, dyspepsia, reverse transcriptase-polymerase chain reaction
Background
Beginning in December 2019, there was an outbreak of pneumonia of an unknown cause in Wuhan, China that was related to the new coronavirus severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2).1,2 Coronavirus disease 2019 (COVID-19) infection has spread worldwide, with almost 2470,000 people infected as of 23 April 2020.3 The spread of COVID-19 has caused a large amount of disruptions to standard hospital services.4 COVID-19 has the main symptoms of fever, fatigue, dry cough, nasal congestion, runny nose, and diarrhea.5,6 Some patients experience dyspnea and hypoxemia. In severe cases, patients may experience acute respiratory distress syndrome and viral septic shock.7 A smaller percentage of patients with COVID-19 have abdominal discomfort as the first symptom compared with patients who are infected by SARS-CoV and Middle East respiratory syndrome coronavirus.8–10 We report a case of a patient who presented to hospital with abdominal discomfort and describe how the patient was diagnosed.
Case presentation
On 22 January 2020, a 42-year-old woman with no history of disease presented to Ningbo First Hospital (Zhejiang, China). She suffered from upper abdominal discomfort, including belching, which had persisted for 5 days. She did not report the common COVID-19 symptoms and had not traveled to Wuhan or other endemic areas of COVID-19. She was otherwise healthy, with no history of thoracic, cardiovascular, or abdominal diseases. Endoscopy showed chronic superficial gastritis with erosion and esophagitis. An abdominal computed tomography (CT) scan showed intrahepatic nodules and no lung infection on 23 January (Figure 1a and b). She was diagnosed with gastritis, dyspepsia, and liver tumors, and was treated with omeprazole, pancreatin, and rebamipide for 3 days.
Figure 1.
(a, b) Abdominal computed tomographic images taken on 23 January 2020. (c, d) Abdominal enhanced magnetic resonance images taken on 26 January 2020, which show a lesion in the right lower lobe of the lungs.
Enhanced magnetic resonance imaging of the abdomen performed on 26 January showed a lesion in the right lower lobe of the lungs (Figure 1c and d). CT scans performed on the same day showed multiple ground-glass opacities in the lungs (Figure 2a, b and c). She was diagnosed as having pneumonia and was referred to the respiratory clinic for treatment.
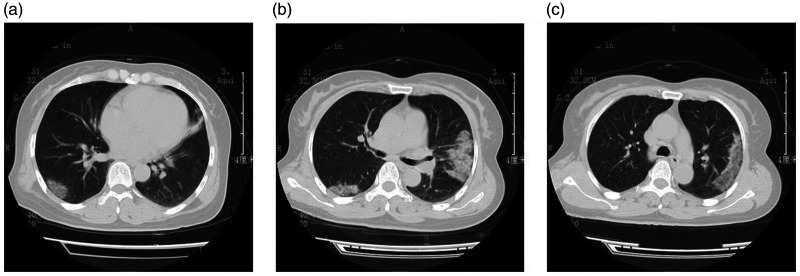
Figure 2.
(a–c) Computed tomographic images show multiple ground-glass opacities in the lungs on 26 January 2020.
On 23 January, she began to experience fever and a runny nose. In consideration of the new scan results and the fever, she was transferred for the second time to the fever clinic on 26 January. Her body temperature was 37.4°C. A complete blood count showed a white blood cell count of 5300 cells/mm3, with 69.4% neutrophils, 22.5% lymphocytes, and 7.9% monocytes. The C-reactive protein level was 5.08 mg/L. Liver function, and creatine kinaselactate dehydrogenase levels were within normal limits.
