Abstract
Background:
Wellness among resident physicians is important to their well-being and ability to provide clinical care. The relationship between physical activity and wellness among anesthesia residents has not yet been evaluated. We surveyed anesthesia residents to evaluate their levels of physical activity and self-perceived wellness scores. We hypothesized that residents with high self-reported physical activity levels would be more likely to have higher wellness scores.
Methods:
Three hundred and twenty-three anesthesia residents were invited to participate in this cross-sectional survey study. The survey included questions regarding demographics (age, gender, clinical anesthesia year, work hours), physical activity (based off the US Department of Health and Human Services [USDHHS] guidelines), and wellness (using the Satisfaction With Life Scale). The relationship between wellness and physical activity levels was evaluated.
Results:
One hundred forty-one residents responded (43.6% response rate). Thirty-eight (27.1%) residents met our activity threshold for physically active. Eighty-six respondents (61.4%) were classified as having high wellness based on their survey answers. No significant associations were found between demographic data and wellness, including age or clinical anesthesia training year. Among those residents who described physical activity consistent with USDHHS guidelines, 29 (76.3%) had high wellness scores. After logistic regression analysis, residents who achieved the physical activity guidelines were more likely to have high wellness scores (odds ratio 2.54, 95% confidence interval 1.13–6.20, P value .03).
Conclusions:
Anesthesia resident physicians with high physical activity levels had higher self-perceived wellness scores.
Keywords: Residency, wellness programs, life quality, burnout, exercise, physical activity
Introduction
Physician wellness—a multidimensional descriptor that includes mental, social, emotional, and physical health1—affects not only the physician but also their ability to care for their patients.1,2 Inadequate wellness may manifest as poor physical health, job dissatisfaction, and depression.3–6
Wellness issues may significantly affect resident physicians. In a 2014 survey of more than 1700 students and residents, the residents were more likely to have higher levels of fatigue, a lower quality of life, and screen positive for depression when compared with the general US population.7 Resident trainees are also at higher risk for burnout than their college graduate peers,7 a condition that can lead to increased risk of alcohol abuse and dependence, and suicidal ideation.8,9 As a consequence, the Accreditation Council for Graduate Medical Education (ACGME) and many individual residency programs have prioritized resident wellness. As an example, the ACGME Clinical Learning Environment Review’s Pathway to Excellence highlights the need for periodic education and monitoring for physician fatigue and burnout.10
One approach to improving resident wellness is to encourage more physical activity. Exercise affords numerous health benefits, including improved sleep and eating habits, and a decreased incidence of type 2 diabetes.11–15 Physical activity also improves cognition, reduces depression and anxiety,16–18 and has been postulated to lower burnout and increase quality of life among practicing physicians.19
We hypothesized that residents with high physical activity levels are more likely to have better wellness. Life satisfaction, measured by the validated Satisfaction With Life Scale (SWLS), was used as a proxy for wellness in our study. To test our hypothesis, we evaluated the association between self-reported physical activity and our primary outcome of wellness, which was assessed among residents at 6 tertiary care academic anesthesia programs.
Methods
Participants and Data Collection
The study was deemed exempt from formal review by the institutional review board at the University of Chicago (IRB19-0673). A cross-sectional online survey was created using SurveyMonkey software (SurveyMonkey Inc, Portland, OR) and sent in May–June 2019 to 323 clinical anesthesia (CA) year 1, 2, and 3 residents at 6 anesthesia residency programs. Programs were chosen to include a diverse spread of geographical locations across the United States (eg, Midwest, East Coast). The number of residents per program varied from 27 to 75. At each program, surveys were distributed by a designated faculty member after approval from the residency program leadership. Written informed consent was not needed because continuation and completion of the survey implied consent, as stated at the beginning of the survey. To allow the survey to remain anonymous, respondent email addresses were unlinked from their responses. Only one response was allowed per survey invitation, and residents were informed that their participation in the survey was voluntary. All residents were sent a reminder email 1 week after initial contact.
