Abstract
Background:
Current trends in medical curricula are shifting from teaching histology and pathology as stand-alone disciplines. Therefore, it would be useful to examine the potential value of integrating these into the anatomical dissection experience.
Objectives:
The aim of this study was to assess the histologic reliability of tissues taken from embalmed cadavers in an anatomy laboratory.
Materials and Methods:
A total of 112 tissue samples were obtained using standard autopsy techniques from various organs (heart, lung, thyroid, skeletal muscle, bone and skin) of 11 cadavers available at the anatomy laboratory of Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia, in 2019. Samples were prepared using the standard paraffin procedure followed by cutting sections at 4-μm thickness and staining with standard hematoxylin and eosin stain. Using predefined criteria, the quality of the samples was evaluated by two board-certified histopathologists and each slide was categorized as good, satisfactory or poor.
Results:
Overall, 34.2% and 60.3% of the slides were of good and satisfactory quality, respectively. A significant difference in tissue quality was found between various organs. Thick skin and bone tissues had the highest “good” rating (84.6% and 81.8%, respectively), while thyroid and lung tissues had the highest “poor” rating (20% and 13.6%, respectively).
Conclusion:
Most of the tissues acquired from the embalmed cadavers were of good or satisfactory quality, thereby indicating the beneficial use of histological tissue from cadavers for educational purposes. Future research into how these findings translate into meaningful medical education would be beneficial.
Keywords: Cadavers, histology, medical education, reliability
INTRODUCTION
The transition of medical schools toward integrating clinical medicine with the basic science-oriented years has allowed medical students to have an enhanced ability to correlate pathophysiological concepts with clinical manifestations and management of diseases.[1,2] However, this has limited practical exposure to previously stand-alone disciplines such as histology and pathology, depriving students of important parts of medical education. This has been aggravated by the steady decline of the educational use of postmortem examinations, even though opinions of medical educators have been positive regarding their yield.[3,4] This calls for innovative approaches to reintegrate these experiences into medical school curricula.
Currently, some medical schools still use embalmed cadavers for teaching purposes, which provide students an opportunity to study and visualize gross human anatomy and sometimes identify gross pathological changes.[5,6] It has been shown that students hold an overwhelmingly positive opinion on the yield of these sessions on their education.[7] Furthermore, cadavers are considered medical students' “ first patient,” as they work through their anatomy and encounter existing pathology during dissections, in reference to the documented clinical data and the cause of death. However, the use of embalmed tissue for histological and histopathological teaching purposes has been limited.
It is not uncommon for cadavers in gross anatomy dissections to have pathological lesions. These gross pathology findings provide students with an opportunity to integrate their basic science understanding with clinical medicine, utilizing astute observations and critical thinking to draw evidence-based conclusions. By integrating pathology with anatomy, it has been shown that students were more able to identify, retain and integrate their understanding of pathology into their discussions and medical reasoning.[8] However, this opportunity has been restricted to gross pathological findings without exploring the histology of these findings. Integration of pathology has been limited by students' lack of technical know-how with regard to preparing and processing tissue samples as well as by the lack of involvement of pathologists with dissection experience.[5]
Reliability of histological specimens from embalmed tissue has shown some promise in recent literature, with heart tissue showing the highest preservation and lung tissue showing the lowest.[6,8] However, some doubts remain over their validity because of previous contradicting literature showing poor preservation and embalmment-related artifacts.[8] To the best of our knowledge, there is no study conducted to explore the histological quality of several organs, such as thyroid, bone, skin or skeletal muscle, from cadavers. Therefore, this study aimed to investigate the histological samples of these organs from embalmed cadavers to provide an initial assessment regarding their reliability, and thus highlight their potential in medical education.
