Abstract
Background
The coronavirus disease 2019 (COVID-19) pandemic has severely affected ICUs and critical care health-care providers (HCPs) worldwide.
Research Question
How do regional differences and perceived lack of ICU resources affect critical care resource use and the well-being of HCPs?
Study Design and Methods
Between April 23 and May 7, 2020, we electronically administered a 41-question survey to interdisciplinary HCPs caring for patients critically ill with COVID-19. The survey was distributed via critical care societies, research networks, personal contacts, and social media portals. Responses were tabulated according to World Bank region. We performed multivariate log-binomial regression to assess factors associated with three main outcomes: limiting mechanical ventilation (MV), changes in CPR practices, and emotional distress and burnout.
Results
We included 2,700 respondents from 77 countries, including physicians (41%), nurses (40%), respiratory therapists (11%), and advanced practice providers (8%). The reported lack of ICU nurses was higher than that of intensivists (32% vs 15%). Limiting MV for patients with COVID-19 was reported by 16% of respondents, was lowest in North America (10%), and was associated with reduced ventilator availability (absolute risk reduction [ARR], 2.10; 95% CI, 1.61-2.74). Overall, 66% of respondents reported changes in CPR practices. Emotional distress or burnout was high across regions (52%, highest in North America) and associated with being female (mechanical ventilation, 1.16; 95% CI, 1.01-1.33), being a nurse (ARR, 1.31; 95% CI, 1.13-1.53), reporting a shortage of ICU nurses (ARR, 1.18; 95% CI, 1.05-1.33), reporting a shortage of powered air-purifying respirators (ARR, 1.30; 95% CI, 1.09-1.55), and experiencing poor communication from supervisors (ARR, 1.30; 95% CI, 1.16-1.46).
Interpretation
Our findings demonstrate variability in ICU resource availability and use worldwide. The high prevalence of provider burnout and its association with reported insufficient resources and poor communication from supervisors suggest a need for targeted interventions to support HCPs on the front lines.
Key Words: burnout, COVID-19, critical care, emotional distress, mechanical ventilation, resource use, survey
FOR EDITORIAL COMMENT, SEE PAGE 469
As of August 27, 2020, the coronavirus disease 2019 (COVID-19) pandemic had resulted in 204,290,582 confirmed cases worldwide and taken 828,070 lives in 188 countries.1 , 2 With 5% to 38% of patients hospitalized with COVID-19 requiring admission to an ICU,3, 4, 5 and 75% to 88% of patients critically ill with COVID-19 requiring mechanical ventilation (MV),5, 6, 7, 8 ICUs around the world have been facing major challenges, including determining the appropriate allocation of resources and balancing the care of patients with COVID-19 and that of other patients who are critically ill, while having to restructure workflows and ensure the safety of patients, their families, and health-care providers (HCPs).
A better characterization of the pandemic’s effects on ICU resources (three crucial elements: stuff, staff, and space9) and on HCPs worldwide is important to identifying strategies to support health-care systems across the world in surmounting this crisis, as well as potential future disasters, when rationing of resources may be necessary. With this international survey, we aimed to assess rapidly the key concerns of interprofessional HCPs on the front lines caring for patients critically ill with COVID-19.
Materials and Methods
Survey Design
An interprofessional health-care team, including physicians, nurses, respiratory therapists (RTs), and advanced practice providers (APPs, defined as advanced registered nurse practitioners, physician assistants, and certified registered nurse anesthetists), developed a 41-question structured questionnaire in English (Appendix 1) to elicit perceptions of international HCPs in the context of available staffing, critical care resources, and space. We followed the Strengthening the Reporting of Observational Studies in Epidemiology guidelines for the reporting of cross-sectional studies.10 Data were collected using Research Electronic Data Capture tools hosted at the Institute of Translational Health Sciences.11 Certain questions were displayed contingent on preceding responses. Before distribution, the survey was pilot tested by 30 HCPs from five countries who were not included in the final analysis.
Ethics Approval
The study was deemed exempt by the University of Washington Institutional Review Board because no personally identifying data were recorded and written consent was not required. Before initiating the survey, respondents were informed that the survey was anonymous, participation was voluntary, and summary results would be shared with the scientific community.
Population
Our target population included physicians, nurses, APPs, and RTs who care for patients with COVID-19 hospitalized in an ICU. We asked survey respondents to self-attest to having direct involvement in the care of patients with COVID-19 requiring intensive care. Respondents who negated this question (n = 426) were excluded from the analysis, along with participants who completed only demographic information (n = 37).
Survey Administration
The survey was distributed electronically between April 23 and May 7, 2020, with the intention of capturing data during or close to the time of peak surges in many countries. HCPs were reached via the following strategies. The World Federation of Intensive and Critical Care e-mailed its 85 scientific member societies and encouraged them to distribute the survey among their membership. We collaborated with 16 critical care professional societies (e-Appendix 1) who shared the link with their membership (via e-mail or post on websites or social media). The survey link was distributed to relevant subgroups within the Global Sepsis Alliance and the Prevention and Early Treatment of Acute Lung Injury network. We e-mailed corresponding authors from clinical publications about patients critically ill with COVID-19 on the basis of a literature search of COVID-19 publications from February 1 to April 22, 2020. Personal contacts of the authors known to care directly for patients with COVID-19 in the ICU were invited to participate and asked to distribute the survey to their colleagues. Lastly, we distributed the link on Twitter and Facebook and shared it within intensive care and critical care forums focusing on COVID-19 that required medical credentials to approve members. Posts were sharable to facilitate widespread distribution.
We chose this convenience sampling approach to reach a large number of HCPs worldwide in a short period. We accepted that we would not be able to gauge accurate individual response rates because of various dissemination mechanisms (eg, critical care societies sharing the link on various websites and social media portals) and that we had limited ability to confirm how many respondents saw or received the link within these forums.
Variable Categorization
Countries were categorized according to World Bank region: East Asia and Pacific, Europe and Central Asia, Latin America and the Caribbean, Middle East and North Africa, North America, South Asia, and sub-Saharan Africa. We categorized countries into before, during, and after the peak of deaths per day12 , 13 and calculated an indicator of how much a country was affected by COVID-19 at the time of survey administration (the severity index in e-Table 1 and data in e-Table 2) by using the average daily death rate by population.13 , 14 Mortality was chosen as a surrogate for peak and severity index instead of incidence because mortality is less confounded by testing availability and serves as an indicator of disease burden on ICUs.