Survey
The survey instrument included 4 questions for demographic data: age, gender, CA year, and work hours. Three subsequent questions pertained to physical activity, and 5 statements addressed wellness. A numerical value was requested for age, and all remaining demographic and physical activity questions were multiple choice. The 5 wellness statements were recorded using a 7-point Likert scale. The full survey as well as details for scoring are available in the Appendix.
Physical Activity Measurement
As a benchmark for physical activity, we used the 2018 US Department for Health and Human Services (USDHHS) “Physical Activity Guidelines for Americans.”20 These guidelines recommend: (1) participating in at least 150 minutes of moderate-intensity exercise per week, 75 minutes of vigorous-intensity exercise per week, or a combination of both and (2) performing muscle-strengthening exercises involving most major muscle groups at least 2 or more days a week. We chose these 2 metrics based on prior studies that have used these to evaluate self-reported physician physical activity.21–23 Three questions, based on a prior study by Weight et al,21 were used to assess adherence to the current physical activity guidelines.
Wellness Evaluation
For purposes of survey analysis, we used the SWLS tool for measuring global cognitive judgments of life satisfaction24 developed in 1985 as a proxy for measuring wellness. Prior studies have used different methods for assessment of wellness, including the SWLS,25,26 single item linear scales for quality of life (ie, 1–100),21 and the Wellness Evaluation of Lifestyle,27 which is considered by some to be the gold standard for wellness measurement.28 The Wellness Evaluation of Lifestyle survey, however, takes longer than 2 hours to complete. For this study, we chose the measurement of life satisfaction using the SWLS to assess residents’ wellness. The ability to complete the SWLS survey questions in less than 2 minutes made it most amenable to our study. Additionally, the SWLS survey has been validated against interview and peer assessment methods29 and is the most widely used instrument for measuring life satisfaction.30 It involves 5 questions, each answered using a 7-point scale ranging from 1 (strongly disagree) to 7 (strongly agree).24 The numerical scores are then summed to translate to different levels of satisfaction, from extremely dissatisfied to extremely satisfied.
Statistical Analysis
The primary outcome, wellness, was defined and established a priori at initiation of the study design. We classified high wellness as scores ranging from extremely satisfied to neutral (20–35) while scores ranging from extremely dissatisfied to slightly dissatisfied (5–19) were classified as low wellness. Survey responses with missing wellness scores were removed from analysis. Demographic characteristics were compared between residents with high and low self-perceived wellness using chi-square tests with Yates correction to evaluate the need of adjustment for confounders. To test the hypothesis that residents with high physical activity levels were more likely to have better wellness, we used a logistic regression model. A two-sided P < .05 was considered statistically significant. All statistical analysis was performed using R software version 3.0.1 (Vienna, Austria).
To verify that our results did not depend on our choice of wellness threshold (score of 20), we reperformed our analysis using a wellness score threshold of 23. This threshold was chosen because it was the median wellness score for our study participants. The results were similar: After logistic regression analysis with the new threshold, residents who met self-reported physical activity guidelines were still more likely to have high wellness scores (odds ratio [OR] 2.17, 95% confidence interval [CI] 1.01–4.67, P value .04).
Results
One hundred forty-one of the 323 residents contacted participated in the survey (43.6% response rate). One respondent was not included in analysis due to an incomplete survey (missing wellness responses), and 1 respondent who was included in the analysis failed to answer 1 question regarding CA year (Figure 1). The demographic characteristics and physical activity level of the residents are listed in Table 1. The mean age of participants was 31.5 years with 60 out of 140 (42.9%) respondents identifying as female. The greatest number of responses was received from CA-1 residents (n = 61); CA-3 residents provided the fewest number of responses (n = 32). Seventy-seven respondents (55%) reported work hours less than 60 hours per week. Thirty-eight (27.1%) residents self-reported physical activity consistent with USDHHS guidelines.
Figure 1.