MATERIALS AND METHODS
This reliability study included all formalin-fixed cadavers available for dissection (N = 11) at the Department of Anatomy, College of Medicine, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia. All 11 cadavers were preserved in cold storage and were embalmed within an average of 6.44 days, with the earliest being 3 days and the latest being 11 days. All cadavers were obtained in 2018, and all samples were collected within 3 months of embalmment at the beginning of 2019. No inclusion criteria were used to ensure that cadavers and tissue samples would reflect those collected by medical students during their dissection experience. Data regarding the embalmment process were obtained from the Department of Anatomy. All cadavers were cold stored in the anatomy laboratory with no preservatives or other material used other than that used in embalming the cadavers.
A total of 112 tissue samples were obtained solely for the purpose of this study under the supervision of an anatomist and a forensic pathologist using standard autopsy techniques from the thyroid, skeletal muscle (rectus abdominis), bone (anterior superior iliac spine), skin (acral skin from the big toe and truncal skin from the abdomen), heart (left and right ventricles and interventricular septum) and from both the lungs. Of the 112 samples, 33 were from the heart, 22 from lungs, 10 from thyroid, 12 from thin skin, 13 from thick skin, 11 from bone and 11 from skeletal muscles. Samples were placed in formalin and were transferred to the pathology laboratory where they were prepared using the standard paraffin procedure followed by cutting sections at 4 μm using a sectioning microtome and staining using standard hematoxylin and eosin stain.[9]
Histological slides were independently evaluated by two board-certified histopathologists with >4 years of experience in anatomical pathology; both these evaluators were not involved in the sample collection or slide preparation and were blinded to each other's evaluations. For evaluating the slides, the criteria were adapted from a previous study.[8] In brief, the cells and extracellular matrix had to (a) be clearly identified at low magnification and when using 200 and 400 objective magnifications, (b) have a sharp definition of cell size and nuclei and (c) have sharp boundaries with adjacent connective tissues.
Each histopathologist categorized the slides as good, satisfactory or poor based on the following criteria: the slide was categorized as “good” if it met all the aforementioned criteria without any cellular definition limitation at different magnifications or limitation to definition of structures, boundaries and surrounding tissue; as “satisfactory” when the slide was mostly adequate but there was some limitation in one of the criteria, and as “poor” when the slide had a significant limitation in two or more of the criteria. A numerical score of 2 was given if an evaluator rated a slide as “good,” whereas “satisfactory” was given a score of 1 and “poor” was given a score of “0.” The average score of the 2 evaluators was calculated, and a slide was considered “good” if the overall average score was 2, as “satisfactory” if the score was <2 but >1 and as “poor” if it was ≤1.
Statistical analysis
Statistical tests were conducted using Statistical Package for the Social Sciences version 21.0 for Windows (IBM Corp., Armonk, NY, USA). Thirty-five samples were used to measure inter-evaluator reliability using two-way mixed effects, absolute agreement and multiple rater intraclass correlation. In addition, the frequency of the overall slide quality rating and the slide rating among different organs was measured. A comparison of the slide rating between organ groups was conducted using the Fisher's exact test at a level of significance of P < 0.05.
RESULTS
The inter-evaluator reliability was found to be 0.73, which is considered a moderate level of reliability.[10]
In terms of the slides, 34.2% and 60.3% of all slides were of good and satisfactory quality, respectively, whereas the remaining 5.5% were of poor quality. Using the Fisher's exact test, the difference in the slide quality between the organs was found to be significant (P < 0.01).
The frequency of slide quality rating across the various organs is shown in Table 1. Thick skin and bone tissues had the highest percentage of “good” rating, with frequencies of 84.6% and 81.8%, respectively. Thyroid and lung tissues had the highest percentage of “poor” rating, with frequencies of 20% and 13.6%, respectively. Figure 1 shows examples of histological photographs of selected fields from three organs (heart, lung and thyroid) that were categorized as good and poor.
Table 1.