Statistical Analysis
We used descriptive statistics to report respondent characteristics and survey outcomes. We used univariate binomial regression to assess associations among region, provider type, and prespecified outcomes of interest. We conducted multivariate log-binomial regression to assess predictors of three main outcomes: limiting the use of MV for patients with COVID-19, changing policies or practices of CPR, and reporting emotional distress and burnout. These outcomes were selected as surrogates for ICU resource use (the first two items) and the psychological burden of the pandemic on HCPs (the third item). Exposures considered included provider type, sex, perceived lack of resources (organized by three crucial elements: stuff, staff, and space9), time from COVID-19 peak, and severity index. Exposures that were statistically significant in the univariate regression were considered for inclusion in the multivariate model. We performed a complete case analysis; respondents with missing data were removed from regressions. Analyses were conducted using software (R Software; R Foundation for Statistical Computing).15, 16, 17
Results
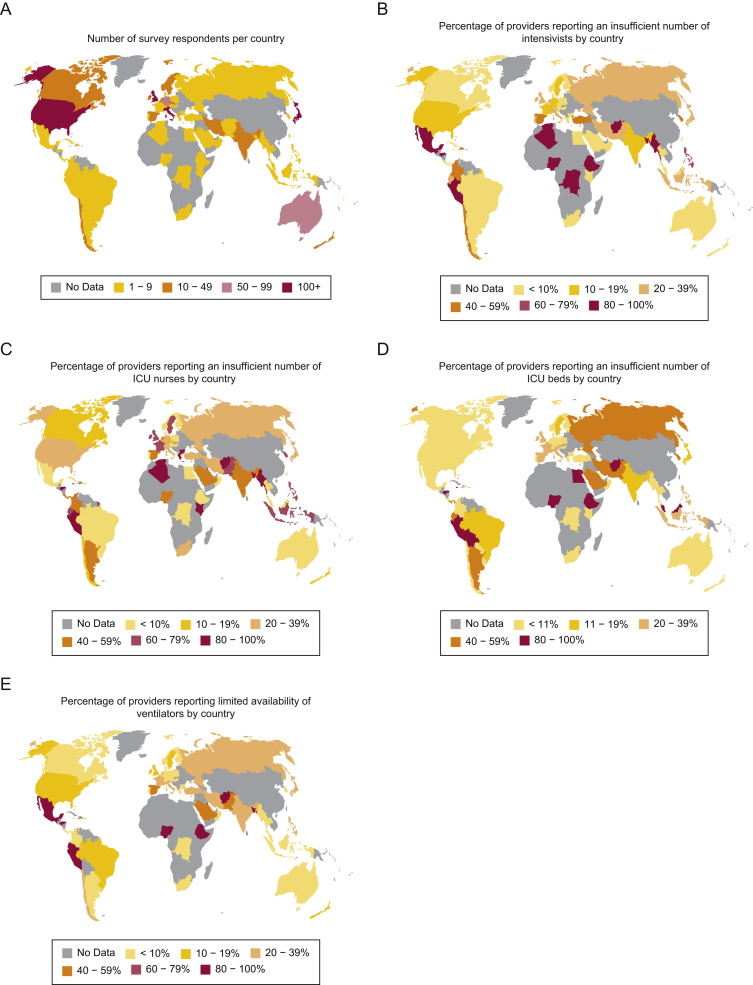
We identified and approached contacts in 95 countries and received 3,182 responses from 93 countries; 2,700 respondents from 77 countries were included in the analysis (81% of countries contacted) (Fig 1 A). HCPs within China reported being unable to access the survey link. Reasons for excluding responses are outlined in e-Figure 1. Detailed respondent characteristics by World Bank region are displayed in Table 1 . Most respondents were from North America (63%) and Europe and Central Asia (23%). The top responding countries (with > 50 respondents per country) were the United States, United Kingdom, Italy, Japan, Australia, and Germany. Survey respondents were physicians (41%), nurses (40%), RTs (11%), and APPs (8%). Most participants reported working in urban, large teaching hospitals (71%), and 65% were female. Among the 798 (30%) respondents who opted to disclose their institution, 422 different institutions were reported (e-Table 6). Most respondents listed critical care medicine as a subspecialty: 85% of attending physicians, 69% of physicians in training, and 93% of nurses (e-Table 3). Overall, 76% of respondents (n = 2,056) completed all survey questions.
Figure 1.
World maps displaying number of survey respondents per country (A), percentage of health-care providers (HCPs) reporting an insufficient number of intensivists by country (B), percentage of HCPs reporting an insufficient number of ICU nurses by country (C), percentage of HCPs reporting an insufficient number of ICU beds by country (D), and percentage of HCPs reporting limited availability of ventilators by country (E).
Table 1.
Respondent Characteristics by Region
| Characteristic | East Asia and Pacific (n = 243) | Europe and Central Asia (n = 630) | Latin America and The Caribbean (n = 45) | Middle East and North Africa (n = 50) | North America (n = 1,696) | South Asia (n = 27) | Sub-Saharan Africa (n = 9) | Total (N = 2,700) |
|---|---|---|---|---|---|---|---|---|
| Sex, No. (%) | ||||||||
| Female | 83 (34) | 380 (60) | 14 (31) | 26 (52) | 1,251 (74) | 9 (33) | 4 (44) | 1,767 (65) |
| Male | 158 (65) | 244 (39) | 30 (67) | 23 (46) | 432 (25) | 16 (59) | 5 (56) | 908 (34) |
| Nonbinary | 0 (0) | 2 (0) | 1 (2) | 1 (2) | 1 (0) | 1 (4) | 0 (0) | 6 (0) |
| Not disclosed | 2 (1) | 4 (1) | 0 (0) | 0 (0) | 12 (1) | 1 (4) | 0 (0) | 19 (1) |
| Years in clinical practice, mean (SD) | 18.4 (9.05) | 15.7 (9.78) | 16.9 (9.24) | 14.3 (10.6) | 11.6 (9.40) | 17.7 (11.0) | 12.7 (7.25) | 13.3 (9.79) |
| No. of patients with COVID-19 cared for, No. (%) | ||||||||
| < 10 | 217 (89) | 163 (26) | 25 (56) | 20 (40) | 676 (40) | 19 (70) | 7 (78) | 1,127 (42) |
| 10-50 | 26 (11) | 380 (60) | 16 (36) | 20 (40) | 819 (48) | 8 (30) | 2 (22) | 1,271 (47) |
| > 50 | 0 (0) | 86 (14) | 4 (9) | 10 (20) | 201 (12) | 0 (0) | 0 (0) | 301 (11) |
| Hospital setting, No. (%) | ||||||||
| Rural, < 100 beds | 1 (0) | 6 (1) | 2 (4) | 5 (10) | 33 (2) | 2 (7) | 0 (0) | 49 (2) |
| Rural, ≥ 100 beds | 12 (5) | 28 (4) | 1 (2) | 2 (4) | 89 (5) | 0 (0) | 0 (0) | 132 (5) |
| Urban, no teaching, < 200 beds | 4 (2) | 19 (3) | 8 (18) | 4 (8) | 83 (5) | 3 (11) | 0 (0) | 121 (4) |
| Urban, no teaching, ≥ 200 beds | 25 (10) | 69 (11) | 5 (11) | 3 (6) | 244 (14) | 6 (22) | 0 (0) | 352 (13) |
| Urban, teaching, < 200 beds | 6 (2) | 34 (5) | 9 (20) | 3 (6) | 78 (5) | 1 (4) | 0 (0) | 131 (5) |
| Urban, teaching, ≥ 200 beds | 195 (80) | 473 (75) | 20 (44) | 33 (66) | 1,168 (69) | 15 (56) | 9 (100) | 1,913 (71) |
| Qualification, No. (%) | ||||||||
| Attending physician | 181 (74) | 295 (47) | 34 (76) | 29 (58) | 349 (21) | 23 (85) | 6 (67) | 907 (33) |
| Physician in training | 21 (9) | 59 (9) | 2 (4) | 11 (22) | 109 (6) | 3 (11) | 2 (22) | 207 (8) |
| Nurse | 30 (12) | 248 (39) | 1 (2) | 8 (16) | 738 (44) | 1 (4) | 1 (11) | 1,077 (40) |
| APP | 5 (2) | 22 (3) | 0 (0) | 1 (2) | 183 (11) | 0 (0) | 0 (0) | 211 (8) |
| RT | 6 (2) | 5 (1) | 8 (18) | 1 (2) | 277 (16) | 0 (0) | 0 (0) | 297 (11) |
The number of respondents in each category varies slightly because some responses were optional; multiple responses were possible per respondent regarding area of specialization, so the most frequent subspecialties are reported. Not all percentages total 100% because of rounding. Years in clinical practice includes years in training. Regions are categorized using the World Bank classification of countries (https://datatopics.worldbank.org/world-development-indicators/the-world-by-income-and-region.html). APP = advanced practice provider; COVID-19 = coronavirus disease 2019; RT = respiratory therapist.
