Abstract
Background and aims
Lockdown during the COVID-19 pandemic imposed many restrictions on the public. Loss of continuum of care along with improper lifestyle was expected to worsen glycemic control in people with type 2 diabetes (T2D). We aimed to identify the effects of lockdown on their glycemic status, lifestyle changes and psychosocial health.
Methods
The pre- and post-lockdown data of 110 adults with T2D who were under regular follow up was collected by direct interview during their visit to the diabetes clinic. The variables analyzed included demographic data, HbA1c, body weight, lifestyle changes, psychosocial factors and use of technology.
Result
The overall physical activity and dietary adherence remained unchanged in more than 80% of the participants. There was increased consumption of vegetables (80.9%), fruits (42.7%), and decreased unhealthy snacking (63%). 90% of them had access to medications. No significant change was noted in the mean HbA1c and body weight before and after lockdown. Most of them (99%) watched television and 73.6% of them spent time with their family members. Those with mental stress and poor sleep had unhealthy dietary habits. Poor glycemic control was seen in those with less physical activity and an unhealthy diet.
Conclusion
Lockdown did not cause a major change in the overall glycemic control. Measures to promote healthy lifestyle practices along with ways to reduce psychosocial stress must be implemented for better T2D management during such restricted times.
Keywords: Diabetes, Glycemic control, Lifestyle, Stress, Lockdown, COVID-19
Highlights
-
•
Lockdown did not show a major change in glycemic control, lifestyle, psychosocial health or availability of medicines. .
-
•
Unhealthy lifestyle habits in young and increased psychosocial stress in females and elderly are findings of concern.
-
•
Overall increase in vegetable and fruit consumption with less of unhealthy snacking are affirmative findings.
-
•
More time spent with family and for household chores, better use of technology for communication are encouraging results.
1. Introduction
The Novel Coronavirus disease 2019 (COVID-19) pandemic posed medical and social challenges to mankind. In order to contain the spread of the disease, nationwide lockdowns were implemented in many parts of the world and hence millions of people were confined to remain indoors [1]. In Pathanamthitta district of South Kerala, the lockdown was enforced on March 16, 2020, one week earlier than the nationwide 21-day lockdown 1.0 which was announced on March 24, 2020. This was followed by lockdown 2.0 and 3.0 which ended on May 17, 2020 [2]. On the other hand, the burden of Type 2 diabetes (T2D) in our country has remained unchanged. It is well known that proper lifestyle forms an essential component of diabetes management. Reports from other countries showed that sudden disruption of social contacts led to the deprivation of mental and emotional well-being, which eventually affected the physical activity, sleep, employment and quality of life of many individuals [3]. It is still unknown if these interruptions had any influence on the glycemic control in people living with diabetes.
As the nation went into lockdown in the wake of dire COVID-19 conditions, the Government of Kerala clarified that provisions to ensure uninterrupted stocks of food and essential commodities were being put in place. But the sudden change in lifestyle and inaccessibility to routine healthcare visits to hospitals can take its toll on patients having chronic non-communicable diseases like T2D hypertension, dyslipidemia, coronary artery disease, etc. It was also hypothesized that the lockdown would adversely influence the glycemic status of individuals with T2D [4]. Disruption of healthcare services and the loss of continuum of care, along with disrupted meal patterns and increased consumption of processed foods was also expected to have a negative impact on glycemia [5]. Few authors questioned these projections and concluded that they do not expect any alarming change in glycemic status [6]. While an online and telephonic survey showed that people with diabetes remained unaffected to a greater extent [7], another survey showed improvement in glycemic status and body weight [8]. A survey from Kerala examining the social impact showed that lockdown reduced income, expenditure and the happiness of households [9]. Previous observations concluded with either simulated projections [4] or were not able to assess the exact changes in body weight or HbA1c [5]. There still remains a paucity of real-world data on these aspects particularly from Kerala, which received much appreciation at the international level for its model of COVID-19 control measures [10]. This necessitated us to attempt and analyze the actual effect of lockdown on glycemic control, lifestyle and psychosocial aspects in this population.
