Abstract
Context:
High blood pressure is one of the leading preventable causes of cardiovascular death worldwide. In this regard, several studies have shown interest in the benefits of isometric exercise on blood pressure regulation.
Objective:
To assess whether low-intensity isometric handgrip exercise (LI-IHE) is an effective strategy to lower blood pressure levels in prehypertensive and hypertensive patients.
Data Source:
This study was conducted according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement and registered with PROSPERO. Potentially eligible studies were identified after a systematic search conducted on 4 international databases: PubMed, Cochrane Central Register of Controlled Trials (CENTRAL), PEDro, and SPORTDiscus.
Study Selection:
We included randomized controlled trials that comprised patients who received LI-IHE.
Study Design:
Systematic review with meta-analysis.
Level of Evidence:
Level 3.
Data Extraction:
Data related to patient characteristics, exercise programs, risk-of-bias assessment, and outcomes of interest were systematically reviewed independently by 2 authors.
Results:
The following reductions (mean differences) were observed after LI-IHE: systolic blood pressure (SBP), (MD) = −5.43 mm Hg; (95% CI, −8.47 to −2.39; P = 0.0005); diastolic blood pressure (DBP), −2.41 mm Hg (95% CI, −4.33 to −0.48; P = 0.01); mean arterial pressure (MAP), −1.28 mm Hg (95% CI, −2.99 to 0.44; P = 0.14).
Conclusion:
LI-IHE seems to lower SBP, DBP, and MAP values in prehypertensive and hypertensive adults. It appears that LI-IHE reduces, in greater magnitude, blood pressure levels in hypertensive patients, specifically in patients aged <45 years, those who are overweight, and those on medications. Nevertheless, substantial heterogeneity in the main results and in the analyses by subgroups generated uncertainty about the real reduction magnitude that LI-IHE can produce on blood pressure.
Keywords: blood pressure, handgrip, isometric training, systematic review, meta-analysis
High blood pressure, described as blood pressure levels above 140 mm Hg systolic and/or 90 mm Hg diastolic when resting, is one of the leading preventable causes of cardiovascular death worldwide.21 There is a strong, independent correlation between cardiovascular disease (CVD) morbidity and mortality and high blood pressure.9 The occurrence of hypertension is increasing globally12,39; it may affect over 1 billion people worldwide.39 This pathophysiological state specially affects the elderly.11 To diminish the risk of CVD, achieving optimal blood pressure levels is recommended.33 Several strategies have been suggested; however, performing significant lifestyle changes is one of the most relevant.11,33 In this regard, physical activity plays a crucial role as a hypotensive agent.10,32 Recently, a meta-analysis in which 391 trials were considered concluded that physical activity treatment has shown the same effect as pharmacological treatment for lowering blood pressure in hypertensive patients (>140 mm Hg).29 In fact, when considering scientific data on this topic, different international organizations have recommended the inclusion of physical exercise as part of antihypertensive strategies.31,32 Previously published literature shows different types of exercises that could be effective as hypotensive agents.32 Furthermore, current international guidelines show the importance of physical exercise as a nonpharmacological way to control hypertension, the following being those with the most notable evidence: (1) aerobic: 90 to 150 min/wk, 65% to 75% heart rate reserve (maximum heart rate baseline or resting heart rate); (2) dynamic resistance training: 90 to 150 min/wk, 50% to 80% 1 repetition maximum, 6 exercises, 3 sets per exercise, 10 repetitions per set; (3) isometric resistance training (IRT): 4 × 2 minutes (handgrip), 1 minute rest, 30% to 40% maximal voluntary contraction (MVC), 3 days per week.1
In recent years, studies have documented that IRT results in greater hypotensive responses than other types of exercise.6,19 For instance, the meta-analysis by Cornelissen et al10 highlights that isometric exercise displays the most relevant reductions in systolic blood pressure (SBP) and diastolic blood pressure (DBP) levels when compared with other types of training: 10.9 and 6.2 mm Hg, respectively, in adult hypertensive patients who were not suffering from cardiovascular or other diseases. The isometric protocol or doses have been already established by Millar et al,28 who reported that effective interventions should be characterized by (1) 4 × 2 minutes (with 1-4 min rest) of 20% to 50% of the MVC, (2) 3 to 4 days per week for at least 4 to 10 weeks, and (3) being able to carry out lower limb (eg, leg press or squat) or upper limb (eg, handgrip) exercises. Since then, several studies have shown interest in the benefits of isometric exercise on the hemodynamic response, and different reviews and meta-analyses have collected data about the benefits and blood pressure regulation provided by isometric exercise.4,6,19,20,24,28,31
On the other hand, the physiological mechanisms that explain the reduction of blood pressure using isometric exercise remain unknown,28 although they may be associated with the release of endothelial substances that favor vasodilation.34 Therefore, it is convenient to persist researching this method of exercise, particularly on the type of dose that is the most appropriate in different groups of patients.
