Abstract
Background
MONARCH 3, a phase III trial (NCT02246621) of postmenopausal women with hormone receptor–positive (HR+), human epidermal growth factor receptor 2–negative (HER2−) advanced breast cancer (ABC), previously demonstrated significantly improved progression‐free survival in patients receiving abemaciclib plus a nonsteroidal aromatase inhibitor (NSAI). This study evaluated patient‐reported outcomes, including global health‐related quality of life (HRQoL), functioning, and symptoms.
Methods
Patients were randomly assigned 2:1 to receive abemaciclib (150 mg twice daily; n = 328) or placebo (n = 165), plus 1 mg anastrozole or 2.5 mg letrozole daily. The European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core 30 and Breast Cancer–Specific Quality of Life Questionnaire HRQoL instruments were administered at baseline, every two cycles during cycles 2 through 19 (each cycle being 28 days), every three cycles thereafter, and once at a short‐term posttherapy follow‐up visit (approximately 30 days after discontinuation). Longitudinal mixed regression and Cox proportional hazards models evaluated postbaseline change and time to sustained deterioration (TTSD), respectively.
Results
Baseline scores were similar between treatment arms. Although select scores statistically favored the placebo arm, global HRQoL, most symptoms, and functioning scales did not meet the threshold for clinically meaningful differences between treatment arms. Only diarrhea favored the placebo arm with statistically and clinically meaningful differences. There were no TTSD differences between treatment arms for global HRQoL, most symptoms (except diarrhea), or functioning.
Conclusion
Over a 2‐year period, there were no clinically meaningful differences in global HRQoL, functioning, and most symptoms for patients receiving abemaciclib plus NSAI compared with NSAI alone. Only diarrhea favored the placebo arm, consistent with prior safety data, which has been shown to be manageable and reversible. Combined with clinical efficacy, results support treatment with abemaciclib plus NSAI for postmenopausal women with HR+, HER2− ABC.
Implications for Practice
The addition of abemaciclib to a nonsteroidal aromatase inhibitor (NSAI) was not associated with a clinically meaningful detriment in patient‐reported global health‐related quality of life, functioning, and most symptoms in postmenopausal women with hormone receptor–positive (HR+), human epidermal growth factor receptor 2–negative (HER2−) advanced breast cancer (ABC). Prior studies have also demonstrated clinical efficacy of abemaciclib plus NSAI compared with NSAI alone, including improved progression‐free survival and objective response rate. These results also complement previously reported toxicity data, as measured by investigator‐assessed adverse events. Taken together, these results support treatment with abemaciclib plus NSAI for postmenopausal women with HR+, HER2− ABC.
Keywords: Abemaciclib, Advanced breast cancer, Cyclin‐dependent kinase 4/6 inhibitor, Health‐related quality of life, Patient‐reported outcomes
Short abstract
Previous reports have detailed the efficacy and toxicity of abemaciclib, but results detailing patient‐reported health‐related quality of life have not yet been published. This report assesses the effect of abemaciclib plus NSAI compared with placebo plus NSAI on patient‐reported global health‐related quality of life, functioning, and symptoms in postmenopausal women with HR+, HER2− advanced breast cancer in the phase III MONARCH 3 trial.
Introduction
Breast cancer, the most common cancer among women, had an estimated worldwide incidence of 2.1 million cases annually in 2018 [1]. The hormone receptor–positive (HR+), human epidermal growth factor receptor 2–negative (HER2−) subtype accounts for 73% of all breast cancer diagnoses [2]. Although early stage breast cancer has an excellent prognosis, treatments for HR+, HER2− advanced breast cancer (ABC) are palliative, and, historically, median overall survival (OS) with standard sequential single agent hormonal therapy and chemotherapy is only 2 to 3 years [3]. Nonsteroidal aromatase inhibitors (NSAIs), including letrozole and anastrozole, are a standard treatment for women with postmenopausal ABC [3]. Given the results of multiple phase III trials demonstrating improvements in progression‐free survival (PFS) and OS with the addition of cyclin‐dependent kinase (CDK) 4 and 6 inhibitors to standard endocrine therapy (ET), the National Comprehensive Cancer Network [4] and the European Society for Medical Oncology now recommend that ET be combined with CDK4 and CDK6 inhibitors for treatment of HR+, HER2− ABC [5].
Abemaciclib, a potent small‐molecule CDK4 and CDK6 inhibitor, is administered on a twice daily continuous schedule [6, 7, 8, 9]. In MONARCH 2, a phase III study of women with HR+, HER2− ABC that progressed on prior ET in either the adjuvant or first‐line metastatic setting, treatment with abemaciclib plus fulvestrant demonstrated a significant median OS improvement of 9.4 months (hazard ratio, 0.76; 95% confidence interval [CI], 0.61–0.95) compared with patients receiving placebo plus fulvestrant [10]. In MONARCH 3, among postmenopausal women treated with abemaciclib or placebo plus NSAI as initial therapy for HR+, HER2− ABC [11, 12], the addition of abemaciclib demonstrated statistically significant increases in investigator‐assessed PFS (hazard ratio, 0.54; 95% CI, 0.42–0.70; p < .001) [12]. Furthermore, in patients with measurable disease (80%), the objective response rate (ORR) was 61% among those in the abemaciclib arm versus 46% in the placebo arm (p = .003) [12]. The toxicity profile of abemaciclib in MONARCH 3, based on investigator‐assessed adverse events, has been previously reported, and abemaciclib plus NSAI demonstrated a tolerable safety profile [11, 12]. The most frequent adverse events in the abemaciclib arm were diarrhea, neutropenia, fatigue, and nausea [11].
