Abstract
The COVID-19 pandemic has caused monumental mortality, and there are still no adequate therapies. Most severely ill COVID-19 patients manifest a hyperactivated immune response, instigated by interleukin 6 (IL6) that triggers a so called “cytokine storm” and coagulopathy. Hypoxia is also associated with COVID-19. So far overlooked is the fact that both IL6 and hypoxia depress the abundance of a key anticoagulant, Protein S. We speculate that the IL6-driven cytokine explosion plus hypoxemia causes a severe drop in Protein S level that exacerbates the thrombotic risk in COVID-19 patients. Here we highlight a mechanism by which the IL6-hypoxia curse causes a deadly hypercoagulable state in COVID-19 patients, and we suggest a path to therapy.
Keywords: Protein S, hypoxia, cytokine storm, IL6, coagulopathy, ACE2, COVID-19
INTRODUCTION
The menacing SARS-CoV2 virus has caused a pandemic with over 6.9 million cases and around 400,000 deaths. As of to date (07/11/2020), there are more than 3.2 million confirmed cases and ~134,729 deaths in the U.S. Clinical features of patients admitted to the hospital with the viral disease COVID-19 are bilateral pneumonia, systemic inflammation, endothelial dysfunction, coagulation activation, acute respiratory distress syndrome, and multi-organ failure. Signs of myocardial injury are also observed in at least one quarter of severe cases. Although the lung is the main target organ, the virus can infect other tissues (small intestine, testis, kidneys, heart, thyroid, adipose tissue, colon, liver, bladder, adrenal gland [1]).
The infection risk of SARS-CoV2 has no remarkable correlation with age because the expression of the virus receptor ACE2 does not vary much between young and old; however, mortality is significantly higher in older people compared with the young, (Table 1). SARS-CoV2 infection was found to reduce the expression of ACE2 in lungs, leading to a renin-angiotensin system (RAS) dysfunction. This RAS dysfunction, in turn, would enhance inflammation and vascular permeability in the airways [2].
Table 1. Different parameters of COVID-19 patients.
| Place | Time and Date | No of patient | Sex | Age | Mortality | |
| Male | Female | |||||
| Netherlands[42] | 7th March - 5th April, 2020 | 184 | 139 | 45 | Average : 64 | 23 |
| Lombardy region of Italy[43] | 20th February -18th March, 2020 | 1591 | 1304 | 287 | Median : 63 | 405 |
| Italy[44] | Until 15th March, 2020 | 22512 | 13462 | 9050 | Median : 64 | 1625 |
| Zhongnan Hospital of Wuhan University in Wuhan, China[4] | 1st January to 13th March, 2020 | 449 | 268 | 181 | Average : 65.1 | 134 |
| Fatal Cases of COVID-19 from Wuhan China[20] | 9th January-15th February, 2020 | 85 | 62 | 23 | Median: 65.8 | All |
| Wuhan Jin Yin-tan Hospital, Wuhan, China[45] | Late December, 2019-26th January, 2020 | 52 | 36 | 17 | Average: 59.7 | 32 |
However, unlike the SARS-CoV pandemic in 2003, COVID-19 is not simply a disease of the upper respiratory tract. COVID-19 patients experience hypercoagulability and increased risk of venous thromboembolism (Table 2). These thrombotic complications have been referred to as thrombo-inflammation or COVID-19-associated coagulopathy [3–7]. Moreover, several reports indicate that hypercoagulability, as measured by the D-Dimer levels, is present mostly in critically ill and deceased patients (Table 2). In addition to blood clots of all sizes throughout the body, doctors who treat coronavirus patients report a range of other odd and frightening syndromes, such as kidney failure, cardiac inflammation, and immune complications. These syndromes appear to arise from a SARS-CoV2 virus-induced local inflammatory response.
