Abstract
Lessons Learned
The findings from this study using monotherapy with pemetrexed in a pretreated patient population are, overall, encouraging.
Unlike high‐dose methotrexate, which requires several days of inpatient hospitalization, pemetrexed is relatively easy to administer in the outpatient setting and remains a viable treatment option in this patient population.
The maximum tolerated dose of pemetrexed administered (900 mg/m2 every 2 weeks) was generally well tolerated and showed activity in patients with relapsed or refractory CNSL.
Background
There is currently no standard salvage treatment for patients with relapsed/refractory central nervous system (CNS) lymphoma (CNSL). We report the results of a phase I study of pemetrexed, an antifolate drug with broader activity than methotrexate (MTX). We provide the safety, tolerability, and maximum tolerated dose (MTD) of pemetrexed in patients with recurrent CNSL.
Methods
Through October 2015, 17 patients with relapsed/refractory CNSL received pemetrexed every 2 weeks with the first cohort receiving 600 mg/m2 and dose escalation in increments of 300 mg/m2 to a maximum of 1,200 mg/m2. Three patients were to enroll at each dose level with expansion to six patients in the event of dose‐limiting toxicity. Patients with both primary CNS lymphoma (PCNSL) and secondary CNS lymphoma (SCNSL) could be enrolled.
Results
Seventeen patients were evaluable with a median age of 63.7 years. Main adverse events included fatigue (82.4%), anemia (82.4%), and neutropenia (70.6%). The MTD was established at 900 mg/m2. Dose‐limiting toxicities were recorded in one patient in the 600 mg/m2 cohort and in two patients in the 1,200 mg/m2 cohort. Fourteen patients were evaluable for response assessment; 21.4% achieved a complete response, 35.7% had a partial response, 14.3% had stable disease, and 28.6% had progressive disease. The median progression‐free survival was 4.2 months. The median overall survival was 44.5 months.
In the original study protocol, the plan was to add an expansion cohort of six patients at MTD level. However, the first phase of the study was characterized by slow recruitment. Therefore, after achieving the primary objective of the study and establishing the MTD, the investigators decided to amend the protocol and to close the study.
Conclusion
Pemetrexed administered at 900 mg/m2 every 2 weeks exhibits single‐agent activity in patients with recurrent CNSL; it is well tolerated, and side effects are manageable.
Short abstract
This Letter to the Editor adds to recent reports to provide guidance for cancer care during the COVID‐19 pandemic.
Discussion
The MTD of 900 mg/m2 every 2 weeks was identified. Treatment was generally well tolerated with encouraging activity of pemetrexed. Pemetrexed responses were promising, with overall response rate (ORR) of 57.1%, disease control rate (DCR) of 71.4%, median progression‐free survival (PFS) of 4.2 months, and median overall survival (OS) of 44.5 months. All patients received at least one line of treatment including methotrexate prior to enrollment in this study. Figure 1 shows a swimmer plot of the durations and responses of treatment.
Figure 1.
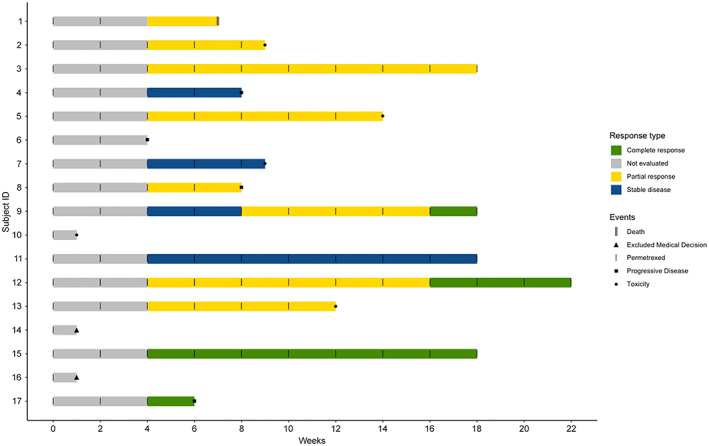
Swimmer plot representing the durations and responses of treatment (pemetrexed) in patients with CNSL. Response rate was evaluated by magnetic resonance imaging of the brain every two cycles (4 weeks).
Zhang et al. [1] reported outcomes and toxicities for 30 patients with CNSL (18 PCNSL and 12 SCNSL) with pemetrexed. The median number of prior CNS relapses was 1.5, and most patients (86.7%) had received prior MTX, suggesting that pemetrexed may not exhibit cross‐resistance with MTX; 73.3% of their patients received pemetrexed at 900 mg/m2 every 3 weeks as their initial dose. The ORR was 62%, and the DCR was 68.9%. The median PFS was 4.1 months (5.8 months in the PCNSL subgroup). The median OS was not reached, but at 22.6 months, the OS rate was 54%. There was no significant difference in PFS or OS between patients who received pemetrexed at 900 mg/m2 (22 patients) and those who received lower initial doses of pemetrexed (8 patients). The most common grade > 3 adverse events included leukopenia and fatigue, consistent with the findings from our study.
