Abstract
Background
Patients with ischaemic stroke or transient ischaemic attack (TIA) are at high risk of recurrent stroke and other cardiovascular diseases and commonly suffer from reduced quality of life. We aimed to determine whether the disease management programme STROKE-CARD can prevent cardiovascular diseases and improve quality of life in these patients.
Methods
In this pragmatic open-label two-centre randomised controlled trial with blinded outcome assessment, we randomly assigned patients with acute ischaemic stroke or TIA (ABCD2 score ≥3) in a 2:1 ratio to receive STROKE-CARD care or standard care. STROKE-CARD care is a disease management programme by a multidisciplinary stroke team that comprises a standardised 3-month visit and access to a web-based patient portal targeting risk factor management, post-stroke complications, comorbidities and cardiovascular warning signs, rehabilitation demands, and patient education, counselling, and self-empowerment. Co-primary outcomes were analysed on an intention-to-treat basis and were: (i) major cardiovascular disease events defined as nonfatal ischaemic or haemorrhagic stroke, nonfatal myocardial infarction, or vascular death occurring between hospital discharge and 12 months; and (ii) health-related quality of life at 12 months quantified with the EuroQol-5-Dimensions-3-Levels (EQ-5D-3L) overall utility score. This trial is registered with ClinicalTrials.gov, number NCT02156778.
Findings
Of 2149 patients enrolled between January 2014 and December 2017 (mean age 69 years, 41% female, 83% with ischaemic stroke, 17% with TIA), 1438 were assigned to STROKE-CARD care and 711 to standard care. Major cardiovascular disease events occurred in 78 patients in the STROKE-CARD care group (5.4%) and in 59 patients in the standard care group (8.3%) (hazard ratio, 0.63; 95% confidence interval: 0.45-0.88; P=0.007). STROKE-CARD care also led to a better EQ-5D-3L overall utility score at 12 months (P<0.001). Among pre-specified secondary outcomes, STROKE-CARD care improved all individual EQ-5D-3L dimensions and functional outcome on the modified Rankin Scale at 12 months. Post hoc explanatory analyses identified considerable demands for additional rehabilitation and refinement of preventive therapy regimes at the 3-month visit and high proportions of post-stroke complications and warning signs of imminent cardiovascular diseases within the first three months.
Interpretation
The pragmatic and easily implementable STROKE-CARD care programme reduced cardiovascular risk and improved health-related quality of life and functional outcome in patients with acute ischaemic stroke or TIA.
Funding
Tirol Kliniken, Tyrolean Health Insurance Company, Tyrol Health Care Funds, Boehringer Ingelheim, Nstim Services, Sanofi, Bayer Healthcare.
Keywords: Randomised controlled trial, Ischaemic stroke, Transient ischaemic attack, Disease management programme, Secondary prevention, Quality of life
Research in context.
Evidence before the study
We searched PubMed for relevant clinical trials published up to June 28, 2020, with the terms “disease management” and “stroke” OR “transient isch(a)emic attack”. We additionally scanned reference lists of relevant articles and reviews. On top of several trials, we identified a 2018 Cochrane review on interventions for improving modifiable risk factor control in the secondary prevention of stroke, which included 42 completed trials (involving 33,840 patients) and 24 ongoing trials. This review highlights that the effects of disease management programmes after stroke or transient ischaemic attack on cardiovascular risk, quality of life, and functional independence is still uncertain.
Added value of this study
STROKE-CARD care is the first disease management programme that significantly reduced cardiovascular risk and improved health-related quality of life in patients with ischaemic stroke or transient ischaemic attack, as shown by our large-scale pragmatic open-label randomised controlled trial with blinded outcome assessment. Our study suggests an important role for the multidisciplinary stroke team in post-acute stroke management and included patients with a broad spectrum of disease severities ranging from moderate-risk transient ischaemic attack to major ischaemic stroke.