Staff
Table 2 and e-Table 4 summarize perceived lack of resources, changes in clinical practice, and HCPs’ concerns by region. Although 15% of respondents reported insufficient numbers of intensivists to care for patients critically ill with COVID-19, 32% reported insufficient numbers of ICU nurses. Regions with the highest report of insufficient numbers of intensivists were sub-Saharan Africa (50%) and Latin America and the Caribbean (37%) compared with North America (11%). The highest report of insufficient numbers of ICU nurses was in South Asia (57%) and Europe and Central Asia (47%) compared with North America (27%). Figures 1B and 1C display the proportion of respondents reporting shortages of intensivists and ICU nurses by country.
Table 2.
Provider Perceptions Regarding Supplies, Treatment of Patients With COVID-19, and Concerns by Region
| Perception | East Asia and Pacific (n = 243) | Europe and Central Asia (n = 630) | Latin America and the Caribbean (n = 45) | Middle East and North Africa (n = 50) | North America (n = 1,696) | South Asia (n = 27) | Sub-Saharan Africa (n = 9) | Total (N = 2,700) |
|---|---|---|---|---|---|---|---|---|
| Perceived lack of ICU resources by region | ||||||||
| Shortages reported | ||||||||
| Intensivists | 40 (18) | 115 (20) | 15 (37) | 13 (29) | 191 (11) | 7 (30) | 4 (50) | 385 (15) |
| ICU nurses | 52 (24) | 277 (47) | 15 (37) | 14 (31) | 432 (27) | 13 (57) | 3 (38) | 806 (32) |
| ICU beds | 25 (13) | 63 (13) | 11 (34) | 10 (29) | 150 (11) | 10 (50) | 3 (50) | 272 (13) |
| PPE availability limited | ||||||||
| Gloves | 22 (10) | 27 (5) | 4 (11) | 5 (11) | 4 (3) | 0 (0) | 2 (24) | 101 (4) |
| Gowns | 56 (26) | 133 (24) | 11 (29) | 16 (37) | 348 (24) | 8 (36) | 6 (75) | 578 (24) |
| Surgical masks | 34 (16) | 70 (12) | 4 (10) | 6 (14) | 201 (14) | 1(5) | 4 (50) | 320 (13) |
| Eye protection | 95 (45) | 213 (38) | 18 (47) | 22 (51) | 561 (37) | 13 (59) | 7 (87) | 929 (39) |
| Face shields | 117 (57) | 256 (45) | 20 (53) | 23 (54) | 627 (42) | 11 (50) | 6 (75) | 1,050 (44) |
| N95 masks | 127 (60) | 285 (53) | 17 (45) | 26 (61) | 877 (58) | 14 (64) | 6 (75) | 1,362 (57) |
| PAPRs | 80 (38) | 147 (27) | 9 (24) | 13 (31) | 825 (55) | 1 (5) | 0 (0) | 1,075 (46) |
| Ventilator supplies limited | ||||||||
| Mechanical ventilation | 21 (10) | 87 (17) | 11 (31) | 13 (34) | 102 (7) | 6 (27) | 3 (43) | 243 (11) |
| NIPPV | 29 (14) | 156 (30) | 20 (57) | 15 (38) | 239 (17) | 10 (45) | 3 (43) | 472 (21) |
| HFNC | 29 (14) | 189 (37) | 15 (43) | 14 (37) | 271 (19) | 9 (41) | 0 (0) | 527 (23) |
| Changes in resource use and provider concerns | ||||||||
| Limiting mechanical ventilation | 32 (16) 161 (31) | 7 (20) | 13 (33) | 140 (10) | 7 (32) | 2 (29) | 362 (16) | |
| CPR policy changes | ||||||||
| Unchanged | 59 (29) | 210 (41) | 12 (34) | 16 (41) | 460 (32) | 7 (32) | 2 (29) | 766 (34) |
| New policy implemented | 83 (41) | 198 (38) | 11 (31) | 12 (31) | 547 (38) | 5 (23) | 2 (29) | 858 (38) |
| No policy change but practice has changed | 59 (29) | 109 (21) | 12 (34) | 11 (28) | 421 (29) | 10 (45) | 3 (43) | 625 (28) |
| CPR in patients with COVID-19 | ||||||||
| Not performed | 18 (9) | 19 (4) | 7 (20) | 4 (10) | 17 (1) | 5 (23) | 4 (57) | 74 (3) |
| Physicians determine | 123 (61) | 368 (71) | 21 (60) | 22 (56) | 450 (32) | 15 (68) | 3 (43) | 1,002 (45) |
| Families determine | 60 (30) | 130 (25) | 7 (20) | 13 (33) | 961 (67) | 2 (9) | 0 (0) | 1,173 (52) |
| Allow families to participate in critical decisions for patients with COVID-19 | ||||||||
| More than other patients in the ICU | 14 (7) | 17 (3) | 1 (3) | 5 (13) | 74 (5) | 4 (18) | 3 (43) | 118 (5) |
| Same as other patients in the ICU | 165 (82) | 386 (75) | 24 (71) | 25 (64) | 1,189 (84) | 13 (59) | 3 (43) | 1,805 (81) |
| Less than other patients in the ICU | 21 (10) | 112 (22) | 9 (26) | 9 (23) | 155 (11) | 5 (23) | 1 (14) | 312 (14) |
| Palliative care consultations for patients with COVID-19 | ||||||||
| ≥ 50% of patients | 9 (5) | 31 (6) | 1 (3) | 5 (14) | 411 (30) | 1 (5) | 1 (17) | 459 (21) |
| < 50% of patients | 42 (22) | 111 (22) | 9 (26) | 4 (11) | 416 (31) | 0 (0) | 2 (33) | 584 (27) |
| Did not consult palliative care specialists | 83 (44) | 249 (50) | 11 (32) | 15 (43) | 105 (8) | 7 (35) | 1 (17) | 471 (22) |