Given the incurable nature of ABC, the impact on health‐related quality of life (HRQoL) is essential in guiding treatment decisions and should be considered alongside treatment efficacy [13, 14, 15, 16]. Although improving HRQoL is ideal, it may not be realistic, especially when adding a new treatment to an existing regimen [17]. Additional agents are likely to introduce new toxicities and may therefore worsen HRQoL. Thus, maintenance or restoration of HRQoL and minimization of treatment‐related toxicities combined with clinical efficacy are key objectives when adding a new treatment to an existing therapy [5, 17, 18]. In MONARCH 2, post hoc analyses demonstrated that patients in the abemaciclib arm (n = 446) experienced a significantly longer time to sustained deterioration (TTSD) on most patient‐reported symptoms, including pain, fatigue, nausea/vomiting, and functioning, including cognitive, physical, and social functioning, compared with patients in the placebo arm (n = 223) [19]. Only TTSD for diarrhea significantly favored the placebo arm (hazard ratio, 1.60; 95% CI, 1.20–2.10) [19].
Previous reports have detailed the efficacy and toxicity of abemaciclib [11, 12], but results detailing patient‐reported HRQoL have not yet been published. The objective of this report was to assess the impact of abemaciclib plus NSAI compared with placebo plus NSAI on patient‐reported global HRQoL, functioning, and symptoms in postmenopausal women with HR+, HER2− ABC in MONARCH 3.
Materials and Methods
Study Design and Treatment
A detailed study design has been previously reported [11, 12]. Data included here are from the final PFS cutoff, November 3, 2017. Briefly, MONARCH 3 was a phase III, randomized, double‐blind, placebo‐controlled trial of abemaciclib or placebo plus NSAI as initial therapy in the advanced setting in postmenopausal women with HR+, HER2− ABC. Patients were randomized 2:1 to receive either 150 mg twice daily abemaciclib or matching placebo, plus either 1 mg anastrozole or 2.5 mg letrozole per physician's choice. Treatment continued until disease progression, unacceptable toxicity, death, or patient withdrawal for any reason. Prior to enrollment, all patients provided informed consent. MONARCH 3 received all necessary ethical and institutional review board approvals. The trial was conducted in accordance with the Declaration of Helsinki and was overseen by a steering committing. An independent data monitoring committee evaluated safety data quarterly.
Patient‐Reported Outcomes and Quality of Life Measures
Patient‐reported outcomes (PROs) were assessed at baseline, every two cycles during cycles 2 through 19, then every three cycles thereafter, and once at a short‐term follow‐up visit, approximately 30 days after discontinuation using the European Organization for Research and Treatment of Cancer (EORTC) Quality of Life Questionnaire Core 30 (QLQ‐C30) [20] and Breast Cancer Questionnaire (BR23) [21].
The EORTC QLQ‐C30 evaluated global HRQoL, five functional scales (physical, role, emotional, cognitive, and social), three symptom scales (fatigue, nausea/vomiting, and pain), and a number of single‐item assessments of additional symptoms commonly reported by patients with cancer (dyspnea, insomnia appetite loss, constipation, diarrhea, and financial impact) [20]. Specific items used to create the above scales are detailed in supplemental online Table 1, and all scores were calculated based on EORTC guidelines [20]. Symptom items were scored on a four‐point response scale; higher scores indicated greater symptom burden. Functioning items were also scored on a four‐point response scale; higher scores indicated better functioning. Global HRQoL was scored on a scale of 1 to 7 (higher scores indicated better global HRQoL). Symptoms and functions measured in the EORTC QLQ‐C30 were correlated with treatment toxicity when it was developed and validated [20].
The BR23 assessed additional disease‐specific symptoms and functions shown to be relevant among patients with breast cancer [21]. It was designed to include items that assess symptoms, functions, and side effects commonly related to different treatment modalities, including surgery, chemotherapy, radiotherapy, and hormonal treatment [21]. Functioning (body image, sexuality, and future perspective) and symptom scales (arm symptoms, breast symptoms, upset by hair loss, and systemic therapy side effects) were collected. Similar to the QLQ‐C30 items, symptom items were scored on four‐point scale with higher scores indicating greater symptom burden; functioning items were also scored on a four‐point scale, but higher scores indicated higher functioning.
Statistical Analysis
Questionnaire compliance was measured as the number of on‐treatment patients completing each instrument per cycle divided by the number of patients expected to contribute data at each visit. Reasons for noncompliance were recorded and included “missing” (i.e., patient compliance data were missing, but no reason was recorded), “study site failed to administer questionnaire,” and “patient refusal.”
All analyses were performed using the safety population. Mixed effects repeated measures models assessed between treatment arm differences in change from baseline for each item of the QLQ‐C30 and BR23 by cycle. All models controlled for baseline scores and included all data/cycles for which at least 25% of patients in each arm had an assessment. For all EORTC scores, a clinically meaningful difference (deterioration or improvement) in symptom, function, or global HRQoL was defined as a 10‐point difference compared with a patient's baseline score based on a previously established threshold [22, 23].
Post hoc analyses investigated TTSD with Cox proportional hazards models. TTSD was defined as time from randomization to the time of a ≥10‐point deterioration, consistent with previously established thresholds [22, 23], compared with a patient's baseline score, followed by all subsequent scores meeting this clinically meaningful change criterion compared with baseline or death, whichever occurred first. TTSD outcomes capture the full course of treatment [24] and allow for a brief worsening of symptoms followed by an improvement in an attempt to differentiate between a transient worsening of outcomes and a sustained decline in health status. For all analyses, no adjustments for multiple comparisons were made and p values indicating statistical significance were a priori set at ≤.05. All analyses were conducted using SAS version 9.2 or later.
Results
Patients and Disease Characteristics
A total of 493 patients were randomly assigned to receive either abemaciclib plus NSAI (n = 328) or placebo plus NSAI (n = 165; Fig. 1) [11]. At baseline, patient and disease characteristics previously described in detail were well balanced [11]. Briefly, 56.7% of patients in the abemaciclib arm were white, 31.4% Asian, 1.5% black, and 1.8% self‐reported as other race; in the placebo arm, 61.8% were white, 27.3% Asian, 1.8% black, and 2.4% self‐reported as other race. The median age of patients in the abemaciclib arm was 63 years (range: 38–87 years), and age in the placebo arm was similar (median, 63 years, range: 32–88 years). In the abemaciclib arm, 52.4% of patients had visceral metastatic sites, 21.3% had bone only, and 26.2% other; this is compared with 53.9% in the placebo arm with visceral metastatic sites, 23.6% with bone only, and 22.4% with other [11].
Figure 1.