Table 2. Studies which indicate that hypercoagulability (supra-physiological levels of D-dimer), is almost always associated with disease severity and mortality of COVID-19.
| Study | Sample size | Mean D-dimer (<0.5 μg/ml) | p-values | Comment |
| Tang et al, Feb 2020,[34] | Survivors (162) | 0.6 | <0.001 | Disseminated intravascular coagulation (DIC) was found in most deaths |
| Non-survivors (21) | 2.12 | |||
| Han et al, Mar 2020, [33] | Ordinary patient (49) | 2.14 ±2.88 | <0.001 | Huge increase in D-dimer in critically ill COVID patients |
| Critical (10) | 20.04 ± 32.39 | <0.05 | ||
| Wang et al, Mar 2020, [46] | ICU (36) | 4.14 | <0.001 | In the non-survivors, D-dimer increased continuously |
| Non-ICU (102) | 1.66 | |||
| Zhang et al, April 2020, [47] | Ordinary (276) | 0.41 | <0.001 | 12 non-survivors had D-dimer values greater than 2.0 |
| Severe (67) | 4.76 | |||
| Spiezia et al, April 2020, [48] | ICU (22) | 5.343 ±2.099 | <0.0001 | All ICU patients with acute respiratory failure showed severe hypercoagulability, one patient with the most hypercoagulable state died. |
| Ranucci et al, April 2020, [35] | Total (16) | 3.5 | 0.017 | Seven patients died of hypoxia and multi-organ failure |
| Tang et al, May 2020, [49] | Survivors (315) | 1.47 | <0.001 | 30 of the non survivors died even after treated with low molecular weight heparin |
| Non-survivors (134) | 4.7 |
Because of lung involvement, most COVID-19 patients have exceedingly low blood oxygen levels, but, inexplicably, some of these hypoxic patients hardly gasp for breath. Alarmingly, these individuals are subject, without warning, to sudden shortness of breath and massive pulmonary embolism [8]. Note that bleeding is rare in the current onset of the disease.
Our past studies [9–13] with the natural anticoagulant Protein S illuminated our understanding about the significance of Protein S -Factor IXa interaction in hemostasis. Further, we identified a critical role of Protein S in regulating hypoxia and associated thrombotic complications [9].
The overarching goal of this article is to propose a strategy to better control the hypoxemia associated hypercoagulability in severe COVID-19 patients.
Inflammation, coagulation and hypoxia
Inflammation, as a part of the innate immunity response to an infection, triggers activation of coagulation pathways. Activation of coagulation influenced by inflammation, in turn, can modulate the inflammatory response. The coordinated activation of both coagulation and inflammation during a severe infection is a well-recognized phenomenon known as thrombo-inflammation. Thrombo-inflammation is associated with microvascular thrombosis, hypoxemic respiratory failure, and, in extreme cases, it may lead to death due to development of multiple organ dysfunction syndrome (MODS) [14]. A disproportionate inflammatory response to SARS-CoV2 is associated with exorbitant circulating levels of inflammatory cytokines, which is thought to be a major cause of disease severity and death [15].
The main mediators of inflammation-activated coagulation are the pro-inflammatory cytokines [16]. In severe sepsis, the pro-inflammatory cytokines stimulate mononuclear cells expressing more and more tissue factor that initiate the coagulation pathways. Interleukin 6 (IL-6) is the most important cytokine that influences the expression of tissue factor which activates coagulation.
Thrombo-inflammation – occurs by overproduction of early response proinflammatory cytokines (TNFα, IL-6, and IL-1β) that create a “cytokine storm” [4, 15, 17–22]. This cytokine explosion leads to increased risk of vascular hyperpermeability, multi-organ failure, and eventually death when high cytokine concentrations persist [23, 24]. The inflammatory effects of cytokines also activate vascular endothelial cells and cause endothelial injury with resultant prothrombotic properties [25]. Independent transcriptome datasets from infection models revealed that IL6 is the major cytokine differentially expressed after infection with SARS- CoV2 [26–30].
Autopsies revealed microthrombi in lungs and other organs with associated foci of hemorrhage [31]. Such observations suggest that severe endothelial dysfunction, driven by the cytokine storm and associated hypoxemia, lead to disseminated intravascular coagulation and thromboembolic complications. Importantly, development of local hypoxia will progressively intensify endothelial cell disruption, tissue factor expression, and activation of the coagulation cascade, thereby establishing a deadly positive thrombo-inflammatory feedback loop with thrombosis and hemorrhage occurring in the small vessels of the lungs.