Although pemetrexed showed efficacy and disease control in the majority of our patients, we were only able to evaluate response is a cohort of 14 patients, limiting the conclusions of our findings. None of our patients had a diagnosis of active ocular or leptomeningeal disease, thereby limiting the conclusion of whether pemetrexed has activity in this context. The efficacy of pemetrexed in recurrent CNS lymphoma warrants further evaluation in future studies, potentially in combination with other agents with known activity in this disease population.
As secondary objectives, analysis of pharmacokinetics and pharmacodynamics was initially included in the protocol. Unfortunately, the lack of a sufficient number of cerebrospinal fluid and serum samples rendered such analyses inconclusive. Finally, although we observed a median OS of 44.5 months in our study, most patients received several additional lines of treatment after pemetrexed, which contributed to their extended survival.
Trial Information
| Disease | Brain cancer – primary |
| Disease | Lymphoma – non‐Hodgkins |
| Stage of Disease/Treatment | Primary |
| Prior Therapy | Two prior regimens |
| Type of Study − 1 | Phase I, 3 + 3 |
| Primary Endpoints | Maximum tolerated dose, tolerability, safety |
| Secondary Endpoints | Progression‐free survival, overall survival, overall response to treatment |
| Additional Details of Endpoints or Study Design | |
| We conducted a multicenter, open‐label, single‐agent phase I study of pemetrexed. Patients were enrolled using a 3 + 3 dose‐escalating design. The MTD was defined as the dose level below which dose‐limiting toxicity (DLT) was encountered in one‐third of the patients. DLT was defined as any grade 4 toxicity (except grade 4 febrile neutropenia lasting less than 5 days) and any grade 3 nonhematologic, non‐neurologic toxicity (except grade 3 hepatic transaminase elevations and grade 3 fatigue or generalized weakness) within the first two cycles (28 days) of therapy or the 14‐day observation period between each dose level cohort. The National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE) version 3.0 was used to grade all the toxicities. | |
| Pemetrexed was administered as an intravenous infusion over 10–20 minutes every 2 weeks. Three patients per dose‐level cohort were treated and evaluated for toxicity over a period of 28 days (two cycles of pemetrexed per dose). After the third patient in each dose‐level cohort completed the second administration of pemetrexed, there was a 14‐day observation period. If no DLT was observed in any of the three patients in the cohort, escalation to the next dose‐level cohort was performed. A starting dose at 600 mg/m2 was chosen. The dose was escalated in increments of 300 mg/m2 to a maximum of 1,200 mg/m2 of pemetrexed. If a drug‐related DLT occurred at any dose‐level cohort, an additional three patients were added to a total accrual of six patients at this dose‐level cohort. | |
| Patients received dexamethasone (4 mg of oral or equivalent) twice daily, on the day before, the day of, and the day after each dose of pemetrexed, for prophylaxis of skin‐related adverse effects and rashes. To reduce potential side effects of pemetrexed, patients were also instructed to take folic acid 800 μg daily, starting 7 days before the first dose of pemetrexed and continuing for 3 weeks after the last dose. Vitamin B12 1,000 μg supplementation, as an intramuscular injection, was also administrated, starting 7–14 days prior to the first dose of pemetrexed, and was repeated every 9 weeks until 3 weeks after the last dose. Because of grade 4 neutropenia toxicity observed in the first treatment cohort, all patients were subsequently treated with granulocyte colony‐stimulating factor. Patients remained on treatment until complete response or cycle 8. Patients with complete response received up to two additional consolidation cycles. | |
| In the original study protocol, the plan was to add an expansion cohort of six patients at MTD level. However, the first phase of the study was characterized by slow recruitment. Therefore, after achieving the primary objective of the study and establishing the MTD, the investigators decided to amend the protocol and to close the study. | |
| Investigator's Analysis | Correlative endpoints met but not powered to assess activity |
Drug Information
| Generic/Working Name | Pemetrexed |
| Trade Name | Alimta |
| Company Name | Eli Lilly & Co. |
| Dose | 600 milligrams (mg) per squared meter (m2) |
| Route | IV |
| Schedule of Administration | Pemetrexed was administered as an intravenous infusion over 10–20 minutes every 2 weeks. |
Dose Escalation Table
| Dose level | Dose of drug: Pemetrexed | Number enrolled | Number evaluable for toxicity |
|---|---|---|---|
| 600 | 600 mg/m2 | 6 | 6 |
| 900 | 900 mg/m2 | 4 | 3 |
| 1,200 | 1,200 mg/m2 | 7 | 6 |
Patient Characteristics
| Number of Patients, Male | 9 |
| Number of Patients, Female | 8 |
| Age | Median (range): 63.7 years (range 47–77 years) |
| Number of Prior Systemic Therapies | Median (range): 1.6 (range 1–3) |
| Performance Status: ECOG |
0 — 0 1 —0 2 —0 3 —0 Unknown — 17 |
| Other | |
| Through October 2015, 18 patients with CNSL were enrolled from three centers in Boston: Massachusetts General Hospital (n = 9), Dana‐Farber Cancer Institute (n = 7), and Beth Israel Deaconess Medical Center (n = 2). Seventeen patients received treatment (one patient withdrew consent before receiving treatment). Basic demographics and patient characteristics are presented in Table 1. The sex ratio was 1:1.1 with a median age of 63.7 (range 47–77 years). Performance status was assessed by Karnofsky performance status. Initial diagnosis of CNSL was established by brain biopsy in all patients. All 17 patients were considered in the intention‐to‐treat (ITT) analysis. Among these, 14 of 17 patients had at least one magnetic resonance imaging (MRI) and were evaluable for response assessment. The remaining 3 of 17 patients prematurely stopped the study before the first MRI was obtained (before the second cycle) because of medical decision by the treating provider (n = 2) or toxicity (n = 1). From the evaluable patients, the median number of treatment cycles was 6.4 ± 3.4. | |
| Cancer Types or Histologic Subtypes | PCNSL, 14; SCNSL, 3 |
Table 1.