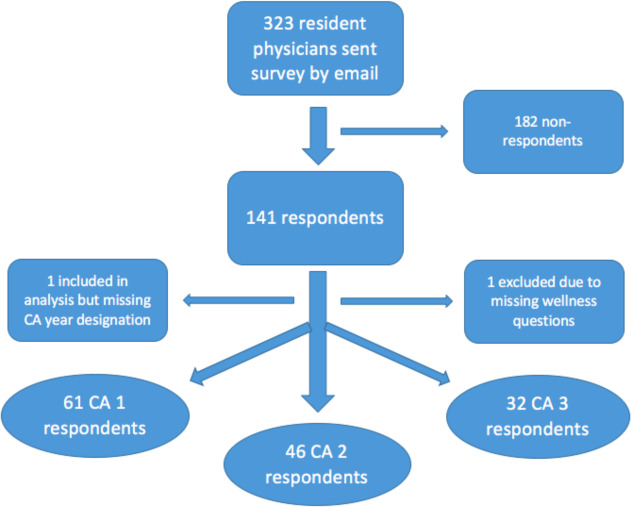
Flow diagram of study participants. Abbreviation: CA, clinical anesthesia.
Table 1.
Study Demographic Characteristics in Residents with High and Low Self-Perceived Wellness a
| Total, n = 140 | Wellnessb | P Value | ||
|---|---|---|---|---|
| High, n = 86 | Low, n = 54 | |||
| Work hours | ||||
| <60 | 77 (55.0) | 49 (57.0) | 28 (51.9) | .675 |
| >60 | 63 (45.0) | 37 (43.0) | 26 (48.2) | |
| Gender | ||||
| Female | 60 (42.9) | 31 (36.1) | 29 (53.7) | .062 |
| Male | 80 (57.1) | 55 (64.0) | 25 (46.3) | |
| CA yearc | ||||
| CA-1 | 61 (43.6) | 35 (40.7) | 26 (49.1) | .425 |
| CA-2 | 46 (32.9) | 29 (33.7) | 17 (32.1) | |
| CA-3 | 32 (22.9) | 22 (25.6) | 10 (18.9) | |
| Age | 31 (3.4) | 30.7 (3.4) | 31.49 (3.4) | .203 |
Abbreviation: CA, clinical anesthesia.
a Data presented as n (%), except for age which is presented as mean (SD).
b According to Satisfaction With Life Scale scores: extremely dissatisfied-slightly dissatisfied = low wellness; neutral-extremely satisfied = high wellness.
c One record removed from CA year category due to missing response (n = 139).
Eighty-six respondents (61.4%) were classified as having high wellness based on their SWLS survey scores ranging from 20–35. No significant associations were found between demographic data and wellness, including age, gender, or clinical anesthesia training year (Table 1). Among those residents who met the physical activity guidelines, 29 (76.3%) had high wellness scores. Figure 2 displays the wellness scores between residents who met the USDHHS physical activity guidelines and those who did not. After logistic regression analysis, residents who met physical activity guidelines were more likely to have high wellness scores (OR 2.54, 95% CI 1.13–6.20, P value .03; Table 2).
Figure 2.
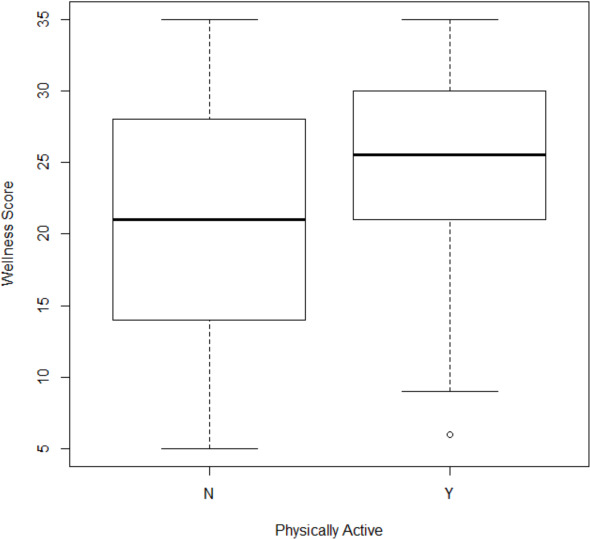
Wellness scores among residents: distribution of wellness scores among survey respondents.
