Abstract
Background and aims
The underestimation of the severity of COVID-19 by the South African government resulted in delayed action against the pandemic. Ever since WHO declared COVID-19 a pandemic preventive action was comprehensively upgraded worldwide. This prompted South African authorities to implement physical distancing, self-isolation, closure of non-essential services, schools, travelling restrictions and recursive national lockdowns to mitigate the impact of COVID-19. This explanatory study sought to review the effects of COVID-19 in the South African health system and society.
Methods
The study applied literature research of COVID-19 reports, policies from the National Department of Health, WHO, Africa CDC, and articles from Google Scholar, Science Direct, Web of Science, Scopus and PubMed.
Results
The South African health system is affected by the lack of PPEs, increased mortality rates, mental health problems, substance abuse, resurgent of NCDs. The closure of international borders, global demand meltdown, supply disruptions, dramatic scaling down of human and industrial activities during lockdown cause socio-economic problems. The prolonged effects of lockdown on psychosocial support services resulted in the outbursts of uncertainties, acute panic, fear, depression, obsessive behaviours, social unrests, stigmatization, anxiety, increased gender-based violence cases and discrimination in the distribution of relief food aid.
Conclusion
To slow down the spread of COVID-19, massive testing must be adopted, contact tracing, isolation, and home quarantine guidelines for asymptomatic cases which promote behavioural change and reviewing of policy on food relief.
Keywords: COVID-19, Health systems, Effects, SARS-CoV-2, Case management
Highlights
-
•
The outbreak of COVID-19 pandemic affects all aspects of life, including the public health and global economy.
-
•
With no WHO-approved vaccines, the South African health system and the society are overwhelmed with the effects of COVID-19.
-
•
Integration of technology is inevitable in the South African health system to combat COVID-19 pandemic.
1. Introduction
The outbreak of novel coronavirus 2019 (COVID-2019) was first reported in Wuhan, Hubei Province, China in December 2019 [1,2], and the disease spread rapidly around the world with an incubation period of 12 days or more after exposure. The COVID-19 is contagious and can spread during the incubation period or recessive infection, making it difficult to identify suspected cases without clinical symptoms and epidemiological history. The lack of information on how COVID-19 spreads delayed COVID-19 preparedness which resulted in underestimating its severity until the World Health Organization (WHO) declared public health emergency and health crisis [[3], [4], [5]]. After that, COVID-19 prevention methods were comprehensively upgraded and this marked the beginning of universal concern; and prompted WHO to implement physical distancing and self-isolation [6].
Globally, COVID-19 cases are increasing exponentially. As of August 30, 2020, WHO reported 25,225,566 confirmed COVID-19 cases, 847,676 deaths and 17,574,888 recovered patients while African continent reported 1,237,070 cases, 29,430 deaths and 968,962 recoveries [7]. In Africa, the first imported COVI-19 case from China was reported in Egypt on the February 14, 2020 [8]. The fact that China is the largest commercial investor in Africa led to large numbers of people travelling to and from China hence o the importation of COVID-19 cases. The Africa Centres for Disease Control and Prevention (Africa CDC) in collaboration with Southern Africa Center for Infectious Disease Surveillance (SACIDS) formed Africa Taskforce on Coronavirus Preparedness and Response (AFTCOR) which consists of Health Ministries of all member states of African Union Commission [9,10]. AFTCOR together with the Africa CDC implemented prevention and containment strategies such as case management, infection prevention and control (IPC), surveillance and publicity to mitigate the spread of COVID-19 [9] and minimizing its potential impact on fragile health systems.
Therefore, this explanatory study sought to provide effects of COVID-19 in the South African health system and society. Also, the study provides an overview of South Africa COVID-19 preparedness and prevailing challenges to combat the pandemic.
