Abstract
Background:
A large number of systematic reviews and meta-analyses regarding the meniscus have been published.
Purpose:
To provide a qualitative summary of the published systematic reviews and meta-analyses regarding the meniscus.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A systematic search of all meta-analyses and systematic reviews regarding the meniscus and published between July 2009 and July 2019 was performed with PubMed, CINAHL, EMBASE, and the Cochrane database. Published abstracts, narrative reviews, articles not written in English, commentaries, study protocols, and topics that were not focused on the meniscus were excluded. The most pertinent results were extracted and summarized from each study.
Results:
A total of 332 articles were found, of which 142 were included. Included articles were summarized and divided into 16 topics: epidemiology, diagnosis, histology, biomechanics, comorbid pathology, animal models, arthroscopic partial meniscectomy (APM), meniscal repair, meniscal root repairs, meniscal allograft transplantation (MAT), meniscal implants and scaffolds, mesenchymal stem cells and growth factors, postoperative rehabilitation, postoperative imaging assessment, patient-reported outcome measures, and cost-effectiveness. The majority of articles focused on APM (20%), MAT (18%), and meniscal repair (17%).
Conclusion:
This summary of systematic reviews and meta-analyses delivers surgeons a single source of the current evidence regarding the meniscus.
Keywords: meniscus, surgery, systematic review, meta-analysis
Staying current with the increasing number of systematic reviews and meta-analyses on the topic of the meniscus can be quite challenging. Systematic reviews and meta-analyses are designed to provide an up-to-date summary of the available evidence on a particular condition for busy clinicians, and systematic summaries of systematic reviews and meta-analyses are being conducted to further condense this large body of evidence.5,62 A simple PubMed search for meniscus yielded 869 items in 2018 alone. To assist clinicians and researchers with staying abreast of this topic, we summarized the literature pertaining to topics related to the meniscus. The purpose of this study was to quantify the number of systematic reviews and meta-analyses published on the meniscus in the past decade and to provide a condensed summary of the literature for easy reference.
Methods
To identify all systematic reviews and meta-analyses pertaining to the meniscus, we performed a literature search of articles published in English between July 2009 and July 2019. We searched PubMed, CINAHL, EMBASE, and the Cochrane database. The search terms were (“meniscus” OR “meniscal”) AND (“systematic review” OR “meta-analysis”). All systematic reviews and meta-analyses that focused on research topics pertaining to the meniscus (eg, epidemiology, diagnosis, treatment) were included. We excluded published abstracts, narrative reviews, articles not written in English, commentaries, study protocols, and topics not centered on the meniscus. The results of the literature search were independently reviewed by 4 of the authors; 3 authors (J.B.S., J.R.M., A.V.V.) reviewed each study in detail and summarized the pertinent results. The articles were divided into the following 16 topics, and the major results were synthesized for each topic: epidemiology, diagnosis, histology, biomechanics, comorbid pathology, animal models, arthroscopic partial meniscectomy (APM), meniscal repair, meniscal root repairs, meniscal allograft transplantation (MAT), meniscal implants and scaffolds, mesenchymal stem cells and growth factors, postoperative rehabilitation, postoperative imaging asseessment, patient-reported outcome measures, and cost-effectiveness. Less than 5% of included papers were categorized under >1 topic because multiple study aims were evaluated.
Results
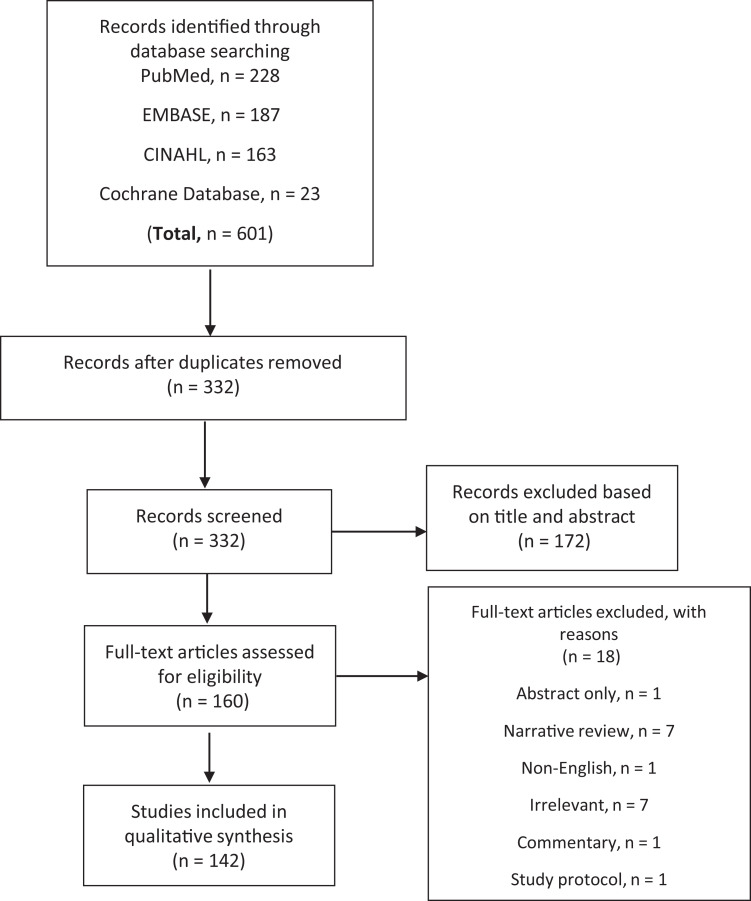
The PRISMA (Preferred Reporting Items for Systematic Meta-Analyses) flowchart for the literature search is presented in Figure 1. A total of 332 unique articles were obtained by the literature search, and of these, 142 met the inclusion criteria. The number of articles included for each meniscus-related topic is presented in Table 1.
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart.
Table 1.
Number of Articles by Topica
| Topic of Systematic Review | No. of Articles Retrieved |
|---|---|
| Epidemiology | 5 |
| Diagnosis | 15 |
| Histology | 1 |
| Biomechanics | 1 |
| Comorbid pathology | 15 |
| Animal models | 2 |
| Arthroscopic partial meniscectomy | 28 |
| Meniscal repair | 24 |
| Meniscal root repairs | 5 |
| Meniscal allograft transplantation | 26 |
| Meniscal implants and scaffolds | 15 |
| Mesenchymal stem cells and growth factors | 4 |
| Postoperative rehabilitation | 6 |
| Postoperative imaging assessment | 1 |
| Patient-reported outcome measures | 1 |
| Cost-effectiveness | 2 |
aTopics are not mutually exclusive.
Epidemiology
Culvenor et al26 found that the overall pooled prevalence of meniscal tears confirmed on magnetic resonance imaging (MRI) was 10% (95% CI, 7%-13%) in 3761 asymptomatic, uninjured knees and that meniscal tears were more prevalent in adults aged 40 and older (19%; 95% CI, 13%-26%) compared with adults younger than 40 years (4%; 95% CI, 2%-7%). Liu et al83 found that the prevalence of bilateral discoid lateral meniscal tears in patients with symptomatic discoid lateral meniscal tears ranged from 6% to 97% in 8 studies, and bilateral discoid meniscal tears were most prevalent in East Asia and among male patients. A meta-analysis by Snoeker et al129 identified several risk factors for degenerative meniscal tears, including increased age, male sex, work-related kneeling and squatting, standing or walking >2 hours per day, walking >2 miles per day, climbing > 30 flights of stairs per day, and lifting or carrying >10 kg >10 times per week. There was also some evidence suggesting that body mass index (BMI) >25 kg/m2 is a risk factor for degenerative tears, although too much heterogeneity between studies precluded the authors from conducting a meta-analysis. Sitting for >2 hours per day was actually shown to protect against degenerative tears. Risk factors for acute meniscal tears included playing soccer, rugby, and swimming; further, delayed anterior cruciate ligament (ACL) surgery (>12 months) was a risk factor for meniscal tears associated with knee laxity. Reid et al111 found that meniscal tears were one of the most common work-related knee disorders, and common risk factors for meniscal tears included kneeling, squatting or crouching, crawling, stair or ladder climbing, lifting/carrying/moving, standing up from a kneel, and sitting while driving.
Beals et al12 systematically reviewed 14 studies and found that 27% of asymptomatic athletes (recreational and high level) had intrasubstance pathology on MRI, of which 3.9% had meniscal tears. Meniscal tears were more prevalent in athletes participating in nonpivoting sports (5.4%) compared with pivoting sports (2.5%). Cramer et al25 found that yoga practitioners had increased odds of meniscal injury compared with non–yoga practitioners (odds ratio [OR], 1.72; 95% CI, 1.23-2.41); however, theirs was the only study to have documented this finding.
Diagnosis
Clinical Examination
Brady and Weiss18 systematically reviewed 5 studies and concluded that clinical examination was moderately accurate for diagnosing medial (sensitivity, range 85%-94%; specificity, range 56%-75%) and lateral (sensitivity, range 66%-99%; specificity, range 66%-99%) meniscal tears compared with MRI. Hing et al57 concluded that (1) the McMurray test had high specificity but low sensitivity and (2) the modified McMurray test may be more accurate than the traditional McMurray test, although the studies included in their review were of low methodological quality. Several systematic reviews found that the McMurray test, joint line tenderness, and the Thessaly test were poor indicators of meniscal tears, suggesting that these tests should not be used on their own for diagnostic purposes.17,31,32,124 Both interrater reliability and sensitivity were low to moderate for the McMurray test (κ, range 0.16-0.38; sensitivity, range 61%-70.5%),31,32,124 Thessaly test (κ, range 0.37-0.72; pooled sensitivity, 75% [95% CI, 53%-89%]),31,124 and joint line tenderness (κ, range 0.11-0.25; sensitivity, range 44%-83%).17,31,32,124
Imaging
Phelan et al107 conducted a meta-analysis of 19 studies and determined that MRI was accurate for diagnosing both medial (sensitivity, 89% [95% CI, 77%-94%]; specificity, 88% [95% CI, 82%-93%]) and lateral (sensitivity, 78% [95% CI, 66%-87%]; specificity, 95% [95% CI, 91%-97%]) meniscal tears. Several systematic reviews have found no difference in diagnostic accuracy between 1.0-T, 1.5-T, and 3.0-T MRI.20,109,125 Shakoor et al121 found that 3-dimensional (3D) fast spin-echo and 3D gradient-echo MRI sequences had similar diagnostic accuracy in detecting meniscal tears compared with 2-dimensional MRI sequences, but sensitivity of 3D fast spin-echo was slightly better than 3D gradient-echo sequences for detecting lateral meniscal tears. Troupis et al135 concluded that localized synovitis and displacement of the meniscus on MRI scans may be predictive of patients who could benefit from meniscal intervention. A further 3 meta-analyses27,35,142 found good to moderate pooled sensitivity (78%-89%) and specificity (84%-90%) for ultrasound in diagnosing meniscal tears with arthroscopy as the reference standard, although Dai et al27 noted considerable heterogeneity between studies.