Implications of all the available evidence
Patients with stroke or transient ischaemic attack may benefit from well-designed disease management programmes. The pragmatic and easily implementable STROKE-CARD care programme reduced cardiovascular risk and improved health-related quality of life and functional outcome in patients with acute ischaemic stroke or TIA. Our findings emphasise that optimal stroke care does not end with hospital discharge but should extend to a comprehensive 3-month reassessment performed by a multidisciplinary stroke team.
Alt-text: Unlabelled box
1. Introduction
Stroke is the second leading cause of death worldwide and one of the main contributors to disability. According to the latest Global Burden of Disease Study, there are 80.1 million individuals that have had a stroke and stroke is responsible for 6.2 million deaths each year worldwide [1,2]. Patients with ischaemic stroke and those with transient ischaemic attack (TIA) are at elevated risk of subsequent stroke, particularly in the first year after the event (one-year cumulative risk 5.1%-13.1%) [3,4]. Importantly, recurrent strokes are associated with higher social and economic impact, higher case fatality, and worse clinical outcome than first-ever strokes [5]. Risk for other atherosclerotic cardiovascular diseases (CVD) is also increased after stroke or TIA [6]. It has been estimated that guideline-compliant treatment may prevent about 80% of recurrent CVD events [7], but – in reality – recommended target levels for modifiable risk factors are rarely achieved [8]. Moreover, post-stroke complications frequently manifest after hospital discharge and may remain undetected. The burden of post-stroke complications, residual deficits, and inadequate medical and psycho-social care contribute to long-term disability and reduced quality of life in these patients.
For these reasons, comprehensive disease management programmes performed by a multidisciplinary stroke team are required that focus on patient care after hospital discharge. Prior trials showed beneficial effects on blood pressure control but did not yield convincing evidence for improvements of other modifiable risk factors nor reductions in recurrent CVD events [9]. Furthermore, effects on quality of life and long-term functional independence are particularly under-investigated [9].
We herein report the results of a large randomised controlled trial employing the multifaceted disease management programme STROKE-CARD care to patients with ischaemic stroke or TIA. Our trial had two co-primary endpoints. It aimed to (i) reduce one-year risk of major cardiovascular events and (ii) improve health-related quality of life one year after the index event.
2. Methods
2.1. Trial design
We conducted this pragmatic block-randomised controlled open-label trial with blinded outcome assessment at Innsbruck University Hospital and Hospital St. John's of God Vienna. Its design has been described previously [10]. The study was approved by the ethics committees of the two study centres and is registered with ClinicalTrials.gov, number NCT02156778. Enrolled patients provided written informed consent.
2.2. Patients
Patients aged ≥18 years hospitalised due to acute ischaemic stroke (defined according to American Heart Association criteria [11]) or TIA (ABCD2 score 3 or higher [12]) were eligible for inclusion. Eligible patients were enrolled in the trial during the acute hospital stay. Exclusion criteria were malignancies or other severe diseases with an estimated life expectancy <1 year, drug addiction, severe alcohol abuse, residence outside the catchment area, or severe disability with low probability of successful rehabilitation indicated by a modified Rankin Scale (mRS) score of 5 at hospital discharge.
2.3. Interventions
Patients were allocated to STROKE-CARD or standard care in a 2:1 ratio by block-randomisation using prescheduled alternating blocks of 8 and 4 weeks. Allocation was based on the exact date and time of the qualifying event [10]. Standard care involved in-hospital patient counselling and education, dietary advice, smoking cessation support, printed information materials (book: “After a stroke”), and a detailed discharge-from-hospital report (including patient-tailored target levels for risk factor management) to the general practitioner and the patient. Patients with persisting deficits were transferred to rehabilitation services within the scope of the local stroke pathways [13]. Selected high-risk patients (e.g. patients after carotid surgery) were seen in the outpatient clinics. As part of the Austrian Stroke Unit Registry (outside the current study), study nurses conducted routine telephone interviews to assess the patients’ 3-month functional outcome [14].
