Abstract
Background
In resource-limited contexts, available data indicate that people with disability are disproportionally affected by the HIV epidemic. While disability resulting from chronic HIV infection has received some attention, few epidemiologic studies have examined the vulnerability of people with disability to HIV acquisition. The aims of the study were as follows: to estimate and compare HIV prevalence among people with and without disability living in Bujumbura, Burundi; to examine how the interaction among disability, gender and socioeconomic environment shapes vulnerability to HIV; and to identify potential pathways to higher HIV risk.
Methods
In this cross-sectional population-based study, 623 persons with disability (302 with disability onset ≤10 years [“early disability”]) and 609 persons without disability matched for age, sex and location were randomly selected to be tested for HIV and to participate in an interview about their life history, their social environment and their knowledge of sexual health.
Findings
A total of 68% of men and 75% of women with disability were affected by multidimensional poverty compared to 54% and 46% of their peers without disability (p<0.0001). Higher HIV prevalence was observed among women with disability (12.1% [8.2–16]) than among those without (3.8% [1.7–6], ORa 3.8, p<0.0001), while it was similar among men with disability and those without (p = 0·8). Women with disability were also at higher risk of sexual violence than were those without (ORa 2.7, p<0.0001). The vulnerability of women with early disability to HIV was higher among those who were socially isolated (HIV prevalence in this group: 19% [12–27]). In addition, education level and sexual violence mediated 53% of the association between early disability and HIV (p = 0.001).
Interpretation
This study highlights how the intersection of disability, gender and social environment shapes vulnerability to HIV. It also shows that the vulnerability to HIV of women who grew up with a disability is mediated by sexual violence.
Funding
This research was funded by the Netherlands Organization for Scientific Research (Grant W08.560.005) and the Initiative HIV-TB-Malaria (new name of the organisation)
Keywords: Disability, HIV, Sexual violence, Gender, Intersection, Sub-Saharan African
Research in context.
Evidence before this study
A recent population-based study conducted in Cameroon in 2015, which used a probability-based sampling design and included a control group, showed higher prevalence of HIV among men and women with disability compared to controls matched for sex and age. Most of the other published studies that have examined the prevalence of HIV infection among people with disability living in African contexts have methodological limitations and showed heterogenous results. Therefore, additional evidence is needed with data collected in other settings. In addition, the understanding of the factors influencing the association between HIV and disability remains poorly understood and more research is important to better identify the factors shaping the HIV and disability intersection.
Added value of this study
This study was designed to provide quality evidence on the intersection between HIV and disability. First of all, it confirms the higher prevalence of HIV infection among women with disability compared to those without and shows how the intersection of disability, gender and social environment shapes the vulnerability to HIV. In addition, this study highlights the important role of sexual violence in women with disability's vulnerability to HIV.
Implications of all the available evidence
This research adds strength to the growing evidence showing the vulnerability of women with disability to HIV infection and indicates areas for future interventions. It also show the complexity of the intersection between HIV and disability and the need for more specific studies.
Alt-text: Unlabelled box
1. Introduction
In resource-limited contexts, people with disability are disproportionally affected by the HIV epidemic [[1], [2], [3], [4], [5]]. Available studies have found that HIV prevalence is at least twice as high among people with disability compared to the general population [3,4]. There are various pathways that could result in this high burden of HIV among people with disability, and a better understanding of the HIV-disability relation is necessary to develop relevant interventions. First, disability can be a consequence of HIV infection. There is an increasing body of literature showing that chronic HIV infection remains associated with various impairments and functional limitations despite the tremendous progress made in the treatment of HIV/AIDS over the last several decades [[6], [7], [8]]. According to available studies, between one-quarter and one-half of the people living with HIV and treated with antiretroviral therapy (ART) experience some form of activity limitation [6,[9], [10], [11], [12], [13], [14]]. On the other hand, people with disability can be at increased risk of acquiring HIV infection. In contrast to the former direction, this direction of the relationship between HIV and disability has been less examined. Most of the data available come from qualitative research [2], which offers important insight into the contextual factors associated with vulnerability to HIV among people with disabilities but has more limited empirical generalizability. Epidemiological evidence on the vulnerability to HIV infection among people who grow up with disability (early disability) is therefore needed to help decision-makers prioritize interventions towards this group.
Although biological and behavioral risk factors have been the main focus of epidemiologic research until recently, there is increasing awareness that HIV infection results more from the social and economic constraints surrounding people than from their individual choices [15,16]. Economic deprivation, social isolation and power inequality shape individual HIV-related behaviors, thereby creating risk environments [[17], [18], [19]]. In the case of people with disability, the social vulnerability resulting from disability is likely to play an important role in HIV risk. There is consistent evidence showing that people with disability are at higher risk of multidimensional poverty, which includes a lack of education, a lack of access to health services and employment and other forms of social exclusion [11,20]. All of these conditions are well-established determinants of negative health outcomes [[12], [13], [14]]. However, the relation between poverty and HIV infection is more complex, and discordant findings have been reported, suggesting that contextual factors may modify the direction of this relation; therefore, these factors need to be examined [21,22]. Interpersonal factors related to partnerships and to social networks also influence the risk of HIV acquisition [[23], [24], [25]] and possibly intersect with poverty. For instance, economic constraints can push people to engage into risky sexual activities such as sex work [26]. At the intersection between the structural and interpersonal levels, sexual violence merits special attention, as it is associated with HIV infection, poverty and disability [27,28]. However, little is known about the intersection between HIV risk and sexual violence among men and women with disability.
Building on previous research conducted in Cameroon [3], we conducted a population-based survey in Bujumbura, Burundi, to estimate and compare the prevalence of HIV infection among people with and without disability. In this analysis, in addition to reporting on HIV prevalence, we examined how it varies across the intersection of gender, disability and categories related to the social and economic environment and whether it was associated with other adverse sexual events like sexual violence and risky sexual activities. More specifically, we aim to provide answers to the following questions: 1) among people with disability, how can the most vulnerable persons to HIV infection be identified so that they can be prioritized, and 2) what are the potential pathways to higher HIV risk that could be targeted by intervention?
2. Methods
2.1. Study design and sampling strategy
This cross-sectional study took place in Bujumbura between 20 December 2017, and 20 December 2018. A two-stage sampling strategy was used to randomly select people with and without disability from the general population. In the first stage, enumeration areas that have been defined for the 2016 DHS were sampled with probability proportional to the number of households. The total number of enumeration areas was 16,244. Each sampled enumeration area was enumerated again in an exhaustive way to update the data. Then, 100 households were randomly sampled in each sampled enumeration area from the updated list of households and contacted for the second stage. During this stage, study interviewers collected general information on the households and used the Washington Group disability questionnaire with each households’ member to ascertain the presence of activity limitation and, thereby, identify people with disabilities eligible for the study. People without disabilities of similar age, sex and residential area were randomly sampled from the list of eligible household members without functional limitation. A sample size of 600 participants with disability was targeted to detect with a power ≥80% and an alpha risk set at 5% a prevalence ratio of HIV infection or of sexual violence ≥1·5 among participants with disability compared to controls under the assumptions that these prevalence range from 10 to 50% and that 10% of the subjects may refuse the HIV test.
2.2. Study population
All people aged 15 to 49 years with severe difficulties performing basic activities in at least one domain of the Washington Group Short Set (WGSS) or with moderate difficulties in at least two domains for ≥12 months were considered to have a disability and eligible for the study [20]. The WGSS covers six functional domains: seeing, hearing, walking, cognition, self-care, and communication (see details in Appendix A). For each person with disability included in the study, a person of similar age and sex who was living in the same enumeration area but in a different household and who did not meet the functional limitation criteria was recruited.
2.3. Procedures
Face-to-face structured interviews were conducted with eligible subjects identified from the screening stage after informed consent is granted. During the informed consent process, special attention was given to provide adapted information to people with intellectual and/or hearing disabilities, for instance using pictogram. For people with intellectual disabilities and minors, informed consent was sought from both participants and from their representatives. These interviews were conducted in the subjects’ homes or in another place when asked. Eligibility of the participant was first confirmed with the Washington Group questions.
Then, the following data were collected during the interview: activity limitations; economic characteristics; social participation and social environment; knowledge, attitudes and behaviors regarding HIV and sexual and reproductive health; experience of physical and sexual violence; and life-course history of employment, resources, sexual partnership and fertility.