2. Methods
The study was conducted in the outpatient diabetes clinic of MGM Muthoot Hospitals, Pathanamthitta. Adult patients with T2D on regular follow up for the past one year, who consulted during the immediate post lockdown period (during 4 weeks ranging from the third week of May to the third week of June 2020) were included in the study. Those who recently changed or modified antidiabetic drug therapy in the immediate past 3 months before the lockdown period, patients who received treatment for other illness which might influence diabetes control in the past 3 months, those who were hospitalized during lockdown period, pregnant ladies and terminally ill patients were excluded from the study.
A well-structured questionnaire was formulated after compiling information from various reference studies [3,[5], [6], [7]]. The data was collected by face to face interaction during the follow-up visit to the hospital and entered using Google forms after obtaining the informed consent. Completing the procedure for each patient took approximately 7–10 min.
Data collected included demographic parameters, HbA1c and body weight values pre and post lockdown, questions related to the type of treatment, management and complications of T2D, changes in diet and lifestyle, use of digital technology for personal communication, infotainment and teleconsultation, factors related to psychosocial stress and also the status of first degree relatives abroad or in other states. The pre lockdown and post lockdown biochemical tests and the anthropometric data were collected based on the information from the patient’s electronic medical records (Supplementary Table 1).
A significant change in HbA1c (deltaA1c) was considered as a change of 0.5% or more from baseline [11]. A modest change in body weight (deltaBW) more than 3% was considered significant [12]. Parameters like sleep quality, overall physical activity and dietary adherence, blood glucose monitoring, mental stress, use of digital media were compared to the those of the participants before the onset of lockdown. Anxiousness about COVID-19 spread was assessed using simple questions based on the Hospital Anxiety and Depression Scale (HADS) [13]. Dietary changes during lockdown and questions on the utilization of free time during lockdown had multiple answers from which the participants were asked to select the most important changes they made during the lockdown period compared to the pre-lockdown period. Consumption of a diet rich in vegetables and fruits and less of snacks, fried or processed food was considered as a “healthy diet pattern”, whereas those who consumed higher quantity of snacks, fried or processed food with less of vegetables and fruits were considered to have an “unhealthy diet pattern”. (Supplementary Table 1).
Considering the mean and standard deviation (SD) of baseline HbA1c [14] and post lockdown mean HbA1c [4], a confidence level of 99% and power of the study as 99%, the sample size was calculated and it was decided to take 110 samples. Continuous variables were summarized with descriptive statistics like N (%), mean, median, standard deviation. Paired t-test was used to compare the mean values and Chi-square test to assess differences in proportions as appropriate before and after the lockdown. Alpha was set at 0.05 to determine statistical significance. IBM SPSS Statistics subscription was used for statistical analysis.
3. Results
The mean age of the study population was 58.67 ± 10.8 years. Those in the age group of 50–65 years constituted 45.5%, whereas 30% were above 65 years of age. Females constituted 61.8%. Duration of diabetes was 5–15 years in 60% of the study population, whereas in 33.6% it was more than 15 years. 53.6% were on oral antidiabetic agents (OADs) alone whereas rest were on OADs with insulin. History of previous heart disease was present in 10.9% and chronic kidney disease in 2.7%. Ramadan fasting was observed only by 8.2%. More than 60% of the participants lived outside the city limits (approximately 5 km).
More than 80% of the study population reported no major change in their physical activity pattern and overall dietary adherence. Increased mental stress was seen in 15.5%. Quality of sleep was better in 23.6% and also worse in 23.6%, whereas it was unchanged in 52.8%. There was an increase in the use of digital media for personal or social communication in 30% of the study population, whereas telemedicine services in the hospital were used by only 7.3%. Only 10% had missed their medications whereas 90% had access to their medications during the lockdown (Table 1 ).
Table 1.
Lifestyle changes before and during lockdown (N = 110).
| Increased (%) | Decreased (%) | Same as before (%) | |
|---|---|---|---|
| Overall dietary adherence during lockdown | 6.4 | 7.3 | 86.4 |
| Physical activity/exercise during lockdown | 2.7 | 14.5 | 82.7 |
| Frequency of blood sugar monitoring | – | 6.4 | 93.7 |
| Mental stress during lockdown | 15.5 | 10.9 | 73.6 |
| Sleep during lockdown | 23.6 | 23.6 | 52.7 |
| Use of digital media for communication | 30 | 4.5 | 65.5 |
It was noted that 36.3% were anxious about missing appointments with their doctor, 27.3% were anxious about the spread of COVID-19 pandemic and 20% were anxious about the availability of medicines. It was found that 73.6% had at least one of their first-degree relatives abroad or in other states. Whereas 10.9% had first-degree relatives working in COVID-19 care centers abroad or in other states, 3.6% had their first-degree relatives diagnosed with COVID-19 infection. Overall, 10% reported that their diabetes management was affected by lockdown (Table 2 ).
