Abstract
Study Design:
Literature review.
Objective:
The aim of this literature review is to examine the effects of psychological disorders on postoperative complications, surgical outcomes, and long-term narcotic use. We also hope to detail the value of preoperative identification and treatment of these pathologies.
Methods:
A series of systematic reviews of the relevant literature examining the effects of psychological disorders and spine surgery was conducted using PubMed and Cochrane databases.
Results:
Combined, the database queries yielded 2275 articles for consideration. After applying screening criteria, 96 articles were selected for inclusion. Patients with underlying psychological disease have higher rates of delirium, readmission, longer hospital stays, and higher rates of nonroutine discharge following spine surgery. They also have higher rates of chronic postoperative narcotic use and may experience worse surgical outcomes. Because of these defined issues, researchers have developed multiple screening tools to help identify patients with psychological disorders preoperatively for potential treatment. Treatment of these disorders prior to surgery may significantly improve surgical outcomes.
Conclusion:
Patients with psychological disorders represent a unique population with respect to their higher rates of spinal pain complaints, postoperative complications, and worsened functional outcomes. However, proper identification and treatment of these conditions prior to surgery may significantly improve many outcome measures in this population. Future investigations in this field should attempt to develop and validate current strategies to identify and treat individuals with psychological disorders before surgery to further improve outcomes.
Keywords: psychological disorder, anxiety, depression, low back pain
Introduction
Up to 59% of patients presenting to outpatient spine clinics demonstrate symptoms of an active psychological disorder.1,2 While researchers have not yet explained the mechanism of this correlation, most spine surgeons recognize the unique challenges of this patient population. Though the term psychological disorder encompasses a multitude of separate pathologies, to date the majority of spine-related publications only evaluate depression or anxiety. While this focused research provides a magnitude of knowledge on these 2 disease processes, important gaps in knowledge exist regarding the effects of relatively common psychological diseases, such as schizophrenia and bipolar disorder, on outcomes in spine surgery. Current evidence suggests that patients with psychologic disorders have higher rates of both acute and chronic spine complaints,3 worse outcomes with treatment,4-6 and more frequent use of narcotic medications.7 Additionally, those that undergo surgical intervention have higher complication rates than the general population.8-11 In response, physicians have developed and validated objective screening tools to help identify patients with psychological disorders who are at risk of experiencing suboptimal surgical outcomes. Fortunately, early identification and treatment of these disorders may substantially improve the objective and subjective outcomes of operative intervention. The purpose of this comprehensive review of the existing literature is to describe the correlation between psychological disorders and treatment outcomes. Additionally, we summarize the current understanding of preoperative screening and the value of concomitant perioperative treatment of these disorders.
Link Between Psychologic Conditions and Spine Pain