Histology
We found only 1 systematic review, that by Longo et al,84 which examined the histological scoring systems used to assess meniscal tissue. The Copenhaver classification can be used to identify degeneration of collagen bundles in the meniscus, and the Mankin score can be used to classify cartilage structure but only at the microscopic level. The Pauli score is reproducible and can be used to evaluate macroscopic and histologic meniscal changes related to aging and degenerative changes. The Zhang score can be used to assess meniscal healing, and the Ishida score is the most accurate for evaluating tissue-engineered meniscal repairs. Several histological scoring systems are available for assessing the meniscal structure, but few have been validated.
Biomechanics
Scholes et al119 systematically reviewed 12 studies and found that the lateral meniscus translates more posteriorly than the medial meniscus during flexion and that meniscal translation is affected by loading and not by ACL deficiency. However, the included studies were of low methodological quality.
Comorbid Pathology
ACL Ruptures
Noyes and Barber-Westin99 found that meniscal tears were commonly observed during ACL reconstruction, and most were treated with APM (63% medial APM; 71% lateral APM). However, based on the available literature, the authors were unable to examine potential predictors of meniscal treatment including characteristics of meniscal tear (ie, size, location, type, chronicity) and the sex and age of the patient. Mehl et al89 conducted a meta-analysis of 40 studies and concluded that medial meniscal tears were more common at least 6 months after ACL rupture. Sommerfeldt et al130 found that recurrent instability episodes were associated with increased medial meniscal injury after first-time ACL injury in 6 of 7 studies in their review, emphasizing the importance of early diagnosis and treatment of ACL ruptures associated with instability.
Rothermich et al115 systematically reviewed 8 studies and found that clinical outcomes did not differ for stable meniscal tears treated with benign neglect compared with surgical treatment at the time of ACL reconstruction. Stable meniscal tears were defined as both longitudinal tears that were displaced <3 mm from the intact peripheral rim and radial tears that involved less than the inner one-third of the meniscus. Magnussen et al86 found that patients who underwent partial or complete meniscectomy at the time of ACL reconstruction were more likely to develop radiographic signs of osteoarthritis at 5 to 10 years postoperatively; however, the results for concomitant meniscal repair and later development of osteoarthritis were inconclusive. Kay et al69 conducted a meta-analysis of 9 studies and found that earlier ACL reconstruction was associated with decreased risk of concomitant medial meniscal tears in children and adolescents (pooled relative risk, 0.49; 95% CI, 0.36-0.65). However, the definitions of early (eg, <6 weeks, <1 year) and delayed (eg, >2 weeks, >1 year) ACL reconstruction varied considerably between studies. Sarraj et al118 found that the Knee injury and Osteoarthritis Outcome Score (KOOS) was better after ACL reconstruction plus concomitant APM compared with concomitant meniscal repair. Concomitant meniscal repair was associated with less anterior knee joint laxity and higher rates of reoperation than APM. Westermann et al141 conducted a meta-analysis of 21 studies and found higher failure rates for all-inside (16%) versus inside-out (10%) meniscal repairs performed concurrently with ACL reconstruction. Poulsen et al108 found increased odds of osteoarthritis 2 years after combined ACL and meniscal injury (OR, 6.4; 95% CI, 4.9-8.3). In their meta-analysis of 16 studies, Claes et al23 found that osteoarthritis was more prevalent after ACL reconstruction with APM (50%) compared with ACL reconstruction only (16%). Patients undergoing ACL reconstruction with APM were 3.54 times more likely to develop osteoarthritis than those having ACL reconstruction alone.
Knee Osteoarthritis
Karpinski et al68 found that arthroscopic treatment may improve clinical outcomes in patients with osteoarthritis and nontraumatic meniscal tears; however, there was much heterogeneity in what constituted arthroscopic treatment between studies. Based on a systematic review of 6 studies, Lamplot and Brophy73 found conflicting evidence regarding the efficacy of APM in patients with meniscal tears and degenerative changes. Some evidence was found suggesting that patients with mild osteoarthritis improve more than those with more advanced osteoarthritis; however, there was significant heterogeneity in the inclusion of different grades of osteoarthritis between studies. A consensus report concluded that there was no difference in pain or function for arthroscopic debridement with or without meniscectomy versus sham surgery or physical therapy in patients with knee osteoarthritis or degenerative meniscal tear.43
Bone Marrow Lesions
Lim et al82 found that meniscal derangement and extrusion were associated with ipsilateral compartment bone marrow lesions, which were likely due to increased susceptibility of the subchondral bone to trauma and loading.
Spontaneous Osteonecrosis of the Knee
Hussain et al60 found that 21 of 26 studies included in their systematic review had an association between meniscal injury or APM and the development of spontaneous osteonecrosis of the knee. Physicians should be especially aware of medial meniscal root tears that are associated with increased contact pressures because they may lead to insufficiency fractures and consequently to spontaneous osteonecrosis of the knee.
Animal Models
Bansal et al9 found that the majority of animal studies involving the meniscus focused on augmented repair (48%), most used rabbit models (46%), and the most frequently evaluated outcomes were macroscopic (85%), histologic (90%), and healing (83%). Edouard et al37 found that intra-articular hyaluronic acid injections improved the healing process after APM and protected the articular cartilage in animal models.
Arthroscopic Partial Meniscectomy
Efficacy of APM Versus Conservative Treatment
One review found no difference in pain or function when comparing the pooled results for (1) exercise therapy versus APM and (2) different types of exercise therapy for treating meniscal tears.132 However, conflicting evidence was found regarding the effectiveness of exercise therapy versus no exercise therapy after APM. Loras et al85 found 2 studies of degenerative meniscal tears, both of which demonstrated longer duration of pain relief after medical exercise therapy compared with APM or no treatment. The pooled results from 9 randomized controlled trials (RCTs) demonstrated no difference in pain or function after APM versus conservative management in patients older than 40 years, although arthroscopic technique varied between studies.77 Both Lee et al77 and Monk et al90 recommended that APM be performed only in patients with a degenerative meniscal tear for whom conservative management had failed. Petersen et al106 found no difference in outcomes between APM versus nonoperative management for meniscal tears, although patients who crossed over from physical therapy to APM had similar outcomes to patients who initially opted for APM. A meta-analysis of 7 RCTs found improvement in function, but not pain, up to 2 years after APM versus nonoperative treatment or sham surgery.70 The pooled results of 5 RCTs showed no difference in pain or function for APM versus nonoperative treatment or sham surgery for patients with degenerative meniscal tears.78 Abram et al1 conducted a meta-analysis of 20 studies and found (1) short-term improvement in pain, function, and quality of life after APM versus physical therapy, especially in patients without osteoarthritis; (2) improvement in pain and function at <6 months after APM versus intra-articular steroid injection but no improvement at 6- to 12-month follow-up; and (3) no difference in short-term outcomes after APM versus sham surgery.
We found 2 systematic reviews that evaluated study quality and risk of bias for RCTs and that examined the effectiveness of APM.58,87 Hohmann et al58 found insufficient evidence to conclude superiority of APM or physical therapy for treating degenerative meniscal tears, owing to high risk of bias and studies being moderate to low quality. Also, the study samples were small and there was heterogeneity in eligibility criteria, outcome measures, and physical therapy protocols. Malmivaara87 found that baseline characteristics, adherence to interventions, and treatment crossover were poorly reported in 7 RCTs. Furthermore, only 1 study used an outcome measure that was validated for meniscal tears, and the other 6 studies used outcome measures that were validated for osteoarthritis.
Postoperative Complications
A systematic review by Balato et al8 found that the incidence of septic arthritis after APM was approximately 0.12%. One study in the Balato et al review found no difference in the incidence of sepsis between patients who did and did not receive perioperative antibiotics, suggesting that perioperative antibiotics may not be beneficial; but further research is needed.14
Clinical Outcomes
Beaufils et al13 found good long-term outcomes after both medial and lateral APM; however, joint space narrowing was more common at an average of 13 years after lateral APM than medial APM (42% vs 21%, respectively). Mosich et al92 found unsatisfactory long-term outcomes (ie, pain, stiffness, range of motion, and osteoarthritis) in adolescents who underwent APM. Hall et al53 conducted a meta-analysis of 11 studies and concluded that knee extensor strength at baseline and postoperatively was reduced in middle-aged and older patients undergoing APM. Thorlund et al134 also found that patients younger than 30 years had reduced knee extensor strength up to 12 months after APM; however, only 6 studies were included in their systematic review and all were determined to be at high risk for bias. McLeod et al88 found that quadriceps weakness persists up to 4 years after APM. Lee et al79 found that patients returned to sport at approximately 7 to 9 weeks after APM; however, concurrent procedures (eg, ACL reconstruction) prolonged return to sport. Return to play was faster after meniscectomy versus meniscal repair in elite athletes (4.3 vs 7.6 months; P < .0001); however, National Football League players had a shorter career after meniscectomy compared with controls.39 Reoperation rates after APM were 1.4% in the short term and 3.9% in the long term according to a systematic review by Paxton et al,104 and lateral APM was associated with higher reoperation rates compared with medial APM. According to a review by Papalia et al,102 there is strong evidence to support the development of knee osteoarthritis after APM. Moreover, longer duration of symptoms and excision of degenerative menisci were predictive of knee osteoarthritis after APM.