There is a lack of analyses concerning low-intensity isometric handgrip exercise (LI-IHE) in different population groups regarding age, body mass index (BMI), blood pressure status, or use of antihypertensive medication.20 These data could explain whether there are confusing variables on the hypotensive effects of LI-IHE. Therefore, the aim of this systematic review and meta-analysis was to assess whether LI-IHE is an effective strategy for lowering blood pressure in prehypertensive and hypertensive patients.
Methods
This systematic review and meta-analysis was carried out following the PRISMA (Preferred Reporting Items for Systematic Meta-Analyses) statement criteria and recommendations.23 This study was registered with PROSPERO on March 20, 2019 (CRD42019125235).
Inclusion and Exclusion Criteria
The studies considered for this review met the following inclusion criteria: (1) randomized controlled trials (RCTs) including patients who received LI-IHE; (2) involved patients diagnosed with prehypertension or hypertension; (3) involved male and female patients, aged ≥18 years; (4) reported ≤50% MVC intensity; and (5) involved ≥6 weeks of training with at least 2 days per week. Articles were excluded if they (1) were RCTs on pregnant women; (2) were RCTs that did not perform the IRT with handgrip; (3) were RCTs in progress; or (4) did not report original data (eg, editorial).
Search Strategy
Potentially eligible studies were identified after a systematic search was conducted on 4 international databases: PubMed, Cochrane Central Register of Controlled Trials (CENTRAL), PEDro, and SPORTDiscus. No restrictions were set to either publication period or language. The search strategy contained keywords, Medical Subject Headings terms, and Boolean connectors as follows: isometric handgrip OR handgrip OR isometric strength OR hand-gripping OR handgrips AND blood pressure OR hypertension OR hypertensive OR high blood pressure. Specific filters were applied for each database (“randomized controlled trials” and “performed in humans”). Likewise, reference lists of the resulting articles were reviewed to identify potentially eligible studies within the inclusion criteria.
Data Collection and Risk-of-Bias Assessment
Participant characteristics (ie, age, sex, BMI, training status, baseline blood pressure values, and medication type), exercise dose, and outcomes of interest were systematically and independently reviewed by the authors. To follow the criteria and recommendations in the PRISMA statement and the Cochrane Handbook for Systematic Reviews of Interventions, the post hoc decision was made to use the risk-of-bias tool of the Cochrane Collaboration17,23; previously in the protocol it was described that the PEDro scale would be used.16 The authors worked independently to assess the risk of bias by using criteria described in the Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0.17 This set of criteria is based on evidence of associations between potential overestimation of effect and the level of risk of bias of the article that may be due to aspects of sequence generation, allocation concealment, blinding, incomplete outcome data, and selective reporting. Each criterion was rated as low, high, or unclear risk of bias.
Studies Included
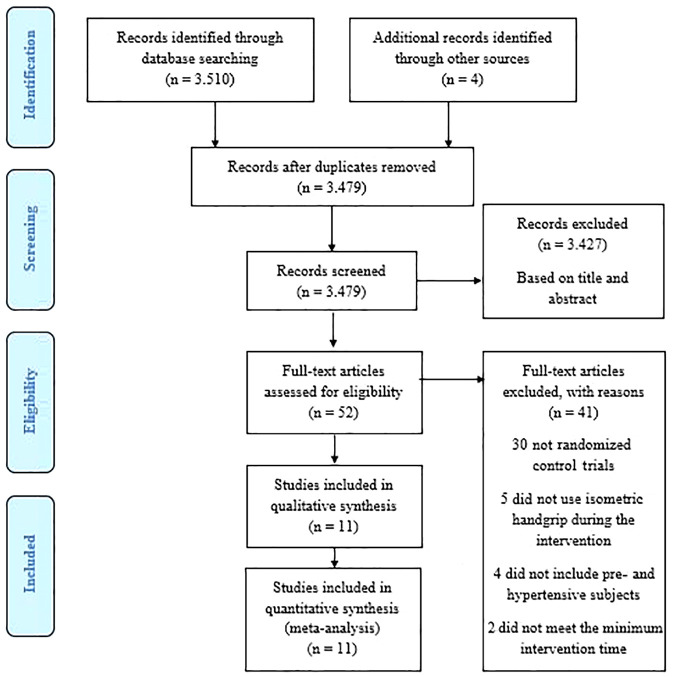
Initial database searches yielded a total of 3510 articles. After screening by title and abstract, and then removing duplicates, a total of 3427 research papers were discarded, thus obtaining a total of 52 RCTs for full-text review. Subsequently, after reviewing reference lists, 4 articles were included for full-text reading (Figure 1).
Figure 1.
Flowchart of study following the PRISMA (Preferred Reporting Items for Systematic Meta-Analyses) guidelines.
Data Synthesis
Information on the outcomes of interest was stored in a database. The main results for this study were SBP, DBP, and mean arterial pressure (MAP).