| No palliative care specialists available | 19 (10) | 59 (12) | 9 (26) | 7 (20) | 48 (4) | 11 (55) | 2 (33) | 155 (7) |
| Not sure | 36 (19) | 48 (10) | 4 (12) | 4 (11) | 376 (28) | 1 (5) | 0 (0) | 469 (22) |
| Palliative care consultations | ||||||||
| More than before pandemic | 6 (12) | 26 (18) | 3 (30) | 3 (33) | 371 (45) | 1 (100) | 1 (33) | 411 (39) |
| Provider concerns | ||||||||
| Emotional distress and burnout | 73 (30) | 305 (48) | 19 (42) | 22 (44) | 974 (57) | 9 (33) | 3 (33) | 1,405 (52) |
| Worried about infecting family at home | 122 (50) | 345 (55) | 21 (47) | 25 (50) | 1,119 (66) | 17 (63) | 5 (56) | 1,654 (61) |
| Worried about own health | 10 (31) | 80 (50) | 3 (43) | 5 (38) | 91 (65) | 6 (86) | 1 (50) | 196 (54) |
| Social stigma from community | 37 (15) | 91 (14) | 6 (13) | 7 (14) | 434 (26) | 4 (15) | 0 (0) | 579 (21) |
| Feel that hospital unable to keep me safe | 36 (15) | 107 (17) | 7 (16) | 7 (14) | 433 (26) | 6 (22) | 2 (22) | 598 (22) |
| Poor communication from supervisors | 30 (12) | 134 (21) | 3 (7) | 8 (16) | 366 (22) | 4 (15) | 2 (22) | 547 (20) |
| Worries about financial situation | 20 (8) | 36 (6) | 11 (24) | 6 (12) | 212 (13) | 6 (22) | 0 (0) | 292 (11) |
Data are presented as No. (%). The number of respondents in each category is slightly different because of missing data and some responses being optional. HFNC = high-flow nasal cannula; NIPPV = noninvasive positive pressure ventilation; PAPR = powered air-purifying respirator; PPE = personal protective equipment. See Table 1 legend for expansion of other abbreviation.
Space
Shortages of ICU beds were reported by 13% of respondents (ranging from 11% in North America to 50% in South Asia) to care for patients critically ill with COVID-19 (Fig 1D) and by 17% (ranging from 13% in North America to 41% in Latin America and the Caribbean) for other patients requiring ICU care. e-Figure 2 displays reported measures that were implemented to mitigate the effect of ICU bed shortages, including the conversion of postoperative recovery rooms (reported by 20%) and operating rooms (12%).
Stuff
Testing
The severe acute respiratory syndrome coronavirus 2 real-time polymerase chain reaction test was available for all patients according to 35% of respondents and for “select patients based on symptoms” according to 56% (e-Table 4). For HCPs, the test was available for all according to 15% of respondents and for “select HCPs based on symptoms and area of work” according to 62%. Among the respondents who reported testing was available, 41% indicated that it required hospital approval. Few respondents reported absence of testing capabilities for patients (0.5%) or HCPs (6%).
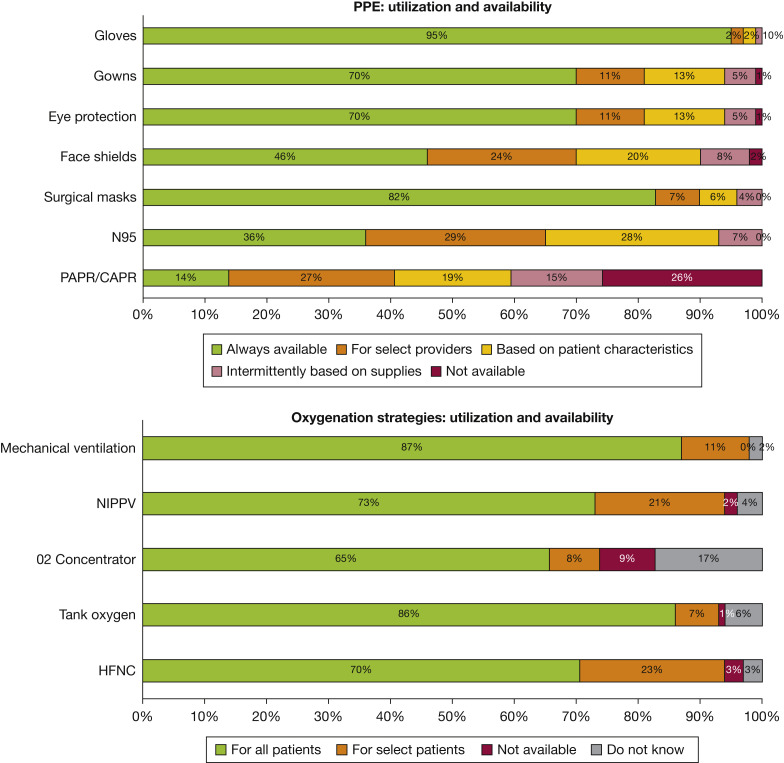
Personal Protective Equipment
Surgical masks and gloves were reported to be always available according to 95% and 83% of respondents, respectively. Other personal protective equipment (PPE) was generally restricted to select HCPs or HCPs caring for patients with certain characteristics (Fig 2 A): N95 masks (35% available for all HCPs, 57% restricted), dedicated eye protection (50% and 40%), and face shields (46% and 44%). The largest shortage was reported for powered air-purifying respirators (PAPRs; 14% available for all and 48% restricted), with 26% of respondents reporting a complete lack of PAPRs in their hospital (least in North America at 12%). One in four respondents (23%) thought that their hospital’s policy on PPE was not appropriate or safe (e-Table 4); in univariate regressions, this sentiment was significantly higher among nurses (48%), RTs (27%), APPs (19%), and physicians in training (21%) compared with attending physicians (7%) (e-Table 5) and was higher in North America (27%) than in other regions. P < .05 (P values are different but always statistically significant for each subspecialty compared to attending physicians).
Figure 2.
ICU resource use and availability of personal protective equipment (A), oxygenation strategies (B), and medical tests and procedures (C) in patients with coronavirus disease 2019. Not all percentages across all rows total 100% because of rounding. CAPR = controlled air-purifying respirator; HFNC = high-flow nasal cannula; NIPPV = noninvasive positive pressure ventilation; PAPR = powered air-purifying respirator.
