Abstract
Study Design:
Retrospective study.
Objective:
In this study, we examined whether the size of a lumbar disc herniation (LDH) is predictive of the need for surgical intervention within 2 years after obtaining an initial magnetic resonance imaging (MRI) scan. We hypothesized that a fragment that occupied a larger percentage of the spinal canal would not predict which patients failed conservative management.
Methods:
Using the ICD-10 code M51.26, we identified patients at a single academic institution, across the 2-year period from 2015 to 2016, who received a diagnosis of primary lumbar radicular pain, had MRI showing a disc herniation, and underwent at least 6 weeks of nonoperative management. Patients experiencing symptoms suggesting cauda equina syndrome and those with progressive motor neurological deficits were excluded from analysis, as were patients exhibiting “hard” disc herniations. Within the axial view of an MRI, the following measurements were made on AGFA-IMPACS for a given disc herniation: the length of both the canal and the herniated disc along the anterior-posterior axis, the average width of the disc within the canal; the total canal area, and the area of the disc herniation. Data analysis was conducted in SPSS and a 2-tailed reliability analysis using Cronbach’s alpha as a measure of reliability was obtained.
Results:
A total of 368 patients met the inclusion and exclusion criteria for this study. Of these, 14 (3.8%) had L3-L4 herniations, 185 had L4-L5 herniations (50.3%), and 169 had L5-S1 herniations (45.9%). Overall, 336 (91.3%) patients did not undergo surgery within 1 year of the LDH diagnosis. Patients who did not receive surgery had an average herniation size that occupied 31.2% of the canal, whereas patients who received surgery had disc herniations that occupied 31.5% of the canal on average. A Cronbach’s alpha of .992 was observed overall across interobserver measurements. After controlling for age, race, gender, and location of herniation through a logistic regression, it was found that the size of the herniation and the percentage of the canal that was occupied had no predictive value with regard to failure of conservative management, generating an odds ratio for surgery of 1.00.
Conclusions:
The percentage of the spinal canal occupied by a herniated disc does not predict which patients will fail nonoperative treatment and require surgery within 2 years after undergoing a lumbar spine MRI scan.
Keywords: disc herniation, lumbar, discectomy, MRI, low back pain, back pain, cauda equina syndrome, failed back surgery
Introduction
Some surgeons use the size of a lumbar disc herniation (LDH) to determine whether or not a patient will ultimately fail nonoperative management and require surgery.1-3 Perhaps this practice is the result of an underlying belief that spontaneous resolution of large herniations is rare and will ultimately require surgical intervention.4 Alternatively, Cribb et al1 suggest that unnecessarily high surgical rates, without a proper attempt at conservative management, may be due to the fear of potentially missing a diagnosis of cauda equina in the setting of a large, “fearsome” disc herniation. Regardless, literature is controversial at best in its support of utilizing disc size to inform surgical management of LDH.5,6
Standard treatment of LDH involves an initial attempt at conservative therapy for a minimum of 6 weeks.7,8 Conservative therapy varies, but typically involves a combination of nonsteroidal anti-inflammatory drugs, pain medications, steroid injections, and physical therapy.7,9 Unless patients are suffering from exigent conditions such as cauda equina syndrome, or a profound or progressive neurological deficit necessitating immediate surgery, most patients’ symptoms resolve without significant intervention.7,10-13 The SPORT Trial showed significant improvement with nonoperative management in patients suffering from LDH.14 However, in patients who are persistently symptomatic following a thorough course of conservative treatment, lumbar discectomy was shown to be of benefit.7
One commonly cited study by Carragee and Kim,2 suggests a 6 mm anteroposterior threshold below which patients are less likely to experience relief or resolution of symptoms postoperatively.2 Another study by En’Wezoh et al,15 also describes an association between disc size and postoperative success. However, it does not support such a threshold and highlights the lack of a standardized measurement of LDH.