Table 2.
Physical Activity Levels and Logistic Regression Analysis According to Resident Wellness a
| Physically Activeb | Total | Wellnessc | Logistic Regression Analysis for High Wellness Scores | |||
|---|---|---|---|---|---|---|
| High | Low | OR | 95% CI | P Value | ||
| No | 102 (72.9) | 57 (66.3) | 45 (83.3) | ref. | NA | NA |
| Yes | 38 (27.1) | 29 (33.7) | 9 (16.7) | 2.54 | 1.13–6.20 | .03 |
Abbreviations: CI, confidence interval; NA, not applicable; OR, odds ratio; ref., reference.
a Data listed as n (%) except for OR, CI, and P value.
b Designated for those respondents who fulfill the Health and Human Services guidelines for physical activity.
c According to Satisfaction With Life Scale scores: extremely dissatisfied-slightly dissatisfied = low wellness; neutral-extremely satisfied = high wellness.
Discussion
In this cross-sectional survey-based study, we observed that resident physicians who reported physical activity consistent with USDHHS guidelines were more likely to have better self-reported wellness, using life satisfaction as a proxy for wellness. We also found no clear relationship between other respondent factors including work hours, training year, gender, or age.
Numerous studies have found a positive correlation between wellness or life satisfaction with physical activity among the general population. A study by Maher et al31 evaluating 150 adults longitudinally found a weak positive correlation between physical activity and life satisfaction. Other studies have found similar positive correlations among other populations, including school-aged children,32 university students,33 and older adults.34
The link between physical fitness and positive mood is described in the literature. One 2018 review35 found that many types of physical activity including exercise, yoga, and walking interventions can improve mental well-being across office-based settings. Exercise reduces anxiety, improves physical self-perception, and boosts global self-esteem.36 The World Health Organization has found that well-being plays an important role in job satisfaction and productivity,37 and multiple studies have reinforced the cost-effectiveness of physical activity interventions.38,39
The physical activity levels of our study participants give some insight regarding their activity relative to other populations. A study evaluating activity levels of the general US population in 2008 using the USDHSS guidelines found that 18.2% were physically active40 versus 38% of residents in our study. However, one prior study22 demonstrated a relative decrease in physical activity in residents compared with attendings and medical students. In that study, this difference was strongly associated with work hours per week, suggesting that residents’ higher work hours affect their ability to participate in physical activities in their leisure time.
Existing data suggest that fitness initiatives improve wellness and satisfaction among physicians. A 2013 study21 tested the effect of a 12-week, team-based elective exercise program for residents and fellows on quality of life and burnout. The program engaged 23% of residents and fellows, and improved quality of life but not burnout. More recently, a 2017 study41 offered a 12-week wellness curriculum to residents in several specialties involving didactic sessions, positive thinking exercises, and competitions to promote physical fitness. In that study, all programs that participated chose to continue these sessions after the 12-week period ended due to strong participant satisfaction with the curriculum.
Our observational study did not intervene but rather examined current physical activity patterns and their relationship to self-perceived wellness. Our participants did not participate in an exercise program but did self-report their wellness based on their current individual exercise routine. Given residents’ typically heavy and highly variable work schedules, an important solution in implementing programs to encourage greater physical activity may be to offer individualized activity regimens and exercise programs to maximize participation. Systematic reviews suggest a dose-dependent effect of physical activity on mortality and prevention of chronic disease.42 However, the levels of physical activity required to improve mental well-being may differ from the levels of activity required to improve physical well-being.
Although most previous work on wellness targets multiple medical specialties, our study specifically evaluated anesthesia residents’ fitness and wellness. We cannot speculate as to potential differences in responses between our results and how residents from other specialties may respond, but anesthesiology practice does involve both a considerable amount of physical activity and long periods of relative stillness. In addition, anesthesiologists mostly practice alone and must navigate intermittent periods of high stress and acuity. As a result, correlations between physical activity and wellness, and drivers of self-satisfaction may be different between anesthesiologists and other medical specialists.