2.4. Research tools
The life-grid method was used to retrospectively collect the life-course data [29,30] (Appendix A). Knowledge of HIV transmission and prevention was assessed through open questions. Social participation was assessed with the participation scale [31]. This scales includes 18 questions and provides a global score ranging from to 0 to 90. Social participation restriction was defined as a participation score >12. Different components of the social environment were explored. First, difficulties in accessing health care and difficulties in daily life resulting from the attitudes of other people were assessed on a four-point scale. Second, social capital was another aspect of the social environment used in the analysis. It is a multifaceted concept that can be loosely defined as the resources available from the community [32]. Two dimensions of social capital were distinguished: structural social capital, which refers to the presence of community linkage, and cognitive social capital, which refers to the appreciation of this linkage in terms of trust, mutual help and reciprocity [33,34]. Structural social capital was measured by the reported number of persons (friends or family) who could provide help to the participant if needed. Cognitive social capital was measured with the sub-scale of the Short Social Capital Assessment Tool (SASCAT) [35]. It provides a score ranging from 0 to 4 that was further dichotomized into low cognitive social capital (1–2) and high cognitive social capital (3–4), as suggested by De Silva et al. [35]. The list of the scales used in this study is provided in Table 1.
Table 1.
Overview of questionnaires and scales used in the HandiSSR.
| Scale name | Measurement | Type of scale | No of items | Reliability (alpha) | Dimensionality [56] |
|---|---|---|---|---|---|
| Washington Group questionnaire on disability (short and extended sets) [51] | Activity limitations for basic activities (mobility, seeing, hearing, taking care of oneself, remembering or concentrating, communicating) | Ordinal scale (4 points Likert scale) | 6 in the short set + 2 in the extended set added | NA | NA |
| Participation scale [31] | Social participation | Ordinal scale. Provides a score ranging from 0 to 90 | 18 | 0.98 | EFA: single factor explains 72% CFA (one factor): chi2 634.1, p<0.0001 |
| Short Social Capital Assessment Tool (ASCAT) [35] | Structural and cognitive social capital (SC). Only cognitive social capital subscale was used in this study. | Ordinal scale Structural SC: score from 0 to 20 Cognitive SC: score from 1 to 4 |
9 Structural SC: 5 Cognitive SC: 4 |
Structural SC: 0.68 Cognitive SC: 0.85 |
Structural SC - EFA: single factor explains 44% of variance - CFA (one factor): chi2 4.8, p = 0.091 Cognitive SC: - EFA: single factor explains 62% of variance - CFA (one factor): chi2 14.7, p = 0.001 |
| Craig Hospital Inventory of Environmental Factors (CHIEF) Short-Form [57,58] | Effect of environmental factors on functioning and social participation | Ordinal scale (4 points Likert scale) | 12 in the original version but only 5 in the survey | 0.91 | - EFA: single factor EFA explains 66% of variance - CFA (one factor): chi2 19.4, p = 0.002 |
| Knowledge and attitude on HIV, sexuality and reproductive health | Questions derived from the “Illustrative questionnaire for interview-survey with young people” designed by Cleland et al. [59]. | Open and closed questions | 34 items | NA | NA |
| Access to sexual and reproductive health services | Inspired from a questionnaire developed by the NGO Humanity & Inclusion | Mixed (open and closed questions, visual rating scale) | 7 items | NA | NA |
| Abuse assessment screeen - disability (AAS-D) [60] | Explore abuse, physical and sexual violence. Derived from AAS-D (item 3 removed) | Mixed (nominal and ordinal) | 8 items | NA | NA |
| Transactional sex and sex in exchange for money | Questions included in the DHS surveys (optional) [61] | Ordinal | 2 items | NA | NA |
| Social network index [62] | Questions adapted from the social network index exploring availability of social support. | Ordinal | 6 items | NA | NA |
EFA: exploratory factorial analysis; CFA: confirmatory factorial analysis; TLI: Tucker-Lewis index; CFI: Comparative Fit Index; RMSEA: root mean square error of approximation.
In addition to the interview, participants were offered voluntary HIV counselling and testing. HIV infection was initially screened using the sensitive rapid blood test Parallel Determine® (Abbott, Japan) and confirmed using the HIV 1/2 Stat-pak® (Chembio Diagnostic Systems) assay. Test results were communicated after the interview to people who desired them. The proportion of participants who refused the test was 3.2%.
2.5. Statistical analysis
The primary outcome was the prevalence of HIV infection among participants with and without disability. It was estimated accounting for the sampling design for the following groups: men and women with disability, men and women without disability, men and women with disability onset before 10 years as a proxy of people who grew up with disability (“early disability”), and men and women with disability onset after 10 years (“late disability”). The Mantel-Haenzel method and logistic regression adjusted for age (<30, [30–40), ≥40) were used to compare binary outcomes between the different groups. As a sensitivity analysis, the E-value approach was used to assess the potential effect of unmeasured confounding on the estimated associations [36]. In short, the E-value represents the minimum strength of association that an unmeasured confounder would need to have with both disability and HIV-infection to fully explain away the disability - HIV association.
We adopted a socio-ecological framework to describe the multiple levels of influence (e.g., individual, social environment) on HIV risk. More specifically, we assessed if the association between disability and HIV varied across economic and social environmental categories or in the presence of violence or risky sexual activity. This analysis was restricted to women because of the excessively small number of such events among men. Different economic and social indicators were considered to define the economic and social categories, as no single indicator can capture the multiple aspects of poverty or of the social environment [37]. Economic indicators for poverty included low household wealth index, low education level, important difficulties in accessing health care and reduced lifetime participation in education or work (see Table 2 for detailed definitions of the indicators). For the social environment, the social support network size, the cognitive social capital score and the presence of important difficulties related to the attitude of other people were used in the analysis. Economic and social indicators were considered separately and were combined into a multidimensional index (MPI) by summing them up in a second step [37]. Two distinct variables were used for risky sexual activity: reported multiple and/or casual relationships and reported sexual activity in exchange for money. Modification of the association between disability and HIV infection by factors related to economic or social categories, violence and risky sexual activity was assessed using the relative excess risk due to interaction (RERI), the synergy index (SI) and the attributable proportion (AP) after estimating the odds ratio (OR) of HIV infection for each stratum defined by disability and factor levels, with participants without disability and from the better-off category as the reference groups [38] (Appendix B). This analysis was conducted for the entire sample and by disability subgroup (early versus late disability). In addition, in the subset of participants with early disability onset, further analysis was performed to identify whether education, social capital, violence and risky sexual activity mediate the HIV disparities associated with disability [39]. The potential outcome approach was used to conduct this mediation analysis, as detailed in the appendix [40] (Appendix B). The mediation analysis was adjusted for childhood poverty, measured by the education level of each parent, the characteristics of paternal work (paid versus not paid), and the occurrence of food insecurity at age 10, which is a potential confounding factor of the associations between disability and HIV and the mediating factors. Missing values were not imputed. All analyses were performed using R [41].
Table 2.
Definitions of categories and factors.
| Label | Definition | Categories |
|---|---|---|
| Education and living conditions | ||
| Household wealth | Index computed from household assets using principal component analysis [63] | First quartile versus quartiles 3 to 4 |
| Educational achievement | Highest completed level of education | Primary level not completed versus higher level |
| Lifetime participation in education or work | Proportion of one's lifetime since age 10 year during which the participant was studying or working Time spent working or studying (years) since age 10/(age at survey – 10) |
Reduced lifetime participation: <75% in women and <90% in men (versus ≥75% in women and ≥90% in men) |
| Access to health care | Over the last 12 months, was access to health care an important/moderate/small/no problem? | Important problem versus moderate or less |
| Social resources and environment | ||
| Social support network | Number of friends or family members who could provide help to the participant if needed | Low social support: ≤1 versus >1 |
| Cognitive social capital score | ASCAT subscale (score ranging from 0 to 4) | Low score: 1 – 2 versus high score: 3 - 4 |
| Other people's negative attitudes | Over the last 12 months, was the attitude of other people an important/moderate/small/no problem? | Important problem versus moderate or less |
| Multidimensional poverty index | Index combining low education level, low household wealth, reduced lifetime participation in work/education, low social network and low cognitive social capital | Coded 1 if at least two indicators indicate poverty (i.e., if the sum of the indicators >1) |
| Violence | ||
| Physical violence | Frequent physical violence reported by participant | Yes versus no |
| Sexual violence | Any unwanted sex reported by participant on one of the questions | Yes versus no |
| Sexual activities | ||
| Multiple / casual partners | Other sexual partner(s) while already engaged in a long term relationships (>12 months) and/or any short term relationship (<12 months) This information was collected with the life-course grid |
Yes or no |
| Sex in exchange for money | Any sexual intercourse in exchange for money | Yes or no |
The final protocol was approved by the “Comité National d'Ethique pour la Protection des Etres Humains participants à la Recherche Biomédicale et Comportementale” in Burundi (No. 214/CAB/SN/243/2017) and “Comité Consultatif de Déontologie et d'Ethique” from the Institut de Recherche pour le Développement.