To treat pneumonia, we empirically started ceftriaxone 2.0 g once daily and levofloxacin 0.4 g once daily. Reverse transcription- polymerase chain reaction (RT-PCR) using a throat swab sample was performed on 27 January, but the result was negative for SARS-CoV-2. The Ningbo First Hospital response team decided that a second RT-PCR assay was required to exclude COVID-19. The patient was persuaded to return to the hospital and tested positive for SARS-CoV-2 with a throat swab specimen by RT-PCR on 29 January. Therefore, her diagnosis was confirmed as COVID-19 in accordance with the Diagnosis and Treatment Guideline of the National Health Committee of China.11
The patient was treated with Lianhua Qingwen capsules 16.8 g three times daily, umifenovir 200 mg three times daily, and lopinavir and ritonavir tablets 600 mg twice daily for 2 days. She was transferred to Ningbo No. 2 Hospital on 30 January. She was then treated with moxifloxacin, umifenovir, lopinavir, and ritonavir tablets, interferon-2α, and thymosin. After several days of symptomatic treatment, cough and suffocation in the chest gradually subsided. A chest CT scan showed major improvement. RT-PCR for SARS-CoV-2 was negative twice from throat swab specimens on 5 and 6 February 2020 and once with a rectal swab specimen on 6 February 2020. In accordance with the guidelines, the patient was clear of SARS-CoV-2 and was discharged from the hospital on 6 February 2020.7
Discussion and conclusions
The main symptoms of COVID-19 are fever, dry cough, expectoration, and fatigue. Some of these patients present with anorexia, diarrhea, nausea, and vomiting.12,13 Our previous study reported the symptoms of 91 patients with COVID-19 in whom 71.43% had fever, 60.44% reported a dry cough, 32.97% reported expectoration, and 23.08% had diarrhea. Asymptomatic infections were also reported.14,15 The current patient was a middle-aged woman with no epidemiological history of COVID-19. She did not have fever or dry cough, which are the two most common COVID-19 symptoms. Gastrointestinal symptoms were the first manifestations for COVID-19 in this case.
A mechanism for COVID-19 first manifesting as gastrointestinal symptoms has been identified. A recent study showed that the spike (S) glycoprotein of SARS-CoV-2 is responsible for mediating viral cell membrane and host membrane fusion during infection.16 Angiotensin-converting enzyme 2 has been identified as a functional receptor for SARS-CoV-2, which is similar to the sequence of SARS-CoV.1,17,18 On the basis of angiotensin-converting enzyme 2 mRNA and protein expression in normal tissue as shown in the Human Protein Atlas database (https: //www.proteinatlas.org/ENSG00000130234-ACE2) (Figure 3), we speculate that angiotensin-converting enzyme 2 is not only expressed in lung cells, but also highly expressed in epithelial cells of the digestive tract. Therefore, the digestive system is a potential route of infection.19 This explains why gastrointestinal symptoms can be the first manifestations of COVID-19.
Figure 3.
Angiotensin-converting enzyme 2 (ACE-2) mRNA and protein expression in normal tissues based on the Human Protein Atlas database (https: //www.proteinatlas.org/ENSG00000130234-ACE2).
The clinical manifestations of COVID-19 are common to many diseases. When the first manifestations of COVID-19 are gastrointestinal symptoms, the process of being diagnosed with COVID-19 is extended and patients may transmit this disease to many others while they seek treatment. Before the positive diagnosis of COVID-19, our patient had been treated at the Internal Medicine Department, Hepatological Surgery Department, Digestive Department, Respiratory Department, and fever clinic. She underwent a series of examinations, including abdominal enhanced magnetic resonance imaging, a chest CT scan, and electronic gastroscopy. Seventeen medical staff in our hospital had to be isolated for 14 days following her positive diagnosis. Fortunately, none of the medical staff were infected, which could have been a result of the strict measures applied to prevent nosocomial infection.
COVID-19 can first manifest as nonspecific symptoms and lead to a delayed diagnosis, with the possibility of nosocomial infections. Medical staff should take measures to prevent being infected by patients with COVID-19 who are asymptomatic or have nonspecific symptoms.
Ethics statement
The study was reviewed and approved by the Medical Ethical Committee at Ningbo First Hospital (2020-R018). Written informed consent was obtained from the patient for publication of this case report and the accompanying images. A copy of the written consent has been seen by the Journal Editor.
Acknowledgements
The authors gratefully acknowledge the patient in this report for granting us permission to describe her case.