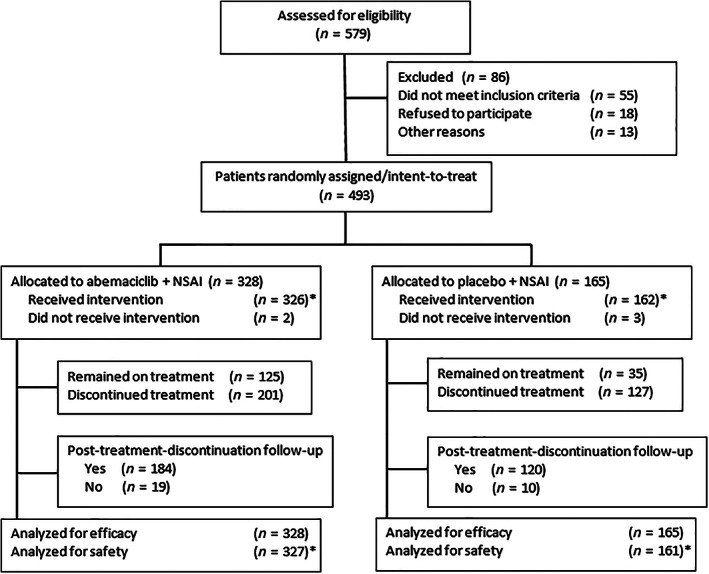
CONSORT diagram.
*, One patient who was randomly assigned to the placebo arm actually received abemaciclib during cycle 1. This patient is counted in the abemaciclib safety population.
Abbreviation: NSAI, nonsteroidal aromatase inhibitor.
Patient‐Reported Outcomes
Compliance
In the abemaciclib arm, patient compliance rates for both questionnaires were ≥96% at baseline, ≥88% for the duration of abemaciclib treatment, and ≥70% at the follow‐up visit after discontinuation (supplemental online Table 2). Nonresponse was balanced between study arms and across questionnaires. The most common reasons for noncompliance across all study visits was “study site failed to administer” (supplemental online Table 1).
Change from Baseline
At baseline, the EORTC QLQ‐C30 global health status score and the functional and symptom scores from the QLQ‐C30 and the BR23 were similar between study arms (Table 1). Baseline scores were comparable to established reference values for patients with ABC (Table 1) [25]. Similarly, baseline scores in the MONARCH 3 population were comparable to average scores from two normative populations: (a) a female population from 13 European Union countries, aged 18 to >70 years, and (b) a male and female population from the U.S. with the same age ranges (Table 1) [26].
Table 1.
Baseline mean scores by treatment arm and within‐treatment group change from baseline for the European Organization for Research and Treatment of Cancer QLQ‐C30 and BR23, and normative scores (range for all scales: 0 to 100)
| Baseline score, mean ± SD | Change from baseline, a LS mean ± SE | Baseline reference values, mean ± SD | |||||
|---|---|---|---|---|---|---|---|
| Abemaciclib b | Placebo b | Abemaciclib b | Placebo b | MBC population c | General population d | General population e | |
| Global health status | 65.0 ± 21.7 | 58.9 ± 22.5 | 0.0 ± 0.8 | 4.3 ± 1.2 | 60.2 ± 25.5 | 64.3 ± 21.8 | 63.9 ± 22.9 |
| QLQ‐C30 functional scales f | |||||||
| Physical | 76.4 ± 20.1 | 73.2 ± 21.9 | −1.0 ± 0.9 | 1.7 ± 1.2 | 81.6 ± 18.7 | 84.3 ± 18.5 | 80.8 ± 25.2 |
| Role | 76.8 ± 27.8 | 71.5 ± 29.3 | −1.4 ± 1.1 | 2.9 ± 1.6 | 67.4 ± 31.1 | 84.1 ± 24.6 | 81.7 ± 28.2 |
| Emotional | 71.1 ± 23.3 | 69.4 ± 23.2 | 4.7 ± 0.9 | 4.0 ± 1.3 | 65.9 ± 24.6 | 71.9 ± 25.3 | 73.3 ± 28.0 |
| Cognitive | 85.3 ± 18.5 | 86.1 ± 19.0 | −4.0 ± 0.9 | −4.0 ± 1.3 | 80.5 ± 23.2 | 84.3 ± 20.9 | 80.9 ± 25.6 |
| Social | 81.3 ± 24.5 | 78.1 ± 27.8 | −0.1 ± 1.0 | 3.3 ± 1.4 | 74.2 ± 28.4 | 85.7 ± 24.6 | 81.6 ± 29.4 |
| QLQ‐C30 symptom scales f | |||||||
| Fatigue | 32.2 ± 22.8 | 38.3 ± 25.6 | 2.4 ± 1.0 | −2.6 ± 1.4 | 36.3 ± 27.0 | 31.7 ± 25.9 | 31.9 ± 27.8 |
| Nausea and vomiting | 7.2 ± 15.7 | 8.1 ± 18.3 | 2.4 ± 0.6 | −0.4 ± 0.9 | 10.3 ± 19.7 | 5.7 ± 14.9 | 10.9 ± 22.6 |
| Pain | 28.7 ± 26.3 | 36.3 ± 30.2 | −4.8 ± 1.0 | −5.7 ± 1.5 | 30.9 ± 29.6 | 25.3 ± 27.9 | 27.5 ± 30.2 |
| Dyspnea | 19.4 ± 25.4 | 21.9 ± 30.0 | 0.9 ± 1.0 | −1.6 ± 1.4 | 20.4 ± 28.2 | 16.3 ± 24.5 | 19.9 ± 28.5 |
| Insomnia | 26.2 ± 26.9 | 32.9 ± 31.1 | −1.7 ± 1.2 | −4.1 ± 1.7 | 33.1 ± 32.6 | 29.3 ± 30.7 | 30.8 ± 33.2 |
| Appetite loss | 17.9 ± 25.5 | 22.4 ± 28.3 | 0.2 ± 1.1 | −3.9 ± 1.6 | 21.7 ± 31.0 | 10.3 ± 21.6 | 14.1 ± 25.3 |
| Constipation | 13.2 ± 22.1 | 13.6 ± 24.5 | −0.8 ± 0.9 | 1.6 ± 1.3 | 19.2 ± 28.8 | 14.1 ± 24.4 | 18.6 ± 28.6 |
| Diarrhea | 8.3 ± 18.5 | 7.3 ± 15.9 | 18.2 ± 1.0 | −0.5 ± 1.5 | 5.8 ± 15.2 | 9.0 ± 20.3 | 13.7 ± 27.1 |
