Abstract
Objective
We estimated the caseload of providers, practices, and clinics for psychosocial services (including psychotherapy) to Medicaid-insured children to improve the understanding of the current supply of such services and to inform opportunities to increase their accessibility.
Methods
We used 2012-2013 Medicaid claims data and data from the 2013 National Plan and Provider Enumeration System to identify and locate therapists, psychiatrists, and mental health centers along with primary, rehabilitative, and developmental care providers in the United States who provided psychosocial services to Medicaid-insured children. We estimated the per-provider, per-location, and state-level caseloads of providers offering these services to Medicaid-insured children in 34 states with sufficiently complete data to perform this analysis, by using the most recent year of Medicaid claims data available for each state. We measured caseload by calculating the number of psychosocial visits delivered by each provider in the selected year. We compared caseloads across states, urbanicity, provider specialty (eg, psychiatry, psychology, primary care), and practice setting (eg, mental health center, single practitioner).
Results
We identified 63 314 providers, practices, or centers in the Medicaid claims data that provided psychosocial services to Medicaid-insured children in either 2012 or 2013. The median provider-level per-year caseload was <25 children and <250 visits across all provider types. Providers with a mental health center–related taxonomy accounted for >40% of visits for >30% of patients. Fewer than 10% of providers and locations accounted for >50% of patients and visits.
Conclusions
Psychosocial services are concentrated in a few locations, thereby reducing geographic accessibility of providers. Providers should be incentivized to offer care in more locations and to accept more Medicaid-insured patients.
Keywords: Medicaid, psychosocial services, provider caseload
Mental health disorders are prevalent but undertreated among children.1 For common psychiatric disorders among children (eg, depression, anxiety disorder, attention deficit/hyperactivity disorder), psychotherapy and/or other psychosocial services are recommended as a first line of treatment.2-5 Guidelines from the National Institute of Mental Health specify that children with mental health and behavioral disorders should receive psychotherapeutic or psychosocial intervention and that psychotropic medication should be complemented by provision of these services.6 Several studies examined the efficacy of various psychosocial interventions.7-9 Two studies found that about 75% of persons undergoing psychotherapy showed improvement for their condition.10,11
Medicaid is the largest insurer of children12 and the single-largest payer of mental health services.13 Studies have documented that many Medicaid-insured children with mental health and behavioral disorders do not receive any psychosocial treatment, including psychotherapy.14-19 Only 49% of young persons aged ≤20 received psychosocial services before starting antipsychotics,20 and only 68% of children and adolescents aged 6-17 years received concurrent therapy.18 Fewer than 38% of children aged 6-12 years who initiated medication for attention deficit/hyperactivity disorder received any psychotherapy visits.14 Among children who initiate treatment, many do not receive a minimal number of psychotherapy19,21 or psychosocial22,23 visits.
Several studies have posited lack of health care access as a major barrier to psychosocial services for this population. Not only is there an overall shortage of mental health providers in most states,24,25 but many mental health providers do not accept Medicaid.25-27 A national survey of office-based psychiatrists found that the percentage of psychiatrists who accept Medicaid declined from 2010 to 2015, and only 35.4% accepted new Medicaid patients during the most recent period examined (2014-2015).27 Studies have also examined the geographic availability of mental health treatment facilities that accept Medicaid28,29 and/or serve children.30 Those studies reported that many communities lack these resources.
Although some studies have provided information about geographic availability and distribution of Medicaid-participating providers,28-30 these studies did not describe the volume of services provided at each location. Anecdotal evidence suggests that a small percentage of mental health treatment facilities and clinics may provide the majority of services to this population (ie, high-volume providers). These studies also focused on specialty mental health providers; however, psychosocial services can also be delivered in other settings such as primary care practices.31-34 To date, empirical data are lacking on how the supply of psychosocial services for Medicaid-enrolled children varies across provider types (eg, primary care, mental health specialists). A nuanced understanding has important implications for informing the accessibility of services for Medicaid-enrolled children.
To address this gap in the literature, our study linked 2 large national databases to conduct a comprehensive analysis on the supply of psychosocial services available to Medicaid-insured children across provider types and settings. Our objectives were to provide new information about who delivers psychosocial services to Medicaid-enrolled children and how visit volume is distributed across provider types and geography.
Methods
Data Sources
We used data from the 2013 National Plan and Provider Enumeration System (NPPES) database35 and 2012-2013 Medicaid Analytic eXtract (MAX) claims acquired from the Centers for Medicare & Medicaid Services (CMS).36 NPPES is a national database listing all health care providers with a National Provider Identifier (NPI) number. An NPI number can be assigned to a person (entity type 1) or an organization, such as a hospital or physician group (entity type 2). We used NPPES to determine whether a provider seeing Medicaid-insured children for psychosocial services specializes in a mental health–related field, as defined by the Health Resources and Services Administration,37 or another field, such as primary care, rehabilitative care, or developmental care. We considered providers who fell into 1 of the following 11 provider categories: psychiatrist, psychologist, counselor, social worker, mental health center, other entity 1 mental health, other entity 2 mental health, primary care, rehabilitative/developmental care, other care center (including general acute-care hospitals and federally qualified health centers), and other entity 2 related care. (A full description of taxonomies in each category is available from the authors upon request.) We included psychiatric hospitals and residential treatment facilities in the category of mental health center because they can have outpatient clients.38
For the MAX data, the most recent years of data available from CMS when this study began were 2013 for 28 states and 2012 for all states. We used information from the MAX Personal Summary file, which contains demographic data for Medicaid beneficiaries, and the MAX Other Therapy file, which contains claims for services received by Medicaid beneficiaries outside of inpatient hospitals, long-term care facilities, and pharmacies. We used Current Procedural Terminology (CPT) codes39 to identify health care encounters involving psychotherapy (including individual, group, or family psychotherapy) or other psychosocial services, such as skills training and development, psychosocial rehabilitation services, and activity therapy. The selected CPT codes are level 1 Healthcare Common Procedure Coding System codes that are based on codes used in a Centers for Disease Control and Prevention study.40 The Georgia Institute of Technology Institutional Review Board approved this study.
Linking the NPPES Provider Database to the MAX Claims Database
We developed an algorithm to link providers in the NPPES database with the health care data from the MAX Other Therapy file. The latter contains 2 separate identifiers for the billing provider (the NPI number and a unique Medicaid identification number) and 1 identifier for the service provider (a unique Medicaid identification number). We assumed the Medicaid beneficiary received services from the provider listed in the “service provider” field, which can differ from the provider listed in the “billing provider” field. For example, individual providers may work for a subsidiary organization but bill under the NPI number of a parent organization. Because the “service provider” field in the MAX data only contains the unique Medicaid identification number, we created an algorithm to match an NPI number to the service provider field using information from the billing provider fields. This algorithm is described hereinafter.