The STROBE guidelines were used to ensure the reporting of this study (Appendix C) [42]. The dataset used for this analysis is available at Zenodo (http://doi.org/10.5281/zenodo.3885141 )
2.6. Funding
Netherlands Organization for Scientific Research (Grant W08.560.005) and the Initiative HIV-TB-Malaria (new name of the organisation). The funding sources was not involved in the writing of the manuscript nor in the decision to submit it for publication.
3. Results
3.1. Study participants characteristics
Of the 43,339 persons initially screened for disabilities, 623 persons with disability (302 with disability onset before 10 years) and 609 persons without disability were eventually included in the study (Fig. 1). The demographic and socioeconomic characteristics of the participants are displayed in Table 3. In analyses adjusted for age and sex, people with disability achieved lower education levels (p<0.0001), lived in more deprived households (p = 0.03), were more likely to report food insecurity during childhood (p = 0.0005), and had reduced lifetime participation in education or work (p<0.0001). Participants with early disability had the lowest education levels (p = 0.0003) and the shortest lifetime participation in education or work (p = 0.07), while those with later disability onset were more likely to live in poorer households (p = 0.07).
Fig. 1.
Study flowchart.
Table 3.
Study participant characteristics.
| Participants with disability |
Participants without disability | |||
|---|---|---|---|---|
| All participants with disability | Disability onset before age 10 years | Disability onset >10 years | ||
| Men | N = 319 | N = 155 | N = 164 | N = 312 |
| Age, median (IQR) | 28 (21 – 38) | 24 (19 – 31) | 34·5 (26 – 41) | 28 (21 – 37) |
| Education level, n (%) | ||||
| Never been to school | 54 (17) | 33 (21) | 21 (13) | 12 (4) |
| < Primary level | 51 (16) | 34 (22) | 17 (10) | 15 (5) |
| Primary | 73 (23) | 20 (13) | 53 (32) | 64 (20) |
| Secondary | 65 (20) | 25 (16) | 40 (24) | 84 (27) |
| Higher education level | 11 (3) | 5 (3) | 6 (4) | 37 (12) |
| Still a student | 65 (20) | 38 (25) | 27 (17) | 100 (3) |
| Food insecurity | ||||
| N (%) reporting | 225 (70·5) | 100 (64·5) | 125 (76·2) | 240 (77) |
| Household wealth index | ||||
| Median score (IQR) | −0·32 (−0·56 to 0·33) | −0·32 (−0·56 to 0·57) | −0·54 (−0·56 to −0·15) | −0·32 (−0·56 to 0·41) |
| Lifetime participation in work and education | ||||
| % of lifetime working or studying, median (IQR) | 62 (23 – 95) | 57 (12 – 100) | 67 (31 – 91) | 92 (70 - 100) |
| Social participation scale | ||||
| Median score (IQR) | 23 (10 - 42) | 31 (12 – 47) | 19 (6 – 37) | 0 (0 – 1) |
| N (%) with score >12 | 202 (70) | 105 (77) | 97 (63) | 1 (0·5) |
| Missing | 30 | 11 | 19 | 6 |
| Social capital | ||||
| No of people close to the respondentc who could bring support, median (IQR) | 2 (1 – 4) | 2 (1 – 4) | 2 (1 – 4) | 3 (2 – 5) |
| N (%) with low cognitive social capital score | 108 (34) | 59 (38) | 49 (30) | 45 (14) |
| Environmental barriers: n (%) reporting important difficulties in | ||||
| Transportation | 102 (32) | 51 (33) | 51 (31) | 5 (2) |
| Missing | 2 | 0 | 2 | 0 |
| Access to information | 108 (35) | 71 (47) | 37 (23) | 5(2) |
| Missing | 6 | 2 | 4 | 0 |
| Access to health services | 139 (44) | 72 (47) | 67 (41) | 11 (4) |
| Missing | 2 | 1 | 1 | 0 |
| Related to the attitude of other people | 62 (20) | 35 (23) | 27 (17) | 4 (1) |
| Missing | 5 | 2 | 3 | 0 |
| Aid for daily tasks | 127 (40) | 65 (43) | 62 (38) | 29 (9) |
| Missing | 4 | 1 | 3 | 0 |
| Participation in organizations for disabled persons | 23 (8) | 15 (10) | 8 (5) | – |
| Multidimensional poverty, n (%) | 51 (68) | 23 (64) | 28 (72) | 108 (54) |
| Activity limitation, n (%)a | ||||
| Mobility | 113 (35) | 48 (31) | 65 (40) | – |
| Visual | 36 (11) | 15 (10) | 21 (13) | – |
| Hearing | 48 (15) | 31 (20) | 17 (10) | – |
| Intellectual or mentalb | 105 (33) | 65 (42) | 40 (24) | – |
| Women | N = 304 | N = 147 | N = 157 | N = 297 |
| Age, median (IQR) | 32 (23 – 41) | 25 (19 – 35) | 37 (30 – 44) | 30 (23 – 39) |
| Education level | ||||
| Never been to school | 61 (20) | 32 (22) | 29 (19) | 26 (9) |
| < Primary level | 52 (17) | 21 (14) | 31 (20) | 19 (6) |
| Primary | 76 (25) | 37 (25) | 39 (25) | 58 (20) |
| Secondary | 68 (22) | 23 (16) | 45 (29) | 108 (36) |
| Higher education level | 11 (4) | 4 (3) | 7 (4·5) | 23 (8) |
| Still student | 36 (12) | 30 (20) | 6 (4) | 63 (21) |
| Food insecurity | ||||
| N (%) reporting | 213 (70) | 95 (65) | 118 (75) | 216 (73) |
| Household wealth index | ||||
| Median score (IQR) | −0.32 (−0.56 to 0.39) | −0.2 (−0.56 to 0.09) | −0.52 (−0.56 to 0.29) | −0.32 (−0.56 to 0.33) |
| Time spent in activity | ||||
| Time spent in activity (work/study) | 38 (11–81) | 47 (8–100) | 32 (12–67) | 79 (35–100) |
| Social participation scale | ||||
| Median score (IQR) | 26 (13–44) | 29 (15–50) | 25 (12–37) | 0 (0–2) |
| N (%) with score >20 | 214 (78) | 107 (81) | 107 (75) | 5 (2) |
| Missing | 29 | 15 | 14 | 14 |
| Social capital | ||||
| No of people close to the respondentc who could bring support, median (IQR) | 2 (1–4) | 2 (1–4) | 2 (1–4) | 3 (2–5) |
| N (%) with low cognitive social capital score | 127 (42) | 72 (49) | 55 (35) | 46 (16) |
| Environmental barriers: n (%) reporting Important difficulties in | 17 (11) | 9 (5.5) | ||
| Transportation | 109 (36) | 58 (40) | 51 (33) | 15 (5) |
| Missing | 2 | 1 | 1 | 1 |
| Access to information | 94 (32) | 55 (39) | 39 (25) | 7 (2) |
| Missing | 6 | 1 | 5 | 1 |
| Access to health services | 150 (49) | 70 (48) | 80 (51) | 24 (8) |
| Missing | 0 | 0 | 0 | 1 |
| Related to the attitude of other people | 81 (27) | 43 (30) | 38 (25) | 5 (2) |
| Missing | 5 | 2 | 3 | 0 |
| Aid for daily tasks | 136 (45) | 71 (49) | 65 (42) | 36 (12) |
| Missing | 4 | 1 | 3 | 0 |
| Participation in organizations for disabled persons | 26 (8.2) | 17(11) | 9 (5.5) | – |
| Multidimensional poverty, n (%) | 46 (75) | 22 (82) | 24 (71) | 76 (46) |
| Activity limitation, n (%)a | ||||
| Mobility | 97 (32) | 52 (35) | 45 (29) | – |
| Visual | 54 (18) | 20 (14) | 34 (22) | – |
| Hearing | 49 (16) | 33 (22) | 16 (10) | – |
| Intellectual or mentalb | 82 (27) | 49 (33) | 33 (21) | – |
Regarding the social environment, people with disability reported a smaller social support network (p<0.0001) as well as lower scores for social participation (p<0.0001) and for cognitive social capital (p<0.0001). The prevalence of multidimensional poverty was significantly higher among participants with disability than among those without (p < 0.0001), without a difference between those with early versus late disability onset (p = 0.8).