Patients with psychological disorders report higher rates of acute pain and are more likely to develop chronic pain than the general population.3,12,13 Anxiety and depression represent the 2 pathologies most frequently and strongly associated with back or neck pain. In a review of 85 088 patients collected through a multinational survey, Demyttenaere and associates reported a near 2-fold increase in pooled odds ratio (OR) for anxiety 2.2 (95% confidence interval [CI] = 2.1-2.4) and mood disorders 2.3 (95% CI = 2.1-2.5) in individuals with chronic neck and back pain.14 These associations remained consistent both in developed and developing nations.14 Similarly, in a retrospective review of 118 533 individuals through the Canadian Community Health Survey, Currie and Wang reported that 19.8% of individuals with chronic low back pain suffered from major depression compared with only 5.9% of the pain-free population.13 Individuals with underlying psychological disorders also have a higher risk of developing chronic spine-related pain than the unaffected population. In a prospective study of 9909 adults without preexisting low back pain, Currie and Wang reported that individuals with depression were nearly 3 times as likely to develop chronic low back pain over a 2-year period (OR = 2.9, 95% CI = 1.2-7).15 Together, these large well-designed studies establish a link between the coexistence and development of spine-related pain in individuals with anxiety or depression.
The mechanism underlying the correlation between increased rates and psychological disease is most likely multifactorial. Intuitively, chronic pain may predispose to higher rates of psychological disorders as a result of its effects on quality of life and activity levels. A Dutch epidemiological study of 5303 individuals provides support for pain as a risk for the development of both mood and anxiety disorders. Within this study, de Heer et al report a near 2-fold increase in the odds ratio of individuals with moderate to very severe pain developing mood disorders (OR = 2.10, 95% CI = 1.33-3.29) or anxiety disorders (OR = 2.12, 95% CI = 1.30-3.54) over the normal population.16 Additionally, individuals reporting moderate to severe interference due to pain were also almost twice as likely to develop a mood disorder or anxiety within 3 years.16 Evidence of pain’s contribution to mood disorders may also be reflected in the 37% to 48% spontaneous improvement in mood disorders reported following successful surgery.17,18
Methods
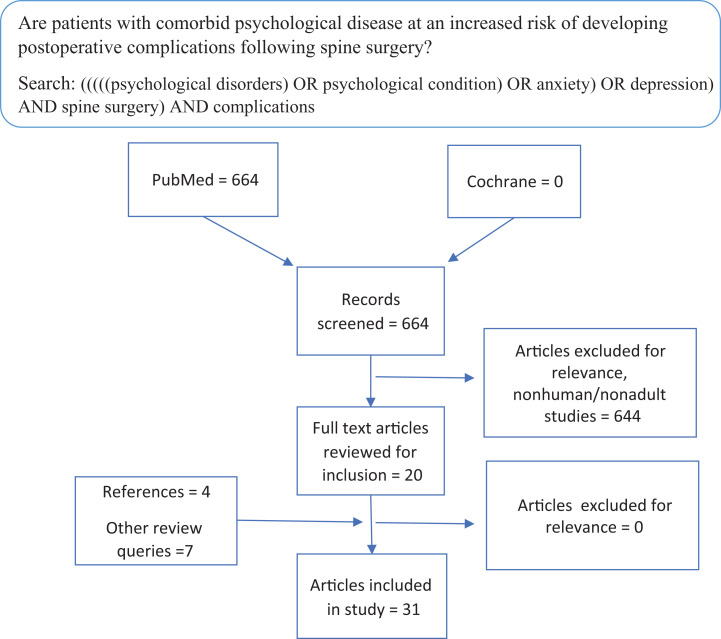
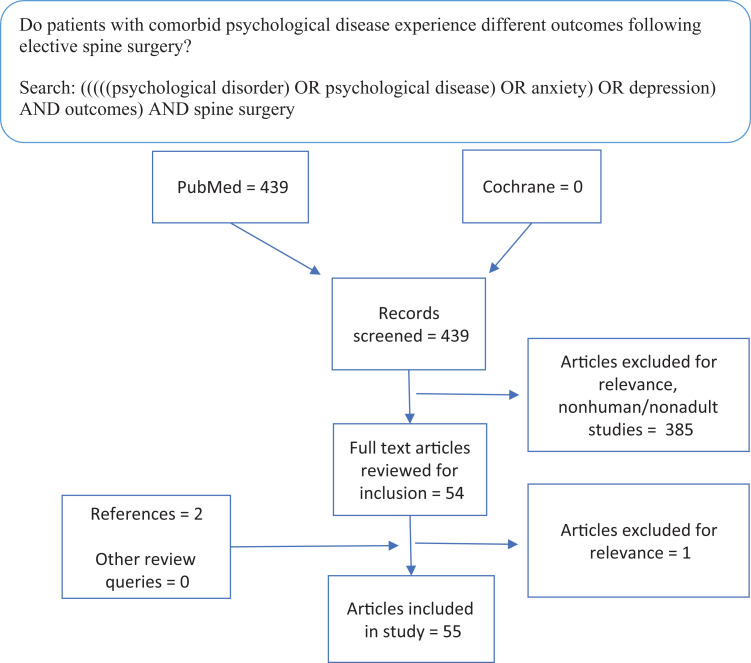
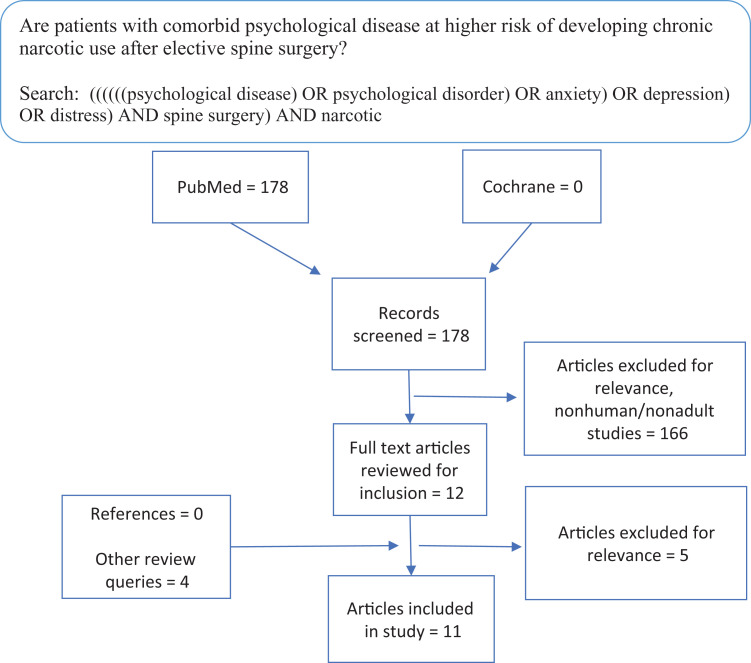
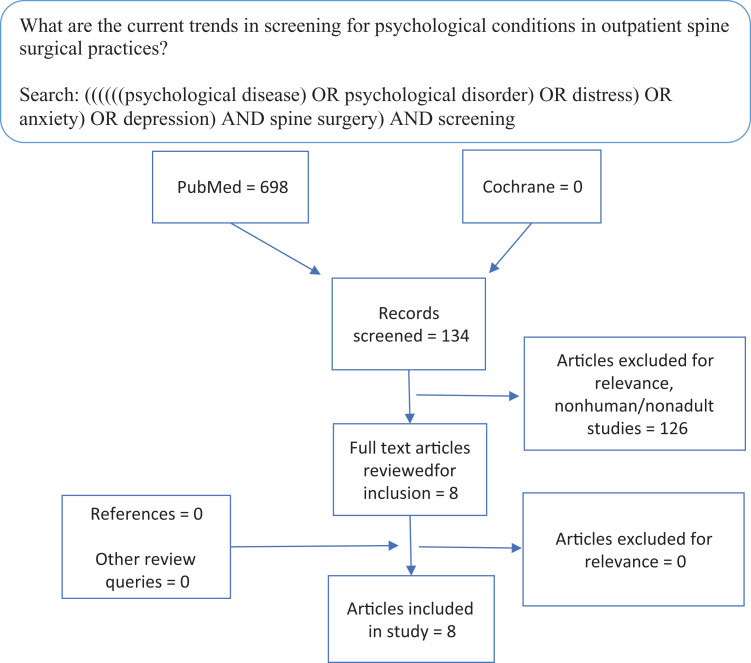
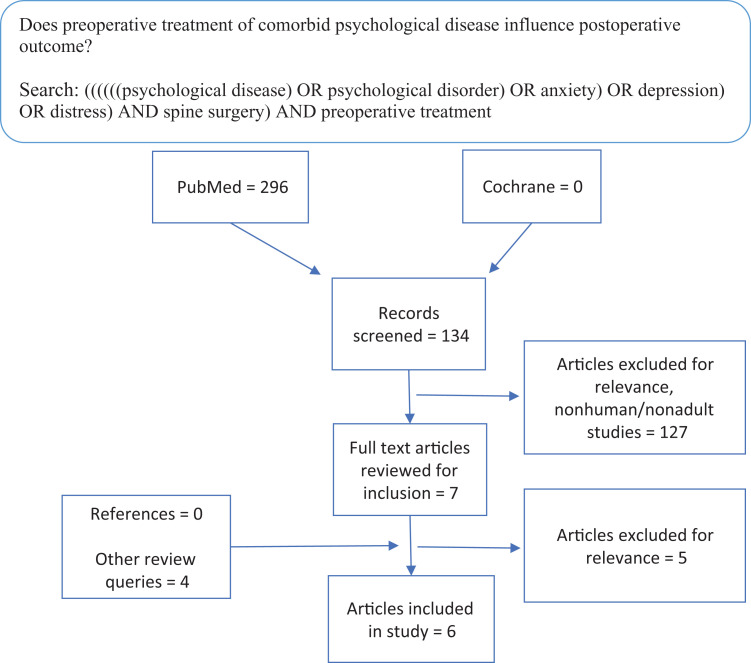
This study sought to address 5 discrete questions through systematic review of the existing literature: (1) Are patients with comorbid psychological disease at an increased risk of developing postoperative complications following spine surgery? (2) Do patients with comorbid psychological disease experience different outcomes following elective spine surgery? (3) Are patients with comorbid psychological disease at higher risk of developing chronic narcotic use after elective spine surgery? (4) What are the current trends in screening for psychological conditions in outpatient spine surgical practices? (5) Does preoperative treatment of comorbid psychological disease influence postoperative outcome? To accomplish this, 5 systematic reviews of the PubMed database and the Cochrane Library were performed targeting each study question independently in September 2019. Specific search strings are contained in Figures 1 to 5. Articles were excluded if they involved animal subjects, nonelective procedures, or focused on a pediatric population. Articles were initially screened by title and abstract. Those that suggested relevance to the specific question underwent full text review to reach an inclusion decision. A single fellowship-trained spine surgeon (KJ) conducted all article reviews. References were reviewed from included studies to identify articles that may have not been captured in the initial database queries.