2. Methods
The study applied literature search of journal articles written in English from electronic databases such as Google Scholar, Science Direct, Web of Science, Scopus and PubMed. Reports, policies and guidelines from WHO, National Institute for Communicable Diseases (NICD), South African Department of Health, World Health Organization African Region, South Africa’s COVID-19 Online portal and resources and Africa CDC were also analyzed. Articles, reports and policies were searched using the following key terms, “COVID-19” OR “SARS-CoV2” OR “Coronavirus” AND “impact of COVID-19”, “effects of COVID-19”, “novel coronavirus disease” “COVID-19 preparedness in South Africa”, “COVID-19” OR “Corona positive”, “COVID-19 policy” OR “COVID-19 guidelines”, “COVID-19 pandemic”. The literature search was done up till August 27, 2020. The study excluded information from blogs and other unverified sources. Also, the study excluded articles and reports that did not include the effects or impact of COVID-19 pandemic in South Africa.
3. Results
3.1. South Africa COVID-19 preparedness and current status
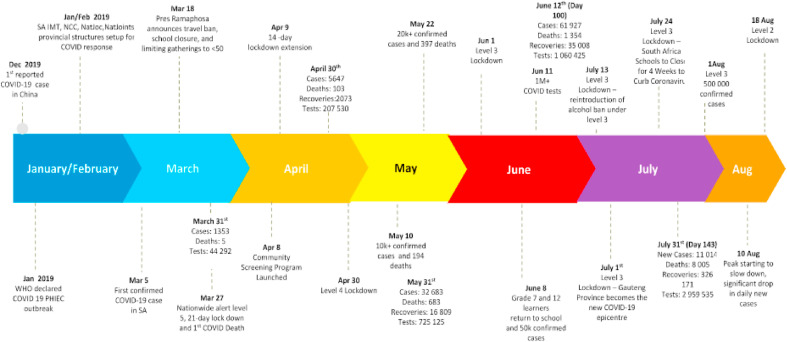
South Africa reported first imported COVID-19 cases from nine adults who returned from a holiday in Italy, where cases were rampant, on February 29, 2020 [11]. The returnees started showing flu-like symptoms which later confirmed COVID-19 positive by the reverse transcription-polymerase chain reaction on the March 5, 2020. Some of the returnees were asymptomatic but tested positive. The aftermath of imported cases prompted the President of the Republic of South Africa to declare a national state of disaster to mitigate the potential impact of COVID-19 pandemic. With increasing COVID-19 cases and no approved vaccines [12], the South Africa authorities and health system implemented drastic measures in addition to WHO recommendations and Africa CDC COVID-19 mitigation strategies and guidelines. These measures include scaling up the testing process, national total lockdown as shown in Fig. 1 , travelling restrictions internally and local (interprovincial) except workers providing essential services, bans on large gatherings (music, sports, religious and other social gatherings) as well as selling of alcohol and cigarettes, campaigns for physical distancing, practising good hygiene, implementation of curfew, stay at home, and establishment of communication protocol for the reporting cases and closure of unit or department if an employee tested positive. To strengthen COVID-19 mitigation efforts, the health system embarked on awareness campaigns, case management, infection prevention and control (IPC), surveillance, risk communication and human capacity (training in surveillance, epidemic response, and diagnostic testing kits).
Fig. 1.
Evolution of COVID-19 in South Africa and measures undertaken, Source: SAcoronavirus [13].
As of August 24, 2020, within Southern African Development Region (SADC) region, South Africa continues to record highest cumulative COVID-19 cases and account for 90% of 91% of the confirmed deaths, with fatality ratio of 7% [13]. With the high level of government commitment, COVID-19 screening and testing are decentralized to provincial, districts and sub-districts to the scaling-up testing process, coordination of action and enforcing collaboration amongst COVID-19 task teams. A series of national lockdowns and the evolution of COVID-19 in South Africa and measures undertaken are shown in Fig. 1.
3.1.1. COVID-19 awareness campaigns
Several COVID-19 awareness campaigns are intensified to fight stigmatization, anxiety and debunking myths and misinformation about COVID-19 especially the 5G technology conspiracy theory. The Ministry of Health engaged media platforms such as television, radio, social media, short messaging services (SMS), leaflets, banners and also road campaigns to create COVID-19 awareness. These platforms are engaged to teach the community about the effective ways of handwashing techniques and preventive measures such as wearing masks, sanitizing and social distancing among others.
