Abstract
Purpose
To evaluate associations between counties’ COVID-19 cases and racial-ethnic and nativity composition, considering heterogeneity across Latin American-origin subgroups and regions of the United States.
Methods
Using county-level data and multilevel negative binomial models, we evaluate associations between COVID-19 cases and percentages of residents that are foreign-born, Latinx, Black, or Asian, presenting estimates for all counties combined and stratifying across regions. Given varying risk factors among Latinx, we also evaluate associations for percentages of residents from specific Latin American-origin groups.
Results
Percentage of foreign-born residents is positively associated with COVID-19 case rate (IRR = 1.106; 95% CI: 1.074–1.139). Adjusted associations for percentage Latinx are nonsignificant for all counties combined, but this obscures heterogeneity. Counties with more Central Americans have higher case rates (IRR = 1.130; 95% CI: 1.067–1.197). And, in the Northeast and Midwest, counties with more Puerto Ricans have higher case rates. Associations with percentage Asians are nonsignificant after adjusting for percentage foreign-born. With the confirmation of prior evidence, the percentage of Black residents is positively and robustly associated with COVID-19 case rate (IRR = 1.031; 95% CI: 1.025–1.036).
Conclusions
Counties with more immigrants, as well as more Central American or Black residents, have more COVID-19 cases. In the Northeast and Midwest, counties with more Puerto Rican residents also have more COVID-19 cases.
Keywords: COVID-19, Disparities, Immigrant communities, Latinx communities
The COVID-19 epidemic in the United States (U.S.) is unfolding onto multifaceted social, health, and geographic inequities. Individual-level data from selected locations show that Black Americans are substantially overrepresented among those infected and dying [[1], [2], [3], [4]]. Individual-level data from New York state also show elevated infections among Latinos/as (hereafter, Latinx) [5]. Lacking information on COVID-19 patients’ race-ethnicity, some authors have sought a broader national-level picture with county-level analyses. Millett and colleagues show that counties with large shares of Black residents (>13%) account for more than half of COVID-19 cases and deaths nationwide [6]. Another study shows positive pairwise correlations between COVID-19 and percentages of Black or Asian residents in counties [7]. Recent newspaper reports have also included descriptive evidence of rising cases in counties with more Latinx residents [8]. While county-level analyses are motivated in part by insufficient information on individual-level race-ethnicity in COVID-19 data, it is important to not downplay the significance of geography and local populations as meaningful determinants of health. As part of systemic racism, racial-ethnic and socioeconomic hierarchies spatially concentrate and segregate (dis)advantaged individuals, which, in turn, creates inequities in area-level risks and resources (e.g., poverty, health care access, etc.), which can impact both individual and community health outcomes [[9], [10], [11], [12], [13]].
Building on this growing evidence, we explore previously understudied questions about disparities in COVID-19 burden across communities with larger immigrant and Latinx populations, while also supplementing prior evidence on disparities across Black and Asian communities. Using county-level data and multilevel negative binomial models, we evaluate associations between COVID-19 cases and percentages of residents that are foreign-born, Latinx, Black, or Asian, stratifying across U.S. regions. Risk factors for COVID-19 differ substantially within the pan-ethnic category of Latinx; we, therefore, explore county-level disparities across Latin American-origin subgroups.
Compared to U.S. born whites, Latinx and foreign-born populations in the U.S. face elevated rates of sociodemographic and area-level risk factors that may increase COVID-19 exposure and limit access to health care—most notably, segregation, concentrated poverty, poorer quality housing, and crowding [[14], [15], [16], [17], [18]]. On the other hand, Latinx and foreign-born individuals have lower rates of underlying conditions that complicate COVID-19 (particularly heart disease), relative to white or Black native-born Americans [19]. While county-level data do not allow for the parsing of ethnicity and nativity, it is worth noting that Latin American and Asian countries account for the majority of immigrants in the U.S., with Mexico alone accounting for 25% [20]. Heterogeneity in risk factors across Latinx-origin subgroups may further lead to distinct patterns of geographic disparities in COVID-19 [[21], [22], [23]]. Poverty rates among Mexicans, Puerto Ricans, and Central Americans are approximately 25%–30%, roughly double those for Cubans and South Americans [[24], [25], [26]]. Puerto Ricans also have higher rates of chronic disease [27,28], relative to other Latin American subgroups or whites, and face high rates of residential segregation, particularly in the Northeast and Midwest [17].
Associations between COVID-19, geography, nativity, and race-ethnicity may also emerge differently across regions of the U.S. Early stages of the pandemic were concentrated in the Northeast and West, potentially creating more opportunity for disparities to take hold in these areas, particularly in advance of testing and mitigation efforts [29]. Racial-ethnic groups and immigrants are also differentially distributed across regions. The largest share of Black Americans is in the South, while Asian Americans are more concentrated on the coasts of the country [30,31]. Latinx Americans, as a pan-ethnic group, are concentrated in the West and South, although this primarily reflects the clustering of Mexican Americans along the U.S./Mexico border. Central Americans (excluding Mexicans) tend to live in the Atlantic Coastal Plain and the Midwest. By contrast, Cubans and Puerto Ricans are concentrated in Florida and the Northeast [32]. Finally, about two-thirds of immigrants live in the West and South, roughly one-fifth in the Northeast, with the remainder in the Midwest [20].
This study goes beyond current literature by exploring how counties’ COVID-19 cases are associated with nativity and racial-ethnic compositions, with an emphasis on how these associations vary across regions and within the pan-ethnic category of Latinx.
Methods
Study population/data sources
To analyze all contiguous counties in the U.S. (n = 3106), we compiled a dataset from several sources: (i) 2019 County Health Rankings and Roadmaps (CHRR), which synthesizes multiple sources of national health surveillance data covering 2015–2018 from government agencies [33]; (ii) 2014–2018 American Community Survey (ACS) 5-year estimates, an annual survey of sociodemographic information through the U.S. Census Bureau [34]; (iii) the 2017 Chronic Conditions Data Warehouse (CCDW) produced by the Center for Medicare and Medicaid Services [35]; (iv) the 2018–2019 Area Health Resource File (AHRF) managed by the U.S. Health Resources and Services Administration [36], and (v) USAFacts COVID-19 counts compiled from the CDC and local government agencies [37]. Sources in brackets below.
Outcome
The outcome is the total number of confirmed COVID-19 cases in a county as of May 28, 2020. [USAFacts].
Racial-ethnic and nativity composition
We consider the percentages of Blacks, Asians, Latinx, and foreign-born residing in a county. In additional models, percentage Latinx is replaced with separate indicators for the percentage of Mexicans, Puerto Ricans, Cubans, Central Americans, South Americans, and other Latinx-origin. (In the ACS data, estimates for Latinx subgroups are missing in 14 counties where the numbers of sampled cases are too small. In the analyses shown here, these missing values are replaced with 0 given that the population of the Latinx subgroups is small in these counties. As a sensitivity test, models excluding these counties are also estimated. There was no difference in results with these two approaches.) [ACS].
County control variables
Population density reflects the total population divided by the land area of a county (in square miles). We log-transformed this variable to avoid multicollinearity and singularity in the analysis [ACS].
Age and sex composition are measured with three variables: percentage of females, percentage of age 19–64 (working age), and percentage of 65 and over [ACS].
Socioeconomic conditions are measured with two variables: the unemployment rate and logged median household income [ACS].
Economic inequality and racial-ethnic segregation are measured with three variables: the ratio of the 20th and 80th percentiles of income in a county and two dissimilarity indices capturing White/Black and White/non-White segregation [ACS]. Dissimilarity indices measure the percentage of one group that would have to move across neighborhoods to be distributed similarly to the second group [17].
