Abstract
Study Design:
Retrospective cohort study.
Objective:
Develop a simple scoring system to estimate proximal junctional kyphosis (PJK) risk.
Methods:
A total of 417 adult spinal deformity (ASD) patients (80% females, 57.8 years) with 2-year follow-up were included. PJK was defined as a >10° kyphotic angle between the upper-most instrumented vertebra (UIV) and the vertebrae 2 levels above the UIV (UIV+2). Based on a previous literature review, the following point score was attributed to parameters likely to impact PJK development: age >55 years (1 point), fusion to S1/ilium (1 point), UIV in the upper thoracic spine (UIV-UT: 1 point), UIV in the lower thoracic region (UIV-LT: 2 points), flattening of the thoracic kyphosis (TK) relative to the lumbar lordosis (LL; ie, ▵LL − ▵TK) greater than 10° (1 point).
Results:
At 2 years, the overall PJK rate was 43%. The odds ratios for each risk factor were the following: age >55 years (2.52), fusion to S1/ilium (5.17), UIV-UT (6.63), UIV-LT (8.24), and ▵LL − ▵TK >10° (1.59). Analysis by risk factor revealed a significant impact on PJK (no PJK vs PJK): age >55 years (28% vs 51%, P < .001), LIV S1/ilium (16.3% vs 51.4%, P < .001), UIV in lower thoracic spine (12.0% vs 38.7% vs 52.9%, P < .001), and a >10° surgical reduction in TK relative to LL increase (40.0% vs 51.5%, P < .001). The PJK rate by point score was as follows: 1 = 17%, 2 = 29%, 3 = 40%, 4 = 53%, and 5 = 69%.
Conclusion:
A pragmatic scoring system was developed that is tied to the increasing risk of PJK. These findings are helpful for surgical planning and preoperative counseling.
Keywords: proximal junctional kyphosis, adult spinal deformity, scoring system, risk factors, sagittal alignment
Introduction
Symptomatic adult spinal deformity (ASD), an increasingly prevalent disorder with the aging population, may warrant surgical intervention as a means of improving pain and disability.1,2 There has been a marked increase in the number of ASD surgeries over the past decade.3 While there are clear benefits to ASD surgery, complication rates remain high.4 Among the potential complications, instrumentation-related (ie, mechanical) complications are among the most common; consequently, these high mechanical complication rates necessitate further research.
Among the most common complications of ASD surgery is proximal junctional kyphosis (PJK).3 While many cases of PJK are incidental, benign radiographic findings, a subset of these complications can be more severe and warrant extensive revision surgery. There remains debate over the risk factors that predispose patients to PJK. Past studies have suggested that pathology of adjacent segments may predispose patients to developing PJK, while other research has linked both the type of surgical correction5-7 (eg, anterior vs posterior approach, choice of the upper-most instrumented vertebra [UIV]) and the operative instrumentation (rod bending, screws, hooks, etc)6-9 to the development of PJK. Additionally, the development of PJK has been suggested to be associated with patient demographics.6,10,11
These risk factors were recently identified and studied in a systematic literature review and meta-analysis. The results reported are extensive and demonstrate the relationship between more than 20 risk factors and PJK development.6,9,12 However, these factors cannot be easily applied in the clinical setting due to the extensive number of factors. Consequently, there is a need for a simplified score to assess risk of PJK on the basis of previously identified risk factors. Our objective in the present study was to focus on the risk factors for PJK that appear to be most impactful based on previous studies and generate a simplified scoring system that can be applied preoperatively as a means of predicting the risk of PJK following surgical correction of ASD.
Methods
Ethical Standards
This study was conducted in compliance with all applicable local, state, and national laws and regulations. Furthermore, all data were collected and analyzed with institutional review board approval.
Study Design
This was a retrospective review of a prospectively collected, multicenter database. Data were collected at 11 sites throughout the United States.
Subjects
The first inclusion criterion was surgical treatment for ASD. Furthermore, patients were only included if they were eligible for a minimum of 2 years of follow-up following surgical treatment. Radiographic measures served as further inclusion criteria. Specifically, we only included patients with a major coronal Cobb angle of equal to or greater than 20° (Cobb ≥ 20°), a sagittal vertical axis (SVA) greater than or equal to 5 cm (SVA ≥ 5 cm), a pelvic tilt (PT) greater than or equal to 25° (PT ≥ 25°), and/or a thoracic kyphosis (TK) greater than or equal to 60° (TK ≥ 60°). Last, patients were excluded if they underwent a revision procedure between their baseline, postsurgical encounter, and their second-year follow-up.
Data Collection
Following inclusion and exclusion of subjects, data of interest were queried, measured, and calculated. First, demographic data including age and sex were queried from our database. Subsequently, utilizing surgical information, the positions of the UIV and lower-most instrumented vertebra (LIV) were determined. Radiographic measures were obtained from standing full-length (36-inch) radiographs that were measured at a central location using the validated Spineview Software (Spineview, ENSAM, Paris).13 To ensure reliability, all X-ray measurements were performed by a single, experienced reader and verified by a second experienced reader. Measurements were then used to generate radiographic parameters within the Matlab suite (Matlab 2015b, MathWorks, Natick, MA).
