Abstract
Objectives
A growing body of research has demonstrated a robust link between parental chronic pain and child pain and psychological function. Although the association between parent and child pain is strong, there are limited data to understand environmental and behavioral processes that account for the association and how this develops over time. This longitudinal cohort study was designed to understand potential mechanisms that confer risk or resilience for chronic pain among child offspring of mothers with chronic pain.
Methods
The current paper presents baseline data on the cohort to describe pain and psychosocial characteristics of mothers with chronic pain and their 8–12-year old children. 400 mothers with chronic pain and their children were enrolled into the longitudinal study and completed measures of pain, physical, and psychosocial functioning.
Results
Mothers reported a range of pain and pain-related disability, and were grouped into four pain grades representing different pain and disability levels. Mothers in these groups differed on rates of widespread pain and opioid use. Maternal pain grades also differed by physical function, fatigue, sleep disturbance, and psychological function. Most children in this sample reported pain and psychosocial symptoms in the non-clinical range, and child variables did not differ by maternal pain grade. Maternal disability and function were concurrently associated with child psychosocial function.
Discussion
While maternal pain grades map broadly onto several dimensions of maternal functioning, they were not significantly related to child pain or function. Results may help identify potential protective factors in the intergenerational transmission of risk for chronic pain.
Introduction
Chronic pain in children and adults is a significant public health concern with a tremendous impact on economic, health, and psychosocial outcomes1,2. Rates of chronic pain among women of child-bearing and child-rearing age tend to exceed prevalence rates within the general population3. A growing body of clinical, community, and epidemiological research has demonstrated a robust link between parental chronic pain and child pain and related disability4–8. Notably, the strongest association between maternal and child pain occurs when children are living solely with their mother or their mother and new partner9, highlighting the role of environmental factors and maternal behaviors as significant risk factors for the development of chronic pain in youth.
Theoretical models of intergenerational transmission of risk for chronic pain highlight several potential environmental mechanisms through which maternal chronic pain may influence child outcomes10. Candidate environmental mechanisms that may increase a child’s vulnerability to developing chronic pain include parent modeling of disability and pain behaviors, parent transmission of maladaptive cognitive and affective responses to pain, negative influences of general family and household stress, and family habits related to general health such as low physical activity participation10–12. Importantly, not all offspring of mothers with chronic pain develop chronic pain themselves, and many of these risk factors may be ameliorated by protective factors, such as psychological well-being, parental social support, and positive coping with pain and stress.
The majority of studies examining associations between parent and offspring chronic pain have examined concordance and prevalence rates of chronic pain conditions13. A more thorough and nuanced understanding of pain, physical, and psychosocial functioning among parents with chronic pain will help inform gaps in understanding about potential mechanisms through which parent pain influences child outcomes. To address these gaps, we designed a longitudinal study following a cohort of mother-child dyads for 3 years to examine associations between maternal and child pain, disability, and physical and psychosocial functioning over time and to inform our understanding of intergenerational transmission of pain-related risks. We selected children ages 8–12 years to characterize youth as they transition into early adolescence, a developmental period in which pain experiences increase in the general population5.
The current study presents baseline data, characterizing this large cohort sample of mother-child dyads (n = 400) and reporting associations among mother and child functioning at study entry. To our knowledge, this is the first large study to describe the function of mothers with chronic pain conditions and their children using a comprehensive and nuanced approach. The majority of previous studies of mothers or parents with chronic pain have focused on differences in pain and psychological symptoms among children who do and do not have a parent with chronic pain, with minimal consideration for parent characteristics beyond the presence of a chronic pain condition, and no assessment of pain and disability using validated self-report measures.4,9,14. Given the importance of parent’s mental and physical health in children’s development and in the context of pain15–17, gaining a more in depth understanding of these factors in a sample of mothers with chronic pain will inform intergenerational models as well as potential prevention approaches. Understanding how this cohort of mother-child dyads are functioning at baseline across a number of pain characteristics and domains of health and function will elucidate patterns of concurrent risk for chronic pain in offspring and serve as a foundation for evaluating subsequent trajectories of pain, pain-related disability, and psychological functioning over the study’s next two data collection points.
The present manuscript has three specific aims. The first aim is to describe sociodemographic, pain and psychosocial characteristics of a large cohort of mothers with chronic pain and their 8–12 year old children. The second aim is to characterize mothers by pain grade and validate the use of the pain grade system by examining concurrent associations between pain grade and maternal physical and psychosocial functioning. Pain grades consider both the intensity of pain and pain-related disability to more fully capture the impact of chronic pain on function than looking at these variables in isolation. Pain grades have been validated and used in adult chronic pain samples18,19, and have been used in adolescents20. We hypothesize that as in previous studies, about 1/3 of the sample will fall into the most severe pain grade19, which will be characterized by lowest physical and psychosocial function. Finally, aim three is to examine associations among maternal and child characteristics to evaluate baseline associations between mother and child pain and psychological functioning, and to examine whether child pain and function differs by maternal pain grade, child gender, or are associated with child age. We hypothesize that child pain and psychosocial function will differ by maternal grade, such that functioning is better in lower pain grade categories. We also hypothesize that compared to males, female children will report higher pain, somatic symptoms, and psychological symptoms, and that older age would be associated with higher pain, somatic symptoms, and psychological symptoms.
Method
Mothers with chronic pain and their children (n = 400 dyads) were recruited for a longitudinal, multisite study examining the impact of maternal chronic pain on children’s emotional and physical functioning. Eligibility criteria for mothers included self-report of: (a) the presence of a current chronic pain condition for at least the past 6 months that has been diagnosed by a physician, (b) pain occurs at least weekly, (c) received medical care (e.g., physician, physical therapy, acupuncture) for chronic pain within the past 6 months, (d) living in the same home as a biological child (age 8–12 years) at least 50% of the time, and (e) ability to complete online questionnaires in English. Exclusion criteria for mothers included: (a) current pain attributable to a diagnosed life-threatening or chronic disease (e.g., cancer, lupus), and (b) psychiatric hospitalization within the past 6 months. Children were eligible to participate in the present study if they had the cognitive and English language abilities to complete online questionnaires, and did not have a life-threatening illness or chronic disease (e.g., cancer, inflammatory bowel disease).
The current publication reports findings from the complete baseline dataset collected as part of a longitudinal study that includes dyadic data collection occurring at three annual time points. Previous publications using incomplete subsamples of this baseline dataset explored the impact of maternal adverse childhood experiences on maternal function and the intergenerational impact on child depression21, and described a methodological approach for utilizing the PROMIS-29 domains to create profiles of health and function of mothers with chronic pain22. Neither of these prior publications examined the validity or utility of pain grades in characterizing mothers with chronic pain, and the PROMIS-29 manuscript included consideration of a limited number of pain characteristics (pain intensity and pain interference) only in the context of the other PROMIS domains. The present manuscript makes a novel contribution by broadly examining concurrent associations between maternal and child pain and physical and psychological function in the complete baseline dataset, which is a large national sample. It also uses pain grades to classify women with chronic pain who are mothers, and uses this classification to examine concurrent associations between maternal pain grade and child pain and psychosocial function.