Commuting and living patterns are measured with three variables: percentage using public transportation for work; the average household size, and percentage of households having at least one of the following severe housing problems: (i) being without complete kitchen facilities, (ii) being without complete plumbing, (iii) overcrowded (i.e., more than one person per room), and (iv) housing cost being > 50% of income [ACS & CHRR].
Chronic disease is measured with an index that captures chronic disease burden among residents 65+ [CCDW]. We applied principal component analysis (PCA) to four variables, specifically the percentages of elders with kidney disease, chronic obstructive pulmonary disease, diabetes, and hypertension. Higher scores indicate more disease burden. The PCA results suggest that one factor is sufficient, as it explains almost 80% of the variation among these variables.
Healthcare shortage is measured with a dichotomous variable coded one if some or all of the ZIP codes in the county have less than one primary care provider per 3500 residents [AHRF]. We also adjust for the percentage of uninsured in the county [ACS].
Models are also adjusted for the number of days since the first case in the county, with both linear and squared terms, to account for possible confounding from longer epidemics in coastal and urban areas with more minority and immigrant residents. [USAFacts].
Statistical analysis
We estimate multilevel negative binomial regression models for count data. To adjust for the population-at-risk, we use the logged total population as the offset, allowing us to interpret the outcome as a rate. We include random state-level intercepts to adjust for state-level clustering and use Huber White Sandwich estimation for standard errors.
Our analysis proceeds as follows. First, we estimate models that include only variables measuring racial-ethnic composition, adjusting for time since the first case (model 1). Second, we add to the model percentage of foreign-born (model 2). Third, we estimate a fully adjusted model that adds all the aforementioned variables (model 3). Fourth, we replicate the fully adjusted model, replacing the percentage of Latinx measures with percentages for distinct Latinx-origin groups (model 4). We then replicate models 3 and 4, stratifying across regions (i.e., replicating for regional subsets from the Northeast, Midwest, South, and West).
Results
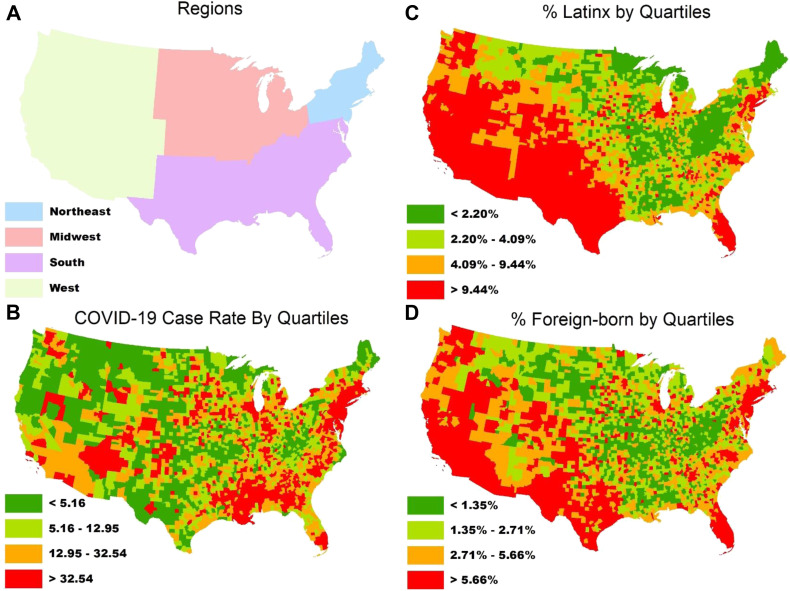
Table 1 presents means for contiguous U.S. counties, by region. Figure 1 shows distributions of key variables. As of May 28, 2020, the average county had 30 COVID-19 cases per 10,000 residents, with the Northeast having the highest mean value (58) and a concentration of higher quartile values (Fig. 1, B). An average county has 9% Latinx; however, the means and concentrations of Latinx are highest in the West and South (18.3% and 10.6% means respectively, see also Fig. 1, C). The average county is 4.7% foreign-born, and immigrants are spatially clustered in the Northeast and West (~7% means, see also Fig. 1, D). Mexicans are the biggest Latinx subgroup, with the largest percentage of values in the West and South. The percentage of Puerto Ricans and the percentage of South Americans are highest in the Northeast, while the percentage of Cubans and the percentage of Central Americans are highest in the South and Northeast.
Table 1.
Means for racial-ethnic and nativity composition, COVID-19 outcomes, and risk factors for contiguous counties in the United States, by region
| Variable | All counties (n = 3106) | Northeast (n = 216) | Midwest (n = 1055) | South (n = 1422) | West (n = 413) |
|---|---|---|---|---|---|
| Total COVID-19 cases∗ | 548.024 (3075.068) | 3471.417 (8654.146) | 317.953 (2528.075) | 293.209 (1060.792) | 484.150 (2665.677) |
| COVID-19 cases per 10,000∗ | 30.190 (60.166) | 57.870 (75.249) | 25.633 (57.780) | 32.893 (63.657) | 18.048 (34.369) |
| Percentage of Blacks | 9.025 (14.371) | 5.057 (6.342) | 2.544 (4.571) | 16.668 (17.874) | 1.344 (1.882) |
| Percentage of Asians | 1.400 (2.405) | 2.780 (3.796) | 1.060 (1.464) | 1.195 (1.774) | 2.251 (4.193) |
| Percentage of of Latinx | 9.328 (13.731) | 6.758 (8.169) | 4.639 (5.793) | 10.600 (15.731) | 18.270 (17.354) |
| Percentage of Mexicans | 6.941 (12.258) | 1.057 (1.240) | 3.544 (4.960) | 8.277 (14.870) | 14.091 (14.171) |
| Percentage of Puerto Ricans | 0.566 (1.355) | 2.616 (3.236) | 0.271 (0.441) | 0.559 (1.237) | 0.271 (0.292) |
| Percentage of Cubans | 0.157 (0.793) | 0.217 (0.351) | 0.075 (0.179) | 0.225 (1.142) | 0.100 (0.254) |
| Percentage of Central Americans | 0.546 (1.237) | 0.691 (1.212) | 0.340 (1.033) | 0.686 (1.431) | 0.514 (0.890) |
| Percentage of South Americans | 0.255 (0.687) | 0.873 (1.662) | 0.108 (0.202) | 0.268 (0.693) | 0.261 (0.314) |
| Percentage of Other Latinx-origin | 0.856 (3.137) | 1.303 (2.502) | 0.287 (0.350) | 0.579 (0.819) | 3.030 (7.894) |
| Percentage of Foreign born | 4.675 (5.650) | 7.176 (8.091) | 2.922 (3.454) | 4.794 (5.556) | 7.438 (7.111) |
| Total population (log) | 10.282 (1.476) | 11.686 (1.259) | 9.935 (1.398) | 10.332 (1.303) | 10.264 (1.841) |
| Days since the first case | 58.669 (20.206) | 71.486 (8.690) | 53.606 (21.933) | 60.833 (15.983) | 57.453 (27.502) |
| Population density (log) | 3.818 (1.749) | 5.342 (1.673) | 3.491 (1.582) | 4.154 (1.510) | 2.696 (2.043) |
| Percentage of age 18 and below | 22.337 (3.398) | 19.946 (2.371) | 22.645 (3.056) | 22.412 (3.190) | 22.540 (4.671) |
| Percentage of age 19–64 | 59.217 (3.746) | 61.663 (2.757) | 58.255 (3.524) | 59.719 (3.567) | 58.666 (4.406) |
| Percentage of age 65 and over | 18.446 (4.511) | 18.392 (3.085) | 19.100 (4.178) | 17.869 (4.434) | 18.793 (5.797) |
| Percentage of females | 49.933 (2.215) | 50.395 (1.770) | 49.811 (1.514) | 50.193 (2.586) | 49.111 (2.317) |
| Median household income (log) | 10.777 (0.241) | 10.951 (0.228) | 10.831 (0.183) | 10.692 (0.251) | 10.839 (0.240) |
| Income inequality (80/20 ratio) | 4.524 (0.740) | 4.543 (0.648) | 4.184 (0.566) | 4.810 (0.757) | 4.397 (0.719) |
| Unemployment rate | 5.227 (1.817) | 5.063 (1.285) | 4.547 (1.488) | 5.714 (1.790) | 5.377 (2.295) |
| White/non-White segregation | 27.515 (15.789) | 37.933 (12.157) | 27.252 (17.277) | 27.464 (14.134) | 22.914 (16.452) |
| White/Black segregation | 29.833 (25.496) | 48.056 (23.979) | 24.345 (28.691) | 31.968 (19.841) | 26.973 (29.326) |
| Chronic disease index | 0.000 (1.780) | 0.184 (0.864) | –0.480 (1.778) | 0.840 (1.318) | –1.762 (1.806) |
| Average household size | 2.515 (0.261) | 2.467 (0.222) | 2.415 (0.230) | 2.576 (0.226) | 2.587 (0.361) |
| Percentage of severe housing problems | 14.353 (4.354) | 16.370 (4.709) | 12.150 (3.466) | 14.876 (3.800) | 17.123 (5.247) |
| Percentage of public transportation | 0.932 (3.113) | 3.834 (9.252) | 0.563 (1.027) | 0.618 (1.831) | 1.440 (2.957) |
| Health care shortage | 0.894 (0.307) | 0.870 (0.337) | 0.843 (0.364) | 0.911 (0.284) | 0.981 (0.138) |
| Percentage of uninsured | 10.002 (4.984) | 6.094 (2.533) | 7.840 (4.512) | 12.175 (4.711) | 10.086 (4.349) |
Standard deviations in parentheses.