In step 1, if a service provider appeared as a billing provider in the MAX Other Therapy file, we assessed whether the claims for which he or she was the listed billing provider had the same NPI number. In this case, we considered that NPI number the “match.” This step produced 33% of all matches for psychosocial service providers.
If the service provider was not matched, in step 2 we assessed whether the billing NPI field was valid and identical in all claims in which he or she was listed as the service provider. If so, we considered that to be the matched NPI number (42% of all matches). If still not matched, in step 3, from among the claims in which he or she was the listed billing provider, we randomly selected a billing NPI number with a mental health–related primary taxonomy if one existed (3.4% of all matches). If not, we randomly selected a billing NPI number with a mental health–related primary taxonomy from his or her service provider claims (5.4% of all matches).
In our analysis, we included 21 states from 2013 and 13 additional states from 2012 (34 states total) for which we could match at least 75% of psychosocial service providers to a single NPI number in the NPPES database. States for which we could match <75% of psychosocial service providers to a single NPI number in the NPPES database either had a large number of service providers, each with multiple potential NPI numbers (eg, Indiana, Nebraska, Wyoming), or had a large number of billing NPI numbers not listed in the NPPES database and, therefore, service providers could not be matched to any NPI number (eg, Michigan, Missouri, New Hampshire).
Address Classification
To avoid a provider’s caseload being split between his or her own entity 1 NPI number and his or her organization’s entity 2 NPI number, we also grouped providers with the same practice address together and performed an address-level analysis. That is, for each address where at least 1 Medicaid psychosocial service provider practices, we took the following 3 steps: (1) we identified all providers in the 2013 NPPES database sharing that practice address, (2) we determined the provider category of each of those providers using their entity type and primary taxonomy, and (3) we categorized the practice setting of the address. We performed these steps in a hierarchical fashion based on the presence or absence of each provider category. For example, the presence of a mental health center provider resulted in a “mental health practice setting” categorization, whereas the presence of an “other” care center provider and absence of a mental health center provider resulted in an “other care center practice setting” categorization. Remaining categories were “mental health entity 2,” “entity 2 containing mental health entity 1 providers,” “primary/rehabilitative/developmental entity 2,” “multiple entity 1 mental health providers,” “single mental health provider,” and “primary/rehabilitative/developmental entity 1.”
Caseload Estimation
We measured the caseload of each Medicaid-participating provider delivering psychosocial services by estimating the number of Medicaid-enrolled children who received psychosocial services from that provider in a given year and adding all the psychosocial visits delivered by that provider. We obtained the unique address-level caseloads by combining the caseloads of all service providers practicing at the same address.
We examined state-level variations in the distribution of services across provider and location categories, as well as by practice location urbanicity. We determined urbanicity by using the zip code approximation of the rural–urban commuting area codes41: codes 1-3 represented large urban areas (ie, areas with a primary flow to or within an urbanized area), codes 4-6 represented small urban areas (ie, areas with a primary flow to or within a large urban cluster), and codes 7-10 represented rural areas.
Results
In the 34 states (21 states from 2013 and 13 states from 2012), we identified 83 727 mental health providers who provided psychosocial services to Medicaid-insured enrollees. Of these, 51 638 (61.7%) provided psychosocial services to Medicaid-insured children. We also identified 18 721 practitioners in related health care settings who provided psychosocial services to Medicaid-insured persons, 11 676 (62.4%) of whom served children. Combined, these providers saw more than 1.6 million Medicaid-insured children and provided more than 32 million psychosocial services visits to these children across 32 238 provider locations. Of these children, 60% were aged <13 and 91% had a mental health diagnosis.
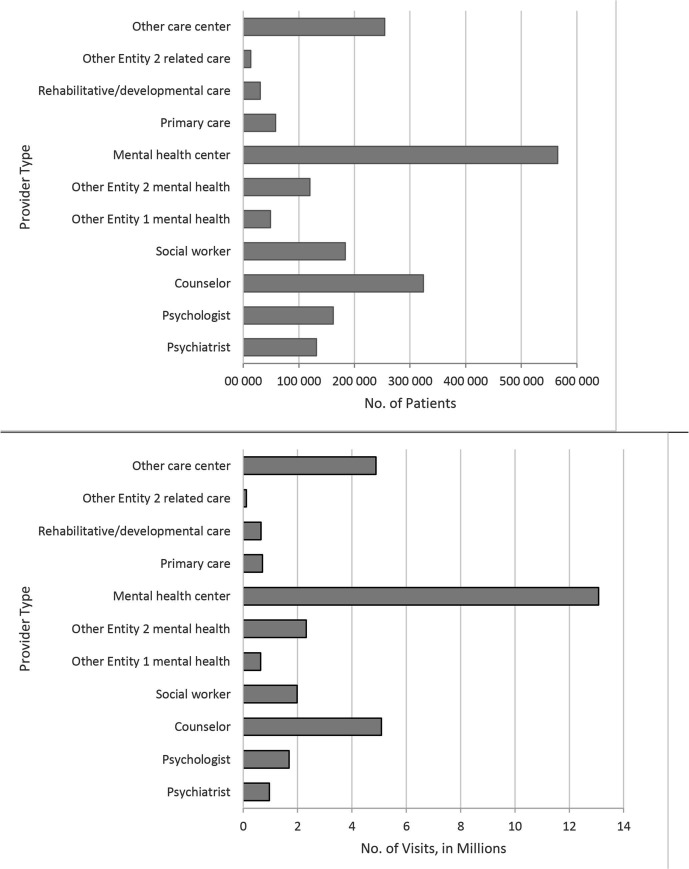
Mental health practitioners conducted more psychosocial treatments than non–mental health practitioners (Figure 1). More than one-third of children were treated at mental health centers, which accounted for >40% of mental health visits. Counselors, the largest group of the 11 provider types, treated 20% of children and accounted for 16% of mental health visits. Other care centers treated 16% of children and accounted for 15% of mental health visits.
Figure 1.
Total number of Medicaid-insured children seen for psychosocial services and their corresponding total number of psychosocial visits aggregated among 34 US states in 1 selected year (2012 or 2013), by provider category. Data source: Medicaid Analytic eXtract.36
More than 58% of psychosocial services occurred at addresses with at least 1 mental health center. In addition, about 21% of children were treated and 19% of visits took place at other care center locations. Only about 12% of children were treated at locations with entity 1 mental health providers but no organization NPI number. These locations were responsible for only 9% of visits.
State-Level Distribution of Services
The distribution of psychosocial services across provider and address categories varied considerably by state. The percentage of children who received psychosocial services from mental health centers ranged from 2.4% (Washington) to 81.8% (Kentucky), whereas the percentage of psychosocial service visits from mental health centers ranged from 1.2% (Iowa) to 86.8% (Kentucky). In Oklahoma and Texas, counselors treated the majority of children, whereas in Minnesota, psychologists treated the majority of children. In 3 states (Iowa, Illinois, and Washington), more children were treated by non–mental health providers than by mental health providers.