Table 2.
Psychosocial changes during lockdown (N = 110).
| Yes (%) | No(%) | |
|---|---|---|
| Anxious about spread of COVID-19 pandemic | 27.3 | 72.7 |
| Anxious about availability of medicines | 20 | 80 |
| Anxious about missing appointment with doctor | 36.4 | 63.6 |
| Family members living abroad or in other states | 73.6 | 6.4 |
| Family members involved in COVID-19 care | 10.9 | 89.1 |
| Family members affected with COVID-19 | 3.6 | 96.4 |
| Overall diabetes management affected by COVID-19 | 10 | 90 |
There was no statistically significant difference in the mean HbA1c before (8.2 ± 1.3%) and after (8.12 ± 1.6%) lockdown. The mean body weight after the lockdown was numerically higher (71.8 ± 13.6 kg) compared to that before lockdown (71.5 ± 14.8 kg), but could not achieve statistical significance.
DeltaA1c increase was seen in 28.8%, a decrease in 31.8%, whereas 39.4% had HbA1c change less than 0.5%. DeltaBW increase was seen in 22.7%, a decrease in 11.8%, whereas 65.5% had a change in body weight less than 3%.
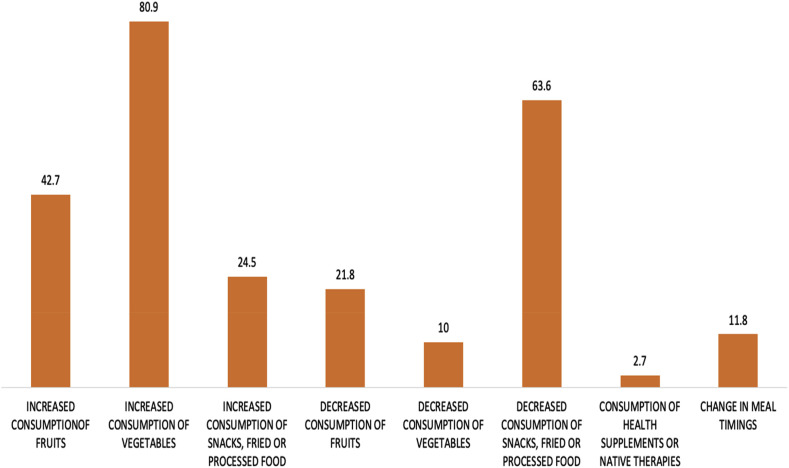
Considering the most important dietary change during the lockdown, 80.9% reported increased consumption of vegetables, 42.7% reported increased consumption of fruits, whereas only 24.5% reported increased consumption of snacks, fried or processed foods. 63% reported decreased consumption of snacks, fried or processed foods, whereas only 11.8% had a change in meal timings. Less than 3% consumed health supplements or home remedies as a preventive strategy against COVID-19 (Fig. 1 ).
Fig. 1.
Important dietary changes during lockdown (%).
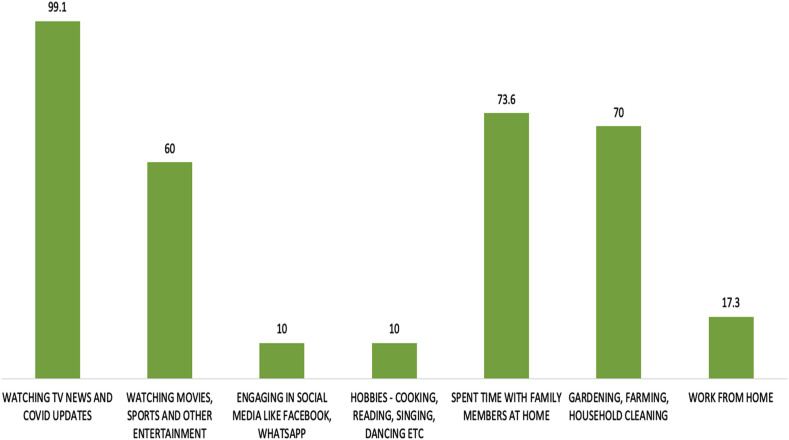
The time utilized during lockdown was predominantly for watching COVID-19 updates in television (99%), spending time with family members (73.6%), engaging in household chores (70%) and engaging in watching movies, sports and other entertainment (60%).