| Financial difficulties | 16.4 ± 26.4 | 18.0 ± 29.2 | −0.7 ± 1.1 | −1.2 ± 1.6 | 18.6 ± 28.6 | 10.9 ± 24.2 | 17.5 ± 30.8 |
| BR23 functional scales f , g | |||||||
| Body image | 81.6 ± 21.4 | 79.8 ± 26.1 | −4.5 ± 1.1 | 0.6 ± 1.6 | 81.9 ± 22.6 | N/A | N/A |
| Sexual functioning | 10.2 ± 17.3 | 7.7 ± 15.7 | −0.2 ± 0.7 | −0.1 ± 1.0 | 19.2 ± 23.2 | N/A | N/A |
| Future perspective | 42.5 ± 32.2 | 41.5 ± 32.8 | 12.7 ± 1.3 | 11.9 ± 1.9 | 47.6 ± 34.1 | N/A | N/A |
| Symptom scales f , g | |||||||
| Systemic therapy side effects | 15.8 ± 13.1 | 18.1 ± 13.5 | 8.3 ± 0.7 | 3.7 ± 1.0 | 15.8 ± 14.3 | N/A | N/A |
| Breast symptoms | 17.9 ± 19.7 | 14.8 ± 17.3 | −6.1 ± 0.7 | −6.1 ± 1.0 | 17.6 ± 16.7 | N/A | N/A |
| Arm symptoms | 21.0 ± 24.7 | 23.5 ± 22.1 | −1.8 ± 0.9 | −2.2 ± 1.3 | 21.0 ± 21.1 | N/A | N/A |
Abbreviations: BR23, Breast Cancer–Specific Quality of Life Questionnaire; LS, least squares; MBC, metastatic breast cancer; N/A, not applicable; QLQ‐C30, Quality of Life Questionnaire Core 30.
Across all postbaseline visits.
Both arms were also treated with a nonsteroidal aromatase inhibitor.
Reference baseline values for patients with recurrent/metastatic breast cancer across all lines of treatment [25].
Reference baseline values for general female population normative data, aged 18 to ≥70, for 11 European Union countries weighted by age, sex, and country, according to the United Nations Department of Economic and Social Affair population distribution statistics for the year 2015 [26].
Reference baseline values for general population (male and female) normative data, aged 18 to ≥70, for the U.S. weighted by individual country weights and sex and age distributions, according to the United Nations Department of Economic and Social Affair population distribution statistics for the year 2015 [26].
For symptoms, higher scores indicate greater symptom burden. For functioning, higher scores indicate better function.
Sexual enjoyment (functional scale) and upset by hair loss (symptom scale) were not analyzed because of small sample size.
There were no clinically meaningful (≥10 points) between treatment differences in change from baseline scores for the majority of symptom scores (except diarrhea) and any functioning scores for the EORTC QLQ‐C30 or BR23 (Figs. 2 and 3). Some QLQ‐C30 and BR23 symptoms statistically favored the placebo arm: fatigue (between treatment group difference ± SE, 4.96 ± 1.72; p = .004), nausea/vomiting (2.77 ± 1.12; p = .01), appetite loss (4.03 ± 1.89; p = .03), body image (−5.11 ± 1.95; p = .01), and systemic therapy side effects (4.48 ± 1.20; p < .001; Figs. 2 and 3). The same was true for global HRQoL (−4.36 ± 1.45; p = .003) and role functioning (−4.25 ± 1.90; p = .03). None of these differences met the ≥10‐point predefined criteria indicating clinically meaningful declines.
Figure 2.
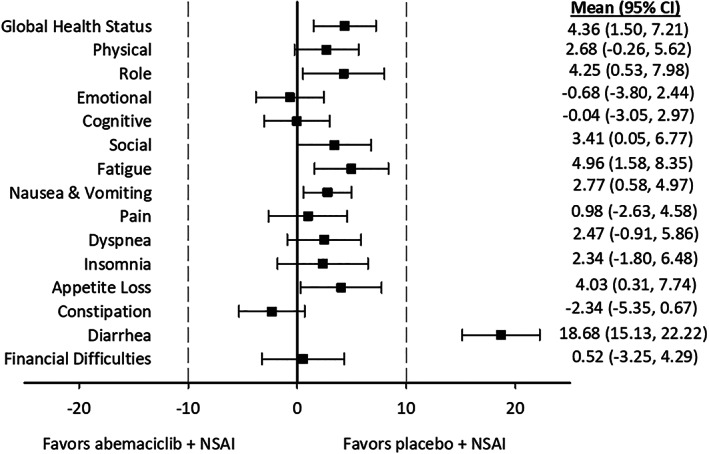
Forest plot of mean differences, obtained with longitudinal mixed regression models, between study arms in change from baseline scores for the European Organization for Research and Treatment of Cancer Quality of Life Core 30. Higher scores on symptoms indicated greater symptom burden or worsening, and higher scores for global health status and functioning items indicated better function or improvement. Given this discrepancy, the sign for scores for the global health status and functioning items were reversed for this figure to be consistent with the symptom scores.
Abbreviations: CI, confidence interval; NSAI, nonsteroidal aromatase inhibitor.
Figure 3.