Many clinicians determine the extent of a lumbar disc herniation by measuring how far a disc herniates into the spinal canal.2,16,17 This technique is simple and easy to execute on a magnetic resonance imaging (MRI) scan; however, it is considered subjective in nature and prone to error.18 Others have used the cross-sectional area of the herniation within the canal space as a metric to assess the extent of the herniation.3,19 Regardless of method, convention for the assessment of lumbar spine-related impairments is not standardized within the orthopedic and neurosurgical community.15,20
To our knowledge, the association between lumbar disc herniation size and the probability that a patient will fail 6 weeks of nonoperative management (and ultimately require surgery) is not well understood. In this study, we seek to quantify this association. In the process, we also hope to identify the reliability of using cross-sectional area to measure the size of an LDH, in comparison to the linear anterior-posterior measurements described in other studies.2,16,17 We hypothesize that a fragment that occupies a larger percentage of the spinal canal will not predict which patients fail conservative treatment.
Methods
This retrospective study analyzed patients at a single academic institution. All patients who received a diagnosis of primary lumbar radicular pain with MRI documentation of a lumbar disc herniation, across the 2-year period from 2015 through 2016, and who also had documented completion of at least 6 weeks of nonoperative management were eligible for inclusion in the study. Conservative management was defined as receiving a combination of at least two of the following treatment modalities for a minimum of 6 weeks: nonsteroidal anti-inflammatory drugs, gabapentin, pregabalin, or pain medication; steroid injection; and physical therapy. Patients were identified using the ICD-10 (International Classification of Diseases, 10th Revision) code M51.26 (other intervertebral disc displacement, lumbar region). Specifically, only those herniations occurring between L3-L4, L4-L5, or L5-S1, were included in this study, as herniations occurring at other vertebral levels were regarded as being atypical.21 All patients were at least 18 years of age. They were followed for a minimum of two years after receiving an initial lumbar spine MRI scan to determine whether or not lumbar surgery was eventually required for treatment of symptoms.
Exclusion criteria consisted of any previous lumbar surgery (regardless of level), or lumbar surgery for any indication other than LDH. Patients who either had a herniation smaller than 2 mm in the anterior-posterior dimension or had a chart from which imaging was not accessible were excluded from the study. Finally, patients receiving emergency surgery due to a diagnosis of cauda equina syndrome were excluded from analysis. All patients in this study exhibited “soft” lumbar disc herniation on review of MRI scans. “Hard” disc herniations involving bony fragmentation, spurs, or endplate material were excluded.
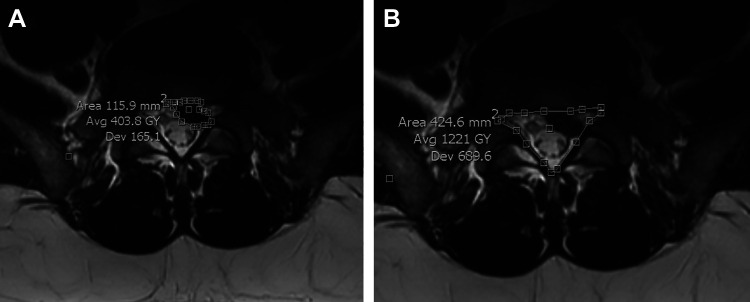
Once inclusion and exclusion criteria for a given patient were met, medical records and data regarding the date of MRI and initial diagnosis were noted. Axial imaging on the MRI was then evaluated to determine the image that contained the maximal amount of canal compromise due to the disc herniation. The herniated disc was then measured using AGFA-IMPACS software. This program enables the measurement of both area and the distance between 2 user-defined points with a strong degree of precision, allowing the user to choose various points of an irregularly shaped object. Figure 1a and b provides sample images that contain measurements of a patient’s disc herniation and canal area, respectively.
Figure 1.
(a) A sample measurement of a patient’s disc herniation. (b) A sample measurement of that same patient’s canal area.
