At the onset of the COVID-19 pandemic, emergency legislation expanding the coverage of telehealth service swept across the nation to allow for continued access to medical care despite strict shelter-in-place guidelines.1 In the wake of this, telehealth usage has increased dramatically.2 Dermatology, in particular, is uniquely amenable to virtual visits, and teledermatology has the potential to become a permanent platform from which we provide specialty care.
As telehealth expands, additional data are needed on the impact of telehealth on health equity. Missed appointments, or no-shows, are a measure of health disparity, with low-income, Medicaid, and minority patients traditionally having the highest no-show rates.3 Given the ability of teledermatology to theoretically improve patient convenience and eliminate potential barriers to care, we sought to investigate the impact of telehealth on no-show rates and patient access at a large academic medical center.
The institutional review board of the University of Massachusetts designated this study exempt from institutional review as a quality improvement project. A retrospective chart review was conducted on all patients with completed or no-show appointments with a dermatologist at the UMass Memorial Hahnemann Campus during the months of May and June of 2019 and 2020. Procedural appointments were excluded. In-person visits and televisits, which were conducted using Doximity (San Francisco, CA) or AmWell (Boston, MA) software, were included. Clinic and televisit no-show rates were calculated using data from 2019 and 2020, respectively. Statistical analysis was performed with the Fisher exact test and 2-tailed P values < .05 were considered statistically significant. The Bonferroni method was applied to correct P values where indicated.
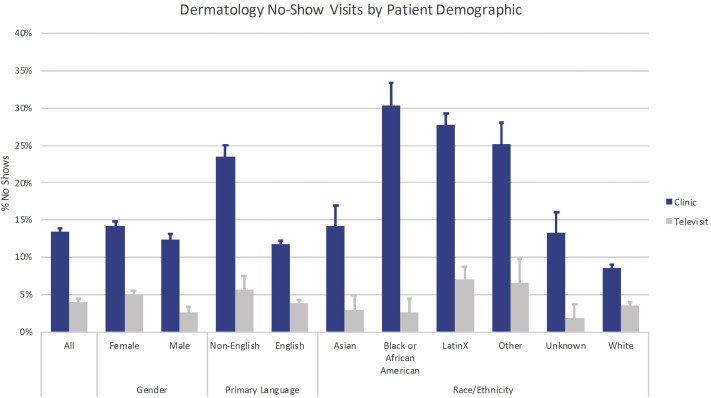
Compared with clinic visits, televisits had significantly lower no-show rates, with the greatest reductions seen for Black or African American, LatinX, and primary non–English-speaking patients (Fig 1 , Table I ). Compared with clinic visits, televisits served a greater percentage of Medicaid enrollees and patients under 50 years of age (Table I). There was no significant difference in the racial/ethnic background of patients seen via the 2 platforms, with a similar proportion of minority patients seen in televisits versus clinic visits (504 of 1568 [32.1%] vs 1581 of 5315 [29.7%]; P = .19).
Fig 1.
No-show rates between clinic and teledermatology visits for all patients and stratified by patient demographic subgroups: gender, primary language, and race/ethnicity. Error bars show the standard error of the mean.
Table I.
Comparison of patient composition and no-show rates in clinic versus teledermatology visits for all patients and stratified by patient demographic subgroups
| Patient demographics | Percent no-show (no-show visits/total visits) |
||
|---|---|---|---|
| Televisits | Clinic visits | P value | |
| All | 4.0% (63/1568) | 13.4% (711/5315) | <.0001∗ |
| Gender | |||
| Female | 4.9% (47/969) | 14.2% (423/2992) | <.0001∗ |
| Male | 2.7% (16/599) | 12.4% (288/2322) | <.0001∗ |
| Primary language | |||
| Non-English | 5.6% (8/143) | 12.5% (174/742) | <.0001∗ |
| English | 3.9% (55/1425) | 11.8% (538/4573) | <.0001∗ |
| Race/Ethnicity | Adjusted P value | ||
| Asian | 2.9% (2/69) | 14.2% (24/169) | .15 |
| Black or African American | 2.6% (2/77) | 30.4% (68/224) | .0006∗ |
| LatinX | 7.0% (17/242) | 27.7% (229/826) | .0006∗ |
| Other | 6.6% (4/61) | 25.1% (53/211) | .04 |
| Unknown | 1.8% (1/55) | 13.3% (20/151) | .18 |
| White | 3.5% (37/1064) | 8.5% (318/3734) | .0006∗ |
| Age, y | |||
| <50 | 4.3% (41/964) | 18.7% (423/2268) | <.0001∗ |
| ≥50 | 3.6% (22/604) | 8.6% (289/3372) | <.0001∗ |
| Insurance payer | Completed televisits | Completed clinic visits | Adjusted P value |
| Private | 60.6% (975/1607) | 54.5% (2462/4514) | .08 |
| Medicaid | 25.5% (410/1607) | 19.6% (885/4514) | .0003∗ |
| Medicare | 13.8% (222/1607) | 25.9 % (1167/4514) | .0003∗ |
| Total | 1607 | 4514 | |
Statistically significant.
The data show a particularly striking reduction in no-show rates for minority patients seen via teledermatology. At the same time, both platforms served a similar population of patients with respect to race/ethnicity, while televisits saw a greater percentage of Medicaid but smaller percentage of Medicare enrollees, possibly reflecting age-dependent differences in comfort with virtual visits. Lack of private transportation, access to childcare, and inflexible work schedules contribute to higher no-show rates in minority patients and patients with Medicaid.4 , 5 Significant reductions in no-show rates with teledermatology suggest that televisits may help mitigate barriers to care and improve access for these patients.
Limitations of this study include its small sample size and single institution experience. However, this study provides early evidence that teledermatology may play an important role in mitigating no-show rates and improving access to our most vulnerable populations. Further investigation into the impact of telehealth on health inequity is vital to informing future policy making regarding continued insurance coverage of telemedicine moving forward.
Footnotes
Funding: Supported by Harvard Catalyst, The Harvard Clinical and Translational Science Center (National Center for Advancing Translational Sciences, National Institutes of Health Award UL 1TR002541) and financial contributions from Harvard University and its affiliated academic health care centers. The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic health care centers, or the National Institutes of Health.
Conflicts of interest: None declared.
IRB status: The institutional review board of the University of Massachusetts designated this study exempt from institutional review as a quality improvement project.
Reprints not available from the authors.
References
- 1.Kassamali B., Haddadi N.S., Rashighi M., Cavanaugh-Hussey M., LaChance A. Telemedicine and the battle for health equity: translating temporary regulatory orders into sustained policy change. J Am Acad Dermatol. 2020 doi: 10.1016/j.jaad.2020.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Newswire P.R. Telehealth claim lines increase 4,347 percent nationally from March 2019 to March 2020. https://www.prnewswire.com/news-releases/telehealth-claim-lines-increase-4-347-percent-nationally-from-march-2019-to-march-2020--301069182.html Available at:
- 3.Dantas L.F., Fleck J.L., Cyrino Oliveira F.L., Hamacher S. No-shows in appointment scheduling - a systematic literature review. Health Policy. 2018;122:412–421. doi: 10.1016/j.healthpol.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 4.Syed S.T., Gerber B.S., Sharp L.K. Traveling towards disease: transportation barriers to health care access. J Community Health. 2013;38:976–993. doi: 10.1007/s10900-013-9681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sharp D.J., Hamilton W. Non-attendance at general practices and outpatient clinics. BMJ. 2001;323:1081–1082. doi: 10.1136/bmj.323.7321.1081. [DOI] [PMC free article] [PubMed] [Google Scholar]