Confirmed cases as of May 28, 2020.
Fig. 1.
Maps of continuous U.S. counties reflecting (A) regions, (B) COVID-19 rates per 10,000 as of May 28, 2020, (C) percentages of Latinx residents, and (D) foreign-born residents.
Table 2 presents incident rate ratios (IRR), reflecting a predicted percent change in county case rate, and 95% confidence intervals. In model 1, adjusting for only days since the first case, a one-point increase in the percentage of Blacks is associated with a 3.1% increase (IRR = 1.031; 95% CI 1.024–1.038) in the COVID-19 case rate. A similar increase in the percentage of Latinx is associated with a 3.4% increase (IRR = 1.034; 95% CI 1.011–1.058) in case rate. The same one-point increase for the percentage of Asians is associated with a 5.4% increase (IRR = 1.054; 95% CI 1.011–1.100). Model 2 includes the percentage of foreign-born, for which a one-point increase is associated with an 11.1% increase (IRR = 1.111; 95% CI 1.082–1.142) in COVID-19 case rate. The estimate for the percentage of Blacks is robust to the inclusion of the percentage of foreign-born. However, the positive association for the percentage of Latinx is rendered statistically insignificant when controlling for the percentage of foreign-born. Adjusting for the percentage of foreign-born also makes the estimate for the percentage of Asians negative, suggesting that, for each point increase in the percentage of Asian residents, the COVID-19 case rate declines by 6.1% (IRR = 0.939; 95% CI 0.904–0.974). In model 3, adjusting for the full range of county-level controls does not significantly alter the racial-ethnic and nativity composition estimates.
Table 2.
Associations of racial-ethnic composition with COVID-19 cases in counties adjusting for days since the first case, Percentage of foreign born, and all risk factors combined
| Variable | Model 1 |
Model 2 |
Model 3 |
Model 4 |
|---|---|---|---|---|
| IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | |
| Percentage of Blacks | 1.031‡ [1.024, 1.038] | 1.031‡ [1.024, 1.037] | 1.031‡ [1.025, 1.036] | 1.030‡ [1.025, 1.036] |
| Percentage of Latinx | 1.034† [1.011, 1.058] | 0.998 [0.987, 1.010] | 0.991 [0.980, 1.003] | |
| Percentage of Asians | 1.054∗ [1.011, 1.100] | 0.939‡ [0.904, 0.974] | 0.947† [0.913, 0.983] | 0.949‡ [0.920, 0.979] |
| Percentage of Mexicans | 0.991 [0.976, 1.006] | |||
| Percentage of Puerto Ricans | 1.038 [0.969, 1.112] | |||
| Percentage of Cubans | 0.927‡ [0.900, 0.956] | |||
| Percentage of Central Americans | 1.130‡ [1.067, 1.197] | |||
| Percentage of South Americans | 0.838‡ [0.769, 0.912] | |||
| Percentage of Other Latinx-origin | 0.987 [0.967, 1.008] | |||
| Percentage of Foreign born | 1.111‡ [1.082, 1.142] | 1.106‡ [1.074, 1.139] | 1.092‡ [1.067, 1.118] | |
| Days since the first case | 1.078‡ [1.061, 1.095] | 1.078‡ [1.062, 1.094] | 1.074‡ [1.060, 1.087] | 1.072‡ [1.059, 1.086] |
| Days since the first case squared | 1.000‡ [0.999, 1.000] | 1.000‡ [0.999, 1.000] | 1.000‡ [0.999, 1.000] | 1.000‡ [0.999, 1.000] |
| Population density (log) | 0.929 [0.857, 1.006] | 0.920∗ [0.850, 0.996] | ||
| Percentage of age 19–64 | 0.973 [0.935, 1.013] | 0.975 [0.934, 1.017] | ||
| Percentage of age 65 and over | 0.989 [0.943, 1.037] | 0.990 [0.941, 1.041] | ||
| Percentage of females | 0.912‡ [0.872, 0.952] | 0.915‡ [0.876, 0.956] | ||
| Median household income (log) | 0.930 [0.548, 1.577] | 1.062 [0.645, 1.747] | ||
| Income Inequality (80/20 ratio) | 1.015 [0.898, 1.146] | 1.027 [0.911, 1.158] | ||
| Unemployment rate | 0.911‡ [0.872, 0.952] | 0.920‡ [0.879, 0.963] | ||
| White/non-White segregation | 1.008† [1.003, 1.014] | 1.007† [1.002, 1.012] | ||
| White/Black segregation | 1.001 [0.999, 1.003] | 1.001 [0.999, 1.003] | ||
| Chronic disease index | 1.044 [0.965, 1.129] | 1.042 [0.965, 1.124] | ||
| Average household size | 1.818 [0.924, 3.575] | 1.792 [0.883, 3.637] | ||
| Percentage of severe housing problems | 1.009 [0.991, 1.028] | 1.010 [0.992, 1.029] | ||
| Percentage of public transportation | 1.003 [0.985, 1.021] | 1.013 [0.995, 1.031] | ||
| Health care shortage | 0.927 [0.802, 1.073] | 0.954 [0.834, 1.091] | ||
| Percentage of uninsured | 1.005 [0.978, 1.034] | 1.004 [0.979, 1.030] | ||
| Constant | 0.000‡ [0.000, 0.000] | 0.000‡ [0.000, 0.000] | 0.039 [0.000, 460.388] | 0.007 [0.000, 73.035] |
| lnalpha | –0.181∗ [–0.340, –0.022] | –0.235† [–0.390, –0.081] | –0.331‡ [–0.458, –0.203] | –0.354‡ [–0.487, ––0.220] |
| S.D.(constant) | 0.576‡ [0.420, 0.697] | 0.524‡ [0.400, 0.623] | 0.536‡ [0.398, 0.644] | 0.510‡ [0.349, 0.631] |
| N | 3106 | 3106 | 3106 | 3106 |
| AIC | 31,875.027 | 31,689.572 | 31,427.934 | 31,356.837 |
P < .05.