3.2. HIV prevalence and other outcomes
Higher HIV prevalence was observed among women with disability than among women without disability (age-adjusted OR [ORa]: 3.8, 95%CI: 1.9 - 7.6, p<0·0001), while the prevalence of HIV infection was similar among men with disability and men without disability (p = 0.8, Table 4). This translated into a significant additive interaction with a synergy index of 4.3, 95%CI 1.2–16 (RERI: 7, 95%CI 0–14 and AP: 69%, 95%CI 44–94). In other words, the intersection of sex and disability was responsible for a 4-fold increase in the OR of HIV infection compared to the effects of sex or disability alone. Because of the low prevalence of HIV infection observed among men (1.6%, 95%CI 0·8–2.5, n = 10), the remaining results on HIV are restricted to women. In the age-adjusted analysis, the ORs of HIV infection were 4.6 (95%CI 2.2–9.7) in women with late disability and 3.0 (95%CI 1.2–7.4) in those with early disability compared to participants without disability. The E-values for these ORs were 8.7 and 5.4, respectively, meaning that the OR between HIV and an unmeasured confounder should be greater than 8.7 and 5.4, respectively, to explain the observed OR between disability and HIV.
Table 4.
Prevalence of HIV infection and sexual violence among men and women with and without disability, overall and by subgroups (disability onset before and after 10 years, overall and with restricted social participation [participation score≥12]).
| Men |
Women |
|||||||
|---|---|---|---|---|---|---|---|---|
| HIV infection |
Sexual violence |
HIV infection |
Sexual violence |
|||||
| N | % (95%CI) | N | % (95%CI) | N | % (95%CI) | N | % (95%CI) | |
| Participants without disability | 301 | 1.3 (0.1–2.6) | 303 | 2.9 (1.2–4.6) | 286 | 3.8 (1.7–6) | 297 | 12.1 (8.2–16.0) |
| Participants with disability | ||||||||
| Overall | 309 | 1.9 (0.5–3.4) | 309 | 2.8 (1.2–4.5) | 296 | 13.5 (9.5–17·5) | 303 | 23.8 (18.9–28.6) |
| Onset before age 10 years | ||||||||
| All subjects in this subset | 152 | 0.7 (0.1–3.6) | 155 | 0.6 (0.1–3.6) | 144 | 7.6 (4.3–13.2) | 146 | 18.5 (13–25.6) |
| Restricted social participation | 103 | 1 (0–2.9) | 107 | 1 (0–2.8) | 104 | 7.7 (2·2–13.1) | 106 | 17.9 (10.5–25.4) |
| Onset after age 10 years | ||||||||
| All subjects in this subset | 157 | 1.9 (0.8–4.4) | 271 | 2.6 (1.3–5.2) | 242 | 14 (10.2–18.9) | 248 | 21.4 (16.7–26.9) |
| Restricted social participation | 92 | 4.3 (0.5–8.2) | 96 | 4.2 (0.1–8.2) | 104 | 24.0 (15.5–32.5) | 105 | 32.7 (23.3–42.1) |
Women with disability were also at increased risk of sexual violence (Table 4): the age-adjusted OR for sexual violence was 2.7 (95%CI 1.6–4.4) in women with late disability onset and 1.8 (95%CI 1–3.1) in those with early disability onset compared to participants without disability. The prevalence of sexual violence was similar among men with disability and those without (p = 1).
Risky sexual activities were reported with a similar frequency by women without and with late disability (49% and 50%, respectively, p = 0·8) but less often by those with early disability (32%, p = 0.0007). In contrast, risky sexual activities were more often reported by men without disability (64%) than by those with late (53%, p = 0.001) or early (34%, p<0.0001) disability. Sexual activities in exchange for money were more frequent among women with late disability onset (15%) than among those without or with early disability (3.4% and 4%, respectively; p = 0.0002). Few men reported having had sex in exchange for money (without disability: 3%, with late disability onset: 2%, with early disability onset: 1·3%; p = 0.6).
3.3. Risk factors and interactions
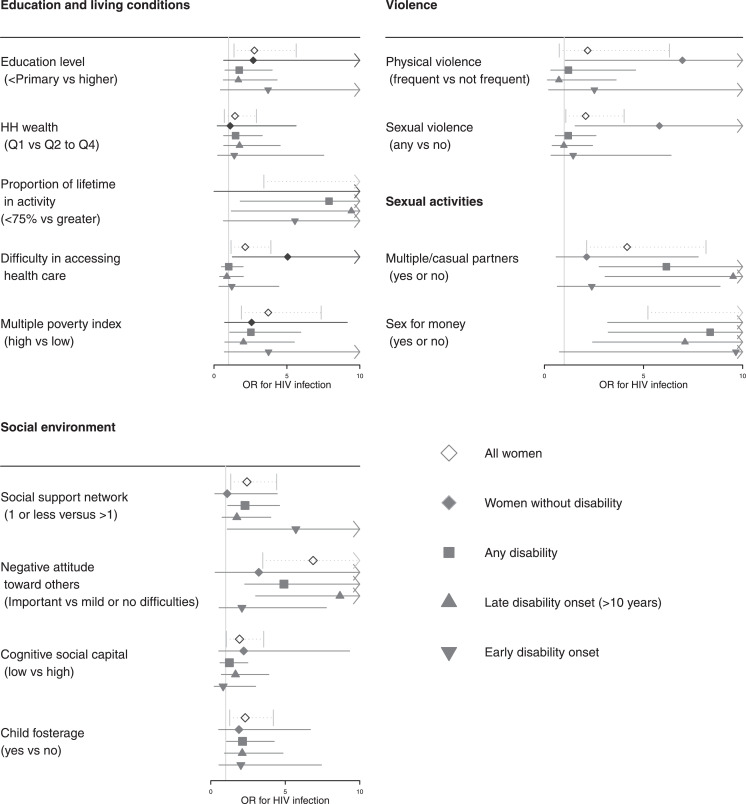
When the entire population of female participants was considered, the different risk factors assessed (economic, social environment, sexual activity at risk and violence) were all significantly associated with HIV infection (Fig. 2). Overall, ORs were similar among women without disability, those with early disability onset or those with late disability onset. There was a significant interaction on the additive scale between early disability and the social support network size regarding the risk of HIV infection (p = 0.05, Table 5), indicating that the vulnerability of women with early disability to HIV infection was higher among those who were socially isolated (HIV prevalence in this group: 19%, 95%CI 12–27%). In fact, the prevalence of multidimensional poverty and of sexual activities in exchange for money was high in this group (64%, 95%CI 55–73% and 13%, 95%CI 6–20%, respectively). There was no evidence of interaction for the other socioeconomic variables on the additive scale (Table 5), although interactions on the multiplicative scale were found for sexual violence (p = 0.04).
Fig. 2.
Age-adjusted association (OR) between HIV risk and (a) economic factors (upper left), (b) social environment characteristics (bottom left), (c) experience of violence and (d) risky sexual activity (upper right) overall and by subgroups (women without disability, women with disability, women with disability since age 10 years, women with disability onset after age 10 years, women with disability and restricted social participation). Note at the bottom of the figure : symbols and horizontal lines represent ORs and their confidence intervals of HIV infection for each variable (indicated on the left) and for each sub-group (as indicated by the legend).
Table 5.