Patient demographics, clinical characteristics, and treatment data
| Age, (years) | Gender | KPS | Disease status | Focality | Tumor localization | Prior treatment | Disease status prior to pemetrexed | Time between last treatment and start of pemetrexed, (months) | Dose | Cycle number | Response |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 76 | F | 60 | PCNSL | Multi | Frontal lobe, thalamus/basal ganglia | HD‐MTX | Relapse | 1 | 600 | 2 | PR |
| 77 | M | 60 | PCNSL | Uni | Occipital lobe | HD‐MTX | Relapse | 1 | 600 | 5 | PR |
| 66 | M | 90 | PCNSL | Uni | Midbrain/pons | (a) HD‐MTX, (b) MTX‐thiotepa | Relapse | 38 | 600 | 10 | PR |
| 68 | F | 80 | PCNSL | Uni | Temporal lobe | MTX‐TMZ‐R then HD‐MTX | Relapse | 1 | 600 | 4 | PD |
| 64 | M | 80 | PCNSL | Uni | Thalamus/basal ganglia | HD‐MTX | Intolerant to MTX | 1 | 600 | 7 | PR |
| 53 | F | 90 | PCNSL | Uni | Parietal lobe | MTX‐TMZ‐R then HD‐MTX | Relapse | 1 | 600 | 2 | PD |
| 71 | M | 80 | SCNSL | Uni | Corpus callosum | (a) HD‐MTX, (b) R‐CHOP, (c) radiation | Relapse | 2 | 900 | 5 | SD |
| 67 | M | 70 | SCNSL | Uni | Fronto‐parieto‐temporal | (a) R‐CHOP, (b) HD‐MTX | Relapse | 1 | 900 | 4 | PD |
| 54 | F | 100 | PCNSL | Uni | Frontal lobe | MTX‐TMZ‐R, then cytarabine/etoposide | Relapse | 19 | 900 | 10 | CR |
| 49 | M | 90 | PCNSL | Multi | Frontal lobe | (a) R‐EPOCH avastin + MTXi, (b) MTX‐TMZ‐R, R‐Ara‐C, and radiation | Relapse | 1 | 1,200 | 1 | — |
| 72 | F | 100 | PCNSL | Multi | Frontal/temporal lobe | MTX‐TMZ | Relapse | 4 | 1,200 | 10 | SD |
| 66 | F | 100 | PCNSL | Uni | Temporal lobe | (a) HD‐MTX, (b) HD‐MTX‐R and radiation, (c) HD‐MTX | Relapse | 1 | 1,200 | 12 | CR |
| 51 | M | 90 | PCNSL | Uni | Corpus callosum | MTX‐TMZ‐R then ASCT | Relapse | 44 | 1,200 | 6 | PR |
| 61 | M | 80 | SCNSL | Uni | Parietal lobe | (a) R‐CVP, (b) R‐CHOP, (c) HD‐MTX | Refractory | 1 | 1,200 | 1 | — |
| 47 | M | 60 | PCNSL | Multi | Cerebellum | HD‐MTX‐TMZ‐R then ASCT | Relapse | 30 | 1,200 | 10 | CR |
| 68 | F | * | PCNSL | Multi | Parieto‐occipital lobe | (a) HD‐MTX, (b) ioMTX, (c) ioMTX | Relapse | 24 | 900 | 1 | — |
| 73 | F | 90 | PCNSL | Multi | Parietal lobe, periventricular, mid brain | MTX‐TMZ‐R, Ara‐C | Relapse | 11 | 1,200 | 3 | PD |
Abbreviations: *, not evaluable; CR, complete response; F, female; HD‐MTX, high‐dose methotrexate; HD‐MTX‐R, high‐dose methotrexate rituximab; ioMTX, intraocular methotrexate; KPS, Karnofsky performance status; M, male; MTXi, methotrexate intrathecal; MTX‐TMZ‐R, methotrexate temozolomide rituximab; OS, overall survival; PCSNL, primary central system nervous lymphoma; PD, progressive disease; PFS, progression‐free survival; PR, partial response; R‐Ara‐C, rituximab cytarabine; R‐CHOP, rituximab cyclophosphamide hydroxydaunomycin oncovin prednisone; R‐CVP, rituximab cyclophosphamide vincristine prednisone; R‐EPOCH, rituximab etoposide prednisone oncovin cyclophosphamide hydroxydaunomycin; SCNL, secondary central system nervous lymphoma; SD, stable disease.