Figure 1.
Systematic review evaluating the association between psychological disease and postoperative complications.
Figure 2.
Systematic review examining the effect of psychological disorders on postoperative outcomes.
Figure 3.
Systematic review evaluating the association between psychological disease and chronic opioid use after spine surgery.
Figure 4.
Systematic review examining trends in outpatient screening for comorbid psychological disease in patients presenting for spine surgical care.
Figure 5.
Systematic review evaluating if preoperative treatment of comorbid psychological conditions improves postoperative outcomes in surgery.
Results
Figures 1 to 5 demonstrate the results for each systematic review. Cumulatively, the 5 queries identified 2275 articles. Screening by title and abstract for relevance yielded 101 articles for review. Ninety articles were deemed relevant to one of the questions posed after full-text review. Evaluation of references in each relevant study yielded 6 additional studies that were deemed germane to the posed question after full-text review. Fifteen additional articles, discovered in queries designed to answer other questions, were deemed relevant to another question posed in this review and were included.
The Effects of Psychological Disorders on Postoperative Complications and Nonroutine Discharge
Psychological disorders have been linked with higher rates of postoperative delirium,19-22 postoperative readmission, length of stay,11,23 and nonroutine hospital discharge.9,23,24 In a retrospective review of 923 patients who underwent elective spine surgery, Elsamadicy et al reported an almost 2-fold increase in the rate of postoperative delirium in patients with depression compared with the unaffected population (10.59% vs 5.84%, P = .01).19 Within this study the authors noted the link between depression and elevated rates of postoperative delirium in multiple other fields of surgery. They further hypothesized that depressed individuals have higher cortisol levels that increase the risk of postoperative delirium.19,25 Multiple studies have also reported a link between depression and postoperative readmission.8,26,27 In their retrospective review of 14 939 patients who underwent instrumented spine surgery, Akins and colleagues found that preoperative depression was a significant risk for 30-day readmission (OR = 1.48, 95% CI = 1.14-193).8 Schairer et al noted a similar link between depression and readmission following both surgery for adult spinal deformity26 and oncologic spine procedures.27 These factors likely contribute to the reported increased rates of nonroutine hospital discharge observed in individuals with psychological disorders.9 In a review of 5 382 343 patients undergoing decompression and spinal fusion contained within the National Hospital Discharge Survey database, Menendez et al noted higher rates of nonroutine discharge in patients with anxiety, depression, schizophrenia, and dementia (Table 1).9 These observed higher rates of delirium, nonroutine discharge, and readmission may increase the cost of care for individuals with psychological disorders.28,29 In a cross-sectional study of 305 patients who had surgical treatment of a herniated lumbar or cervical disc, Konnopka et al found a significant association between psychiatric comorbidity and direct costs in lumbar disc herniation (€7042 vs €5534, P < .01).28 While the Konnopka study is the only to correlate psychological disease and increased hospital costs in the spine literature, Rasoulli et al reported a $3420 increase in the cost of care for patients undergoing total joint arthroplasty with anxiety or depression.29 Future population studies to both evaluate and quantify this increase in cost after spine surgery may add to the current understanding of the challenges psychologic diseases present in surgical treatment of spinal pathology.
Table 1.
Rates of Nonroutine Discharge Associated With Common Psychological Disorders: Odds Ratios of Nonroutine Discharge Compared With Patients Without These Conditions.
| Diagnosis | Odds Ratio, 95% Confidence Interval, P |
|---|---|
| Depression | 1.4, 1.3-1.4, P < .001 |
| Anxiety | 1.2, 1.2-1.2, P < .001 |
| Schizophrenia | 4.3, 4.0-4.6, P < .001 |
| Dementia | 1.1, 1.1-1.1, P < .001 |
Effects of Psychological Disorders on Postoperative Outcome Measures
The published literature demonstrates inconsistencies on the effect preoperative psychological disorders have on postoperative outcomes. While the vast majority of studies demonstrate a negative correlation between the presence of these conditions and objective and subjective outcomes,6,17,18,30-60 large trials conflict these results.61-68 Evaluating this disconcordant data may promote understanding of both current knowledge gaps and potential areas of future investigation.
In a prospective review of 102 patients undergoing lumbar surgery, Trief et al found that both preoperative depression and anxiety predicted failure to return to work and failure to report improvement in both pain and functional abilities 1 year after surgery.4 Multiple investigations have linked the presence of psychological disorders to worse functional outcome scores.5,6 The association between preoperative psychological disorders and worse functional outcomes persists over long-term clinical follow-up. In a prospective observational study, Tuomainen et al reported a significant correlation between higher preoperative Beck’s Depressive Index scores (worse depression) and worse ODI (Oswestry Disability Index) and VAS (Visual Analogue Scale) scores 10 years after surgery.5 Importantly, the authors noted that while individuals with higher depressive scores demonstrated statistically significant improvement from preoperative ODI scores, observed improvements in VAS and walking distance were not significantly different at 10 years.5 These results sharply contrast with the significant improvements in all measures observed in the nondepressed cohort in this study. In a review of 67 adults undergoing lumbar discectomy, Chaichana et al noted that individuals with anxiety or depression were significantly less likely to achieve a minimum clinical important difference in disability and quality of life (QOL).35
Though these studies suggest that patients with underlying psychological diseases experience worse postoperative outcomes, other evidence challenges this assessment and warrants close review of a perceived association. In a database review of a single surgeon’s elective spine practice, Maratos et al noted that patients with increased levels of preoperative anxiety or depression reported worse Short Form-36 physical functioning (SF36PF) and bodily pain scores (SF36BP) before and after surgery than patients who did not have these conditions.61 However, after accounting for these patients’ worse preoperative functional status through 2-way ANOVA testing, the authors noted no significant contribution from depression or anxiety.61 Similarly, in a review of 267 patients treated surgically for adult spinal deformity, Theologis et al noted that patients with baseline depression had higher levels of preoperative back pain, higher levels of obesity and medical comorbidity, and worse functional scores than unaffected patients.67 When controlling for these differences, depressed patients did not demonstrate significantly worse functional outcomes 2 years after surgery.67 These studies suggest that the frequently noted worse preoperative pain and functional status reported by patients with psychological conditions6,63,65,67,69,70 serve as an important confounding variable when evaluating postoperative outcomes in this population. Spine surgeons should use this information to engage patients demonstrating depressive symptoms in a candid preoperative conversation regarding the expected long-term benefits of elective surgery based on their individualized risks.