Factors associated with HIV infection among women with and without disability.
| Women without disability | Women with disability | ORa (95%CI) within factors strata |
|||
|---|---|---|---|---|---|
| Onset ≤age 10 years | Onset >age 10 years | ||||
| ORa (95%CI) | ORa (95%CI) | ORa (95%CI) | ≤age 10 years | >age 10 years | |
| Education and living conditions | |||||
| Household wealth | |||||
| Quartile Q2–Q4 | Ref | 2.9 (1–7.8) | 4.2 (1.8–9.5) | 1.7# (0.1–25.1) | |
| Lower quartile Q1 | 1.0 (0.2–5.2) | 3.8 (0.7–20.6) | 7 (2.3 – 20.6) | 2.8 (1.0–7.6) | |
| RERI (95%CI) | 0.9 (−5.4 to 7.2) | 2.7 (−3.8 to 9.3) | |||
| Educational achievement | |||||
| Primary or greater | Ref | 1.9 (0.2–18.9) | 7.6 (1.9–30.8) | 3.3 (0.2–49.1) | 3.2 (1.3–7.7) |
| <Primary level | 3 (0.8–12) | 6.9 (1.8–26.6) | 10.9 (3.1–38.4) | 1.9 (0.7–5.5) | 7.7 (1.9–32.1) |
| RERI (95%CI) | 3.1 (−3•8 to 10•0) | 0.7 (−7.8 to 9.3) | |||
| % of lifetime working/studying | |||||
| >75% | Ref | 3.52 (0.84–14.80) | 4.71 (1.26–17.55) | ||
| ≤75% | 3.18 (0.88–11.54) | 5.03 (1.41–17.96) | 10.64 (3.42–33.12) | ||
| RERI (95%CI) | −0.7 (−6.8 to 5.4) | 3.8 (−4 to 11.5) | |||
| Access to health care | |||||
| Important difficulties | Ref | 3.7 (0.97– 10.65) | 7.01 (2.69–18.32) | ||
| No or mild difficulty | 5.82 (1.52–22.33) | 4.09 (1.30–12.87) | 6.20 (2.36–16.30) | ||
| RERI (95%CI) | −3.9 (−12.7 to 4.8) | −5.6 (−15.5 to 4.2) | |||
| Multidimensional poverty index | |||||
| Above threshold | Ref | 1.65 (0.31–8.89) | 5.09 (1.47–17.65) | ||
| Below threshold | 3.58 (1.03–12.47) | 6.02 (1.93–18.81) | 9.12 (3.26–25.49) | ||
| RERI (95%CI) | 1.8 (−4 to 7.6) | 1.5 (−5.5 to 8.4) | |||
| Social resources and environment | |||||
| Social support network | |||||
| >1 persons | Ref | 0.91 (0.19–4.49) | 3.63 (1.43–.22) | ||
| ≤1 person | 1.19 (0.30–4.69) | 4.81 (1.73–13.34) | 6.92 (2.73–17.57) | ||
| RERI (95%CI) | 3.7 (−0.7 to 8.1) | 3.1 (−2 to 8.2) | |||
| Cognitive social capital | |||||
| Low score | 1 (ref) | 1.26 (0.28–5.76) | 3.28 (0.84–12.76) | ||
| High score | 0.45 (0.11–1.79) | 1.45 (0.33–6.29) | 1.99 (0.53–7.46) | ||
| RERI (95%CI) | 0.7 (−1 to 2.5) | −0.7 (−3.9 to 2.5) | |||
| Attitude of other people | |||||
| Important difficulties | Ref | 2.22 (0.76–6.46) | 2.42 (1.01–5.82) | ||
| Mild or no difficulty | 3.58 (0.34–38.29) | 4.91 (1.50–16.10) | 23.03 (8.54–62.15) | ||
| RERI (95%CI) | 0.1 (−9.6 to 9.9) | 18 (−4.4 to 40.5) | |||
ORa: odds ratio adjusted for age; 95%CI: 95% confidence interval; RERI: relative excess risk due to interaction.
3.4. Mediation analysis
Mediation analysis was performed for the subset of women with disability onset before 10 years compared to those without disability and showed evidence that the association between early disability and HIV infection could be mediated by low education level (proportion mediated: 28%, p = 0.05) and sexual violence (proportion mediated: 28%, p = 0.07). Taken together, low education and sexual violence mediated approximately half of the association between disability and HIV (OR of the natural indirect effect: 1.7, 95%CI 1·3–2.4; OR of the natural direct effect: 1.7, 95%CI 0.6–4.4). There was no evidence of a mediated effect for the other variables (Table 6).
Table 6.
Mediation analysis between early disability (onset ≤age 10 years) and HIV infection.
| % mediated (p-value) | Natural indirect effect (95%CI) | Natural direct effect (95%) | |
|---|---|---|---|
| Education | |||
| <Primary level vs greater | 30% (p = 0.05) | 1.4 (1–1.9) | 2. (0.8–5.5) |
| Social resources | |||
| Social support network <1 person vs ≥1 | 22% (p = 0.1) | 1.3 (1–1.7) | 2.4 (1.0–5.3) |
| Any sexual violence | 32% (p = 0.03) | 1.4 (1–2.1) | 2.1 (0.8 - 5.5) |
| Any multiple/casual partners | 2% (p = 0.8) | 1 (0.8–1.3) | 2.7 (1.2–6.2) |
| Sex in exchange for money | 0% (p = 0.3) | 0.9 (0.7–1.1) | 2.9 (1.3–6.8) |
Analyses were adjusted for a nonlinear effect of age and for childhood poverty using the following variables: father's and mother's education level, father's work and experience of food insecurity ≤10 years.
4. Discussion
This study adds to previous work showing a strong association between disability and HIV [3] and provides some insight into the complex relation between disability and HIV, which is crucial for planning future interventions. Using a large and representative sample of people with disability from Bujumbura and a control group of similar age, sex and residential location, we found a three-fold higher prevalence of HIV infection among women with disability than among women without, which translates into a ten-fold increase compared to men. These results are in line with those of a previous survey conducted in Cameroon, in which women with disability had nearly twice the risk of HIV infection compared to those without (OR 1.7) [3], and with those of a meta-analysis indicating a 1.25 relative risk of HIV infection among women with disability compared to those without [4]. By contrast, we found a non-significant slight increase in HIV prevalence among men with disability. This highlights the intersectionality of gender and disability regarding vulnerability to HIV infection in the urban context of Burundi. Although intersectional studies on disability have developed over the last decade, few have examined vulnerability to HIV [43,44]. Most often, intersectional studies adopt a qualitative approach, which seems to be more suitable to report on the multidimensionality of individual experiences. However, epidemiologic studies such as this one could provide some insight into the multiple levels of disadvantage and oppression that shape women with disability's vulnerability [45]. As it has been done with gender over the last decades, disability should be included as a category of analysis in epidemiologic work to better understand the diversity of human experience [46].
An important aspect of the association between HIV and disability is the bidirectional relationship that needs to be accounted for when interpreting the results. In this study, we differentiated between people who grew up with a disability and were therefore exposed to HIV infection after becoming disabled and those who acquired a disability later in their lives. Although HIV could be acquired at birth or during childhood, no participant reported such a situation. In contrast to participants with early disability, those with late disability constitute a more heterogeneous group, with some persons having functional limitations resulting from HIV infection. Therefore, the time ordering between disability and HIV infection may not be respected in the latter group, which was not included in the mediation analysis.
Differences and commonalities between these two groups need to be highlighted. Both groups were affected by a higher prevalence of multidimensional poverty, sexual violence and HIV infection. However, participants with late disability were older than those with early disability. In addition, negative sexual health outcomes and deprivation were more frequent among participants with late disability, while those with early disability were more likely to have lower education levels, spend less time working and report more difficulties in social participation. The relatively better standard of living of the participants with early disability compared to participants with late disability may have resulted from a selection of the population whereby children from better-off families were more likely to survive [47].
Our results show that among women with early disability, those with restricted support networks were highly vulnerable to HIV infection. Although we cannot rule out the possibility that part of this interaction could result from the negative impact of HIV on people's lives (so-called inverse causality), we believe that this result warrants attention, as it highlights possible methods of intervention. A first approach could focus on interventions that would develop support networks through disabled person organizations (DPOs). However, in this study, as in the study conducted in Cameroon, it was found that only a small proportion of the participants with disability were involved in such organizations. Intervening through DPOs will therefore require increasing the identification of people with disabilities and their participation in DPOs. An alternative (or complementary) approach would be to work with the whole community to increase its social capital, i.e., its social cohesion and the resources that could be available to its more vulnerable members. It has been shown that social capital has a protective influence against HIV infection [48]. In this study, we found an association between disability, HIV and structural social capital measured by the support network size but not by cognitive social capital. However, there were limitations in our evaluation of social capital: first, the questions used only partially covered the different components of social capital, and second, the assessment was made at the individual level and not at the community level. Therefore, more research in this area with the perspective of identifying interventions to decrease the vulnerability of people with disability to HIV is needed.
It is important to point out that disability is not directly modifiable. However, it is possible to intervene in its social and economic impacts, and our results show that at least one-third of the disparity in HIV infection associated with disability would be removed if we were able to improve education and reduce poverty from the levels observed among women with disability to the levels observed among those without. Another third of the disparity may also be removed if we were able to reduce the rate of sexual violence among women with disability. These results also help to identify interventions that could reduce vulnerability to HIV infection among women with disability. They show that a broad approach addressing structural factors is needed for this population rather than only interventions focusing on behavioral factors, as is common in many programmes [49].