In summary, severe hypoxia is now considered associated with gravely ill COVID-19 patients, and IL6 is upregulated in COVID-19 and promotes cis and trans signaling to produce a cytokine storm [32]. Further, it is reasonable to conclude that subtle clotting begins early in the lungs, perhaps due to an inflammatory reaction in their fine web of blood vessels, which then sets off a cascade of proteins that prompt blood to clot and prevent proper oxygenation. Blood clots are clearly a major contributor to COVID-19 disease severity and mortality.
Crosstalk between thrombotic complications and inflammation/cytokine storm in SARS-CoV2 infection
Severity of COVID-19 is commonly associated with coagulopathy; disseminated intravascular coagulation (DIC) being the predominant condition along with high venous thromboembolism rates, and pulmonary congestion with microvascular thrombosis [33]. In general, hemostatic system alterations were indicated by prolonged aPTT, elevated platelet count, increased D-dimer level and fibrin degradation product for patients with severe COVID 19 [34]. Fibrin deposition in alveolar and interstitial lung spaces, in addition to microcirculation thrombosis, may exacerbate respiratory symptoms that require prolonged mechanical ventilation, and which are associated with poor prognosis and death. D-dimer levels have been identified as markers of severity of the disease and predictive of mortality [34]. Ranucci et. al. [35] incorporated viscoelastic tests for ICU patients along with the other commonly performed examinations. The test provides information about clot time (CT), clot strength (CS), fibrinogen contribution (FCS), and platelet contribution (PCS) to clot strength. Patient procoagulant profiles were confirmed by increased CS, FCS and PCS. Increased clot strength has been correlated to high fibrinogen level and somewhat to elevated platelet count.
COVID-19 disease severity is also associated with acute lung injury and hypoxemic respiratory failure, the most common cause of death. High levels of cytokines and chemokines associated with T cell depletion, pulmonary inflammation, and extensive lung damage have been documented in individuals who experienced similar viral respiratory diseases such as SARS and MERS. Thus, the wide-spread lung damage associated with this kind of infection may be caused more by an exaggerated immune response than by the virus itself. In addition, supraphysiological levels of IL-6, IL-10 and TNF-α have been found in the sera of severely ill COVID 19 patients [35]. Therefore, all patients with severe COVID-19 should be screened for excessive inflammation by measuring cytokine levels to stratify patients eligible for a specific immunosuppressive treatment [36].
The prevalence of both a cytokine storm and derangement of coagulation in critically ill COVID-19 patients signifies the aforesaid synergy between inflammation and coagulation. A clear association between increased IL-6 and fibrinogen level was reported for a set of COVID 19 ICU patients [35]. Recent guidance from the International Society on Thrombosis and Hemostasis (ISTH) stresses the need for monitoring coagulation parameters for patients who develop sepsis from the infection. The only widely available standard of care in this respect is a prophylactic dose of low molecular weight heparin, which should be considered for all COVID 19 patients (including non-critically ill) with high D-dimer levels, except for patients in whom anticoagulants are not advisable. For patients allergic to heparin, fondaparinux, a synthetic pentasaccharide, is an alternative. Fondaparinux has antithrombotic activity due to anti-thrombin-mediated selective inhibition of FXa. Systematic anticoagulation therapy for hospitalized COVID 19 patients is now routine treatment.