Psychological Disorders and Long-Term Postoperative Narcotic Use
Comorbid psychological conditions appear to increase a patient’s risk of chronic opioid use after spine surgery.71-78 In a retrospective review of 819 patients who underwent lumbar spine surgery, Wright et al noted that patients with preoperative depression were significantly more likely to develop postoperative opioid dependence (OR = 1.73, 95% CI = 1.13-2.66, P = .012).78 In a retrospective review of 28 813 patients undergoing 1- or 2-level anterior cervical discectomy and fusion, Harris noted a significant relationship between chronic postoperative opioid use and both anxiety (OR = 1.5, 95% CI = 1.4-1.6) and depression (OR = 1.7, 95% CI = 1.6-1.9).78 Though the mechanism behind this increased risk of chronic opioid use in patients with psychological conditions has not been discovered, this population’s higher rates of preoperative narcotic use7,79 and worse subjective postoperative pain scores45,54,64 may contribute.
The Value of Preoperative Screening for Psychological Disorder
In an attempt to identify which patients with psychological disorders are at risk of suboptimal postoperative outcomes, researchers have developed several screening tools. The Minnesota Multiphasic Personality Inventory (MMPI) has historically been the most common psychological screening tool administered to patients with chronic pain.80 Though evidence suggests this tool can aid in predicting postoperative outcome,81 its length and time requirements limit its usefulness as an office screening tool.82 As a result, many investigators have used the Distress and Risk Assessment Method (DRAM). The DRAM is a 2-page 45-question patient questionnaire that combines the Modified Somatic Perception Questionnaire (MPSQ) and the Zung Depression Index (ZDI).82 Combined scoring then allows stratification into 1 of 4 categories: Type N (normal), Type R (at risk), Type DD (distressed-depressive), and Type DS (distressed-somatic; Table 2). The DRAM has been validated to both correlate with the more extensive MMPI82-84 and predict worse clinical outcomes in patients with higher levels of distress.83,85 In a retrospective review of 103 patients, Abtahi noted significantly higher overall patient satisfaction scores (91.5 ± 10.4 vs 81.8 ± 19.9; P = .005) and satisfaction with provider scores (94.2 ± 11.3 vs 83.0 ± 25.8; P = .042) in patients from the combined normal (N) and at-risk (R) groups versus the combined grouping of distressed-depressive (DD) and distressed-somatic (DS) patients.85 In a prospective study of 267 individuals treated with surgery for adult spinal deformity, Theologis et al noted worse functional scores in patients within both the distressed-depressive and distressed-somatic categories.67 Interestingly, within this study the probability of improving by at the least the minimum clinical important differences demonstrated a near linear negative correlation with the Modified Somatic Perceptions Questionnaire (MSPQ) portion of the DRAM.67 Together, these studies suggest that patients within the distressed-depressive and distressed-somatic groups are at higher risk of experiencing a suboptimal treatment outcome and support use of DRAM as a screening tool for this purpose.
Table 2.
Distress and Risk Assessment Method (DRAM) Categories.a
| Category | Criteria |
|---|---|
| Normal (N) | Modified Zung score <17 |
| At risk (R) | Modified Zung score 17-33 or MSPQ <12 |
| Distressed depressive (DD) | Modified Zung score >33 |
| Distressed somatic (DS) | Modified Zung score 17-33 and MSPQ >12 |
a Categories are assigned from a composite of the Zung Depression Index and The Modified Somatic Perception Questionnaire (MSPQ).28
Current Use of Screening Tools in Spine Surgery
Despite solid evidence of the role psychologic disorders have in treatment outcomes and the availability of current validated screening tools to help identify these patients, most spine surgeons do not formally screen their patients. In a survey of 110 practicing spine surgeons, 37% reported the routine use of a formal tool to screen for depression or anxiety.86 This number matches a study of British spine surgeons that reported 64% either never or rarely use a formal psychological assessment tool.87 Some spine surgeons may rely on their ability and intuition to identify patients with psychological disorders. However, this method has proven unreliable in comparison to the use of an objective screening tool. In a prospective study of 400 new patients comparing the subjective ratings of spine providers to the results of DRAM, Daubs et al reported a sensitivity of 28.7% (95% CI = 19.5% to 39.4%) and a positive predictive value of 47.2% (95% CI = 33.3% to 61.4%) for identifying individuals with high levels of distress.82 Interestingly, the authors reported significantly improved sensitivity for nonoperative providers over surgeons and trends toward improved sensitivity in less experienced surgeons.82 Similarly, in a prospective study of 125 patients comparing surgeon DRAM scoring to patients’ actual DRAM results, Grevitt et al reported a surgeon sensitivity level of 26% and a predictive value of 69% for a “distressed evaluation.”87 Perhaps best demonstrating the inaccuracies of subjective screening measures, Omidi-Kashani et al reported a failure to diagnose severe psychological disorders in 21% of patients undergoing spine surgery.88 These studies highlight the difficulty of attempting to identify patients at risk of suboptimal outcomes using subjective measures or intuition. From an economic and patient care standpoint, providers who routinely refer patients with suspected psychological disorders should consider the use of an objective screening tool in lieu of subjective assessment.
Does Presurgical Referral to Behavioral Health Influence Outcomes
Treatment of psychological disorders before surgery may lead to improved outcomes. In a study of 27 patients undergoing anterior cervical discectomy and fusion with preoperative anxiety, Adogwa et al noted statistically significant improvement in postoperative neck pain at 1 year in patients who received treatment for their anxiety compared those who had not.89 In a similar study of 140 patients undergoing anterior cervical discectomy and fusion, Elsamadicy et al identified 25 individuals with depression preoperatively and provided treatment.90 In this study, patients with treated depression demonstrated no significant difference in objective or subjective outcomes up to 24 months after surgery.90 These similar results suggest that treating depression prior to surgery may mitigate the difference in outcomes observed in the historic literature. Sinikallio et al also demonstrated this correlation between the improvement of depressive symptoms and improvement in surgical outcomes.18 In their retrospective review of 99 patients undergoing surgical treatment of lumbar stenosis, these investigators identified 19 patients with evidence of depression on Beck’s Depression Inventory.18 Following treatment 7 patients (37%) experienced resolution of their depressive symptoms. Three months after surgery patients with depression that resolved postoperatively experienced functional and pain-related improvements that resembled, “in all essential respects,” the improvement seen in the baseline normal mood group.18 Conversely, patients with continuous depression experienced worse postoperative symptom severity, worse ODI scores, less walking capacity, and more pain intensity.18 The improvements in patients who noted resolution of depressive symptoms remained durable at the 2- and 5-year follow-up periods.34,91 In a similar review of 58 patients who underwent surgery for lumbar stenosis, Urban-Baeza noted spontaneous improvement of depressive symptoms in 48% of effected patients (14/29).17 Patients who remained depressed 1 year after surgery experienced higher rates of severe back pain, severe leg pain, and severe disability than individuals in the combined never depressed and resolved depression groups.17 Additionally, patients who remained depressed were less likely to agree with the statement, “Surgery helped a lot” (33% vs 76%).17 These findings suggest that treating underlying depression in the perioperative period may mitigate this population’s risk of developing the historically reported suboptimal objective and subjective outcomes after surgery.