Procedures
Mothers were recruited from multiple sources, including from three multidisciplinary pain management clinics at academic medical centers in urban areas (i.e., Oregon Health & Science University in Portland, OR, Stanford University in Palo Alto, CA, and the University of Washington in Seattle, WA; 21.5% of sample), online social media advertisements (e.g., Facebook, Twitter; 55.5%), and research and patient support group databases (e.g., ResearchMatch, local university postings, electronic mailing to patient groups; 23.0%). The resulting national sample included representation from 47 states in the United States (no participants from Delaware, Rhode Island, or Wyoming were enrolled). Mothers completed an initial online contact form indicating interest in receiving more information about the study. Trained research assistants spoke with interested mothers over the phone to provide further information regarding the study and screen for eligibility. If there was more than one eligible child in the target age range who was willing to participate in the study, the mother was asked to select just one child to participate in the study. Children were not specifically recruited or selected for participation in the study based on gender or chronic pain status.
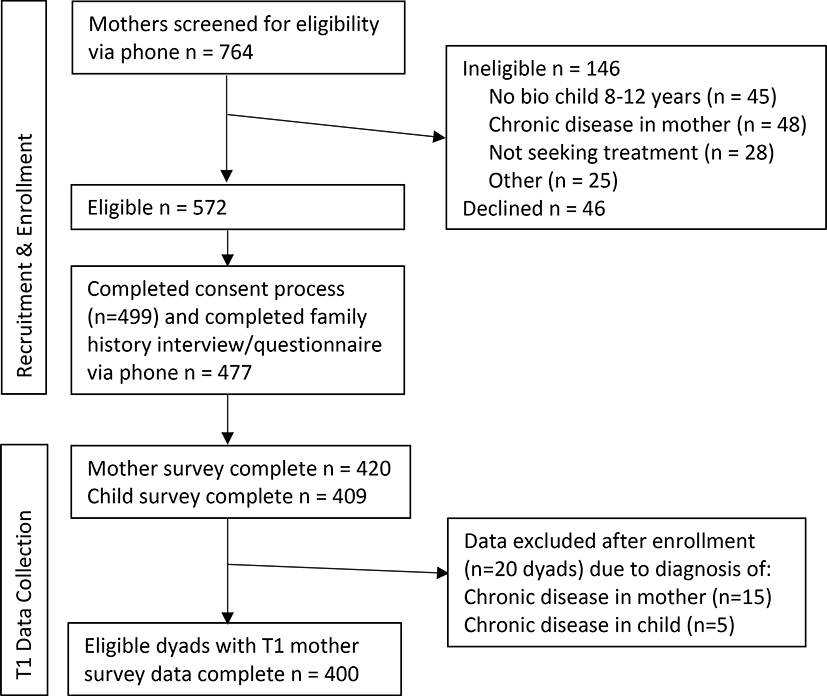
Interested and eligible participants were provided with electronic copies of the consent and assent forms which were reviewed over the phone. Following consent, mothers completed an interview via phone and both mothers and children completed an online battery of study questionnaires as well as a 7-day electronic daily diary. See Figure 1 for enrollment and eligibility.Planned annual follow-up is ongoing, and includes completion of questionnaires and diaries once a year over three years, to provide data for testing longitudinal hypotheses. All questionnaires and diary reports were administered via Research Electronic Data Capture (REDCap)23. The study procedures were approved by the institutional review board at each participating academic medical center.
Figure 1.
Screening, enrollment, and data collection
Measures
Maternal Report Measures
Family, Pain History, and Sociodemographic Information
Upon enrollment, mothers completed a structured phone interview with a trained research assistant. Mothers provided information about family structure, maternal age of onset of chronic pain, and maternal pain diagnoses. Mothers also completed a sociodemographic questionnaire, including items assessing maternal education, family income, child gender, and maternal and child racial, and ethnic background.
Maternal Pain Characteristics
Mothers were asked to report on their current pain characteristics (e.g., frequency, average intensity) using the Brief Pain Inventory (BPI). The BPI has been widely used and demonstrated excellent reliability and construct validity in adults with chronic pain24,25. Current pain locations were assessed with a standardized female front and back body map with 74 possible regions26,27. These regions were collapsed to capture overlap in the front and back views, resulting in a range of 0–25 pain locations. The presence or absence of generalized pain was determined based off of criteria for diagnosing fibromyalgia through computing sum scores for each of five body regions (left upper, right upper, axial, left lower, right lower).28 The participant met criteria for generalized pain if four out of five regions were reported as having pain on the Widespread Pain Index (WPI) body map, as per previous research29. Mothers also reported on current prescription and over the counter (OTC) medication. For each medication, mothers listed their reason for use. Research staff coded each medication list based on prescription medication type (e.g., antidepressants, opioid analgesics, and gabapentinoids).
Maternal pain grades were created using an aggregate of severity and disability based on maternal responses on the Brief Pain Inventory (BPI). This pain grade system is adapted from the Chronic Pain Grade Scale19, but uses BPI pain interference scores to represent disability, which reflects pain interference in the past 7 days. A 0–100 summary score for pain severity was derived by calculating maternal mean ratings of worst, average, and present pain ratings and then multiplying by 100. Similarly, the disability score was generated by maternal reports of pain interference with general, recreational/social, and work-related activities. Mean ratings were multiplied by 100 to create a 0–100 disability scale. Quartiles were used to determine cutoffs for disability status and thereafter translated to assigned point values: ≤ 39 = 0 points; 40–56 = 1 point; 57–72 = 2 points; and ≥ 70 = 3 points. Chronic pain grades were assigned based on the following criteria: Grade I, pain severity < 50, disability points ≤ 1 (low pain intensity, low disability); Grade II, pain severity ≥ 50, disability points ≤ 1 (high pain intensity, low disability); Grade III, any pain severity, disability points = 2 (high disability, moderately limiting); and Grade IV, any pain severity, disability points = 3 (high disability, severely limiting).
Maternal Physical and Psychological Function
Mothers completed the PROMIS-29 Profile v2.030, which assesses general emotional health and physical functioning in 7 domains (4 questions each). The domains of Physical Functioning, Fatigue, and Sleep Disturbance were used to assess physical and health function, and the domains of Anxiety, Depression, and Ability to Participate in Social Roles and Activities were used to assess psychological function. For each PROMIS scale with greater than 50% of items completed, a prorated total raw score was computed based on the number of items completed and raw scores were converted to T-scores based on the data tables provided through scoring manuals in the Assessment Center.
Child Report Measures
Child Pain Characteristics
Frequency and intensity of child pain was assessed with questions that referenced one’s experience in the past 3 months. Pain intensity was measured using an 11-point Numeric Rating Scale (0–10). Frequency was assessed via a Likert scale with seven response options, ranging from “not at all” to “daily.”31 Current pain locations were assessed with a standardized male or female front and back body map with 74 possible regions 32. These regions were collapsed to capture overlap in the front and back views, resulting in a range of 0–25 pain locations. The presence or absence of generalized pain was determined by computing sum scores for each of five body regions (left upper, right upper, axial, left lower, right lower).28 The child met criteria for generalized pain if four out of five regions were reported as having pain on the Widespread Pain Index (WPI) body map29. The presence or absence of chronic pain was defined as pain at least weekly at an intensity at or above 3 on the 11-point NRS scale. Categories of widespread pain and chronic pain were not mutually exclusive.