Smuin et al128 found that long-term outcomes improved after saucerization versus total meniscectomy for discoid lateral meniscal tears, but there was no difference in short-term outcomes for these procedures. Lee et al76 found better radiographic outcomes after APM versus total meniscectomy for discoid lateral meniscal tears; however, the results were not stratified by different types of discoid lateral meniscal tears. Mild joint space narrowing was observed in the lateral compartment after meniscectomy in patients with a discoid lateral meniscal tear; however, there were no cases of moderate or advanced degenerative changes.80 Moreover, increased age, longer follow-up, and subtotal or total meniscectomy may have contributed to degenerative changes in those with a discoid lateral meniscal tear. Dai et al28 conducted a meta-analysis of 15 studies and found that (1) patients undergoing partial APM had better clinical outcomes than those undergoing total meniscectomy for treatment of discoid lateral meniscus, (2) patients younger than 20 years had better outcomes than those 20 years and older, and (3) clinical outcomes were better at short- versus long-term follow-up. Shanmugaraj et al122 found that the complication rate was 1.3% after APM for horizontal cleavage tears.
Predictors of Clinical Outcomes
Eijgenraam et al38 identified several predictors of worse outcomes after APM, including radiographic knee osteoarthritis at baseline, symptoms lasting >12 months, resection of >50% of the meniscus, and resection of the peripheral meniscal rim.38 Factors that did not affect outcomes after APM included sex, traumatic onset, preoperative activity level, and type of meniscal tear, and there was conflicting evidence regarding the effect of age, BMI, limb malalignment, and chondral damage found during arthroscopy on outcomes of APM. Salata et al116 reported that predictors of poor outcomes after meniscectomy included total meniscectomy with removal of the peripheral meniscal rim, degenerative meniscal tears, preexisting chondral lesions, presence of radiographic hand osteoarthritis, ACL deficiency, and increased BMI.
Meniscal Repair
Biomechanical Research
Alentorn-Geli et al4 systematically reviewed 6 biomechanical studies and found that stiffness was higher for all-inside repairs compared with the inside-out technique, but there was no difference in load to failure. The results regarding displacement, sites of failure, contact pressure, and superiority were inconclusive, mainly because of between-study variation in the type of all-inside devices and suture constructs used. Alentorn-Geli et al concluded that the meniscal repair technique was based on surgeon preference and there was no clear benefit of any single technique over the others.
Buckland et al19 conducted a meta-analysis of 41 studies and found that meniscal sutures had higher load to failure and more stiffness properties than meniscal repair devices. The strongest meniscal sutures were No. 0-PDS Vertical (145 N), No. 2-0 OrthoCord (144 N), and Ethibond No. 0 Vertical (136 N); the strongest meniscal repair devices were Meniscal Viper (141 N), MaxFire Vertical (136 N), and FasT-Fix Vertical (115 N).
Zone of Repair
Beaufils et al13 concluded that meniscal repair should be used only to treat peripheral lesions in young, healthy meniscal tissue in vascularized regions (ie, red-red or red-white zones) and that the rate of failure for meniscal repairs ranged from 4% to 28%. Barber-Westin and Noyes10 found that approximately 58% of meniscal repairs (767/1326) were in the red-white zone, or central-third, and 72% of meniscal repairs (955/1326) were conducted concurrently with ACL reconstruction. Most repairs were clinically healed (83%), and only 3% of patients reported complications, although follow-up time periods varied considerably between studies. Clinical outcomes were not affected by age, chronicity of injury, involved tibiofemoral compartment, sex, or concurrent ACL reconstruction.
Comparison of Repair Techniques
Several systematic reviews found no difference in clinical outcomes, failure rates, or complication rates between all-inside versus inside-out meniscal repairs.41,42,48,49,67,90 Grant et al49 reported that all-inside repairs required up to 50% less operative time than inside-out repairs. Several limitations of reviews that compared all-inside with inside-out repairs were noted, including variation in the type of implant used between studies and considerable heterogeneity of repair location (ie, tears in the red-red, red-white, and white-white zones and ramp lesions).41,67 One systematic review reported a higher healing rate for outside-in versus all-inside repairs (OR, 4.23; 95% CI, 1.10-16.0).41 Nepple et al96 conducted a meta-analysis of 13 studies and found similar rates of failure at 5 years after open (23%), outside-in (24%), inside-out (22%), and all-inside (24%) meniscal repairs. Furthermore, repair failure was not affected by laterality of repair or ACL status (intact vs deficient). Ayeni et al6 systematically reviewed 4 studies and found no difference in retear rates between meniscal arrow repair and traditional meniscal suture repair. However, this study was limited by poor study quality and substantial heterogeneity with respect to follow-up time. Mutsaerts et al94 found no difference in retear rates or complication rates after meniscal arrow repair versus inside-out repair. Overall complication rates for inside-out and all-inside meniscal repairs were similar according to both Elmallah et al41 and Grant et al49; however, a higher incidence of implant prominence or irritation for all-inside repairs and a higher incidence of neurapraxia or nerve irritation for inside-out repairs were noted.
Clinical Outcomes
Paxton et al104 found lower reoperation rates (1) for lateral versus medial meniscal repairs and (2) when concomitant ACL reconstruction was performed compared with isolated meniscal repair. In a systematic review of 8 studies, Liechti et al81 found an overall failure rate of 17% after meniscal repair in patients younger than 18 years as well as better meniscal healing among patients who underwent concomitant ACL reconstruction. Ferrari et al45 found good clinical outcomes, high healing rates, and low complication rates after meniscal repair in children and adolescents. Concomitant ACL reconstruction was performed in 60% of patients and did not have an effect on outcomes. Mosich et al92 found an overall failure rate of 37% after meniscal repair in adolescents, and repair success rates were worse for adolescents with complex tear patterns compared with simple tear patterns. Rothermel et al114 found that age and concomitant ACL reconstruction did not affect meniscal healing after repair. A meta-analysis of 7 studies found that meniscal repair was associated with better long-term outcomes compared with APM.143 Kurzweil et al72 found that the success rate after repair of horizontal meniscal tears was 79%, although the results may have been biased toward younger patients since the median age was 23 years among a total of 98 repairs. Shanmugaraj et al122 found that the complication rate was 12.9% after meniscal repair for horizontal cleavage tears, and clinical outcomes showed improvement. Moulton et al93 found good outcomes, satisfactory healing, and no serious complications after repair of radial meniscal tears in the short term. Constantinescu et al24 systematically reviewed the effect of perioperative nonsteroidal anti-inflammatory drug (NSAID) administration on soft tissue healing and found only 1 study regarding NSAID use and meniscal repair; that study demonstrated no difference in surgical failure rate for those patients who received NSAIDs versus those who did not receive NSAIDs (34% vs 35%; P = .99). In their review of 28 studies, Eberbach et al36 found that 90% of mixed-level (recreational and professional) athletes and 86% of professional athletes returned to sport at an average of 4 to 7 months after isolated meniscal repair. The failure rate was lower in professional athletes (9%) compared with mixed-level athletes (22%).
Meniscal Root Repairs
Biomechanical Research
Jiang et al65 systematically reviewed 17 studies that evaluated biomechanical properties of various meniscal root repair techniques. No consensus was found regarding the superiority of transtibial pullout repair versus suture anchor repair. Modified Mason-Allen sutures were superior to simple sutures in transtibial pullout repair, and 2-suture repair was superior to 1-suture repair in terms of increased stiffness and maximum load. Placing sutures farther from the meniscal root also increased the maximum load to failure. Anatomic meniscal root repairs led to greater joint surface contact area and lower contact pressure compared with nonanatomic meniscal root repairs.
Clinical Outcomes
Chung et al22 found improvement in Lysholm scores after medial meniscal posterior root repair. Meniscal extrusion was not significantly reduced after repair; however, there was a trend toward less extrusion (mean, –0.55 mm; 95% CI, –1.42 to 0.33), which the authors speculated could be due to the restoration of hoop tension forces. Although root repair did not halt progression of arthrosis, the authors reported that it occurred at a rate much lower than that reported after meniscectomy. Feucht et al46 found that 16% of patients had radiographic progression of Kellgren-Lawrence grade at 3 years after arthroscopic transtibial pullout repair for posteromedial meniscal root tears. Further, 18% of patients had deterioration of cartilage grade at 30 months and 56% had reduced medial meniscal extrusion at 3 years after repair. Complete healing was found in 62% of patients, partial healing in 34%, and failure to heal in 4%. One systematic review found that (1) preoperative Outerbridge grade 3 or grade 4 chondral lesions and (2) varus alignment >5° were predictive of poor outcomes after meniscal root repair in 5 studies.64 Pooled results from 9 studies showed that rates of osteoarthritis were 53% after meniscal repair, 99% after meniscectomy, and 95% after nonoperative management in patients with medial meniscal root tears. Meniscal repair was found to be the most cost-effective treatment for root tears, and 10-year rates of total knee arthroplasty were 33.5%, 51.5%, and 45.5% after meniscal repair, meniscectomy, and nonoperative management, respectively.44
Meniscal Allograft Transplantation
Biomechanical Research
Seitz and Durselen120 found that the most important biomechanical properties for MAT were secure fixation and proper graft sizing. Bone plugs or bone blocks for allograft attachment were superior to circumferential suturing and were associated with chondroprotective effects. The authors concluded that grafts that were too small did not compensate for knee joint incongruity and grafts that were too large could lead to extrusion.
Indications and Techniques
Rosso et al113 found good agreement in the literature pertaining to indications for MAT, including joint line tenderness associated with prior APM, younger age, absence of diffuse Outerbridge grades 3 or 4 cartilage damage, and a stable well-aligned knee. Several systematic reviews and meta-analyses found that cryopreserved (40%-55%), fresh frozen (61%), and deep-frozen grafts (36%) were most commonly used for MAT, and graft sizing was typically done using plain radiography.29,40,97,113 However, surgical techniques varied considerably and included double bone plug, minimally invasive arthroscopy, onlay, sutures only, bony fixation, open surgery, and anchoring of horns with or without tunnels.29 Novaretti et al97 reported that bone-fixation technique was the most commonly used (54%), although Rosso et al113 concluded that insufficient evidence was available to determine which fixation technique was superior. ACL reconstruction and procedures for treating chondral injuries have been shown to be the most frequently performed concomitant procedures in patients undergoing MAT.40,97
Clinical Outcomes
Smith et al126 systematically reviewed 35 studies and found that clinical outcomes improved after MAT; however, the included studies were at high risk for bias. Myers and Tudor95 systematically reviewed 41 studies and concluded that MAT generally resulted in good outcomes and should be considered only in patients with localized pain and a stable and well-aligned knee, although none of the studies they reviewed were randomized or controlled. Hergan et al56 systematically reviewed 14 studies and found that 63% to 100% of patients had good clinical outcomes. Samitier et al117 found that (1) clinical outcomes improved at 7 to 14 years after MAT, (2) 75% to 85% of patients were able to return to the same level of competition after MAT, and (3) performing MAT plus a concomitant procedure did not result in worse outcomes. Lee et al74 conducted a meta-analysis of 24 studies and found no difference in clinical outcomes scores between isolated MAT versus MAT combined with other procedures. In that meta-analysis, 4 studies found that additional procedures did not affect MAT survivorship, although 3 studies found that combining MAT with ligament surgery, realignment osteotomy, and osteochondral autograft transfer was a risk factor for MAT failure. ElAttar et al40 found that immediate range of motion exercises after MAT were associated with a good outcome. Barber-Westin and Noyes11 found that 70% to 92% of 285 patients from 7 studies returned to sports, with the mean Tegner score <5 in 58% of 24 studies, indicating that the majority of patients participated in light recreational activity. Tegner scores were not associated with transplant failure, and data regarding the progression of tibiofemoral osteoarthritis were insufficient. Two overlapping systematic reviews found that 67% to 92% of athletes returned to play between 8 and 17 months after MAT.66,79 Grassi et al50 conducted a meta-analysis of the results of 9 studies and found that 77% of patients returned to sport or physical activity after MAT, 13% had a graft-related reoperation, and 1% went on to have a partial or total knee replacement.