Aggregating services by location revealed that in more than half of the states, most services occurred at mental health center locations (Tables 1 and 2). However, large variations occurred. The percentage of children seeking psychosocial services at mental health center locations (vs other locations) ranged from 7.8% (Washington) to 88.6% (Kentucky). In Illinois, Iowa, Montana, and Washington, most children (54.5% to 87.2%) were treated in other care center locations. Only in Vermont were more than 50% of children seen at locations with entity 1 mental health providers but no entity 2 providers; however, only 28.2% of visits by children were made at those locations.
Table 1.
Distribution of Medicaid-insured child psychosocial patients across address categoriesa for 34 US states, in 2012 or 2013b
| State | Total no. of patients |
% of patients | |||||||
|---|---|---|---|---|---|---|---|---|---|
| MHC | OCC | MHE2 | CMH | MMH | SMH | PDE2 | PDE1 | ||
| Alabamac | 35 040 | 65.9 | 20.5 | 11.2 | 1.1 | 3.4 | 8.2 | 0.3 | 0.1 |
| Arizona | 56 045 | 77.0 | 22.9 | 2.9 | 0.2 | 0.1 | 0.3 | 0.3 | 0.02 |
| Connecticut | 29 903 | 51.4 | 36.2 | 12.2 | 7.2 | 5.5 | 6.7 | 0.1 | 0.3 |
| District of Columbiac | 5868 | 58.4 | 41.8 | 7.3 | 0 | 0.3 | 0.9 | 0 | 0 |
| Floridac | 80 695 | 47.0 | 20.5 | 12.6 | 4.4 | 11.7 | 14.6 | 2.5 | 4.6 |
| Georgia | 67 249 | 55.5 | 10.9 | 27.8 | 1.5 | 6.2 | 8.5 | 1.1 | 1.4 |
| Hawaii | 1551 | 56.0 | 44.7 | 0 | 0.7 | 0 | 0 | 0 | 0 |
| Idaho | 18 394 | 61.6 | 28.5 | 22.1 | 1.5 | 1.7 | 1.0 | 0.7 | 0 |
| Illinoisc | 115 650 | 29.6 | 70.5 | 1.8 | 0.7 | 0.8 | 2.3 | 0.5 | 5.6 |
| Iowa | 5667 | 17.5 | 81.5 | 1.7 | 0.4 | 0 | 0 | 3.2 | 0.3 |
| Kentuckyc | 50 774 | 88.6 | 4.5 | 6.2 | 1.7 | 2.1 | 0.2 | 0.3 | 0.2 |
| Louisiana | 39 574 | 68.7 | 17.6 | 8.1 | 3.2 | 4.0 | 6.0 | 0.2 | 0.7 |
| Marylandc | 39 829 | 65.7 | 23.0 | 8.5 | 1.3 | 3.5 | 6.6 | 0.1 | 0 |
| Massachusetts | 87 878 | 75.0 | 20.5 | 6.2 | 3.1 | 2.5 | 1.8 | 0.1 | 0 |
| Minnesota | 35 874 | 47.0 | 25.1 | 34.2 | 0.2 | 7.0 | 1.6 | 0.3 | 0.2 |
| Mississippi | 32 157 | 63.2 | 13.1 | 17.4 | 3.9 | 3.9 | 10.9 | 0 | 0 |
| Montanac | 10 465 | 25.5 | 54.5 | 18.1 | 2.5 | 12.1 | 11.2 | 0.6 | 1.3 |
| Nevadac | 10 025 | 85.5 | 12.8 | 24.7 | 6.7 | 3.3 | 21.5 | 1.5 | 27.7 |
| New Jersey | 31 482 | 73.8 | 13.8 | 16.8 | 0.7 | 0.8 | 3.3 | 0.1 | 0 |
| New Mexicoc | 37 938 | 45.4 | 36.2 | 25.0 | 0.9 | 3.3 | 6.5 | 0.9 | 1.0 |
| New York | 61 925 | 31.9 | 14.4 | 10.0 | 35.2 | 11.5 | 10.9 | 0.5 | 0.6 |
| North Carolinac | 78 468 | 42.0 | 16.8 | 24.1 | 6.0 | 5.6 | 19.3 | 2.7 | 1.0 |
| Ohio | 122 127 | 80.2 | 10.6 | 12.7 | 0.6 | 1.0 | 0.9 | 0.9 | 0.1 |
| Oklahoma | 98 125 | 52.7 | 7.4 | 31.5 | 2.5 | 10.3 | 23.5 | 0.0 | 0.8 |
| Oregon | 22 438 | 62.4 | 18.3 | 20.0 | 1.8 | 7.9 | 3.3 | 0.1 | 0 |
| Pennsylvania | 110 304 | 76.9 | 15.5 | 9.2 | 0.6 | 2.1 | 2.2 | 0.5 | 0.1 |
| Tennessee | 43 134 | 59.0 | 12.0 | 10.9 | 10.0 | 10.2 | 9.6 | 0.2 | 0.5 |
| Texasc | 145 564 | 26.9 | 30.1 | 24.7 | 5.7 | 11.4 | 18.6 | 0.2 | 0.2 |
| Utah | 13 963 | 49.1 | 6.0 | 43.2 | 0.9 | 11.6 | 6.5 | 0 | 0.2 |
| Vermont | 10 530 | 42.0 | 7.7 | 21.2 | 7.3 | 29.6 | 21.0 | 0 | 0 |
| Virginiac | 35 166 | 47.0 | 20.3 | 29.0 | 4.2 | 9.2 | 9.1 | 0.4 | 0.1 |
| Washington | 50 662 | 7.8 | 87.2 | 4.8 | 1.8 | 1.7 | 1.8 | 0.3 | 0.7 |
| West Virginia | 14 364 | 10.7 | 5.9 | 28.4 | 2.1 | 3.8 | 3.4 | 0.1 | 0.2 |
| Wisconsinc | 34 200 | 45.3 | 23.2 | 18.1 | 12.4 | 10.2 | 7.0 | 0.5 | 0.9 |
aAddress categories are the following: mental health center (MHC), other care center (OCC), mental health entity 2 (MHE2), entity 2 containing entity 1 mental health (CMH), multiple entity 1 mental health (MMH), single mental health provider (SMH), primary/rehabilitative/developmental entity 2 (PDE2), primary/rehabilitative/developmental entity 1 (PDE1).
bData collected for each state are from the most recent available year of the Medicaid Analytic eXtract.36
c2012 data use.
Table 2.