3.1.2. Disinfection and environmental
As part of the precautionary measures, the washing of hands, as well as cleaning and disinfection of frequently touched objects and surfaces, is done especially in densely populated places including school buildings, taxi and bus ranks among others [14]. Disinfection of objects and surfaces is further extended to healthcare settings, where furniture, rooms, toilets, medical equipment and other computer peripherals in isolation and quarantine centres are often disinfected using chemical disinfectant (chlorine or alcohol). This is done to reduce pathogens on contaminated objects and surfaces.
3.1.3. Case management
The South African health system implemented temperature screening at ports of entry, laboratory testing facilities, clinical diagnosis, quarantine facilities and refurbishment of designated hospitals as COVID-19 isolation centres in each province. The isolation centres are equipped with ventilators and dexamethasone for COVID-19 patients with severe respiratory distress [13]. If someone tests positive, health workers do contact tracing and collect information about the person to determine the level of risk for COVID-19. The information includes symptoms, travel, exposure to anyone with COVID-19 infection, exposure to healthcare facilities, and details about how to contact the person.
3.1.4. Infection prevention and control
In addition to case management activities, South Africa healthcare system implements infection prevention and control to slow down the spread of COVID-19. These COVID-19 preventive measures include maintaining of physical distancing (individual and community) [15], reduction of face-to-face contact during staff meetings, wearing of N95 respirators, sterile gloves and surgical masks only for frontline healthcare workers, wearing of face masks by the general public, decontamination and disinfection of contaminated areas and objects using sanitizers. Moreover, the health system also recommends social distancing as infection prevention and control to combat COVID-19 [7] as well as risk communication and surveillance.
3.2. Effects of COVID-19 - South African perspective
3.2.1. Increased mortality rate and deaths
As of August 24, 2020, South Africa recorded 611,450 cumulative confirmed COVID-19 cases and 13,226 deaths from March 2020, and national case fatality rate of 2, 2% based on deaths from August 24, 2020 reflecting an increase of new deaths [13]. The deaths are attributed to limited access to medical care especially for women that are in need for antenatal and postnatal care services as more women deliver at home. Also, more attention is given to COVID-19 which prompts the resurgence of other deadly non-communicable diseases (NCDs) during the lockdown. This burdens the government and the communities as the number of children requiring social support increases. The death of the breadwinner of the family caused hardships, hunger and pain especially in the vulnerable families that are living below the poverty line. Although the estimated fatality rate is inclusive of people who already had underlying conditions, however, more precise information of infected individuals that include asymptomatic or minimally symptomatic cases would make precise fatality rate [16]. Again, it is unclear how many people have died of COVID-19 in areas including rural settlers, where testing is not intensified or people avoiding seeking medical care for fear of getting infected or stigmatization.
3.2.2. Mental health and substance abuse
The uncertainty of COVID-19 pandemic threatens both people’s physical health and affect people’s mental health [5]. Once someone experiences pneumonia-like symptoms, the close relatives are likely to develop negative emotions and avoidant behaviours by avoiding contact with the person and affect their mental health. In addition to that, high infectivity, unemployment and fatality rates, financial losses, continuous lockdowns, forced quarantine, restrictions on the movement of people caused by COVID-19 [17], significantly change the daily lives and ultimately lead to mental health problems and substance abuse. This brought uncertainties, acute panic, fear of contracting the virus, obsessive behaviours, post-traumatic stress disorder, stigmatization, anxiety, depression, hoarding among others. These problems have increased drastically as evidenced by the increased number of reported gender-based violence cases in South Africa fueled by restrictive access to psychosocial support services and lack of financial support [18]. The prolonged effects of COVID-19 on psychosocial support services resulted in the outbursts of riotous acts, racism, stigmatization, and xenophobia against communities with high COVID-19 cases and discrimination in the distribution of COVID-19 relief food aid.