P < .01.
P < .001.
Model 4 presents fully adjusted estimates, substituting Latin American-origin subgroup measures for percentage Latinx. With all counties, the percentage of Mexicans, the percentage of Puerto Ricans, and the percentage of other Latinx-origin are not significantly associated with the COVID-19 case rate; the percentage of Cubans and the percentage of South Americans are significantly negatively associated with the outcome (IRR for Cuban = 0.927; 95% CI 0.990–0.956; IRR for S. American = 0.838; 95% CI 0.769–0.912). However, the percentage of Central Americans is significant and positive. A one-point increase in Central American residents is associated with a 13% increase (IRR = 1.130; 95% CI 1.067–1.197) in the COVID-19 case rate.
Table 3 shows fully adjusted estimates from model 3 stratified by region. The percentage of Blacks is positively associated with the COVID-19 case rate in the Northeast, Midwest, and South, with all CIs overlapping (IRRs between 1.022 and 1.058). In the West, the estimate for the percentage of Blacks is positive but imprecise—the confidence interval contains the null value, as well as the point estimate for the other regions. The percentage of Asians is negative in direction in all regions, but the estimate is precise enough to attain statistical significance only in the West (IRR = 0.954; 95% CI 0.914–0.977). Estimates for the percentage of Latinx are heterogeneous across regions. The percentage of Latinx is positive and significant in the Northeast, such that a one-point increase in the percentage of Latinx residents is associated with a 5.2% increase in the COVID-19 case rate (IRR = 1.052; 95% CI 1.031–1.073). In the Midwest, the percentage of Latinx is also positive in direction, but nonsignificant. In the West, the percentage of Latinx is nonsignificant with a magnitude very close to the null. However, in the South, the percentage of Latinx is statistically significant and negative in direction, such that a one-point increase in the percentage of Latinx residents is associated with a 1.3% decrease (IRR = 0.987; 95% CI 0.977–0.997) in the case rate. The percentage of foreign-born is positive and significant in the Midwest, South, and West (IRRs between 1.067 and 1.137). However, in the Northeast, the percentage foreign-born is nonsignificant.
Table 3.
Associations of racial-ethnic composition with COVID-19 cases in counties adjusting all risk factors combined, by region
| Variable | Northeast |
Midwest |
South |
West |
|---|---|---|---|---|
| IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | |
| Percentage of Blacks | 1.022† [1.009, 1.037] | 1.058‡ [1.026, 1.091] | 1.026‡ [1.020, 1.031] | 1.034 [0.986, 1.084] |
| Percentage of Latinx | 1.052‡ [1.031, 1.073] | 1.026 [0.999, 1.053] | 0.987∗ [0.977, 0.997] | 1.001 [0.982, 1.021] |
| Percentage of Asians | 0.983 [0.961, 1.006] | 0.913 [0.809, 1.031] | 0.972 [0.920, 1.026] | 0.954∗ [0.914, 0.997] |
| Percentage of Foreign born | 0.999 [0.969, 1.029] | 1.137† [1.036, 1.248] | 1.067‡ [1.031, 1.104] | 1.064∗ [1.001, 1.130] |
| Days since the first case | 1.121‡ [1.054, 1.193] | 1.078‡ [1.049, 1.107] | 1.093‡ [1.069, 1.117] | 1.069‡ [1.047, 1.092] |
| Days since the first case squared | 0.999‡ [0.999, 1.000] | 0.999‡ [0.999, 1.000] | 0.999‡ [0.999, 1.000] | 1.000‡ [1.000, 1.000] |
| Population density (log) | 1.146 [0.959, 1.371] | 0.965 [0.755, 1.234] | 0.895 [0.798, 1.004] | 0.949 [0.897, 1.004] |
| Percentage of age 19–64 | 1.030∗ [1.002, 1.060] | 0.965 [0.913, 1.020] | 0.959 [0.912, 1.007] | 0.982 [0.928, 1.040] |
| Percentage of age 65 and over | 1.075† [1.021, 1.132] | 0.955 [0.905, 1.007] | 0.980 [0.914, 1.052] | 0.999 [0.949, 1.051] |
| Percentage of females | 0.998 [0.959, 1.038] | 0.956 [0.839, 1.090] | 0.900‡ [0.847, 0.955] | 0.895∗ [0.817, 0.979] |
| Median household income (log) | 5.294‡ [2.435, 11.509] | 0.613 [0.199, 1.889] | 0.876 [0.371, 2.068] | 1.231 [0.324, 4.673] |
| Income Inequality (80/20 ratio) | 1.114 [0.967, 1.284] | 0.770‡ [0.692, 0.857] | 0.972 [0.822, 1.149] | 1.255 [0.947, 1.662] |
| Unemployment rate | 0.883∗ [0.787, 0.989] | 0.964 [0.900, 1.033] | 0.892‡ [0.841, 0.945] | 0.944∗ [0.891, 0.999] |
| White/non-White segregation | 1.004 [0.993, 1.016] | 1.004 [0.997, 1.011] | 1.006 [0.999, 1.012] | 1.016† [1.006, 1.026] |
| White/Black segregation | 1.002 [0.997, 1.008] | 1.001 [0.998, 1.004] | 0.997∗ [0.993, 1.000] | 1.001 [0.996, 1.006] |
| Chronic disease index | 1.450‡ [1.275, 1.648] | 0.996 [0.938, 1.058] | 1.080 [0.948, 1.231] | 0.893 [0.776, 1.028] |
| Average household size | 1.641 [0.760, 3.546] | 1.402 [0.698, 2.814] | 1.418 [0.423, 4.750] | 2.502∗ [1.010, 6.198] |
| Percentage of severe housing problems | 1.034∗ [1.006, 1.063] | 1.001 [0.966, 1.038] | 1.012 [0.982, 1.043] | 1.005 [0.955, 1.057] |
| Percentage of public transportation | 0.975‡ [0.961, 0.988] | 1.009 [0.899, 1.134] | 1.041‡ [1.018, 1.064] | 1.020 [0.982, 1.059] |
| Health care shortage | 0.842∗ [0.722, 0.983] | 0.909 [0.734, 1.126] | 0.972 [0.792, 1.193] | 1.211 [0.840, 1.745] |
| Percentage of uninsured | 0.970 [0.897, 1.049] | 0.976∗ [0.955, 0.997] | 1.027 [0.971, 1.087] | 1.021 [0.954, 1.091] |
| Constant | 0.000‡ [0.000, 0.000] | 7.064 [0.000, 139,100,000.000] | 0.681 [0.000, 2,695,583.040] | 0.000 [0.000, 3451.810] |
| lnalpha | –1.292‡ [–1.748, –0.836] | –0.401‡ [–0.619, –0.183] | –0.390‡ [–0.618, –0.163] | –0.422† [–0.732, –0.112] |
| S.D.(constant) | 0.136 [0.014, 0.323] | 0.316† [0.168, 0.414] | 0.465‡ [0.296, 0.587] | 0.426 [., 0.605] |
| N | 216 | 1055 | 1422 | 413 |
| AIC | 2866.233 | 9448.018 | 14,993.582 | 3698.238 |
P < .05.
P < .01.
P < .001.
Table 4 shows results by region substituting Latin American-origin subgroups for the combined percentage of Latinx variable. The models contain all covariates, but they are not shown for the efficiency of space (see Table S1 in supplemental results for complete models). Correlations are nonsignificant or negative in direction across all regions for the percentage of Mexicans, Cubans, South Americans, or other Latinx group. The percentage of Central Americans is positive and significant in the Northeast, Midwest, and South (IRRs between 1.098 and 1.194), but nonsignificant with a large confidence interval in the West. The percentage of Puerto Ricans is positively associated with the COVID-19 case rate in the Northeast and Midwest (IRRs between 1.067 and 1.207) but is negatively associated with the outcome in the South (IRR = 0.958; 95% CI 0.918–1.000). In the West, the percentage of Puerto Ricans is nonsignificant with a large confidence interval.