Within the axial view of an MRI, the following measurements were made on AGFA-IMPACS for a given disc herniation: the anterior-posterior length of both the canal and the herniated disc, the average width of the disc within the canal, the total canal area, and the total disc area. For anterior-posterior measurements the longest possible measurement was utilized, that is, where the canal or disc measured is at its maximum length while parallel to the sagittal plane. Mid-width measurements were made from the midpoint of the herniation along the anterior-posterior axis. These measurements are similar to those made in a study by Carragee and Kim,2 provided for reference (with the authors’ permission) in Figure 2.2 Finally, area was measured using as many points as the user felt were necessary in order to trace a reasonable outline of a given canal or disc herniation. To our knowledge, no other lumbar disc herniation study has measured area via this methodology—this method allows for a more precise measurement of area rather than simply extrapolating from length and width as has been previously described.
Figure 2.
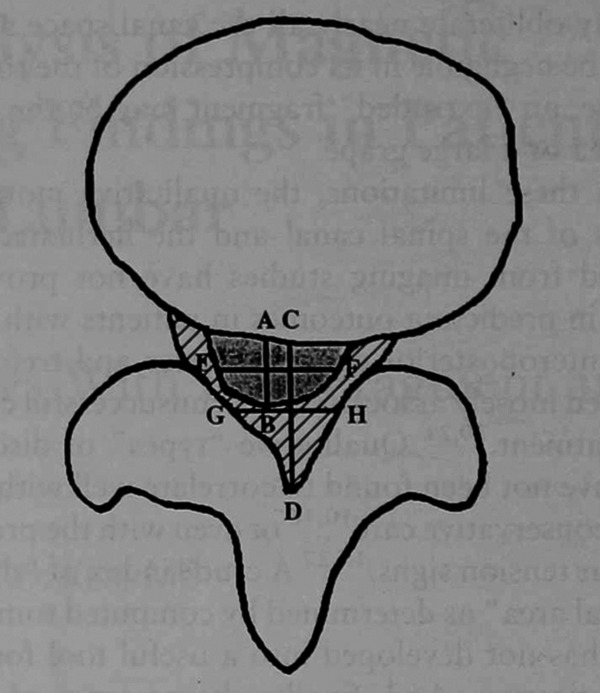
Schematic of a disc herniation as seen on magnetic resonance imaging. The shaded area represents the disc herniation. The shaded area and the hashed area in combination represent the canal area. Segment AB is the anterior-posterior length of the disc. Segment CD is the anterior-posterior measurement of the canal. Segments EF and GH represent the mid-width of the disc and canal, respectively. This image was adopted with permission from the study by Carragee and Kim.2
One observer (AG) performed the lumbar disc herniation and canal measurements for the patients in our study. Additional measurements were then conducted by 3 independent observers (SU, CY, PO) in triplicate for a sample set of 10 randomly selected patients. In so doing, each of the 4 observers conducted 3 trials of measurements for a given lumbar disc herniation, in order to assess inter- and intraobserver reliability. Data analysis was conducted in SPSS and a 2-tailed reliability analysis using Cronbach’s alpha as a measure of reliability was obtained. Correlation coefficients for both single and average measurements were identified. A logistic regression controlling for age, gender, race, and the location of the herniated disc was conducted to determine whether the size of a disc herniation, as a percentage of the canal area, was correlated with the likelihood that a patient received surgery after failing nonoperative care. Finally, a t test between the surgical and nonsurgical groups was conducted utilizing the anterior-posterior length measurement.
This study received approval from the institutional review board. No external funding sources was received in support of this study.
Results
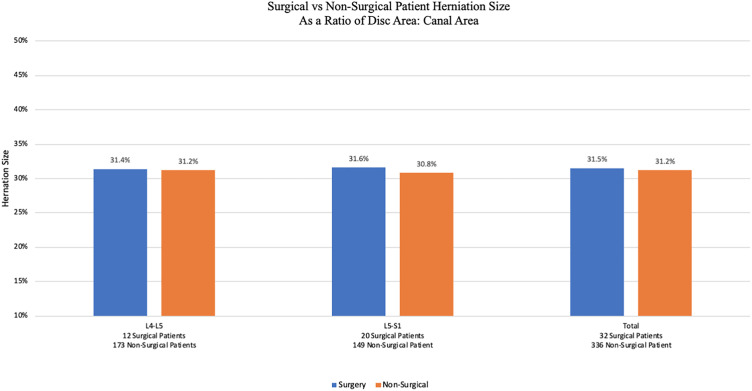
After exclusion, 368 patients met the inclusion criteria for this study. Of these, 14 (3.8%) had an L3-L4 herniation, 185 (50.3%) had an L4-L5 herniation, and 169 (45.9%) had a herniation at the L5-S1 level. Overall, 32 (8.7%) patients required surgical treatment after failing conservative management for at least 6 weeks. Table 1 provides data comparing patients who received surgery with those that were successfully managed with conservative management. The populations were similar in age, gender, and race. Of note, the average size of the disc herniation (measured as a percentage of the herniation to the total canal area) was nearly identical in both groups. Figure 3 highlights this similarity across the L4-L5 region and the L5-S1 region. Data on L3-L4 is not provided since none of the 14 patients in this study with an L3-L4 herniation required surgery.