3.2.3. Closure of schools and universities
South African government announced the temporary closure of schools and universities to reduce the spread of the COVID-19 pandemic [19]. The suspension of teaching and learning activities affect learning and the academic calendar and implies less economic opportunities and human capital in the future as well as the increasing number of teenage marriages. However, the Government through the Ministry of Education implemented strategies such as practising social distancing, limiting the number of learners and students at schools and universities (completing students) [20]. Despite the closure of the schools, the Department of Basic Education (DBE) introduced online learner support programmes such as COVID-19 Television and radio curriculum support programmes for learners. Institutions in Higher Education and Training adopted online learning facilities (blended learning) such as Learning Management Systems (Moodle), as wells as social media platforms such as WhatsApp [21] and video-conferencing platforms such as Zoom, Skype and Microsoft Teams among others. However, teaching and learning practicals and labs remain a daunting task especially in the medical field, engineering and science practical-oriented courses during the lockdown period. Also, the digital divide among students is another limitation to facilitate blended learning.
3.2.4. Increasing cases of gender-based violence (GBV)
Gender-based violence cases continue to increase rapidly amid COVID-19, especially violence against women [22]. This is evident with received 120,000 calls by the South African National helpline from victims of gender-based violence within three weeks [23]. With this upsurge, it is evident that South Africa battles another deadly epidemic of domestic violence amidst the coronavirus lockdown. Sadly, some perpetrators of GBV are the breadwinners of the family [24]; therefore, victims find themselves in juxtaposition, whether to report their perpetrators or keep silent for food. Measures to deal with rampant cases of GBV together with mental health and substance abuse must be enforced. Programmes to assist victims must be accessible, remain open and treated as part of essential services; these include shelters, helplines, and place of safety and counselling services and be afforded necessary financial, political support, provision of rehabilitation and psychosocial support services during COVID-19.
3.2.5. Business implications of COVID-19 socio-economic issues
The closure of borders, global demand meltdown, supply disruptions, sharp depreciation of currencies, a sharp decline in share prices and commodity prices (Brent crude oil price), flights as well as dramatic scaling down of human and industrial activities during COVID-19 causes socio-economic crisis in South Africa and globally. China, the major supplier of inputs for manufacturing and production industries stopped shipping out of goods which tremendously affected business operations in South Africa. Several sectors of the economy have been disrupted with the COVID-19 pandemic [12]. This inflicts high and rising human costs and daily expenditure because of depreciating exchange rates and supply shortages and poses risk to the near term inflation outlook as well as fiscal positions and debt trajectories.
3.2.6. Increased social unrest and demonstration
With continued travelling restrictions, poverty and national lockdowns without sustainable COVID-19 relief food aid, social unrests [25], confrontation, shop looting [26] and obsessive behaviours are inevitable because of lack of food supply, loss of income, panic, and anxiety, especially in the informal settlement [24]. Loss of employment, which is the main source of income for many informal settlers, is a psychological blow with knock-on effects on entire households and families concerned, as one income earner typically supports extended family members. Social unrests have posed new challenges to combat COVID-19 pandemic as an imposition of contact tracing and social distancing become difficult.
3.2.7. A sudden change of lifestyle and reduced physical activity levels
Due to reduced physical activities and active intake of snacks especially in quarantine and isolation centres results in weight gain which poses diabetes-related complications [27]. This is exacerbated with limited movements and access to the gym facilities, controlled movements which further restricts outdoor and open space physical exercises. Reduced physical activities, restricted access to entertainment, loneliness and weight gain increases health risk factors such as obesity [16], hypertension, cardiorespiratory and mental health disorders among others. This could prompt a resurgence of non-communicable diseases during or post COVID-19.