Table 4.
Associations of race and Latinx subgroup composition with COVID-19 cases in counties adjusting all risk factors combined, by region§
| Northeast |
Midwest |
South |
West |
|
|---|---|---|---|---|
| IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | |
| Percentage of Blacks | 1.016∗ [1.000, 1.033] | 1.057‡ [1.027, 1.089] | 1.026‡ [1.020, 1.032] | 1.060∗ [1.002, 1.120] |
| Percentage of Asians | 0.974 [0.949, 1.001] | 0.931 [0.843, 1.028] | 0.966 [0.917, 1.018] | 0.963 [0.927, 1.000] |
| Percentage of Mexicans | 1.032 [0.974, 1.093] | 1.016 [0.993, 1.039] | 0.985 [0.968, 1.001] | 1.008 [0.978, 1.039] |
| Percentage of Puerto Ricans | 1.067‡ [1.030, 1.106] | 1.207∗ [1.032, 1.412] | 0.958∗ [0.918, 1.000] | 0.877 [0.539, 1.426] |
| Percentage of Cubans | 0.882 [0.763, 1.019] | 1.213 [0.894, 1.647] | 0.957 [0.914, 1.001] | 0.567 [0.185, 1.743] |
| Percentage of Central Americans | 1.130† [1.038, 1.231] | 1.194∗ [1.014, 1.405] | 1.098† [1.035, 1.165] | 0.961 [0.811, 1.139] |
| Percentage of South Americans | 1.005 [0.916, 1.102] | 0.670‡ [0.536, 0.836] | 0.885 [0.779, 1.004] | 1.367 [0.800, 2.338] |
| Percentage of Other Latinx-origin | 1.031 [0.990, 1.073] | 0.760† [0.621, 0.930] | 1.059 [0.922, 1.217] | 0.995 [0.962, 1.029] |
Discussion
These results document higher COVID-19 case rates in counties with larger immigrant populations. When analyzing all contiguous counties combined (hereafter, combined analysis), the estimate for the percentage of foreign-born was significantly larger than for any of the racial-ethnic composition measures. When stratifying across regions (hereafter, regional analysis), the percentage of foreign-born was positively associated with the COVID-19 cases in the Midwest, South, and West, however, not in the Northeast. The relatively high correlations between the percentage of foreign-born and the percentage of Latinx in the Northeast could underestimate the parameters. As a check, we regressed the outcome on the percentage of foreign-born in the Northeast without racial-ethnic composition measures and found that the percentage of foreign-born was positive when adjusting for only days since the first case. It becomes nonsignificant when other controls are considered. Immigrants, particularly those recently arrived in the U.S., are concentrated in lower-income neighborhoods, low-wage employment, and crowded housing, all of which may increase exposure to COVID-19 [9,14,18].
In the combined analysis, adjusted estimates for the percentage of Latinx were nonsignificant, but this obscured heterogeneity across subgroups and regions. Estimates from the combined analysis, and for the Northeast, Midwest, and South, showed that counties with more Central Americans had higher COVID-19 case rates. In the Northeast and Midwest, counties with more Puerto Rican residents also had higher case rates. These results align with elevated poverty rates among Puerto Ricans and Central Americans, relative to Cubans and South Americans [[24], [25], [26]], as well as stronger residential segregation and geographic concentration of disadvantage among Puerto Ricans in the Northeast and Midwest [38]. Mexican Americans, the largest Latinx group in the U.S., also face elevated poverty rates; however, these case counts (captured on May 28, 2020) did not show a correlation with percentage of Mexican residents, net of controls. However, this could change, as cases rise in states with large Mexican American populations (e.g., Texas, Florida).
These data replicated robust positive correlations between county-level percentage of Black residents and COVID-19 case rates, which were present in the combined analysis and in all four regions (although the estimate in the West was imprecise). As discussed elsewhere [1,3,6], Black Americans have the highest chronic disease burden and are overrepresented in essential occupations [19]. Housing discrimination also subjects Black Americans to the highest levels of residential segregation [17,39].
Adjusted estimates for the percentage of Asian residents were generally negative in direction and were significant in the combined analysis and Western regional analysis. Relative to U.S. born whites, Asian Americans are more likely to live in dense urban areas and larger households [16,40]; however, higher average incomes and lower rates of chronic disease may also offer protection [19,41]. Importantly, as with Latinx populations, there is variation in sociodemographic risk factors facing Asian-origin subgroups, future research should explore whether the COVID-19 burden differs within the pan-ethnic category of Asians.
In the combined analysis, adjusting for the percentage of foreign-born in model 2, caused a positive percentage of Latinx estimate to become nonsignificant and a positive percentage of Asians estimate to become negative. In additional combined analyses (not shown), a positive estimate for the percentage of Mexicans also became nonsignificant when adjusting for the percentage of foreign-born. (Other positive subgroup estimates were robust to adjusting for the percentage of foreign-born residents). These changes may imply that nativity composition, and/or other associated county attributes, contribute to heavier COVID-19 burdens in counties with more Asian or Latinx residents.
Disparities in COVID-19 cases reflect inequities related to exposure, susceptibility, and likelihood of significant symptoms, and access to testing. It is also important to note that some confirmed cases are fatal (e.g., someone tests positive and later dies). In these county-level data, pairwise correlations between COVID-19 cases and deaths were >.90; therefore, we did not treat these as distinct outcomes, choosing to focus on cases given greater sparsity in area death counts. We replicated most of the analysis predicting death counts rather than cases and found similar patterns in the direction of estimates, although a handful of significance levels differed (see supplemental results). We also conducted a sensitivity test by including two state-level control variables—one for days since the state passed stay-at-home orders, and another for state testing rate (i.e., the number of COVID-19 tests performed as of May 28, 2020, divided by state population)—and found the results robust. We do not present these estimates, given that these variables are likely endogenous to disease trends.
This study has several limitations. First, COVID-19 cases underestimate true disease prevalence [42], and because of unequal access to testing, confirmed cases could suffer from biases. Second, our covariates cannot capture all plausible risk factors, and unmeasured county attributes may shape racial-ethnic disparities. Third, the cross-sectional and observational research design only permits associational interpretations. Finally, our county-level results cannot be referred to as individual-level disease risk.
Conclusions
U.S. counties with more immigrant residents, as well as more Central American or Black residents, have more COVID-19 cases. In the Northeast and Midwest, counties with more Puerto Rican residents also have more COVID-19 cases. These results add to a growing literature documenting area-level disparities in the COVID-19 burden. As the epidemic continues, geographic, racial-ethnic, and socioeconomic disparities may change, and on-going evaluation is needed.
CRediT authorship contribution statement
Kate Strully: Conceptualization, Writing - original draft. Tse-Chuan Yang: Methodology, Writing - review & editing. Han Liu: Formal analysis, Writing - review & editing.
Footnotes
The authorship team—Strully, Yang, and Liu—have no conflicts of interest to report for this study.
Appendix
Table S1.