Our results raise the possibility that developing fitness programs or other opportunities for physical activity may improve wellness among anesthesia residents. Focusing on ways to improve resident well-being should remain a high priority for training programs, as provider well-being has been correlated to better patient care and decreased medical errors,2 in addition to improved resident satisfaction. Specifically, in light of the time constraints on anesthesia residents, future work should focus on identifying time-effective, convenient opportunities to expose residents to exercise-based wellness improvement strategies.
Our study has limitations. Our survey response rate was 43%, which introduces the possibility of responder bias that may have confounded our results. Specifically, a higher proportion of CA-1 residents responded to our survey compared with CA-3 residents. However, our response rates are similar to other studies21,43 and it is not clear whether non-responders would be more or less likely to exercise or demonstrate positive wellness. The question regarding resident work hours was based on self-recall and could have led to inaccurate reporting. Furthermore, the subjectivity of the wellness questions in our survey may have led to potential misinterpretation. However, wellness is inherently subjective and we used a survey tool that has been repeatedly validated29 as consistent with more involved strategies such as in-depth interviews. Additionally, while we verified our results using the median wellness score of our participants, the average wellness score of all residents is unclear, and our results would need to be confirmed through larger studies. The use of life satisfaction as a proxy measure of wellness may leave out other components of wellness. While it was created to measure the judgmental component of well-being, it may not cover all emotional aspects that contribute to wellness. However, there is no single instrument that is widely used in the literature to measure wellness. Our measurement of physical activity was dependent on accurate reporting by our participants, which opens opportunities for inaccurate reporting. Additionally, there may have been variations between what residents considered for their physical activity count; some only would have considered purposeful physical activity after hours while others may have included physical activity incurred at work. However, for this initial study, the survey used was the most efficient and cost-effective way to evaluate the relationship between physical activity and wellness. Future studies would benefit from the use of accelerometers or other means for objective reporting of physical activity. Furthermore, our survey was only sent to 6 large academic centers, and results may not be generalizable. Finally, because our data are observational only, we cannot speak to a causative relationship between exercise and wellness. It is possible that generally well residents are more motivated to exercise.
In conclusion, we found that anesthesia resident physicians who self-described as meeting USDHHS guidelines for physical fitness had an increased likelihood of better self-perceived wellness. Age, gender, and training year did not affect self-described wellness. Further work is needed to determine whether exposing anesthesia residents to fitness opportunities improves their self-described wellness and patient care.
Appendix
Appendix 1: Survey
Consent:
This survey is part of a research project studying resident wellness. Your participation in this research project is completely voluntary, and will not influence your training or evaluations in any way. By completing this survey, you are giving permission for use of your deidentified responses in aggregate form in order to evaluate influencing factors on resident wellness. Your name will not be associated with your responses in any way. The survey should take approximately 2 minutes to complete. If you have any questions about this survey or research project, you can contact Sarah Nizamuddin, MD at snizamuddin@dacc.uchicago.edu.
What is your age (in years)? ______
-
Please select your gender.
Female
Male
-
What is your CA year?
CA-1
CA-2
CA-3
-
What is the average hours you work per week?
<40 hours
40–50 hours
51–60 hours
61–70 hours
>70 hours
-
In the past week, how often have you participated in vigorous-intensity aerobic physical activity (e.g. running, swimming laps, bicycling faster than 10 mph, hiking uphill)?
<30 minutes per week
30–75 minutes per week
75–150 minutes per week
>150 minutes per week
-
In the past week, how often have you participated in moderate-intensity physical activity (e.g. brisk walking, recreational swimming, yard work)?
<30 minutes per week
30–75 minutes per week
75–150 minutes per week
>150 minutes per week
-
In the past week, how often have you engaged in muscle-strength training that worked most major muscle groups (e.g. legs, hips, back, abdomen, chest, shoulders, arms)?
Never
1 time per week
2 times per week
3 or more times per week
Below are five statements that you may agree or disagree with. Using the scale below, indicate your agreement with each item by placing the appropriate number on the line preceding that item. Please be open and honest in your responding.