Child Somatic Symptoms
The 24-item Child Somatic Symptom Inventory (CSSI-24)33 was used to assess the presence and severity of somatic complaints.34 Children report on how much they were bothered by a range of physical symptoms in the past 2 weeks on a scale ranging from 0 “Not at all” to 4 “A whole lot”. Symptoms include difficulty breathing, chest pain, nausea, headache, and heart beating too fast. Formerly known as the Children’s Somatization Inventory, clinical reference points derived from a sample of youth with chronic pain have established that total scores between 0 and 18 reflect low somatic symptoms, scores between 19 and 31 reflect moderate somatic symptoms, and scores ≥ 32 reflect high somatic symptoms.33
Child Functional Disability
Children rated their perceived difficulty in daily physical psychosocial activities using the 15-item Functional Disability Inventory (FDI).35,36 Children rate how much difficulty they have had completing daily activities (e.g., “walking up stairs,” “doing chores at home,” “being at school all day”) on a 5-point scale ranging from 0 “No trouble” to 4 “Impossible.” Responses are summed to create a total score. Established clinical reference points indicate that total scores of 0–12 represent low disability, 13 to 29 represent moderate disability, and ≥ 30 represents severe disability.37
Child Anxiety Symptoms, Depressive Symptoms, and Perceived Stress
Children completed the 8-item PROMIS Pediatric Anxiety and Depressive Symptoms short forms, as well as the 4-item Perceived Stress short form. Developed by the National Institutes of Health (NIH) using item response theory, the anxiety and depressive symptoms short forms have demonstrated construct validity and convergent validity among youth.38,39 A total raw score was computed for each short-form by summing individual items. Raw scores were then converted to T-scores based on the data tables provided through scoring manuals in the Assessment Center.
Data Analytic Plan
Analyses were conducted with SPSS v25.0. Descriptive statistics were used to characterize the sample by key demographic factors and pain-related variables. Analysis of variance (ANOVA) evaluated potential differences in maternal characteristics (e.g., age, pain intensity number of pain locations) by recruitment source (i.e., pain clinic, online social media, and other advertisement). Chi-squared analyses evaluated potential differences in categorical maternal characteristics (e.g., race, marital status, annual household income) by recruitment source. Descriptive statistics were used to characterize maternal healthcare and medication use, and to describe physical and psychological functioning of children in the sample.
Mothers were classified into chronic pain grades, and separate multivariate analysis of covariance (MANCOVAs) with household income and maternal education level as covariates evaluated the relation between maternal chronic pain grade and the following domains of interest: maternal physical function (physical function, sleep disturbance, and fatigue), maternal psychosocial function (ability to function in social roles, anxiety, and depression symptoms), child pain and disability (usual pain intensity, somatic symptoms, disability), and child psychological function (anxiety, depression, stress). These sets of dependent variables were determined a priori based on maternal and child domains of interest, to broadly test the association between maternal pain grades and outcomes of interest. Chi-squared analyses also examined the presence of maternal widespread pain and prescription medication class by pain grade. Bivariate correlations were also used to evaluate concurrent associations between maternal pain and psychosocial characteristics and child pain and psychological function. Independent samples t-tests and bivariate correlations were used to examine associations between child age, gender, and child pain and psychological function variables.
Results
Maternal characteristics
See Table 1 for sociodemographic and clinical pain characteristics of mothers in the sample. Mothers were an average of 40.14 years of age (SD = 5.81), with mean pain duration of 15.75 years (range = 6 months – 46 years; SD = 10.19 years). Pain onset during childhood or adolescence (<18 years) was reported by 27.5% of the sample. Primary pain problems included fibromyalgia (36.0%), neck/back pain (25.0%), head pain (migraine, headaches, orofacial pain; 17.3%), other musculoskeletal pain (e.g., limb, joint; 14.1%), Complex Regional Pain Syndrome (4.8%), pelvic pain (2.3%), and irritable bowel syndrome (0.8%). The majority of the sample (74.7%) reported two or more pain problems. Mothers reported an average of 10.58 pain locations (possible range 0–25; SD = 6.57), with 56.0% of mothers meeting criteria for generalized pain. Maternal pain duration was associated with the presence of generalized pain (Spearman’s rho = .17, p = .001). Mothers reported on the age that they were when they first had a problem with chronic pain, and reported pain onset as follows: childhood or adolescence (<18 years), n = 110 (27.5%); young adulthood (18–24 years), n = 74 (18.5%); adulthood 25–39 years, n = 181 (45.3%), and adulthood ≥40 years, n = 35 (8.8%). Distribution of the maternal pain grade classification was as follows: Grade I (low intensity, low disability), n = 102 (25.6%); Grade II (high intensity, low disability), n = 111 (27.8%); Grade III (high disability, moderately limiting), n = 83 (20.8%); and Grade IV (high disability, severely limiting), n = 103 (25.8%). The majority of mothers (60.5%) reported taking prescription medications for pain. Specifically, 42.0% of the sample reported currently taking a prescription opioid analgesic (either as needed or daily), 44.1% of the sample reported a current antidepressant prescription, 29.7% reported a current gabapentinoid prescription, 26.2% reported a current muscle relaxant, and 22.4% reported a current prescription NSAID.
Table 1.
Descriptive statistics of maternal and child sociodemographic variables
| Maternal Factors | |||
| M (SD) or n (%) | M (SD) or n (%) | ||
| Age in Years | 40.14 (5.81) | Annual Household Income | |
| Race/Ethnicity | ≤ $25,000 | 49 (12.7) | |
| White | 361 (90.5) | $25,0001–$49,999 | 83 (20.8) |
| Asian | 10 (2.5) | $50,000–$79,999 | 73 (18.3) |
| Black or African American | 4 (1.0) | $80,0000–$119,000 | 108 (27.0) |
| American Indian or Alaska Native | 4 (1.0) | $120,000–$149,999 | 31 (7.8) |
| Other | 2 (.5) | ≥$150,000 | 43 (10.8) |
| Bi- or Multiracial | 18 (4.5) | Educational Background | |
| Hispanic or Latina | 21 (5.3) | ≤ High School | 26 (6.5) |
| Marital Status | Vocational School/Some College | 120 (30.0) | |
| Married | 301 (75.4) | College | 155 (38.8) |
| Divorced | 51 (12.8) | Graduate/Professional School | 98 (24.5) |
| Separated | 11 (2.8) | Employment Status | |
| Remarried | 11 (2.8) | Full-time | 108 (27.3) |
| Never Married | 25 (6.3) | Part-time | 83 (20.8) |
| Number of Children in Home | 2.28 (1.23) | Unemployed | |
| Not working by choice | 92 (23.3) | ||
| Currently unemployed | 44 (11.0) | ||
| Receiving disability | 68 (17.0) | ||
| Child Factors | |||
| n (%) | M (SD) or n (%) | ||
| Race/Ethnicity | Age in Years | 9.82 (1.36) | |
| White | 333 (83.3) | Gender | |
| Asian | 10 (2.5) | Female | 201 (50.2) |
| Black or African American | 6 (1.5) | Male | 196 (49.0) |
| American Indian or Alaska Native | 3 (0.8) | Other/Non-binary | 3 (0.8) |
| Other | 3 (0.8) | ||
| Bi- or Multiracial | 45 (11.3) | ||
| Hispanic or Latina | 49 (12.3) | ||
Data on income reported by n = 387 mothers; all other variables n = 399–400
Maternal sociodemographic characteristics (see Table 1), including maternal age, race, ethnicity, education level, number of children in the home, and marital status did not differ by recruitment source. Family income significantly differed by recruitment source, F(2, 384) = 8.11, p < .001. Post hoc contrasts indicated that mothers recruited through pain clinics had significantly higher income than those recruited through social media (p < .001) and those recruited through research and patient databases (p = .05). Maternal pain intensity, pain interference, and pain grade classification were similar by recruitment source. Recruitment sources differed on number of pain locations, F(2, 297) = 5.64, p = .004. Post hoc contrasts indicated that mothers recruited through social media reported a significantly higher number of pain locations assessed via survey administered body map (M = 11.46, SD = 6.53) than those recruited through pain clinics (M = 8.85, SD = 6.28; p = .001).
