Abstract
Introduction
Angiosarcoma is a rare and aggressive malignancy with a high metastatic potential and recurrence rate. Despite optimal treatment with surgery, with or without radiation, the prognosis remains poor and, therefore, new treatment strategies are warranted. Recently, propranolol has effectively been repurposed for the treatment of infantile haemangioma. Propranolol is a β3-sparing antagonist of the β-adrenergic receptor. In infantile haemangioma, the β1, β2 and β3 receptors are highly expressed. Angiosarcoma has several similarities with haemangioma, including its high β-adrenergic receptor expression and the supposedly important role of vascular endothelial growth factor in malignant growth. As a result, propranolol has been administered small scale in individual angiosarcoma cases with promising results. The precise effect of propranolol, however, is not yet established.
Methods and analysis
The goal of this neoadjuvant window of opportunity study is to prospectively evaluate the activity of propranolol monotherapy in patients with cutaneous angiosarcoma. The neoadjuvant setting provides a good opportunity to rapidly evaluate both the clinical response and histological response, without a significant delay in standard anticancer treatment. Fourteen patients with primary, recurrent or metastatic cutaneous angiosarcoma will be included. Propranolol will be administered orally in an escalating dose during 3–6 weeks, before the initiation of standard treatment. The primary endpoint is clinical response according to Response Evaluation Criteria in Solid Tumours, as measured on consecutive coloured photographs or CT/MRI. The histological response will be determined as secondary endpoint, comparing the difference in proliferation index before and after propranolol by measuring the change in immunohistochemistry staining of Ki-67. The study will be considered positive when at least three patients have a response to propranolol.
Ethics and dissemination
Ethical approval was obtained from the Medical Ethical Committee of the Netherlands Cancer Institute. Independent of the outcome, results of this study will be shared and submitted for publication in an international peer-reviewed journal.
Trial registration number
NL8118; registry through the Netherlands Trial Register.
Keywords: oncology, adult oncology, sarcoma, vascular medicine
Strengths and limitations of this study.
The neoadjuvant setting provides the opportunity to evaluate the antitumor response of propranolol monotherapy without delaying the standard treatment.
The propranolol dose will be escalated to optimise the safety profile of the treatment.
As it is a window of opportunity study, the study duration will be relatively short.
A limitation of the current design (proof of principle study) is the absence of randomisation.
Introduction
Angiosarcoma is a rare and aggressive malignancy with a high metastatic potential. The estimated incidence of angiosarcoma is 0.4 per million patients per year, making it a very rare disease.1 The standard of care for localised angiosarcoma is currently complete surgical resection with or without radiation. Unfortunately, despite the current standard of care, only 60% of patients with localised disease survive for more than 5 years.2 Physicians and researchers are, therefore, in urgent need to find better treatment options for these patients.
Various additional drugs for systemic treatment have been investigated before.2–4 Although the role of (neo)adjuvant chemotherapy remains controversial for localised disease, neoadjuvant chemotherapy is often administered for locally advanced angiosarcoma.3 5–8 Several cytotoxic drugs, including anthracyclines, taxanes and gemcitabine, have shown activity in angiosarcoma in the locally advanced and metastatic setting, with overall response rates varying from 17% to 89%.2–4 However, for the treatment of resectable angiosarcoma, none of the previous studies shows a prolonged disease-free survival or overall survival.3 5–10 Improved treatment in the neoadjuvant setting might reduce the local and distant recurrence rates by treating micrometastases at an early stage and by improving the resection margins, potentially leading to higher survival rates. As a result, new drugs are urgently needed to prolong the survival.