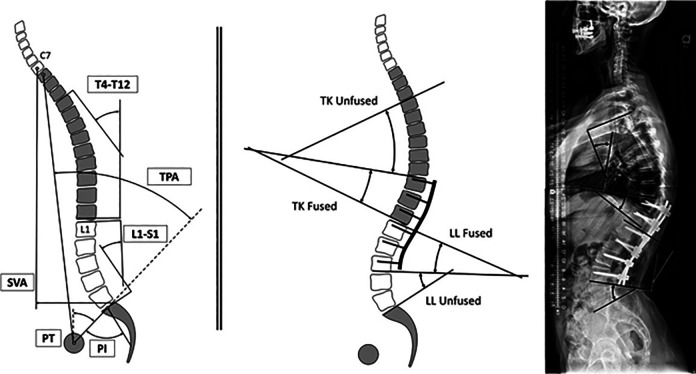
Spinopelvic parameters, shown in Figure 1, including pelvic incidence (PI), PT, lumbar lordosis (LL), and T1 pelvic angle (T1PA) were assessed using standard methodology based on previous literature.14-17 Furthermore, the magnitude of the thoracic and lumbar curvatures were assessed in both fused and unfused portions of the cures.
Figure 1.
Left: Classic spino-pelvic parameters included on this analysis: pelvic incidence (PI), pelvic tilt (PT), lumbar lordosis (LL; L1-S1), thoracic kyphosis (T4-T12), sagittal vertical axis (SVA), and T1 pelvic angle (TPA). Right: Lumbar and thoracic curvatures analyzed by segment: L1-S1 = LL fused + LL Unfused; T4-T12 = TK Fused + TK unfused.
Additionally, angles of spinal alignment were also calculated. The PJK angle was calculated as the Cobb angle between the inferior endplate of the previously identified UIV and the superior endplate of the vertebra 2 levels above the UIV (UIV+2). With respect to identifying surgical fusions, we considered each curvature of the spine as “fused” if the fused vertebral levels were within the boundaries of the instrumentation. To be specific, the LL was considered fused between the LIV and L1 and unfused between S1 and the LIV. For example, an L1-L4 fusion would be considered unfused between S1 and L4, and fused between L1 and L4. Accordingly, the TK was considered fused between T12 and the UIV and considered unfused between UIV and T4. Following calculation of relevant parameters, the SRS-Schwab classification system was employed for deformity classification.18
PJK Scoring
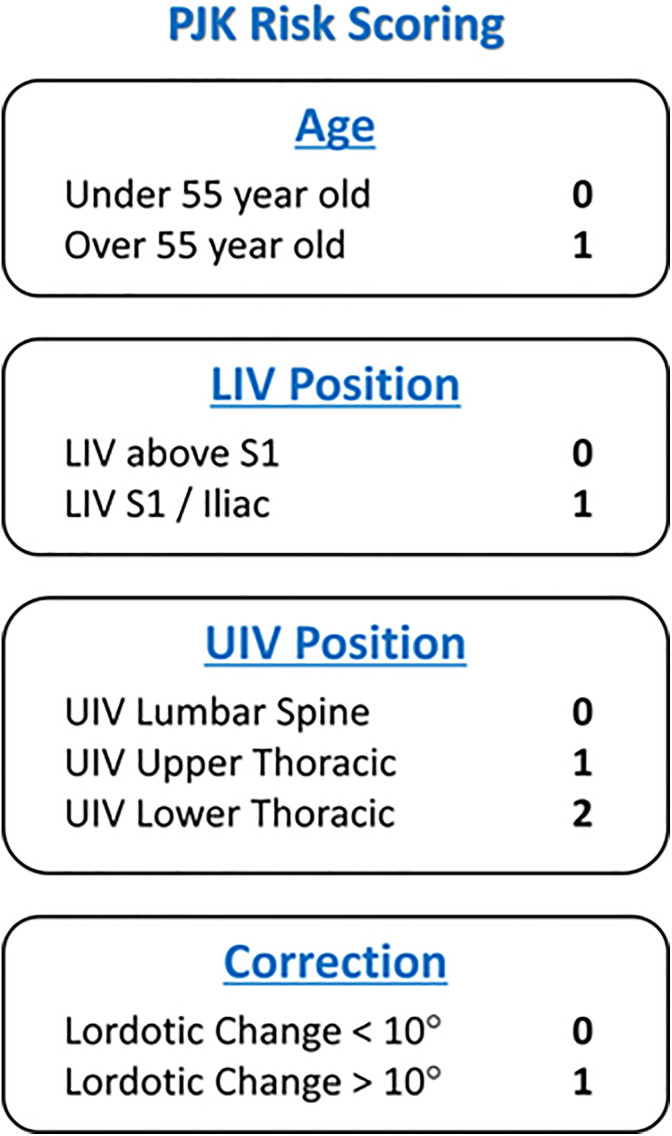
In order to determine the rate of PJK, we first used the definition of PJK previously reported by Glattes et al,19 as a kyphotic angle greater than 10° between the UIV and the UIV+2 and a kyphotic change greater than 10° between baseline and follow-up at 2 years. Accordingly, we then determined the rate of radiographic PJK using radiographs at the 2-year follow-up. Using the risk factors previously identified by meta-analysis, the following 5 risk factors were then assessed on our dataset: (1) age >55 years, (2) fusion including S1/Ilium, (3) UIV within the upper thoracic region (T1-T6), (4) UIV within the lower thoracic region (T7-T12), and (5) magnitude of lordotic correction.6 To define this lordotic correction, we assigned the angle associated with the kyphotic curvature as negative and the angle associated with the lordotic curvature as positive. The change in TK and LL within the fused spine was recorded between baseline and 2-year follow-up. Subsequently, the sum of these values was identified as the magnitude of lordotic correction. If the magnitude of lordotic correction was greater