Distribution of Medicaid-insured child psychosocial visits across address categoriesa for 34 US states, in 2012 or 2013b
| State | Total no. of visits |
% of visits | |||||||
|---|---|---|---|---|---|---|---|---|---|
| MHC | OCC | MHE2 | CMH | MMH | SMH | PDE2 | PDE1 | ||
| Alabamac | 840 858 | 80.3 | 13.0 | 3.0 | 0.1 | 0.8 | 2.7 | 0.1 | 0.03 |
| Arizona | 745 061 | 84.2 | 13.1 | 2.4 | 0.1 | 0.1 | 0.2 | 0.02 | 0.01 |
| Connecticut | 517 747 | 40.1 | 34.7 | 8.4 | 6.2 | 4.0 | 6.4 | 0.1 | 0.1 |
| District of Columbiac | 138 044 | 69.8 | 18.8 | 11.0 | 0 | 0.1 | 0.3 | 0 | 0 |
| Floridac | 1 030 037 | 45.6 | 15.0 | 9.2 | 2.8 | 8.9 | 11.5 | 1.6 | 5.4 |
| Georgia | 1 186 922 | 73.5 | 5.2 | 13.5 | 0.7 | 2.1 | 3.5 | 0.8 | 0.8 |
| Hawaii | 32 971 | 83.9 | 16.0 | 0 | 0.1 | 0 | 0 | 0 | 0 |
| Idaho | 878 843 | 45.7 | 43.7 | 10.1 | 0.1 | 0.2 | 0.1 | 0.1 | 0 |
| Illinoisc | 1 706 700 | 33.7 | 56.0 | 0.9 | 0.2 | 0.3 | 2.1 | 0.4 | 6.5 |
| Iowa | 368 572 | 3.82 | 95.7 | 0.1 | 0.04 | 0 | 0 | 0.3 | 0.03 |
| Kentuckyc | 513 478 | 91.0 | 2.9 | 3.9 | 0.6 | 1.5 | 0.04 | 0.1 | 0.04 |
| Louisiana | 1 076 208 | 84.4 | 4.7 | 7.2 | 1.0 | 0.8 | 1.7 | 0.1 | 0.1 |
| Marylandc | 762 003 | 64.9 | 18.8 | 7.1 | 0.9 | 2.1 | 6.0 | 0.3 | 0 |
| Massachusetts | 2 635 936 | 80.0 | 11.9 | 4.7 | 1.7 | 0.9 | 0.7 | 0.02 | 0.01 |
| Minnesota | 778 272 | 47.5 | 16.9 | 28.3 | 0.04 | 6.1 | 1.0 | 0.2 | 0.1 |
| Mississippi | 821 511 | 61.6 | 9.1 | 17.4 | 1.4 | 2.1 | 8.5 | 0 | 0 |
| Montanac | 467 083 | 16.2 | 70.4 | 4.9 | 0.6 | 3.3 | 3.9 | 0.2 | 0.5 |
| Nevadac | 620 908 | 54.2 | 3.0 | 8.1 | 2.5 | 6.1 | 8.2 | 0.7 | 17.3 |
| New Jersey | 466 525 | 63.6 | 14.5 | 18.5 | 0.2 | 0.5 | 2.7 | 0.01 | 0 |
| New Mexicoc | 940 717 | 50.0 | 29.6 | 13.8 | 0.5 | 1.3 | 3.4 | 0.8 | 0.6 |
| New York | 571 711 | 27.8 | 10.3 | 11.2 | 31.7 | 9.9 | 8.7 | 0.2 | 0.3 |
| North Carolinac | 1 745 610 | 45.6 | 24.5 | 11.7 | 2.2 | 2.1 | 11.1 | 2.4 | 0.4 |
| Ohio | 2 571 918 | 87.2 | 3.5 | 8.5 | 0.1 | 0.3 | 0.3 | 0.1 | 0.03 |
| Oklahoma | 3 224 014 | 46.4 | 2.8 | 25.7 | 1.5 | 6.5 | 16.7 | 0.02 | 0.4 |
| Oregon | 249 955 | 61.6 | 12.8 | 16.2 | 0.8 | 6.4 | 2.4 | 0.04 | 0 |
| Pennsylvania | 2 987 005 | 77.5 | 12.8 | 6.7 | 0.5 | 1.3 | 1.2 | 0.03 | 0.01 |
| Tennessee | 368 921 | 61.5 | 10.9 | 6.8 | 5.8 | 6.8 | 7.6 | 0.1 | 0.6 |
| Texasc | 1 377 028 | 25.4 | 22.7 | 18.7 | 4.8 | 8.5 | 19.8 | 0.1 | 0.2 |
| Utah | 396 217 | 44.7 | 8.6 | 40.6 | 0.2 | 3.8 | 2.2 | 0 | 0.02 |
| Vermont | 342 033 | 42.1 | 2.5 | 24.9 | 2.3 | 18.1 | 10.1 | 0 | 0 |
| Virginiac | 531 231 | 51.8 | 12.6 | 18.7 | 2.4 | 5.7 | 8.5 | 0.3 | 0.01 |
| Washington | 752 035 | 8.4 | 84.2 | 3.2 | 1.6 | 0.9 | 1.1 | 0.2 | 0.6 |
| West Virginia | 152 185 | 65.6 | 2.5 | 27.2 | 0.8 | 2.4 | 1.3 | 0.1 | 0.2 |
| Wisconsinc | 351 274 | 49.1 | 14.0 | 14.7 | 8.8 | 6.4 | 6.3 | 0.3 | 0.4 |
aAddress categories are the following: mental health center (MHC), other care center (OCC), mental health entity 2 (MHE2), entity 2 containing entity 1 mental health (CMH), multiple entity 1 mental health (MMH), single mental health provider (SMH), primary/rehabilitative/developmental entity 2 (PDE2), primary/rehabilitative/developmental entity 1 (PDE1).
bData collected for each state are from the most recent available year of the Medicaid Analytic eXtract.36
c2012 data use.
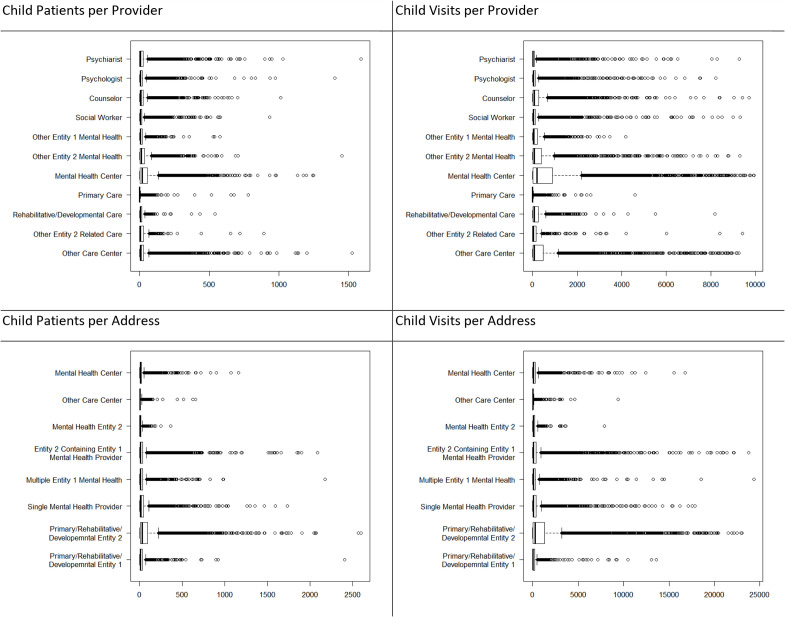
Per-Provider Distribution
Most providers saw <25 children and provided <250 psychosocial service visits during their selected year of data (Table 3 and Figure 2). More than 75% of entity 1 mental health providers saw at most 20 Medicaid-enrolled children per year or provided <170 psychosocial visits to Medicaid-enrolled children. Among entity 1 mental health providers, counselors had the highest 75th percentile child–patient caseload (with 25 children) and the highest 75th percentile and 90th percentile child–visit caseloads (with 302 and 730 visits, respectively). However, psychiatrists had the highest 90th percentile child–patient caseload (with 84 children). Social workers generally had the lowest caseloads.