IL6, Hypoxia and Protein S
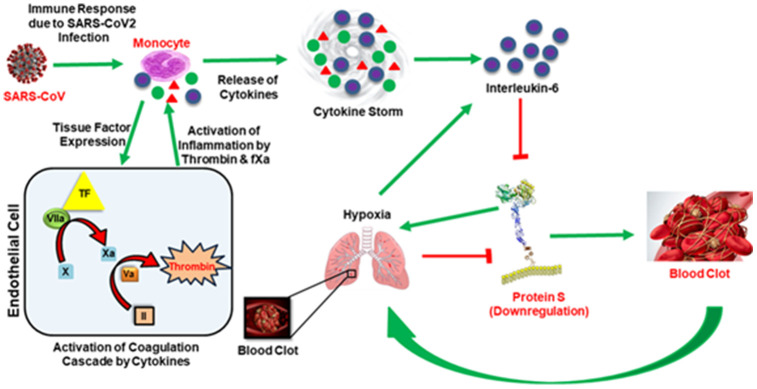
An overlooked aspect of hypoxia and the IL6-induced cytokine storm is that both factors downregulate a key anticoagulant, Protein S [9, 32] (Figure 1). For example, in a population of stroke patients, IL6 was upregulated, and it caused downregulation of Protein S that resulted in venous thrombosis [37]. We demonstrated that hypoxia downregulates Protein S expression in HepG2 cells [9]. Further, we showed that Protein S supplementation in thrombotic mice (mimicking hypoxic niche due to constitutive stabilization of HIF1α) plasma was able to alleviate the thrombotic risk [9]. Notably, addition of Protein S in normal mice plasma reduced thrombin generation as well [9]. These data indicate that Protein S supplementation could be useful in treating thrombotic complications. A substantial number of severe COVID-19 patients manifest both hypoxia and prothrombotic complications [34, 38–40] and we speculate that reduced Protein S level might play a key role in the disease progression of these patients.
Figure 1.
In the presence of the SAR-COV2 virus, early response proinflammatory cytokines (IL-6, TNFα, IL-1β etc.) are induced and activate the coagulation cascade by stimulating tissue factor (TF) expression from monocytes. The presentation of tissue factor leads to the formation of thrombin by the TF-VIIa pathway. Thrombin produces clots, and clots get wedged into arteries in the lungs and cause thrombotic complications and hypoxia. Hypoxia also induces IL-6. Simultaneously, thrombin augments inflammation and accelerates the production of proinflammatory cytokines, termed ‘cytokine storm’. Both cytokine storm and hypoxia downregulate Protein S, leading to coagulopathy. Green arrows represent upregulation and red blockage represent downregulation.
Ordinarily, Protein S deficiency is due either to homozygous or heterozygous genetic alteration, and Protein S deficiency can result from various pathological states and diseases. In all cases, Protein S deficiency is associated with a higher risk of venous thrombosis. Because both hypoxia and IL6-induced inflammation depress Protein S abundance, it’s reasonable to consider administration of Protein S as an effective therapy in severe Covid19 patients. Indeed, therapeutic heparin has improved the conditions of COVID-19 patients who experienced hypoxia. However, heparin targets FIXa, FXa and thrombin [41] through antithrombin. Therefore, direct administration of Protein S should have a highly specific anticoagulant effect in any thrombotic complications caused by Protein S deficiency. Of course, the possibility of bleeding would need attention, but, fortunately, even high doses of heparin have not caused bleeding in COVID-19 patients. Nonetheless, before Protein S administration can be deemed a new therapeutic approach, it is necessary to determine the extent to which Protein S is downregulated in a large cohort of COVID-19 patients. In view of the double curse of hypoxia and IL6, we expect Protein S deficiency to be severe in COVID-patients. However, we acknowledge that testing for safety and efficacy as well as FDA approval would be required before this approach could be implemented.
ACKNOWLEDGMENTS
We thank Dr. Howard Fried (UNC, Chapel Hill) for editorial assistance.
Footnotes
AUTHOR CONTRIBUTIONS: SC and TS - contributed to writing the first draft, assembling the references, and composing the Figure. SM - provided critical biological input, edited the final Figure and revised the resubmitted manuscript. RM- conceptualized the work and wrote the final draft.
CONFLICTS OF INTEREST: The author declares no conflicts of interest.
FUNDING: 2R01HL118557-06 to RM, ASH Bridge Award to RM.