Overall slide quality sorted by organs
| Organ | Rating | ||
|---|---|---|---|
| Good (%) | Satisfactory (%) | Poor (%) | |
| Heart | 5 (15.2) | 27 (81.8) | 1 (3.0) |
| Lung | 5 (22.7) | 14 (63.7) | 3 (13.6) |
| Thyroid | 2 (20.0) | 6 (60.0) | 2 (20.0) |
| Thin skin | 0 (0.0) | 12 (100.0) | 0 (0.0) |
| Thick skin | 11 (84.6) | 2 (15.4) | 0 (0.0) |
| Bone | 9 (81.8) | 2 (18.2) | 0 (0.0) |
| Skeletal muscle | 6 (54.5) | 5 (45.5) | 0 (0.0) |
Figure 1.
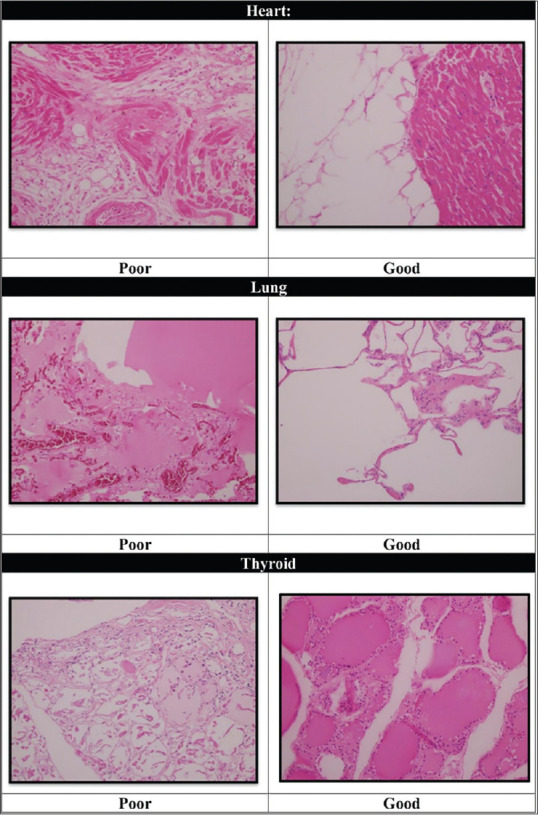
Examples of good and poor rating of tissue obtained from cadaveric heart, lung and thyroid (H & E, 20× magnification)
DISCUSSION
The present study showed that almost all the tissues obtained from embalmed cadavers were of good or satisfactory quality, and these findings are in agreement with those of a previous study.[8] This could be a testament to the quality of embalmment and fixation of the bodies, which are important factors in later obtaining high-quality samples. Moreover, the samples were collected from relatively new cadavers, which could also be a factor contributing to the overall good quality of the slides. It should be noted that the study used strict criteria that may have resulted in increased representation of “satisfactory” slides compared to “good;” nonetheless, such criteria were chosen to ensure that the slides are of adequate educational benefit.
Another finding of this study is that the quality of tissue preservation varies between organs. Although the exact reason for such disparity remains unclear, there are several factors that may have contributed to this observation. First, information about the individual circumstances of the body donors and their timing of death is lacking; this is important because the clots formed within the vascular system of the body during the death process might limit the quality of the fixation, and the delay from the timing of death until the initiation of the embalming process might alter the structure of tissues. Second, structural and vascular differences between the studied organs might explain why some organs deteriorate at faster rates. For example, the heart is fixated internally by the solution passing through its chambers and externally by the solution passing through the coronary arteries. The skin might be adequately preserved due to structural factors and the delivery of adequate fixation solution externally. The bones contain collagen fibers, which are highly durable structures that offer resilience to the bone and contribute to its long survival. The lungs, one of the organs that showed the highest percentage of “poor” slide rating in this study (13.6%), are supplied by fine capillaries, which might clot, and thus limit the fixation process. These factors might explain the reason behind the different qualities of preservation. To the best of our knowledge, this is the first study that investigated the histological quality of tissues obtained from cadaveric organs such as skin, muscle, bone and thyroid.