Table 3.
Summary statistics of Medicaid-insured child psychosocial caseload per address during 1 selected year (2012 or 2013),a aggregated among 34 states, by urbanicity and address categoryb
| Urbanicityc | Patients | Visits | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MHC | OCC | MHE2 | CMH | MMH | SMH | PDE2 | PDE1 | MHC | OCC | MHE2 | CMH | MMH | SMH | PDE2 | PDE1 | ||
| Overall | No. | 7092 | 7071 | 4236 | 1391 | 2944 | 7247 | 648 | 1609 | 7092 | 7071 | 4236 | 1391 | 2944 | 7247 | 648 | 1609 |
| Mean | 140 | 53 | 57 | 36 | 34 | 20 | 15 | 12 | 2629 | 762 | 695 | 327 | 352 | 257 | 161 | 186 | |
| 50% | 30 | —d | 15 | —d | —d | —d | —d | —d | 296 | 66 | 103 | 48 | 76 | 64 | —d | 59 | |
| 75% | 108 | 35 | 47 | 30 | 34 | 22 | —d | 14 | 1571 | 381 | 401 | 204 | 297 | 256 | 54 | 235 | |
| 90% | 331 | 109 | 124 | 77 | 78 | 47 | 32 | 30 | 5820 | 1423 | 1165 | 596 | 785 | 680 | 402 | 495 | |
| Large urban | No. | 5661 | 5396 | 3582 | 1183 | 2377 | 5749 | 504 | 1402 | 5661 | 5396 | 3582 | 1183 | 2377 | 5749 | 504 | 1402 |
| Mean | 146 | 61 | 56 | 35 | 32 | 20 | 15 | 12 | 2742 | 821 | 681 | 317 | 316 | 258 | 144 | 188 | |
| 50% | 29 | —d | 14 | —d | —d | —d | —d | —d | 285 | 66 | 93 | 43 | 62 | 60 | —d | 63 | |
| 75% | 109 | 39 | 44 | 27 | 30 | 20 | —d | 15 | 1561 | 381 | 381 | 182 | 252 | 233 | 52 | 236 | |
| 90% | 348 | 130 | 120 | 69 | 71 | 46 | 31 | 30 | 6296 | 1473 | 1162 | 549 | 697 | 663 | 435 | 487 | |
| Small urban | No. | 859 | 795 | 431 | 143 | 336 | 793 | 96 | 132 | 859 | 795 | 431 | 143 | 336 | 793 | 96 | 132 |
| Mean | 149 | 38 | 64 | 47 | 43 | 21 | 18 | —d | 2744 | 702 | 678 | 428 | 481 | 264 | 266 | 179 | |
| 50% | 41 | —d | 23 | 14 | 18 | 11 | —d | —d | 420 | 64 | 164 | 80 | 170 | 88 | 16 | 31 | |
| 75% | 132 | 35 | 66 | 53 | 50 | 27 | 13 | 13 | 1971 | 410 | 511 | 377 | 490 | 363 | 77 | 245 | |
| 90% | 334 | 85 | 153 | 117 | 110 | 50 | 47 | 26 | 5802 | 1529 | 1121 | 889 | 1109 | 759 | 276 | 495 | |
| Rural | No. | 555 | 866 | 220 | 63 | 224 | 683 | 48 | 72 | 555 | 866 | 220 | 63 | 224 | 683 | 48 | 72 |
| Mean | 70 | 22 | 51 | 26 | 39 | 19 | —d | 12 | 1310 | 449 | 927 | 294 | 540 | 239 | 127 | 173 | |
| 50% | 28 | —d | 19 | —d | 22 | —d | —d | —d | 225 | 73 | 169 | 78 | 167 | 87 | —d | 30 | |
| 75% | 73 | 20 | 51 | 32 | 48 | 25 | —d | 15 | 1131 | 347 | 584 | 173 | 500 | 310 | 30 | 200 | |
| 90% | 157 | 56 | 122 | 59 | 96 | 45 | 25 | 28 | 3050 | 1120 | 1327 | 601 | 1174 | 691 | 245 | 527 | |
aData collected for each address are from the most recent year of the Medicaid Analytic eXtract36 available for that address’s state.
bAddress categories are the following: mental health center (MHC), other care center (OCC), mental health entity 2 (MHE2), entity 2 containing mental health (CMH), multiple entity 1 mental health (MMH), single mental health provider (SMH), primary/rehabilitative/developmental entity 2 (PDE2), primary/rehabilitative/developmental provider entity 1 (PDE1). Values given are total number of addresses seeing Medicaid-insured children for psychosocial services (no.), mean caseload among those addresses (mean), 50th percentile (50%), 75th percentile (75%), and 90th percentile (90%).
cAddresses were divided into 3 urbanicity classes based on their zip code’s approximation of the rural–urban commuting area codes.41 Codes 1-3 represented large urban areas (ie, areas with a primary flow to or within an urbanized area), codes 4-6 represented small urban areas (ie, areas with a primary flow to or within a large urban cluster), and codes 7-10 represented rural areas.
dBlank cells indicate a caseload <11.
Figure 2.
Boxplots displaying per-provider/per-year and per-address/per-year caseloads of Medicaid-insured child psychosocial patients and visits observed during 1 selected year (2012 or 2013) in 34 US states, by provider and address category. Data source: Medicaid Analytic eXtract.36
Across address categorizations, median caseload was at most 30 children and 296 visits. Mental health centers had the highest mean, median, 75th percentile caseload, and 90th percentile caseload, in both patients and visits, which was at least twice those of the next-highest category (generally locations with other entity 2 mental health). Caseload was generally lowest at locations without mental health providers. All these caseload distributions were heavily skewed (Figure 2). For example, about 7% of locations with entity 1 mental health providers but without entity 2 mental health providers saw half of the Medicaid-enrolled children seeking psychosocial services from such locations. Similarly, 4% of mental health centers saw half the children seeking psychosocial services at mental health center locations.