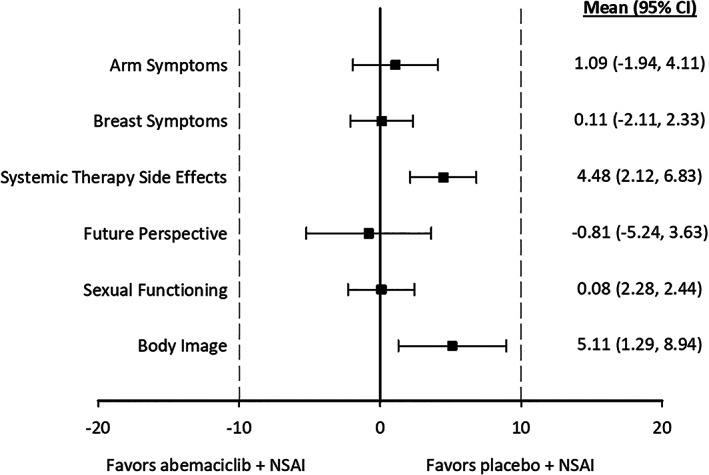
Forest plot of mean differences, obtained with longitudinal mixed regression models, between study arms in change from baseline scores for the Breast Cancer Questionnaire. Higher scores on symptoms indicated greater symptom burden or worsening, and higher scores for functioning items indicated better function or improvement. Given this discrepancy, the sign for scores of functioning items were reversed for this figure to be consistent with the symptom scores.
Abbreviations: CI, confidence interval; NSAI, nonsteroidal aromatase inhibitor.
The only symptom for which there was both a statistically significant and clinically meaningful (≥10 points) difference favoring the placebo arm was diarrhea (18.68 ± 1.80; p < .001; Fig. 2). Importantly, patient‐reported diarrhea was greatest during early study visits, peaking at cycle 3 and subsequently decreasing over time (Fig. 4). There was a similar trend for investigator‐assessed diarrhea adverse events, with the greatest incidence of any grade diarrhea and grade 3 diarrhea occurring in the first three cycles, and following antidiarrheal treatment and/or dose adjustments, incidence was lower later in treatment (supplemental online Fig. 1) [27].
Figure 4.
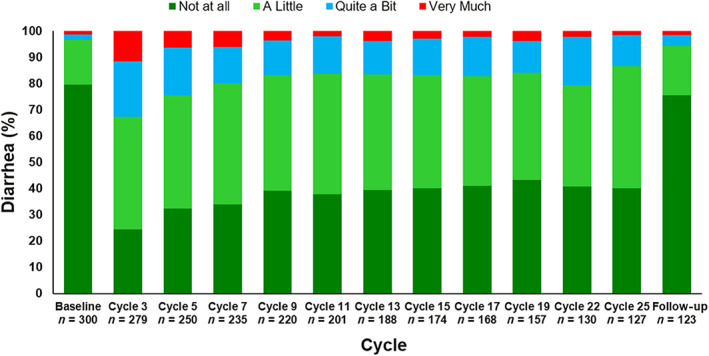
Patient‐reported diarrhea, as measured by the European Organization for Research and Treatment of Cancer, by cycle among patients taking abemaciclib plus a nonsteroidal aromatase inhibitor.
Time to Sustained Deterioration
When investigating TTSD on the QLQ‐C30 (Fig. 5) and BR23 (Fig. 6), there were no statistically significant or clinically meaningful differences between treatment arms for global HRQoL, most symptoms, or any functional items. Diarrhea was the only symptom that clinically and statistically favored the placebo arm (hazard ratio, 1.74; 95% CI, 1.25–2.40; Fig. 5).
Figure 5.
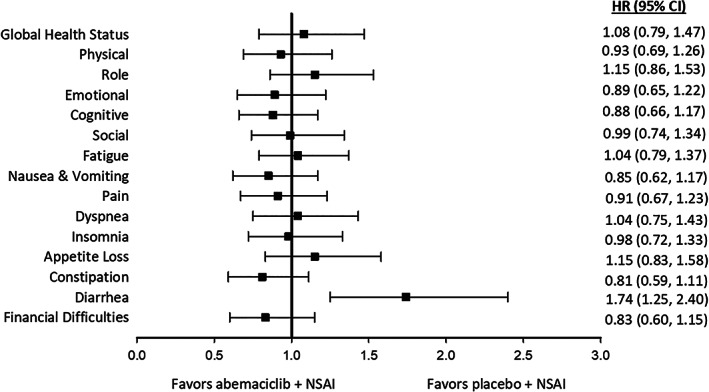
Forest plot of time to sustained deterioration of European Organization for Research and Treatment of Cancer Quality of Life Core 30 global health, symptoms, and functioning items.
Abbreviations: CI, confidence interval; HR, hazard ratio; NSAI, nonsteroidal aromatase inhibitor.
Figure 6.
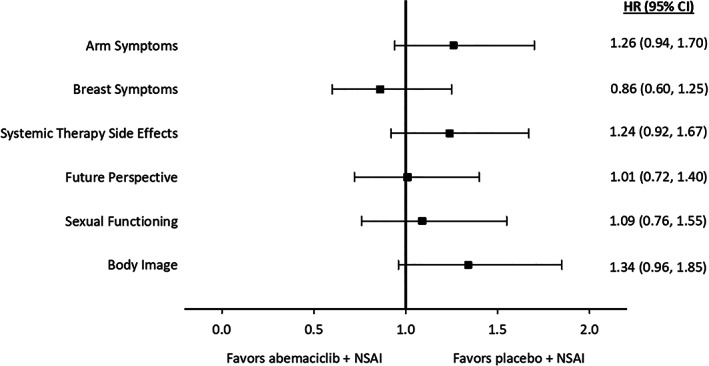
Forest plot of time to sustained deterioration of the Breast Cancer Questionnaire symptoms and functioning items.
Abbreviations: CI, confidence interval; HR, hazard ratio; NSAI, nonsteroidal aromatase inhibitor.
Discussion
Given the palliative nature of metastatic breast cancer combined with relatively long OS and PFS, patients with ABC will likely undergo multiple lines of sequential regimens including the addition of new therapies, which may introduce new treatment‐related toxicities that could negatively affect HRQoL [17]. Thus, minimizing treatment impact on HRQoL, symptoms, and functioning is a key objective when adding a new treatment to an existing regimen [5, 17, 18], and PROs should be monitored closely alongside treatment efficacy [13, 14, 16]. In MONARCH 3, patient‐reported global HRQoL, most symptoms (except diarrhea), and functioning scales did not show clinically meaningful differences in the abemaciclib plus NSAI arm compared with NSAI alone. Furthermore, patients in the abemaciclib arm did not have statistically significant or clinically meaningful differences in TTSD (except diarrhea) compared with the placebo arm.