Table 1.
A Comparison Between Patients Who Required Surgery for Treatment of Lumbar Disc Herniation With Those Who Did Not.a
| Surgery | Nonsurgery | Total | |
|---|---|---|---|
| Mean herniation size, % | 31.5 | 31.2 | 31.2 |
| Number of patients | 32 | 336 | 368 |
| Age, years, mean (SD) | 33.3 (7.6) | 32.1 (6.8) | 32.2 (6.9) |
| Gender, % female | 50.0 | 47.9 | 48.1 |
| Race, % | |||
| Caucasian | 78.1 | 73.2 | 73.6 |
| African American | 6.3 | 5.4 | 5.4 |
| Asian | 3.1 | 5.1 | 4.9 |
| Hispanic | 3.1 | 5.1 | 4.9 |
| Other | 6.3 | 7.1 | 7.1 |
| None | 3.1 | 4.2 | 4.1 |
| Location, % | |||
| L3-IA | 0.0 | 4.2 | 3.8 |
| L4-L5 | 37.5 | 51.5 | 50.3 |
| L5-Sl | 62.5 | 44.3 | 45.9 |
a All patients, both surgical and nonsurgical, underwent at least 6 weeks of nonoperative management.
Figure 3.
A stratified comparison (based on lumbar spine location) of disc herniation sizes between patients who ultimately required surgery versus those who were successfully managed through conservative treatment.
Table 2 depicts the results of a logistic regression analysis that considers the impact of race, gender, sex, location of herniation, and size of the disc herniation with regard to the likelihood that patients would improve with nonoperative treatment. None of these factors were statistically significant predictors of failed nonoperative management. In particular, the size of a disc herniation had an odds ratio of 1.003, implying no correlation between disc herniation size (as a percentage of canal area) and the likelihood a patient would require surgical intervention after 6 weeks of conservative treatment.
Table 2.
A Logistic Regression Assessing the Impact of Race, Gender, Sex, and the Size/Location of a Herniation on the Likelihood That a Patient Will Require Surgery After 6 Weeks of Conservative Management.a
| Logistic Regression Analysis (N = 339) | |||
|---|---|---|---|
| Variable | Odds Ratio | P | 95% CI |
| Size of herniation | 1.003 | .822 | 0.98-1.03 |
| Demographic | |||
| Age | 1.00 | .305 | 0.97-1.09 |
| Sex | |||
| Female | Reference | Reference | Reference |
| Male | 1.03 | .937 | 0.48-2.19 |
| Race | |||
| Caucasian | Reference | Reference | Reference |
| African American | 0.95 | .948 | 0.20-4.42 |
| Asian | 0.51 | .527 | 0.06-4.08 |
| Hispanic | 0.69 | .722 | 0.08-5.53 |
| Other | 0.89 | .875 | 0.19-4.04 |
| Location of herniation | |||
| L5-S1 | Reference | Reference | Reference |
| L4-L5 | 0.52 | .05 | 0.24-1.11 |
a A total of 15 patients were excluded due to no reported race. An additional 14 patients were excluded due to the herniation being at L3-L4 (no patients with herniations at this level required surgical treatment after 6 weeks of nonoperative management).