Survival and Failure Rates
De Bruycker et al30 found a high survival rate (81%) at an average of 5 years after MAT in a meta-analysis of 65 studies; however, increased age and BMI may have had a negative influence on outcomes. After conducting a meta-analysis of 38 studies, Jauregui et al63 did not find any differences in clinical outcome scores, meniscal allograft tear rates, or failure rates after MAT with soft tissue suture versus bone fixation. Novaretti et al97 conducted a meta-analysis of 11 studies and found good survivorship at 10 to 15 years after MAT. A different meta-analysis found similar rates of survivorship for both medial and lateral MAT at short-term and long-term follow-up in 9 studies.16 Patients undergoing lateral MAT experienced more pain relief and functional improvement compared with those undergoing medial MAT. Several studies have noted considerable variation in rates of failure (0%-35%), reoperation (31%-60%), and complications (14%-46%) after MAT.29,40,56,117,126 In a systematic review of 6 studies, Harris et al54 noted that the failure rate was 12% in 110 patients undergoing combined MAT plus cartilage repair or restoration, and most failures were related to MAT as opposed to the cartilage procedure.
Graft Extrusion
In a meta-analysis of 8 studies, Bin et al15 found that major graft extrusion (>3 mm) was 5 times more likely to occur after medial versus lateral MAT using the arthroscopic-assisted technique; however, the odds of graft extrusion did not differ between medial and lateral MAT using the complete arthroscopic procedure. Wei et al140 found increased graft extrusion for medial versus lateral MAT, with better clinical outcomes for lateral versus medial MAT. Lee75 conducted a meta-analysis of the results of 21 studies and found that the absolute mean (3.26 vs 3.01 mm; P = .001) and relative percentage (33% vs 29%; P < .001) of extrusion were both greater after medial versus lateral MAT. Major graft extrusion (>3 mm) was also greater for medial versus lateral MAT (61% vs 39%; P < .001). In a systematic review of 38 studies, Smith et al127 found that (1) the weighted mean joint space loss was 0.032 mm at 4.5 years after MAT for 11 studies, (2) meniscal extrusion was present in the majority of cases but was not related to clinical outcomes, and (3) meniscal healing rates were high but the size, shape, and signal intensity varied from the native meniscus. Noyes and Barber-Westin98 found that mean extrusion ranged from 2.96 to 3.87 mm and relative percentage of extrusion ranged from 29% to 43% in 5 studies of fresh-frozen meniscal transplants implanted with bone fixation, and 2 studies reported approximately 47% extrusion >3 mm. Additionally, they found that 70% to 100% of patients with fresh-frozen meniscal transplants without bone fixation had some degree of extrusion, but no association was found between transplant extrusion and clinical outcome scores or other radiographic factors in these cases.
Chondroprotective Effects
Two systematic reviews demonstrated good clinical outcomes after MAT, although both concluded that there was insufficient evidence for determining the chondroprotective effects of MAT.113,139 In a systematic review and meta-analysis of 17 animal studies, MAT was associated with less gross macroscopic cartilage damage compared with meniscectomy but more damage compared with a control group.112 No difference in osteoarthritic changes after MAT versus meniscectomy was seen, although MAT was associated with more osteoarthritic changes versus a control group. MAT was associated with less histological damage to articular cartilage versus meniscectomy; however, MAT was associated with increased histological damage to cartilage versus a control group.
Second-Look Arthroscopy
Oh et al101 found that second-look arthroscopy was performed after MAT in 100% of cases in 2 studies and about 46% of cases in 12 studies; the rate was not reported in 1 study. The authors were unable to find distinct indications for performing second-look arthroscopy, however most studies performed second-look arthroscopy for objective evaluation or to treat another knee problem. The rate of complete allograft healing ranged from 74% to 88% in 3 studies, and failure rate was 21% in 2 studies.
Meniscal Implants and Scaffolds
Two overlapping systematic reviews examined the efficacy of collagen meniscal implant in >300 patients, of whom 41% to 49% underwent a concomitant procedure (eg, ACL reconstruction, high tibial osteotomy, microfracture).51,55 Although clinical outcomes generally improved after implantation, most studies were of poor quality or did not include a control group. Dangelmajer et al29 found failure rates ranging from 1% to 8% in 4 studies evaluating collagen meniscal implants. The collagen meniscal implant and Actifit scaffold were associated with good clinical outcomes, few complications (13%), and a low failure rate (6%) in 23 studies reviewed by Filardo et al,47 although the studies in this review were of low quality. Furthermore, a meta-analysis by Houck et al59 found no difference in the rate of treatment failure between the collagen meniscal implant and the Actifit (10% vs 7%; P > .05), and a systematic review by Ranmuthu et al110 found some evidence that these 2 types of scaffolds were porous, mature, and resorbable and had possible chondroprotective effects as seen on MRI. A systematic review by Warth and Rodkey138 examined outcomes of resorbable collagen meniscal implantation and generally found good clinical outcomes, minimal degenerative changes on postoperative radiographs, decreased signal intensity on MRI, the presence of meniscus-like tissue at second-look arthroscopy, and good integration of new tissue based on histological analysis.
The size and MRI signal intensity of meniscal scaffold were comparable with those of a normal meniscus at long-term follow-up in a systematic review of 6 studies, although the studies were of low quality and there were not enough follow-up evaluations within each study.144 Shin et al123 conducted a meta-analysis of 18 studies that examined MRI and clinical outcomes in patients treated with polyurethane meniscal scaffolds. Postoperative pain and function improved, whereas articular cartilage and absolute meniscal extrusion worsened on postoperative MRI. Other MRI parameters, such as morphology and size of the implant, signal intensity, and interface of the implant-residual meniscal complex, did not change postoperatively. In a systematic review of polyurethane meniscal scaffolds, Tark et al133 reported improvement in outcomes and found that implant failure ranged from 4% to 6%; however, most included studies lacked a control group and none assessed long-term outcomes. Dangelmajer et al29 found failure rates ranging from 0% to 17% in 3 studies that evaluated polyurethane scaffolds. Two systematic reviews concluded that cell-based scaffolds tended to be associated with successful outcomes in the short term (12-24 weeks after surgery), however results for synthetic scaffolds were limited because most studies lacked a proper control group.52,105 Papalia et al103 found that the average rate of failure for meniscal scaffolds was 10% and the average rate of severe complications was 5% (either definitely or possibly related to the scaffold).
Moran et al91 found that various types of meniscal scaffolds (eg, synthetic, tissue derived) were successful during in vitro studies, but in vivo studies were limited and the optimal meniscal scaffold type remains unknown. Di Matteo et al33 examined 34 studies that evaluated the use of meniscal scaffolds in animal models and found that most biomaterials and bioengineered scaffolds were safe and capable of stimulating meniscal healing and providing chondral protection. However, poor results were found for Dacron-based scaffolds, and there was inconclusive evidence regarding cell augmentation for these implants.
Mesenchymal Stem Cells and Growth Factors
Korpershoek et al71 found evidence to suggest that repair and regeneration of meniscal tissue may occur when mesenchymal stem cells from bone marrow, adipose tissue, meniscus, or synovium were injected intra-articularly; however, there was no consensus regarding the number of stem cells needed and superiority of technique for augmentation of meniscal repair or regeneration. According to a systematic review by Chew et al,21 the method of stem cell harvest varied between studies such that 3 of 4 studies administered stem cells via percutaneous injection in the knee and 1 of 4 studies used a collagen scaffold for administration. Clinical outcomes generally improved and there were no adverse events; however, only 1 study included a control group. A systematic review by Moran et al91 also found promising results for stem cells and growth factor therapy for treating meniscal injuries; however, the optimal dosing and route of administration are not known. Haddad et al52 found limited evidence from animal studies demonstrating that human insulin-like growth factor–1 was associated with meniscal healing but platelet-rich plasma was not.
Postoperative Rehabilitation
Meniscal Repair
Several systematic reviews examined the effect of restricted and accelerated rehabilitation protocols on outcomes after meniscal repair.100,131,136,137 Spang et al131 found no difference in clinical outcomes or rates of failure between restricted (nonweightbearing for at least 2 weeks) and accelerated (immediate weightbearing) rehabilitation protocols in 17 studies; however, only 3 of 17 studies actually made a head-to-head comparison of restricted versus accelerated rehabilitation protocols. Likewise, O’Donnell et al100 found similar clinical outcomes for accelerated, motion-restricted, weight-restricted, and dual-restricted rehabilitation groups. Furthermore, early range of motion and weightbearing status did not affect clinical outcomes in O’Donnell’s review. According to VanderHave et al,136 successful clinical outcomes were found in 70% to 94% of patients after restricted rehabilitation (nonweightbearing for 2-6 weeks) in 4 studies and in 64% to 96% of patients after accelerated rehabilitation (immediate weightbearing). Vascellari et al137 found no difference in repair failure between accelerated versus restricted (nonweightbearing for 4-6 weeks) rehabilitation (13% vs 10%, respectively).
APM
A systematic review by Imoto et al61 revealed no benefit of adding electrical stimulation to rehabilitation after APM; however, this conclusion was based on evidence from only 2 studies. Dias et al34 conducted a systematic review of 18 RCTs and found that physical therapy plus home exercise was more effective at improving range of motion and function than home exercise alone after APM.