Patient caseloads for entity 1 mental health providers were generally lowest in large urban zip codes and highest in small urban areas (75th percentile of 18 children in large urban areas vs 29 children in small urban areas). Entity 1 mental health provider visit caseloads, however, were highest in rural zip codes (75th percentile of 144 visits from children in large urban areas vs 312 visits from children in rural areas). Small urban zip codes generally had the highest patient caseload across all address categories and the highest child visit caseloads for mental health center, other care center, and single mental health provider locations. Rural zip codes had the lowest patient and visit caseloads for both mental health centers and other care centers (Table 3).
Discussion
Our study provides a comprehensive analysis of the current supply of psychosocial services available for Medicaid-enrolled children across provider types, revealing the important role of mental health centers, especially those that serve a high volume of Medicaid-enrolled children. More than half of the visits occurred in a mental health center, yet only 4% of mental health centers saw half the children seeking psychosocial services.
Across all practice settings, fewer than 10% of locations were responsible for more than half of the patients served and more than half of the visits provided. This finding suggests that Medicaid-insured children have little choice in treatment location. Concentrating the supply of psychosocial services to few locations may partly explain why many studies cite distance as a barrier to care.42-44 These findings underscore the limits of studies that assess geographic accessibility of mental health treatment by only examining where mental health clinics and providers are located, without taking into account the volume of services provided at those locations.
Fewer than 15% of patients who seek psychosocial services receive these services from providers not associated with a center or organization. This concentration of treatment at centers and organizations may be due to barriers against Medicaid participation among providers, such as reimbursement rates and administrative costs. Administrative requirements and the cost of overhead to handle paperwork and insurance billing have been reported as a barrier to psychiatrists participating in Medicaid.45,46 This barrier may be even more pronounced for therapists in solo or small group practices. Easing these burdens may enable providers to accept more Medicaid-insured patients.
Service distribution is not consistent across states, which may be explained, in part, by differences in the organization of mental health care systems available to serve Medicaid-insured children and/or differences in state policies. For example, Florida required behavioral health clinicians such as psychologists to work under physician supervision, which may explain why it has more services provided by psychiatrists and related care providers than most other states.47 In Massachusetts, private practice psychologists can provide therapy only through licensed mental health clinics, which may account for its low rate of services from entity 1 providers.48
Our findings have key implications for policy makers and program planners who aim to improve the accessibility of psychosocial services for Medicaid-enrolled children. These decision makers should recognize that high-volume mental health clinics play an important role in providing psychosocial services to Medicaid-insured children. Policy makers can provide incentives and resources to encourage increased geographic accessibility of services provided by high-volume clinics. One approach would be for these facilities to partner with schools to deliver psychosocial services on school grounds.49,50 Another approach would be to incentivize these clinics to provide home-based services, in which counselors or therapists travel to the child’s home to deliver care.51
Policy makers could also consider approaches to encourage all providers to increase their supply of psychosocial services. These approaches would include increasing current levels of investment in policies to expand the mental health workforce capacity in clinics and practices that accept Medicaid, such as loan forgiveness programs.52,53 Another option would entail increasing Medicaid reimbursement rates for psychosocial services to enable clinics and practices to offer higher salaries than could be offered without the increased reimbursement rates as a strategy to improve recruitment and retention efforts of these providers.54
Limitations
This study had several limitations. First, our results were for 34 states; patterns in these states may differ from patterns in the rest of the country. Second, the latest data available were for 2013, before the Affordable Care Act went into effect. With an increase in the proportion of mental health services covered by health insurance after implementation of the Affordable Care Act, the proportion of their caseload that providers dedicate to persons insured by Medicaid may have changed in recent years. For example, one study comparing a 2013-2014 survey with a 2016-2017 survey found that among outpatient substance use disorder treatment programs, the total number of clients remained constant but more clients used Medicaid during 2016-2017 than during 2013-2014.55
Third, our data relied on Medicaid claims. To be registered as a service to a child, a claim must have a child listed as the beneficiary rather than an adult family member. However, family therapies listing an adult family member as the beneficiary would still be of benefit for the child. Medicaid-enrolled children may also have other resources for obtaining psychosocial services, such as community or school programs, which do not bill Medicaid. However, we were unable to capture these data.17,56
Fourth, some providers bill solely through their organization’s NPI number. Our matching algorithm would link these providers only to the organization’s NPI number, preventing us from identifying the type of practitioner providing the service. This linkage of providers solely to an organization’s NPI number occurred for 20% of the psychosocial service providers. Similarly, some providers working for an organization may still bill as individuals, resulting in a lower caseload captured for that organization in the per-provider results than if the provider had billed through his or her organization. Although our address-level analysis reduced the likelihood of these errors, it did not allow us to distinguish among individual provider types. In addition, we assumed that all providers worked at their single practice address listed in NPPES, but some providers may travel to treat patients. A study in Georgia found that primary care providers had, on average, 2.6 practice locations whereas psychiatrists had 1.8.57 Finally, we examined only the caseload of psychosocial services. Some providers may still see Medicaid beneficiaries for other mental health–related treatment, such as prescribing medication.
Conclusions
To our knowledge, our study is the largest and most comprehensive to date examining Medicaid caseload for psychosocial services by a broad range of mental health providers. Most providers across all provider types had relatively low caseloads. Fewer than 10% of providers were responsible for more than half of services, with the largest proportion of services provided by mental health treatment centers. Services concentrated in few locations would reduce geographic access to services for the Medicaid-insured population.
Additional Material
The following items are available from the authors upon request: a full description of taxonomies in each provider category; the CPT codes used in our study; full details on the procedure used to match an NPI to each service provider; service provider-to-NPI matching rates for each US state; detailed definitions of each address category; demographic characteristics of Medicaid-insured children, both overall and among those seeking psychosocial services; plots displaying the total number of patients and visits by address category; data on state-level distribution of providers, children, and visits across provider types; the mean, median, 75th percentile, and 90th percentile per-provider caseloads; and the minimum percentages of providers and addresses needed to serve half the children who sought psychosocial services for each provider and address category.
Footnotes
Disclaimer: Any opinions, findings, and conclusions or recommendations expressed in this article are those of the authors and do not necessarily reflect the views of the National Science Foundation.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This article is based upon work supported by the National Science Foundation Graduate Research Fellowship Program under grant no. DGE-1650044.