Propranolol hydrochloride, a synthetic β3-sparing-adrenergic receptor antagonist, was registered by the Food and Drug Agency decades ago for the treatment of hypertension. Drug repurposing is a drug development strategy focused on the reuse of existing drugs for new medical indications. Recently, propranolol has been repurposed and is now used in the treatment of infantile haemangioma. Infantile haemangioma is a benign vascular tumour and propranolol dosed 3 mg/kg led to a complete to near-complete resolution in approximately 88% of the treated infants with infantile haemangioma.11 12 The pharmacological effects of propranolol in infantile haemangioma are presumed to cause vasoconstriction, a decreased expression of vascular endothelial growth factor (VEGF) and basic fibroblast growth factor, inhibition of migration and proliferation of tumour cells and induction of apoptosis of endothelial cells.12–16 Angiosarcoma have several similarities with infantile haemangioma, including its high β-adrenergic receptor expression and the suggested important role of VEGF in malignant growth.14 17 18
Several small case reports and case series have confirmed the idea that propranolol could be repurposed to treat angiosarcoma. In these case reports, patients with locally advanced or metastatic angiosarcoma were treated with propranolol, in combination with various chemotherapy regimens, including combination therapy with cyclophosphamide, etoposide, paclitaxel and vinblastine-based chemotherapy. The dose of propranolol in combination therapy varied between 80 mg and 120 mg per day.19–24 In one case, there was a response after 1 week of propranolol monotherapy 40 mg two times per day.22 These doses of propranolol are much lower than the standard maintenance dose of 160–320 mg daily for patients with hypertension.25 Furthermore, there was a reduction in the proliferative index of 34%, stabilisation of tumour growth and less necrosis.22 Additionally, one case described a patient with metastatic cardiac angiosarcoma who showed a long-term response (>12 months) to propranolol monotherapy, while the mean survival time is only 4 months.26
Since literature regarding the activity and mode of action of propranolol as a single agent for angiosarcoma is scarce, our aim is to evaluate the activity of propranolol monotherapy in patients with primary, recurrent or metastatic cutaneous angiosarcoma before they proceed to their standard anticancer treatment. The neoadjuvant setting provides a good opportunity to rapidly evaluate both the clinical and histological responses, without delaying the standard anticancer treatment. Additional advantages of propranolol therapy would be the ease of use and the relatively mild toxicity profile. If this study turns out to be positive, further (randomised) clinical trials are thereby substantiated and highly recommended.
Methods and analysis
Aim and objectives
The aim of this study is to investigate the effect of neoadjuvant propranolol monotherapy in patients with primary, recurrent or metastatic cutaneous angiosarcoma, before they proceed to their standard anticancer treatment (eg, isolated limb perfusion, chemotherapy, targeted therapy, surgical resection or radiotherapy). The primary objective is to determine the clinical response of propranolol monotherapy and the histologic response will be evaluated as secondary objective.
Study design and study treatment
This is a prospective proof of principle study with neoadjuvant propranolol monotherapy in patients with cutaneous angiosarcoma. We will use the neoadjuvant window as an opportunity to explore the activity of propranolol monotherapy, without delaying the standard treatment. The duration of treatment will be 3–6 weeks. In this single arm trial, patients with angiosarcoma will be treated with propranolol monotherapy in an intrapatient escalating dose, which will be adjusted to the tolerability of propranolol. The treatment plan of propranolol is provided in table 1. The treatment plan was designed based on doses used in the previous literature15 21 24 26 and not exceeding the maximum maintenance dose of 320 mg/day for the registered indication hypertension (maximum daily dose in our study 240 mg/day).25 In case of hypotension (blood pressure <90/60 mm Hg) or bradycardia (heart rate <55 bpm) or symptoms of bradycardia or hypotension (dizziness, syncope), the dose will be reduced to the previous dose level. In case of serious bradycardia (heart rate <50 bpm), the treatment will be stopped until an acceptable heart rate (>55 bpm) is reached and propranolol will be restarted in the dose of the previous level.
Table 1.
Propranolol treatment plan
| Dose escalation scheme | ||
| Period | Dose level | Dose |
| Day 1–day 7 | 1* | 2 x/day 40 mg |
| Day 8–day 14 | 2* | 2 x/day 80 mg |
| Day 15–day of surgery or biopsy | 3* | 3 x/day 80 mg |
| Tapering off scheme after surgery/biopsy | ||
| Period | Dose | |
| Day 1–day 7 | 2 x/day 80 mg | |
| Day 8–day 14 | 2 x/day 40 mg | |
*All patients start on day 1 with dose level 1.