Ventilators and Oxygenation Therapies
Limited availability (ie, only for select patients) was reported for MV (11%) (Fig 1E), noninvasive positive pressure ventilation (21%), and high-flow nasal cannula (23%) (Fig 2B). The percentage of respondents reporting limited ventilator availability varied across regions and was lowest in North America (7%) compared with sub-Saharan Africa (43%), the Middle East and North Africa (34%), and Europe and Central Asia (17%). No respondent reported a complete lack of ventilators, and only 1% reported simultaneously using the same ventilator for multiple patients.
Diagnostics
Tests and procedures for patients critically ill with COVID-19 were frequently restricted, with a substantial proportion of respondents reporting limiting the use of bronchoscopy (54%), CT scanning (60%), echocardiography (47%), MRI (44%), ultrasonography (41%), lumbar puncture (40%), and paracentesis (39%) to select patients. Approximately one-quarter of respondents reported not performing bronchoscopy (22%) or MRI (25%) despite availability to do so (Fig 2C).
Limiting the Use of MV in Patients With COVID-19
One in six (16%) respondents reported limiting the use of MV in patients with COVID-19 on the basis of clinical severity (54%), comorbidities (42%), age (29%), or health insurance or financial means (3%). In the multivariate regression, the likelihood of limiting MV was two to three times higher in all other world regions than in North America (Table 3 ), highest in settings where a lack of ventilators was reported (absolute risk reduction [ARR], 2.10; 95% CI, 1.61-2.74), and marginally associated with lack of PAPRs and caring for > 50 patients with COVID-19. Shortages of intensivists, nurses, and ICU beds were univariately associated with limiting MV, but these associations disappeared (ARR close to 1) after adjustment for other covariates.
Table 3.
Univariate and Multivariate Predictors of Limiting Mechanical Ventilation and Changes in CPR Policy
| Characteristic | RR (95% CI) | P Value | ARR (95% CI) | P Value |
|---|---|---|---|---|
| Mechanical ventilation limited in patients with COVID-19 | ||||
| Region | ||||
| North America | Ref | Ref | ||
| East Asia and Pacific | 1.58 (1.07-2.33) | .02 | 2.25 (1.05-4.85) | .04 |
| Europe and Central Asia | 3.17 (2.53-3.98) | < .001 | 2.95 (2.30-3.79) | < .001 |
| Latin America and the Caribbean | 2.09 (0.98-4.45) | .06 | 1.83 (0.76-4.41) | .17 |
| Middle East and North Africa | 3.38 (1.91-5.96) | < .001 | 2.93 (1.15-7.46) | .02 |
| South Asia | 3.55 (1.66-7.57) | < .001 | 4.20 (1.52-11.6) | .01 |
| Sub-Saharan Africa | 2.89 (0.72-11.7) | .14 | 2.90 (0.61-13.8) | .18 |
| Reported lack of stuff, staff, and space | ||||
| Limited availability of PAPRs | 1.62 (1.12-2.32) | .01 | 1.49 (0.98-2.27) | .06 |
| Limited ventilator availability | 2.99 (2.39-3.74) | < .001 | 2.10 (1.61-2.74) | < .001 |
| Lack of intensivists | 1.99 (1.58-2.52) | < .001 | 1.11 (0.83-1.50) | .47 |
| Lack of nurses | 1.78 (1.45-2.19) | < .001 | 1.07 (0.82-1.39) | .62 |
| Lack of ICU beds | 2.02 (1.56-2.61) | < .001 | 1.21 (0.88-1.65) | .24 |
| No. of patients with COVID-19cared for | ||||
| < 10 | Ref | Ref | ||
| 10-50 | 1.16 (0.92-1.46) | .2 | 1.03 (0.78-1.35) | .19 |
| > 50 | 1.73 (1.28-2.35) | < .001 | 1.40 (0.98-1.99) | .06 |
| COVID-19 severity indexa | ||||
| Less severe | Ref | Ref | ||
| Most severe | 0.78 (0.60-1.02) | .07 | 1.34 (0.69-2.58) | .38 |
| CPR and DNR policies and practices changed since COVID-19 | ||||
| Region | ||||
| North America | Ref | Ref | ||
| East Asia and Pacific | 1.04 (0.87-1.24) | .68 | 1.23 (0.82-1.85) | .32 |
| Europe and Central Asia | 0.87 (0.77-0.99) | .04 | 0.86 (0.76-0.99) | .03 |
| Latin America and the Caribbean | 0.95 (0.63-1.46) | .83 | 1.04 (0.65-1.66) | .87 |
| Middle East and North Africa | 0.87 (0.58-1.32) | .51 | 1.02 (0.57-1.82) | .96 |
| South Asia | 1.03 (0.61-1.75) | .9 | 1.04 (0.59-1.80) | .9 |
| Sub-Saharan Africa | 1.05 (0.44-2.54) | .91 | 1.23 (0.47-3.19) | .67 |
| Reported lack of stuff, staff, and space | ||||
| Limited availability of PAPRs | 1.14 (0.98-1.34) | .09 | 1.12 (0.96-1.31) | .16 |
| Limited ventilator availability | 1.04 (0.89-1.21) | .61 | … | |
| Lack of intensivists | 1.09 (0.95-1.25) | .22 | … | |
| Lack of nurses | 1.11 (0.99-1.23) | .06 | 0.89 (0.80-1.00) | .05 |
| Lack of ICU beds | 1.12 (0.96-1.30) | .14 | … | |
| No. of patients with COVID-19 cared for | ||||
| < 10 | Ref | Ref | ||
| 10-50 | 1.03 (0.92-1.15) | .61 | … | |
| > 50 | 1.08 (0.91-1.27) | .4 | … | |
| COVID-19 severity indexa | ||||
| Less severe | Ref | Ref | ||
| Most severe | 1.02 (0.88-1.17) | .83 | 1.19 (0.82-1.72) | .37 |
The severity index indicates daily deaths by population during the time of survey administration. Physicians in training include residents and fellows. Time from peak (mortality) was not associated with outcomes in univariate or multivariate regressions (data not shown). Variables not statistically associated with the outcomes in univariate regression or whose inclusion did not improve model fit were not included in the multivariate regression. No. of observations for multivariate regressions: mechanical ventilation limited (n = 2,231), CPR and DNR policies and practices changed since COVID-19 (n = 2,230), emotional distress and burnout (n = 2,477). ARR = absolute risk reduction; DNR = do not resuscitate; Ref = reference; RR = relative risk. See Tables 1 and 2 legends for expansion of other abbreviations.
Changes in CPR Practices, Shared Decision-making, and Palliative Care
Changes in CPR practices because of COVID-19 were reported by 66% of respondents, with 38% reporting implementation of a new policy. In multivariate analyses, changes in CPR policy and practices were significantly lower in Europe and Central Asia than in North America (ARR, 0.86; 95% CI, 0.76-0.99) and were not associated with shortage of staff, ICU beds, or resources (Table 3).