Cadavers are received from donors mostly with the intention to help advance medicine and its practice.[11,12,13,14] The results of this study emphasize that the yield obtained from cadavers can be of significant value in medical education when used efficiently. Currently, cadavers are used for educational purposes in anatomy laboratories for dissection and learning gross anatomy, but there is a shift away from classical microscopic histology education toward digital slides. This is certainly more convenient, but, unfortunately, students might lose their hands-on training and laboratory experience in disciplines such as histology and pathology.
Moreover, with the currently budding whole-body plastination, many are considering moving away all together from the wet dissection experience, as plastinated cadavers last for a longer time and can move the educational process from the laboratory to the classroom.[15] However, in our opinion, plastination should be used as a supplement to wet dissection, and not as a replacement. A 2016 study on veterinary students showed that students reported better learning experience when combining both modalities.[16]
This study suggests that tissue samples obtained by students during dissection sessions can be processed and used for their histology training. This would bridge the educational gap and create a more integrated experience in the medical education.
Using an integrated approach where students get to interact fully with their “ first patient”, the cadaver, starting from gross anatomy and going deeper into histology and possible histopathological findings, will allow them to develop a finer clinical sense and a deeper understanding of the human body. This will also introduce the students to the practical field of histology and pathology and widen their horizon for future specialties, which are not regularly encountered in the hospital setting. Furthermore, these expected benefits emphasize the importance of cadavers, dissection and histology in a system that is increasingly adopting a digitalized approach in medical education, resulting in the decline in the use of human cadavers and the exposure of the students to their potential benefit.[17,18,19,20]
Limitations and recommendations
A major limitation of this study was that the information about the clinical history of the body donors and their timing of death is lacking. Moreover, while the number of cadavers used in this study could provide useful data to achieve the objectives of the research, a study using a larger number of cadavers with a detailed clinical history would have allowed for a better extrapolation of results. Another limitation was that the intra-evaluator reliability was not measured, which would have helped establish the degree of confidence in the evaluator's ratings.
Future studies can include more organs not highlighted in the literature such as brain, spleen, testes, ovaries and pancreas. It would also be interesting to study how the slide quality translates into meaningful educational value when integrated in medical curricula.
CONCLUSION
This study found that almost all the tissues taken from cadavers were either of good or satisfactory quality, with thick skin and muscle being the best rated and thyroid and lung tissue being the worst. These results serve as the first step in establishing that histological slides obtained from embalmed cadavers can be useful additional educational tools in medical curricula.
Ethical considerations
Ethical approval for this study was obtained from the Institutional Review Board of Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia (IRB No.: IRB-UGS-2018-01-271), on December 12, 2018.
Peer review
This article was peer-reviewed by three independent and anonymous reviewers.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ghosh SK. Cadaveric dissection as an educational tool for anatomical sciences in the 21st century. Anat Sci Educ. 2017;10:286–99. doi: 10.1002/ase.1649. [DOI] [PubMed] [Google Scholar]