Child pain experiences and psychological characteristics
See Table 1 for child sociodemographic characteristics. Descriptive statistics for child pain and psychological variables can be found in Table 2. Missingness was low in the child data, with at least 96.8% (n = 387–393) of the sample providing responses across all child report variables. Many of the children in the sample reported minimal pain in the past 30 days, with 59.8% reporting pain 1–3 times per month or less. When asked to consider the past three months, mean usual pain intensity on a 0–10 NRS was 3.30 (SD = 2.26). Approximately one-third of children reported pain consistent with chronic or recurrent pain (32.8%, n = 131), when defined as pain at least weekly at an intensity at or above 3 on an 11-point NRS scale. When defined more stringently as pain at least weekly at an intensity at or above 4 on an 11-point NRS, n = 70 (17.8%) met these criteria. Children reported a mean of 2.49 (SD = 2.96) of 25 possible pain locations, and 5.1% of the sample met criteria for Widespread Pain. The majority of the sample reported low levels of somatic symptoms, but 30.0% were in the moderate to high range. A small proportion of children reported moderate to high functional disability (20.8%). The majority of children reported normative levels of anxiety, depression, and perceived stress, with less than 15% of the sample reporting elevated symptoms in these domains (see Table 2).
Table 2.
Child report of pain-related characteristics and psychological function
| Pain-related Characteristics | M (SD) or n (%) | Elevated/Clinical Range % | |
|---|---|---|---|
| Pain Frequency in Past 3 months | ≥ 2–3 times/week | 22.6% | |
| Not at all | 77 (19.3%) | ||
| Less than 1 time per month | 64 (16.0%) | ||
| 1–3 times per month | 98 (24.5%) | ||
| About 1 time per week | 63 (15.8%) | ||
| 2–3 times per week | 40 (10.0%) | ||
| 4–6 times per week | 21 (5.3%) | ||
| Daily (n = 392) | 29 (7.3%) | ||
| Usual Pain Intensity (0–10 NRS) (n = 391) | 3.30 (2.26) | NRS 4–6 | 40.4% |
| NRS 7–10 | 8.2% | ||
| Number of Pain Locations (0–25) (n = 393) | 2.49 (2.96) | ≥ 3 locations | 37.9% |
| Widespread Pain | 5.1% | ||
| Somatic Symptoms (n = 386) | 13.72 (12.71) | Moderate (19–31) | 16.0% |
| High (≥ 32) | 14.0% | ||
| Functional Disability (n = 387) | 6.56 (8.86) | Moderate (13–29) | 14.5% |
| Severe (≥ 30) | 6.3% | ||
| Psychological Function | |||
| Anxiety Symptoms (n = 393) | 47.97 (10.28) | T scores > 60: | 13.5% |
| Depressive Symptoms (n = 391) | 48.01 (9.79) | T scores > 60: | 12.3% |
| Perceived Stress (n = 388) | 52.04 (9.23) | T scores > 60: | 18.3% |
Maternal physical and clinical factors by pain grade
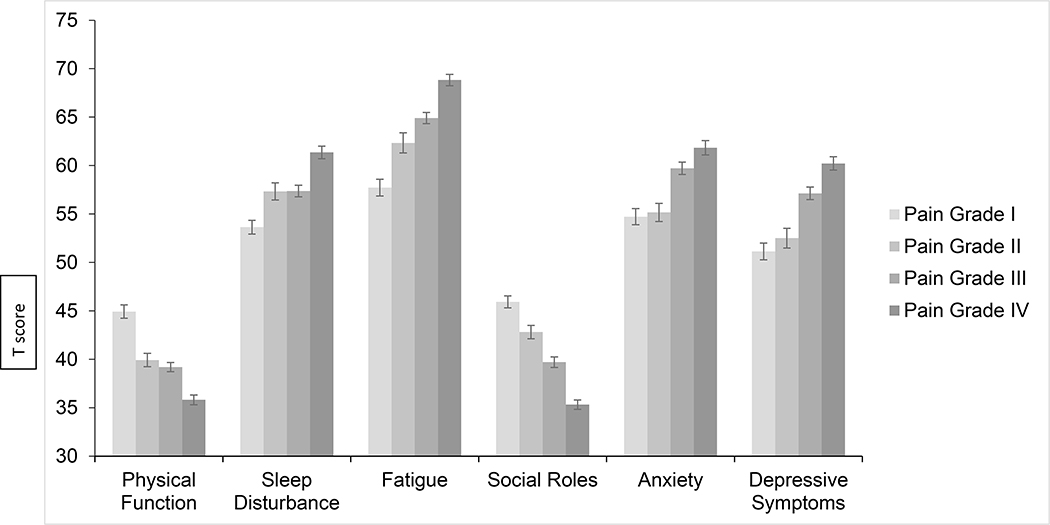
Results indicated significant differences by pain grade for physical function, fatigue, and sleep disturbance, Wilk’s Λ = .68, F(9, 917.6) = 17.19, p < .001, ηp2 = .12 (see Table 3 for descriptive statistics by pain grade). Follow-up univariate tests indicated maternal chronic pain grades significantly differed for all three variables: physical function, F(3, 379) = 33.99, p < .001, ηp2 = .21, fatigue, F(3, 379) = 33.41, p < .001, ηp2 = .21, and sleep disturbance, F(3, 379) = 16.37, p < .001, ηp2 = .12 (see Figure 2). Post hoc tests with Bonferonni adjustments for multiple comparisons evaluated pairwise comparisons between maternal chronic pain grades. Mothers in Grade I, compared to mothers in Grades II-IV, reported significantly higher physical functioning, lower fatigue, and lower sleep disturbance (p-values range from < .001 to .029). Mothers in Grade IV, compared to mothers in Grades I-III, reported significantly lower physical functioning, greater fatigue, and greater sleep disturbance (p-values range from < .001 to .008). Mothers in Grades II and III did not significantly differ on physical functioning, fatigue, or sleep disturbance (all p-values > .05).
Table 3.
Descriptive statistics of maternal and child function by pain grade
| Pain Grade I (n = 86) | Pain Grade II (n = 60) | Pain Grade III (n = 126) | Pain Grade IV (n = 128) | |
|---|---|---|---|---|
| Maternal Physical Function | ||||
| Physical Functionb | 44.92 (6.47)c | 39.92 (5.42)d | 39.19 (5.67)d | 35.81 (5.67)d,e |
| Sleep Disturbancea | 53.64 (6.53)c | 57.33 (6.92)d | 57.37 (6.58)d | 61.36 (7.40)d,e |
| Fatiguea | 57.72 (8.17)c | 62.34 (8.09)d | 64.91 (6.55)d | 68.83 (6.62)d,e |
| Maternal Psychosocial Function | ||||
| Social Rolesb | 45.93 (5.77)c | 42.81 (5.34)d | 39.70 (5.04)e | 35.32 (5.47)f |
| Anxietya | 54.72 (7.98)c | 55.16 (8.09)c | 59.71 (7.43)d | 61.83 (8.10)d |
| Depressive Symptomsa | 51.14 (8.03)c | 52.51 (7.59)c | 57.13 (7.26)d | 60.22 (7.81)d,e |
| Child Pain, Somatic Symptoms, and Disability | ||||
| Usual Pain Intensity | 2.95 (2.18) | 3.41 (2.41) | 3.24 (2.14) | 3.55 (2.35) |
| Somatic Symptoms | 10.68 (10.45) | 13.52 (12.04) | 14.07 (12.47) | 15.55 (14.31) |
| Functional Disability | 5.05 (6.59) | 4.69 (5.79) | 6.99 (10.25) | 8.02 (9.59) |
| Child Psychological Symptoms | ||||
| Anxietya | 46.42 (9.21) | 46.22 (9.67) | 49.06 (10.60) | 48.71 (10.77) |
| Depressive Symptomsa | 45.81 (8.84) | 46.50 (7.89) | 48.23 (10.42) | 49.92 (10.22) |
| Stressa | 50.25 (8.02) | 50.42 (7.70) | 52.61 (10.14) | 53.46 (9.48) |
Scores are T scores, with higher scores indicating higher levels of symptoms.