ORCID iD
Pravara M. Harati https://orcid.org/0000-0002-5437-9269
References
- 1. Merikangas KR., He J-P., Burstein M. et al. Service utilization for lifetime mental disorders in U.S. adolescents: results of the National Comorbidity Survey Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. 2011;50(1):32-45. 10.1016/j.jaac.2010.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Pliszka S, AACAP Work Group on Quality Issues Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2007;46(7):894-921. 10.1097/chi.0b013e318054e724 [DOI] [PubMed] [Google Scholar]
- 3. Connolly SD, Bernstein GA, Work Group on Quality Issues Practice parameter for the assessment and treatment of children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry. 2007;46(2):267-283. 10.1097/01.chi.0000246070.23695.06 [DOI] [PubMed] [Google Scholar]
- 4. Birmaher B, Brent D, AACAP Work Group on Quality Issues et al. Practice parameter for the assessment and treatment of children and adolescents with depressive disorders. J Am Acad Child Adolesc Psychiatry. 2007;46(11):1503-1526. 10.1097/chi.0b013e318145ae1c [DOI] [PubMed] [Google Scholar]
- 5. Geller DA., March J. Practice parameter for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry. 2012;51(1):98-113. 10.1016/j.jaac.2011.09.019 [DOI] [PubMed] [Google Scholar]
- 6. National Institute of Mental Health Mental health medications. Updated October 2016. Accessed February 15, 2018 https://www.nimh.nih.gov/health/topics/mental-health-medications/index.shtml
- 7. England MJ., Butler AS., Gonzalez ML. , eds Psychosocial Interventions for Mental and Substance Use Disorders: A Framework for Establishing Evidence-Based Standards. National Academies Press; 2015. [PubMed] [Google Scholar]
- 8. Hibbs ED., Jensen PS. , eds Psychosocial Treatments for Child and Adolescent Disorders: Empirically Based Strategies for Clinical Practice. American Psychological Association; 1996. [Google Scholar]
- 9. Riosa PB., McArthur BA., Preyde M. Effectiveness of psychosocial intervention for children and adolescents with comorbid problems: a systematic review. Child Adolesc Ment Health. 2011;16(4):177-185. 10.1111/j.1475-3588.2011.00609.x [DOI] [PubMed] [Google Scholar]
- 10. McNeilly CL., Howard KI. The effects of psychotherapy: a reevaluation based on dosage. Psychother Res. 1991;1(1):74-78. 10.1080/10503309112331334081 [DOI] [Google Scholar]
- 11. American Psychological Association. Understanding psychotherapy and how it works. Accessed February 15, 2018 https://www.apa.org/helpcenter/understanding-psychotherapy
- 12. American Academy of Pediatrics Medicaid facts. January 2017. Accessed February 16, 2018 https://downloads.aap.org/AAP/PDF/federaladvocacy_medicaidfactsheet_all_states.pdf
- 13. Centers for Medicare & Medicaid Services Medicaid & CHIP: Strengthening Coverage, Improving Health. January 2017. Accessed April 26, 2020 https://www.medicaid.gov/medicaid/downloads/accomplishments-report.pdf
- 14. Cummings JR., Ji X., Allen L., Lally C., Druss BG. Racial and ethnic differences in ADHD treatment quality among Medicaid-enrolled youth. Pediatrics. 2017;139(6):e20162444. 10.1542/peds.2016-2444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hoagwood KE., Kelleher K., Zima BT., Perrin JM., Bilder S., Crystal S. Ten-year trends in treatment services for children with attention deficit hyperactivity disorder (ADHD) enrolled in Medicaid. Health Aff (Millwood). 2016;35(7):1266-1270. 10.1377/hlthaff.2015.1423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Young J., Ramachandran S., Freeman AJ., Bentley JP., Banahan BF. Patterns of treatment for psychiatric disorders among children and adolescents in Mississippi Medicaid. PLoS One. 2019;14(8):e0221251. 10.1371/journal.pone.0221251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hincapie-Castillo JM., Liu X., Bussing R., Winterstein AG. Prevalence of psychotherapy surrounding initiation of psychotropic polypharmacy in the Medicaid-insured population, 1999-2010. Psychiatr Serv. 2017;68(11):1120-1126. 10.1176/appi.ps.201600511 [DOI] [PubMed] [Google Scholar]
- 18. Harris E., Sorbero M., Kogan JN., Schuster J., Stein BD. Concurrent mental health therapy among Medicaid-enrolled youths starting antipsychotic medications. Psychiatr Serv. 2012;63(4):351-356. 10.1176/appi.ps.201100329 [DOI] [PubMed] [Google Scholar]
- 19. Gellad WF., Stein BD., Ruder T. et al. Geographic variation in receipt of psychotherapy in children receiving attention-deficit/hyperactivity disorder medications. JAMA Pediatr. 2014;168(11):1074-1076. 10.1001/jamapediatrics.2014.1647 [DOI] [PubMed] [Google Scholar]
- 20. Finnerty M., Neese-Todd S., Pritam R. et al. Access to psychosocial services prior to starting antipsychotic treatment among Medicaid-insured youth. J Am Acad Child Adolesc Psychiatry. 2016;55(1):69-76. 10.1016/j.jaac.2015.09.020 [DOI] [PubMed] [Google Scholar]
- 21. Stein BD., Sorbero MJ., Dalton E. et al. Predictors of adequate depression treatment among Medicaid-enrolled youth. Soc Psychiatry Psychiatr Epidemiol. 2013;48(5):757-765. 10.1007/s00127-012-0593-7 [DOI] [PubMed] [Google Scholar]
- 22. US Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation Best practices and barriers to engaging people with substance use disorders in treatment. March 2019. Accessed December 23, 2019 https://aspe.hhs.gov/pdf-report/best-practices-and-barriers-engaging-people-substance-use-disorders-treatment
- 23. de Haan AM., Boon AE., de Jong JT., Hoeve M., Vermeiren RR. A meta-analytic review on treatment dropout in child and adolescent outpatient mental health care. Clin Psychol Rev. 2013;33(5):698-711. 10.1016/j.cpr.2013.04.005 [DOI] [PubMed] [Google Scholar]
- 24. Health Resources and Services Administration State-Level Projections of Supply and Demand for Behavioral Health Occupations: 2016-2030. US Department of Health and Human Services; 2018. [Google Scholar]
- 25. Bisgaier J., Rhodes KV. Auditing access to specialty care for children with public insurance. N Engl J Med. 2011;364(24):2324-2333. 10.1056/NEJMsa1013285 [DOI] [PubMed] [Google Scholar]
- 26. Lipson DJ., Libersky J., Bradley K., Lewis C., Siegwarth AW., Lester R. Promoting Access in Medicaid and CHIP Managed Care: A Toolkit for Ensuring Provider Network Adequacy and Service Availability. Centers for Medicare & Medicaid Services, Division of Managed Care Plans; 2017. [Google Scholar]