Work from home (17.3%), social media use (10%), and getting engaged with old hobbies (10%) were less common (Fig. 2).
Fig. 2.
Utilization of time during lockdown (%).
DeltaA1c increase was significantly more common in those who were less physically active (p = 0.009). Compared to those who ate a diet rich in vegetables and fruits (healthy diet pattern), those who consumed a higher quantity of snacks, fried or processed food with less of vegetables and fruits (unhealthy diet pattern) had a significant increase in deltaA1c (p = 0.04).
Physical inactivity was inversely proportional to age. Only 12.5% of those above 65 years had reduced physical activity during lockdown compared to 31.3% of those between 50 and 65 years and 56.3% of those less than 50 years of age (p = 0.017). Younger patients had an unhealthy diet pattern compared to older patients. (p = 0.001). The majority of the study participants who had increased mental stress also followed an unhealthy diet pattern (p = 0.002).
Those who had less sleep also had an unhealthy diet pattern (p = 0.04). Sleep quality was less affected (p = 0.04) in those who were less anxious regarding the spread of the pandemic. Quality of sleep was also adversely affected in older age groups (p = 0.005) and in females (p = 0.005). Anxiety regarding the spread of the pandemic was also more common in females (p = 0.016). A significant increase in mental stress was noted in those who had their first-degree relatives involved in COVID-19 care centers (p = 0.016). Anxiety about the spread of COVID-19 pandemic was also significantly more in those who had their first-degree relatives involved in COVID-19 care centers (p = 0.01).
Though only 10% of the study population missed their medicines partially or fully due to availability issues, it was seen that these were predominantly in the younger age groups (p = 0.004), and most of these patients were exclusively on OADs (p = 0.009). Among the 10%, who missed their medicines, most felt that the lockdown scenario badly affected their diabetes management (p = 0.001).
4. Discussion
This is probably the first study from Kerala which has looked upon the metabolic, lifestyle and psychosocial aspects of patients with T2D before and during lockdown due to the COVID-19 pandemic.
The majority of the study population was having a duration of diabetes between 5 and 15 years and more than half of the study population was on OADs which are in conjunction with the study by Sukanya Nachimuthu et al. [7]. In contrast, a female predominance was noted in our study.
During the lockdown restrictions, though the physical activity of individuals was expected to be limited, a majority of them (82.7%) continued their usual physical activity pattern, a finding which was also observed in few other studies [3], [5], [7].
Unlike the previous studies which predicted a significant worsening of glycemic control [4,15], there was no significant overall change in the HbA1c and body weight in this study. Body weight maintenance has been defined as less than 3% change from baseline weight with more than 5% change in body weight considered as clinically significant [12]. More than three-fourths of the study population were able to prevent weight gain and modest weight gain was noted only in 22.3%. This could be because there was a reassuring overall increase in the “healthy diet pattern”, and increased involvement in household chores, which could have helped in preventing significant HbA1c and body weight change in the majority of the study population. The increased seasonal availability of locally cultivated fruits and vegetables during this period could have helped this positive lifestyle change. In a study involving a predominantly urban population, 88% of them reported no change in their overall dietary pattern during the lockdown [7].
RM Anjana et al. [8] showed that 30.6% utilized the telemedicine facility, which was much less in our study, which had a predominantly semi-urban and rural population. Yet, we could find increased utilization of visual and digital media for obtaining COVID-19 related information, entertainment and also for personal communication. In a multicentric study predominantly involving urban areas, there was 15.9% increased screen time and nearly 11.4% utilized social media for improving their knowledge regarding diabetes management [3].
The frequency of blood sugar monitoring remained the same as before for most patients which is in contrast to previous studies which reported decreased [7] and increased [8] frequency of monitoring. Even though more than 60% of the participants stayed beyond the city limits (approximately 5 km), less than 10% had issues with the availability of medicines which eventually led to the discontinuation of medicines either partially or totally. Availability and accessibility to medicines away from big cities were important concerns raised in earlier studies [4,5], which did not seem to affect our study population.