3.3. Challenges faced with South African health systems in tackling COVID-19 pandemic cases
Despite the impact of COVID-19 in Africa, there is a paucity of healthcare professionals worldwide, especially in developing countries (World Health Organisation 2013). This serious impediment to healthcare progress is influenced by factors such as brain drain, shortage healthcare training and educational facilities [28]. In many countries, the deficit is even caused and exacerbated by the disproportionate distribution of healthcare professionals in rural and urban areas. The World Health Organisation (WHO) estimated a deficit of skilled healthcare professionals globally because of population growth [29]. The concern of inadequate healthcare staffing levels was raised many years ago in the World Health Report 2013, which described the global shortage as a “crisis” then. The situation is even more critical today amid COVID-19 since nurses are part of the front-line healthcare professionals. The push factors such as poor remuneration and poor working conditions fueled the shortage of skilled medical doctors and nurses through cross-border migration of health workers to developed economies [30,31].
South African health system is overwhelmed with COVID-19 pandemic in addition to the existing challenges in healthcare service delivery. Despite significant progress in the South African health system since 1994, the country faces challenges in healthcare service delivery which include lack of funding and insufficient budget [32], environmental change [33] and unequal distribution of resources (including health facilities, healthcare workers, inadequate production, and inadequate recruitment especially in rural areas, for both the public sector and private sector [34]. Other challenges include slow progress in restructuring the healthcare system [35,36], Increased disease burden [34], management and leadership crisis caused by poor leadership and inadequate management, and reflected in a lack of vision, lack of clear philosophy and poor goal setting in the healthcare sector [37,38]. Ensuring universal access to skilled, motivated and supported health workers, especially in remote and rural communities is a challenge because of the existing health facilities disparities between urban and remote areas [39,40]. In addition to these challenges, South African health system is plagued with acute shortage of personal protective equipment (PPE) such as face shield or goggles, heavy-duty apron and gloves, as well as N95 respirators for frontline healthcare professionals due to disruptions in the global supply chain of medical equipment. Shortage of equipped health facilities and PPE for COVID-19 healthcare workers, patients and suspected individuals in quarantine and self-isolation centres increased chances of infection of healthcare workers [13]. In addition to that, striking a balance providing essential healthcare to COVID-19 patients and protecting healthcare workers from infection, especially in the face increasing healthcare workers infections due to lack of PPEs is a challenging task for the COVID-19 response team. The situation is exacerbated by rampant corruption, abuse of funds allocated to fight COVID-19, lack of PPE local reprocessing companies that can manufacture PPEs due to huge capital investment required, which is not always available in most African countries including South Africa.
3.4. South African perspective- COVID-19 research opportunities and themes
Fighting COVID-19 pandemic brought new multidisciplinary research opportunities for sustainable solutions globally. For instance, Vaishya [41], Pan [42], Lalmuanawma [43] and Ting [44] highlighted how emerging and digital technologies could mitigate COVID-19 in terms of identification, detecting, screening, drugs development as well monitoring COVID-19 patients and contact-persons. In addition to the existing research opportunities highlighted by Vaishya [41], Pan [42], Lalmuanawma [43], Ting [44], Table 1 illustrate research opportunities for integrating emerging technologies that can alleviate the effects of COVID-19 in South African health systems and society.
Table 1.
Research opportunities amid COVID-19.