Scores are T scores, with lower scores indicating lower functioning.
Differing superscripts denote significant post hoc contrasts.
Figure 2.
Maternal reports on PROMIS measures by pain grade
Maternal pain grades significantly differed on the proportion of mothers who met criteria for generalized pain, Χ2(3, 397) = 7.77, p = 0.05, and the proportion of mothers who reported an opioid analgesic prescription, Χ2(3, 397) = 22.01, p < .001. Specifically, a greater proportion of mothers in Grade IV (62.2%) reported generalized pain compared to mothers in Grade I (43.5%). Grades II (60.0%) and III (56.8%) did not significantly differ from Grades I and IV on generalized pain. Regarding opioid use, a greater proportion of mothers in Grades II (43.3%), III (47.2%), and IV (50.4%) reported an opioid prescription compared to Grade I (20.0%). Maternal pain grades did not significantly differ on antidepressant medications, Χ2(3, 397) = 7.07, p = 0.07, range: 31.8%−49.6%, or gabapentinoid medications, Χ2(3, 397) = 5.18, p = 0.16, range: 20% – 33.6%.
Maternal psychosocial function by pain grade
Results indicated maternal chronic pain grade groups significantly differed on maternal psychosocial function, Wilk’s Λ = .62, F(9, 920.10) = 22.14, p < .001, ηp2 = .15 (see Table 3 for descriptive statistics by pain grade). Follow-up univariate tests indicated maternal chronic pain grades significantly differed for all three psychosocial function variables: ability to function in social roles, F(3, 380) = 61.09, p < .001, ηp2 = .33, anxiety, F(3, 380) = 15.07, p < .001, ηp2 = .11, and depressive symptoms, F(3, 380) = 24.71, p < .001, ηp2 = .16 (see Figure 2). Post hoc tests with Bonferonni adjustments for multiple comparisons evaluated pairwise comparisons between maternal chronic pain grades. Regarding ability to function in social roles, mothers in Grade I reported significantly better functioning than mothers in Grade II, who reported significantly better functioning than mothers in Grade III, who, in turn reported significantly better functioning than mothers in Grade IV (p-values range from < .001 to .009). For anxiety, mothers in Grades I and II reported lower anxiety than mothers in Grades III and IV (p-values < .002). Regarding depressive symptoms, mothers in Grades I and II reported significantly lower depressive symptoms than mothers in Grades III and IV (p-values < .001). Mothers in Grade IV reported significantly greater depressive symptoms than mothers in Grade III (p-value = .02).
Child pain and functioning in the context of maternal factors
Correlations among maternal and child factors are presented in Table 4. Maternal pain intensity was significantly positively associated with child pain intensity. Maternal pain-related disability was positively correlated with child pain-related disability, somatic symptoms, anxiety, depressive symptoms, and stress. Maternal pain duration and presence of widespread pain were positively associated with child pain frequency, and widespread pain was also significantly correlated with child number of pain locations and pain-related disability. Maternal anxiety and depressive symptoms were positively correlated with child pain-related disability, somatic symptoms, perceived stress, anxiety, and depressive symptoms. Maternal physical function, fatigue, and social function were also significantly associated with child perceived stress, anxiety and depressive symptoms. Maternal fatigue and social function were associated with child somatic symptoms. All correlations were in the expected direction but were small, with better maternal function associated with better child function (see Table 4).
Table 4.
Bivariate correlations among parent and child pain and psychological factors
| Child Factors | ||||||||
|---|---|---|---|---|---|---|---|---|
| Pain Intensity | Pain Frequency | Number of Pain Locations | Pain-related Disability | Somatic Symptoms | Anxiety | Depressive Symptoms | Stress | |
| Child Factors | ||||||||
| Child Gender | −.01 | −.14** | −.05 | −.06 | −.10 | −.04 | −.07 | −.03 |
| Child Age | .09 | .14** | .06 | .05 | .13** | −.06 | −.04 | .12* |
| Maternal Factors | ||||||||
| Pain Intensity | .13* | .02 | .09 | .06 | .07 | .04 | .02 | .04 |
| Pain-related Disability | .01 | .02 | .06 | .15** | .15** | .14** | .18** | .16** |
| Pain Duration | .06 | .13* | −.01 | .07 | .09 | .02 | .08 | .08 |
| Widespread Pain | .01 | .12* | .13** | .12* | .07 | .04 | .02 | .08 |
| Fatigue | .03 | .04 | .12* | .09 | .15** | .13** | .17** | .11* |
| Sleep Disturbances | .01 | .01 | .05 | .01 | .07 | −.01 | .02 | −.00 |
| Anxiety | −.02 | .05 | .08 | .10* | .10* | .17** | .18** | .16** |
| Depressive Symptoms | .01 | .10* | .07 | .10* | .15** | .17** | .22** | .18** |
| Social Function | .01 | −.06 | −.07 | −.13** | −.13** | −.15** | −.20** | −.17** |
| Physical Function | −.06 | −.04 | −.03 | −.07 | −.10 | −.14** | −.16** | −.16** |
Notes
p <.05
p <.001
Gender coded as 0=female, 1=male; correlations with categorical variables are Spearman’s Rho; All maternal report variables n = 400 with the exception of Physical Function (n = 399).
MANCOVA results examining child pain intensity, somatic symptoms, and functional disability indicated that children did not differ significantly by maternal chronic pain grade groups in the overall model, Wilk’s Λ = .97, F(9, 881.16) = 1.34, p = .212, ηp2 = .01 (see Table 3 for descriptive statistics by pain grade). Univariate tests found no significant differences by maternal chronic pain grades in any of these individual variables, although univariate tests for somatic symptoms and functional disability had trend level p values. The MANCOVA result examining child psychological function (anxiety, depression, stress) by maternal pain grade was also not significant, Wilk’s Λ = .96, F(9, 888.46) = 1.51, p = .139, ηp2 = .01 (see Table 3 for descriptive statistics by pain grade). Univariate tests were not significant with the exception of the depression domain, F(3, 367) = 2.84, p < .05.
Analyses examining child gender differences included those identified as male or female, and found pain frequency was higher in females than in males t(387) = 2.73, p = .007; females were about twice as likely to report pain ≥ 2–3 times per week (29.1%) compared to males (16.6%; OR = 2.06, 95% CI: 1.27, 3.36). Usual pain intensity did not significantly differ by child gender. Child age showed small but significant correlations with pain frequency, such that older children reported greater pain frequency in the past 3 months. Somatic symptoms, functional disability, and psychological function were not different by child gender. Older child age also showed small but significant associations with somatic symptoms and perceived stress (see Table 4).