The exception to these results was diarrhea, as patients in the abemaciclib arm experienced both a clinically meaningful and statistically significant worsening from baseline and a shorter TTSD compared with patients in the placebo arm. These results are not surprising given previously disclosed safety data from MONARCH 3 and other abemaciclib trials that have shown diarrhea to be the most commonly reported adverse event [6, 8, 9, 10, 11, 12]. Although there was an overall increase in diarrhea in patients taking abemaciclib, it was predominantly low grade with 72.8% of all cases in the abemaciclib arm being grade 1 or grade 2 and no cases of grade 4 diarrhea [12]. The median onset for diarrhea was 8 days in the abemaciclib arm, and the median duration was 10.5 days for grade 2 and 8 days for grade 3. As shown in Figure 4 and supplemental online Figure 1, incidence of both patient‐reported diarrhea symptoms and investigator‐assessed diarrhea adverse events was highest by cycle 3 and was lower in subsequent cycles. Diarrhea did not frequently result in abemaciclib discontinuation (1.8%) [12]. There is clear evidence that when abemaciclib‐related diarrhea is treated at the first loose stool with over‐the‐counter antidiarrheal medication and/or dose modifications, it resolves over time with no impact on efficacy and returns to baseline levels after discontinuation [27].
MONARCH 2 post hoc analyses demonstrated patients in the abemaciclib arm experienced a significantly longer TTSD on most patient‐reported symptom and functioning scores compared with patients in the placebo arm [19]. These results differ from MONARCH 2 in that there were no differences in PROs statistically favoring the abemaciclib arm; this may be explained, at least in part, by later line of therapy, shorter PFS in MONARCH 2, different endocrine partners, and/or different study population characteristics [19].
This study has several strengths and limitations to consider. A strength of this study is the use of the EORTC QLQ‐C30 [20]. Broadly used in cancer trials as a well‐validated and reliable tool, the QLQ‐C30 has supported HRQoL claims in both U.S. Food and Drug Administration and European Medicines Evaluation Agency labels [20]. Additionally, it assesses global health status and a multitude of symptoms and functions, making it a well‐rounded tool to characterize the patient experience. Previous studies have shown that pain, fatigue, and overall HRQoL have ranked as very important issues to patients while receiving treatment [28, 29, 30], which were all assessed and described here. Furthermore, physical and social function have been reported as important functioning items from a patient perspective while receiving cancer treatment [29]. In MONARCH 3, physical, social, and cognitive function did not show statistically significant and clinically meaningful worsening among patients taking abemaciclib plus NSAI compared with NSAI alone. High compliance rates during the study, including the follow‐up after discontinuation, are another strength. The use of a sustained definition for the time to event analyses is considered a strength as it differs from time to first deterioration, which only considers the initial worsening of a symptom and may not reflect the patient's full experience on therapy. For example, the TTSD approach allows for a brief worsening of symptoms immediately after adding a treatment and subsequent improvement, which is useful when adding an additional treatment to an existing regimen. However, TTSD analyses are also limited in the potential for an imbalance in study arms in the number of potential assessment points, as data collection is stopped at the time of disease progression. Longitudinal analytic techniques for HRQoL are evolving, and future studies should continue to evaluate the optimal approach for palliative treatment settings. Although the EORTC QLQ‐C30 and BR23 include items to measure symptoms associated with drug toxicity (such as diarrhea, fatigue, and nausea/vomiting), these are primarily intended to characterize the patient experience during treatment as part of a holistic assessment of HRQoL rather than investigator‐assessed treatment‐related adverse events. It is possible that all symptoms experienced by patients were not captured by these instruments. Although selected symptom and functional item scores generated in the EORTC QLQ‐C30 were shown to be correlated with treatment toxicity during the development and validation of the instrument [20], future oncology trials may benefit from use of fit‐for‐purpose instruments, such as the National Institutes of Health–National Cancer Institute PRO–Common Terminology Criteria for Adverse Events that measures patient‐felt toxicities at frequent intervals to directly inform the assessment of safety/tolerability. Another limitation is data cannot be assumed to be missing at random since it is likely that patients who were more ill had lower compliance. However, high compliance percentages among those on‐treatment across all study visits minimizes the impact of this limitation to the greatest extent possible. PROs were not collected at every study cycle, and, thus, health‐state changes could have occurred between assessments. Conclusions are limited to the treatment period, as PROs were not assessed after the 30‐day visit after discontinuation. Finally, there was no adjustment for multiplicity; thus, there is potential inflation of type I error.
Conclusion
In MONARCH 3, the assessment of PROs across a 2‐year treatment period in patients with HR+, HER2− ABC indicated that, although select scores statistically favored the placebo arm, most symptoms and functioning scales did not meet the threshold for clinically meaningful differences among those receiving abemaciclib plus NSAI as initial endocrine‐based therapy compared with NSAI alone. Diarrhea was the only patient‐reported symptom with a clinically meaningful and statistically significant negative impact from abemaciclib treatment, but these data were consistent with previous safety reports indicating that it was well managed, reached its maximum frequency and severity in early cycles, and subsequently reduced over the treatment period. Taken alongside prior efficacy results demonstrating superior PFS and ORR in patients taking abemaciclib plus NSAI compared with NSAI alone [11, 12] and prior reports of abemaciclib toxicity profiles in the abemaciclib and placebo arms [11, 12, 27], this study further supports treatment with abemaciclib plus either letrozole or anastrozole for postmenopausal women with HR+, HER2− ABC.