Statistical Analysis
For continuous outcomes, the group size, the mean values, and the standard deviations were recorded for each group compared in the included studies. Pooled effects were calculated using an inverse of variance model, and the data were pooled to generate a weighted mean difference (mm Hg) with corresponding 95% CIs. All the studies for each outcome reported data in the same units, so it was possible to pool all studies regardless of whether they reported changes in between data at baseline and final data. Significance was set at P < 0.05. Statistical heterogeneity was evaluated using the I2 statistic and classified according to the Cochrane Handbook17: negligible heterogeneity, 0% to 40%; moderate heterogeneity, 30% to 60%; substantial heterogeneity, 50% to 90%; and considerable heterogeneity, 75% to 100%. Other possible sources of heterogeneity were evaluated via subgroup analysis. A random-effects model was used. Subject to data availability, the following subgroup analyses were conducted: prehypertensive, hypertensive, normal weight, overweight, obese, age ≥45 years, age <45 years, and medicated participants. All analyses were performed by a single reviewer using Review Manager (RevMan Version 5.3; The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) and checked against the extracted data by the other author.
Results
Study Characteristics
In total, 11 studies were included in the qualitative and quantitative analyses, with a total of 13 intervention groups and 311 participants (intervention groups, n = 174; control groups, n = 137).2,7,13-15,25,27,30,35,36,38 Ten studies were RCTs with parallel group design.2,7,13-15,25,30,35,36,38 In particular, 1 study reported a parallel group design27; however, no random assignments were performed. Seven studies included hypertensive patients,7,13,15,25,35,37,38 while 4 articles included prehypertensive men and women.2,14,27,30 One study included patients of normal weight,2 while 4 research papers included overweight individuals,14,15,27,30 and 2 of the RCTs reported data on obese patients.7,35 Four studies reported insufficient data to categorize patients according to their BMI.13,25,36,38
Moreover, 10 articles reported on studies that recruited both male and female patients.2,7,13-15,25,27,30,35,36 The remaining study did not report the sex of the patients included.38 Regarding age, 8 studies provided data of individuals aged ≥45 years7,13,15,25,27,30,35,36 and 3 RTCs included patients aged <45 years.2,14,38 In addition, 7 studies recruited medicated individuals.7,13,25,27,30,35,36 In particular, 4 studies did not report whether patients took medication.2,14,15,38 Additionally, 2 studies measured blood pressure with brachial oscillometry,25,35 while 3 others reported blood pressure measurement using a sphygmomanometer.15,36,38 Four studies measured variables of interest with an automatic monitor,2,13,14,30 while 1 study did so with a finometer.7 The remaining study did not report a blood pressure measurement method.27 To conclude, 3 studies included physically active patients.25,30,36 while 3 recruited sedentary patients.2,13,14 The remaining RCTs did not describe whether patients were either sedentary or physically active.7,15,27,35,38 See Appendix 1, available in the online version of this article.
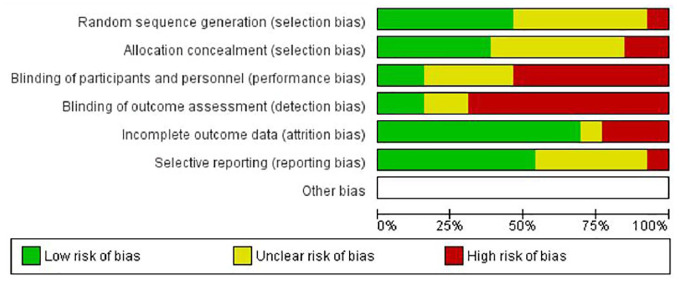
Risk-of-Bias Assessment
Only 5 studies reported the random sequence generation and were judged with a low risk of bias7,13,14,30,35; also, 5 RCTs were judged with an unclear risk of bias2,15,25,36,38 and the remaining study with a high risk of bias.27 Furthermore, 4 of the included studies reported a valid method of allocation concealment7,13,14,35; nevertheless, for this domain, 5 studies were judged with an unclear risk of bias,2,15,25,30,36 while 2 had a high risk of bias.27,38 Also, only 1 study reported blinding of outcome assessors.13 For this same domain, 2 were judged with an unclear risk of bias14,35 and the remaining 8 with a high risk of bias.2,7,15,25,27,30,36,38 Two RCTs describe the blinding of staff and study participants,7,30 6 had a high risk of bias,2,15,25,27,36,38 and 3 had an unclear risk of bias.13,14,35 On the other hand, 7 studies were judged with a low risk of bias with respect to the domain of incomplete data,2,7,13,15,25,27,30 3 were judged with a high risk of bias,14,35,38 and the remaining with an unclear risk of bias.36 Finally, 6 RCTs were judged with a low risk of bias with reference to the selective report,7,13,14,25,30,38 4 reported having unclear risk of bias,15,27,35,36 and 1 study was judged with a high risk of bias.2 Figure 2 presents further details on the risk of bias of the studies.
Figure 2.