- 2.Knollmann-Ritschel BE, Regula DP, Borowitz MJ, Conran R, Prystowsky MB. Pathology competencies for medical education and educational cases. Acad Pathol. 2017;4:e2374289517715040. doi: 10.1177/2374289517715040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Burton JL. The autopsy in modern undergraduate medical education: A qualitative study of uses and curriculum considerations. Med Educ. 2003;37:1073–81. doi: 10.1046/j.1365-2923.2003.01710.x. [DOI] [PubMed] [Google Scholar]
- 4.Wood A, Struthers K, Whiten S, Jackson D, Herrington CS. Introducing gross pathology to undergraduate medical students in the dissecting room. Anat Sci Educ. 2010;3:97–100. doi: 10.1002/ase.136. [DOI] [PubMed] [Google Scholar]
- 5.Gopalan V, Dissabandara L, Nirthanan S, Forwood MR, Lam AK. Integrating gross pathology into teaching of undergraduate medical science students using human cadavers. Pathol Int. 2016;66:511–7. doi: 10.1111/pin.12448. [DOI] [PubMed] [Google Scholar]
- 6.Wood A, Whiten S, McVee J, Issberner J, Jackson D, Herrington CS. Histopathology from the dissecting room: Are cadavers a suitable source of educationally useful histopathology specimens? Anatomy. 2015;9:26–33. [Google Scholar]
- 7.Eisma R, Wilkinson T. From “silent teachers” to models. PLoS Biol. 2014;12:e1001971. doi: 10.1371/journal.pbio.1001971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rae G, Newman WP, 3rd, McGoey R, Donthamsetty S, Karpinski AC, Green J. The histopathologic reliability of tissue taken from cadavers within the gross anatomy laboratory. Anat Sci Educ. 2018;11:207–14. doi: 10.1002/ase.1743. [DOI] [PubMed] [Google Scholar]
- 9.Balta JY, Cronin M, Cryan JF, O'Mahony SM. Human preservation techniques in anatomy: A 21st century medical education perspective. Clin Anat. 2015;28:725–34. doi: 10.1002/ca.22585. [DOI] [PubMed] [Google Scholar]
- 10.Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15:155–63. doi: 10.1016/j.jcm.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bolt S, Venbrux E, Eisinga R, Kuks JB, Veening JG, Gerrits PO. Motivation for body donation to science: More than an altruistic act. Ann Anat. 2010;192:70–4. doi: 10.1016/j.aanat.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 12.Cornwall J, Perry GF, Louw G, Stringer MD. Who donates their body to science? An international, multicenter, prospective study. Anat Sci Educ. 2012;5:208–16. doi: 10.1002/ase.1278. [DOI] [PubMed] [Google Scholar]
- 13.Gunderman RB. Giving ourselves: The ethics of anatomical donation. Anat Sci Educ. 2008;1:217–9. doi: 10.1002/ase.39. [DOI] [PubMed] [Google Scholar]
- 14.Rokade SA, Gaikawad AP. Body donation in India: Social awareness, willingness, and associated factors. Anat Sci Educ. 2012;5:83–9. doi: 10.1002/ase.1263. [DOI] [PubMed] [Google Scholar]
- 15.Bamber AR, Quince TA, Barclay SI, Clark JD, Siklos PW, Wood DF. Medical student attitudes to the autopsy and its utility in medical education: A brief qualitative study at one UK medical school. Anat Sci Educ. 2014;7:87–96. doi: 10.1002/ase.1384. [DOI] [PubMed] [Google Scholar]
- 16.Sora MC, Latorre R, Baptista C, López-Albors O. Plastination: A scientific method for teaching and research. Anat Histol Embryol. 2019;48:526–31. doi: 10.1111/ahe.12493. [DOI] [PubMed] [Google Scholar]
- 17.Latorre R, Bainbridge D, Tavernor A, López-Albors O. Plastination in anatomy learning: An experience at Cambridge University. J Vet Med Educ. 2016;43:226–34. doi: 10.3138/jvme.0715-113R1. [DOI] [PubMed] [Google Scholar]
- 18.Bamber AR, Quince TA. The value of postmortem experience in undergraduate medical education: Current perspectives. Adv Med Educ Pract. 2015;6:159–70. doi: 10.2147/AMEP.S46669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marshall R, Cartwright N, Mattick K. Teaching and learning pathology: A critical review of the English literature. Med Educ. 2004;38:302–13. doi: 10.1111/j.1365-2923.2004.01775.x. [DOI] [PubMed] [Google Scholar]
- 20.Talmon G. The use of autopsy in preclinical medical education: A survey of pathology educators. Arch Pathol Lab Med. 2010;134:1047–53. doi: 10.5858/2009-0333-OA.1. [DOI] [PubMed] [Google Scholar]