than 10°, a single point was given. Henceforth, this arithmetic sum will be referred to lordotic correction. For risk factors (1), (2), (3), and (5), a single point was assigned for each criterion met, while 2 points were assigned if criterion (4) was met (Figure 2). This scoring methodology was based on the odds ratios presented in a previous meta-analysis.6 The sum of points was defined as the PJK risk score. Patients were stratified by each of the 5 criteria, and the rate of radiographic PJK was assessed using χ2 test. The relationship between an increase in PJK score and postoperative PJK angle was assessed using Spearman correlation.
Figure 2.
Chart of the PJK Risk Scoring System. LIV, lower-most instrumented vertebra; UIV, upper-most instrumented vertebra.
Results
Radiographic Measures and SRS-Schwab Classification
Of 603 eligible patients, 417 (69.1%) had sufficient data to be included in the analysis. The mean age was 57.8 ± 14.9 years with a mean body mass index (BMI) of 27.2 ± 5.68. Women comprised a majority of included subjects (80.8%). At baseline, the mean coronal C7 plumb line (C7PL) offset was 35.5 ± 34.3 mm with a mean absolute major Cobb angle of 42.1 ± 20.2°.
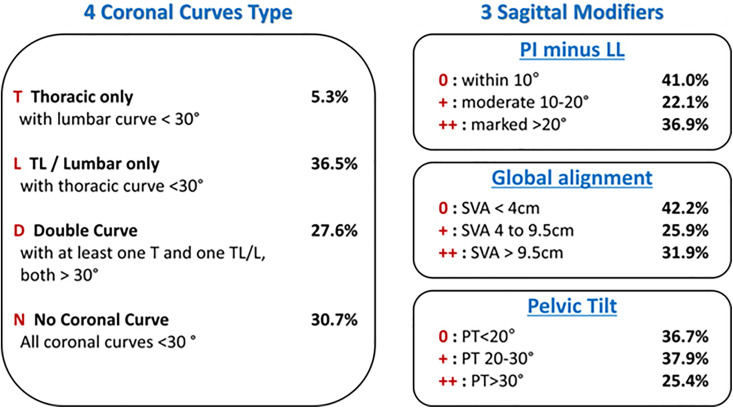
Sagittal alignment changed significantly between baseline and 2-year follow-up. PT significantly decreased from a mean of 23.5° to a mean of 21.0° at 2-year follow-up (P < .001). Similarly, PI-LL mismatch significantly decreased (80.7%) between baseline and 2-year follow-up (P < .001). Significant decreases at 2-year follow-up were observed for SVA and T1 pelvic angle (TPA; 53.4% and 23.2%, respectively, P < .001; Table 1). The prevalence of curve type and sagittal modifiers, based on the SRS-Schwab Classification, are shown in Figure 3.
Table 1.
Description of Sagittal Parameters Between Baseline and 2-Year Follow-up.
| Parameters | Baseline | 2 Years | Change (▵) | P | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| PT (°) | 23.5 | 11.0 | 21.0 | 10.2 | −2.4 | 8.2 | <.001 |
| PI-LL (°) | 15.0 | 21.4 | 2.8 | 15.2 | −12.1 | 18.4 | <.001 |
| SVA (mm) | 65.1 | 75.8 | 30.3 | 55.4 | −34.8 | 67.3 | <.001 |
| TPA (°) | 22.4 | 13.8 | 17.2 | 11.2 | −5.2 | 10.8 | <.001 |
Abbreviations: PT, pelvic tilt; PI, pelvic incidence; LL, lumbar lordosis; SVA, sagittal vertical axis; TPA, T1 pelvic angle.
Figure 3.
SRS-Schwab classification threshold. Percentage of the population associated with each category.
Patients were stratified into groups on the basis of each individual scoring criterion. There was a minimum of 25 patients in each possible score within each group. Furthermore, within each scoring criteria group, there was increase in the proportion of patients with PJK as the score increased (Table 2).