The percentage of respondents who reported not performing CPR at all in patients with COVID-19 varied by region (from 1% in North America to 57% in sub-Saharan Africa). A number of factors were considered when deciding prospectively whether to perform CPR, including clinical severity (66% of respondents), comorbidities (31%), and patient age (18%). Among those who did perform CPR, respondents were split in their practices whether to base the decision on family or surrogate wishes vs physician determination. North America was the only region in which most respondents (67%) performed CPR on the basis of family or surrogate wishes; in all other regions, most respondents stated that this decision was made by the treating physicians (100% in sub-Saharan Africa, 88% in South Asia, 75% in Latin America and the Caribbean, and 74% in Europe and Central Asia).
When critical decisions had to be made regarding withholding or withdrawing life-sustaining treatments, 16% of respondents allowed families less participation in decision-making for patients with COVID-19 than for other patients in the ICU: 11% in North America and East Asia and Pacific compared with 22% in Europe and Central Asia and 27% in Latin America and the Caribbean. One-half of respondents (48%) reported consulting palliative care specialists for patients with COVID-19 in the ICU, with the highest proportion in North America (61%). In contrast, not consulting palliative care specialists for patients critically ill with COVID-19 despite availability of palliative care was reported by 50% of respondents from Europe and Central Asia vs 8% from North America. Overall, 39% thought that palliative care consultations had increased during the pandemic (45% in North America vs 18% in Europe and Central Asia).
Provider Concerns
The most common concerns among HCPs included transmitting infection to their families (61%), emotional distress and burnout (52%), concerns about their own health (44%), and experiencing social stigma from their communities (21%). All HCPs’ concerns were highest in North America. A substantial minority (11%) expressed worries about their financial situation, most commonly in Latin America and the Caribbean (24%) and South Asia (22%). Most HCPs (65%) stated that caring for patients with COVID-19 was mandatory at their institution. When not in the hospital, 12% of HCPs reported relocating to a separate residence from their families to protect them, and an additional 53% reported taking extra precautions while at home (e-Table 4).
In multivariate regression, emotional distress and burnout were significantly associated with being female (ARR, 1.16; 95% CI, 1.01-1.33) and being a nurse (ARR, 1.31; 95% CI, 1.13-1.53) (Table 4 ). Compared with providers who had cared for < 10 patients with COVID-19, those who had cared for 10 to 50 and > 50 patients had a 17% and 28% higher risk of burnout, respectively. Pandemic severity or time from peak within a respondent’s country was not associated with burnout. Providers experiencing poor communication from their supervisors had a 30% higher likelihood of reporting burnout (95% CI, 1.16-1.46). Limited availability of PAPRs and shortages of nurses were associated with a 30% and 18% increased risk of burnout, respectively. Providers in Europe and Central Asia were 14% less likely to report burnout than were providers in North America (95% CI, 0.75-1.00).
Table 4.
Univariate and Multivariate Predictors of Emotional Distress and Burnout
| Emotional Distress and Burnout Predictor Characteristic | RR (95% CI) | P Value | ARR (95% CI) | P Value |
|---|---|---|---|---|
| Sex | ||||
| Male | Ref | Ref | ||
| Female | 1.36 (1.21-1.53) | <.001 | 1.16 (1.01-1.33) | .03 |
| Region | ||||
| North America | Ref | Ref | ||
| East Asia and Pacific | 0.52 (0.41-0.66) | < .001 | 0.85 (0.52-1.37) | .5 |
| Europe and Central Asia | 0.84 (0.74-0.96) | .01 | 0.86 (0.75-1.00) | .04 |
| Latin America and the Caribbean | 0.71 (0.45-1.13) | .15 | 1.07 (0.63-1.80) | .8 |
| Middle East and North Africa | 0.78 (0.51-1.19) | .25 | 1.15 (0.63-2.09) | .65 |
| South Asia | 0.56 (0.28-1.11) | .1 | 0.84 (0.37-1.90) | .68 |
| Sub-Saharan Africa | 0.58 (0.19-1.80) | .34 | 0.89 (0.26-2.98) | .85 |
| Provider type | ||||
| Attending physicians | Ref | Ref | ||
| Physicians in training | 0.97 (0.77-1.23) | .82 | 0.90 (0.71-1.15) | .41 |
| Nurses | 1.45 (1.28-1.65) | < .001 | 1.31 (1.13-1.53) | .01 |
| APPs | 1.30 (1.06-1.60) | .01 | 1.11 (0.89-1.39) | .35 |
| RTs | 1.29 (1.07-1.55) | .01 | 1.14 (0.93-1.40) | .2 |
| Poor communication from my supervisors | 1.85 (1.66-2.07) | < .001 | 1.30 (1.16-1.46) | < .001 |
| Reported lack of stuff, staff, and space | ||||
| Limited availability of PAPRs | 1.36 (1.15-1.62) | < .001 | 1.30 (1.09-1.55) | < .001 |
| Limited ventilator availability | 1.16 (1.00-1.35) | .04 | 1.03 (0.88-1.20) | .71 |
| Lack of intensivists | 1.14 (0.99-1.31) | .06 | … | … |
| Lack of nurses | 1.34 (1.21-1.50) | < .001 | 1.18 (1.05-1.33) | .01 |
| Lack of ICU beds | 1.19 (1.02-1.37) | .02 | … | … |
| No. of patients with COVID-19 cared for | ||||
| < 10 | Ref | Ref | ||
| 10-50 | 1.33 (1.18-1.49) | < .001 | 1.17 (1.04-1.33) | .01 |
| > 50 | 1.41 (1.19-1.68) | < .001 | 1.28 (1.06-1.53) | .01 |
| COVID-19 severity indexa | ||||
| Less severe | Ref | Ref | ||
| Most severe | 1.73 (1.45-2.07) | < .001 | 1.22 (0.80-1.85) | .35 |
The severity index indicates daily deaths by population during the time of survey administration. Physicians in training include residents and fellows. Time from peak (mortality) was not associated with outcomes in univariate or multivariate regressions (data not shown). Variables not statistically associated with the outcomes in univariate regression or whose inclusion did not improve model fit were not included in the multivariate regression. No. of observations for multivariate regressions: mechanical ventilation limited (n = 2,231), CPR and DNR policies and practices changed since COVID-19 (n = 2,230), emotional distress and burnout (n = 2,477). See Tables 1 and 3 legends for expansion of abbreviations.