| Research Themes | Opportunity for integrating emerging technologies |
|---|---|
| Physical distancing and social distancing | •There is a need for low-cost preventive technology-based measures to monitor and improve physical distancing and social distancing especially in social and religious gatherings, bus ranks, cities and towns. •Developing strategic ways and technologies of engaging communities including people living in resource-constrained areas to educate them about the Coronavirus, preventive measures, mental health issues and provision of counselling services |
| Mental health and Substance Abuse | •Find ways of integrating modern technologies in providing mental health services to the affected people while maintaining physical distancing and social distancing •Integration of smart apps for remote monitoring of human activity and recognition |
| Contact Tracing | •There is a need for developing low-cost and adaptive contact tracing apps for monitoring and tracing COVID-19 patients and close contacts while enforcing security and privacy of health data •Integration of Geographical Information System (GIS) technology into contact tracing apps for monitoring migration patterns of patients and contact-persons. This technology can be used for mapping COVID-19 hotspots areas for effective and efficiency allocate of resources to combat the pandemic •Integration of Internet of Things and big data into contact tracing apps for real-time access, sharing, storing and processing of COVID-19 data to disseminate insightful patterns from the data for the decision-making process. •Ways of creating a balance in contact tracing apps between containment of COVID-19 and security and privacy of health data |
| Gender-Based Violence | •Integration of mobile applications (apps) in reporting GBV cases •Big data to store names of GBV perpetrators and remotely monitor their behaviour •Integration of Internet of Things and mobile apps for remote counselling and virtual consultations of GBV victims •GIS technology to monitor the migration patterns GBV perpetrators •Intensify “Stop Gender-based Violence” campaigns on radio, instant messaging, SMS, teleconferences, television and evaluate the effectiveness of these platforms •Find strategies to involve vulnerable women living in resource-constrained areas in South Africa |
4. Conclusion
COVID-19 pandemic presents unprecedented and catastrophic effects in the South African health system, society and the economy. Continued national lockdowns have affected the GDP of the country and makes it imperative for the government at all levels to reassess and re-evaluate the effects of lockdown as the pandemic unfolds. Social protection and provision of basic services remain vital mitigation strategies, especially for the vulnerable populace. However, to slow down the spread of COVID-19, massive testing must be adopted [27], crafting of policy for food relief, contact tracing programmes [6], isolation activities as well as home quarantine guidelines for asymptomatic cases which promote behavioural change. Integration of emerging technologies in fighting COVID-19 in South Africa is inevitable as the country moves from one lockdown level to another. However, security and privacy [6] should be carefully observed when integrating digital technologies to combat COVID-19 pandemic to avoid violating people’s rights.
Funding
No funding
Declaration of competing interest
None.
References
- 1.Zhu Hengbo, Li Wei, Niu Ping. The novel coronavirus outbreak in Wuhan, China. Global Health Res Pol. 2020;5(6):1–3. doi: 10.1186/s41256-020-00135-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singhal Tanu. A review of coronavirus disease-2019 (COVID-19) Indian J Pediatr. 2020;87(4):281–286. doi: 10.1007/s12098-020-03263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jef Akst. WHO comments breed confusion over asymptomatic spread of COVID-19. 2020. https://www.the-scientist.com/news-opinion/who-comments-breed-confusion-over-asymptomatic-spread-of-covid-19-67626 [Online]
- 4.Meng L., Hua F., Bian Z. Coronavirus disease 2019 (COVID-19): emerging and future challenges for dental and oral medicine. J Dent Res. 2020;99(5):481–487. doi: 10.1177/0022034520914246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li Sijia, Wang Yilin, Jia Xue, Zhao Nan, Zhu Tingshao. The impact of COVID-19 epidemic declaration on psychological consequences: a study on active weibo users. Int J Environ Res Publ Health. 2020;17(6):1–19. doi: 10.3390/ijerph17062032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elliot Mbunge. Diabetes & metabolic syndrome. Clinical Research & Reviews; August 2020. Integrating emerging technologies into COVID-19 contact tracing: opportunities, challenges and pitfalls; pp. 1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Africa C.D.C. 2020, August. https://africacdc.org/covid-19/#https://africacdc.org/covid-19/# [Online]