Conclusion
Though most of the current spine literature evaluating the influence of psychological diseases on outcomes focuses only on depression and anxiety, a clear correlation between the development of spine complaints and these disorders exists. While the exact mechanism underlying this relationship has not been fully defined, this patient population experiences both higher rates of perioperative complications and nontraditional discharge and are more likely to continue narcotic use after surgery. Furthermore, patients with psychological disorders report lower rates of satisfaction and worse improvements in both objective and subjective outcomes following surgical care. Historically, physicians have struggled to identify individuals with psychological disorders using subjective clinical assessment alone. However, newer objective screening measures have shown promise in improving the accuracy of identifying patient populations at risk for suboptimal outcomes. Once identified, perioperative treatment of these underlying psychological conditions may substantially improve outcomes in this patient population. Future research in this field should focus on developing and validating improved methods of preoperative identification and treatment of patients with these disorders. Additionally, further investigation into the effects of psychological diseases, other than depression and anxiety, may prove beneficial.
Footnotes
Authors’ Note: The views expressed herein are those of the author(s) and do not reflect the official policy of the Department of the Army, Department of Defense, or the U.S. Government.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Keith L. Jackson, MD  https://orcid.org/0000-0002-3883-8760
https://orcid.org/0000-0002-3883-8760
John DeVine, MD  https://orcid.org/0000-0002-8958-2996
https://orcid.org/0000-0002-8958-2996
References
- 1. Polatin PB, Kinney RK, Gatchel RJ, Lillo E, Mayer TG. Psychiatric illness and chronic low-back pain. The mind and the spine—which goes first? Spine (Phila Pa 1976). 1993;18:66–71. [DOI] [PubMed] [Google Scholar]
- 2. Brooks DE, Agochukwu UF, Arrington ED, Mok JM. Psychological distress in the active duty military spine patient. Mil Med. 2013;178:1059–1064. [DOI] [PubMed] [Google Scholar]
- 3. Linton SJ. A review of psychological risk factors in back and neck pain. Spine (Phila Pa 1976). 2000;25:1148–1156. [DOI] [PubMed] [Google Scholar]
- 4. Trief PM, Grant W, Fredrickson B. A prospective study of psychological predictors of lumbar surgery outcome. Spine (Phila Pa 1976). 2000;25:2616–2621. [DOI] [PubMed] [Google Scholar]
- 5. Tuomainen I, Pakarinen M, Aalto T, et al. Depression is associated with the long-term outcome of lumbar spinal stenosis surgery: a 10-year follow-up study. Spine J. 2018;18:458–463. [DOI] [PubMed] [Google Scholar]
- 6. Chapin L, Ward K, Ryken T. Preoperative depression, smoking, and employment status are significant factors in patient satisfaction after lumbar spine surgery. Clin Spine Surg. 2017;30:E725–E732. [DOI] [PubMed] [Google Scholar]
- 7. Armaghani SJ, Lee DS, Bible JE, et al. Preoperative narcotic use and its relation to depression and anxiety in patients undergoing spine surgery. Spine (Phila Pa 1976). 2013;38:2196–2200. [DOI] [PubMed] [Google Scholar]
- 8. Akins PT, Harris J, Alvarez JL, et al. Risk factors associated with 30-day readmissions after instrumented spine surgery in 14 939 patients: 30-day readmissions after instrumented spine surgery. Spine (Phila Pa 1976). 2015;40:1022–1032. [DOI] [PubMed] [Google Scholar]
- 9. Menendez ME, Neuhaus V, Bot AG, Ring D, Cha TD. Psychiatric disorders and major spine surgery: epidemiology and perioperative outcomes. Spine (Phila Pa 1976). 2014;39:E111–122. [DOI] [PubMed] [Google Scholar]
- 10. Dedeogullari E, Paholpak P, Barkoh K, et al. Effect of mental health on post-operative infection rates following cervical spine fusion procedures. J Orthop. 2017;14:501–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Floyd H, Sanoufa M, Robinson JS. Anxiety’s impact on length of stay following lumbar spinal surgery. Perm J. 2015;19:58–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pincus T, Burton AK, Vogel S, Field AP. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine (Phila Pa 1976). 2002;27:E109–E120. [DOI] [PubMed] [Google Scholar]
- 13. Currie SR, Wang J. Chronic back pain and major depression in the general Canadian population. Pain. 2004;107:54–60. [DOI] [PubMed] [Google Scholar]
- 14. Demyttenaere K, Bruffaerts R, Lee S, et al. Mental disorders among persons with chronic back or neck pain: results from the World Mental Health Surveys. Pain. 2007;129:332–342. [DOI] [PubMed] [Google Scholar]
- 15. Currie SR, Wang J. More data on major depression as an antecedent risk factor for first onset of chronic back pain. Psychol Med. 2005;35:1275–1282. [DOI] [PubMed] [Google Scholar]
- 16. de Heer EW, Ten Have M, van Marwijk HWJ, et al. Pain as a risk factor for common mental disorders. Results from the Netherlands Mental Health Survey and Incidence Study-2: a longitudinal, population-based study. Pain. 2018;159:712–718. [DOI] [PubMed] [Google Scholar]
- 17. Urban-Baeza A, Zarate-Kalfopulos B, Romero-Vargas S, Obil-Chavarria C, Brenes-Rojas L, Reyes-Sanchez A. Influence of depression symptoms on patient expectations and clinical outcomes in the surgical management of spinal stenosis. J Neurosurg Spine. 2015;22:75–79. [DOI] [PubMed] [Google Scholar]
- 18. Sinikallio S, Aalto T, Airaksinen O, et al. Depression is associated with poorer outcome of lumbar spinal stenosis surgery. Eur Spine J. 2007;16:905–912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Elsamadicy AA, Adogwa O, Lydon E, et al. Depression as an independent predictor of postoperative delirium in spine deformity patients undergoing elective spine surgery. J Neurosurg Spine. 2017;27:209–214. [DOI] [PubMed] [Google Scholar]