Postoperative Imaging Assessment
Baker et al7 conducted a systematic review that examined the accuracy of various imaging modalities for assessing recurrent meniscal tears after meniscal surgery. The accuracy of diagnosing recurrent tears after APM and meniscal repair was 57% to 80% after conventional MRI, 85% to 93% after direct magnetic resonance arthrography, and 81% to 93% after indirect magnetic resonance arthrography. Conventional MRI was comparable with clinical examination for assessing meniscal healing after MAT. Baker et al concluded that direct and indirect magnetic resonance arthrography was superior to conventional MRI for assessment of meniscal healing after APM or meniscal repair; however, few studies have directly compared different imaging modalities.
Patient-Reported Outcome Measures
Abram et al2 performed a systematic review to summarize and critically appraise the patient-reported outcome measures that are used in patients with meniscal tears. The study quality of 11 studies was evaluated with the COSMIN (Consensus-based Standards for the Selection of Health Measurement Instruments) checklist. A total of 10 outcome measures were evaluated, and of these, the Western Ontario Meniscal Evaluation Tool demonstrated the strongest evidence for content validity. Limited evidence was found to support use of the Lysholm knee scale and the International Knee Documentation Committee Subjective Knee Form for evaluating symptoms and function in patients with meniscal tears.
Cost-Effectiveness
Afzali et al3 performed a systematic review to evaluate the cost-effectiveness of treatment for nonosteoarthritic knee pain conditions, which included 2 high-quality studies of meniscal injuries. One study found no clear evidence of cost-effectiveness for either APM or meniscal scaffold procedures, whereas the other study found that APM was more cost-effective than MAT in the short term but MAT was more effective at delaying total knee arthroplasty in the long term compared with APM. Waugh et al139 set out to examine cost-effectiveness of MAT in a systematic review; however, they found that a cost-effectiveness analysis was not feasible because they did not find any studies that compared MAT versus nonoperative management.
Discussion
This systematic review provides a thorough summary of systematic reviews and meta-analyses pertaining to the meniscus. For some topics substantial evidence is available, and for others evidence is lacking or biased. For instance, substantial evidence is available demonstrating that increased age; male sex; kneeling or squatting; standing, walking, or lifting for long periods of time; and delayed ACL reconstruction are risk factors for meniscal tears, however minimal evidence is available suggesting that increased BMI is also a risk factor.111,129 Several studies demonstrated that MRI was accurate for diagnosing meniscal tears,20,107,108,121,124 but physical examination was only moderately accurate at best.17,18,31,32,123 Meniscal tears are commonly found at the time of ACL reconstruction, especially when ACL reconstruction has been delayed by 6 months or more and after recurrent instability episodes.89,99,130 Furthermore, APM done at the time of ACL reconstruction is a risk factor for developing osteoarthritis in the future.23,86,108 In patients with concomitant degenerative meniscal tears and osteoarthritis, evidence regarding the efficacy of APM has been conflicting.43,68,73 Substantial evidence is available demonstrating no difference in clinical outcomes for APM versus conservative management for degenerative meniscal tears1,70,77,78,106,132; however, the available evidence may be biased and of low quality.58,87 Clinical outcomes tended to improve after APM and reoperation rates were low, although knee osteoarthritis is likely to develop after APM.13,102,104
Meniscal repairs have been associated with good clinical outcomes overall,45,81,143 and for isolated meniscal repairs there has been no difference in clinical outcomes between all-inside versus inside-out repairs.41,42,48,49,67,90 Meniscal root repairs were shown to be cost-effective, to be associated with high rates of complete or partial healing, and to lessen the progression of arthrosis.44,46,64 Substantial evidence has shown good clinical outcomes after MAT and high survival rates, although studies may have been biased and RCTs are lacking.30,56,95,97,117,126 The optimal type of both meniscal scaffolds and implants remains unknown; however, good clinical outcomes, few complications, and low failure rates have been observed for various types of meniscal scaffolds (eg, synthetic, tissue derived) and implants (eg, collagen implant, Actifit), although further research is needed.‡ Minimal evidence is available to suggest that stem cell or growth factor therapy is effective, and the optimal route of administration and optimal dosing remain unknown.21,52,71,91
To our knowledge, this is the first systematic review of systematic reviews and meta-analyses focused on the meniscus. This study is not without limitations. We have summarized a large body of literature ranging from level 1 to level 4 evidence. Each individual systematic review and meta-analysis comes with its own limitations including potential biases, such as selection bias or publication bias, which may have affected our overall results. Because of the heterogeneity between reviews, we did not attempt any meta-analyses and kept our review to a qualitative summary of the literature.
Conclusion
This summary of systematic reviews and meta-analyses delivers surgeons a single source of the current evidence regarding the meniscus.
Final version submitted March 19, 2020; accepted April 9, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was funded by the Ralph C. Wilson, Jr. Foundation. L.J.B. has received funding from Arthrex, Prodigy Surgical Distribution, and Zimmer Biomet. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Abram SGF, Hopewell S, Monk AP, et al. Arthroscopic partial meniscectomy for meniscal tears of the knee: a systematic review and meta-analysis. Br J Sports Med. 2020;54(11):652–663. [DOI] [PubMed] [Google Scholar]
- 2. Abram SGF, Middleton R, Beard DJ, Price AJ, Hopewell S. Patient-reported outcome measures for patients with meniscal tears: a systematic review of measurement properties and evaluation with the COSMIN checklist. BMJ Open. 2017;7(10):e01724 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Afzali T, Fangel MV, Vestergaard AS, et al. Cost-effectiveness of treatments for non-osteoarthritic knee pain conditions: a systematic review. PloS One. 2018;13(12):e02092 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Alentorn-Geli E, Choi JH, Stuart JJ, et al. Inside-out or outside-in suturing should not be considered the standard repair method for radial tears of the midbody of the lateral meniscus: a systematic review and meta-analysis of biomechanical studies. J Knee Surg. 2016;29(7):604–612. [DOI] [PubMed] [Google Scholar]
- 5. Anderson MJ, Browning WM III, Urband CE, Kluczynski MA, Bisson LJ. A systematic summary of systematic reviews on the topic of the anterior cruciate ligament. Orthop J Sports Med. 2016;4(3):2325967116634074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ayeni O, Peterson D, Chan K, Javidan A, Gandhi R. Suture repair versus arrow repair for symptomatic meniscus tears of the knee: a systematic review. J Knee Surg. 2012;25(5):397–402. [DOI] [PubMed] [Google Scholar]
- 7. Baker JC, Friedman MV, Rubin DA. Imaging the postoperative knee meniscus: an evidence-based review. AJR Am J Roentgenol. 2018;211(3):519–527. [DOI] [PubMed] [Google Scholar]
- 8. Balato G, Di Donato SL, Ascione T, et al. Knee septic arthritis after arthroscopy: incidence, risk factors, functional outcome, and infection eradication rate. Joints. 2017;5(2):107–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bansal S, Keah NM, Neuwirth AL, et al. Large animal models of meniscus repair and regeneration: a systematic review of the state of the field. Tissue Eng Part C Methods. 2017;23(11):661–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Barber-Westin SD, Noyes FR. Clinical healing rates of meniscus repairs of tears in the central-third (red-white) zone. Arthroscopy. 2014;30(1):134–146. [DOI] [PubMed] [Google Scholar]
- 11. Barber-Westin SD, Noyes FR. Low-impact sports activities are feasible after meniscus transplantation: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2018;26(7):1950–1958. [DOI] [PubMed] [Google Scholar]
- 12. Beals CT, Magnussen RA, Graham WC, Flanigan DC. The prevalence of meniscal pathology in asymptomatic athletes. Sports Med. 2016;46(10):1517–1524. [DOI] [PubMed] [Google Scholar]
- 13. Beaufils P, Hulet C, Dhenain M, et al. Clinical practice guidelines for the management of meniscal lesions and isolated lesions of the anterior cruciate ligament of the knee in adults. Orthop Traumatol Surg Res. 2009;95(6):437–442. [DOI] [PubMed] [Google Scholar]
- 14. Bert JM, Giannini D, Nace L. Antibiotic prophylaxis for arthroscopy of the knee: is it necessary? Arthroscopy. 2007;23(1):4–6. [DOI] [PubMed] [Google Scholar]
- 15. Bin SI, Kim HJ, Lee DH. Graft extrusion after medial and lateral MAT differs according to surgical technique: a meta-analysis. Arch Orthop Trauma Surg. 2018;138(6):843–850. [DOI] [PubMed] [Google Scholar]
- 16. Bin SI, Nha KW, Cheong JY, Shin YS. Midterm and long-term results of medial versus lateral meniscal allograft transplantation: a meta-analysis. Am J Sports Med. 2018;46(5):1243–1250. [DOI] [PubMed] [Google Scholar]
- 17. Blorstad A, Perry K, Haladay D. The diagnostic accuracy of joint line tenderness for assessing meniscal tears: a systematic review with meta-analysis. Orthopaedic Physical Therapy Practice. 2011;23(2):76–82. [Google Scholar]