Risk of bias graph: review authors’ judgments about each risk of bias item presented as percentages across all included studies.
Primary Analyses
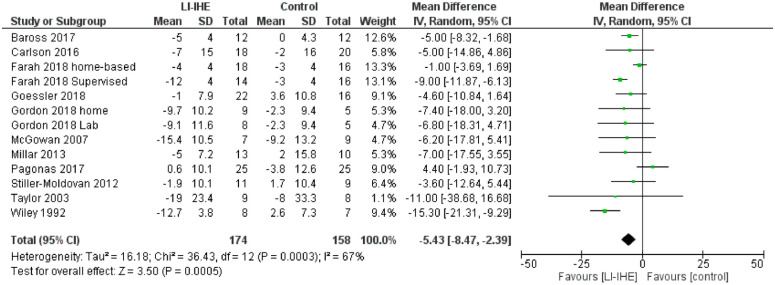
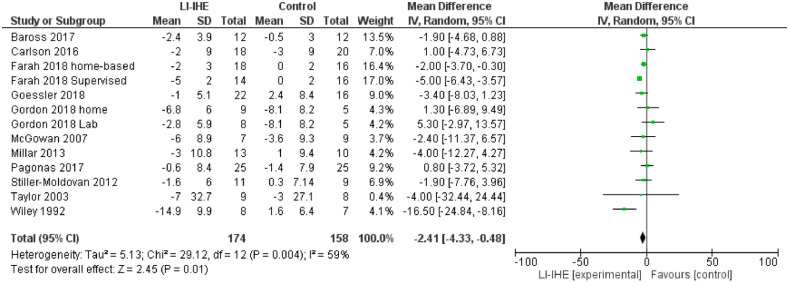
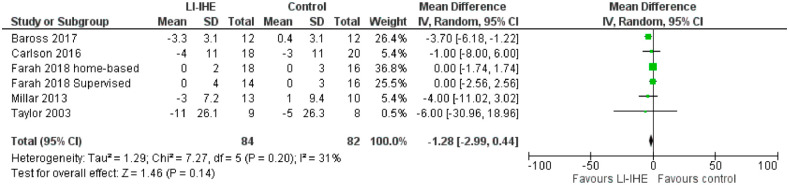
LI-IHE showed statistically significant reductions in SBP (mean difference [MD] = −5.43 mm Hg; 95% CI, –8.47 to −2.39, P = 0.0005; I2 = 67%), and DBP (MD = −2.41 mm Hg; 95% CI, –4.33 to −0.48, P = 0.01; I2 = 59%), as compared to the control group. MAP showed reductions but these were not statistically significant (MD = −1.28 mm Hg; 95% CI, –2.99 to 0.44, P = 0.14; I2 = 31%) (Figures 3, 4, and 5, respectively).
Figure 3.
Effect of LI-IHE on systolic blood pressure (mm Hg). IV, inverse variance; LI-IHE, low-intensity isometric handgrip exercise.
Figure 4.
Effect of LI-IHE on diastolic blood pressure (mm Hg). IV, inverse variance; LI-IHE, low-intensity isometric handgrip exercise.
Figure 5.
Effect of LI-IHE on mean arterial pressure (mm Hg). IV, inverse variance; LI-IHE, low-intensity isometric handgrip exercise.
Subgroup Analysis
Hypertensive Status
MAP (MD = −3.73 mm Hg; 95% CI, −6.07 to −1.39; P = 0.002; I2 = 0) was significantly reduced in prehypertensive patients. In prehypertensive patients, SBP and DBP did not decrease in a statistically significant manner (P = 0.24, I2 = 59% and P = 0.92, I2 = 0%, respectively). Particularly, in hypertensive subjects, only the SBP had a significant decrease (MD = −6.92 mm Hg; 95% CI, –11.09 to −2.76; P = 0.001; I2 = 70%). DBP and MAP did not decrease significantly (P = 0.06, I2 = 68% and P = 0.93, I2 = 0%, respectively).
Body Mass Index
In patients of normal weight, LI-IHE had a statistically significant decrease in SBP (MD = −5.00 mm Hg; 95% CI, –8.32 to −1.68; P = 0.003). Nevertheless, DBP did not decrease significantly. In overweight individuals, the SBP (P = 0.21; I2 = 43%) and DBP (P = 0.58; I2 = 49%) did not decrease in a statistically significant manner. Equally, SBP and DBP did not have a significant decrease in obese patients (P = 0.21, I2 = 0 and P = 0.84, I2 = 0, respectively). Unfortunately, data were insufficient to report effects on MAP for a BMI analysis.