Primary Assessment Method
| Number of Patients Screened | 18 |
| Number of Patients Enrolled | 17 |
| Number of Patients Evaluable for Toxicity | 17 |
| Number of Patients Evaluated for Efficacy | 14 |
| Evaluation Method | Other (toxicity: CTCAE version 3; efficacy: MacDonald criteria) |
| Response Assessment CR | n = 3 (21.4%) |
| Response Assessment PR | n = 5 (35.7%) |
| Response Assessment SD | n = 2 (14.3%) |
| Response Assessment PD | n = 4 (28.6%) |
| Response Assessment OTHER | n = 0 (0%) |
| (Median) Duration Assessments PFS | 4.2 months |
| (Median) Duration Assessments OS | 44.5 months |
| Outcome Notes |
Treatment response was assessed by MRI of the brain every 4 weeks. Patients remained on treatment until complete response was achieved, or after completion of a maximum of eight cycles. Response assessment was defined using modified MacDonald criteria on brain MRI, as follows: • Complete response (CR): absence of gadolinium enhancing tumor on MRI or clearance/absence of malignant cells in cerebrospinal fluid. • Partial response (PR): 50% or more decrease in gadolinium enhancing tumor on MRI on cross‐sectional dimensions but not qualifying for complete response. • Stable disease (SD): does not qualify for complete response, partial response, or progression. • Progressive disease (PD): 25% or more increase in gadolinium enhancing tumor on MRI on cross‐sectional dimensions lesion. The response was assessed at the end of the treatment for each patient. Among all 17 patients, 14 patients were evaluable for response assessment: 3 patients achieved a CR, 5 patients had a PR, 2 patients had SD, and 4 patients had PD (Table 1, Fig. 1). CR was seen after two and eight cycles of pemetrexed in two patients at 1,200 mg/m2 and after eight cycles in one patient at 900 mg/m2. An additional patient achieved CR as the best response after two cycles at a dose level of 1,200 mg/m2; however, this patient ultimately progressed after two more cycles. The ORR including CR + PR was 57.1%, and the DCR including PR + CR + SD was 71.4%. The 6‐month PFS and 12‐month PFS were 35.7% (95% confidence interval [CI], 18%–72%) and 21.4% (95% CI, 8%–58%), respectively, with a median PFS of 4.2 months (95% CI, 2 months, not reached [NR]). The median OS was 44.5 months (95% CI, 19 months, NR). The estimated 1‐year, 2‐year, and 5‐year survival rates were 78.6%, 64.3%, and 35.7%, respectively. In the ITT analysis (17 patients), the DCR and ORR were 58.8% and 47.1%, respectively, with a median OS at 30 months (95% CI, 17 months, NR; Figs. 2, 3). Reason for study discontinuation was completion of treatment in five patients, PD in four patients, toxicity in five patients, medical decision in two patients, death for one patient, and withdrawal of consent for one patient. |
Figure 2.
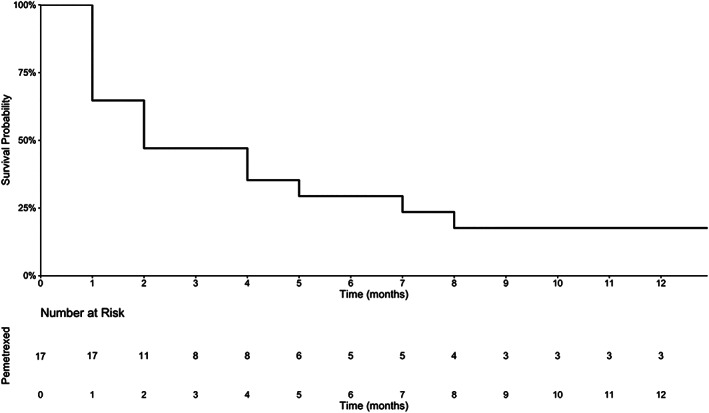
Progression‐free survival in all 17 patients with CSNL (intention‐to‐treat analysis).
Figure 3.