- 27. Wen H., Wilk AS., Druss BG., Cummings JR. Medicaid acceptance by psychiatrists before and after Medicaid expansion. JAMA Psychiatry. 2019;76(9):981-983. 10.1001/jamapsychiatry.2019.0958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cummings JR., Allen L., Clennon J., Ji X., Druss BG. Geographic access to specialty mental health care across high- and low-income US communities. JAMA Psychiatry. 2017;74(5):476-484. 10.1001/jamapsychiatry.2017.0303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cummings JR., Wen H., Ko M., Druss BG. Geography and the Medicaid mental health care infrastructure: implications for health care reform. JAMA Psychiatry. 2013;70(10):1084-1090. 10.1001/jamapsychiatry.2013.377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cummings JR., Case BG., Ji X., Marcus SC. Availability of youth services in U.S. mental health treatment facilities. Adm Policy Ment Health. 2016;43(5):717-727. 10.1007/s10488-015-0685-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Rushton J., Bruckman D., Kelleher K. Primary care referral of children with psychosocial problems. Arch Pediatr Adolesc Med. 2002;156(6):592-598. 10.1001/archpedi.156.6.592 [DOI] [PubMed] [Google Scholar]
- 32. Williams J., Klinepeter K., Palmes G., Pulley A., Foy JM. Diagnosis and treatment of behavioral health disorders in pediatric practice. Pediatrics. 2004;114(3):601-606. 10.1542/peds.2004-0090 [DOI] [PubMed] [Google Scholar]
- 33. Stein REK., Zitner LE., Jensen PS. Interventions for adolescent depression in primary care. Pediatrics. 2006;118(2):669-682. 10.1542/peds.2005-2086 [DOI] [PubMed] [Google Scholar]
- 34. Collins C., Hewson DL., Munger R., Wade T. Evolving Models of Behavioral Health Integration in Primary Care. Milbank Memorial Fund; 2010. [Google Scholar]
- 35. Centers for Medicare & Medicaid Services NPI files. Accessed November 12, 2013 https://download.cms.gov/nppes/NPI_Files.html [PubMed]
- 36. Centers for Medicare & Medicaid Services Medicaid Analytic eXtract (MAX) general information. Accessed October 9, 2018 https://www.cms.gov/research-statistics-data-and-systems/computer-data-and-systems/medicaiddatasourcesgeninfo/maxgeneralinformation.html
- 37. Heisler EJ., Bagalman E. The Mental Health Workforce: A Primer. Congressional Research Service; 2015. [Google Scholar]
- 38. Substance Abuse and Mental Health Services Administration National Mental Health Services Survey (N-MHSS): 2018. Data on Mental Health Treatment Facilities. US Department of Health and Human Services; 2019. [Google Scholar]
- 39. American Medical Association CPT overview and code approval. Accessed May 6, 2020 https://www.ama-assn.org/practice-management/cpt/cpt-overview-and-code-approval
- 40. Visser SN., Danielson ML., Wolraich ML. et al. Vital signs: national and state-specific patterns of attention deficit/hyperactivity disorder treatment among insured children aged 2-5 years—United States, 2008-2014. MMWR Morb Mortal Wkly Rep. 2016;65(17):443-450. 10.15585/mmwr.mm6517e1 [DOI] [PubMed] [Google Scholar]
- 41. US Department of Agriculture. Economic Research Service Rural-urban commuting area codes. Updated October 2016. Accessed November 8, 2018 https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx
- 42. Bauer MS., Williford WO., McBride L., McBride K., Shea NM. Perceived barriers to health care access in a treated population. Int J Psychiatry Med. 2005;35(1):13-26. 10.2190/U1D5-8B1D-UW69-U1Y4 [DOI] [PubMed] [Google Scholar]
- 43. Kruzich JM., Jivanjee P., Robinson A., Friesen BJ. Family caregivers’ perceptions of barriers to and supports of participation in their children’s out-of-home treatment. Psychiatr Serv. 2003;54(11):1513-1518. 10.1176/appi.ps.54.11.1513 [DOI] [PubMed] [Google Scholar]
- 44. Foutz J., Artiga S., Garfield R. The Role of Medicaid in Rural America. Kaiser Family Foundation; 2017. [Google Scholar]
- 45. Bishop TF., Press MJ., Keyhani S., Pincus HA. Acceptance of insurance by psychiatrists and the implications for access to mental health care. JAMA Psychiatry. 2014;71(2):176-181. 10.1001/jamapsychiatry.2013.2862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Cummings JR. Rates of psychiatrists’ participation in health insurance networks. JAMA. 2015;313(2):190-191. 10.1001/jama.2014.12472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Hornberger J., Franko B., Freeman D. The Impact of State Health Policies on Integrated Care at Health Centers. National Association of Community Health Centers; 2016. [Google Scholar]
- 48. Clay RA. Removing barriers to Medicaid. Monitor Psychol. 2015;46(5):63. [Google Scholar]
- 49. Weist MD., Evans SW. Expanded school mental health: challenges and opportunities in an emerging field. J Youth Adolesc. 2005;34(1):3-6. 10.1007/s10964-005-1330-2 [DOI] [Google Scholar]
- 50. Weist MD., Albus KE. Expanded school mental health: exploring program details and developing the research base. Behav Modif. 2004;28(4):463-471. 10.1177/0145445503259498 [DOI] [PubMed] [Google Scholar]
- 51. Fox RA., Mattek RJ., Gresl BL. Evaluation of a university–community partnership to provide home-based, mental health services for children from families living in poverty. Community Ment Health J. 2013;49(5):599-610. 10.1007/s10597-012-9545-7 [DOI] [PubMed] [Google Scholar]
- 52. Mace S., Dormond M. The Impact of the Patient Protection and Affordable Care Act on Behavioral Health Workforce Capacity: Results From Secondary Data Analysis. Behavioral Health Workforce Research Center, University of Michigan; 2018. Accessed December 23, 2019 http://www.behavioralhealthworkforce.org/wp-content/uploads/2018/05/ACA-Full-Paper_4.16.18-1-1.pdf
- 53. Olfson M. Building the mental health workforce capacity needed to treat adults with serious mental illnesses. Health Aff (Millwood). 2016;35(6):983-990. 10.1377/hlthaff.2015.1619 [DOI] [PubMed] [Google Scholar]
- 54. National Council Medical Director Institute The Psychiatric Shortage: Causes and Solutions. National Council for Behavioral Health; 2017. Accessed December 23, 2019 https://www.thenationalcouncil.org/wp-content/uploads/2017/03/Psychiatric-Shortage_National-Council-.pdf?daf=375ateTbd56
- 55. Andrews CM., Pollack HA., Abraham AJ. et al. Medicaid coverage in substance use disorder treatment after the Affordable Care Act. J Subst Abuse Treat. 2019;102:1-7. 10.1016/j.jsat.2019.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Bushnell GA., Dusetzina SB., Compton SN., Gaynes BN., Brookhart MA., Stürmer T. Psychotherapy claims surrounding pharmacotherapy initiation in children and adolescents with anxiety disorders. J Child Adolesc Psychopharmacol. 2019;29(2):100-106. 10.1089/cap.2018.0108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Xierali IM. Physician multisite practicing: impact on access to care. J Am Board Fam Med. 2018;31(2):260-269. 10.3122/jabfm.2018.02.170287 [DOI] [PMC free article] [PubMed] [Google Scholar]