Table 2.
Patients Sorted by Score Criteria With Associated Proximal Junctional Kyphosis (PJK) Rates.
| Age | <55 years | >55 years | P | |
| Number of Patients | 141 | 276 | — | |
| PJK rate | 28.40% | 50.00% | P < .001 | |
| LIV Position | Within Spine | S1/Ilium | P | |
| Number of patients | 92 | 325 | — | |
| PJK rate | 16.30% | 50.20% | P < .001 | |
| UIV Position | L1-S1 | T12-T7 | T6-T1 | P |
| Number of patients | 25 | 172 | 215 | — |
| PJK rate | 12.00% | 38.70% | 52.90% | P < .001 |
| Correction Criteria | ▵ Lordosis >10° | ▵ Lordosis <10° | P | |
| Number of patients | 171 | 215 | — | |
| PJK rate | 40.00% | 51.50% | P < .001 |
Abbreviations: PJK, proximal junctional kyphosis; LIV, lower-most instrumented vertebra; UIV, upper-most instrumented vertebra.
Analysis of individual scoring criteria revealed that a positive score for each criterion was associated with increased odds of developing PJK. A UIV within the lower thoracic region was the most significantly associated with developing PJK, while LIV within the pelvis was the second most significantly associated criterion (Table 3).
Table 3.
Odds Ratio of Scoring Criteria as Independent Predictors of PJK.
| Dependent Variable | Covariate | OR [95% CI] | P |
|---|---|---|---|
| Age | <55 years | Ref | — |
| >55 years | 2.525 [1.633-3.903] | ||
| LIV | LIV within spine | Ref | — |
| LIV within pelvis | 5.165 [2.851-9.358] | ||
| Upper thoracic UIV | Lumbar UIV | Ref | — |
| Upper thoracic UIV | 4.632 [1.345-15.954] | ||
| Lower thoracic UIV | Lumbar UIV | Ref | — |
| Lower thoracic UIV | 8.239 [2.377-28.552] | ||
| Correction | ▵ Lordosis >10° | Ref | — |
| ▵ Lordosis <10° | 1.590 [1.060-2.395] |
Abbreviations: PJK, proximal junctional kyphosis; OR, odds ratio; CI, confidence interval; LIV, lower-most instrumented vertebra; UIV, upper-most instrumented vertebra.
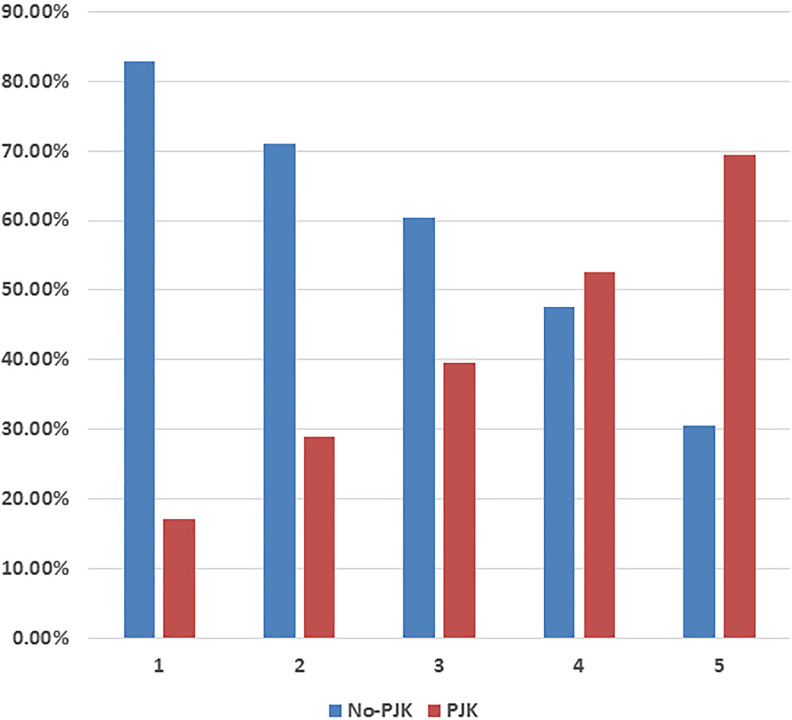
A comparison of the rate of PJK among patients with varying PJK risk scores revealed a significant difference between the score groups (P < .001). At a score of 1, approximately 17% met the inclusion criteria for radiographic PJK, while 69% of patients with a PJK score of 5 met the radiographic inclusion criteria for PJK. Thus, an increase in PJK risk score was associated with a progressive increase in the proportion of scored patients which met the previously defined radiographic inclusion criteria for PJK (Figure 4).
Figure 4.
Rate of proximal junctional kyphosis (PJK) across the score groups.
Appropriately, as the PJK risk score increased there was a progressive increase in the odds associated with developing PJK. While progressive score increases were linked to increased odds, a PJK risk score of 5 was most strongly associated (11.0 times) the odds of developing PJK, while a risk score of 4 was the second most strongly associated with 5.3 times the odds of developing PJK (P < .001; Table 4).