Age
In subjects aged ≥45 years, LI-IHE produced statistically significant reductions in SBP (MD = −4.28 mm Hg; 95% CI, −7.98 to −0.57; P = 0.02; I2 = 63%). On the other hand, LI-IHE did not cause a significant decrease in DBP (P = 0.10; I2 = 51%) and MAP (P = 0.76; I2 = 0%). Both SBP (MD = −8.08 mm Hg; 95% CI, −14.45 to −1.71; P = 0.01; I2 = 78%) and MAP (MD = −3.70 mm Hg; 95% CI, −6.18 to −1.22; P = 0.003) had a statistically significant reduction in patients aged <45 years. For patients aged <45 years, LI-IHE lowered DBP (MD = −6.20 mm Hg; 95% CI, −12.49 to 0.35). Nonetheless, this reduction was not statistically significant (P = 0.06; I2 = 81%).
Antihypertensive Medication Status
In medicated individuals, LI-IHE significantly lowered DBP (MD = −2.43 mm Hg; 95% CI, −4.40 to −0.45; P = 0.02; I2 = 47%). Meanwhile, SBP and MAP did not have a statistically significant decrease (P = 0.08; I2 = 71% and P = 0.76, I2 = 0%, respectively). All the results of the analysis by subgroups are listed in Appendix 2 (available online).
Discussion
The main findings of this systematic review and subsequent meta-analysis report that, apparently, LI-IHE is a sufficient stimulus to reduce blood pressure levels in prehypertensive and hypertensive patients. Nevertheless, substantial heterogeneity is present, which is also statistically significant for SBP and DBP, generating a high degree of uncertainty about the true effect of LI-IHE on blood pressure.18
In general, possible causes of heterogeneity were studied with subgroup analyses previously reported in the protocol.17,18 However, when grouping the studies by blood pressure levels, BMI (overweight), age (patients aged ≥45 years or <45 years), and consumption of antihypertensive medication, moderate and substantial heterogeneity was also generated for SBP and DBP, which was also statistically significant. Particularly, in the subgroups of prehypertensive and hypertensive, the results for MAP did not show heterogeneity, possibly because of the low number of studies in each subgroup (prehypertensive, n = 2; hypertensive, n = 3). Likewise, in the subgroup of obese patients, the results for SBP and DBP did not report heterogeneity for the same reason described above (obese, n = 2).
Apparently, methodological diversity would be the cause of the heterogeneity between the studies of this research, mainly due to the nonreporting or performance of allocation concealment, as well as therapist and assessor blinding of the outcomes.17 Nevertheless, similar results to those of other studies with a similar methodological design were obtained, even with the same levels of heterogeneity over the main results and those reported in the subgroup analyses.6,19,20,24,34
In addition, this research reported statistically significant and clinically relevant reductions in SBP (−5.43 mm Hg; P < 0.0005) and DBP (−2.41 mm Hg; P = 0.01). Nowadays, it is known that a reduction of 5 mm Hg for SBP is associated with a decline in the risk of death due to stroke by 14%, due to coronary heart disease by 9%, and due to all causes by 7%.22,28,37 Likewise, a reduction of 2 mm Hg DBP reduces the prevalence of hypertension by 17% and reduces both the incidence of stroke-related events by 15% and of coronary heart disease by 6%.8 Furthermore, to our knowledge, this is the first systematic review and meta-analysis that studied the effects of LI-IHE only in prehypertensive and hypertensive patients. Particularly, previous research included studies with normotensive, prehypertensive, and hypertensive patients.20
Hypertensive Status
A study conducted in 2007 concluded that there is an inverse relationship between patients with the highest levels of blood pressure and LI-IHE.26 In general, those with higher blood pressure levels reduced SBP and DBP in greater magnitude.26 The results of this research showed that, in prehypertensive patients, LI-IHE lowered MAP to a statistically significant magnitude; however, SBP and DBP were not reduced significantly. Particularly, in hypertensive individuals, only SBP was significantly reduced, while in this same population, LI-IHE did not reduce DBP and MAP in a statistically significant manner. Furthermore, similar data were reported in a meta-analysis where IRT generated reductions of greater magnitude in SBP, DBP, and MAP in hypertensive patients, compared with individuals who had normal blood pressure levels.6
Additionally, the results of recently published research showed that in hypertensive patients, IRT generated larger decreases in MAP when compared with normotensive patients (−5.91 mm Hg vs −3.01 mm Hg).19 In this same study, SBP and DBP were significantly reduced in hypertensive patients.19 Likewise, an analysis by subgroups reported in a systematic review showed statistically significant and clinically important decreases generated by LI-IHE on SBP and DBP in prehypertensive and hypertensive patients.20 On the other hand, another study described larger reductions generated by the IRT on SBP and DBP in favor of normotensive patients when compared with those reported in hypertensive individuals.24
Body Mass Index
In both men and women, a higher BMI increased SBP. In women with a BMI ≥30 kg/m2, SBP showed higher values (~11 mm Hg) compared to women categorized with a BMI ≤25 kg/m2 (116 vs 127 mm Hg, respectively). Likewise, men categorized with a high BMI (≥30 kg/m2) reported higher SBP values (~9 mm Hg) when compared to those with a BMI≤25 kg/m2 (131 vs 121 mm Hg).5 The analysis by subgroups of this research showed that LI-IHE significantly reduced SBP in patients with normal weight. However, analyses in patients with normal weight only included 1 research.2 On the other hand, in overweight individuals, LI-IHE significantly decreased SBP. Nevertheless, DBP did not show significant changes. LI-IHE did not decreased statistically significantly SBP and DBP. Likewise in obese patients, LI-IHE did not show significant changes in SBP and DBP. There are few scientific studies that have studied the effects of LI-IHE on the blood pressure of patients with different levels of BMI and diagnosed with prehypertension or hypertension. In comparison with the current state of science, a systematic review from subgroup analysis reported that IRT did not generate significant reductions in SBP, DBP, and MAP in patients with different BMI categories when they were compared with each other.34 Additionally, an experiment performed on overweight patients who underwent IRT reported significant reductions in SBP and MAP; however, DBP was not reduced in a statistically significant manner.3