REFERENCES
- 1.Li MY, Li L, Zhang Y, Wang XS. Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues. Infect Dis Poverty. 2020; 9:45. 10.1186/s40249-020-00662-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tay MZ, Poh CM, Rénia L, MacAry PA, Ng LF. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. 2020; 20:363–74. 10.1038/s41577-020-0311-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Connors JM, Levy JH. Thromboinflammation and the hypercoagulability of COVID-19. J Thromb Haemost. 2020; 18:1559–61. 10.1111/jth.14849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, Nigoghossian C, Ageno W, Madjid M, Guo Y, Tang LV, Hu Y, Giri J, et al. , and Global COVID-19 Thrombosis Collaborative Group, Endorsed by the ISTH, NATF, ESVM, and the IUA, Supported by the ESC Working Group on Pulmonary Circulation and Right Ventricular Function. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J Am Coll Cardiol. 2020; 75:2950–73. 10.1016/j.jacc.2020.04.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fogarty H, Townsend L, Ni Cheallaigh C, Bergin C, Martin-Loeches I, Browne P, Bacon CL, Gaule R, Gillett A, Byrne M, Ryan K, O'Connell N, O'Sullivan JM, et al. COVID19 coagulopathy in Caucasian patients. Br J Haematol. 2020; 189:1044–1049. 10.1111/bjh.16749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Becker RC. COVID-19 update: covid-19-associated coagulopathy. J Thromb Thrombolysis. 2020; 50:54–67. 10.1007/s11239-020-02134-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Levi M, Thachil J, Iba T, Levy JH. Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet Haematol. 2020; 7:e438–40. 10.1016/S2352-3026(20)30145-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ullah W, Saeed R, Sarwar U, Patel R, Fischman DL. COVID-19 complicated by acute pulmonary embolism and right-sided heart failure. JACC Case Rep. 2020; 2:1379–82. 10.1016/j.jaccas.2020.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pilli VS, Datta A, Afreen S, Catalano D, Szabo G, Majumder R. Hypoxia downregulates protein S expression. Blood. 2018; 132:452–55. 10.1182/blood-2018-04-841585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chattopadhyay R, Sengupta T, Majumder R. Inhibition of intrinsic xase by protein S: a novel regulatory role of protein S independent of activated protein C. Arterioscler Thromb Vasc Biol. 2012; 32:2387–93. 10.1161/ATVBAHA.112.250928 [DOI] [PubMed] [Google Scholar]
- 11.Plautz WE, Chattopadhyay R, Goldfeld EI, Samelson-Jones BJ, Pilli VS, Campello E, Datta A, Arruda VR, Simioni P, Majumder R. Padua FIXa resistance to protein S and a potential therapy for hyperactive FIXa. Thromb Res. 2018; 170:133–41. 10.1016/j.thromres.2018.08.018 [DOI] [PubMed] [Google Scholar]
- 12.Plautz WE, Sekhar Pilli VS, Cooley BC, Chattopadhyay R, Westmark PR, Getz T, Paul D, Bergmeier W, Sheehan JP, Majumder R. Anticoagulant protein S targets the factor IXa heparin-binding exosite to prevent thrombosis. Arterioscler Thromb Vasc Biol. 2018; 38:816–28. 10.1161/ATVBAHA.117.310588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fricke DR, Chatterjee S, Majumder R. Protein S in preventing thrombosis. Aging (Albany NY). 2019; 11:847–48. 10.18632/aging.101798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zaim S, Chong JH, Sankaranarayanan V, Harky A. COVID-19 and multiorgan response. Curr Probl Cardiol. 2020; 45:100618. 10.1016/j.cpcardiol.2020.100618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ, and HLH Across Speciality Collaboration, UK. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020; 395:1033–34. 10.1016/S0140-6736(20)30628-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Levi M, van der Poll T. Inflammation and coagulation. Crit Care Med. 2010; 38:S26–34. 10.1097/CCM.0b013e3181c98d21 [DOI] [PubMed] [Google Scholar]