Discussion
In this global survey of ICU providers during the COVID-19 pandemic, shortages of ICU staff and resources were reported frequently, as were emotional distress and burnout. Participants reported that the pandemic had changed practices concerning MV and CPR, in part based on resource availability. In addition, more than one-half of the respondents reported concerns about their own health and their families’ health. Finally, our results highlight substantial variation across regions. For example, providers in North America reported higher levels of emotional distress or burnout, despite reporting fewer shortages of resources, and were also more likely to base CPR and other critical decisions on family wishes compared with findings in other world regions. Our results, which underscore the psychological burden on HCPs, complement results in recent reports about provider well-being from China, Italy, and the United States during the pandemic,18, 19, 20, 21, 22 as well as results from studies before the pandemic (3%-50% burnout rates across various types of ICU providers).23, 24, 25, 26
We found modifiable and nonmodifiable predictors of burnout that may inform targeted interventions to improve provider experiences and protect their mental well-being. First, across all regions, female HCPs and nurses were more likely to experience burnout. Second, provider burnout was independently associated with having cared for a larger number of patients with COVID-19. However, we did not find an association between pandemic severity and burnout. This finding likely indicates that the number of patients with COVID-19 an individual has cared for is a more reliable predictor of this individual’s experiences than is the number of patients with COVID-19 in a given region. Finally, burnout was associated with reporting a shortage of ICU nurses, insufficient PAPR availability, and poor communication from supervisors. A recently published survey of 9,120 ICU clinicians from the United States showed that the perceived need for both PPE masks and ICU staffing shortages exceeded all other resource challenges.22 Further analysis of our data showed that insufficient access to PPE was the strongest predictor of all provider concerns in the United States (data not shown). Communication in the COVID-19 era poses a major challenge, given the need constantly to adapt and implement new policies while remaining transparent to all affected HCPs.
Strengths of this study include its large sample size consisting of interprofessional HCPs at the front line of the pandemic in 77 countries. Furthermore, it was conducted during a time when many countries were severely affected by COVID-19, and we were able to capture the highest number of responses in many of the most affected countries (on the basis of case numbers, mortality, and case fatality rates). To our knowledge, this is the first global survey to assess of the pandemic’s effect comprehensively regarding ICU resources, practices, and provider well-being.
Several limitations need to be considered. First, the lack of a clearly defined sample introduces a substantial risk of response and sampling bias. We specifically targeted our distribution strategy to reach HCPs working in ICUs, but our convenience sampling approach may have limited the generalizability of our results. Also, because the survey was anonymous, we cannot exclude the possibility that respondents took the survey more than once. Second, most respondents were from North America and Europe and Central Asia, with low representation from low- and middle-income countries (LMIC). Future studies will need to target LMIC specifically to assess COVID-19’s effects in the context of resource-constrained health systems. Third, our survey was available only in English, and language barriers might have resulted in inaccurate responses and contributed to low numbers of participants in some countries. In addition, responses reflect the views of individual respondents but may not be representative of all HCPs in any given country, particularly in countries with few participants. Fourth, respondents were mostly from large urban centers, which are likely to have more resources than rural hospitals have. However, these regions were also hardest hit in the COVID-19 pandemic. Fifth, reported practices during COVID-19 are rapidly changing as ICUs and HCPs continue to adjust to the burden imposed by the pandemic, so responses might differ within the 15-day window in which the survey was distributed. Also, practices captured in this survey were perceived by the respondents rather than reflecting actual practices. Sixth, changes in CPR practices might not purely reflect ICU resource use but rather represent measures to ensure the safety of HCPs. Finally, practice differences within regions, such as involving families in decision-making or limiting life-sustaining therapy, likely reflect cultural and medicolegal differences rather than a differential effect of the pandemic.26
Our findings suggest an important need to create collaborative strategies for ventilatory support in resource-limited settings, in particular in anticipation of surges affecting LMIC,27 as well as repeated surges in countries currently relaxing their strict measures to mitigate spread. Finally, our study emphasizes the personal sacrifices by HCPs, especially nurses, on the front lines worldwide and the need to support them proactively by implementing interventions to promote mental health and well-being.
Interpretation
COVID-19 has significantly affected ICU practices, resources, and staff. Across all regions, the reported lack of ICU nurses was higher than that of intensivists, and the use of standard diagnostic tests has been largely limited in patients with COVID-19.
High rates of provider emotional distress and burnout are reported across geographic regions. Providers in North America report the highest levels of emotional distress or burnout, despite reporting fewer shortages of resources, and they were also more likely to base CPR and other critical decisions on family wishes compared with findings in other world regions.
MV was largely limited based on restricted ventilator availability. Strategies for allocating ventilatory support will be important in light of anticipated surges in developing countries. Female HCPs; nurses; and those reporting lack of ICU nurses, PAPRs, and poor communication were at highest risk for burnout. Targeted interventions to support HCPs by addressing modifiable risk factors, such as insufficient access to PPE and poor communication, are needed.
Acknowledgments
Author contributions: On behalf of all authors, the corresponding author affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained. S. W., M. S., P. V. P., and C. J. C. had full access to all of the data and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors contributed substantially to the study design, data acquisition and analysis, and interpretation. M. S. and N. J. K. performed the statistical analysis. S. W. and C. J. C. wrote the manuscript, and all authors edited the manuscript.
Financial/nonfinancial disclosures: None declared.
Role ofsponsors: The sponsor had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript.
Other contributions: We thank all of our colleagues around the world who have taken the time to participate in our survey while being very busy caring for patients in the ICU. We thank the following societies and groups for collaborating in distributing the surveys to their memberships and supporting our study: World Federation of Intensive and Critical Care (Janice Zimmerman, Ignacio Martin-Loeches, and Phil Taylor), American Association of Critical Care Nurses, Australian & New Zealand Intensive Care Society, American Thoracic Society, British Association of Critical Care Nurses, Bangladesh Society of Critical Care Medicine, Cambia Health Foundation, Canadian Critical Care Society, Deutsche Interdisziplinäre Vereinigung für Intensiv- und Notfallmedizin, European Society of Intensive Care Medicine (Ethics section), Russian Federation of Anesthesiologists and Reanimatologists, Global Sepsis Alliance, Japanese Society of Intensive Care Medicine, Neurocritical Care Society, Prevention and Early Treatment of Acute Lung Injury, Società Italiana di Anestesia Analgesia Rianimazione e Terapia Intensiva (especially Ilenia Rossini), La Sociedad Española de Medicina Intensiva Crítica y Unidades Coronarias, and Thai Society of Critical Care Medicine. We would also like to acknowledge the following colleagues for their input and support in reviewing, testing, and distributing our survey: Edilberto Amorim, MD (UCSF, San Francisco, CA); Ayush Batra, MD (Northwestern University, Chicago, IL); Denise Batura, RN (University of Washington, Seattle, WA); Molly Bjierstrom, RN (University of Washington, Seattle, WA); Xuemei Cai, MD (Tufts University, Boston. MA); Guadalupe Castillo-Abrego, MD (Pacifica Salud Hospital, Panama City, Panama); Maria Chumbe, MD (Instituto Nacional Ciencias Neurologicas, Lima, Peru); Hanna Demissie, MD (Tikkur Anbessa Hospital, University of Addis Ababa, Addis Ababa, Ethiopia); Cedric P. Van Dijck, MD (University of Washington, Seattle, WA); Robb Glenny, MD (University of Washington); Justin Granstein, MD (Mount Sinai, New York, NY); Roop Gursahani, MD (Hinduja hospital, Mumbai, India); Saef Izzy, MD (Brigham and Women's Hospital, Boston, MA); Nicholas Johnson, MD (University of Washington, Seattle, WA); Niru Kaur, RT (University of Washington, Seattle, WA); Minjee Kim, MD (Northwestern University, Chicago, IL); Mikhail Kirov, MD (Northern State Medical University, Arkhangelsk, Russia); Joshua Krieger, MD (University of Washington, Seattle, WA); Karen March, RN, CNRN, CNS; Klaus T. Meinhof, MD (Bangor, ME); Grace Mellor, RN (University of Washington, Seattle, WA); Rocio Mendivil, MD (Quironsalud del Valles, Barcelona, Spain); Rajen Nathwani, MD (University of Washington, Seattle, WA); Paolo Navalesi, MD (SIAARTI, Italy); Soojin Park, MD (Columbia University, New York, NY); Flavia Petrini, MD (SIAARTI, Italy); Alireza Ranjbar, MD (University of Bonn, Bonn, Germany); Anthony Roche, MD (University of Washington, Seattle, WA); Kelsey Rock, P.A. (University of Washington, Seattle, WA); Katerina Rusinova, MD (Charles University Prague, Czech Republic); Seynab Sangsari, MD (Homburg/Saar, Germany); Stefan J Schaller, MD (Charité, Universitätsmedizin Berlin, Germany); Roseate Scott, RT (University of Washington, Seattle, WA); Amanda Severson, A.R.N.P. (University of Washington, Seattle, WA); Deepak Sharma, MD (University of Washington, Seattle, WA); Christopher Teegardin, RT (University of Washington, Seattle, WA); Ludo Vanopdenbosch, MD (AZ Sint-Jan, Brugge, Belgium); Craig Williamson (University of Michigan, MI); Thilo Witsch, MD (Universitätsklinik Freiburg, Freiburg, Germany); Sahar Zafar, MD (Massachusetts General Hospital, Boston, MA). We would also like to thank Dr Kathryn Peebles (University of Washington) for her advice on the statistical analysis, and all members of the Women in Neurocritical Care Whatsapp group for advice and support.