- 20. Wang J, Li Z, Yu Y, Li B, Shao G, Wang Q. Risk factors contributing to postoperative delirium in geriatric patients postorthopedic surgery. Asia Pac Psychiatry. 2015;7:375–382. [DOI] [PubMed] [Google Scholar]
- 21. Fineberg SJ, Nandyala SV, Marquez-Lara A, Oglesby M, Patel AA, Singh K. Incidence and risk factors for postoperative delirium after lumbar spine surgery. Spine (Phila Pa 1976). 2013;38:1790–1796. [DOI] [PubMed] [Google Scholar]
- 22. Susano MJ, Scheetz SD, Grasfield RH, et al. Retrospective analysis of perioperative variables associated with postoperative delirium and other adverse outcomes in older patients after spine surgery. J Neurosurg Anesthesiol. 2019;31:385–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Rothrock RJ, Morra RP, Jr, Deutsch BC, Neifert SN, Cho SK, Caridi JM. Effect of psychiatric comorbidities on in-hospital outcomes and cost for cervical spondylotic myelopathy. World Neurosurg. 2019;129:e718–e725. [DOI] [PubMed] [Google Scholar]
- 24. Kalakoti P, Sciubba DM, Pugely AJ, et al. Impact of psychiatric comorbidities on short-term outcomes following intervention for lumbar degenerative disc disease. Spine (Phila Pa 1976). 2018;43:1363–1371. [DOI] [PubMed] [Google Scholar]
- 25. Kazmierski J, Banys A, Latek J, Bourke J, Jaszewski R. Cortisol levels and neuropsychiatric diagnosis as markers of postoperative delirium: a prospective cohort study. Crit Care. 2013;17:R38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Schairer WW, Carrer A, Deviren V, et al. Hospital readmission after spine fusion for adult spinal deformity. Spine (Phila Pa 1976). 2013;38:1681–1689. [DOI] [PubMed] [Google Scholar]
- 27. Schairer WW, Carrer A, Sing DC, et al. Hospital readmission rates after surgical treatment of primary and metastatic tumors of the spine. Spine (Phila Pa 1976). 2014;39:1801–1808. [DOI] [PubMed] [Google Scholar]
- 28. Konnopka A, Heinrich S, Zieger M, et al. Effects of psychiatric comorbidity on costs in patients undergoing disc surgery: a cross-sectional study. Spine J. 2011;11:601–609. [DOI] [PubMed] [Google Scholar]
- 29. Rasouli MR, Menendez ME, Sayadipour A, Purtill JJ, Parvizi J. Direct cost and complications associated with total joint arthroplasty in patients with preoperative anxiety and depression. J Arthroplasty. 2016;31:533–536. [DOI] [PubMed] [Google Scholar]
- 30. Levy HI, Hanscom B, Boden SD. Three-question depression screener used for lumbar disc herniations and spinal stenosis. Spine (Phila Pa 1976). 2002;27:1232–1237. [DOI] [PubMed] [Google Scholar]
- 31. Slover J, Abdu WA, Hanscom B, Weinstein JN. The impact of comorbidities on the change in short-form 36 and Oswestry scores following lumbar spine surgery. Spine (Phila Pa 1976). 2006;31:1974–1980. [DOI] [PubMed] [Google Scholar]
- 32. Donceel P, Du Bois M. Predictors for work incapacity continuing after disc surgery. Scand J Work Environ Health. 1999;25:264–271. [DOI] [PubMed] [Google Scholar]
- 33. Sinikallio S, Aalto T, Lehto SM, et al. Depressive symptoms predict postoperative disability among patients with lumbar spinal stenosis: a two-year prospective study comparing two age groups. Disabil Rehabil. 2010;32:462–468. [DOI] [PubMed] [Google Scholar]
- 34. Sinikallio S, Aalto T, Airaksinen O, Lehto SM, Kroger H, Viinamaki H. Depression is associated with a poorer outcome of lumbar spinal stenosis surgery: a two-year prospective follow-up study. Spine (Phila Pa 1976). 2011;36:677–682. [DOI] [PubMed] [Google Scholar]
- 35. Chaichana KL, Mukherjee D, Adogwa O, Cheng JS, McGirt MJ. Correlation of preoperative depression and somatic perception scales with postoperative disability and quality of life after lumbar discectomy. J Neurosurg Spine. 2011;14:261–267. [DOI] [PubMed] [Google Scholar]
- 36. Adogwa O, Parker SL, Shau DN, et al. Preoperative Zung Depression scale predicts outcome after revision lumbar surgery for adjacent segment disease, recurrent stenosis, and pseudarthrosis. Spine J. 2012;12:179–185. [DOI] [PubMed] [Google Scholar]
- 37. Adogwa O, Parker SL, Shau DN, et al. Preoperative Zung Depression Scale predicts patient satisfaction independent of the extent of improvement after revision lumbar surgery. Spine J. 2013;13:501–506. [DOI] [PubMed] [Google Scholar]
- 38. Smith JS, Shaffrey CI, Lafage V, et al. Comparison of best versus worst clinical outcomes for adult spinal deformity surgery: a retrospective review of a prospectively collected, multicenter database with 2-year follow-up. J Neurosurg Spine. 2015;23:349–359. [DOI] [PubMed] [Google Scholar]
- 39. McKillop AB, Carroll LJ, Battie MC. Depression as a prognostic factor of lumbar spinal stenosis: a systematic review. Spine J. 2014;14:837–846. [DOI] [PubMed] [Google Scholar]
- 40. Adogwa O, Carr K, Fatemi P, et al. Psychosocial factors and surgical outcomes: are elderly depressed patients less satisfied with surgery? Spine (Phila Pa 1976). 2014;39:1614–1619. [DOI] [PubMed] [Google Scholar]
- 41. Miller JA, Derakhshan A, Lubelski D, et al. The impact of preoperative depression on quality of life outcomes after lumbar surgery. Spine J. 2015;15:58–64. [DOI] [PubMed] [Google Scholar]
- 42. Alvin MD, Miller JA, Lubelski D, et al. The impact of preoperative depression and health state on quality-of-life outcomes after anterior cervical diskectomy and fusion. Global Spine J. 2016;6:306–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. He J, Xiong W, Li F, Luo W, Gao SC. Depression influences pain and function after cervical disc arthroplasty. J Neurosurg Sci. 2017;61:39–45. [DOI] [PubMed] [Google Scholar]
- 44. Parker SL, Godil SS, Zuckerman SL, Mendenhall SK, Devin CJ, McGirt MJ. Extent of preoperative depression is associated with return to work after lumbar fusion for spondylolisthesis. World Neurosurg. 2015;83:608–613. [DOI] [PubMed] [Google Scholar]