Associations of race and Latinx subgroup composition with COVID-19 cases in counties adjusting all risk factors combined, by region (full results)
| Variable | Northeast |
Midwest |
South |
West |
|---|---|---|---|---|
| IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | |
| Percentage of Blacks | 1.016∗ [1.000, 1.033] | 1.057∗∗∗ [1.027, 1.089] | 1.026∗∗∗ [1.020, 1.032] | 1.060∗ [1.002, 1.120] |
| Percentage of Asians | 0.974 [0.949, 1.001] | 0.931 [0.843, 1.028] | 0.966 [0.917, 1.018] | 0.963 [0.927, 1.000] |
| Percentage of Mexicans | 1.032 [0.974, 1.093] | 1.016 [0.993, 1.039] | 0.985 [0.968, 1.001] | 1.008 [0.978, 1.039] |
| Percentage of Puerto Ricans | 1.067∗∗∗ [1.030, 1.106] | 1.207∗ [1.032, 1.412] | 0.958∗ [0.918, 1.000] | 0.877 [0.539, 1.426] |
| Percentage of Cubans | 0.882 [0.763, 1.019] | 1.213 [0.894, 1.647] | 0.957 [0.914, 1.001] | 0.567 [0.185, 1.743] |
| Percentage of Central Americans | 1.130∗∗ [1.038, 1.231] | 1.194∗ [1.014, 1.405] | 1.098∗∗ [1.035, 1.165] | 0.961 [0.811, 1.139] |
| Percentage of South Americans | 1.005 [0.916, 1.102] | 0.670∗∗∗ [0.536, 0.836] | 0.885 [0.779, 1.004] | 1.367 [0.800, 2.338] |
| Percentage of Other Latinx-origin | 1.031 [0.990, 1.073] | 0.760∗∗ [0.621, 0.930] | 1.059 [0.922, 1.217] | 0.995 [0.962, 1.029] |
| Percentage of Foreign born | 1.015 [0.975, 1.057] | 1.119∗ [1.023, 1.222] | 1.062∗∗ [1.024, 1.101] | 1.050 [0.993, 1.109] |
| Days since the first case | 1.146∗∗∗ [1.088, 1.207] | 1.074∗∗∗ [1.047, 1.102] | 1.092∗∗∗ [1.068, 1.117] | 1.068∗∗∗ [1.045, 1.091] |
| Days since the first case squared | 0.999∗∗∗ [0.999, 1.000] | 0.999∗∗∗ [0.999, 1.000] | 0.999∗∗∗ [0.999, 1.000] | 1.000∗∗∗ [1.000, 1.000] |
| Population density (log) | 1.151 [0.943, 1.406] | 0.952 [0.747, 1.212] | 0.878∗ [0.786, 0.980] | 0.942 [0.879, 1.010] |
| Percentage of age 19–64 | 1.029 [0.987, 1.073] | 0.972 [0.919, 1.027] | 0.957 [0.904, 1.012] | 0.990 [0.950, 1.032] |
| Percentage of age 65 and over | 1.069∗ [1.012, 1.129] | 0.956 [0.908, 1.006] | 0.979 [0.906, 1.057] | 1.005 [0.959, 1.053] |
| Percentage of females | 0.992 [0.953, 1.034] | 0.967 [0.850, 1.099] | 0.906∗∗ [0.853, 0.963] | 0.905∗ [0.829, 0.989] |
| Median household income (log) | 4.761∗∗∗ [2.242, 10.109] | 0.700 [0.223, 2.201] | 1.005 [0.457, 2.211] | 1.167 [0.331, 4.121] |
| Income Inequality (80/20 ratio) | 1.091 [0.900, 1.323] | 0.792∗∗∗ [0.707, 0.887] | 0.986 [0.842, 1.153] | 1.252 [0.943, 1.663] |
| Unemployment rate | 0.909 [0.814, 1.015] | 0.960 [0.906, 1.018] | 0.901∗∗ [0.847, 0.959] | 0.945 [0.872, 1.024] |
| White/nonwhite segregation | 1.004 [0.994, 1.014] | 1.003 [0.997, 1.010] | 1.006 [1.000, 1.012] | 1.016∗∗ [1.006, 1.026] |
| White/Black segregation | 1.003 [0.997, 1.008] | 1.001 [0.998, 1.004] | 0.996∗∗ [0.994, 0.999] | 1.001 [0.997, 1.006] |
| Chronic disease index | 1.428∗∗∗ [1.270, 1.606] | 0.998 [0.940, 1.058] | 1.091 [0.961, 1.240] | 0.899 [0.774, 1.043] |
| Average household size | 1.654 [0.960, 2.848] | 1.478 [0.768, 2.846] | 1.365 [0.367, 5.078] | 2.525∗ [1.075, 5.927] |
| Percentage of severe housing problems | 1.025∗∗∗ [1.013, 1.037] | 1.001 [0.967, 1.035] | 1.015 [0.986, 1.045] | 1.004 [0.952, 1.059] |
| Percentage of public transportation | 0.981∗∗∗ [0.971, 0.991] | 1.014 [0.904, 1.137] | 1.040∗∗∗ [1.017, 1.064] | 1.022 [0.987, 1.058] |
| Healthcare shortage | 0.843∗ [0.734, 0.967] | 0.941 [0.785, 1.127] | 0.989 [0.808, 1.210] | 1.162 [0.726, 1.859] |
| Percentage of uninsured | 0.966 [0.906, 1.030] | 0.977∗ [0.956, 0.998] | 1.021 [0.966, 1.079] | 1.022 [0.958, 1.090] |
| Constant | 0.000∗∗∗ [0.000, 0.000] | 0.590 [0.000, 39,212,668.926] | 0.131 [0.000, 453,208.228] | 0.000 [0.000, 946.336] |
| lnalpha | –1.276∗∗∗ [–1.653, –0.899] | –0.428∗∗∗ [–0.624, –0.232] | –0.408∗∗∗ [–0.650, –0.167] | –0.443∗∗ [–0.756, –0.131] |
| S.D.(constant) | 0.000 [0.000, 0.000] | 0.301∗ [0.136, 0.403] | 0.406∗∗∗ [0.270, 0.507] | 0.438∗ [0.058, 0.616] |
| N | 216 | 1055 | 1422 | 413 |
| AIC | 2862.844 | 9414.555 | 14,960.464 | 3692.637 |
∗P < .05; ∗∗ P < .01; ∗∗∗P < .001.
Table S2.
Associations of racial-ethnic composition with COVID-19 deaths in counties adjusting for days since the first case, percentage of foreign born, and all risk factors combined
| Variable | Model 1 |
Model 2 |
Model 3 |
|---|---|---|---|
| IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | |
| Percentage of Blacks | 1.031∗∗∗ [1.023, 1.039] | 1.030∗∗∗ [1.022, 1.038] | 1.030∗∗∗ [1.022,1.038] |
| Percentage of Latinx | 1.011 [0.998, 1.024] | 0.987∗ [0.976, 0.998] | 0.986∗ [0.974, 0.999] |
| Percentage of Asians | 1.044∗∗ [1.010, 1.079] | 0.959∗∗ [0.933, 0.986] | 0.964∗ [0.929, 1.000] |
| Percentage of Foreign born | 1.076∗∗∗ [1.047, 1.106] | 1.079∗∗∗ [1.050, 1.108] | |
| Days since the first case | 1.089∗∗∗ [1.066, 1.113] | 1.091∗∗∗ [1.068, 1.114] | 1.096∗∗∗ [1.069, 1.123] |
| Days since the first case squared | 1.000∗∗∗ [0.999, 1.000] | 1.000∗∗∗ [0.999, 1.000] | 1.000∗∗∗ [0.999, 1.000] |
| Population density (log) | 0.953 [0.858, 1.058] | ||
| Percentage of age 19–64 | 0.977 [0.930, 1.026] | ||
| Percentage of age 65 and over | 1.022 [0.972, 1.074] | ||
| Percentage of females | 0.994 [0.949, 1.040] | ||
| Median household income (log) | 1.030 [0.493, 2.148] | ||
| Income Inequality (80/20 ratio) | 1.077 [0.938, 1.236] | ||
| Unemployment rate | 0.978 [0.930, 1.029] | ||
| White/non-White segregation | 1.012∗∗∗ [1.006, 1.018] | ||
| White/Black segregation | 0.997∗∗ [0.994, 0.999] | ||
| Chronic disease index | 1.107 [0.955, 1.285] | ||
| Average household size | 1.622 [0.804, 3.270] | ||
| Percentage of severe housing problems | 1.003 [0.973, 1.034] | ||
| Percentage of public transportation | 1.014 [0.994, 1.035] | ||
| Healthcare shortage | 0.783∗∗ [0.672, 0.912] | ||
| Percentage of uninsured | 0.980 [0.951, 1.010] | ||
| Constant | 0.000∗∗∗ [0.000, 0.000] | 0.000∗∗∗ [0.000, 0.000] | 0.000∗ [0.000, 0.149] |
| lnalpha | 0.277∗∗∗ [0.130, 0.424] | 0.255∗∗∗ [0.111, 0.399] | 0.215∗∗ [0.064, 0.365] |
| S.D.(constant) | 0.756∗∗∗ [0.578, 0.899] | 0.730∗∗∗ [0.589, 0.848] | 0.678∗∗∗ [0.520, 0.806] |
| N | 3106 | 3106 | 3106 |
| AIC | 13,913.622 | 13,876.635 | 13,841.311 |
∗P < .05; ∗∗ P < .01; ∗∗∗P < .001.