Age
There is a strong correlation between rise in blood pressure due to age and mortality by stroke, ischemic heart disease, and other causes of vascular death.22 However, the results of this systematic review and meta-analysis showed that patients aged ≥45 years had a statistically significant decrease in SBP (−4.28 mm Hg; P = 0.02). In contrast, a meta-analysis from 2016 studied subgroups composed of patients aged ≥45 years, where statistically significant decreases were found for SBP, DBP, and MAP.19 Meanwhile, the results of our research showed no statistically significant reductions in DBP and MAP in patients with the same age range (DBP ≥45-year-olds, P = 0.10; MAP ≥45-year-olds, P = 0.76). Furthermore, 1 meta-analytic review reported statistically significant reductions in SBP, DBP, and MAP in patients aged ≥45 years.24 Likewise, this study reported statistically significant reductions in SBP, DBP, and MAP in patients aged <45 years.24 In addition to this, the current research reports that LI-IHE significantly lowers SBP and MAP in patients aged <45 years. These data are similar to those reported in a systematic review and meta-analysis that found a statistically significant reduction for MAP in patients aged <45 years.19 The same research found no statistically significant reductions for SBP and DBP in individuals with the same age range after undergoing isometric training with different types of exercises.19
Antihypertensive Medication Status
In particular, patients with higher blood pressure levels obtain the greatest benefits from LI-IHE, showing reductions of greater magnitude even in medicated individuals.26 The results of this systematic review and meta-analysis showed statistically significant reductions on DBP in patients medicated after the intervention with LI-IHE, while SBP and MAP were not significantly reduced. Contrasting with current scientific evidence, recent data reported statistically significant reductions in SBP after IRT interventions.34 Moreover, another meta-analysis showed a statistically significant reduction in SBP and DBP in medicated hypertensive patients after undergoing interventions with LI-IHE.20 Another study reported statistically significant decreases in SBP, DBP, and MAP in medicated patients undergoing different IRT exercises.6 It seems that LI-IHE significantly reduces DBP in prehypertensive and hypertensive medicated patients, and the data were corroborated with studies of similar methodological design.6,20 Nonetheless, this study did not show significant reductions for MAP in medicated patients after the intervention with LI-IHE, which differs from those reported in a meta-analysis.6 A possible reason for these findings is that this study combined data from research using IRT with different types of exercises.6
Limitations
There are several limitations to be considered in this systematic review and meta-analysis: (1) substantial and statistically significant heterogeneity were reported in primary outcome and subgroup analysis; (2) only 4 studies that were part of this research reported allocation concealment; (3) most RCTs included did not specify assessor blinding of outcomes; (4) only 2 primary research studies described whether there was blinding of participants and personnel of intervention; (5) a limited number of studies reporting data concerning patients with normal weight and obesity made it difficult to quantify the effect of LI-IHE on blood pressure in this type of population; (6) 4 clinical trials did not report whether the patients were taking antihypertensive medication during the intervention; and (7) in our analysis, we did not take into account ethnic demographic information. Because of these limitations, we recommend being prudent about the interpretation of these results. Besides, for primary research RCTs, we recommend performing and adequately describing allocation concealment, in addition to blinding main researchers and outcome assessors. On the other hand, it is suggested to conduct future systematic reviews to evaluate, with statistical methods such as meta-regression (if available), the possible causes of heterogeneity from methodological variables of primary research (such as concealing allocation, blinding therapists and assessors outcomes), since meta-analyses with similar topics reported substantial heterogeneity in their main results (SBP, DBP, and MAP) and mostly performed similar analyses for subgroups also reporting significant heterogeneity.6,19,20,24
Conclusion
LI-IHE seems to reduce the values of SBP, DBP, and MAP in prehypertensive and hypertensive adults. Nevertheless, substantial heterogeneity in the main results and in the analyses by subgroups generated uncertainty about the real reduction magnitude LI-IHE can produce on blood pressure. For this reason, we suggest that the scientific community be cautious with the interpretation of these results. The magnitude of the reductions reported in this research was similar to those generated by aerobic exercise, dynamic resistance training, and IRT performed in the lower kinetic chain, although it is necessary to improve the methodological quality of primary research for future systematic reviews with the aim of achieving more precise results. Finally, a robust body of evidence currently suggests that LI-IHE should be considered as a complementary therapy in the prevention, control, and clinical treatment of hypertension.