- 18. Brady MP, Weiss W. Clinical assessment versus MRI diagnosis of meniscus tears. J Sport Rehabil. 2015;24(4):423–427. [DOI] [PubMed] [Google Scholar]
- 19. Buckland DM, Sadoghi P, Wimmer MD, et al. Meta-analysis on biomechanical properties of meniscus repairs: are devices better than sutures? Knee Surg Sports Traumatol Arthrosc. 2015;23(1):83–89. [DOI] [PubMed] [Google Scholar]
- 20. Cheng Q, Zhao FC. Comparison of 1.5- and 3.0-T magnetic resonance imaging for evaluating lesions of the knee: a systematic review and meta-analysis (PRISMA-compliant article). Medicine. 2018;97(38):e12401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chew E, Prakash R, Khan W. Mesenchymal stem cells in human meniscal regeneration: a systematic review. Ann Med Surg (Lond). 2017;24:3–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Chung KS, Ha JK, Ra HJ, Kim JG. A meta-analysis of clinical and radiographic outcomes of posterior horn medial meniscus root repairs. Knee Surg Sports Traumatol Arthrosc. 2016;24(5):1455–1468. [DOI] [PubMed] [Google Scholar]
- 23. Claes S, Hermie L, Verdonk R, Bellemans J, Verdonk P. Is osteoarthritis an inevitable consequence of anterior cruciate ligament reconstruction? A meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21(9):1967–1976. [DOI] [PubMed] [Google Scholar]
- 24. Constantinescu DS, Campbell MP, Moatshe G, Vap AR. Effects of perioperative nonsteroidal anti-inflammatory drug administration on soft tissue healing: a systematic review of clinical outcomes after sports medicine orthopaedic surgery procedures. Orthop J Sports Med. 2019;7(4):2325967119838873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cramer H, Ostermann T, Dobos G. Injuries and other adverse events associated with yoga practice: a systematic review of epidemiological studies. J Sci Med Sport. 2018;21(2):147–154. [DOI] [PubMed] [Google Scholar]
- 26. Culvenor AG, Oiestad BE, Hart HF, et al. Prevalence of knee osteoarthritis features on magnetic resonance imaging in asymptomatic uninjured adults: a systematic review and meta-analysis. Br J Sports Med. 2019;53:1268–1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Dai H, Huang ZG, Chen ZJ, Liu JX. Diagnostic accuracy of ultrasonography in assessing meniscal injury: meta-analysis of prospective studies. J Orthop Sci. 2015;20(4):675–681. [DOI] [PubMed] [Google Scholar]
- 28. Dai WL, Zhang H, Zhou AG, Zhang G, Zhang J. Discoid lateral meniscus. J Knee Surg. 2017;30(9):854–862. [DOI] [PubMed] [Google Scholar]
- 29. Dangelmajer S, Familiari F, Simonetta R, Kaymakoglu M, Huri G. Meniscal transplants and scaffolds: a systematic review of the literature. Knee Surg Relat Res. 2017;29(1):3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. De Bruycker M, Verdonk PCM, Verdonk RC. Meniscal allograft transplantation: a meta-analysis. SICOT J. 2017;3:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Decary S, Ouellet P, Vendittoli PA, Desmeules F. Reliability of physical examination tests for the diagnosis of knee disorders: evidence from a systematic review. Man Ther. 2016;26:172–182. [DOI] [PubMed] [Google Scholar]
- 32. Decary S, Ouellet P, Vendittoli PA, Roy JS, Desmeules F. Diagnostic validity of physical examination tests for common knee disorders: an overview of systematic reviews and meta-analysis. Phys Ther Sport. 2017;23:143–155. [DOI] [PubMed] [Google Scholar]
- 33. Di Matteo B, Perdisa F, Gostynska N, et al. Meniscal scaffolds—preclinical evidence to support their use: a systematic review. Open Orthop J. 2015;9:143–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Dias JM, Mazuquin BF, Mostagi FQ, et al. The effectiveness of postoperative physical therapy treatment in patients who have undergone arthroscopic partial meniscectomy: systematic review with meta-analysis. J Orthop Sports Phys Ther. 2013;43(8):560–576. [DOI] [PubMed] [Google Scholar]
- 35. Dong F, Zhang L, Wang S, et al. The diagnostic accuracy of B-mode ultrasound in detecting meniscal tears: a systematic review and pooled meta-analysis. Med Ultrason. 2018;20(2):164–169. [DOI] [PubMed] [Google Scholar]
- 36. Eberbach H, Zwingmann J, Hohloch L, et al. Sport-specific outcomes after isolated meniscal repair: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2018;26(3):762–771. [DOI] [PubMed] [Google Scholar]
- 37. Edouard P, Rannou F, Coudeyre E. Animal evidence for hyaluronic acid efficacy in knee trauma injuries: review of animal-model studies. Phys Ther Sport. 2013;14(2):116–123. [DOI] [PubMed] [Google Scholar]
- 38. Eijgenraam SM, Reijman M, Bierma-Zeinstra SMA, van Yperen DT, Meuffels DE. Can we predict the clinical outcome of arthroscopic partial meniscectomy? A systematic review. Br J Sports Med. 2018;52(8):514–521. [DOI] [PubMed] [Google Scholar]
- 39. Ekhtiari S, Khan M, Kirsch JM, Thornley P, Larson CM, Bedi A. Most elite athletes return to competition following operative management of meniscal tears: a systematic review. J ISAKOS. 2018;3:110–115. [Google Scholar]
- 40. ElAttar M, Dhollander A, Verdonk R, Almqvist KF, Verdonk P. Twenty-six years of meniscal allograft transplantation: is it still experimental? A meta-analysis of 44 trials. Knee Surg Sports Traumatol Arthrosc. 2011;19(2):147–157. [DOI] [PubMed] [Google Scholar]
- 41. Elmallah R, Jones LC, Malloch L, Barrett GR. A meta-analysis of arthroscopic meniscal repair: inside-out versus outside-in versus all-inside techniques. J Knee Surg. 2019;32(8):750–757. [DOI] [PubMed] [Google Scholar]
- 42. Everhart JS, Higgins JD, Poland SG, Abouljoud MM, Flanigan DC. Meniscal repair in patients age 40 years and older: a systematic review of 11 studies and 148 patients. Knee. 2018;25(6):1142–1150. [DOI] [PubMed] [Google Scholar]
- 43. Evidence Development and Standards Branch, Health Quality Ontario. Arthroscopic debridement of the knee: an evidence update. Ont Health Technol Assess Ser. 2014;14(13):1–43. [PMC free article] [PubMed] [Google Scholar]
- 44. Faucett SC, Geisler BP, Chahla J, et al. Meniscus root repair vs meniscectomy or nonoperative management to prevent knee osteoarthritis after medial meniscus root tears: clinical and economic effectiveness. Am J Sports Med. 2019;47(3):762–769. [DOI] [PubMed] [Google Scholar]
- 45. Ferrari MB, Murphy CP, Gomes JLE. Meniscus repair in children and adolescents: a systematic review of treatment approaches, meniscal healing, and outcomes. J Knee Surg. 2019;32(6):490–498. [DOI] [PubMed] [Google Scholar]
- 46. Feucht MJ, Kuhle J, Bode G, et al. Arthroscopic transtibial pullout repair for posterior medial meniscus root tears: a systematic review of clinical, radiographic, and second-look arthroscopic results. Arthroscopy. 2015;31(9):1808–1816. [DOI] [PubMed] [Google Scholar]
- 47. Filardo G, Andriolo L, Kon E, de Caro F, Marcacci M. Meniscal scaffolds: results and indications: a systematic literature review. Int Orthop. 2015;39(1):35–46. [DOI] [PubMed] [Google Scholar]
- 48. Fillingham YA, Riboh JC, Erickson BJ, Bach BR, Jr, Yanke AB. Inside-out versus all-inside repair of isolated meniscal tears: an updated systematic review. Am J Sports Med. 2017;45(1):234–242. [DOI] [PubMed] [Google Scholar]
- 49. Grant JA, Wilde J, Miller BS, Bedi A. Comparison of inside-out and all-inside techniques for the repair of isolated meniscal tears: a systematic review. Am J Sports Med. 2012;40(2):459–468. [DOI] [PubMed] [Google Scholar]
- 50. Grassi A, Bailey JR, Filardo G, et al. Return to sport activity after meniscal allograft transplantation: at what level and at what cost? A systematic review and meta-analysis. Sports Health. 2019;11(2):123–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Grassi A, Zaffagnini S, Marcheggiani Muccioli GM, Benzi A, Marcacci M. Clinical outcomes and complications of a collagen meniscus implant: a systematic review. Int Orthop. 2014;38(9):1945–1953. [DOI] [PubMed] [Google Scholar]
- 52. Haddad B, Haddad B, Konan S, Adesida A, Khan WS. A systematic review of tissue engineered meniscus and replacement strategies: preclinical models. Curr Stem Cell Res Ther. 2013;8(3):232–242. [DOI] [PubMed] [Google Scholar]
- 53. Hall M, Juhl CB, Lund H, Thorlund JB. Knee extensor muscle strength in middle-aged and older individuals undergoing arthroscopic partial meniscectomy: a systematic review and meta-analysis. Arthritis Care Res (Hoboken). 2015;67(9):1289–1296. [DOI] [PubMed] [Google Scholar]
- 54. Harris JD, Cavo M, Brophy R, Siston R, Flanigan D. Biological knee reconstruction: a systematic review of combined meniscal allograft transplantation and cartilage repair or restoration. Arthroscopy. 2011;27(3):409–418. [DOI] [PubMed] [Google Scholar]
- 55. Harston A, Nyland J, Brand E, McGinnis M, Caborn DN. Collagen meniscus implantation: a systematic review including rehabilitation and return to sports activity. Knee Surg Sports Traumatol Arthrosc. 2012;20(1):135–146. [DOI] [PubMed] [Google Scholar]
- 56. Hergan D, Thut D, Sherman O, Day MS. Meniscal allograft transplantation. Arthroscopy. 2011;27(1):101–112. [DOI] [PubMed] [Google Scholar]
- 57. Hing W, White S, Reid D, Marshall R. Validity of the McMurray’s test and modified versions of the test: a systematic literature review. J Man Manip Ther. 2009;17(1):22–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Hohmann E, Glatt V, Tetsworth K, Cote M. Arthroscopic partial meniscectomy versus physical therapy for degenerative meniscus lesions: how robust is the current evidence? A critical systematic review and qualitative synthesis. Arthroscopy. 2018;34(9):2699–2708. [DOI] [PubMed] [Google Scholar]
- 59. Houck DA, Kraeutler MJ, Belk JW, McCarty EC, Bravman JT. Similar clinical outcomes following collagen or polyurethane meniscal scaffold implantation: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2018;26(8):2259–2269. [DOI] [PubMed] [Google Scholar]
