Dear Editor,
I have read with interest the published article entitled “Mortality rate of acute kidney injury in SARS, MERS, and COVID-19 infection: a systematic review and meta-analysis” by Chen et al. [1]. The article is well written, and I have three concerns as explained below.
Firstly, the mortality rate for COVID-19 patients with AKI is different in the text (i.e., 76.5%; 95% CI 61.0–89.0) from one reported in the authors’ Figure 1 (i.e., 78.0%; 95% CI 63.0–90.0). The authors might need to clarify this discrepancy.
Secondly, the authors mistakenly made a duplicate entry of the study by Chen et al. (2020) in the COVID-19 forest plot. This mistake resulted in a pooled AKI mortality rate of 78.0% (CI 63.0–90.0), I2 = 97.1%, P < 0.0001, instead of 53.99% (CI 52.34–55.65), I2 = 98.4%, P < 0.0001, had the authors sorted the duplicate-entry problem.
Thirdly, the authors concluded the mortality rate for COVID-19 patients with AKI from an otherwise a high heterogeneity of I2 = 97.1%, P < 0.0001. This strongly impacts the reliability of the conclusion drawn [2].
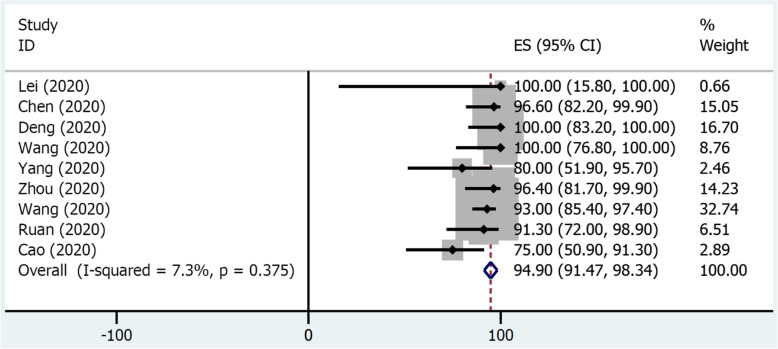
I, on the other hand, reanalyzed authors’ data and performed sensitivity analysis according to the Cochrane Library recommendation [3]. I excluded six peculiar studies from the analysis. Alberici et al. and Banerjee et al. involved kidney transplant patients, unlike the rest of the studies. Wang et al. utilized intensive care unit patients, unlike other studies. Moreover, Alberici et al., Banerjee et al., Hirsch et al., Suwanwongse et al., and Richardson et al. included racially diverse participants. Different races have different COVID-19 mortalities [4, 5]. The nine remaining studies represented all-Asian Chinese hospitalized patients with COVID-19 and AKI. The newly obtained mortality rate for COVID-19 patients with AKI was 94.90% (CI 91.47–98.34), with non-statistically significant heterogeneity, I2 = 7.4%, P < 0.375, see Fig. 1. Sensitivity analysis could not be conducted in MERS and SARS outcomes because of an insufficient number of studies.
Fig. 1.
A forest plot of AKI mortality in coronavirus infections from included studies: COVID-19
Acknowledgements
Not applicable.
Author’s contributions
JS drafted the manuscript. JS revised the manuscript critically for valuable intellectual content. JS approved the final manuscript.
Funding
There was no external funding regarding the letter.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The author has no conflict of interest to declare.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Chen YT, Shao SC, Lai EC, Hung MJ, Chen YC. Mortality rate of acute kidney injury in SARS, MERS, and COVID-19 infection: a systematic review and meta-analysis. Crit Care. 2020;24(1):439. doi: 10.1186/s13054-020-03134-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Imrey PB. Limitations of meta-analyses of studies with high heterogeneity. JAMA Netw Open. 2020;3(1):e1919325. doi: 10.1001/jamanetworkopen.2019.19325. [DOI] [PubMed] [Google Scholar]
- 3.Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10:Ed000142. doi: 10.1002/14651858.ED000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. COVID-19 in Racial and Ethnic Minority Groups, Inc.; c2020 [Updated 2020 Jun 25; cited 2020 Jul 22]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/racial-ethnic-minorities.html.
- 5.Golestaneh L, Neugarten J, Fisher M, Billett HH, Gil MR, Johns T, et al. The association of race and COVID-19 mortality. EClinicalMedicine. 2020;8(1):38. [DOI] [PMC free article] [PubMed]
- 6.Fisher M, Neugarten J, Bellin E, et al. AKI in hospitalized patients with and without COVID-19: a comparison study [published online ahead of print, 2020 Jul 15]. J Am Soc Nephrol. 2020:ASN.2020040509. 10.1681/ASN.2020040509. [DOI] [PMC free article] [PubMed]