Statistical Analysis
Table 3 provides data on the reliability of measurements made in this study. Overall, interobserver data across all measurements generated a Cronbach alpha value of .992. With regard to the various measurements made for a given herniation, Table 4 shows that, on average, measurement of area was more reliable than linear measurements. In other words, measurements such as the anterior-posterior length of the canal or the width of the herniated disc, both of which involve the simple drawing of a line, were less reproducible than, for example, tracing the spinal canal border to measure area. Finally, a t test between the surgical and nonsurgical groups, using either the less accurate anterior-posterior measurement or the more reliable disc area: canal area ratio, failed to show a statistically significant difference between herniation size and the likelihood that a patient would fail conservative management.
Table 3.
Interobserver Data Including Correlation Statistics and Cronbach’s Alpha Value.
| Overall Intraclass Correlation Coefficient (Interobserver) | |||||
|---|---|---|---|---|---|
| Intraclass Correlation | 95% Confidence Interval | Cronbach’s Alpha | No. of Items | ||
| Lower Bound | Upper Bound | ||||
| Single measures | .970 | 0.962 | 0.976 | .992 | 4 |
| Average measures | .992 | 0.990 | 0.994 | ||
Table 4.
Cronbach’s Alpha Values by Measurement.a
| Measurement | Cronbach’s Alpha | Average Cronbach’s Alpha |
|---|---|---|
| Disc anterior-posterior | .851 | .672 |
| Disc midwidth | .381 | |
| Canal anterior-posterior | .659 | |
| Canal midwidth | .798 | |
| Disc area | .707 | .785 |
| Canal area | .863 |
a Linear measurements on average have a lower reliability than multipoint measurements using AGFA-IMPACS.
Discussion
Results from this study show that there is no statistical association between the size of a lumbar disc herniation and the likelihood that a patient will fail conservative treatment and ultimately require surgery. In fact, the 1.003 odds ratio between herniation size and the likelihood for surgery, as reported in Table 2, demonstrates that the size of the disc herniation did not predict whether nonoperative treatment would not be successful. This is consistent with findings from a study by Benson et al,22 which states that even massive disc herniations can successfully be treated conservatively. In fact, on several occasions in this study, patients with nearly complete dural sac stenosis, some as great as 85.1%, were successfully managed without surgery.
Since, age, gender, race, and location also fail to show an association, our data suggests that all patients except those with cauda equina syndrome or a profound neurologic deficit should undergo 6 weeks of nonoperative management before surgery is considered. Jeon et al23 arrived at a similar conclusion in their study. This point is emphasized by the similarities in the surgical and nonsurgical populations in this study, as illustrated in Table 1.
Literature shows that over 90% of lumbar disc herniations will resolve on their own.24 Since Guinto et al12 first reported spontaneous regression of lumbar disc herniations in 1984, clinicians have offered various mechanisms for the disappearance of the herniated fragment. Theories such as retraction from posterior longitudinal ligament tension, resorption by macrophage phagocytosis, lymphatic drainage, an immunologic reaction, and dehydration have all been proposed.25-27 Regardless, our study suggests that in nonemergent settings, managing lumbar disc herniations conservatively for several weeks before offering surgery as a treatment option appears to be prudent. In this study, only 8.7% of the 368 patients analyzed ultimately required surgery—this rate is consistent with previous literature.28
New to this study is the method in which herniation size was measured. As mentioned earlier, while many have utilized anterior-posterior measurement of the disc within the spinal canal as a means of characterization,2,16,17 others have utilized cross-sectional area.3,19 One of the best ways to study internal consistency of measurement, and therefore reliability, is through a Cronbach alpha value.29 This metric ranges from 0 to 1, with 1 indicating perfect reliability; any measurement value over 0.7 is generally considered useful or satisfactory.29 In this study, we found that both the anterior-posterior method and cross-sectional method were acceptable forms of measurement. However, point-to-point measurements, such as the anterior-posterior method, simply quantify the distance between 2 planar points and were shown to be far less reliable than area measurements. Area measurements made use of several user-defined points and generated a Cronbach alpha of .785 compared with the .672 value for point-to-point measurements.