- 60. Hussain ZB, Chahla J, Mandelbaum BR, Gomoll AH, LaPrade RF. The role of meniscal tears in spontaneous osteonecrosis of the knee: a systematic review of suspected etiology and a call to revisit nomenclature. Am J Sports Med. 2019;47(2):501–507. [DOI] [PubMed] [Google Scholar]
- 61. Imoto AM, Peccin S, Almeida GJ, Saconato H, Atallah AN. Effectiveness of electrical stimulation on rehabilitation after ligament and meniscal injuries: a systematic review. Sao Paulo Med J. 2011;129(6):414–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Jancuska J, Matthews J, Miller T, Kluczynski MA, Bisson LJ. A systematic summary of systematic reviews on the topic of the rotator cuff. Orthop J Sports Med. 2018;6(9):2325967118797891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Jauregui JJ, Wu ZD, Meredith S, et al. How should we secure our transplanted meniscus? A meta-analysis. Am J Sports Med. 2018;46(9):2285–2290. [DOI] [PubMed] [Google Scholar]
- 64. Jiang EX, Abouljoud MM, Everhart JS, et al. Clinical factors associated with successful meniscal root repairs: a systematic review. Knee. 2019;26(2):285–291. [DOI] [PubMed] [Google Scholar]
- 65. Jiang EX, Everhart JS, Abouljoud M, et al. Biomechanical properties of posterior meniscal root repairs: a systematic review. Arthroscopy. 2019;35(7):2189–2206. [DOI] [PubMed] [Google Scholar]
- 66. Jochimsen K, Whale Conley CE, Malempati CS, Jacobs CA, Mattacola CG, Lattermann C. Meniscus transplantation: a systematic review of return-to-play rates. Athl Train Sports Health Care. 2018;10(2):76–81. [Google Scholar]
- 67. Kang DG, Park YJ, Yu JH, Oh JB, Lee DY. A systematic review and meta-analysis of arthroscopic meniscus repair in young patients: comparison of all-inside and inside-out suture techniques. Knee Surg Relat Res. 2019;31(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Karpinski K, Muller-Rath R, Niemeyer P, Angele P, Petersen W. Subgroups of patients with osteoarthritis and medial meniscus tear or crystal arthropathy benefit from arthroscopic treatment. Knee Surg Sports Traumatol Arthrosc. 2019;27(3):782–796. [DOI] [PubMed] [Google Scholar]
- 69. Kay J, Memon M, Shah A, et al. Earlier anterior cruciate ligament reconstruction is associated with a decreased risk of medial meniscal and articular cartilage damage in children and adolescents: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2018;26(12):3738–3753. [DOI] [PubMed] [Google Scholar]
- 70. Khan M, Evaniew N, Bedi A, Ayeni OR, Bhandari M. Arthroscopic surgery for degenerative tears of the meniscus: a systematic review and meta-analysis. CMAJ. 2014;186(14):1057–1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Korpershoek JV, de Windt TS, Hagmeijer MH, Vonk LA, Saris DB. Cell-based meniscus repair and regeneration: at the brink of clinical translation? A systematic review of preclinical studies. Orthop J Sports Med. 2017;5(2):2325967117690131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Kurzweil PR, Lynch NM, Coleman S, Kearney B. Repair of horizontal meniscus tears: a systematic review. Arthroscopy. 2014;30(11):1513–1519. [DOI] [PubMed] [Google Scholar]
- 73. Lamplot JD, Brophy RH. The role for arthroscopic partial meniscectomy in knees with degenerative changes: a systematic review. Bone Joint J. 2016;98(7):934–938. [DOI] [PubMed] [Google Scholar]
- 74. Lee BS, Kim HJ, Lee CR, et al. Clinical outcomes of meniscal allograft transplantation with or without other procedures: a systematic review and meta-analysis. Am J Sports Med. 2018;46(12):3047–3056. [DOI] [PubMed] [Google Scholar]
- 75. Lee DH. Incidence and extent of graft extrusion following meniscus allograft transplantation. BioMed Res Int. 2018;2018:5251910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Lee DH, D’Lima DD, Lee SH. Clinical and radiographic results of partial versus total meniscectomy in patients with symptomatic discoid lateral meniscus: a systematic review and meta-analysis. Orthop Traumatol Surg Res. 2019;105(4):669–675. [DOI] [PubMed] [Google Scholar]
- 77. Lee DY, Park YJ, Kim HJ, et al. Arthroscopic meniscal surgery versus conservative management in patients aged 40 years and older: a meta-analysis. Arch Orthop Trauma Surg. 2018;138(12):1731–1739. [DOI] [PubMed] [Google Scholar]
- 78. Lee SH, Lee OS, Kim ST, Lee YS. Revisiting arthroscopic partial meniscectomy for degenerative tears in knees with mild or no osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. Clin J Sport Med. 2020;30(3):195–202. [DOI] [PubMed] [Google Scholar]
- 79. Lee YS, Lee OS, Lee SH. Return to sports after athletes undergo meniscal surgery: a systematic review. Clin J Sports Med. 2019;29(1):29–36. [DOI] [PubMed] [Google Scholar]
- 80. Lee YS, Teo SH, Ahn JH, et al. Systematic review of the long-term surgical outcomes of discoid lateral meniscus. Arthroscopy. 2017;33(10):1884–1895. [DOI] [PubMed] [Google Scholar]
- 81. Liechti DJ, Constantinescu DS, Ridley TJ, et al. Meniscal repair in pediatric populations: a systematic review of outcomes. Orthop J Sports Med. 2019;7(5):23259 67119843355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Lim YZ, Wang Y, Wluka AE, et al. Are biomechanical factors, meniscal pathology, and physical activity risk factors for bone marrow lesions at the knee? A systematic review. Semin Arthritis Rheum. 2013;43(2):187–194. [DOI] [PubMed] [Google Scholar]
- 83. Liu WX, Zhao JZ, Huangfu XQ, He YH, Yang XG. Prevalence of bilateral involvement in patients with discoid lateral meniscus: a systematic literature review. Acta Orthop Belg. 2016;83(1):153–160. [PubMed] [Google Scholar]
- 84. Longo UG, Loppini M, Romeo G, Maffulli N, Denaro V. Histological scoring systems for tissue-engineered, ex vivo and degenerative meniscus. Knee Surg Sports Traumatol Arthrosc. 2013;21(7):1569–1576. [DOI] [PubMed] [Google Scholar]
- 85. Loras H, Osteras B, Torstensen TA, Osteras H. Medical exercise therapy for treating musculoskeletal pain: a narrative review of results from randomized controlled trials with a theoretical perspective. Physiother Res Int. 2015;20(3):182–190. [DOI] [PubMed] [Google Scholar]
- 86. Magnussen RA, Mansour AA, Carey JL, Spindler KP. Meniscus status at anterior cruciate ligament reconstruction associated with radiographic signs of osteoarthritis at 5- to 10-year follow-up: a systematic review. J Knee Surg. 2009;22(4):347–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Malmivaara A. Validity and generalizability of findings of randomized controlled trials on arthroscopic partial meniscectomy of the knee. Scand J Med Sci Sports. 2018;28(9):1970–1981. [DOI] [PubMed] [Google Scholar]
- 88. McLeod MM, Gribble P, Pfile KR, Pietrosimone BG. Effects of arthroscopic partial meniscectomy on quadriceps strength: a systematic review. J Sport Rehabil. 2012;21(3):285–295. [DOI] [PubMed] [Google Scholar]
- 89. Mehl J, Otto A, Baldino JB, et al. The ACL-deficient knee and the prevalence of meniscus and cartilage lesions: a systematic review and meta-analysis (CRD42017076897). Arch Orthop Trauma Surg. 2019;139(6):819–841. [DOI] [PubMed] [Google Scholar]
- 90. Monk P, Garfjeld Roberts P, Palmer AJ, et al. The urgent need for evidence in arthroscopic meniscal surgery. Am J Sports Med. 2017;45(4):965–973. [DOI] [PubMed] [Google Scholar]
- 91. Moran CJ, Busilacchi A, Lee CA, Athanasiou KA, Verdonk PC. Biological augmentation and tissue engineering approaches in meniscus surgery. Arthroscopy. 2015;31(5):944–955. [DOI] [PubMed] [Google Scholar]
- 92. Mosich GM, Lieu V, Ebramzadeh E, Beck JJ. Operative treatment of isolated meniscus injuries in adolescent patients: a meta-analysis and review. Sports Health. 2018;10(4):311–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Moulton SG, Bhatia S, Civitarese DM, et al. Surgical techniques and outcomes of repairing meniscal radial tears: a systematic review. Arthroscopy. 2016;32(9):1919–1925. [DOI] [PubMed] [Google Scholar]
- 94. Mutsaerts EL, van Eck CF, van de Graaf VA, Doornberg JN, van den Bekerom MP. Surgical interventions for meniscal tears: a closer look at the evidence. Arch Orthop Trauma Surg. 2016;136(3):361–370. [DOI] [PubMed] [Google Scholar]
- 95. Myers P, Tudor F. Meniscal allograft transplantation: how should we be doing it? A systematic review. Arthroscopy. 2015;31(5):911–925. [DOI] [PubMed] [Google Scholar]
- 96. Nepple JJ, Dunn WR, Wright RW. Meniscal repair outcomes at greater than five years: a systematic literature review and meta-analysis. J Bone Joint Surg Am. 2012;94(24):2222–2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Novaretti JV, Patel NK, Lian J, et al. Long-term survival analysis and outcomes of meniscal allograft transplantation with minimum 10-year follow-up: a systematic review. Arthroscopy. 2019;35(2):659–667. [DOI] [PubMed] [Google Scholar]
- 98. Noyes FR, Barber-Westin SD. A systematic review of the incidence and clinical significance of postoperative meniscus transplant extrusion. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):290–302. [DOI] [PubMed] [Google Scholar]
- 99. Noyes FR, Barber-Westin SD. Treatment of meniscus tears during anterior cruciate ligament reconstruction. Arthroscopy. 2012;28(1):123–130. [DOI] [PubMed] [Google Scholar]
- 100. O’Donnell K, Freedman KB, Tjoumakaris FP. Rehabilitation protocols after isolated meniscal repair: a systematic review. Am J Sports Med. 2017;45(7):1687–1697. [DOI] [PubMed] [Google Scholar]
- 101. Oh KJ, Sobti AS, Yoon JR, Ko YB. Current status of second-look arthroscopy after meniscal allograft transplantation: review of the literature. Arch Orthop Trauma Surg. 2015;135(10):1411–1418. [DOI] [PubMed] [Google Scholar]
- 102. Papalia R, Del Buono A, Osti L, Denaro V, Maffulli N. Meniscectomy as a risk factor for knee osteoarthritis: a systematic review. Br Med Bull. 2011;99:89–106. [DOI] [PubMed] [Google Scholar]