A number of limitations of this study should be noted. First, the main limitation concerns our ability to draw strong conclusions regarding causality because of the study design. Retrospective longitudinal data were collected to overcome the limitations of the cross-sectional design, but these data may be prone to recall bias. Although attention was given in the analysis on potential confounding factors, there may be residual unmeasured confounding factors responsible for bias. For instance, childhood living conditions was imperfectly captured through parents education and work and through the reporting of food insecurity at age 10. However, the high E-values found in the analysis indicate that the effect of confounding need to be very strong to explain the observed OR, which does not seem likely. Another challenge encountered in this study was the evaluation of disability [50]. The pragmatic approach adopted in this study was to first focus on functional limitations using the WGSS questionnaire, which has been extensively evaluated and used [51]. However, it should be noted that this instrument does not measure cognitive and mental disability well, which prompted us to add questions to better capture this dimension. It is also important to remember that, given the specific urban coverage of this study, these results cannot be extrapolated to other settings such as rural areas. Including disability indicators such as the WGSS questions in national HIV surveys would be an efficient way to collect additional data from different contexts.
In summary, in Bujumbura, the HIV prevalence was higher among women with disability than among women without, higher in women than in men and similar between men with and without disability. Among women who grew up with disability, those with limited social networks were highly vulnerable to HIV infection. Future interventions to reduce HIV acquisition among women with disability may target education and sexual violence, as these two risk factors mediate a large part of the association between disability and HIV.
Funding
Netherlands Organization for Scientific Research (Grant W08.560.005) and the Initiative HIV-TB-Malaria (new name of the organisation). The funding sources was not involved in the writing of the manuscript nor in the decision to submit it for publication.
Data sharing
The dataset used for this analysis is available at Zenodo (http://doi.org/10.5281/zenodo.3885141 ).
Declaration of Competing Interest
The authors declare they have no conflicts of interest.
Acknowledgments
The corresponding author has full access to all the study data and had final responsibility for the decision to submit for publication.
Appendix A. Study tools
Washington Group questionnaire
To overcome the practical and conceptual difficulties in measuring disability, a group of experts set up by the UN Statistical Commission has proposed an operational tool for the identification of people with disabilities in surveys with good accuracy and reproducibility from one setting to another. This tool includes a small number of questions covering six functional domains or basic actions: seeing, hearing, walking, cognition, self-care, and communication. Each question asks the respondent to rate how much difficulty he/she has experienced in the domain on a four-point scale (see below). The Washington Group questionnaire is available in various forms; a short set questionnaire includes six questions and is recommended for use in national surveys because of its simplicity. Additional questions are available from the extended set to supplement those from the short set and provide more detail on functional limitations.
Short set of the Washington Group questionnaire:
Because of a physical, mental, or emotional health condition…
-
1
Do you have difficulty seeing even if wearing glasses?
-
2
Do you have difficulty hearing even if using hearing aid/s, or are you deaf?
-
3
Do you have difficulty walking or climbing stairs?
-
4
Do you have difficulty remembering or concentrating?
-
5
Do you have difficulty (with self-care such as) washing all over or dressing?
-
6
Do you have difficulty communicating (for example, understanding or being understood by others)? Two additional questions from the extended set of the Washington Group questionnaire were added to better capture individuals with intellectual disabilities:
-
7
Do you have difficulty learning a new task, for example, learning how to get to a new place?
-
8
Do you have difficulty analysing and finding solutions to problems in day-to-day life?
Question response categories: No, Some, A lot, and Unable.
Life-grid method
The life grid comprised two A3 sheets divided into several columns. The vertical axis is divided into the time units for which the events are to be recorded; the first column shows the time (in years) from birth to the current year, the second column shows the age from 0 to the current age, and the third column shows the time elapsed. The other columns related to the different areas explored during the life-history interview are as follows: family environment, main occupations/activities, resources, quality of life, sexual relationships, periods of transactional sex or sexual violence, pregnancies, children and disability onset.
Appendix B. Statistical analysis
Additive interaction
Three measures of additive interaction between two risk factors can be derived from the results of logistic regression [52]. Let OR11 denotes the odds ratio of exposure to both factors compared to none and OR01 or OR10 the odds ratio of exposure to only one factor compared to none. The relative excess risk due to interaction (RERI) is defined as
| RERI = OR11 - OR01 - OR10 + 1 |
It measures the extent to which the OR under joint exposure exceeds the risk that is expected on the basis of the addition of the ORs under each exposure.
The attributable proportion due to interaction (AP) is defined as AP = RERI/OR11 and is interpreted as the proportion of risk in the group with joint exposure that is due to interaction.
The synergy index (S) is defined as S = [OR11–1]/[(OR10–1)+(OR01–1)] and can be interpreted as the excess risk from exposure to both exposures when there is interaction relative to the risk from exposure without interaction.
Mediation analysis
The potential outcome approach is based on the counterfactual framework. Let D denotes the exposure of interest (disability), Y the outcome, and M a potential mediator (e.g., education level). In addition, C denotes the baseline covariates (e.g. age or sex).
The counterfactual outcome Yd (counterfactual mediator Md) is defined as the value of the outcome (mediator) that would have been observed had exposure D been set to level d. The total (counterfactual) effect (TE) of D on outcome Y is defined as Y1 − Y0, and the total effect of D on mediator M is defined as M1 − M0. As one of the counterfactual outcomes is unobservable (“counter to the fact”), the counterfactual effect cannot be measured at the individual level. However, it can be estimated at the population level.
In addition, the natural direct effect of D on Y is defined as Y1M0 – Y0M0 and compares the counterfactual outcome under D = 1 with D = 0 assuming M is set to what it would have been if exposure had been D = 0. The natural indirect effect, defined as Y1M1 – Y1M0, assumes that D is set to the level D = 1 and compares the outcome for the mediator M set to what it would have been with D = 1 with the outcome for M set to what it would have been with D = 0.
The primary analysis was conducted using the Medflex package for R [53]. An alternative approach to mediation based on weighted regression was also used to assess the robustness of our results [54]. The later approach consists first in modeling the relation between mediator(s) and exposure (disability) then computing weights from the odds ratios estimated during the first step that will be used to assess the marginal association between the exposure and the outcome. A detailed description of the procedure is given in Nguyen et al. 2015 [55].
Appendix C. STROBE checklist
STROBE Statement—Checklist of items that should be included in reports of cross-sectional studies
| Item No | Recommendation | Page No | |
|---|---|---|---|
| Title and abstract | 1 | (a) Indicate the study's design with a commonly used term in the title or the abstract | 2 |
| (b) Provide in the abstract an informative and balanced summary of what was done and what was found | 2 | ||
| Introduction | |||
| Background/rationale | 2 | Explain the scientific background and rationale for the investigation being reported | 2 |
| Objectives | 3 | State specific objectives, including any prespecified hypotheses | 2 |
| Methods | |||
| Study design | 4 | Present key elements of study design early in the paper | 6 |
| Setting | 5 | Describe the setting, locations, and relevant dates, including periods of recruitment, exposure, follow-up, and data collection | 6 |
| Participants | 6 | (a) Give the eligibility criteria, and the sources and methods of selection of participants | 6 |
| Variables | 7 | Clearly define all outcomes, exposures, predictors, potential confounders, and effect modifiers. Give diagnostic criteria, if applicable | 8 - 9 Table 2 |
| Data sources/ measurement | 8* | For each variable of interest, give sources of data and details of methods of assessment (measurement). Describe comparability of assessment methods if there is more than one group | 7 Table 1 |
| Bias | 9 | Describe any efforts to address potential sources of bias | 8–9 |
| Study size | 10 | Explain how the study size was arrived at | 6 |
| Quantitative variables | 11 | Explain how quantitative variables were handled in the analyses. If applicable, describe which groupings were chosen and why | 8 |
| Statistical methods | 12 | (a) Describe all statistical methods, including those used to control for confounding | 8–9 |
| (b) Describe any methods used to examine subgroups and interactions | 8–9 | ||
| (c) Explain how missing data were addressed | 10 | ||
| (d) If applicable, describe analytical methods taking account of sampling strategy | 10 | ||
| (e) Describe any sensitivity analyses | 8 | ||
| Results | |||
| Participants | 13* | (a) Report numbers of individuals at each stage of study—eg numbers potentially eligible, examined for eligibility, confirmed eligible, included in the study, completing follow-up, and analysed | 10 Fig. 1 |
| (b) Give reasons for non-participation at each stage | NA | ||
| (c) Consider use of a flow diagram | Fig. 1 | ||
| Descriptive data | 14* | (a) Give characteristics of study participants (eg demographic, clinical, social) and information on exposures and potential confounders | Table 3 |
| (b) Indicate number of participants with missing data for each variable of interest | Table 3 | ||
| Outcome data | 15* | Report numbers of outcome events or summary measures | Table 4 |
| Main results | 16 | (a) Give unadjusted estimates and, if applicable, confounder-adjusted estimates and their precision (eg, 95% confidence interval). Make clear which confounders were adjusted for and why they were included | Table 4 p11 |
| (b) Report category boundaries when continuous variables were categorized | - | ||
| (c) If relevant, consider translating estimates of relative risk into absolute risk for a meaningful time period | - | ||
| Other analyses | 17 | Report other analyses done—eg analyses of subgroups and interactions, and sensitivity analyses | 12 Table 4 |
| Discussion | |||
| Key results | 18 | Summarize key results with reference to study objectives | 13 |
| Limitations | 19 | Discuss limitations of the study, taking into account sources of potential bias or imprecision. Discuss both direction and magnitude of any potential bias | 15–16 |
| Interpretation | 20 | Give a cautious overall interpretation of results considering objectives, limitations, multiplicity of analyses, results from similar studies, and other relevant evidence | 14–17 |
| Generalisability | 21 | Discuss the generalisability (external validity) of the study results | 16 |
| Other information | |||
| Funding | 22 | Give the source of funding and the role of the funders for the present study and, if applicable, for the original study on which the present article is based | 10 and 17 |
References
- 1.UNAIDS. Disability and HIV. 2017. http://www.unaids.org/en/resources/documents/2017/jc2905_disability-and-hiv.