Author Contributions
Conception/design: Matthew P. Goetz, Masakazu Toi, Clemens Stoffregen, Sarah Shekarriz, Valerie Andre, M. Corona Gainford, Gregory L. Price
Provision of study material or patients: Matthew P. Goetz, Miguel Martin, Eriko Tokunaga, In Hae Park, Jens Huober, Masakazu Toi, Clemens Stoffregen, Sarah Shekarriz, Valerie Andre, M. Corona Gainford, Gregory L. Price, Stephen Johnston
Collection and/or assembly of data: Matthew P. Goetz, Miguel Martin, Eriko Tokunaga, In Hae Park, Jens Huober, Masakazu Toi, Clemens Stoffregen, Sarah Shekarriz, Valerie Andre, M. Corona Gainford, Gregory L. Price, Stephen Johnston
Data analysis and interpretation: Matthew P. Goetz, Miguel Martin, Eriko Tokunaga, In Hae Park, Jens Huober, Masakazu Toi, Clemens Stoffregen, Sarah Shekarriz, Valerie Andre, M. Corona Gainford, Gregory L. Price, Stephen Johnston
Manuscript writing: Matthew P. Goetz, Miguel Martin, Eriko Tokunaga, In Hae Park, Jens Huober, Masakazu Toi, Clemens Stoffregen, Sarah Shekarriz, Valerie Andre, M. Corona Gainford, Gregory L. Price, Stephen Johnston
Final approval of manuscript: Matthew P. Goetz, Miguel Martin, Eriko Tokunaga, In Hae Park, Jens Huober, Masakazu Toi, Clemens Stoffregen, Sarah Shekarriz, Valerie Andre, M. Corona Gainford, Gregory L. Price, Stephen Johnston
Disclosures
Matthew P. Goetz: Eli Lilly & Co., Biovica, Novartis, Sermonix, Context Pharm, Pfizer (C/A, RF [institutional]); Miguel Martin: Roche, Puma, Novartis (RF), AstraZeneca, Amgen, Taiho Oncology, Roche/Genentech, Novartis, PharmaMar, Eli Lilly & Co., Puma, Daiichi Sankyo, Pfizer (C/A), AstraZeneca, Amgen, Roche/Genentech, Novartis, Pfizer (H); Eriko Tokunaga: Eli Lilly & Co., Chugai, AstraZeneca (IP), Eli Lilly & Co. (SAB); Jens Huober: Celgene, Novartis, Hexal (RF), Eli Lilly & Co., Novartis, Roche, Pfizer, AstraZeneca, Merck Sharp Dohme, Celgene, Eisai, Abbvie (C/A), Lilly, Novartis, Roche, Pfizer, Hexal, AstraZeneca, Merck Sharp Dohme, Celgene, Abbvie (H), Roche, Pfizer, Novartis, Celgene, Daiichi (other); Masakazu Toi: Taiho, Chugai, Shimadzu, Pfizer, Eisai, Daiichi‐Sankyo, AstraZeneca, Ono, Japan Breast Cancer Research Group Association, NipponKayaku, Kyoto Breast Cancer Research Network, Astellas, AFI Technology (RF), Novartis, Takeda, AstraZeneca, Eisai, Genomic Health, Taiho, Devicore Medical Japan, Chugai, Konica Minolta, Eli Lilly & Co., Kyowa‐Kirin, Shimadzu, Pfizer, Yakult, Daiichi‐Sankyo, Nippon Kayaku (ET, H), Kyowa‐Kirin, Daiichi‐Sankyo, Konica‐Minolta (SAB); Clemens Stoffregen: Eli Lilly & Co. (E, OI); Sarah Shekarriz: Eli Lilly & Co. (E); Valerie Andre: Eli Lilly & Co. (E, OI); M. Corona Gainford: Eli Lilly & Co. (E, OI); Gregory L. Price: Eli Lilly & Co. (E, OI); Stephen Johnston: Novartis, Pfizer, Eli Lilly & Co., Puma Biotechnology (C/A), Eisai, AstraZeneca, Eli Lilly & Co., Novartis, Pfizer, Roche (H), Pfizer, Puma Biotechnology, Eli Lilly & Co., AstraZeneca, Novartis, Roche/Genentech (RF—institution). In Hae Park indicated no financial relationships.
(C/A) Consulting/advisory relationship; (RF) Research funding; (E) Employment; (ET) Expert testimony; (H) Honoraria received; (OI) Ownership interests; (IP) Intellectual property rights/inventor/patent holder; (SAB) Scientific advisory board
Supporting information
See http://www.TheOncologist.com for supplemental material available online.
Appendix S1. Supporting Information.
Appendix S2. Supporting Information.
Acknowledgments
We thank all the patients, their families, the study sites, and the study personnel who participated in this study. This research was sponsored by Eli Lilly & Co. Eli Lilly & Co. contracted with Syneos Health for production assistance and editing support from Andrea Metti, Ph.D., M.P.H.; Dana Schamberger, M.A.; and Cynthia Abbott.
Disclosures of potential conflicts of interest may be found at the end of this article.
No part of this article may be reproduced, stored, or transmitted in any form or for any means without the prior permission in writing from the copyright holder. For information on purchasing reprints contact Commercialreprints@wiley.com. For permission information contact permissions@wiley.com.