- 103. Papalia R, Franceschi F, Diaz Balzani L, et al. Scaffolds for partial meniscal replacement: an updated systematic review. Br Med Bull. 2013;107:19–40. [DOI] [PubMed] [Google Scholar]
- 104. Paxton ES, Stock MV, Brophy RH. Meniscal repair versus partial meniscectomy: a systematic review comparing reoperation rates and clinical outcomes. Arthroscopy. 2011;27(9):1275–1288. [DOI] [PubMed] [Google Scholar]
- 105. Pereira H, Frias AM, Oliveira JM, Espregueira-Mendes J, Reis RL. Tissue engineering and regenerative medicine strategies in meniscus lesions. Arthroscopy. 2011;27(12):1706–1719. [DOI] [PubMed] [Google Scholar]
- 106. Petersen W, Achtnich A, Lattermann C, Kopf S. The treatment of non-traumatic meniscus lesions. Deutsches Arzteblatt international. 2015;112(42):705–713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Phelan N, Rowland P, Galvin R, O’Byrne JM. A systematic review and meta-analysis of the diagnostic accuracy of MRI for suspected ACL and meniscal tears of the knee. Knee Surg Sports Traumatol Arthrosc. 2016;24(5):1525–1539. [DOI] [PubMed] [Google Scholar]
- 108. Poulsen E, Goncalves GH, Bricca A, et al. Knee osteoarthritis risk is increased 4-6 fold after knee injury—a systematic review and meta-analysis Br J Sports Med. 2019;53(23):1454–1463. [DOI] [PubMed] [Google Scholar]
- 109. Puig S, Kuruvilla YC, Ebner L, Endel G. Magnetic resonance tomography of the knee joint. Skeletal Radiol. 2015;44(10):1427–1434. [DOI] [PubMed] [Google Scholar]
- 110. Ranmuthu CDS, Ranmuthu CKI, Russell JC, Singhania D, Khan WS. Are the biological and biomechanical properties of meniscal scaffolds reflected in clinical practice? A systematic review of the literature. Int J Mol Sci. 2019;20(3):632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Reid CR, Bush PM, Cummings NH, McMullin DL, Durrani SK. A review of occupational knee disorders. J Occup Rehabil. 2010;20(4):489–501. [DOI] [PubMed] [Google Scholar]
- 112. Rongen JJ, Hannink G, van Tienen TG, van Luijk J, Hooijmans CR. The protective effect of meniscus allograft transplantation on articular cartilage: a systematic review of animal studies. Osteoarthritis Cartilage. 2015;23(8):1242–1253. [DOI] [PubMed] [Google Scholar]
- 113. Rosso F, Bisicchia S, Bonasia DE, Amendola A. Meniscal allograft transplantation: a systematic review. Am J Sports Med. 2015;43(4):998–1007. [DOI] [PubMed] [Google Scholar]
- 114. Rothermel SD, Smuin D, Dhawan A. Are outcomes after meniscal repair age dependent? A systematic review. Arthroscopy. 2018;34(3):979–987. [DOI] [PubMed] [Google Scholar]
- 115. Rothermich MA, Cohen JA, Wright R. Stable meniscal tears left in situ at the time of arthroscopic anterior cruciate ligament reconstruction: a systematic review. J Knee Surg. 2016;29(3):228–234. [DOI] [PubMed] [Google Scholar]
- 116. Salata MJ, Gibbs AE, Sekiya JK. A systematic review of clinical outcomes in patients undergoing meniscectomy. Am J Sports Med. 2010;38(9):1907–1916. [DOI] [PubMed] [Google Scholar]
- 117. Samitier G, Alentorn-Geli E, Taylor DC, et al. Meniscal allograft transplantation, part 2: systematic review of transplant timing, outcomes, return to competition, associated procedures, and prevention of osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):323–333. [DOI] [PubMed] [Google Scholar]
- 118. Sarraj M, Coughlin RP, Solow M, et al. Anterior cruciate ligament reconstruction with concomitant meniscal surgery: a systematic review and meta-analysis of outcomes. Knee Surg Sports Traumatol Arthrosc. 2019;27(11):3411–3452. [DOI] [PubMed] [Google Scholar]
- 119. Scholes C, Houghton ER, Lee M, Lustig S. Meniscal translation during knee flexion: what do we really know? Knee Surg Sports Traumatol Arthrosc. 2015;23(1):32–40. [DOI] [PubMed] [Google Scholar]
- 120. Seitz AM, Durselen L. Biomechanical considerations are crucial for the success of tendon and meniscus allograft integration—a systematic review. Knee Surg Sports Traumatol Arthrosc. 2019;27(6):1708–1716. [DOI] [PubMed] [Google Scholar]
- 121. Shakoor D, Kijowski R, Guermazi A, et al. Diagnosis of knee meniscal injuries by using three-dimensional MRI: a systematic review and meta-analysis of diagnostic performance. Radiology. 2019;290(2):435–445. [DOI] [PubMed] [Google Scholar]
- 122. Shanmugaraj A, Tejpal T, Ekhtiari S, et al. The repair of horizontal cleavage tears yields higher complication rates compared to meniscectomy: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2020;28(3):915–925. [DOI] [PubMed] [Google Scholar]
- 123. Shin YS, Lee HN, Sim HB, Kim HJ, Lee DH. Polyurethane meniscal scaffolds lead to better clinical outcomes but worse articular cartilage status and greater absolute meniscal extrusion. Knee Surg Sports Traumatol Arthrosc. 2018;26(8):2227–2238. [DOI] [PubMed] [Google Scholar]
- 124. Smith BE, Thacker D, Crewesmith A, Hall M. Special tests for assessing meniscal tears within the knee: a systematic review and meta-analysis. Evid Based Med. 2015;20(3):88–97. [DOI] [PubMed] [Google Scholar]
- 125. Smith C, McGarvey C, Harb Z, et al. Diagnostic efficacy of 3-T MRI for knee injuries using arthroscopy as a reference standard: a meta-analysis. AJR Am J Roentgenol. 2016;207(2):369–377. [DOI] [PubMed] [Google Scholar]
- 126. Smith NA, MacKay N, Costa M, Spalding T. Meniscal allograft transplantation in a symptomatic meniscal deficient knee: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):270–279. [DOI] [PubMed] [Google Scholar]
- 127. Smith NA, Parkinson B, Hutchinson CE, Costa ML, Spalding T. Is meniscal allograft transplantation chondroprotective? A systematic review of radiological outcomes. Knee Surg Sports Traumatol Arthrosc. 2016;24(9):2923–2935. [DOI] [PubMed] [Google Scholar]
- 128. Smuin DM, Swenson RD, Dhawan A. Saucerization versus complete resection of a symptomatic discoid lateral meniscus at short- and long-term follow-up: a systematic review. Arthroscopy. 2017;33(9):1733–1742. [DOI] [PubMed] [Google Scholar]
- 129. Snoeker BA, Bakker EW, Kegel CA, Lucas C. Risk factors for meniscal tears: a systematic review including meta-analysis. J Orthop Sports Phys Ther. 2013;43(6):352–367. [DOI] [PubMed] [Google Scholar]
- 130. Sommerfeldt M, Raheem A, Whittaker J, Hui C, Otto D. Recurrent instability episodes and meniscal or cartilage damage after anterior cruciate ligament injury: a systematic review. Orthop J Sports Med. 2018;6(7):2325967118786507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Spang RC III, Nasr MC, Mohamadi A, et al. Rehabilitation following meniscal repair: a systematic review. BMJ Open Sport Exerc Med. 2018;4(1):e000212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Swart NM, van Oudenaarde K, Reijnierse M, et al. Effectiveness of exercise therapy for meniscal lesions in adults: a systematic review and meta-analysis. J Sci Med Sport. 2016;19(12):990–998. [DOI] [PubMed] [Google Scholar]
- 133. Tark JY, Jeong JY, Lee M, et al. Early assessment and prediction of potential impact of the implantation of polyurethane scaffold in partial meniscal lesions: a pilot horizon scanning activity in South Korea. Int J Technol Assess Health Care. 2015;31(6):380–389. [DOI] [PubMed] [Google Scholar]
- 134. Thorlund JB, Ostengaard L, Cardy N, et al. Trajectory of self-reported pain and function and knee extensor muscle strength in young patients undergoing arthroscopic surgery for meniscal tears: a systematic review and meta-analysis. J Sci Med Sport. 2017;20(8):712–717. [DOI] [PubMed] [Google Scholar]
- 135. Troupis JM, Batt MJ, Pasricha SS, Saddik D. Magnetic resonance imaging in knee synovitis: clinical utility in differentiating asymptomatic and symptomatic meniscal tears. J Med Imaging Radiat Oncol. 2015;59(1):1–6. [DOI] [PubMed] [Google Scholar]
- 136. VanderHave KL, Perkins C, Le M. Weightbearing versus nonweightbearing after meniscus repair. Sports Health. 2015;7(5):399–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Vascellari A, Rebuzzi E, Schiavetti S, Coletti N. All-inside meniscal repair using the FasT-Fix meniscal repair system: is still needed to avoid weight bearing? A systematic review. Musculoskelet Surg. 2012;96(3):149–154. [DOI] [PubMed] [Google Scholar]
- 138. Warth RJ, Rodkey WG. Resorbable collagen scaffolds for the treatment of meniscus defects: a systematic review. Arthroscopy. 2015;31(5):927–941. [DOI] [PubMed] [Google Scholar]
- 139. Waugh N, Mistry H, Metcalfe A, et al. Meniscal allograft transplantation after meniscectomy: clinical effectiveness and cost-effectiveness. Knee Surg Sports Traumatol Arthrosc. 2019;27(6):1825–1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Wei G, Liang J, Ru N, et al. Comparison of medial versus lateral meniscus allograft transplantation: literature review and meta-analysis. Saudi Med J. 2016;37(6):613–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Westermann RW, Duchman KR, Amendola A, Glass N, Wolf BR. All-inside versus inside-out meniscal repair with concurrent anterior cruciate ligament reconstruction: a meta-regression analysis. Am J Sports Med. 2017;45(3):719–724. [DOI] [PubMed] [Google Scholar]
- 142. Xia XP, Chen HL, Zhou B. Ultrasonography for meniscal injuries in knee joint: a systematic review and meta-analysis. J Sports Med Phys Fitness. 2016;56(10):1179–1187. [PubMed] [Google Scholar]
- 143. Xu C, Zhao J. A meta-analysis comparing meniscal repair with meniscectomy in the treatment of meniscal tears: the more meniscus, the better outcome? Knee Surg Sports Traumatol Arthrosc. 2015;23(1):164–170. [DOI] [PubMed] [Google Scholar]
- 144. Zaffagnini S, Grassi A, Marcheggiani Muccioli GM, et al. MRI evaluation of a collagen meniscus implant: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23(11):3228–3237. [DOI] [PubMed] [Google Scholar]