- 2.Hanass-Hancock J. Disability and HIV/AIDS - a systematic review of literature on Africa. J Int AIDS Soc. 2009;2(1):9. doi: 10.1186/1758-2652-12-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.De Beaudrap P., Beninguisse G., Pasquier E. Prevalence of HIV infection among people with disabilities: a population-based observational study in Yaounde, Cameroon (HandiVIH) Lancet HIV. 2017;4(4):e161–e168. doi: 10.1016/S2352-3018(16)30209-0. [DOI] [PubMed] [Google Scholar]
- 4.De Beaudrap P., Mac-Seing M., Pasquier E. Disability and HIV: a systematic review and a meta-analysis of the risk of HIV infection among adults with disabilities in Sub-Saharan Africa. AIDS Care. 2014;26(12):1467–1476. doi: 10.1080/09540121.2014.936820. [DOI] [PubMed] [Google Scholar]
- 5.Groce N.E., Rohleder P., Eide A.H., MacLachlan M., Mall S., Swartz L. HIV issues and people with disabilities: a review and agenda for research. Soc Sci Med. 2013;77:31–40. doi: 10.1016/j.socscimed.2012.10.024. [DOI] [PubMed] [Google Scholar]
- 6.Rusch M., Nixon S., Schilder A., Braitstein P., Chan K., Hogg R.S. Prevalence of activity limitation among persons living with HIV/AIDS in British Columbia. Can J Public Health. 2004;95(6):437–440. doi: 10.1007/BF03403989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Banks L.M., Zuurmond M., Ferrand R., Kuper H. The relationship between HIV and prevalence of disabilities in sub-Saharan Africa: systematic review (FA) Trop. Med. Int. Health. 2015;20(4):411–429. doi: 10.1111/tmi.12449. [DOI] [PubMed] [Google Scholar]
- 8.Rajasuriar R., Chong M.L., Ahmad Bashah N.S. Major health impact of accelerated aging in young HIV-infected individuals on antiretroviral therapy. AIDS. 2017;31(10):1393–1403. doi: 10.1097/QAD.0000000000001475. [DOI] [PubMed] [Google Scholar]
- 9.Myezwaa H., Hanass-Hancock J., Ajidahuna A.T., Carpenter B. Disability and health outcomes – from a cohort of people on long-term antiretroviral therapy. J Soc Aspects HIV/AIDS. 2018;15(1):50–59. doi: 10.1080/17290376.2018.1459813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Greene M., Covinsky K., Astemborski J. The relationship of physical performance with HIV disease and mortality. AIDS. 2014;28(18):2711–2719. doi: 10.1097/QAD.0000000000000507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Laverick R., Haddow L., Daskalopoulou M. Self-reported decline in everyday function, cognitive symptoms, and cognitive function in people with HIV. J Acquir Immune Defic Syndr. 2017;76(3):e74–e83. doi: 10.1097/QAI.0000000000001468. [DOI] [PubMed] [Google Scholar]
- 12.Van As M., Myezwa H., Stewart A., Maleka D., Musenge E. The international classification of function disability and health (ICF) in adults visiting the HIV outpatient clinic at a regional hospital in Johannesburg, South Africa. AIDS Care. 2009;21(1):50–58. doi: 10.1080/09540120802068829. [DOI] [PubMed] [Google Scholar]
- 13.Kietrys D., Myezwa H., Galantino M.L. Functional limitations and disability in persons living with HIV in South Africa and United States: similarities and differences. J Int Assoc Provid AIDS Care. 2019;18:1–19. doi: 10.1177/2325958219850558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hanass-Hancock J., Myezwa H., Carpenter B. Disability and living with HIV: baseline from a cohort of people on long term ART in South Africa. PLoS One. 2015;10(12) doi: 10.1371/journal.pone.0143936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Parker R.G., Easton D., Klein C.H. Structural barriers and facilitators in HIV prevention: a review of international research. AIDS. 2000;14(Suppl 1):S22–S32. doi: 10.1097/00002030-200006001-00004. [DOI] [PubMed] [Google Scholar]
- 16.Rhodes T., Singer M., Bourgois P., Friedman S.R., Strathdee S.A. The social structural production of HIV risk among injecting drug users. Soc Sci Med. 2005;61(5):1026–1044. doi: 10.1016/j.socscimed.2004.12.024. [DOI] [PubMed] [Google Scholar]
- 17.Singer M.C., Erickson P.I., Badiane L. Syndemics, sex and the city: understanding sexually transmitted diseases in social and cultural context. Soc Sci Med. 2006;63(8):2010–2021. doi: 10.1016/j.socscimed.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hogben M., Leichliter J.S. Social determinants and sexually transmitted disease disparities. Sex Transm Dis. 2008;35(12 Suppl):S13–S18. doi: 10.1097/OLQ.0b013e31818d3cad. [DOI] [PubMed] [Google Scholar]
- 19.Strathdee S.A., Hallett T.B., Bobrova N. HIV and risk environment for injecting drug users: the past, present, and future. Lancet. 2010;376(9737):268–284. doi: 10.1016/S0140-6736(10)60743-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mitra S. Palgrave Macmillan US; 2017. Disability, health and human development. [Google Scholar]
- 21.Parkhurst J.O. Understanding the correlations between wealth, poverty and human immunodeficiency virus infection in African countries. Bull. World Health Organ. 2010;88(7):519–526. doi: 10.2471/BLT.09.070185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Magadi M.A. Understanding the urban–rural disparity in HIV and poverty nexus: the case of Kenya. J Public Health. 2016;39(3):e63–e72. doi: 10.1093/pubmed/fdw065. [DOI] [PubMed] [Google Scholar]
- 23.Blair J.M., Paxton L.A., Kamb M.L. Chapter 33 – HIV and AIDS in women. In: Goldman MB, Troisi R, Rexrode KM, editors. Women and health. 2nd Ed. Academic Press; 2013. pp. 505–522. [Google Scholar]
- 24.Helleringer S., Kohler H.P. Social networks, perceptions of risk, and changing attitudes towards HIV/AIDS: new evidence from a longitudinal study using fixed-effects analysis. Popul Stud. 2005;59(3):265–282. doi: 10.1080/00324720500212230. [DOI] [PubMed] [Google Scholar]
- 25.Helleringer S., Kohler H.P. Sexual network structure and the spread of HIV in Africa: evidence from Likoma Island, Malawi. Aids. 2007;21(17):2323–2332. doi: 10.1097/QAD.0b013e328285df98. [DOI] [PubMed] [Google Scholar]
- 26.Harcourt C., Donovan B. The many faces of sex work. Sex Transm Infect. 2005;81:201–206. doi: 10.1136/sti.2004.012468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hughes K., Bellis M.A., Jones L. Prevalence and risk of violence against adults with disabilities: a systematic review and meta-analysis of observational studies. Lancet. 2012;379(9826):1621–1629. doi: 10.1016/S0140-6736(11)61851-5. [DOI] [PubMed] [Google Scholar]
- 28.WHO, The World Bank. World report on disability. 2011. http://www.who.int/disabilities/world_report/2011/en/index.html(accessed June 2020).