References
- 1. Bray F, Ferlay J, Soerjomataram I et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394–424. [DOI] [PubMed] [Google Scholar]
- 2. Howlader N, Altekruse SF, Li CI et al. US incidence of breast cancer subtypes defined by joint hormone receptor and HER2 status. J Natl Cancer Inst 2014;106:dju055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cardoso F, Costa A, Senkus E et al. 3rd ESO‐ESMO International Consensus Guidelines for advanced breast cancer (ABC 3). Ann Oncol 2017;28:16–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gradishar W, Salemo KE. NCCN guidelines update: Breast cancer. J Natl Compr Canc Netw 2016;14(suppl 5):641–644. [DOI] [PubMed] [Google Scholar]
- 5. Cardoso F, Senkus E, Costa A et al. 4th ESO‐ESMO International Consensus Guidelines for advanced breast cancer (ABC 4). Ann Oncol 2018;29:1634–1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dickler MN, Tolaney SM, Rugo HS et al. MONARCH 1, a phase II study of abemaciclib, a CDK4 and CDK6 inhibitor, as a single agent, in patients with refractory HR(+)/HER2(‐) metastatic breast cancer. Clin Cancer Res 2017;23:5218–5224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gelbert LM, Cai S, Lin X et al. Preclinical characterization of the CDK4/6 inhibitor LY2835219: In‐vivo cell cycle‐dependent/independent anti‐tumor activities alone/in combination with gemcitabine. Invest New Drugs 2014;32:825–837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Patnaik A, Rosen LS, Tolaney SM et al. Efficacy and safety of abemaciclib, an inhibitor of CDK4 and CDK6, for patients with breast cancer, non‐small cell lung cancer, and other solid tumors. Cancer Discov 2016;6:740–753. [DOI] [PubMed] [Google Scholar]
- 9. Sledge GW Jr, Toi M, Neven P et al. MONARCH 2: Abemaciclib in combination with fulvestrant in women with HR+/HER2‐ advanced breast cancer who had progressed while receiving endocrine therapy. J Clin Oncol 2017;35:2875–2884. [DOI] [PubMed] [Google Scholar]
- 10. Sledge GW Jr, Toi M, Neven P et al. The effect of abemaciclib plus fulvestrant on overall survival in hormone receptor‐positive, ERBB2‐negative breast cancer that progressed on endocrine therapy ‐ MONARCH 2: A randomized clinical trial. JAMA Oncol 2019;6:116–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Goetz MP, Toi M, Campone M et al. MONARCH 3: Abemaciclib as initial therapy for advanced breast cancer. J Clin Oncol 2017;35:3638–3646. [DOI] [PubMed] [Google Scholar]
- 12. Johnston S, Martin M, DiLeo A et al. MONARCH 3 final PFS: A randomized study of abemaciclib as initial therapy for advanced breast cancer. NPJ Breast Cancer 2019;5:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fallowfield LJ. Quality of life assessment using patient‐reported outcome (PRO) measures: Still a Cinderella outcome? Ann Oncol 2018;29:2286–2287. [DOI] [PubMed] [Google Scholar]
- 14. Gerber B, Freund M, Reimer T. Recurrent breat cancer: Treatment strategies for maintaining and prolonging good quality of life. Dtsch Arztebl Int 2010;107:85–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lemay K, Wilson KG, Buenger U et al. Fear of pain in patients with advanced cancer or in patients with chronic noncancer pain. Clin J Pain 2011;27:116–124. [DOI] [PubMed] [Google Scholar]
- 16. Marandino L, La Salvia A, Sonetto C et al. Deficiencies in health‐related quality‐of‐life assessment and reporting: A systematic review of oncology randomized phase III trials published between 2012 and 2016. Ann Oncol 2018;29:2288–2295. [DOI] [PubMed] [Google Scholar]
- 17. Niraula S, Seruga B, Ocana A et al. The price we pay for progress: A meta‐analysis of harms of newly approved anticancer drugs. J Clin Oncol 2012;30:3012–3019. [DOI] [PubMed] [Google Scholar]
- 18. Rugo HS, Dieras V, Gelmon KA et al. Impact of palbociclib plus letrozole on patient‐reported health‐related quality of life: Results from the PALOMA‐2 trial. Ann Oncol 2018;29:888–894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kaufman PA, Toi M, Neven P et al. Health‐related quality of life in MONARCH 2: Abemaciclib plus fulvestrant in hormone receptor‐positive, HER2‐negative advanced breast cancer after endocrine therapy. The Oncologist 2020;25:e243–e251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Aaronson NK, Ahmedzai S, Bergman B et al. The European Organisation for Research and Treatment of Cancer QLQ‐C30: A quality‐of life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 1993;85:365–376. [DOI] [PubMed] [Google Scholar]
- 21. Sprangers MAG, Groenvold M, Arraras JL et al. The European Organization for Research and Treatment of Cancer breast cancer‐specific quality‐of‐life questionnaire module: First results from a three‐country field study. J Clin Oncol 1996;14:2756–2768. [DOI] [PubMed] [Google Scholar]
- 22. Osoba D, Rodrigues G, Myles J et al. Interpreting the significnace of changes in health‐related quality‐of‐life scores. J Clin Oncol 1998;16:139–144. [DOI] [PubMed] [Google Scholar]
- 23. Harbeck N, Iyer S, Turner N et al. Quality of life with plabociclib plus fulvestrant in previously treated hormone receptor‐positive, her2‐negative metastatic breast cancer: Patient‐reported outcomes from the paloma‐3 trial. Ann Oncol 2016;27:1047–1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Anota A, Hamidou Z, Paget‐Bailly S et al. Time to health‐related quality of life score deterioration as a modality of longitudinal analysis for health‐related quality of life studies in oncology: Do we need RECIST for quality of life to acheive standardization? Qual Life Res 2015;24:5–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Scott NW, Fayers PM, Aaronson NK et al. EORTC QLQ‐C30 Reference Values. Brussels, Belgium: European Organisation for Research and Treatment of Cancer, 2008. [Google Scholar]
- 26. Nolet S, Liegl G, Petersen MA et al. General population normative data for the EORTC QLQ‐C30 health‐related quality of life questionnaire based on 15,386 persons across 13 European countries, Canada and the United States. Eur J Cancer 2019;107:153–163. [DOI] [PubMed] [Google Scholar]
- 27. Rugo HS, Sledge GW, Johnston SRD et al. The association of early toxicity and outcomes for patients treated with abemaciclib. J Clin Oncol 2018;36(suppl 15):1053a. [Google Scholar]
- 28. Hollen PJ, Masaouel P, Gralla RJ. Determining issues of importance for the evaluation of quality of life and patient‐reported outcomes in breast cancer: Results of a survey of 1072 patients. Breast Cancer Res Treat 2015;151:679–686. [DOI] [PubMed] [Google Scholar]
- 29. Hofheinz R, Cluth J, Borchardt‐Wagner J et al. Patient preferences for palliative treatment of locally advanced or metastatic breast cancer: An adaptive choice‐based conjoint analysis study from Germany. BMC Cancer 2016;16:937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Reinisch M, Marschner N, Otto T et al. Patient preferences: Results of a German adaptive choice‐based conjoint analysis study in patients on palliative treatment for advanced breast cancer (aBC). Cancer Res 2020;80(suppl 4):P1‐17‐08a. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
See http://www.TheOncologist.com for supplemental material available online.
Appendix S1. Supporting Information.
Appendix S2. Supporting Information.