Table 4.
Logistic Regression of PJK Risk Scores as Independent Predictors of PJK.
| Dependent Variable | Covariate | OR [95% CI] | P |
|---|---|---|---|
| PJK | Risk score of 1 | Ref | — |
| Risk score of 2 | — | .225 | |
| Risk score of 3 | 3.2 [1.9-5.2] | .020 | |
| Risk score of 4 | 5.3 [3.3-8.6] | <.001 | |
| Risk score of 5 | 11.0 [6.4-18.9] | <.001 |
Abbreviations: PJK, proximal junctional kyphosis; OR, odds ratio; CI, confidence interval.
A significant association was found between an increase in PJK score and an increase in PJK angle (r = −0.268; P < .001). A higher PJK score was associated with a larger focal kyphosis at the UIV level.
Discussion
This study has identified that the 5 parameters, identified with literature review and tested using our dataset, are individually associated with an increase in the rate of PJK. Furthermore, the scoring system applied quantifies a significant increase in PJK rates as the score increases. Specifically, while the occurrence of PJK in patients with a score of 1 was approximately 15%, patients with a score of 5 had a PJK rate of nearly 70%. As such, we have demonstrated that a straightforward scale may be used to quantify both the potential risk of developing PJK and the severity of PJK in at-risk populations.
Our findings are consistent with previous reports. Past meta-analyses have identified that an age greater than 55 years had 2.19 times the odds of developing PJK compared with those less than 55 years of age, and we have noted a similar odds ratio of 2.59 within our study population.6 In general, age may be a surrogate measure for a combination of increased comorbidity, frailty, poor muscle quality, and overall poor health. As such, age itself may not present a risk for developing a PJK but may serve as a representative variable that reflects the varied comorbidities that may increase the risk for PJK.
Within the same meta-analysis, the odds of developing PJK were reported as 2.12 times higher in patients with a fusion that included the pelvis; however, we have noted a higher odds ratio of 5.17. This result may simply be due to the small proportion of patients whose fusion did not include the pelvis (22%). As such, it may be that the population studied herein varies from past research with respect to patient profile and number of levels fused. This variation may be attributable to our population, ASD surgical patients, who were typically addressed surgically with a longer fusion that commonly included the pelvis in order to promote lumbosacral fusion and lend increased stability.20
With regard to the impact of the UIV, our analysis yielded an odds ratio that was slightly increased relative to past research (4.63 vs 2.38).21 As past research primarily focused on the idiopathic scoliosis population, this discrepancy may indicate that the impact of UIV selection on the development of PJK may vary based on etiology of deformity. In addition, past research compared an upper thoracic UIV to a lower thoracic UIV while we compared an upper thoracic UIV to a lumbar UIV. As such, relative to an upper thoracic UIV, a lumbar UIV appears associated with a lower rate of PJK than a lower thoracic UIV. Interestingly, we noted that a UIV location within the lower thoracic region was associated with the largest odds of developing PJK. This trend has been previously described in literature22 and, within our study, may simply reflect the large proportion of patients with lower thoracic UIV.
Finally, our last scoring criteria was lordotic correction, which has been frequently linked to PJK.5,11,23 As previously defined, the lordotic correction refers to the difference between the change in LL and TK between preoperative and postoperative end-points (▵LL − ▵TK). While many past studies have examined the role of SVA in assessing the impact of surgical intervention on sagittal alignment, the use of SVA to assess the risk of developing PJK is limited by the nature of SVA. As defined by previous research, SVA varies with patient position and pelvic rotation which classifies SVA as a dynamic parameter. Consequently, SVA is modulated by compensatory mechanisms such as PJK. On the other hand, lordotic and kyphotic change can be controlled through surgical intervention and be quantified preoperatively with software. Thus, while other radiographic parameters are associated with PJK, using lordotic correction as a scoring parameter is justified by its surgical malleability and relative inelasticity to compensatory mechanisms. Furthermore, the degree of lordotic mismatch may be mitigated through preparing the thoracic spine for reciprocal change on restoration of the LL. This may be done through introducing a kyphotic bend in the proximal portion of the rod and may represent a means for mitigating potential risk of developing PJK.