Table S3.
Associations of racial-ethnic composition with COVID-19 deaths in counties adjusting all risk factors combined, by region
| Variable | Northeast |
Midwest |
South |
West |
|---|---|---|---|---|
| IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | |
| Percentage of Blacks | 1.029∗∗ [1.008, 1.049] | 1.018 [0.991, 1.046] | 1.027∗∗∗ [1.019, 1.035] | 0.990 [0.952, 1.028] |
| Percentage of Latinx | 1.045∗∗ [1.012, 1.078] | 0.969 [0.913, 1.029] | 0.990∗ [0.982, 0.998] | 0.974∗ [0.953, 0.994] |
| Percentage of Asians | 0.974 [0.915, 1.036] | 0.825∗∗ [0.732, 0.930] | 1.015 [0.964, 1.069] | 0.957 [0.896, 1.022] |
| Percentage of Foreign born | 1.012 [0.949, 1.079] | 1.185∗∗ [1.060, 1.326] | 1.048∗∗∗ [1.021, 1.076] | 1.123∗∗∗ [1.069, 1.180] |
| Days since the first case | 1.202∗∗∗ [1.137, 1.270] | 1.066∗ [1.012, 1.124] | 1.138∗∗∗ [1.064, 1.218] | 1.153∗∗ [1.051, 1.265] |
| Days since the first case squared | 0.999∗∗∗ [0.999, 0.999] | 1.000 [0.999, 1.000] | 0.999∗∗ [0.999, 1.000] | 0.999∗∗ [0.999, 1.000] |
| Population density (log) | 1.093 [0.792, 1.508] | 1.111 [0.879, 1.405] | 0.864∗ [0.748, 0.999] | 1.041 [0.834, 1.300] |
| Percentage of age 19–64 | 1.038 [0.971, 1.109] | 1.036 [0.942, 1.140] | 0.925∗∗∗ [0.890, 0.960] | 1.051 [0.921, 1.200] |
| Percentage of age 65 and over | 1.089 [0.986, 1.203] | 1.023 [0.936, 1.117] | 0.993 [0.936, 1.054] | 1.000 [0.910, 1.099] |
| Percentage of females | 1.307∗∗∗ [1.207, 1.415] | 1.072 [0.937, 1.226] | 0.963 [0.916, 1.012] | 1.028 [0.820, 1.288] |
| Median household income (log) | 8.858∗∗∗ [4.874, 16.101] | 0.870 [0.158, 4.786] | 0.522 [0.266, 1.026] | 0.210 [0.041, 1.062] |
| Income Inequality (80/20 ratio) | 1.035 [0.882, 1.214] | 0.886 [0.568, 1.383] | 1.015 [0.869, 1.186] | 0.855 [0.605, 1.208] |
| Unemployment rate | 0.927 [0.743, 1.157] | 1.149 [0.992, 1.330] | 0.919∗ [0.854, 0.987] | 0.989 [0.914, 1.071] |
| White/non-White segregation | 0.993 [0.981, 1.006] | 1.017∗∗∗ [1.007, 1.027] | 1.004 [0.994, 1.014] | 1.035∗∗∗ [1.021, 1.050] |
| White/Black segregation | 0.999 [0.990, 1.008] | 0.998 [0.995, 1.002] | 0.994 [0.988, 1.000] | 0.992∗∗ [0.985, 0.998] |
| Chronic disease index | 1.544∗∗∗ [1.281, 1.862] | 1.194 [0.840, 1.696] | 0.979 [0.868, 1.104] | 1.042 [0.663, 1.639] |
| Average household size | 1.153 [0.624, 2.130] | 1.752 [0.334, 9.197] | 0.887 [0.337, 2.339] | 2.430 [0.452, 13.059] |
| Percentage of severe housing problems | 1.011 [0.956, 1.069] | 0.966 [0.899, 1.038] | 1.008 [0.969, 1.049] | 0.957 [0.877, 1.044] |
| Percentage of public transportation | 0.985 [0.956, 1.014] | 1.019 [0.884, 1.176] | 1.076∗∗∗ [1.039, 1.116] | 0.993 [0.923, 1.069] |
| Healthcare shortage | 0.875 [0.563, 1.360] | 0.649∗∗∗ [0.534, 0.790] | 0.838 [0.649, 1.082] | 1.043 [0.534, 2.038] |
| Percentage of uninsured | 1.006 [0.933, 1.085] | 0.979 [0.933, 1.027] | 0.971 [0.930, 1.015] | 1.008 [0.921, 1.104] |
| Constant | 0.000∗∗∗ [0.000, 0.000] | 0.000 [0.000, 7.105] | 1.239 [0.000, 22,211.136] | 0.003 [0.000, 8.697e+11] |
| lnalpha | –0.495∗ [–0.931, –0.059] | 0.265 [–0.020, 0.550] | 0.101 [–0.122, 0.325] | 0.138 [–0.420, 0.697] |
| S.D.(constant) | 0.370 [0.209, 0.541] | 0.438∗ [0.199, 0.587] | 0.621∗∗ [0.368, 0.797] | 0.767 [0.419, 1.141] |
| N | 216 | 1055 | 1422 | 413 |
| AIC | 1813.196 | 3683.159 | 6623.481 | 1523.407 |
∗P < .05; ∗∗ P < .01; ∗∗∗P < .001.