Discussion
This study describes baseline pain-related, clinical, and psychological function in a large dyadic sample of mothers with chronic pain conditions and their 8–12-year old children. To our knowledge, this is the first large cohort study that is designed to test candidate longitudinal mechanisms of intergenerational transmission of chronic pain in a sample of mothers receiving treatment for chronic pain conditions. Mothers in this sample are evenly distributed across pain grade classification groups, and pain grade is broadly related to maternal physical health and function, as well as to psychosocial function. It is notable that about a quarter of this sample (27.5%) reported that their pain problem started in childhood or adolescence, highlighting both the chronicity of pain for these mothers and the importance of considering pain from a lifespan and intergenerational perspective. Results from the current study grouped mothers into previously determined pain grade categories and findings support the validity of the pain grade categorical approach in this sample, in terms of pain grade being associated with physical and psychosocial function. This approach also highlights that there is substantial variability in pain and disability within the sample, and variability in general health and psychosocial functioning, suggesting that for children, having a mother with a chronic pain condition is not a unidimensional risk factor and is likely to create a range of different experiences and environments.
Maternal pain grades, derived from pain intensity and pain interference, were not significantly associated with child pain and function overall. There are various a priori and data-driven statistical approaches for classifying patients based on function across a number of domains22. Some of these classification approaches might be used to help identify which children might be most at risk of developing chronic pain, or which mothers might benefit most from pain, psychology, or parenting interventions. The pain grade system used in the current study is similar to emerging approaches to classify patients as having High Impact Chronic Pain (HICP)40,41, although in addition to considering disability, the classification of HICP incorporates assessment of pain duration (at least 3 or 6 months) and frequency (daily or almost daily). As all participants in the current sample had pain for at least 6 months, use of the HCIP classification approach may not yield much variation. Previously published results from a subset of this sample that considered maternal functioning across a number of domains using a latent profile approach (including sleep disturbance, fatigue, depression, and social function) did observe associations among these profiles and child functioning22, suggesting that at least in this developmental stage, it may be useful to consider a range of maternal characteristics predicting child outcomes in the offspring of mothers with chronic pain. One key difference between the PROMIS 29 profiles and the Pain Grade approach is the inclusion of psychological symptoms and role functioning in classification. The finding that maternal PROMIS 29 profiles were associated with child pain frequency, somatic symptoms, and depressive symptoms, but the same pattern was not observed with maternal pain grades, highlights the potential impact of maternal psychological comorbidities in the intergenerational transmission of risk. Researchers need to consider advantages and disadvantages to these various classification methods in terms of length of assessment, source of data (chart review vs. patient report), timeframe of assessment, the inclusion of domains other than pain intensity and disability, and which approaches are best tailored to the research question of interest.
Future research with this sample will incorporate the use of pain grades as well as other important domains of physical and psychosocial functioning. Longitudinal data will allow us to test the stability of maternal pain grades over time, and associations among pain grade and maternal clinical and psychosocial characteristics over time. Additionally, this high-risk sample is comprised largely of young school-age children who have not yet developed chronic pain, so the relationship between child function and maternal pain grade may change over time. It is also possible that the stability of higher pain grade status or worsening pain grade in mothers in this sample may negatively impact children over time.
Many of the domains of maternal functioning that were assessed in this study, including maternal disability, physical function, fatigue, anxiety, depression, and social roles, were significantly associated with most measures of child function (somatic symptoms, disability, anxiety, depression, and stress), and will also be incorporated into longitudinal models with this sample. However there were two domains of maternal function that were not related to child variables; maternal pain intensity was only associated with child pain intensity, and maternal sleep disturbance was not associated with any child variables. Maternal pain grades, derived from pain intensity and pain interference, were also not significantly associated with child pain or psychological functioning overall (although the univariate test did find differences in child depression by maternal pain grade in the expected direction). However, other maternal pain characteristics (pain duration and presence of widespread pain) were positively associated with child pain frequency, and the presence of widespread pain in mothers was additionally associated with child number of pain locations and pain-related disability.
While pain grades do map onto maternal physical and psychosocial function, they include a limited set of pain characteristics that may not be observable to children. It is possible that some of the other maternal domains examined (fatigue, physical function, depression, widespread pain) are more observable by children or have a more direct impact on children’s daily experiences. Observed associations between individual maternal and child variables were small but significant, and it will be important to examine the potential additive and interactive contributions of maternal pain and function to child outcomes in this sample over time. The pattern of associations found in the current study also provides some glimpse into potential protective factors for these children. For instance, higher maternal social and physical functioning were related to lower child depression, anxiety, and stress, suggesting that supporting mothers in their efforts to maintain social connections and physical function despite chronic pain may have a positive impact on child risk.
It is important to note that at this baseline data collection point, most of the 8–12 year old children of these mothers are doing well and functioning in normative or non-clinical ranges in terms of somatic symptoms and psychological functioning. However, about a third of the sample is experiencing pain that occurs at least weekly in the past 3 months and at ≥3/0–10 in intensity. There are few studies of the offspring of parents with chronic pain that have focused on school-age children in particular, but this rate of pain problems is similar to what has been seen in other samples of the offspring of parents with pain in this age range13,42. Given the increasing prevalence of pain in adolescence43, we do expect that an increasing proportion of the children in this sample will develop clinically significant chronic pain problems over time. The mean level of somatic symptoms reported in this sample is higher than what has been reported in school samples44, but lower than what has been observed in clinical samples of youth with chronic pain33, suggesting that the children of mothers with chronic pain are best characterized as an at-risk sample. Data collected over the three years when these youth transition to early adolescence will allow for examination of mechanisms that might explain trajectories of increasing pain, somatic symptoms, and psychological symptoms, as well as identification of individual, maternal, or family factors that may serve a protective function.
Over 5% of the children in this sample of school-aged children are reporting widespread pain, in 4 out of 5 body regions. These youth are highly likely to have widespread pain persist into adolescence45, and research on adolescents with widespread chronic pain (juvenile fibromyalgia), has shown that the majority of these youth still experience pain in early adulthood46. Similar to adults, children and adolescents with more widespread pain experience lower quality of life and higher functional impairment than youth with fewer pain sites47, and have higher disability trajectories in the context of intense treatment for pain48. Thus, these youth may represent a subgroup that is most at risk for developing highly disabling chronic pain conditions, and might be targeted for intervention. Not every child from this at-risk sample will develop chronic pain, but the early identification of those who are at greatest risk would provide an opportunity to intervene earlier in development and potentially prevent costly and disabling pain in adulthood. Other potential approaches for identifying youth who might benefit from intervention could include providing intervention to children of mothers with chronic pain with higher levels of pain-related disability, fatigue, or depression, or targeting children from this at risk population who exhibit elevations in anxiety, depression, or stress symptoms, particularly given the association between these symptoms and pain in adolescence49.
In addition to incorporating cognitive behavioral therapy components for pain management50, future interventions might target psychosocial factors such as family cohesion and low levels of loneliness, which have been shown to reduce the prevalence of widespread and multisite pain in large adolescent samples51, and might also address lifestyle factors given the additional contribution of child obesity to pain outcomes in the context of parental pain52. Forthcoming longitudinal data from this cohort will help inform which of these approaches might be most efficient or effective. Incorporating parent and child perspectives on the need for and preferences around intervention components will also be essential in future treatment development work.