Additional information: The e-Appendix, e-Figures, and e-Tables can be found in the Supplemental Materials section of the online article.
Footnotes
FUNDING/SUPPORT: The authors received no direct funding for this work. M. S. received support from National Institute of Mental Health [Grant K01MH115789]. C. S. H. reports current funding by the Federal Joint Committee Innovation Fund [Grant FKZ 01VSF17010]. C. J. C. is supported by National Institute of Neurological Disorders and Stroke [Grant NS099421].
Supplementary Data
References
- 1.WHO coronavirus disease (COVID-19) dashboard. https://covid19.who.int/
- 2.Johns Hopkins University & Medicine Coronavirus resource center. https://coronavirus.jhu.edu/
- 3.Guan W.J., Ni Z.Y., Hu Y., et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang C., Wang Y., Li X., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet Lond Engl. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Richardson S., Hirsch J.S., Narasimhan M., et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhatraju P.K., Ghassemieh B.J., Nichols M., et al. Covid-19 in critically ill patients in the Seattle region: case series. N Engl J Med. 2020;382(21):2012–2022. doi: 10.1056/NEJMoa2004500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grasselli G., Zangrillo A., Zanella A., et al. COVID-19 Lombardy ICU Network. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020;323(16):1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang X., Yu Y., Xu J., et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Christian M.D., Devereaux A.V., Dichter J.R., Geiling J.A., Rubinson L. Definitive care for the critically ill during a disaster: current capabilities and limitations—from a Task Force for Mass Critical Care summit meeting, January 26-27, 2007, Chicago, IL. Chest. 2008;133(5 suppl):8S–17S. doi: 10.1378/chest.07-2707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.von Elm E., Altman D.G., Egger M., et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet Lond Engl. 2007;370(9596):1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 11.University of Washington Institute of Translational Health Sciences Citation information. https://www.iths.org/investigators/forms-templates/citation-information/
- 12.Institute for Health Metrics and Evaluation COVID-19 projections. https://covid19.healthdata.org/
- 13.GitHub CSSEGISandData/COVID-19. https://github.com/CSSEGISandData/COVID-19
- 14.United Nations Department of Economic and Social Affairs Population dynamics: world population prospects 2019. https://population.un.org/wpp/Download/Standard/Population/
- 15.R Core Team R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2019. https://www.R-project.org/
- 16.Rich B. Table 1: tables of descriptive statistics in HTML. https://CRAN.R-project.org/package=table1
- 17.Venables W.N., Ripley B.D. 4th ed. Springer-Verlag; New York, NY: 2002. Modern Applied Statistics With S. [Google Scholar]
- 18.Rossi R., Socci V., Pacitti F., et al. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Netw Open. 2020;3(5) doi: 10.1001/jamanetworkopen.2020.10185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lai J., Ma S., Wang Y., et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kaplan L.J., Kleinpell R., Maves R.C., Doersam J.K., Raman R., Ferraro D.M. Critical care clinician reports on coronavirus disease 2019: results from a national survey of 4,875 ICU providers. Crit Care Explor. 2020;2(5) doi: 10.1097/CCE.0000000000000125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Society of Critical Care Medicine Clinicians report high stress in COVID-19 response. https://sccm.org/Blog/May-2020/SCCM-COVID-19-Rapid-Cycle-Survey-2-Report
- 22.Kleinpell R., Ferraro D.M., Maves R.C., et al. Coronavirus disease 2019 pandemic measures: reports from a national survey of 9,120 ICU clinicians. Crit Care Med. 2020;48(10):e846–e855. doi: 10.1097/CCM.0000000000004521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cañadas-de la Fuente G.A., Albendín-García L., Cañadas G.R., San Luis-Costas C., Ortega-Campos E., de la Fuente-Solana E.I. Nurse burnout in critical care units and emergency departments: intensity and associated factors. Emergencias. 2018;30(5):328–331. [PubMed] [Google Scholar]
- 24.Poncet M.C., Toullic P., Papazian L., et al. Burnout syndrome in critical care nursing staff. Am J Respir Crit Care Med. 2007;175(7):698–704. doi: 10.1164/rccm.200606-806OC. [DOI] [PubMed] [Google Scholar]
- 25.Vermeir P., Blot S., Degroote S., et al. Communication satisfaction and job satisfaction among critical care nurses and their impact on burnout and intention to leave: a questionnaire study. Intensive Crit Care Nurs. 2018;48:21–27. doi: 10.1016/j.iccn.2018.07.001. [DOI] [PubMed] [Google Scholar]
- 26.Sprung C.L., Ricou B., Hartog C.S., et al. Changes in end-of-life practices in European intensive care units from 1999 to 2016. JAMA. 2019;322(17):1–12. doi: 10.1001/jama.2019.14608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hopman J., Allegranzi B., Mehtar S. Managing COVID-19 in low- and middle-income countries. JAMA. 2020;323(16):1549–1550. doi: 10.1001/jama.2020.4169. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.