- 8.Gilbert Marius. Preparedness and vulnerability of African countries against importations of COVID-19: a modelling study. Lancet. March 2020;395(10227):871–877. doi: 10.1016/S0140-6736(20)30411-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ayinla, Issideen Osseni. COVID-19 pandemic in sub-Saharan Africa: preparedness, response, and hidden potentials. Trop Med Health. June 2020;48(48):1–3. doi: 10.1186/s41182-020-00240-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Massinga, Marguerite Loembé. COVID-19 in Africa: the spread and response. Nat Med. June 2020;26(13):999–1003. doi: 10.1038/s41591-020-0961-x. [DOI] [PubMed] [Google Scholar]
- 11.Shaheen Mehtar. Limiting the spread of COVID-19 in Africa: one size mitigation strategies do not fit all countries. Lancet Glob Health. July 2020;8(7):881–883. doi: 10.1016/S2214-109X(20)30212-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ahmad Lone Shabir, Ahmad Aijaz. COVID-19 pandemic – an African perspective. Emerg Microb Infect. June 2020;9(1):1300–1308. doi: 10.1080/22221751.2020.1775132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.sacoronavirus South Africa covid-19 experiences to date. 2020, August. https://sacoronavirus.co.za/2020/08/25/slideshow-south-africa-covid-19-experiences-to-date-25th-august-2020/ (25th August 2020). [Online]
- 14.Nxumalo Sakhiseni. KZN municipalities start disinfecting programme. 2020, April. https://www.iol.co.za/mercury/news/kzn-municipalities-start-disinfecting-programme-46483366 [Online]
- 15.UNICEF COVID-19 impact assessment and outlook on personal protective equipment. 2020, May. https://www.unicef.org/supply/stories/covid-19-impact-assessment-and-outlook-personal-protective-equipment [Online]
- 16.Palmer Katie. The potential long-term impact of the COVID-19 outbreak on patients with non-communicable diseases in Europe: consequences for healthy ageing. Aging Clin Exp Res. May 2020;32(12):1189–1194. doi: 10.1007/s40520-020-01601-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dubey Souvik. Psychosocial impact of COVID-19. Diab Metab Syndr: Clin Res Rev. September 2020;14(5):779–788. doi: 10.1016/j.dsx.2020.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gould Chandré. Gender-based violence during lockdown: looking for answers. Sabinet. July 2020;113(7):56–57. [Google Scholar]
- 19.Hassan Isilow. South Africa orders schools closed as COVID-19 spreads. 2020, March. https://www.aa.com.tr/en/africa/south-africa-orders-schools-closed-as-covid-19-spreads/1767271 [Online]
- 20.Mhlanga David, Moloi Tankiso. COVID-19 and the digital transformation of education: what are we learning on 4IR in South Africa? Educ Sci. July 2020;10(80):1–11. [Google Scholar]
- 21.Umviligihozo Gisele. Sub-Saharan Africa preparedness and response to the COVID-19 pandemic: a perspective of early career African scientists. Wellcome Open Res. September 2020;1(1):1–5. doi: 10.12688/wellcomeopenres.16070.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fidelis Udo. COVID-19 lockdown: South Africa battles the deadly epidemic of gender-based violence. 2020, May. https://www.africanwomeninlaw.com/post/covid-19-lockdown-south-africa-battles-the-deadly-epidemic-of-gender-based-violence [Online]
- 23.Mlambo Sihle. SAPS received 87 000 gender-based violence calls during first week of lockdown - Cele. 2020, April. https://www.iol.co.za/news/south-africa/saps-received-87-000-gender-based-violence-calls-during-first-week-of-lockdown-cele-46024648 [Online]
- 24.Nancy Stiegle, Jean-Pierre Bouchard. Annales Médico-psychologiques, revue psychiatrique; May 2020. South Africa: challenges and successes of the COVID-19 lockdown. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mbunge E., Vheremu F., Kajiva K. A tool to predict the possibility of social unrest using sentiments analysis-case of Zimbabwe politics 2017-2018. Int J Sci Res. 2020;6(10) [Google Scholar]
- 26.Wendell Roelf. Crowds loot trucks in Cape Town a month into COVID-19 lockdown. 2020, April. https://www.reuters.com/article/us-health-coronavirus-safrica-looting/crowds-loot-trucks-in-cape-town-a-month-into-covid-19-lockdown-idUSKCN22526W [Online]