- 45. Vialle E, de Oliveira Pinto BM, Vialle LR, Gomez JD. Evaluation of psychosomatic distress and its influence in the outcomes of lumbar fusion procedures for degenerative disorders of the spine. Eur J Orthop Surg Traumatol. 2015;25(suppl 1):S25–S28. [DOI] [PubMed] [Google Scholar]
- 46. Anderson JT, Haas AR, Percy R, Woods ST, Ahn UM, Ahn NU. Clinical depression is a strong predictor of poor lumbar fusion outcomes among workers’ compensation subjects. Spine (Phila Pa 1976). 2015;40:748–756. [DOI] [PubMed] [Google Scholar]
- 47. Kanaan SF, Arnold PM, Burton DC, Yeh HW, Loyd L, Sharma NK. Investigating and predicting early lumbar spine surgery outcomes. J Allied Health. 2015;44:83–90. [PMC free article] [PubMed] [Google Scholar]
- 48. Smith JS, Shaffrey CI, Glassman SD, et al. Clinical and radiographic parameters that distinguish between the best and worst outcomes of scoliosis surgery for adults. Eur Spine J. 2013;22:402–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Wilhelm M, Reiman M, Goode A, et al. Psychological predictors of outcomes with lumbar spinal fusion: a systematic literature review. Physiother Res Int. 2017;22(2). doi:10.1002/pri.1648 [DOI] [PubMed] [Google Scholar]
- 50. Alvin MD, Miller JA, Sundar S, et al. The impact of preoperative depression on quality of life outcomes after posterior cervical fusion. Spine J. 2015;15:79–85. [DOI] [PubMed] [Google Scholar]
- 51. Tetreault L, Nagoshi N, Nakashima H, et al. Impact of depression and bipolar disorders on functional and quality of life outcomes in patients undergoing surgery for degenerative cervical myelopathy: analysis of a combined prospective dataset. Spine (Phila Pa 1976). 2017;42:372–378. [DOI] [PubMed] [Google Scholar]
- 52. Zakaria HM, Mansour TR, Telemi E, et al. Use of Patient Health Questionnaire-2 scoring to predict patient satisfaction and return to work up to 1 year after lumbar fusion: a 2-year analysis from the Michigan Spine Surgery Improvement Collaborative. J Neurosurg Spine. 2019:1-8 doi:10.3171/2019.6.SPINE1963 [DOI] [PubMed] [Google Scholar]
- 53. Watanabe Y, Yoshida G, Hasegawa T, et al. Impact of perioperative mental status on health-related quality of life in patients with adult spinal deformities [published online August 5, 2019]. Spine (Phila Pa 1976). doi:10.1097/BRS.0000000000003186 [DOI] [PubMed] [Google Scholar]
- 54. Patel DV, Yoo JS, Khechen B, et al. PHQ-9 Score predicts postoperative outcomes following minimally invasive transforaminal lumbar interbody fusion [published online March 29, 2019]. Clin Spine Surg. doi:10.1097/BSD.0000000000000818 [DOI] [PubMed] [Google Scholar]
- 55. Ailon T, Tee J, Manson N, et al. Patient-reported outcomes following surgery for degenerative spondylolitshtesis: comparison of a universal and multitier health care system. Spine J. 2019;19:24–33. [DOI] [PubMed] [Google Scholar]
- 56. Diebo BG, Tishelman JC, Horn S, et al. The impact of mental health on patient-reported outcomes in cervical radiculopathy or myelopathy surgery. J Clin Neurosci. 2018;54:102–108. [DOI] [PubMed] [Google Scholar]
- 57. Goh TS, Shin JK, Youn MS, Lee JS. Effects of psychiatric factors on patient-reported outcomes after surgical correction of lumbar degenerative kyphosis. Asian Spine J. 2018;12:126–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Netto MB, Barranco ABS, Oliveira KWK, Petronilho F. Influence of anxiety and depression symptoms on the quality of life in patients undergoing lumbar spine surgery. Rev Bras Ortop. 2018;53:38–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Nayar G, Elsamadicy AA, Zakare-Fagbamila R, Farquhar J, Gottfried ON. Impact of affective disorders on recovery of baseline function in patients undergoing spinal surgery: a single institution study of 275 patients. World Neurosurg. 2017;100:69–73. [DOI] [PubMed] [Google Scholar]
- 60. Alentado VJ, Caldwell S, Gould HP, Steinmetz MP, Benzel EC, Mroz TE. Independent predictors of a clinically significant improvement after lumbar fusion surgery. Spine J. 2017;17:236–243. [DOI] [PubMed] [Google Scholar]
- 61. Maratos EC, Trivedi R, Richards H, Seeley H, Laing RJ. Psychological distress does not compromise outcome in spinal surgery. Br J Neurosurg. 2012;26:466–471. [DOI] [PubMed] [Google Scholar]
- 62. Bakhsheshian J, Scheer JK, Gum JL, et al. Impact of poor mental health in adult spinal deformity patients with poor physical function: a retrospective analysis with a 2-year follow-up. J Neurosurg Spine. 2017;26:116–124. [DOI] [PubMed] [Google Scholar]
- 63. Doi T, Nakamoto H, Nakajima K, et al. Effect of depression and anxiety on health-related quality of life outcomes and patient satisfaction after surgery for cervical compressive myelopathy. J Neurosurg Spine. 2019:1-8 doi:10.3171/2019.6.SPINE19569 [DOI] [PubMed] [Google Scholar]
- 64. Divi SN, Goyal DKC, Mangan JJ, et al. Are outcomes of anterior cervical discectomy and fusion influenced by presurgical depression symptoms on the Mental Component Score of the Short Form-12 Survey [published online September 6, 2019]? Spine (Phila Pa 1976). doi:10.1097/BRS.0000000000003231 [DOI] [PubMed] [Google Scholar]
- 65. Poorman GW, Passias PG, Horn SR, et al. ; International Spine Study Group. Despite worse baseline status depressed patients achieved outcomes similar to those in nondepressed patients after surgery for cervical deformity. Neurosurg Focus. 2017;43:E10. [DOI] [PubMed] [Google Scholar]
- 66. Lee J, Kim HS, Shim KD, Park YS. The effect of anxiety, depression, and optimism on postoperative satisfaction and clinical outcomes in lumbar spinal stenosis and degenerative spondylolisthesis patients: cohort study. Clin Orthop Surg. 2017;9:177–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Theologis AA, Ailon T, Scheer JK, et al. ; International Spine Study Group. Impact of preoperative depression on 2-year clinical outcomes following adult spinal deformity surgery: the importance of risk stratification based on type of psychological distress. J Neurosurg Spine. 2016;25:477–485. [DOI] [PubMed] [Google Scholar]