- 17.Moore JB, June CH. Cytokine release syndrome in severe COVID-19. Science. 2020; 368:473–74. 10.1126/science.abb8925 [DOI] [PubMed] [Google Scholar]
- 18.Panigrahy D, Gilligan MM, Huang S, Gartung A, Cortés-Puch I, Sime PJ, Phipps RP, Serhan CN, Hammock BD. Inflammation resolution: a dual-pronged approach to averting cytokine storms in COVID-19? Cancer Metastasis Rev. 2020; 39:337–40. 10.1007/s10555-020-09889-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Henderson LA, Canna SW, Schulert GS, Volpi S, Lee PY, Kernan KF, Caricchio R, Mahmud S, Hazen MM, Halyabar O, Hoyt KJ, Han J, Grom AA, et al. On the alert for cytokine storm: immunopathology in COVID-19. Arthritis Rheumatol. 2020; 72:1059–63. 10.1002/art.41285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Du Y, Tu L, Zhu P, Mu M, Wang R, Yang P, Wang X, Hu C, Ping R, Hu P, Li T, Cao F, Chang C, et al. Clinical features of 85 fatal cases of COVID-19 from Wuhan. A retrospective observational study. Am J Respir Crit Care Med. 2020; 201:1372–79. 10.1164/rccm.202003-0543OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chau VQ, Oliveros E, Mahmood K, Singhvi A, Lala A, Moss N, Gidwani U, Mancini DM, Pinney SP, Parikh A. The imperfect cytokine storm: severe COVID-19 with ARDS in patient on durable LVAD support. JACC Case Rep. 2020; 2:1315–20. 10.1016/j.jaccas.2020.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chiappelli F, Khakshooy A, Greenberg G. CoViD-19 immunopathology and immunotherapy. Bioinformation. 2020; 16:219–22. 10.6026/97320630016219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Meduri GU, Kohler G, Headley S, Tolley E, Stentz F, Postlethwaite A. Inflammatory cytokines in the BAL of patients with ARDS. Persistent elevation over time predicts poor outcome. Chest. 1995; 108:1303–14. 10.1378/chest.108.5.1303 [DOI] [PubMed] [Google Scholar]
- 24.Magro C, Mulvey JJ, Berlin D, Nuovo G, Salvatore S, Harp J, Baxter-Stoltzfus A, Laurence J. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res. 2020; 220:1–13. 10.1016/j.trsl.2020.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Iba T, Levy JH. Inflammation and thrombosis: roles of neutrophils, platelets and endothelial cells and their interactions in thrombus formation during sepsis. J Thromb Haemost. 2018; 16:231–41. 10.1111/jth.13911 [DOI] [PubMed] [Google Scholar]
- 26.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020; 395:497–506. 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Conti P, Ronconi G, Caraffa A, Gallenga CE, Ross R, Frydas I, Kritas SK. Induction of pro-inflammatory cytokines (IL-1 and IL-6) and lung inflammation by coronavirus-19 (COVI-19 or SARS-CoV-2): anti-inflammatory strategies. J Biol Regul Homeost Agents. 2020; 34:1. 10.23812/CONTI-E [DOI] [PubMed] [Google Scholar]
- 28.McGonagle D, Sharif K, O’Regan A, Bridgewood C. The role of cytokines including interleukin-6 in COVID-19 induced pneumonia and macrophage activation syndrome-like disease. Autoimmun Rev. 2020; 19:102537. 10.1016/j.autrev.2020.102537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen X, Zhao B, Qu Y, Chen Y, Xiong J, Feng Y, Men D, Huang Q, Liu Y, Yang B, Ding J, Li F. Detectable serum SARS-CoV-2 viral load (RNAaemia) is closely correlated with drastically elevated interleukin 6 (IL-6) level in critically ill COVID-19 patients. Clin Infect Dis. 2020. [Epub ahead of print]. 10.1093/cid/ciaa449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ulhaq ZS, Soraya GV. Interleukin-6 as a potential biomarker of COVID-19 progression. Med Mal Infect. 2020; 50:382–83. 10.1016/j.medmal.2020.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Danzi GB, Loffi M, Galeazzi G, Gherbesi E. Acute pulmonary embolism and COVID-19 pneumonia: a random association? Eur Heart J. 2020; 41:1858. 10.1093/eurheartj/ehaa254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.de Wolf CJ, Cupers RM, Bertina RM, Vos HL. Interleukin-6 induction of protein s is regulated through signal transducer and activator of transcription 3. Arterioscler Thromb Vasc Biol. 2006; 26:2168–74. 10.1161/01.ATV.0000236202.39165.eb [DOI] [PubMed] [Google Scholar]