Given the potentially impactful consequences of PJK, a clear, point-based risk assessment tool provides clear clinical applications. During preoperative risk assessment, this scale may be used during patient counseling in order to aid the patient and clinician in the evaluation of risks and benefits posed by operative intervention. Furthermore, the use of a scoring system may allow clinicians to easily quantify risk and assess whether the planned intervention is suitable. For example, a 70-year-old patient that is initially planned to have a fusion from T10 to the ilium with a planned correction of ▵LL = 25 and ▵TK = −10 would be scored as 0 (age < 55) + 1 (LIV = ilium) + 2 (UIV = T10) + 1 (Lordotic-Kyphotic imbalance greater than 10) = PJK Score 5, presenting an overall 69% chance of developing PJK (Figure 5). However, if the same patient is planned to undergo a fusion from T4 to the ilium, with a planned correction of ▵LL = 20 and ▵TK = 10 they would be scored as 0 (age < 55) + 1 (LIV = Ilium) + 1 (UIV = T4) + 0 (LL-TK mismatch < 10) = 2, presenting an overall risk of 29%. The second plan included a smaller correction while restoring thoracic alignment with a longer fusion, and had an appreciable 41% decrease in risk of developing PJK. Consequently, preoperative changes based on risk assessment may allow clinicians to avoid procedures that pose a significant risk for developing PJK.
Figure 5.
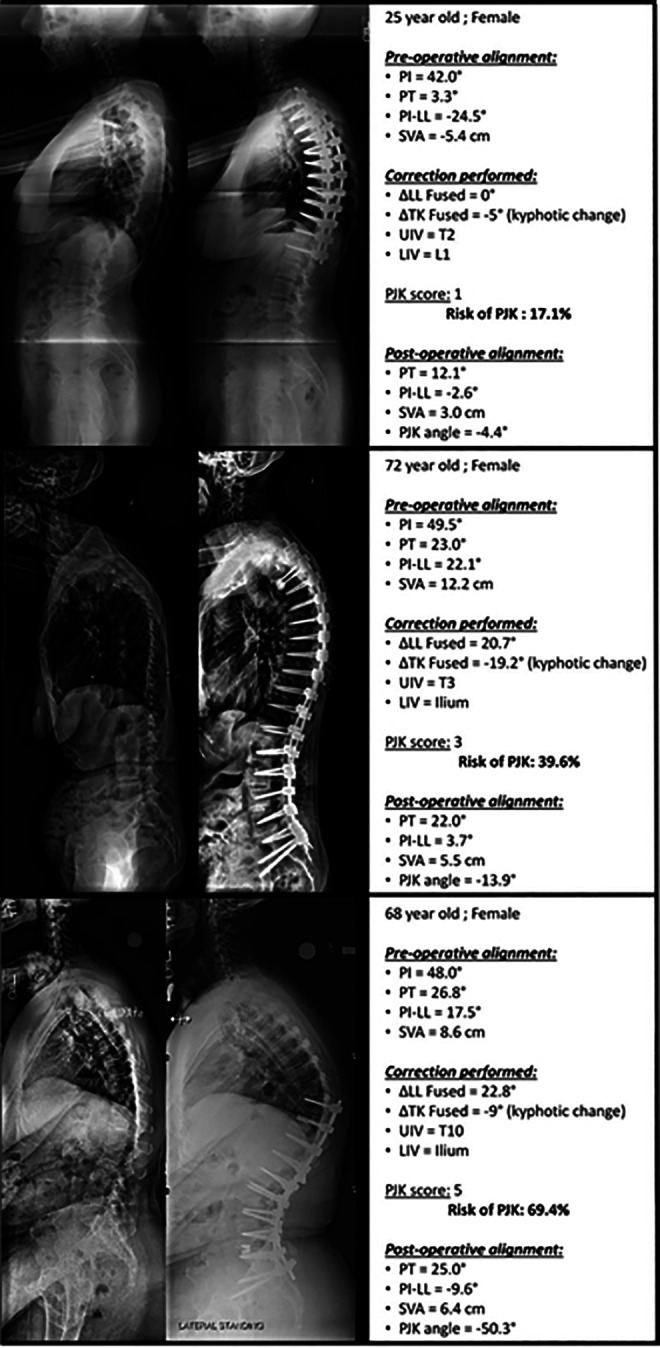
Example of 3 patients with PJK (proximal junctional kyphosis) scores ranging from 1 to 5 and their postoperative sagittal alignment. As the score increases from 1 to 5, postoperative PJK becomes increasingly severe (up to 50° of focal kyphosis).
While the scoring system described herein presents a method to optimize surgical intervention that may decrease risk of developing PJK, this scoring methodology does not suggest that every patient is eligible for preoperative optimization. For patients with a substantial degree of deformity that present at an advanced age, it is possible that corrective surgery will necessarily introduce a higher-than-desired risk of developing PJK. These patients must be addressed individually as the risk of developing PJK should be weighed against the relative benefit of operative intervention over nonoperative treatment. In cases where low bone mineral density (BMD) predisposes a patient to PJK, treatment with teriparatide aimed at increasing BMD may provide a means to reduce the risk of PJK.24 Additionally, past research has identified muscular wasting as a risk factor for the development of PJK.25 Consequently, muscular reinforcement, for example, using prophylactic preoperative physical therapy, may provide additional benefit for patients with compromised muscular integrity.