- 68. Kobayashi Y, Ogura Y, Kitagawa T, et al. The influence of preoperative mental health on clinical outcomes after laminectomy in patients with lumbar spinal stenosis. Clin Neurol Neurosurg. 2019;185:105481. [DOI] [PubMed] [Google Scholar]
- 69. Mayo BC, Massel DH, Bohl DD, et al. Preoperative mental health is not predictive of patient-reported outcomes following a minimally invasive lumbar discectomy. Clin Spine Surg. 2017;30:E1388–E1391. [DOI] [PubMed] [Google Scholar]
- 70. Merrill RK, Zebala LP, Peters C, Qureshi SA, McAnany SJ. Impact of depression on patient-reported outcome measures after lumbar spine decompression. Spine (Phila Pa 1976). 2018;43:434–439. [DOI] [PubMed] [Google Scholar]
- 71. Anderson JT, Haas AR, Percy R, Woods ST, Ahn UM, Ahn NU. Chronic opioid therapy after lumbar fusion surgery for degenerative disc disease in a workers’ compensation setting. Spine (Phila Pa 1976). 2015;40:1775–1784. [DOI] [PubMed] [Google Scholar]
- 72. Connolly J, 3rd, Javed Z, Raji MA, Chan W, Kuo YF, Baillargeon J. Predictors of long-term opioid use following lumbar fusion surgery. Spine (Phila Pa 1976). 2017;42:1405–1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Schoenfeld AJ, Nwosu K, Jiang W, et al. Risk factors for prolonged opioid use following spine surgery, and the association with surgical intensity, among opioid-naive patients. J Bone Joint Surg Am. 2017;99:1247–1252. [DOI] [PubMed] [Google Scholar]
- 74. Menendez ME, Ring D, Bateman BT. Preoperative opioid misuse is associated with increased morbidity and mortality after elective orthopaedic surgery. Clin Orthop Relat Res. 2015;473:2402–2412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Armaghani SJ, Lee DS, Bible JE, et al. Preoperative opioid use and its association with perioperative opioid demand and postoperative opioid independence in patients undergoing spine surgery. Spine (Phila Pa 1976). 2014;39:E1524–E1530. [DOI] [PubMed] [Google Scholar]
- 76. Dunn LK, Durieux ME, Fernandez LG, et al. Influence of catastrophizing, anxiety, and depression on in-hospital opioid consumption, pain, and quality of recovery after adult spine surgery. J Neurosurg Spine. 2018;28:119–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Harris AB, Marrache M, Jami M, et al. Chronic opioid use following anterior cervical discectomy and fusion surgery for degenerative cervical pathology. Spine J. 2019;S1529-9430(19)30975-1 doi:10.1016/j.spinee.2019.09.011 [DOI] [PubMed] [Google Scholar]
- 78. Wright AK, Sikora M, Leveque JC. Characterizing the risk of long-term opioid utilization in patients undergoing lumbar spine surgery [published August 13, 2019]. Spine (Phila Pa 1976). doi:10.1097/BRS.0000000000003199 [DOI] [PubMed] [Google Scholar]
- 79. Patton CM, Hung M, Lawrence BD, et al. Psychological distress in a Department of Veterans Affairs spine patient population. Spine J. 2012;12:798–803. [DOI] [PubMed] [Google Scholar]
- 80. Gatchel RJ, Mayer TG. Psychological evaluation of the spine patient. J Am Acad Orthop Surg. 2008;16:107–112. [DOI] [PubMed] [Google Scholar]
- 81. Marek RJ, Block AR, Ben-Porath YS. The Minnesota Multiphasic Personality Inventory-2-Restructured Form (MMPI-2-RF): incremental validity in predicting early postoperative outcomes in spine surgery candidates. Psychol Assess. 2015;27:114–124. [DOI] [PubMed] [Google Scholar]
- 82. Daubs MD, Patel AA, Willick SE, et al. Clinical impression versus standardized questionnaire: the spinal surgeon’s ability to assess psychological distress. J Bone Joint Surg Am. 2010;92:2878–2883. [DOI] [PubMed] [Google Scholar]
- 83. Main CJ, Wood PL, Hollis S, Spanswick CC, Waddell G. The Distress and Risk Assessment Method. A simple patient classification to identify distress and evaluate the risk of poor outcome. Spine (Phila Pa 1976). 1992;17:42–52. [DOI] [PubMed] [Google Scholar]
- 84. Deyo RA, Walsh NE, Schoenfeld LS, Ramamurthy S. Studies of the Modified Somatic Perceptions Questionnaire (MSPQ) in patients with back pain. Psychometric and predictive properties. Spine (Phila Pa 1976). 1989;14:507–510. [DOI] [PubMed] [Google Scholar]
- 85. Abtahi AM, Brodke DS, Lawrence BD, Zhang C, Spiker WR. Association between patient-reported measures of psychological distress and patient satisfaction scores after spine surgery. J Bone Joint Surg Am. 2015;97:824–828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Young AK, Young BK, Riley LH, 3rd, Skolasky RL. Assessment of presurgical psychological screening in patients undergoing spine surgery: use and clinical impact. J Spinal Disord Tech. 2014;27:76–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Grevitt M, Pande K, O’Dowd J, Webb J. Do first impressions count? A comparison of subjective and psychologic assessment of spinal patients. Eur Spine J. 1998;7:218–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Omidi-Kashani F, Faridhoseini F, Ariamanesh S, Kazar MH, Baradaran A. Failure rate of spine surgeons in preoperative clinical screening of severe psychological disorders. Clin Orthop Surg. 2016;8:164–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Adogwa O, Elsamadicy AA, Cheng J, Bagley C. Pretreatment of anxiety before cervical spine surgery improves clinical outcomes: a prospective, single-institution experience. World Neurosurg. 2016;88:625–630. [DOI] [PubMed] [Google Scholar]
- 90. Elsamadicy AA, Adogwa O, Cheng J, Bagley C. Pretreatment of depression before cervical spine surgery improves patients’ perception of postoperative health status: a retrospective, single institutional experience. World Neurosurg. 2016;87:214–219. [DOI] [PubMed] [Google Scholar]
- 91. Pakarinen M, Vanhanen S, Sinikallio S, et al. Depressive burden is associated with a poorer surgical outcome among lumbar spinal stenosis patients: a 5-year follow-up study. Spine J. 2014;14:2392–2396. [DOI] [PubMed] [Google Scholar]