7 - Strongly agree
6 - Agree
5 - Slightly agree
4 - Neither agree nor disagree
3 - Slightly disagree
2 - Disagree
1 - Strongly disagree
8. In most ways my life is close to my ideal.
9. The conditions of my life are excellent.
10. I am satisfied with my life.
11. So far I have gotten the important things I want in life.
12. If I could live my life over, I would change almost nothing.
Scoring of survey (not available to survey responders):
Items 6–8:
Meets physical activity level if: [5= c or d], [6= d], or [5+6= equivalent to 75 min vigorous or 150 min of moderate activity] AND 7= c or d.
Total equivalent minutes of physical activity= vigorous activity minutes +[moderate activity minutes/2]
Items 9–13:
-
Wellness: Add scores for questions 8–12:
▪31 - 35 Extremely satisfied
▪26 - 30 Satisfied
▪21 - 25 Slightly satisfied
▪20 Neutral
▪15 - 19 Slightly dissatisfied
▪10 - 14 Dissatisfied
▪5 - 9 Extremely dissatisfied
References
- 1.Siedsma M, Emlet L. Physician burnout: can we make a difference together? Crit Care. 2015;19(1) doi: 10.1186/s13054-015-0990-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Oliveira GS, Jr, Chang R, Fitzgerald PC et al. The prevalence of burnout and depression and their association with adherence to safety and practice standards: a survey of United States anesthesiology trainees. Anesth Analg. 2013;117(1):182–93. doi: 10.1213/ANE.0b013e3182917da9. [DOI] [PubMed] [Google Scholar]
- 3.Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet. 2009;374(9702):1714–21. doi: 10.1016/S0140-6736(09)61424-0. [DOI] [PubMed] [Google Scholar]
- 4.Sargent MC, Sotile W, Sotile MO et al. Stress and coping among orthopaedic surgery residents and faculty. J Bone Joint Surg Am. 2004;86(7):1579–86. doi: 10.2106/00004623-200407000-00032. [DOI] [PubMed] [Google Scholar]
- 5.Ramirez AJ, Graham J, Richards MA et al. Mental health of hospital consultants: the effects of stress and satisfaction at work. Lancet. 1996;347(9003):724–8. doi: 10.1016/s0140-6736(96)90077-x. [DOI] [PubMed] [Google Scholar]
- 6.Shanafelt TD, Sloan JA, Habermann TM. The well-being of physicians. Am J Med. 2003;114(6):513–9. doi: 10.1016/s0002-9343(03)00117-7. [DOI] [PubMed] [Google Scholar]
- 7.Dyrbye LN, West CP, Satele D et al. Burnout among US medical students, residents, and early career physicians relative to the general US population. Acad Med. 2014;89(3):443–51. doi: 10.1097/ACM.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 8.Dyrbye LN, Thomas MR, Massie FS et al. Burnout and suicidal ideation among US medical students. Ann Intern Med. 2008;149(5):334–41. doi: 10.7326/0003-4819-149-5-200809020-00008. [DOI] [PubMed] [Google Scholar]
- 9.Dyrbye L, Shanafelt T. A narrative review on burnout experienced by medical students and residents. Med Educ. 2016;50(1):132–49. doi: 10.1111/medu.12927. [DOI] [PubMed] [Google Scholar]
- 10.CLER Pathways to Excellence. Accessed September 19, 2019.http://www.acgme.org/Portals/0/PDFs/CLER/CLER_Brochure.pdf [Google Scholar]
- 11.Ruegsegger GN, Booth FW. Health benefits of exercise. Cold Spring Harb Perspect Med. 2018;8(7):a029694. doi: 10.1101/cshperspect.a029694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Han P, Zhang W, Kang L et al. Clinical evidence of exercise benefits for stroke. Adv Exp Med Biol. 2017;1000:131–51. doi: 10.1007/978-981-10-4304-8_9. [DOI] [PubMed] [Google Scholar]
- 13.Jhamnani S, Patel D, Heimlich L et al. Meta-analysis of the effects of lifestyle modifications on coronary and carotid atherosclerotic burden. Am J Cardiol. 2015;115(2):268–75. doi: 10.1016/j.amjcard.2014.10.035. [DOI] [PubMed] [Google Scholar]