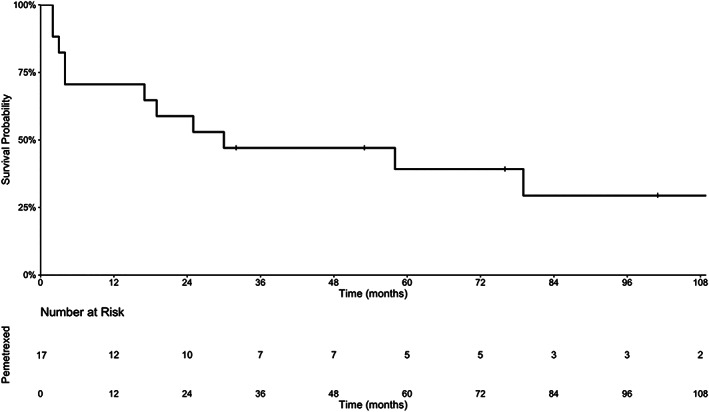
Overall survival in all 17 patients with CSNL (intention‐to‐treat analysis).
Adverse Events
| All Cycles | |||||||
|---|---|---|---|---|---|---|---|
| Name | NC/NA, % | Grade 1, % | Grade 2, % | Grade 3, % | Grade 4, % | Grade 5, % | All grades, % |
| Anemia | 17 | 47 | 24 | 12 | 0 | 0 | 83 |
| Fatigue | 18 | 41 | 35 | 6 | 0 | 0 | 82 |
| Neutropenia | 28 | 18 | 24 | 18 | 12 | 0 | 72 |
| Alanine aminotransferase increased | 29 | 47 | 12 | 12 | 0 | 0 | 71 |
| Hypophosphatemia | 41 | 6 | 41 | 6 | 6 | 0 | 59 |
| Thrombocytopenia | 47 | 47 | 6 | 0 | 0 | 0 | 53 |
| Hyperglycemia | 46 | 24 | 24 | 6 | 0 | 0 | 54 |
| Aspartate aminotransferase increased | 47 | 41 | 6 | 6 | 0 | 0 | 53 |
| Generalized muscle weakness | 58 | 24 | 18 | 0 | 0 | 0 | 42 |
| Leukopenia | 58 | 18 | 6 | 18 | 0 | 0 | 42 |
| Lymphopenia | 53 | 0 | 29 | 6 | 12 | 0 | 47 |
| Anxiety | 65 | 29 | 6 | 0 | 0 | 0 | 35 |
| Nausea | 70 | 24 | 6 | 0 | 0 | 0 | 30 |
| Constipation | 76 | 24 | 0 | 0 | 0 | 0 | 24 |
| Depression | 76 | 24 | 0 | 0 | 0 | 0 | 24 |
| Peripheral sensory neuropathy | 76 | 18 | 6 | 0 | 0 | 0 | 24 |
| Creatinine increased | 76 | 12 | 12 | 0 | 0 | 0 | 24 |
| Low serum bicarbonate | 82 | 18 | 0 | 0 | 0 | 0 | 18 |
| Headache | 82 | 18 | 0 | 0 | 0 | 0 | 18 |
| Hyponatremia | 82 | 18 | 0 | 0 | 0 | 0 | 18 |
| Insomnia | 82 | 18 | 0 | 0 | 0 | 0 | 18 |
| Proteinuria | 82 | 18 | 0 | 0 | 0 | 0 | 18 |
| Seizure | 82 | 18 | 0 | 0 | 0 | 0 | 18 |
Adverse Events Legend
All 17 patients were evaluable for safety and tolerability.
Abbreviation: NC/NA, no change from baseline/no adverse event.
Dose‐Limiting Toxicities
| Dose level | Number enrolled | Number evaluable for toxicity | Number with a dose‐limiting toxicity | Dose‐limiting toxicity information |
|---|---|---|---|---|
| 600 | 6 | 6 | 1 | Neutropenia grade 4 |
| 900 | 4 | 3 | 0 | |
| 1,200 | 7 | 6 | 2 | Lymphopenia grade 4 |
DLT Table Legend
Patients were started at a pemetrexed dose of 600 mg/m2, and dose escalations were done up to 1,200 mg/m2. Pemetrexed at a dose of 600 mg/m2 was administered to six patients, 900 mg/m2 to four patients, and 1,200 mg/m2 to seven patients. Two patients were not evaluable for DLTs (one in the cohort at 900 mg/m2 and one in the cohort at 1,200 mg/m2). DLTs were recorded in one patient in the 600 mg/m2 cohort (neutropenia grade 4) and in two patients in the 1,200 mg/m2 cohort (lymphopenia grade 4).