- 27.Awadhesh Kumar Singh, Misra Anoop. Diabetes & metabolic syndrome. Clinical Research & Reviews; August 2020. Impact of COVID-19 and comorbidities on health and economics: focus on developing countries and India; pp. 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen Lincoln. Striking the right balance: health workforce retention in remote and rural areas. Bull World Health Organ. 2010;88(5):323–A. doi: 10.2471/BLT.10.078477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.WHO Global health workforce shortage to reach 12.9 million in coming decades. 2013, November. https://www.who.int/mediacentre/news/releases/2013/health-workforce-shortage/en/ [Online]
- 30.Christopher Aluttis, Tewabech Bishaw, Frank Martina. The workforce for health in a globalized context global shortages and international migration. Glob Health Action. 2014;7(23611):1–7. doi: 10.3402/gha.v7.23611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hazel, Mumbo Miseda, Odhiambo Were Samuel, Anne Murianki, Peter Cirindi, Milo Mutuku, Mutwiwa Stephen N. The implication of the shortage of health workforce specialist on universal health coverage in Kenya. Hum Resour Health. June 2017;15(80):12–22. doi: 10.1186/s12960-017-0253-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.B Malakoane C., Heunis J., Chikobvu P.G., Kigozi N., H Kruger W. Public health system challenges in the Free State, South Africa: a situation appraisal to inform health system strengthening. BMC Health Serv Res. January 2020;20(58):1–14. doi: 10.1186/s12913-019-4862-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Whiteside Alan. South Africa’s key health challenges. Ann Am Acad Polit Soc Sci. March 2014;652(134):166–185. [Google Scholar]
- 34.Winnie Maphumulo and R., Busisiwe Bhengu. Challenges of quality improvement in the healthcare of South Africa post-apartheid: a critical review. Curationis. May 2019;42(1):1–9. doi: 10.4102/curationis.v42i1.1901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gray A., Vawda Y. health legislation and policy-South African health review. 2018, November. https://www.hst.org.za/publications/South%20African%20Health%20Reviews/SAHR%202018.pdf [Online]
- 36.Coovadia Hoosen, Rachel Jewkes, Peter Barron, Sanders David, Diane McIntyre. The health and health system of South Africa: historical roots of current public health challenges. Lancet. September 2009;374(9692):817–834. doi: 10.1016/S0140-6736(09)60951-X. [DOI] [PubMed] [Google Scholar]
- 37.Pillay-van Wyk Victoria Mortality trends and differentials in South Africa from 1997 to 2012: second national burden of disease study. The Lancet Global Health. September 2016;4(9):642–653. doi: 10.1016/S2214-109X(16)30113-9. [DOI] [PubMed] [Google Scholar]
- 38.Carney Marie. Public health nurses perception of clinical leadership in Ireland: narrative descriptions. J Nurs Manag. May 2009;17(4):435–445. doi: 10.1111/j.1365-2834.2009.01015.x. [DOI] [PubMed] [Google Scholar]
- 39.Versteeg Marije, Lilo du Toit, Couper Ian Building consensus on key priorities for rural health care in South Africa using the Delphi technique. Glob Health Action. June 2013;6(5):119–126. doi: 10.3402/gha.v6i0.19522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McLaren Zoë M., Cally Ardington, Murray Leibbrandt. Distance decay and persistent health care disparities in South Africa. BMC Health Serv Res. November 2014;14(541):1–17. doi: 10.1186/s12913-014-0541-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Raju Vaishya, Mohd Javaid, Ibrahim HaleemKhan, Abid Haleem. Artificial Intelligence (AI) applications for COVID-19 pandemic. Diab Metab Syndr: Clin Res Rev. July–August 2020;14(4):337–339. doi: 10.1016/j.dsx.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shan L Pan, Zhang Sixuan. International Journal of Information Management; July 2020. From fighting COVID-19 pandemic to tackling sustainable development goals: an opportunity for responsible information systems research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lalmuanawma Samuel, Jamal Hussain, Lalrinfela Chhakchhuak. Applications of machine learning and artificial intelligence for Covid-19 (SARS-CoV-2) pandemic: a review. Chaos, Solit Fractals. October 2020;139(13):1–15. doi: 10.1016/j.chaos.2020.110059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Daniel Shu, Ting Wei, Lawrence Carin, Victor Dzau, Wong Tien Y. Digital technology and COVID-19. Nat Med. March 2020;26(21):459–461. doi: 10.1038/s41591-020-0824-5. [DOI] [PMC free article] [PubMed] [Google Scholar]