Supplemental Material
Supplemental material, Appendix_1 for Is Low-Intensity Isometric Handgrip Exercise an Efficient Alternative in Lifestyle Blood Pressure Management? A Systematic Review by Andrés F. Loaiza-Betancur and Iván Chulvi-Medrano in Sports Health: A Multidisciplinary Approach
Supplemental material, Appendix_2 for Is Low-Intensity Isometric Handgrip Exercise an Efficient Alternative in Lifestyle Blood Pressure Management? A Systematic Review by Andrés F. Loaiza-Betancur and Iván Chulvi-Medrano in Sports Health: A Multidisciplinary Approach
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1. Bakris G, Ali W, Parati G. ACC/AHA versus ESC/ESH on hypertension guidelines: JACC guideline comparison. J Am Coll Cardiol. 2019;73:3018-3026. [DOI] [PubMed] [Google Scholar]
- 2. Baross AW, Hodgson DA, Padfield SL, Swaine IL. Reductions in resting blood pressure in young adults when isometric exercise is performed whilst walking. 2017;2017:7123834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Baross AW, Wiles JD, Swaine IL. Double-leg isometric exercise training in older men. Open Access J Sports Med. 2013;4:33-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bentley DC, Nguyen CH, Thomas SG. Resting blood pressure reductions following handgrip exercise training and the impact of age and sex: a systematic review and narrative synthesis. Syst Rev. 2018;7:229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Brown CD, Higgins M, Donato KA, et al. Body mass index and the prevalence of hypertension and dyslipidemia. Obes Res. 2000;8:605-619. [DOI] [PubMed] [Google Scholar]
- 6. Carlson DJ, Dieberg G, Hess NC, Millar PJ, Smart NA. Isometric exercise training for blood pressure management: a systematic review and meta-analysis. Mayo Clin Proc. 2014;89:327-334. [DOI] [PubMed] [Google Scholar]
- 7. Carlson DJ, Inder J, Palanisamy SK, McFarlane JR, Dieberg G, Smart NA. The efficacy of isometric resistance training utilizing handgrip exercise for blood pressure management: a randomized trial. Medicine. 2016;95:e5791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cook NR, Cohen J, Hebert PR, Taylor JO, Hennekens CH. Implications of small reductions in diastolic blood pressure for primary prevention. JAMA Intern Med. 1995;155:701-709. [PubMed] [Google Scholar]
- 9. Cornelissen VA, Fagard RH, Coeckelberghs E, Vanhees L. Impact of resistance training on blood pressure and other cardiovascular risk factors: a meta-analysis of randomized, controlled trials. Hypertension. 2011;58:950-958. [DOI] [PubMed] [Google Scholar]
- 10. Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta-analysis. J Am Heart Assoc. 2013;2:e004473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dregan A, Ravindrarajah R, Hazra N, Hamada S, Jackson SHD, Gulliford MC. Longitudinal trends in hypertension management and mortality among octogenarians: prospective cohort study. Hypertension. 2016;68:97-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Forouzanfar MH, Liu P, Roth GA, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mmHg, 1990-2015. JAMA. 2017;317:165-182. [DOI] [PubMed] [Google Scholar]
- 13. Farah BQ, Rodrigues SLC, Silva GO, et al. Supervised, but not home-based, isometric training improves brachial and central blood pressure in medicated hypertensive patients: a randomized controlled trial. Front Physiol. 2018;9:961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Goessler KF, Buys R, Vandertrappen D, Vanhumbeeck L, Cornelissen VA. A randomized controlled trial comparing home-based isometric handgrip exercise versus endurance training for blood pressure management. J Am Soc Hypertens. 2018;12:285-293. [DOI] [PubMed] [Google Scholar]
- 15. Gordon BDH, Thomas EV, Warren-Findlow J, et al. A comparison of blood pressure reductions following 12-weeks of isometric exercise training either in the laboratory or at home. J Am Soc Hypertens. 2018;12:798-808. [DOI] [PubMed] [Google Scholar]
- 16. Herbert R, Moseley A, Sherrington C. PEDro: a database of randomised controlled trials in physiotherapy. Health Inf Manag. 1998;28:186-188. [DOI] [PubMed] [Google Scholar]
- 17. Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration; 2011. [Google Scholar]
- 18. Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Testing for heterogeneity. BMJ. 2003;327:557-560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Inder JD, Carlson DJ, Dieberg G, McFarlane JR, Hess NCL, Smart NA. Isometric exercise training for blood pressure management: a systematic review and meta-analysis to optimize benefit. Hypertens Res. 2016;39:89-94. [DOI] [PubMed] [Google Scholar]