Furthermore, measuring herniation size as a percentage of the disc area to the total spinal canal area required the user to measure both the disc cross-sectional area and the spinal canal area. Thus, if there was any subjectivity regarding the exact boundary of the canal area, this subjectivity was applied to both measurements. Nonetheless, overall interrater reliability across all measurements was .970. Therefore, we are reasonably confident that our findings are not simply due to a rater-mediated effect. Utilization of length and width alone may not adequately define the area of irregularly shaped objects such as the spinal canal or the LDH.
A study by Lurie et al19 also utilized MRI to evaluate postoperative outcomes but focused on the presence of pathology as opposed to strict disc herniation measurements. Variables included in imaging analysis consisted of stenosis (foraminal and central), facet arthropathy, the presence of (but not size of) a disc herniation and/or disc degeneration, as well as thecal sac compression. They concluded that compression of more than a third of the thecal sac was a predictor of surgical outcome. That finding provides support that the area of compression caused by the size of a disc herniation is more clinically contributory to a good postoperative outcome than any of the other factors investigated. This is consistent with the findings reported by En’Wezoh et al15 who described the “6 mm rule,” but does not address which patients may or may not benefit from nonoperative treatment.
Limitations of this study include the fact that patient data came from only 1 hospital in the northeast.
Documentation of specific physical therapy regimens or when and how many steroid injections were administered were not considered. It is also possible that some patients may have been lost to follow-up or elected to receive a surgery at another center without having such a procedure documented in our medical charts. In future studies, it may be interesting to isolate or study the effect of each to understand what is associated with the highest rate of nonoperative improvement. Furthermore, while only 8.7% of patients ultimately received surgery, it would be interesting to compare this statistic to other hospitals and practices across different geographies. In fact, a similar study by Carlisle et al30 that was conducted at another center demonstrated a higher surgical rate of 19.6%.
This finding may elucidate information on how patients with lumbar disc herniations are treated in the academic setting, the community setting, and in practices with access to ambulatory surgery centers. Since some surgeons do not believe that large disc herniations will improve with nonoperative treatment, it is possible that some patients with large LDH may not have been eligible for inclusion in this study since they did not complete 6 weeks of nonoperative treatment before undergoing surgery. A prospectively controlled study enrolling all patients with LDHs would be able to eliminate this problem.
Logistically, this study considered the initiation of conservative management and the date of an initial MRI scan in determining a 2-year follow-up period for all patients. We could not, however, reliably ascertain the start of LDH-related symptoms, since many patients were not able to reliably convey information regarding the onset of lower-back pain. Often onset of symptoms was “a few weeks ago” or “a couple of months in the past” per medical records. Having this data point may have given additional valuable information. Instead, date of MRI scan and length of conservative management were analyzed in this study.
Moreover, follow-up MRI scans to monitor resolution of lumbar disc herniation on imaging were not obtained. This is largely because of the fact that the vast majority of patients experienced a resolution of their symptoms with conservative management; indications for an MRI scan that would be covered by health insurance were no longer in place, as a result.
Finally, this study made use of 2-dimensional axial slices on MRI scans to assess lumbar disc herniations. No measurements in the cranial-caudal dimension of either the herniated disc or the intervertebral space were made. Thus, no analysis was made for any association between disc height and the rate of failed non-operative management. As Tunset et al18 convey in their study, there is evidence that a decrease in the height of an intervertebral disc is associated with a greater risk for an LDH and therefore, is potentially clinically relevant. Accounting for this third dimension in a future study could be valuable in improving our understanding of treatment options for LDH. In addition, as mentioned, this study only considered “soft” disc herniations containing material from the nucleus pulposus. Hard disc herniations were eliminated from the study. Since hard and soft herniations may exhibit different resolution potential,31 it would be interesting to study and quantify how hard disc herniations resolve over time with conservative management.