A significant increase in HbA1c seen in those who had an “unhealthy diet pattern” and less physical activity reinforces the importance of maintaining a healthy lifestyle practice. These were the most important concerns raised in many of the previously published articles [4,5,14,16]. An important finding of concern is the physical inactivity and “unhealthy food pattern” being more predominant in the younger generation. This trend also applied to those who missed their medications during the lockdown period. These findings point to poor motivation among the younger generation, which we consider as an important area to intervene in the future.
It was reported in an earlier study that as high as 87% of people with T2DM were affected due to psychological stress and 27% experienced sleep deprivation during the lockdown period [5]. Whereas another pilot study [7] reported that 40% of their subjects were anxious about the pandemic and a majority (73%) of them had high hopes that the situation will getter better in the future. Watching entertainment on television, getting engaged with household chores, and spending ample time with family members might have helped the majority of participants in our study to reduce stress and anxiety levels. Yet, there was an unhealthy food pattern prevalent in those with increased mental stress and poor sleep. Anxiety regarding the spread of the pandemic had a significant impact on sleep quality, which was more in females and older age groups. Anxiety levels and mental stress were also high in those who had their relatives working in COVID-19 care centers. Fear and anxiety about a novel disease and what could happen can be enormous and can cause strong reactions to the general public, which in turn can disrupt their psychosocial life. Awareness and education on coping skills during the pandemic in vulnerable populations, especially females, as seen in our study would be essential in maintaining psychosocial harmony during the pandemic. Lifestyle changes and mental stress were recognized as possible factors responsible for upsetting the glycemic control in a recent publication from Central India [14].
The strengths of our study are that we had a direct face to face interview with the participants compared to telephonic and online interviews in the previous studies. This is especially important when recording important parameters like body weight and HbA1c, which can have erroneous reports when measured at different sites [5]. We were able to reach the estimated sample size as calculated based on the reference studies [4,5,7]. We had strong exclusion criteria where we tried to exclude most factors that could have otherwise affected glycemic control and lifestyle during the lockdown period such as a recent change in medications or hospitalizations during the study period and thereby eliminating many confounders. Very few studies have compared the actual HbA1c before and after lockdown like we did, which gave more lucidity regarding the real effects of lockdown in this population.
4.1. Limitations of the study
This is a single-center hospital based study with small sample size, considering the magnitude of the spread of the pandemic. The responses were subjective and the results are from a limited semi-urban geographic area. The findings are from a well aware population visiting hospital and may not be applicable to the general population with poor access to healthcare facilities. Our patients belonged mostly to the upper-middle and higher socioeconomic strata, and they were probably less economically affected by the lockdown.
To conclude, the lockdown did not cause a major disruption in the glycemic control, lifestyle and psychosocial health in our population. However, younger adults were prone to unhealthy lifestyle practices and increased psychosocial stress was noticed in females and older adults. Probably, the duration of lockdown and the restrictions imposed were not long enough to bring about significant changes in glycemic control and body weight. The increased utilization of technology for personal communication was a promising finding and it may pave the way towards increased acceptance of remote telehealth services in the future.
It is crucial to address the needs of the people living with T2D and ensure access to healthcare services and medicines along with maintaining healthy lifestyle habits during similar times of adversity. These can be achieved by the joint effort of the community, government and medical fraternity. At an individual level, each patient with T2D should be encouraged to follow healthy food habits by taking a balanced diet, maintain regular physical activity and follow measures to reduce anxiety and mental stress.
Larger studies from different geographical areas are necessary to identify the actual impact of lockdown in people with T2D on a broader scale. Reaching out to the community to provide a continuum of care and promote healthy lifestyle practices is the need of the hour.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.dsx.2020.09.005.