- 29.Blane D. Collecting retrospective data: development of a reliable method and a pilot study of its use. Soc Sci Med. 1996;42(5):751–757. doi: 10.1016/0277-9536(95)00340-1. [DOI] [PubMed] [Google Scholar]
- 30.Freedman D., Thornton A., Camburn D., Alwin D., Young-demarco L. The life history calendar: a technique for collecting retrospective data. Sociol Methodol. 1988;18:37–68. [PubMed] [Google Scholar]
- 31.van Brakel W.H., Anderson A.M., Mutatkar R.K. The Participation Scale: measuring a key concept in public health. Disabil Rehabil. 2006;28(4):193–203. doi: 10.1080/09638280500192785. [DOI] [PubMed] [Google Scholar]
- 32.Bourdieu P.J. The forms of capital. In: Richardson J, editor. Handbook of theory and research for the sociology of education. Greenwood; New York: 1986. pp. 241–258. [Google Scholar]
- 33.Harpham T., Grant E., Thomas E. Measuring social capital within health surveys: key issues. Health Policy Plan. 2002;17(1):106–111. doi: 10.1093/heapol/17.1.106. [DOI] [PubMed] [Google Scholar]
- 34.Krishna A., Shrader E. Social capital assessment tool. 1999.
- 35.De Silva M.J., Harpham T., Tuan T., Bartolini R., Penny M.E., Huttly S.R. Psychometric and cognitive validation of a social capital measurement tool in Peru and Vietnam. Soc Sci Med. 2006;62(4):941–953. doi: 10.1016/j.socscimed.2005.06.050. [DOI] [PubMed] [Google Scholar]
- 36.VanderWeele T.J., Ding P. Sensitivity analysis in observational research: introducing the e-value. Ann Intern Med. 2017;167(4):268–274. doi: 10.7326/M16-2607. [DOI] [PubMed] [Google Scholar]
- 37.Alkire S., Foster J. Counting and multidimensional poverty measurement. J Public Econ. 2011;95(7–8):476–487. [Google Scholar]
- 38.Knol M.J., VanderWeele T.J. Recommendations for presenting analyses of effect modification and interaction. Int J Epidemiol. 2012;41(2):514–520. doi: 10.1093/ije/dyr218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.VanderWeele T.J., Robinson W.R. On the causal interpretation of race in regressions adjusting for confounding and mediating variables. Epidemiology. 2014;25(4):473–484. doi: 10.1097/EDE.0000000000000105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vansteelandt S., Vanderweele T.J. Natural direct and indirect effects on the exposed: effect decomposition under weaker assumptions. Biometrics. 2012;68(4):1019–1027. doi: 10.1111/j.1541-0420.2012.01777.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.R Core Team . 3.6.0 ed. R Foundation for Statistical Computing; Vienna, Austria: 2019. R: a language and environment for statistical computing. [Google Scholar]
- 42.von Elm E., Altman D.G., Egger M. The strengthening the reporting of observational studies in epidemiology (strobe) statement: guidelines for reporting observational studies. PLoS Med. 2007;4(10):e296. doi: 10.1371/journal.pmed.0040296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yoshida K., Hanass-Hancock J., Nixon S., Bond V. Using intersectionality to explore experiences of disability and HIV among women and men in Zambia. Disabil Rehabil. 2014;36(25):2161–2168. doi: 10.3109/09638288.2014.894144. [DOI] [PubMed] [Google Scholar]
- 44.Chappell P. Dangerous girls and cheating boys: zulu-speaking disabled young peoples' constructs of heterosexual relationships in Kwazulu-Natal, South Africa. Cult Health Sex. 2017;19(5):587–600. doi: 10.1080/13691058.2016.1256433. [DOI] [PubMed] [Google Scholar]
- 45.Bauer G.R. Incorporating intersectionality theory into population health research methodology: challenges and the potential to advance health equity. Soc Sci Med. 2014;110:10–17. doi: 10.1016/j.socscimed.2014.03.022. [DOI] [PubMed] [Google Scholar]
- 46.Garland-Thomson R. Integrating disability, transforming feminist theory. NWSA J. 2002;14(3):1–32. [Google Scholar]
- 47.Abuga J.A., Kariuki S.M., Kinyanjui S.M., Boele Van Hensbroek M., Newton C.R. Premature mortality in children aged 6-9 years with neurological impairments in rural Kenya: a cohort study. Lancet Glob Health. 2019;7(12):e1728–e1e35. doi: 10.1016/S2214-109X(19)30425-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gregson S., Mushati P., Grusin H. Social capital and women's reduced vulnerability to HIV infection in rural Zimbabwe. Popul Dev Rev. 2011;37(2):333–359. doi: 10.1111/j.1728-4457.2011.00413.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gupta G.R., Parkhurst J.O., Ogden J.A., Aggleton P., Mahal A. Structural approaches to HIV prevention. Lancet. 2008;372(9640):764–775. doi: 10.1016/S0140-6736(08)60887-9. [DOI] [PubMed] [Google Scholar]
- 50.Mont D. The World Bank; 2007. Measuring disability prevalence. [Google Scholar]
- 51.Altman B.M. Springer International Publishing; 2016. International measurement of disability: purpose, method and application. [Google Scholar]
- 52.VanderWeele T.J., Knol M.J. A tutorial on interaction. Epidemiol Methods. 2014;3(1):33–72. [Google Scholar]
- 53.Steen J., Loeys T., Moerkerke B., Vansteelandt S. Medflex: an R package for flexible mediation analysis using natural effect models. 20172017;76(11): 46.
- 54.Tchetgen E.J.T. Inverse odds ratio-weighted estimation for causal mediation analysis. Stat Med. 2013;32(26):4567–4580. doi: 10.1002/sim.5864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nguyen Q.C., Osypuk T.L., Schmidt N.M., Glymour M.M., Tchetgen E.J.T. Practical guidance for conducting mediation analysis with multiple mediators using inverse odds ratio weighting. Am J Epidemiol. 2015;181(5):349–356. doi: 10.1093/aje/kwu278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hu Lt, Bentler P.M. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Eq Model: Multidiscip J. 1999;6(1):1–55. [Google Scholar]
- 57.Whiteneck G.G., Harrison-Felix C.L., Mellick D.C., Brooks C.A., Charlifue S.B., Gerhart K.A. Quantifying environmental factors: a measure of physical, attitudinal, service, productivity, and policy barriers. Arch Phys Med Rehabil. 2004;85(8):1324–1335. doi: 10.1016/j.apmr.2003.09.027. [DOI] [PubMed] [Google Scholar]
- 58.Harrison-Felix C. The Center for Outcome Measurement in Brain Injury; 2001. The Craig hospital inventory of environmental factors.http://tbims.org/combi/chief/ [Google Scholar]
- 59.Cleland J., Ingham R., Stone N. Illustrative Core Instruments; 2001. Asking young people about sexual and reproductive behaviours. [Google Scholar]
- 60.McFarlane J., Hughes R.B., Nosek M.A., Groff J.Y., Swedlend N., Dolan Mullen P. Abuse assessment screen-disability (AAS-D): measuring frequency, type, and perpetrator of abuse toward women with physical disabilities. J Womens Health Gend Based Med. 2001;10(9):861–866. doi: 10.1089/152460901753285750. [DOI] [PubMed] [Google Scholar]
- 61.Stoebenau K., Wamoyi J., Ranganathan M., Kyegombe N. Questions on transactional sex in the dhs. 2018. http://strive.lshtm.ac.uk/impact/questions-transactional-sex-dhs. [DOI] [PMC free article] [PubMed]
- 62.Cohen S., Doyle W.J., Skoner D.P., Rabin B.S., Gwaltney J.M., Jr. Social ties and susceptibility to the common cold. JAMA. 1997;277(24):1940–1944. [PubMed] [Google Scholar]
- 63.Filmer D., Pritchett L.H. Estimating wealth effects without expenditure data–or tears: an application to educational enrollments in states of India. Demography. 2001;38(1):115–132. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]