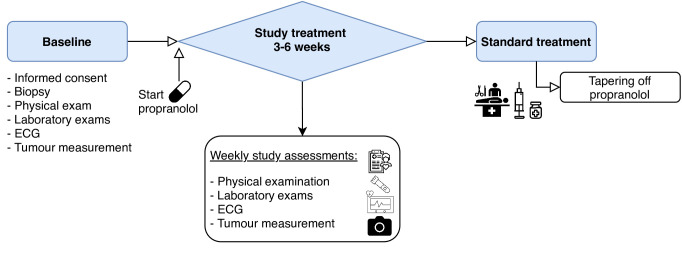
The tolerability will be assessed during weekly visits in the outpatient clinic (figure 1). Each visit consists of a physical examination, blood draw for safety assessment (haematology, hepatic function and renal function), vital signs, ECG, toxicity assessment, concomitant medication registration and tumour response assessment. After the study treatment, a biopsy will be obtained to evaluate the histologic response to propranolol monotherapy. Propranolol will be tapered off after the biopsy to prevent withdrawal symptoms (table 1).
Figure 1.
Study assessments. An overview of the study assessments, which are planned at baseline, during study treatment or when the standard treatment is initiated.
Patient selection
The study population consists of patients with primary, recurrent or metastatic cutaneous angiosarcoma, including angiosarcoma of the breast (radiation induced). Only patients with cutaneous angiosarcoma can participate, since these tumours are easily measurable on coloured photographs for clinical response evaluation. Patients are eligible if they are at least 18 years old; have a good performance status (WHO-PS of 0–2); have an adequate blood count, kidney and renal function; have a window of at least 3 weeks between their diagnosis and the start of the standard anticancer treatment and have evaluable disease according to the Response Evaluation Criteria in Solid Tumours (RECIST) 1.1 criteria. Patients with primary visceral angiosarcoma, contraindications for β-blockade therapy or current treatment with β-blockade therapy (both selective and non-selective β-blockade therapies) or other anticancer treatments are excluded.
Sample size calculation
An exact single-stage phase II design will be used with a one-sided significance level α of 0.05 and a power of 80%. The maximum response rate that would be of no interest was assumed to be 5% and the minimum required response rate was 30%. A total of 14 patients will be included in the study. If 3 or more out of these 14 patients have a response as defined in the study endpoints, the study is considered positive.
Study endpoints
Primary endpoint
The clinical response will be determined according to RECIST 1.1 criteria (progressive disease (PD) is >20% increase in size, partial response (PR) is >30% decrease in size, stable disease (SD) is in between while complete response (CR) is no measurable disease).27 A response is defined as CR, PR or SD with an improvement in clinical characteristics, like thickness, erythaema, necrosis or oedema of the inflicted area. Documentation will be performed with colour photography, including a ruler to measure the size of the lesion. Radiologic assessment will only be done if the patient has radiologic evaluable disease at the beginning of the study treatment. If the study turns out to be positive, this treatment modality is highly interesting and should be tested further in a randomised trial.
Secondary endpoint
The histologic response on propranolol treatment is defined as difference in proliferation index. This will be assessed by measuring the change in immunohistochemistry staining of Ki-67 and the tumour activity between the posttreatment biopsy (obtained during surgery if applicable) and the diagnostic biopsy before the study treatment. A decrease of >30% of the Ki-67 staining will be considered as a positive histologic response.
Exploratory endpoints
To obtain additional data regarding the primary objectives, the percentage of adrenergic receptors (β1-AR, β2-AR, β3-AR) in the pretreatment biopsies will be measured with immunohistochemically staining and the correlation with the antitumour response of the patients with angiosarcoma will be investigated.13 22 With this correlation analysis, the predictive value of adrenergic receptor expression in tumour tissue on the antitumour response will be assessed. Finally, we will compare the PET response before start of treatment and at the end of propranolol treatment.