There are a number of limitations that should be considered when interpreting results from the present study. First, while participants recruited from different sources were similar across most clinical variables, there were two differences that may introduce bias in the data. First, the mothers recruited from pain clinics reported higher family income than those recruited through patient databases or online advertising. This may reflect greater access to specialized healthcare services among individuals receiving care in tertiary care clinics due to higher income or private health insurance, or it may simply be reflective of the relatively high median household incomes in the cities where these clinics are located. Mothers recruited online also reported a significantly higher number of pain locations than those recruited through pain clinics. Future longitudinal analyses might control for the number of pain locations or presence of generalized pain to address this potential source of bias. Another methodological limitation is that when families had more than one child in the age range who was eligible and willing to participate, mothers were given discretion to select which child participated. It is possible that mothers systematically selected children to participate who they were most concerned about in terms of pain experiences, or it is possible that mothers might have selected the child who they perceived as being better adjusted or better able to complete study tasks. Thus the sample could potentially be biased toward higher or lower risk children. Finally, associations in this high-risk sample may not represent what might be found in populations of youth who already have chronic pain and their parents. Examining associations between maternal pain and child outcomes in other pediatric pain samples or in children of different age groups might yield different patterns of results.
Future work with longitudinal data from this sample will characterize the contributions of children’s cognitive, emotional, and general health vulnerabilities to increases in pain and other poor outcomes during this critical developmental transition from middle childhood to early adolescence. The study will use longitudinal data to identify pathways through which maternal chronic pain impacts child vulnerabilities for chronic pain and emotional outcomes over a 3-year period, and will test potential moderators of these pathways (e.g., child gender, presence or absence of chronic pain in second parent or caregiver). Recent work has provided some additional support for the potential role of parent pain behaviors and pain interference in contributing to children’s vulnerability for chronic pain by increasing child pain catastrophizing and threat appraisal11,12. There is also emerging evidence in pediatric pain samples that factors related to interpersonal or parent-child fear avoidance models, such as parent’s catastrophizing about child pain, may play less of a role when parents have chronic pain themselves53. Continued examination of the impact that maternal pain and function may have on child vulnerabilities and subsequent child pain experiences is a key next step for research in this area, as is the identification of potential protective factors. Conducting this work in at risk samples of the offspring of parents with chronic pain conditions will provide unique insight into potential mechanisms of the intergenerational transmission of chronic pain and related outcomes.
Acknowledgments
This study was supported by the National Institutes of Health, Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01 HD082200; PI Wilson), as well as the National Center for Advancing Translational Sciences of the National Institutes of Health under award number UL1TR0002369 and UL1TR000128. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Dr. Cordts is now at the Department of Psychiatry, University of Nebraska Medical Center.
REFERENCES
- 1.Groenewald CB, Essner BS, Wright D, Fesinmeyer MD, Palermo TM. The economic costs of chronic pain among a cohort of treatment-seeking adolescents in the United States. The journal of pain : official journal of the American Pain Society. 2014;15(9):925–933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Simon LS. Relieving pain in America: A blueprint for transforming prevention, care, education, and research. Journal of pain & palliative care pharmacotherapy. 2012;26(2):197–198. [Google Scholar]
- 3.Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: results of an Internet-based survey. The journal of pain : official journal of the American Pain Society. 2010;11(11):1230–1239. [DOI] [PubMed] [Google Scholar]
- 4.Piira T, Pullukat R. Are the children of chronic pain patients more likely to develop pain? Enfance. 2006;58(1):20–25. [Google Scholar]
- 5.Stanford EA, Chambers CT, Biesanz JC, Chen E. The frequency, trajectories and predictors of adolescent recurrent pain: a population-based approach. Pain. 2008;138(1):11–21. [DOI] [PubMed] [Google Scholar]
- 6.Campo JV, Bridge J, Lucas A, et al. Physical and emotional health of mothers of youth with functional abdominal pain. Arch Pediatr Adolesc Med. 2007;161(2):131–137. [DOI] [PubMed] [Google Scholar]
- 7.Goodman JE, McGrath PJ, Forward SP. Aggregation of Pain Complaints and Pain-Related Disability and Handicap in a Community Sample of Families. Pain Research and Management. 1997. [Google Scholar]
- 8.Coenders A, Chapman C, Hannaford P, et al. In search of risk factors for chronic pain in adolescents: a case-control study of childhood and parental associations. Journal of pain research. 2014;7:175–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hoftun GB, Romundstad PR, Rygg M. Association of parental chronic pain with chronic pain in the adolescent and young adult: family linkage data from the HUNT Study. JAMA Pediatr. 2013;167(1):61–69. [DOI] [PubMed] [Google Scholar]
- 10.Stone AL, Wilson AC. Transmission of risk from parents with chronic pain to offspring: an integrative conceptual model. Pain. 2016;157(12):2628–2639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stone AL, Bruehl S, Smith CA, Garber J, Walker LS. Social learning pathways in the relation between parental chronic pain and daily pain severity and functional impairment in adolescents with functional abdominal pain. Pain. 2018;159(2):298–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Higgins KS, Chambers CT, Rosen NO, et al. Testing the intergenerational model of transmission of risk for chronic pain from parents to their children: an empirical investigation of social transmission pathways. PAIN. in press;Articles in Press. [DOI] [PubMed] [Google Scholar]
- 13.Higgins KS, Birnie KA, Chambers CT, et al. Offspring of parents with chronic pain: a systematic review and meta-analysis of pain, health, psychological, and family outcomes. Pain. 2015;156(11):2256–2266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Higgins KS, Birnie KA, Chambers CT, et al. Offspring of parents with chronic pain: a systematic review and meta-analysis of pain, health, psychological, and family outcomes. Pain. 2015;156(11):2256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cordts KMP, Wilson AC, Riley AR. More than Mental Health: Parent Physical Health and Early Childhood Behavior Problems. Journal of developmental and behavioral pediatrics: JDBP. 2020;41(4):265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Birnie KA, Heathcote LC, Bhandari RP, Feinstein A, Yoon IA, Simons LE. Parent physical and mental health contributions to interpersonal fear avoidance processes in pediatric chronic pain. Pain. 2020;161(6):1202–1211. [DOI] [PubMed] [Google Scholar]
- 17.Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal Depression and Child Psychopathology: A Meta-Analytic Review. Clinical Child and Family Psychology Review. 2011;14(1):1–27. [DOI] [PubMed] [Google Scholar]
- 18.Elliott AM, Smith BH, Smith WC, Chambers WA. Changes in chronic pain severity over time: the Chronic Pain Grade as a valid measure. Pain. 2000;88(3):303–308. [DOI] [PubMed] [Google Scholar]