Limitations
While our analysis provides promising results, we were unable to fully assess all factors identified in the literature. Several past studies have referenced the degree to which BMD may influence the development of PJK,26,27 but we were unable to incorporate BMD due to low availability of BMD data within our data set. Future work is needed to determine the degree to which BMD may be incorporated into the PJK scoring criteria listed herein. Additionally, while the scoring criteria provides useful information, it does not provide a method to assess patient-specific factors, which would suggest that prophylactic instrumentation, such as tethering, should be employed to reduce risk of PJK.
Conclusion
This study furthers our understanding of the association between published factors and PJK. We provide a simple pragmatic scoring system for the prediction of risk of PJK following surgery for ASD. The findings from this study may permit enhanced shared decision making and patient counseling preoperatively. Additionally, based on the results of this investigation, surgeons may consider altering their surgical strategy to mitigate the risk of postoperative development of PJK.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The International Spine Study Group (ISSG) is funded through research grants from DePuy Synthes (current), Nuvasive (current), K2M (current), Innovasis (past), Biomet (past), and individual donations.
ORCID iD: Renaud Lafage, MS  https://orcid.org/0000-0002-4820-1835
https://orcid.org/0000-0002-4820-1835
Han Jo Kim, MD  https://orcid.org/0000-0003-2170-3592
https://orcid.org/0000-0003-2170-3592
References
- 1. Schwab F, Dubey A, Gamez L, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine (Phila Pa 1976). 2005;30:1082–1085. [DOI] [PubMed] [Google Scholar]
- 2. Schwab FJ, Lafage V, Farcy JP, Bridwell KH, Glassman SSD, Shainline MR. Predicting outcome and complications in the surgical treatment of adult scoliosis. Spine (Phila Pa 1976). 2008;33:2243–2247. doi:10.1097/BRS.0b013e31817d1d4e [DOI] [PubMed] [Google Scholar]
- 3. Sciubba DM, Yurter A, Smith JS, et al. A comprehensive review of complication rates after surgery for adult deformity: a reference for informed consent. Spine Deform. 2015;3:575–594. doi:10.1016/j.jspd.2015.04.005 [DOI] [PubMed] [Google Scholar]
- 4. Smith JS, Klineberg E, Lafage V, et al. Prospective multicenter assessment of perioperative and minimum 2-year postoperative complication rates associated with adult spinal deformity surgery. J Neurosurg Spine. 2016;25:1–14. doi:10.3171/2015.11.SPINE151036 [DOI] [PubMed] [Google Scholar]
- 5. Mendoza-Lattes S, Ries Z, Gao Y, Weinstein SL. Proximal junctional kyphosis in adult reconstructive spine surgery results from incomplete restoration of the lumbar lordosis relative to the magnitude of the thoracic kyphosis. Iowa Orthop J. 2011;31:199–206. [PMC free article] [PubMed] [Google Scholar]
- 6. Liu FY, Wang T, Yang SD, Wang H, Yang DL, Ding WY. Incidence and risk factors for proximal junctional kyphosis: a meta-analysis. Eur Spine J. 2016;25:2376–2383. doi:10.1007/s00586-016-4534-0 [DOI] [PubMed] [Google Scholar]
- 7. Kim HJ, Bridwell KH, Lenke LG, et al. Patients with proximal junctional kyphosis requiring revision surgery have higher postoperative lumbar lordosis and larger sagittal balance corrections. Spine (Phila Pa 1976). 2014;39:E576–E580. doi:10.1097/BRS.0000000000000246 [DOI] [PubMed] [Google Scholar]
- 8. Cammarata M, Aubin CÉ, Wang X, Mac-Thiong JM. Biomechanical risk factors for proximal junctional kyphosis: a detailed numerical analysis of surgical instrumentation variables. Spine (Phila Pa 1976). 2014;39:E500–E507. doi:10.1097/BRS.0000000000000222 [DOI] [PubMed] [Google Scholar]
- 9. Lau D, Clark AJ, Scheer JK, et al. Proximal junctional kyphosis and failure after spinal deformity surgery: a systematic review of the literature as a background to classification development. Spine (Phila Pa 1976). 2014;39:2093–2102. doi:10.1097/BRS.0000000000000627 [DOI] [PubMed] [Google Scholar]
- 10. Park HJ, Sim T, Suh SW, Yang JH, Koo H, Mun JH. Analysis of coordination between thoracic and pelvic kinematic movements during gait in adolescents with idiopathic scoliosis. Eur Spine J. 2016;25:385–393. doi:10.1007/s00586-015-3931-0 [DOI] [PubMed] [Google Scholar]
- 11. Yagi M, King AB, Boachie-Adjei O. Incidence, risk factors, and natural course of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Minimum 5 years of follow-up. Spine (Phila Pa 1976). 2012;37:1479–1489. doi:10.1097/BRS.0b013e31824e4888 [DOI] [PubMed] [Google Scholar]