Study logistics
Patient recruitment and study duration
Treating physicians will identify patients as possible candidates and inform patients about the study. If patients agree to participate and fulfil the selection criteria, patients will be included during an outpatient clinic visit. As this is a monocentre study, all patients will be included in the Netherlands Cancer Institute (NKI). Approximately 20 new patients with angiosarcoma are seen in the NKI yearly. As a result, the expected duration of the study is 2 years. Enrolment started on 27 December 2019.
Safety assessments
All adverse events will be recorded in the electronic case report forms (eCRF) during the weekly outpatient clinic visits. We will perform extra blood draws, ECGs and measurements of the vital signs during these visits for safety assessments. The recording of the adverse events will be done according to the National Cancer Institute Common Toxicity Criteria for Adverse Events V.5.0.
Data management
The original results will also be recorded in the eCRF by the investigators of the study. The data entry will be supervised by the Clinical Research Monitor.
Study monitoring
Monitoring of the study will be performed according to International Conference on Harmonisation Good Clinical Practie (ICH GCP) by the Clinical Research Monitor of the NKI or the person to whom the monitoring tasks have been delegated. Among others, the following will be reviewed: compliance with the protocol, ICH GCP and all applicable regulatory requirements; consent procedures, including date of consent and signatures; study progress; (serious) adverse events; completion of the (e)CRFs and verification of data against the source data; and storage, dispensing and accountability of study medication.
The Medical Ethical Committee of the NKI will review the study every year throughout the complete study duration. During this review, the committee will focus on monitoring of the safety of patients and evaluate the balance between the efficacy and the harmfulness of propranolol.
Termination of the study
An interim analysis is planned after the treatment of seven patients. If there are already three or more responses at this time point, the study will be stopped and stated positive. Otherwise an additional seven patients will be included. Results of the study will be shared and submitted for publication in an international peer-reviewed journal.
Patient and public involvement
The trial protocol and other trial documents were developed in collaboration with the Dutch sarcoma patient advocacy group. They evaluated the specific patient need for this trial. They fully support this trial and the concept of exploring drug-repurposing strategies to improve outcome in sarcoma. The patient advocacy group will be informed about the progress of the study and the study timelines.
The study is funded by a Belgian non-profit organisation: the Anticancer Fund. Their mission is to complement current cancer care with patient-first thinking and a focus on evidence-based potential for new treatments. Financially, the Anticancer Fund is completely dependent on donations and private funding. The Anticancer Fund supports diverse clinical trials, mainly in underprioritised treatment groups (such as in rare tumours), with non-conventional therapies and repurposed drugs.
Ethics and dissemination
Ethical approval was obtained from the Medical Ethical Committee of the Netherlands Cancer Institute. Independent of the outcome, results of this study will be shared and submitted for publication in an international peer-reviewed journal.
All essential documents (including patient files, the Investigator Study File, CRFs and electronic study data), data management and statistical files will be kept for 15 years.
Summary
Angiosarcoma is an extremely rare and aggressive malignancy with a high metastatic potential and a dismal prognosis. The current standard treatment cannot sufficiently manage the disease. Therefore, new strategies are warranted. Drug repurposing is a process of developing approved drugs for new medical indications. A strong rationale for repurposing of propranolol for the treatment of angiosarcoma patients exists. The precise effect of propranolol monotherapy is not yet established. In this study, we will therefore address the question about the efficacy of propranolol as neoadjuvant monotherapy in patients with cutaneous angiosarcoma. If this study shows positive results, further clinical trials are needed to establish the role of propranolol in the treatment of angiosarcoma, possibly even in combination with other agents such as chemotherapy, targeted therapy or immunotherapy.
Supplementary Material
Acknowledgments
The authors would like to thank the Dutch sarcoma patient advocacy group (Patiëntenplatform Sarcomen) and the Anticancer Fund for their contributions to the study.