- 14.Miller TD, Balady GJ, Fletcher GF. Exercise and its role in the prevention and rehabilitation of cardiovascular disease. Ann Behav Med. 1997;19(3):220–9. doi: 10.1007/BF02892287. [DOI] [PubMed] [Google Scholar]
- 15.Genin PM, Degoutte F, Finaud J et al. Effect of a 5-month worksite physical activity program on tertiary employees overall health and fitness. J Occup Environ Med. 2017;59(2):e3–e10. doi: 10.1097/JOM.0000000000000945. [DOI] [PubMed] [Google Scholar]
- 16.Bielak AA, Cherbuin N, Bunce D, Anstey KJ. Preserved differentiation between physical activity and cognitive performance across young, middle, and older adulthood over 8 years. J Gerontol B Psychol Sci Soc Sci. 2014;69(4):523–32. doi: 10.1093/geronb/gbu016. [DOI] [PubMed] [Google Scholar]
- 17.McKercher C, Sanderson K, Schmidt MD et al. Physical activity patterns and risk of depression in young adulthood: a 20-year cohort study since childhood. Soc Psychiatry Psychiatr Epidemiol. 2014;49(11):1823–34. doi: 10.1007/s00127-014-0863-7. [DOI] [PubMed] [Google Scholar]
- 18.Greenwood BN, Loughridge AB, Sadaoui N et al. The protective effects of voluntary exercise against the behavioral consequences of uncontrollable stress persist despite an increase in anxiety following forced cessation of exercise. Behav Brain Res. 2012;233(2):314–21. doi: 10.1016/j.bbr.2012.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Meldrum H. Exemplary physicians’ strategies for avoiding burnout. Health Care Manag (Frederick) 2010;29(4):324–31. doi: 10.1097/HCM.0b013e3181fa037a. [DOI] [PubMed] [Google Scholar]
- 20.US Department of Health and Human Services. Physical Activity Guidelines for Americans. 2nd ed. Washington, DC: US Department of Health and Human Services; 2018. [Google Scholar]
- 21.Weight CJ, Sellon JL, Lessard-Anderson CR et al. Physical activity, quality of life, and burnout among physician trainees: the effect of a team-based, incentivized exercise program. Mayo Clin Proc. 2013;88(12):1435–42. doi: 10.1016/j.mayocp.2013.09.010. [DOI] [PubMed] [Google Scholar]
- 22.Stanford FC, Durkin MW, Blair SN et al. Determining levels of physical activity in attending physicians, resident and fellow physicians and medical students in the USA. Br J Sports Med. 2012;46(5):360–4. doi: 10.1136/bjsports-2011-090299. [DOI] [PubMed] [Google Scholar]
- 23.Olson SM, Odo NU, Duran AM et al. Burnout and physical activity in Minnesota internal medicine resident physicians. J Grad Med Educ. 2014;6(4):669–74. doi: 10.4300/JGME-D-13-00396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Diener E, Emmons RA, Larsen RJ, Griffin S. The Satisfaction With Life scale. J Pers Assess. 1985;49(1):71–5. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- 25.Lebensohn P, Dodds S, Benn R et al. Resident wellness behaviors: relationship to stress, depression, and burnout. Fam Med. 2013;45(8):541–9. [PubMed] [Google Scholar]
- 26.Degges-White S. Transitions, wellness, and life satisfaction: implications for counseling midlife women. J Ment Health Couns. 2006;28(8):133–50. [Google Scholar]
- 27.Rachele JN, Cuddihy TF, Washington TL, McPhail SM. The association between adolescent self-reported physical activity and wellness: the missing piece for youth wellness programs. J Adolesc Health. 2014;55(2):281–6. doi: 10.1016/j.jadohealth.2014.01.021. [DOI] [PubMed] [Google Scholar]
- 28.Bart R, Ishak WW, Ganjian S et al. The assessment and measurement of wellness in the clinical medical setting: a systematic review. Innov Clin Neurosci. 2018;15(9–10):14–23. [PMC free article] [PubMed] [Google Scholar]