- 19.Von Korff M, Ormel J, Keefe FJ, Dworkin SF. Grading the severity of chronic pain. Pain. 1992;50(2):133–149. [DOI] [PubMed] [Google Scholar]
- 20.Beeckman M, Simons LE, Hughes S, Loeys T, Goubert L. Investigating How Parental Instructions and Protective Responses Mediate the Relationship Between Parental Psychological Flexibility and Pain-Related Behavior in Adolescents With Chronic Pain: A Daily Diary Study. Frontiers in Psychology. 2019;10(2350). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dennis CH, Clohessy DS, Stone AL, Darnall BD, Wilson AC. Adverse Childhood Experiences in Mothers With Chronic Pain and Intergenerational Impact on Children. The journal of pain : official journal of the American Pain Society. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stone AL, Holley AL, Dieckmann NF, Wilson AC. Use of the PROMIS-29(R) to identify subgroups of mothers with chronic pain. Health Psychol. 2019;38(5):422–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Daut RL, Cleeland CS, Flanery RC. Development of the Wisconsin Brief Pain Questionnaire to assess pain in cancer and other diseases. Pain. 1983;17(2):197–210. [DOI] [PubMed] [Google Scholar]
- 25.Keller S, Bann CM, Dodd SL, Schein J, Mendoza TR, Cleeland CS. Validity of the brief pain inventory for use in documenting the outcomes of patients with noncancer pain. Clin J Pain. 2004;20(5):309–318. [DOI] [PubMed] [Google Scholar]
- 26.Karayannis NV, Sturgeon JA, Chih-Kao M, Cooley C, Mackey SC. Pain interference and physical function demonstrate poor longitudinal association in people living with pain: a PROMIS investigation. Pain. 2017;158(6):1063–1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cramer E, Ziadni M, Scherrer K, Mackey S. The somatic distribution of chronic pain and emotional distress utilizing the collaborative health outcomes information registry (CHOIR) bodymap. The Journal of Pain. 2018;19(3):S53–S54. [Google Scholar]
- 28.Wolfe F, Clauw DJ, Fitzcharles M-A, et al. 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Seminars in Arthritis and Rheumatism. 2016;46(3):319–329. [DOI] [PubMed] [Google Scholar]
- 29.Wolfe F, Egloff N, Häuser W. Widespread Pain and Low Widespread Pain Index Scores among Fibromyalgia-positive Cases Assessed with the 2010/2011 Fibromyalgia Criteria. The Journal of Rheumatology. 2016;43(9):1743–1748. [DOI] [PubMed] [Google Scholar]
- 30.Hays RD, Spritzer KL, Schalet BD, Cella D. PROMIS((R))-29 v2.0 profile physical and mental health summary scores. Quality of life research : an international journal of quality of life aspects of treatment, care and rehabilitation. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Peterson CC, Palermo TM. Parental reinforcement of recurrent pain: the moderating impact of child depression and anxiety on functional disability. J Pediatr Psychol. 2004;29(5):331–341. [DOI] [PubMed] [Google Scholar]
- 32.Bhandari RP, Feinstein AB, Huestis SE, et al. Pediatric-Collaborative Health Outcomes Information Registry (Peds-CHOIR): a learning health system to guide pediatric pain research and treatment. Pain. 2016;157(9):2033–2044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stone AL, Walker LS, Heathcote LC, et al. Somatic symptoms in pediatric patients with chronic pain: Proposed clinical reference points for the Children’s Somatic Symptoms Inventory (formerly Children’s Somatization Inventory). The Journal of Pain. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Walker LS, Beck JE, Garber J, Lambert W. Children’s Somatization Inventory: psychometric properties of the revised form (CSI-24). J Pediatr Psychol. 2009;34(4):430–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Claar RL, Walker LS. Functional assessment of pediatric pain patients: psychometric properties of the functional disability inventory. Pain. 2006;121(1–2):77–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Walker LS, Greene JW. The functional disability inventory: measuring a neglected dimension of child health status. J Pediatr Psychol. 1991;16(1):39–58. [DOI] [PubMed] [Google Scholar]
- 37.Kashikar-Zuck S, Flowers SR, Claar RL, et al. Clinical utility and validity of the Functional Disability Inventory among a multicenter sample of youth with chronic pain. Pain. 2011;152(7):1600–1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Irwin DE, Stucky B, Langer MM, et al. An item response analysis of the pediatric PROMIS anxiety and depressive symptoms scales. Quality of Life Research. 2010;19(4):595–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Varni JW, Magnus B, Stucky BD, et al. Psychometric properties of the PROMIS® pediatric scales: precision, stability, and comparison of different scoring and administration options. Quality of Life Research. 2014;23(4):1233–1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pitcher MH, Von Korff M, Bushnell MC, Porter L. Prevalence and Profile of High-Impact Chronic Pain in the United States. The journal of pain : official journal of the American Pain Society. 2019;20(2):146–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dahlhamer J, Lucas J, Zelaya C, et al. Prevalence of Chronic Pain and High-Impact Chronic Pain Among Adults - United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(36):1001–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Arruda MA, Guidetti V, Galli F, Albuquerque RCAP, Bigal ME. Frequency of Headaches in Children is Influenced by Headache Status in the Mother. Headache: The Journal of Head and Face Pain. 2010;50(6):973–980. [DOI] [PubMed] [Google Scholar]
- 43.King S, Chambers CT, Huguet A, et al. The epidemiology of chronic pain in children and adolescents revisited: a systematic review. Pain. 2011;152(12):2729–2738. [DOI] [PubMed] [Google Scholar]
- 44.Vila M, Kramer T, Hickey N, et al. Assessment of somatic symptoms in British secondary school children using the Children’s Somatization Inventory (CSI). J Pediatr Psychol. 2009;34(9):989–998. [DOI] [PubMed] [Google Scholar]
- 45.Mikkelsson M, El-Metwally A, Kautiainen H, Auvinen A, Macfarlane GJ, Salminen JJ. Onset, prognosis and risk factors for widespread pain in schoolchildren: a prospective 4-year follow-up study. Pain. 2008;138(3):681–687. [DOI] [PubMed] [Google Scholar]
- 46.Kashikar-Zuck S, Cunningham N, Sil S, et al. Long-term outcomes of adolescents with juvenile-onset fibromyalgia in early adulthood. Pediatrics. 2014;133(3):e592–e600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rabbitts JA, Holley AL, Groenewald CB, Palermo TM. Association Between Widespread Pain Scores and Functional Impairment and Health-Related Quality of Life in Clinical Samples of Children. The journal of pain : official journal of the American Pain Society. 2016;17(6):678–684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Williams SE, Homan KJ, Crowley SL, et al. The Impact of Spatial Distribution of Pain on Long Term Trajectories for Chronic Pain Outcomes after Intensive Interdisciplinary Pain Treatment. Clin J Pain. 2019. [DOI] [PubMed] [Google Scholar]
- 49.Hoftun GB, Romundstad PR, Rygg M. Factors associated with adolescent chronic non-specific pain, chronic multisite pain, and chronic pain with high disability: the Young-HUNT Study 2008. J Pain. 2012;13(9):874–883. [DOI] [PubMed] [Google Scholar]
- 50.Fisher E, Law E, Dudeney J, Palermo TM, Stewart G, Eccleston C. Psychological therapies for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev. 2018;9:Cd003968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Skrove M, Romundstad P, Indredavik MS. Chronic multisite pain in adolescent girls and boys with emotional and behavioral problems: the Young-HUNT study. Eur Child Adolesc Psychiatry. 2015;24(5):503–515. [DOI] [PubMed] [Google Scholar]
- 52.Zadro JR, Nilsen TIL, Shirley D, et al. Parental multi-site chronic pain and the risk of adult offspring developing additional chronic pain sites: family-linkage data from the Norwegian HUNT Study. J Pain. 2020. [DOI] [PubMed] [Google Scholar]
- 53.Birnie KA, Heathcote LC, Bhandari RP, Feinstein A, Yoon IA, Simons LE. Parent physical and mental health contributions to interpersonal fear avoidance processes in pediatric chronic pain. Pain. in press;Articles in Press. [DOI] [PubMed] [Google Scholar]