Footnotes
KMH and NSI contributed equally.
Contributors: KMH, NSIJ, AMK, WTAvG, RLH, JHB, ADRH, WJvH and NS each made substantial contributions to the conception or design of the study protocol. NSIJ and KMH wrote the first draft of the protocol and this paper. AMK, WTAvG, RLH, WJvH, JHB, ADRH and NS provided critical input regarding the design of the study or study logistics. KMH, NSIJ, AMK, WTAvG, RLH, JHB, ADRH, WJvH and NS revised the protocol critically and approved the final version to be published.
Funding: This work was supported by Anticancer Fund from Belgium, grant number 40117.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Rouhani P, Fletcher CDM, Devesa SS, et al. . Cutaneous soft tissue sarcoma incidence patterns in the U.S. Cancer 2008;113:616–27. 10.1002/cncr.23571 [DOI] [PubMed] [Google Scholar]
- 2.Young RJ, Brown NJ, Reed MW, et al. . Angiosarcoma. Lancet Oncol 2010;11:983–91. 10.1016/S1470-2045(10)70023-1 [DOI] [PubMed] [Google Scholar]
- 3.Oxenberg J, Khushalani NI, Salerno KE, et al. . Neoadjuvant chemotherapy for primary cutaneous/soft tissue angiosarcoma: determining tumor behavior prior to surgical resection. J Surg Oncol 2015;111:829–33. 10.1002/jso.23891 [DOI] [PubMed] [Google Scholar]
- 4.Stacchiotti S, Palassini E, Sanfilippo R, et al. . Gemcitabine in advanced angiosarcoma: a retrospective case series analysis from the Italian rare cancer network. Ann Oncol 2012;23:501–8. 10.1093/annonc/mdr066 [DOI] [PubMed] [Google Scholar]
- 5.DeMartelaere SL, Roberts D, Burgess MA, et al. . Neoadjuvant chemotherapy-specific and overall treatment outcomes in patients with cutaneous angiosarcoma of the face with periorbital involvement. Head Neck 2008;30:639–46. 10.1002/hed.20757 [DOI] [PubMed] [Google Scholar]
- 6.Fayette J, Martin E, Piperno-Neumann S, et al. . Angiosarcomas, a heterogeneous group of sarcomas with specific behavior depending on primary site: a retrospective study of 161 cases. Ann Oncol 2007;18:2030–6. 10.1093/annonc/mdm381 [DOI] [PubMed] [Google Scholar]
- 7.Guadagnolo BA, Zagars GK, Araujo D, et al. . Outcomes after definitive treatment for cutaneous angiosarcoma of the face and scalp. Head Neck 2011;33:661–7. 10.1002/hed.21513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sinnamon AJ, Neuwirth MG, McMillan MT, et al. . A prognostic model for resectable soft tissue and cutaneous angiosarcoma. J Surg Oncol 2016;114:557–63. 10.1002/jso.24352 [DOI] [PubMed] [Google Scholar]
- 9.Li H, Yang S, Chen H, et al. . Survival after heart transplantation for non-metastatic primary cardiac sarcoma. J Cardiothorac Surg 2016;11:145. 10.1186/s13019-016-0540-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abu Saleh WK, Ramlawi B, Shapira OM, et al. . Improved Outcomes With the Evolution of a Neoadjuvant Chemotherapy Approach to Right Heart Sarcoma. Ann Thorac Surg 2017;104:90–6. 10.1016/j.athoracsur.2016.10.054 [DOI] [PubMed] [Google Scholar]
- 11.Léauté-Labrèze C, Hoeger P, Mazereeuw-Hautier J, et al. . A randomized, controlled trial of oral propranolol in infantile hemangioma. N Engl J Med 2015;372:735–46. 10.1056/NEJMoa1404710 [DOI] [PubMed] [Google Scholar]
- 12.Léauté-Labrèze C, Dumas de la Roque E, Hubiche T, et al. . Propranolol for severe hemangiomas of infancy. N Engl J Med 2008;358:2649–51. 10.1056/NEJMc0708819 [DOI] [PubMed] [Google Scholar]
- 13.Chisholm KM, Chang KW, Truong MT, et al. . β-Adrenergic receptor expression in vascular tumors. Mod Pathol 2012;25:1446–51. 10.1038/modpathol.2012.108 [DOI] [PubMed] [Google Scholar]