- 20. Jin YZ, Yan S, Yuan WX. Effect of isometric handgrip training on resting blood pressure in adults: a meta-analysis of randomized controlled trials. J Sports Med Phys Fitness. 2017;57:154-160. [DOI] [PubMed] [Google Scholar]
- 21. Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217-223. [DOI] [PubMed] [Google Scholar]
- 22. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903-1913. [DOI] [PubMed] [Google Scholar]
- 23. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1-e34. [DOI] [PubMed] [Google Scholar]
- 24. López-Valenciano A, Ruiz-Pérez I, Ayala F, Sánchez-Meca J, Vera-Garcia FJ. Updated systematic review and meta-analysis on the role of isometric resistance training for resting blood pressure management in adults. J Hypertens. 2019;37:1320-1333. [DOI] [PubMed] [Google Scholar]
- 25. McGowan CL, Visocchi A, Faulkner M, et al. Isometric handgrip training improves local flow-mediated dilation in medicated hypertensives. Eur J Appl Physiol. 2007;99:227-234. [DOI] [PubMed] [Google Scholar]
- 26. Millar PJ, Bray SR, McGowan CL, MacDonald MJ, McCartney N. Effects of isometric handgrip training among people medicated for hypertension: a multilevel analysis. Blood Press Monit. 2007;12:307-314. [DOI] [PubMed] [Google Scholar]
- 27. Millar PJ, Levy AS, McGowan CL, McCartney N, MacDonald MJ. Isometric handgrip training lowers blood pressure and increases heart rate complexity in medicated hypertensive patients. Scand J Med Sci Sports. 2013;23:620-626. [DOI] [PubMed] [Google Scholar]
- 28. Millar PJ, McGowan C, Cornelissen VA, Araujo CG, Swaine IL. Evidence for the role of isometric exercise training in reducing blood pressure: potential mechanisms and future directions. Sports Med. 2014;44:345-356. [DOI] [PubMed] [Google Scholar]
- 29. Naci H, Salcher-Konrad M, Dias S, et al. How does exercise treatment compare with antihypertensive medications? A network meta-analysis of 391 randomised controlled trials assessing exercise and medication effects on systolic blood pressure. Br J Sports Med. 2019;53:859-869. [DOI] [PubMed] [Google Scholar]
- 30. Pagonas N, Vlatsas S, Bauer F, et al. Aerobic versus isometric handgrip exercise in hypertension: a randomized controlled trial. J Hypertens. 2017;35:2199-2206. [DOI] [PubMed] [Google Scholar]
- 31. Pedersen BK, Saltin B. Exercise as medicine—evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports. 2015;25:1-72. [DOI] [PubMed] [Google Scholar]
- 32. Pescatello LS, MacDonald HV, Lamberti L, Johnson BT. Exercise for hypertension: a prescription update integrating existing recommendations with emerging research. Curr Hypertens Rep. 2015;17:87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Reboussin DM, Allen NB, Griswold ME, et al. Systematic review for the 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. J Am Coll Cardiol. 2018;71:2176-2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Smart NA, Way D, Carlson D, et al. Effects of isometric resistance training on resting blood pressure. J Hypertens. 2019;37:1927-1938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Stiller-Moldovan C, Kenno K, McGowan CL. Effects of isometric handgrip training on blood pressure (resting and 24 h ambulatory) and heart rate variability in medicated hypertensive patients. Blood Press Monit. 2012;17:55-61. [DOI] [PubMed] [Google Scholar]
- 36. Taylor AC, McCartney N, Kamath MV, Wiley RL. Isometric training lowers resting blood pressure and modulates autonomic control. Med Sci Sports Exerc. 2003;35:251-256. [DOI] [PubMed] [Google Scholar]
- 37. Whelton PK, He J, Appel LJ, et al. Primary prevention of hypertension: clinical and public health advisory from the National High Blood Pressure Education Program. JAMA. 2002;288:1882-1888. [DOI] [PubMed] [Google Scholar]
- 38. Wiley RL, Dunn CL, Cox RH, Hueppchen NA, Scott MS. Isometric exercise training lowers resting blood pressure. Med Sci Sports Exerc. 1992;24:749-754. [PubMed] [Google Scholar]
- 39. Zhou B, Bentham J, Di Cesare M, et al. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet. 2017;389:37-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Appendix_1 for Is Low-Intensity Isometric Handgrip Exercise an Efficient Alternative in Lifestyle Blood Pressure Management? A Systematic Review by Andrés F. Loaiza-Betancur and Iván Chulvi-Medrano in Sports Health: A Multidisciplinary Approach
Supplemental material, Appendix_2 for Is Low-Intensity Isometric Handgrip Exercise an Efficient Alternative in Lifestyle Blood Pressure Management? A Systematic Review by Andrés F. Loaiza-Betancur and Iván Chulvi-Medrano in Sports Health: A Multidisciplinary Approach