- 12. Cho SK, Shin JI, Kim YJ. Proximal junctional kyphosis following adult spinal deformity surgery. Eur Spine J. 2014;23:2726–2736. doi:10.1007/s00586-014-3531-4 [DOI] [PubMed] [Google Scholar]
- 13. Champain S, Benchikh K, Nogier A, Mazel C, Guise JD, Skalli W. Validation of new clinical quantitative analysis software applicable in spine orthopaedic studies. Eur Spine J. 2006;15:982–991. doi:10.1007/s00586-005-0927-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Diebo BG, Ferrero E, Lafage R, et al. Recruitment of compensatory mechanisms in sagittal spinal malalignment is age and regional deformity dependent: a full-standing axis analysis of key radiographical parameters. Spine (Phila Pa 1976). 2015;40:642–649. doi:10.1097/BRS.0000000000000844 [DOI] [PubMed] [Google Scholar]
- 15. Lafage V, Diebo BG, Schwab F. Sagittal Spino-Pelvic Alignment: From Theory to Clinical Application. Madrid, Spain: Editorial Medica Panamericana; 2015. [Google Scholar]
- 16. Protopsaltis T, Schwab F, Bronsard N, et al. The T1 pelvic angle, a novel radiographic measure of global sagittal deformity, accounts for both spinal inclination and pelvic tilt and correlates with health-related quality of life. J Bone Joint Surg Am. 2014;96:1631–1640. doi:10.2106/JBJS.M.01459 [DOI] [PubMed] [Google Scholar]
- 17. Lafage R, Schwab F, Challier V, et al. Defining spino-pelvic alignment thresholds: should operative goals in adult spinal deformity surgery account for age? Spine (Phila Pa 1976). 2016;41:62–68. doi:10.1097/BRS.0000000000001171 [DOI] [PubMed] [Google Scholar]
- 18. Schwab FJ, Ungar B, Blondel B, et al. Scoliosis Research Society—Schwab adult spinal deformity classification: a validation study. Spine (Phila Pa 1976). 2012;37:1077–1082. doi:10.1097/BRS.0b013e31823e15e2 [DOI] [PubMed] [Google Scholar]
- 19. Glattes RC, Bridwell KH, Lenke LG, Kim YJ, Rinella A, Edwards C. Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976). 2005;30(14):1643–1649. doi:10.1097/01.brs.0000169451.76359.49. [DOI] [PubMed] [Google Scholar]
- 20. Jain A, Hassanzadeh H, Strike SA, Menga EN, Sponseller PD, Kebaish KM. Pelvic fixation in adult and pediatric spine surgery: historical perspective, indications, and techniques: AAOS exhibit selection. J Bone Joint Surg Am. 2015;97:1521–1528. doi:10.2106/JBJS.O.00576 [DOI] [PubMed] [Google Scholar]
- 21. Kim HJ, Yagi M, Nyugen J, Cunningham ME, Boachie-Adjei O. Combined anterior-posterior surgery is the most important risk factor for developing proximal junctional kyphosis in idiopathic scoliosis. Clin Orthop Relat Res. 2012;470:1633–1639. doi:10.1007/s11999-011-2179-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. O'Shaughnessy BA, Bridwell KH, Lenke LG, et al. Does a long-fusion “T3-sacrum” portend a worse outcome than a short-fusion “T10-sacrum” in primary surgery for adult scoliosis? Spine (Phila Pa 1976). 2012;37:884–890. doi:10.1097/BRS.0b013e3182376414 [DOI] [PubMed] [Google Scholar]
- 23. Maruo K, Ha Y, Inoue S, et al. Predictive factors for proximal junctional kyphosis in long fusions to the sacrum in adult spinal deformity. Spine (Phila Pa 1976). 2013;38:E1469–E1476. doi:10.1097/BRS.0b013e3182a51d43 [DOI] [PubMed] [Google Scholar]
- 24. Yagi M, Ohne H, Konomi T, et al. Teriparatide improves volumetric bone mineral density and fine bone structure in the UIV+1 vertebra, and reduces bone failure type PJK after surgery for adult spinal deformity. Osteoporos Int. 2016;27:3495–3502. doi:10.1007/s00198-016-3676-6 [DOI] [PubMed] [Google Scholar]
- 25. Hyun SJ, Kim YJ, Rhim SC. Patients with proximal junctional kyphosis after stopping at thoracolumbar junction have lower muscularity, fatty degeneration at the thoracolumbar area. Spine J. 2016;16:1095–1101. doi:10.1016/j.spinee.2016.05.008 [DOI] [PubMed] [Google Scholar]
- 26. O’Leary PT, Bridwell KH, Lenke LG, et al. Risk factors and outcomes for catastrophic failures at the top of long pedicle screw constructs: a matched cohort analysis performed at a single center. Spine (Phila Pa 1976). 2009;34:2134–2139. doi:10.1097/BRS.0b013e3181b2e17e [DOI] [PubMed] [Google Scholar]
- 27. Hostin R, McCarthy I, O’Brien M, et al. Incidence, mode, and location of acute proximal junctional failures following surgical treatment for adult spinal deformity. Spine (Phila Pa 1976). 2013;38:1008–1015. doi:10.1097/BRS.0b013e318271319c [DOI] [PubMed] [Google Scholar]