- 14.Stiles JM, Amaya C, Rains S, et al. . Targeting of beta adrenergic receptors results in therapeutic efficacy against models of hemangioendothelioma and angiosarcoma. PLoS One 2013;8:e60021. 10.1371/journal.pone.0060021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Amaya CN, Perkins M, Belmont A, et al. . Non-Selective beta blockers inhibit angiosarcoma cell viability and increase progression free- and overall-survival in patients diagnosed with metastatic angiosarcoma. Oncoscience 2018;5:109–19. 10.18632/oncoscience.413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pasquier E, Ciccolini J, Carre M, et al. . Propranolol potentiates the anti-angiogenic effects and anti-tumor efficacy of chemotherapy agents: implication in breast cancer treatment. Oncotarget 2011;2:797–809. 10.18632/oncotarget.343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Greenberger S, Bischoff J. Pathogenesis of infantile haemangioma. Br J Dermatol 2013;169:12–19. 10.1111/bjd.12435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Itakura E, Yamamoto H, Oda Y, et al. . Detection and characterization of vascular endothelial growth factors and their receptors in a series of angiosarcomas. J Surg Oncol 2008;97:74–81. 10.1002/jso.20766 [DOI] [PubMed] [Google Scholar]
- 19.Daguzé J, Saint-Jean M, Peuvrel L, et al. . Visceral metastatic angiosarcoma treated effectively with oral cyclophosphamide combined with propranolol. JAAD Case Rep 2016;2:497–9. 10.1016/j.jdcr.2016.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pasquier E, André N, Street J, et al. . Effective management of advanced angiosarcoma by the synergistic combination of propranolol and Vinblastine-based metronomic chemotherapy: a bench to bedside study. EBioMedicine 2016;6:87–95. 10.1016/j.ebiom.2016.02.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chow W, Amaya CN, Rains S, et al. . Growth attenuation of cutaneous angiosarcoma with Propranolol-Mediated β-Blockade. JAMA Dermatol 2015;151:1226–9. 10.1001/jamadermatol.2015.2554 [DOI] [PubMed] [Google Scholar]
- 22.Pramanik R, Gogia A, Malik PS, et al. . Metastatic primary angiosarcoma of the breast: can we TAME it the metronomic way. Indian J Med Paediatr Oncol 2017;38:228–31. 10.4103/ijmpo.ijmpo_156_16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Banavali S, Pasquier E, Andre N. Targeted therapy with propranolol and metronomic chemotherapy combination: sustained complete response of a relapsing metastatic angiosarcoma. Ecancermedicalscience 2015;9:499. 10.3332/ecancer.2015.499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Daguzé J, Saint-Jean M, Dréno B. Large nose angiosarcoma treated effectively with oral cyclophosphamide combined with propranolol. J Eur Acad Dermatol Venereol 2018;32:e52–4. 10.1111/jdv.14528 [DOI] [PubMed] [Google Scholar]
- 25.European Medicines Agency Propranolol 40 mg film-coated tablets - Summary of Product Characteristics (SmPC) - (eMC) [Internet]. Available: https://www.medicines.org.uk/emc/product/2904/smpc
- 26.Galván DC, Ayyappan AP, Bryan BA. Regression of primary cardiac angiosarcoma and metastatic nodules following propranolol as a single agent treatment. Oncoscience 2018;5:264–8. 10.18632/oncoscience.472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schwartz LH, Seymour L, Litière S, et al. . RECIST 1.1 - Standardisation and disease-specific adaptations: Perspectives from the RECIST Working Group. Eur J Cancer 2016;62:138–45. 10.1016/j.ejca.2016.03.082 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.