Nevertheless, results from this analysis suggest that there is no correlation between the size of a lumbar disc herniation and the likelihood that a patient will require surgery after 6 weeks of nonoperative management. It serves as a reminder for clinicians and patients to exhibit patience in the treatment of lumbar disc herniations. The desire for a quick resolution of symptoms may entice patients to seek a second opinion or referral to a surgical clinic.32 Though surgery may offer better short-term results, studies have shown that over the long-term this difference diminishes.33 According to Deyo and Mirza,34 the rate of spine surgery in the United States is the highest in the world, approximately 5 times that of England or Scotland. This phenomenon may be due to a lack of standardization of practices across countries.35 Alternatively, Cribb et al1 suggest that high surgical rates may be due to the fear of potentially missing a diagnosis of cauda equina in the setting of a large, “fearsome” disc herniation. Regardless of the reason, implementing evidence based medicine to ensure best practices across the surgical community is perhaps the best way to avoid operating unnecessarily and adding to the economic burden caused by lumbar disc herniations.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Anmol Gupta, BS  https://orcid.org/0000-0001-8320-740X
https://orcid.org/0000-0001-8320-740X
References
- 1. Cribb GL, Jaffray DC, Cassar-Pullicino VN. Observations on the natural history of massive lumbar disc herniation. J Bone Joint Surg Br. 2007;89:782–784. [DOI] [PubMed] [Google Scholar]
- 2. Carragee EJ, Kim DH. A prospective analysis of magnetic resonance imaging findings in patients with sciatica and lumbar disc herniation. Correlation of outcomes with disc fragment and canal morphology. Spine (Phila Pa 1976). 1997;22:1650–1660. [DOI] [PubMed] [Google Scholar]
- 3. Buttermann GR. Treatment of lumbar disc herniation: epidural steroid injection compared with discectomy. A prospective, randomized study. J Bone Joint Surg Am. 2004;86:670–679. [PubMed] [Google Scholar]
- 4. Ryu SJ, Kim IS. Spontaneous regression of a large lumbar disc extrusion. J Korean Neurosurg Soc. 2010;48:285–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Benoist M. The natural history of lumbar disc herniation and radiculopathy. Joint Bone Spine. 2002;69:155–160. [DOI] [PubMed] [Google Scholar]
- 6. Bozzao A, Gallucci M, Masciocchi C, Aprile I, Barile A, Passariello R. Lumbar disk herniation: MR imaging assessment of natural history in patients treated without surgery. Radiology. 1992;185:135–141. [DOI] [PubMed] [Google Scholar]
- 7. Schoenfeld AJ, Weiner BK. Treatment of lumbar disc herniation: evidence-based practice. Int J Gen Med. 2010;3:209–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lee DY, Park YJ, Kim KT, Lee JH, Kim DH. Acute lumbosacral hemorrhagic ganglion cyst after transforaminal epidural steroid injection. Acta Orthop Traumatol Turc. 2018;52:475–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Amin RM, Andrade NS, Neuman BJ. Lumbar disc herniation. Curr Rev Musculoskelet Med. 2017;10:507–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Deyo RA, Loeser JD, Bigos SJ. Herniated lumbar intervertebral disk. Ann Intern Med. 1990;112:598–603. [DOI] [PubMed] [Google Scholar]
- 11. Reddy AP, Mahajan R, Rustagi T, Chhabra HS. Bladder recovery patterns in patients with complete cauda equina syndrome: a single-center study. Asian Spine J. 2018;12:981–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Guinto FC, Jr, Hashim H, Stumer M. CT demonstration of disk regression after conservative therapy. AJNR Am J Neuroradiol. 1984;5:632–633. [PMC free article] [PubMed] [Google Scholar]
- 13. Carragee E. Surgical treatment of lumbar disk disorders. JAMA. 2006;296:2485–2487. [DOI] [PubMed] [Google Scholar]
- 14. Lurie JD, Tosteson TD, Tosteson AN, et al. Surgical versus non-operative treatment for lumbar disc herniation: eight-year results for the Spine Patient Outcomes Research Trial (SPORT). Spine (Phila Pa 1976). 2014;39:3–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. En’Wezoh DC, Leonard DA, Schoenfeld AJ, Harris MB, Zampini JM, Bono CM. Relationship between size of disc and early postoperative outcomes after lumbar discectomy. Arch Orthop Trauma Surg. 2017;137:805–811. [DOI] [PubMed] [Google Scholar]