Author contributions
LPW, NBY, and XPY collected the data. GQQ and CYW conceived the idea and drafted the manuscript. AHYM, GXL, and JJS reviewed the manuscript. All authors read and approved the final manuscript.
Availability of data and materials
All data generated or analyzed during this study are included in the published article.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iD
Guo-Qing Qian https://orcid.org/0000-0003-2427-8042
References
- 1.Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020; 579: 270–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Paules CI, Marston HD, Fauci AS. Coronavirus Infections-More Than Just the Common Cold. JAMA 2020. [DOI] [PubMed] [Google Scholar]
- 3.Chinese Center for Disease Control and Prevention: Chinese Center for Disease Control and Prevention. COVID-19 pneumonia epidemic map. 2020. http: //2019ncov.chinacdc.cn/2019-nCoV/index.html 2020 (accessed 23 April 2020).
- 4.Nepogodiev D, Bhangu A. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xiao F, Tang M, Zheng X, et al. Evidence for Gastrointestinal Infection of SARS-CoV-2. Gastroenterology 2020; 158: 1831–1833.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Di Saverio S, Pata F, Gallo G, et al. Coronavirus pandemic and colorectal surgery: practical advice based on the Italian experience. Colorectal Dis 2020; 22: 625–634. doi: 10.1111/codi.15056 [DOI] [PubMed] [Google Scholar]
- 7.National Health Commission of the People's Republic of China : Diagnosis and treatment plan of pneumonia caused by novel coronavirus infection (Trial Version 5). Chinese Journal of Integrated Traditional Chinese and Western Medicine 2020; 30: 136–138. http://www.cjim.cn/zxyjhcn/zxyjhcn/ch/reader/view_abstract.aspx?file_no=2020020136&flag=1 [Google Scholar]
- 8.Zhou J, Li C, Zhao G, et al. Human intestinal tract serves as an alternative infection route for Middle East respiratory syndrome coronavirus. Sci Adv 2017; 3: eaao4966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Openshaw PJ. Crossing barriers: infections of the lung and the gut. Mucosal Immunol 2009; 2: 100–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaafarani HMA, Moheb ME, Hwabejire JO, et al. Gastrointestinal Complications in Critically Ill Patients With COVID-19. Ann Surg 2020; 272: e61–e62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Health Commission of the People’s Republic of China : Diagnosis and treatment plan of pneumonia caused by novel coronavirus infection (Trial Version 3). Tianjin Journal of Traditional Chinese Medicine 2020; 37: 1–3. http://www.tjzhongyiyao.com/tjzyy/ch/reader/view_abstract.aspx?file_no=20200101&flag=1 [Google Scholar]
- 12.Zhu N, Zhang D, Wang W, et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med 2020; 382: 727–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang D, Hu B, Hu C, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA 2020; 323: 1061–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Qian GQ, Yang NB, Ding F, et al. Epidemiologic and Clinical Characteristics of 91 Hospitalized Patients with COVID-19 in Zhejiang, China: A retrospective, multi-centre case series. QJM 2020; 113: 474–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Qian G, Yang N, Ma AHY, et al. A COVID-19 transmission within a family cluster by presymptomatic infectors in China. Clin Infect Dis 2020; 71: 861–862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang Q, Qiu Y, Li JY, et al. A Unique Protease Cleavage Site Predicted in the Spike Protein of the Novel Pneumonia Coronavirus (2019-nCoV) Potentially Related to Viral Transmissibility. Virol Sin 2020; 35: 337–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.De Wilde AH, Snijder EJ, Kikkert M, et al. Host Factors in Coronavirus Replication. Curr Top Microbiol Immunol 2018; 419: 1–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wan Y, Shang J, Graham R, et al. Receptor recognition by novel coronavirus from Wuhan: An analysis based on decade-long structural studies of SARS. J Virol 2020; 94: e00127-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang H, Kang Z, Gong H, et al. Digestive system is a potential route of COVID-19: an analysis of single-cell coexpression pattern of key proteins in viral entry process. Gut 2020; 69: 1010–1018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in the published article.