The dose of pemetrexed was reduced in three patients: one dose reduction (n = 2, in one patient because of elevated transaminase at the 900 mg/m2 dose level and in one patient because of neutropenia at the 600 mg/m2 dose level) and two dose reductions (n = 1, secondary to neutropenia at the 600 mg/m2 dose level). The most common treatment‐related adverse events (AEs) of any grade encountered in all treatment cycles were fatigue (82.4%), anemia (82.4%), and neutropenia (70.6%). At the 1,200 mg/m2 dose level, hematologic AEs of neutropenia, lymphopenia, and fatigue were the most commonly encountered treatment‐related AEs of grade >3 or higher.
Assessment, Analysis, and Discussion
| Completion | Study completed |
| Investigator's Assessment | Correlative endpoints met but not powered to assess activity |
We here report the safety and tolerability data from a multi‐institutional phase I study using pemetrexed as monotherapy in recurrent/progressive central nervous system lymphoma (CNSL; NCT00916630). This is the first study to establish the maximum tolerated dose (MTD) of pemetrexed in patients with recurrent CNSL. The MTD of 900 mg/m2 every 2 weeks was identified. Treatment was generally well tolerated with encouraging activity of pemetrexed. Additionally, responses were promising, with overall response rate (ORR) of 57.1%, disease control rate (DCR) of 71.4%, median progression‐free survival (PFS) of 4.2 months, and median overall survival (OS) of 44.5 months. All patients received at least one line of treatment including methotrexate (MTX) prior to enrollment in this study. These results are comparable to the findings from a previous phase II study by Raizer et al. [2], assessing the efficacy of pemetrexed in patients with relapsed/refractory primary CNSL (PCNSL). They reported outcomes from 11 patients, treated with 900 mg/m2 of pemetrexed every 3 weeks. All patients in this study had previously received high‐dose MTX. The ORR was 55%, and the DCR was 91%, with a median PFS of 5.7 months, 6‐month PFS of 45%, and 12‐month OS of 45%.
In a retrospective study, Zhang et al. [1] reported outcomes and toxicities for 30 patients with CNSL (18 PCNSL and 12 secondary CNSL) with pemetrexed. The median number of prior central nervous system (CNS) relapses was 1.5, and most patients (86.7%) had received prior MTX, suggesting that pemetrexed may not exhibit cross‐resistance with MTX. Of patients in this study, 73.3% received pemetrexed at 900 mg/m2 every 3 weeks as their initial dose. The ORR was 62%, and the DCR was 68.9%. The median PFS was 4.1 months (5.8 months in the PCNSL subgroup). The median OS was not reached, but at 22.6 months, the OS rate was 54%. There was no significant difference in PFS or OS between patients who received pemetrexed at 900 mg/m2 (22 patients) and those who received lower initial doses of pemetrexed (8 patients). The most common grade > 3 adverse events included leukopenia and fatigue, consistent with the findings from our study.
Han et al. [3] reviewed the efficacy of pemetrexed (dose level of 600 mg/m2 every 3 weeks) in elderly patients with PCNSL. They reported a median PFS of 9 months and median OS of 19.5 months in this population. The ORR and the DCR were 83.3%. This study demonstrated that pemetrexed was active and well tolerated and resulted in less toxicity compared with other chemotherapy regimens used in elderly patients.
Zhao et al. [4] studied the association of pemetrexed plus rituximab as second‐line treatment for PCNSL in 27 patients. All patients had previously received MTX. Rituximab at a dose of 375 mg/m2 was administered on day 0, and pemetrexed 500 mg/m2 was administered every 3 weeks. The response rate was 62.9% and the disease control rate was 92.5% The median PFS was 6.9 months, and the median OS was 11.2 months. These findings were superior to the data from our study in terms of median PFS, ORR, and DCR despite a lower dose of pemetrexed at 500 mg/m2 every 3 weeks. It therefore is possible that the combination with rituximab may have conferred improved outcomes.
A few studies have investigated the distribution of pemetrexed into the brain. In the study by Dai et al., the distributional clearance into the CNS was approximately 10% of the clearance outside the brain in both the compartmental and noncompartmental analyses [5]. Stapleton et al. demonstrated that the cerebrospinal fluid distribution of pemetrexed in nonhuman primates was less than 2% [6]. Despite limited CNS penetration, pemetrexed demonstrated activity in patients with non‐small cell lung carcinoma with brain metastasis [7] and in patients with CNSL.
Prior studies in solid cancer have raised potential concerns of pemetrexed‐associated renal toxicity [8, 9, 10]. However, these findings may have been confounded by using pemetrexed in conjunction with other potentially nephrotoxic chemotherapy regimen. Of note, renal toxicity was not a concerning adverse effect in our study.
MTX remains the most active agent in newly diagnosed CNSL, but the optimal management of recurrent CNSL has not been established. Several studies evaluated second‐line salvage therapies, including rechallenge with high‐dose MTX [11], temozolomide with or without rituximab [12, 13, 14, 15], rituximab [16], rituximab‐ifosfamide‐etoposide [17], topotecan [18, 19], lenalidomide [20], ibrutinib [21], Temozolomide, Etoposide, Doxil, Dexamethasone, Ibrutinib and Rituximab (TEDDI‐R) [22], and whole brain radiotherapy [23] with varying response rates (ranging from 14% to 85%) and survival (ranging from 4 to 61 months). A median PFS of 2–5 months has been achieved with most regimens.