- 16. Fotakopoulos G, Makris D, Kotlia P, Tzerefos C, Fountas K. Recurrence is associated with body mass index in patients undergoing a single-level lumbar disc herniation surgery. J Clin Med Res. 2018;10:486–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mysliwiec LW, Cholewicki J, Winkelpleck MD, Eis GP. MSU classification for herniated lumbar discs on MRI: toward developing objective criteria for surgical selection. Eur Spine J. 2010;19:1087–1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tunset A, Kjaer P, Samir Chreiteh S, Secher Jensen T. A method for quantitative measurement of lumbar intervertebral disc structures: an intra- and inter-rater agreement and reliability study. Chiropr Man Therap. 2013;21:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lurie JD, Moses RA, Tosteson AN, et al. Magnetic resonance imaging predictors of surgical outcome in patients with lumbar intervertebral disc herniation. Spine (Phila Pa 1976). 2013;38:1216–1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Stienen MN, Ho AL, Staartjes VE, et al. Objective measures of functional impairment for degenerative diseases of the lumbar spine: a systematic review of the literature. Spine J. 2019;19:1276–1293. [DOI] [PubMed] [Google Scholar]
- 21. Sanderson SP, Houten J, Errico T, Forshaw D, Bauman J, Cooper PR. The unique characteristics of “upper” lumbar disc herniations. Neurosurgery. 2004;55:385–389. [DOI] [PubMed] [Google Scholar]
- 22. Benson RT, Tavares SP, Robertson SC, Sharp R, Marshall RW. Conservatively treated massive prolapsed discs: a 7-year follow-up. Ann R Coll Surg Engl. 2010;92:147–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Jeon CH, Chung NS, Son KH, Lee HS. Massive lumbar disc herniation with complete dural sac stenosis. Indian J Orthop. 2013;47:244–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gugliotta M, da Costa BR, Dabis E, et al. Surgical versus conservative treatment for lumbar disc herniation: a prospective cohort study. BMJ Open. 2016;6:e012938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Teplick JG, Haskin ME. Spontaneous regression of herniated nucleus pulposus. AJR Am J Roentgenol. 1985;145:371–375. [DOI] [PubMed] [Google Scholar]
- 26. Henmi T, Sairyo K, Nakano S, et al. Natural history of extruded lumbar intervertebral disc herniation. J Med Invest. 2002;49:40–43. [PubMed] [Google Scholar]
- 27. Saal JA, Saal JS, Herzog RJ. The natural history of lumbar intervertebral disc extrusions treated nonoperatively. Spine (Phila Pa 1976). 1990;15:683–686. [DOI] [PubMed] [Google Scholar]
- 28. Sabnis AB, Diwan AD. The timing of surgery in lumbar disc prolapse: a systematic review. Indian J Orthop. 2014;48:127–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bland JM, Altman DG. Cronbach’s alpha. BMJ. 1997;314:572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Carlisle E, Luna M, Tsou PM, Wang JC. Percent spinal canal compromise on MRI utilized for predicting the need for surgical treatment in single-level lumbar intervertebral disc herniation. Spine J. 2005;5:608–614. [DOI] [PubMed] [Google Scholar]
- 31. Ma XL. A new pathological classification of lumbar disc protrusion and its clinical significance. Orthop Surg. 2015;7:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Li AL, Yen D. Effect of increased MRI and CT scan utilization on clinical decision-making in patients referred to a surgical clinic for back pain. Can J Surg. 2011;54:128–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Weber H. Lumbar disc herniation. A controlled, prospective study with ten years of observation. Spine (Phila Pa 1976). 1983;8:131–140. [PubMed] [Google Scholar]
- 34. Deyo RA, Mirza SK. Trends and variations in the use of spine surgery. Clin Orthop Relat Res. 2006;443:139–146. [DOI] [PubMed] [Google Scholar]
- 35. Chen BL, Guo JB, Zhang HW, et al. Surgical versus non-operative treatment for lumbar disc herniation: a systematic review and meta-analysis. Clin Rehabil. 2018;32:146–160. [DOI] [PubMed] [Google Scholar]