References
- 1.Yancy C.W. COVID-19 and African Americans. JAMA. 2020;323(19):1891–1892. doi: 10.1001/jama.2020.6548. [DOI] [PubMed] [Google Scholar]
- 2.CDC COVID-19 provisional counts - weekly updates by select demographic and geographic characteristics. 2020. https://www.cdc.gov/nchs/nvss/vsrr/covid_weekly/index.htm
- 3.Owen W.F., Carmona R., Pomeroy C. Failing Another National Stress Test on Health Disparities. JAMA. 2020;323(19):1905–1906. doi: 10.1001/jama.2020.6547. [DOI] [PubMed] [Google Scholar]
- 4.Garg S. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 — COVID-NET, 14 States, March 1–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:458–464. doi: 10.15585/mmwr.mm6915e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rosenberg E.S., Tesoriero J.M., Rosenthal E.M., Chung R., Barranco M.A., Styer L.M. Cumulative incidence and diagnosis of SARS-CoV-2 infection in New York. Ann Epidemiol. 2020;48:23–29. doi: 10.1016/j.annepidem.2020.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Millett G.A., Jones A.T., Benkeser D., Baral S., Mercer L., Beyrer C. Assessing differential impacts of COVID-19 on black communities. Ann Epidemiol. 2020;47:37–44. doi: 10.1016/j.annepidem.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mahajan U.V., Larkins-Pettigrew M. Racial demographics and COVID-19 confirmed cases and deaths: a correlational analysis of 2886 US counties. J Public Health (Oxf) 2020;42:445–447. doi: 10.1093/pubmed/fdaa070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hubler S., Fuller T., Singhvi A., Love J. Many latinos couldn't stay home. now virus cases are soaring in their communities. The New York Times. 2020. https://www.nytimes.com/2020/06/26/us/corona-virus-latinos.html
- 9.Kawachi I., Berkman L.F. Oxford University Press; Oxford: 2003. Neighborhoods and health. [Google Scholar]
- 10.Macintyre S., Ellaway A., Cummins S. Place effects on health: how can we conceptualise, operationalise and measure them? Soc Sci Med. 2002;55(1):125–139. doi: 10.1016/s0277-9536(01)00214-3. [DOI] [PubMed] [Google Scholar]
- 11.Williams D.R., Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116(5):404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lobao L.M., Hooks G., Tickamyer A.R. SUNY Press; Albany, NY: 2007. The sociology of spatial inequality. [Google Scholar]
- 13.Allen D.W. Social class, race, and toxic releases in American counties, 1995. Soc Sci J. 2001;38(1):13–25. [Google Scholar]
- 14.Friedman S., Rosenbaum E. Nativity status and racial/ethnic differences in access to quality housing: Does homeownership bring greater parity? Hous Policy Debate. 2004;15(4):865–901. [Google Scholar]
- 15.Burr J.A., Mutchler J.E., Gerst K. Patterns of Residential Crowding among Hispanics in Later Life: Immigration, Assimilation, and Housing Market Factors. J Gerontol Ser B. 2010;65B(6):772–782. doi: 10.1093/geronb/gbq069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.U.S. Census Bureau. America's families and living arrangements: 2016. The United States Census Bureau. https://www.census.gov/data/tables/2016/demo/families/cps-2016.html
- 17.Iceland J., Weinbert D., Steinmetz E. Racial and ethnics residential segregation in the U.S.: 1980-2000. 2002. https://www.census.gov/library/publications/2002/dec/censr-3.html
- 18.Denney J.T., Saint Onge J.M., Dennis J.A. Neighborhood concentrated disadvantage and adult mortality: insights for racial and ethnic differences. Popul Res Policy Rev. 2018;37(2):301–321. [Google Scholar]
- 19.Bolen J.C., Rhodes L., Powell-Griner E.E., Bland S.D., Holtzman D. State-specific prevalence of selected health behaviors, by race and ethnicity–Behavioral Risk Factor Surveillance System, 1997. MMWR CDC Surveill Summ. 2000;49(2):1–60. [PubMed] [Google Scholar]
- 20.Radford J. Key findings about U.S. immigrants. Pew Research Center. https://www.pewresearch.org/fact-tank/2019/06/17/key-findings-about-u-s-immigrants/
- 21.Pabon-Nau L.P., Cohen A., Meigs J.B., Grant R.W. Hypertension and diabetes prevalence among U.S. Hispanics by country of origin: The National Health Interview Survey 2000-2005. J Gen Intern Med. 2010;25(8):847–852. doi: 10.1007/s11606-010-1335-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dobbs R.W., Malhotra N.R., Abern M.R., Moreira D.M. Prostate cancer disparities in Hispanics by country of origin: a nationwide population-based analysis. Prostate Cancer Prostatic Dis. 2019;22(1):159–167. doi: 10.1038/s41391-018-0097-y. [DOI] [PubMed] [Google Scholar]
- 23.Weinick R.M., Jacobs E.A., Stone L.C., Ortega A.N., Burstin H. Hispanic healthcare disparities: challenging the myth of a monolithic Hispanic population. Med Care. 2004;42(4):313–320. doi: 10.1097/01.mlr.0000118705.27241.7c. [DOI] [PubMed] [Google Scholar]
- 24.Orrenius P., Madeline Z. Trends in poverty and inequality among Hispanics. In: Rycoft R.S., editor. The economics of inequality, poverty, and discrimination in the 21st Century. Routledge; New York: 2013. pp. 217–235. [Google Scholar]
- 25.National Center for Education Statistics. Indicator 4 snapshot: children living in poverty for racial/ethnic subgroups. https://nces.ed.gov/programs/raceindicators/indicator_rads.asp
- 26.Macartney S., Bishaw A., Fontenot K. US Bureau of the Census; 2013. Poverty rates for selected detailed race and Hispanic groups by state and place: 2007-2011. [Google Scholar]
- 27.Borrell L.N. Racial identity among Hispanics: implications for health and well-being. Am J Public Health. 2005;95(3):379–381. doi: 10.2105/AJPH.2004.058172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Borrell L.N., Crawford N.D. Disparities in self-reported hypertension in Hispanic subgroups, Non-Hispanic Black and Non-Hispanic White adults: The National Health Interview Survey. Ann Epidemiol. 2008;18(10):803–812. doi: 10.1016/j.annepidem.2008.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fothergill A., Maestas E.G.M., Darlington J.D. Race, ethnicity and disasters in the United States: a review of the literature. Disasters. 1999;23(2):156–173. doi: 10.1111/1467-7717.00111. [DOI] [PubMed] [Google Scholar]
- 30.Black/African American - The Office of Minority Health. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=61
- 31.Asian American - The Office of Minority Health. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=63 [PubMed]
- 32.Brown A., Lopez M.H. Mapping the Latino population, by state, county and city. Pew Research Center. 2013. https://www.pewresearch.org/hispanic/2013/08/29/mapping-the-latino-population-by-state-county-and-city/
- 33.Remington P.L., Catlin B.B., Gennuso K.P. The county health rankings: rationale and methods. Popul Health Metr. 2015;13(1):11. doi: 10.1186/s12963-015-0044-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.U.C. Bureau with U.S. Census Bureau so it reads as follows: U.S. Census Bureau. Data release new and notable. The United States Census Bureau. 2018. https://www.census.gov/programs-surveys/acs/news/data-releases/2018/release.html
- 35.Home - chronic conditions data warehouse. https://www2.ccwdata.org/web/guest/home/
- 36.Area Health Resources Files. https://data.hrsa.gov/topics/health-workforce/ahrf
- 37.Coronavirus live map | US coronavirus cases by coUNTY. USAFacts. https://usafacts.org/visualizations/coronavirus-covid-19-spread-map/
- 38.Martin M. Residential segregation patterns of latinos in the United States, 1990–2000 testing the ethnic enclave and inequality theories. Routledge. 2007. https://library.oapen.org/viewer/web/viewer.html?file=/bitstream/handle/20.500.12657/24146/1005985.pdf?sequence=1&isAllowed=y
- 39.Massey D.S., Denton N.A. Harvard University Press; Cambridge, MA: 1993. American Apartheid: Segregation and the Making of the Underclass. [Google Scholar]
- 40.Smelser Neil J., Wilson William Julius, Mitchel Faith. Vol. 1. National Academies Press; Washington, DC: 2001. (America becoming: racial trends and their consequences). [Google Scholar]
- 41.Guzman G. Household Income: 2018. 2019. https://www.census.gov/library/publications/2019/acs/acsbr18-01.html
- 42.Richterich P. Severe underestimation of COVID-19 case numbers: effect of epidemic growth rate and test restrictions. medRxiv. 2020 doi: 10.1101/2020.04.13.20064220. [DOI] [Google Scholar]