Although pemetrexed showed efficacy and disease control in the majority of our patients, we were only able to evaluate response is a cohort of 14 patients, limiting the conclusions of our findings. None of our patients had a diagnosis of active ocular or leptomeningeal disease, thereby limiting the conclusion of whether pemetrexed has activity in this context. The efficacy of pemetrexed in recurrent CNS lymphoma warrants further evaluation in future studies, potentially in combination with other agents with known activity in this disease population.
As secondary objectives, analysis of pharmacokinetics and pharmacodynamics was initially included in the protocol. Unfortunately, the lack of a sufficient number of cerebrospinal fluid and serum samples rendered such analyses inconclusive. Finally, although we observed a median OS of 44.5 months in our study, most patients received several additional lines of treatment after pemetrexed, which contributed to their extended survival.
The 2‐week schedule was based on a phase I study of pemetrexed and gemcitabine in patients with advanced solid tumors [24]. Toxicity data in our study were comparable to the findings from a previous phase II study by Raizer et al. [2] using a 3‐week schedule. PFS and OS were slightly higher with a 3‐week schedule with the limitation of a small number of subjects in both studies (fewer than 20 patients). Because response assessment was not the primary objective of the current study, it presently cannot be determined based on all available data whether a 2‐week or 3‐week regimen is associated with improved outcome.
In this context, the findings from our study using monotherapy with pemetrexed in a pretreated patient population, including some patients with prior bone marrow transplantation, are overall encouraging. Unlike high‐dose methotrexate, which requires several days of inpatient hospitalization, pemetrexed is relatively easy to administer in the outpatient setting and remains a viable treatment option in this patient population. Assessment of potential combination regimens with other active agents should be considered in this challenging disease. In summary, a maximum tolerated dose of pemetrexed administered at 900 mg/m2 every 2 weeks was generally well tolerated and showed activity in patients with relapsed or refractory CNSL.
Disclosures
Jorg Dietrich: Blue Earth Diagnostics, Inc., Unum Therapeutics (C/A), Wolters Kluwer (UpToDate, author royalties); Lakshmi Nayak: Bristol‐Meyers Squibb (C/A); Andrew Norden: COTA, Inc. (E, OI); Bruce Chabner: PharmaMar, EMD Serono, Cyteir (C/A), Cyteir (H), Biomarin, Seattle Genetics, GlaxoSmithKline, PharmaMar, Blueprint, Immunomedics, Constellation (OI), Eli Lilly & Co., Genentech (ET); Fred Hochberg: NX Pharmaceuticals, Tavec Pharmaceuticals (C/A); Tracy Batchelor: Genomicare, Merck, NXDC, Amgen, Proximagen/Upsher, Champions Biotechnology (C/A), Pfizer, Oncoceutics (RF), UpToDate, Oakstone (other—royalties for editorial activities). The other authors indicated no financial relationships.
(C/A) Consulting/advisory relationship; (RF) Research funding; (E) Employment; (ET) Expert testimony; (H) Honoraria received; (OI) Ownership interests; (IP) Intellectual property rights/inventor/patent holder; (SAB) Scientific advisory board
Figures and Table
Acknowledgments
We thank our patients for contributing to this research study. We thank Alexandra Malesz and Kristin C. Moy for assistance with data collection and Dr. Jeffrey Supko and Dr. Shrikanta Chattopadhyay for very helpful discussions in the planning and design of this study.
No part of this article may be reproduced, stored, or transmitted in any form or for any means without the prior permission in writing from the copyright holder. For information on purchasing reprints contact Commercialreprints@wiley.com. For permission information contact permissions@wiley.com.
Footnotes
- ClinicalTrials.gov Identifier: NCT00916630
- Sponsor: Eli Lilly & Co.