- 33.Han H, Yang L, Liu R, Liu F, Wu KL, Li J, Liu XH, Zhu CL. Prominent changes in blood coagulation of patients with SARS-CoV-2 infection. Clin Chem Lab Med. 2020; 58:1116–20. 10.1515/cclm-2020-0188 [DOI] [PubMed] [Google Scholar]
- 34.Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020; 18:844–47. 10.1111/jth.14768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ranucci M, Ballotta A, Di Dedda U, Bayshnikova E, Dei Poli M, Resta M, Falco M, Albano G, Menicanti L. The procoagulant pattern of patients with COVID-19 acute respiratory distress syndrome. J Thromb Haemost. 2020; 18:1747–51. 10.1111/jth.14854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sarzi-Puttini P, Giorgi V, Sirotti S, Marotto D, Ardizzone S, Rizzardini G, Antinori S, Galli M. COVID-19, cytokines and immunosuppression: what can we learn from severe acute respiratory syndrome? Clin Exp Rheumatol. 2020; 38:337–42. [PubMed] [Google Scholar]
- 37.Vila N, Reverter JC, Yagüe J, Chamorro A. Interaction between interleukin-6 and the natural anticoagulant system in acute stroke. J Interferon Cytokine Res. 2000; 20:325–29. 10.1089/107999000312478 [DOI] [PubMed] [Google Scholar]
- 38.Marongiu F, Grandone E, Barcellona D. Pulmonary thrombosis in 2019-nCoV pneumonia? J Thromb Haemost. 2020; 18:1511–13. 10.1111/jth.14818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tang N. Response to ‘Pulmonary thrombosis in 2019-nCoV pneumonia?’. J Thromb Haemost. 2020; 18:1513–14. 10.1111/jth.14843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Arachchillage DR, Laffan M. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020; 18:1233–34. 10.1111/jth.14820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hirsh J, Anand SS, Halperin JL, Fuster V. Mechanism of action and pharmacology of unfractionated heparin. Arterioscler Thromb Vasc Biol. 2001; 21:1094–96. 10.1161/hq0701.093686 [DOI] [PubMed] [Google Scholar]
- 42.Klok FA, Kruip MJ, van der Meer NJ, Arbous MS, Gommers DA, Kant KM, Kaptein FH, van Paassen J, Stals MA, Huisman MV, Endeman H. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020; 191:145–147. 10.1016/j.thromres.2020.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, Cereda D, Coluccello A, Foti G, Fumagalli R, Iotti G, Latronico N, Lorini L, et al. , and COVID-19 Lombardy ICU Network. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the lombardy region, Italy. JAMA. 2020; 323:1574–81. 10.1001/jama.2020.5394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Livingston E, Bucher K. Coronavirus disease 2019 (COVID-19) in Italy. JAMA. 2020. [Epub ahead of print]. 10.1001/jama.2020.4344 [DOI] [PubMed] [Google Scholar]
- 45.Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, Wu Y, Zhang L, Yu Z, Fang M, Yu T, Wang Y, Pan S, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020; 8:475–81. 10.1016/S2213-2600(20)30079-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020; 323:1061–69. 10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhang L, Yan X, Fan Q, Liu H, Liu X, Liu Z, Zhang Z. D-dimer levels on admission to predict in-hospital mortality in patients with covid-19. J Thromb Haemost. 2020; 18:1324–29. 10.1111/jth.14859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Spiezia L, Boscolo A, Poletto F, Cerruti L, Tiberio I, Campello E, Navalesi P, Simioni P. COVID-19-related severe hypercoagulability in patients admitted to intensive care unit for acute respiratory failure. Thromb Haemost. 2020; 120:998–1000. 10.1055/s-0040-1710018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020; 18:1094–99. 10.1111/jth.14817 [DOI] [PMC free article] [PubMed] [Google Scholar]