Appendix A. Supplementary data
The following is/are the supplementary data to this article:
References
- 1.Ahmed W.N., Arun C.S., Koshy T.G., Nair A., Sankar P., Rasheed S.A. Management of diabetes during fasting and COVID-19–Challenges and solutions. J Fam Med Prim Care. 2020;9(8):3797–3806. doi: 10.4103/jfmpc.jfmpc_845_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Onmanorama COVID-19 Timeline: how Kerala fought the pandemic so far. 2020. https://www.onmanorama.com/news/kerala/2020/05/06/covid-19-timeline-kerala-india-coronavirus-chronology-important-dates.html
- 3.Ammar A., Trabelsi K., Brach M., Chtourou H., Boukhris O., Masmoudi L. Effects of home confinement on mental health and lifestyle behaviours during the COVID-19 outbreak: insights from the ECLB-COVID19 multicentre study [Published online ahead of print, August 2020] Biol Sport. 2021;38(1):9–21. doi: 10.5114/biolsport.2020.96857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ghosal S., Sinha B., Majumder M., Misra A. Estimation of effects of nationwide lockdown for containing coronavirus infection on worsening of glycosylated haemoglobin and increase in diabetes-related complications: a simulation model using multivariate regression analysis. Diabetes Metab. Syndr. 2020;14(4):319-323. doi: 10.1016/j.dsx.2020.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ghosh A., Arora B., Gupta R., Anoop S., Misra A. Effects of nationwide lockdown during COVID-19 epidemic on lifestyle and other medical issues of patients with type 2 diabetes in north India [Published online ahead of print, June 2020] Diabetes Metab. Syndr. 2020;14(5):917–920. doi: 10.1016/j.dsx.2020.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kumar A., Arora A., Sharma P. Effect of lockdown on the glycemic control of diabetes patients. Diabetes Metab. Syndr. 2020;14(4):447–448. doi: 10.1016/j.dsx.2020.04.025. [DOI] [PubMed] [Google Scholar]
- 7.Nachimuthu S., Vijayalakshmi R., Sudha M., Viswanathan V. Coping with diabetes during the COVID - 19 lockdown in India: results of an online pilot survey. Diabetes Metab. Syndr. 2020;14(4):579–582. doi: 10.1016/j.dsx.2020.04.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anjana R.M., Pradeepa R., Deepa M., Jebarani S., Venkatesan U., Parvathi S.J. Acceptability and utilization of newer technologies and effects on glycemic control in type 2 diabetes: lessons learned from lockdown. Diabetes Technol Therapeut. 2020:527–534. doi: 10.1089/dia.2020.0240. [DOI] [PubMed] [Google Scholar]
- 9.Sujathan P.K., Azad P. SSRN; 2020. Social impact of lockdown in Kerala: a case study. Published online, April. [DOI] [Google Scholar]
- 10.World Health Organisation Responding to COVID-19 - learnings from Kerala. 2020. https://www.who.int/india/news/feature-stories/detail/responding-to-covid-19---learnings-from-kerala
- 11.Little R.R., Rohlfing C.L. The long and winding road to optimal HbA1c measurement. Clin Chim Acta. 2013;418:63–71. doi: 10.1016/j.cca.2012.12.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Donnelly J.E., Blair S.N., Jakicic J.M., Manore M.M., Rankin J.W., Smith B.K. American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009;41(2):459–471. doi: 10.1249/MSS.0b013e3181949333. [DOI] [PubMed] [Google Scholar]
- 13.Djukanovic I., Carlsson J., Arestedt K. Is the Hospital Anxiety and Depression Scale (HADS) a valid measure in a general population 65–80 years old? A psychometric evaluation study. Health Qual Life Outcome. 2017;15(1):193. doi: 10.1186/s12955-017-0759-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mohan V., Shah S.N., Joshi S.R., Seshiah V., Sahay B.K., Banerjee S. Current status of management, control, complications and psychosocial aspects of patients with diabetes in India: results from the DiabCare India 2011 Study. Indian J. Endrocrinol. Metab. 2014;18(3):370–378. doi: 10.4103/2230-8210.129715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khare J., Jindal S. Observational study on Effect of Lock Down due to COVID 19 on glycemic control in patients with Diabetes: experience from Central India [Published online ahead of print, August 2020] Diabetes Metab. Syndr. 2020;14(6):1571–1574. doi: 10.1016/j.dsx.2020.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jayawardena R., Misra A. Balanced diet is a major casualty in COVID-19 [Published online ahead of print, July 2020] Diabetes Metab. Syndr. 2020;14(5):1085–1086. doi: 10.1016/j.dsx.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.