- Principal Investigator: Jorg Dietrich
- IRB Approved: Yes
References
- 1. Zhang JP, Lee EQ, Nayak L et al. Retrospective study of pemetrexed as salvage therapy for central nervous system lymphoma. J Neurooncol 2013;115:71–77. [DOI] [PubMed] [Google Scholar]
- 2. Raizer JJ, Rademaker A, Evens AM et al. Pemetrexed in the treatment of relapsed/refractory primary central nervous system lymphoma. Cancer 2012;18:3743–3748. [DOI] [PubMed] [Google Scholar]
- 3. Han S, Wang M, Liu B et al. Pemetrexed for primary central nervous system lymphoma in the elderly. Clin Transl Oncol 2016;18:138–143. [DOI] [PubMed] [Google Scholar]
- 4. Zhao HT, Chen J, Shi S et al. Pemetrexed plus rituximab as second‐line treatment for primary central nervous system lymphoma. Med Oncol 2015;32:351. [DOI] [PubMed] [Google Scholar]
- 5. Dai H, Chen Y, Elmquist WF. Distribution of the novel antifolate pemetrexed to the brain. J Pharmacol Exp Ther 2005;315:222–229. [DOI] [PubMed] [Google Scholar]
- 6. Stapleton SL, Reid JM, Thompson PA et al. Plasma and cerebrospinal fluid pharmacokinetics of pemetrexed after intravenous administration in non‐human primates. Cancer Chemother Pharmacol 2007;59:461–466. [DOI] [PubMed] [Google Scholar]
- 7. Inno A, Di Noia V, D'Argentto E et al. State of the art of chemotherapy for the treatment of central nervous system metastases from non‐small cell lung cancer. Trans Lung Cancer Res 2016;5:599–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mita AC, Sweeney CJ, Baker SD et al. Phase I and pharmacokinetic study of pemetrexed administered every 3 weeks to advanced cancer patients with normal and impaired renal function. J Clin Oncol 2006;24:552–562. [DOI] [PubMed] [Google Scholar]
- 9. Glezerman IG, Pietanza MC, Miller V et al. Kidney tubular toxicity of maintenance pemetrexed therapy. Am J Kidney Dis 2011;58:817–820. [DOI] [PubMed] [Google Scholar]
- 10. Visser S, Huisbrink J, van't Veer NE et al. Renal impairment during pemetrexed maintenance in patients with advanced non small cell lung cancer: A cohort study. Eur Respir J 2018;52;1800884. [DOI] [PubMed] [Google Scholar]
- 11. Plotkin SR, Betensky RA, Hochberg FH et al. Treatment of relapsed central nervous system lymphoma with high‐dose methotrexate. Clin Cancer Res 2004;10:5643–5646. [DOI] [PubMed] [Google Scholar]
- 12. Wong SF, Gan HK, Cher L. A single centre study of the treatment of relapsed primary central nervous system lymphoma (PCNSL) with single agent temozolomide. J Clin Neurosci 2004;19:1501–1505. [DOI] [PubMed] [Google Scholar]
- 13. Reni M, Zana F, Mason W et al. Temozolomide as salvage treatment in primary brain lymphomas. Br J Cancer 2007;96:864–867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Enting RH, Demopouolos A, DeAngelis LM et al. Salvage therapy for primary CNS lymphoma with a combination of rituximab and temozolomide. Neurology 2004;63:901–903. [DOI] [PubMed] [Google Scholar]
- 15. Nayak L, Abrey LE, Drappatz J et al. Multicenter phase II study of rituximab and temozolomide in recurrent primary central nervous system lymphoma. Leuk Lymphoma 2012;19:1501–1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bachelor TT, Grossman SA, Mikkelsen T et al. Rituximab monotherapy for patients with recurrent primary CNS lymphoma. Neurology 2011;76:929–930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mappa S, Marturano E, Licata G et al. Salvage chemoimmunotherapy with rituximab, ifosfamide and etoposide (R‐IE regimen) in patients with primary CNS lymphoma relapsed or refractory to high‐dose methotrexate‐based chemotherapy. Hematol Oncol 2013;31:143–150. [DOI] [PubMed] [Google Scholar]
- 18. Fischer L, Thiel E, Klasen HA et al. Prospective trial on topotecan salvage therapy in primary CNS lymphoma. Ann Oncol 2006;17:1141–1145. [DOI] [PubMed] [Google Scholar]
- 19. Voloshin AD, Betensky R, Wen PY et al. Topotecan as salvage therapy for relapsed or refractory primary central nervous system lymphoma. J Neurooncol 2008;86:211–215. [DOI] [PubMed] [Google Scholar]
- 20. Houiller C, Choquet S, Toutou V et al. Lenalidomide monotherapy as salvage treatment for recurrent primary CNS lymphoma. Neurology 2015;84:325–326. [DOI] [PubMed] [Google Scholar]
- 21. Grommes C, Tang SS, Wolfe J et al. Phase 1b trial of an ibrutinib‐based combination therapy in recurrent/refractory CNS lymphoma. Blood 2019;133:436–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lionakis MS, Dunleavy K, Roschewski M et al. Inhibition of B cell receptor signaling by ibrutinib in primary CNS lymphoma. Cancer Cell 2017;31:833–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Khimani NB, Ng AK, Chen YH et al. Salvage radiotherapy in patients with recurrent or refractory primary or secondary central nervous system lymphoma after methotrexate‐based chemotherapy. Ann Oncol 2011;22:979–984. [DOI] [PubMed] [Google Scholar]
- 24. Dudek AL, Melskog CE. A phase I clinical study of biweekly pemetrexed and gemcitabine in patients with advanced solid tumors. J Clin Oncol 2004;22(suppl 14):2141a.15169800 [Google Scholar]