- 29.Pavot W, Diener E, Colvin CR, Sandvik E. Further validation of the Satisfaction With Life Scale: evidence for the cross-method convergence of well-being measures. J Pers Assess. 1991;57(1):149–61. doi: 10.1207/s15327752jpa5701_17. [DOI] [PubMed] [Google Scholar]
- 30.Hinz A, Conrad I, Schroeter ML et al. Psychometric properties of the Satisfaction With Life Scale (SWLS), derived from a large German community sample. Qual Life Res. 2018;27(6):1661–70. doi: 10.1007/s11136-018-1844-1. [DOI] [PubMed] [Google Scholar]
- 31.Maher JP, Pincus AL, Ram N, Conroy DE. Daily physical activity and life satisfaction across adulthood. Dev Psychol. 2015;51(10):1407–19. doi: 10.1037/dev0000037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kleszczewska D, Dzielska A, Salonna F, Mazur J. The association between physical activity and general life satisfaction in lower secondary school students: the role of individual and family factors. Community Ment Health J. 2018;54(8):1245–52. doi: 10.1007/s10597-018-0309-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pengpid S, Peltzer K. Sedentary behaviour, physical activity and life satisfaction, happiness and perceived health status in university students from 24 countries. Int J Environ Res Public Health. 2019;16(12):2084. doi: 10.3390/ijerph16122084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee B, Howard EP. Physical activity and positive psychological well-being attributes among US Latino older adults. J Gerontol Nurs. 2019;45(6):44–56. doi: 10.3928/00989134-20190426-01. [DOI] [PubMed] [Google Scholar]
- 35.Abdin S, Welch RK, Byron-Daniel J, Meyrick J. The effectiveness of physical activity interventions in improving well-being across office-based work-place settings: a systematic review. Public Health. 2018;160:70–6. doi: 10.1016/j.puhe.2018.03.029. [DOI] [PubMed] [Google Scholar]
- 36.Fox KR. The influence of physical activity on mental well-being. Public Health Nutr. 1999;2(3A):411–8. doi: 10.1017/s1368980099000567. [DOI] [PubMed] [Google Scholar]
- 37.Hemp P. Presenteeism: at work – but out of it. Harv Bus Rev. 2004;82(10):49–58. [PubMed] [Google Scholar]
- 38.Roux L, Pratt M, Tengs TO et al. Cost effectiveness of community-based physical activity interventions. Am J Prev Med. 2008;35(6):578–88. doi: 10.1016/j.amepre.2008.06.040. [DOI] [PubMed] [Google Scholar]
- 39.Hagberg LA, Lindholm L. Cost-effectiveness of healthcare-based interventions aimed at improving physical activity. Scand J Public Health. 2006;34(6):641–53. doi: 10.1080/14034940600627853. [DOI] [PubMed] [Google Scholar]
- 40.Carlson SA, Fulton JE, Schoenborn CA, Loustalot F. Trend and prevalence estimates based on the 2008 Physical Activity Guidelines for Americans. Am J Prev Med. 2010;39(4):305–13. doi: 10.1016/j.amepre.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 41.Aggarwal R, Deutsch JK, Medina J, Kothari N. Resident wellness: an intervention to decrease burnout and increase resiliency and happiness. MedEdPORTAL. 2017;13:10651. doi: 10.15766/mep_2374-8265.10651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Warburton DER, Bredin SSD. Health benefits of physical activity: a systematic review of current systematic reviews. Curr Opin Cardiol. 2017;32(5):541–56. doi: 10.1097/HCO.0000000000000437. [DOI] [PubMed] [Google Scholar]
- 43.Sun H, Warner DO, Macario A et al. Repeated cross-sectional surveys of burnout, distress, and depression among anesthesiology residents and first-year graduates. Anesthesiology. 2019;131(3):668–77. doi: 10.1097/ALN.0000000000002777. [DOI] [PubMed] [Google Scholar]