In addition to standard care, STROKE-CARD care involved an outpatient appointment for patients and care-givers scheduled three months after the index event and lasting two to three hours [10]. This additional appointment was performed by a multidisciplinary team of stroke physicians, nurses, physiotherapists, and occupational and speech therapists. It had the following aims: (i) to re-evaluate stroke/TIA aetiology (with potential changes in prevention strategies), (ii) to reassess risk factor levels and optimise secondary prevention (adapting medication lists and reinforcing drug adherence), (iii) to systematically screen for post-stroke complications and other health problems (holistic approach with initiation of therapy and/or referral to specialists), (iv) to assess rehabilitation demands (with referral to rehabilitation services), (v) to manage new-onset CVD and warning signs of imminent CVD (including referral to revascularisation procedures if appropriate), and (vi) to enhance patient self-empowerment and knowledge about CVD and to counsel patients on all matters raised by themselves or their care-givers (Supplementary Methods). The median time from index event to the 3-month outpatient appointment in the STROKE-CARD care group was 99 days (interquartile range [IQR] 93-107) (in-person attendance rate 83.3%). Patients and care-givers were also given access to the web-based patient portal “MyStrokecard” for risk factor monitoring, ascertainment of post-stroke complications, and extended patient education and were offered to contact the study personnel in case of health problems. They received training for this e-tool during hospital stay with a tailored composition according to individual risk profiles and target levels and introduction to easily applicable screening tools for post-stroke complications.
2.4. Outcomes
All trial endpoints were pre-specified. The composite CVD endpoint was adjudicated by a committee blinded to group assignment using standard diagnostic criteria [11,15]. Details on outcome definitions and adjudication procedures are provided in the Supplementary Methods. Co-primary outcomes were (i) a composite outcome of major cardiovascular events defined as nonfatal ischaemic stroke, nonfatal haemorrhagic stroke, nonfatal myocardial infarction, or vascular death (i.e. sudden cardiac death or death due to acute myocardial infarction, ischaemic or haemorrhagic stroke, heart failure, cardiovascular procedures, pulmonary embolism, or peripheral artery disease) between hospital discharge and the 12-month visit; and (ii) health-related quality of life at the 12-month visit, self-reported by the patient with a questionnaire and quantified with the EuroQol-5-Dimensions-3-Levels (EQ-5D-3L) overall health utility score [16] with rescaled European visual analogue scale weights [17]. Definitions of pre-specified secondary outcomes and potential side effects of intensified secondary prevention are provided in the Supplementary Methods.
2.5. Statistical analysis
Analyses were conducted according to a pre-specified statistical analysis plan (Supplementary File 3). We initially planned to enrol 2400 patients to detect a reduction in 12-month CVD risk from 15% with standard care to 10% with STROKE-CARD care with 90% power (α=0.05). When observing a lower-than-expected attrition rate (including withdrawals of consent and losses to follow-up) between January 2014 and June 2017, the target sample size was revised to 2160 patients. For the EQ-5D-3L overall health utility score, we estimated that this sample size allowed detecting a difference of 0.03 with 90% power, assuming a standard deviation (SD) of 0.2. No interim analyses were performed.
The principal analysis was conducted as a complete case analysis and on an intention to treat basis. We considered the trial successful only if the analyses of both co-primary endpoints yielded two-sided P values ≤ 0.05 [18]. For the descriptive analysis and analysis of secondary outcomes and subgroups, we used the Hochberg procedure to correct for multiple testing [18]. We analysed time-to-event data from hospital discharge to occurrence of the event of interest, death, or end of follow-up, whichever had occurred first. For patients who had attended the 12-month visit late (i.e. >13 months after hospital discharge), time-to-event data were censored at 13 months. Cox regression models were stratified by trial centre to account for potential clustering and differences in the baseline hazard function. The proportional hazards assumption was checked using Schoenfeld residuals and was met (Supplementary Figure 1). As we did not anticipate overdispersion, we pre-specified to analyse dichotomous outcomes using Poisson regression with robust error variance and adjustment for trial centre [19]. Ordinal logistic regression was used to test whether the distribution of mRS categories differed between trial arms; the proportional odds assumption was tested with the Brant test and was met. Due to a markedly skewed distribution, the Mann Whitney U-test (rather than linear regression as initially proposed in the design paper [10]) was used to test for a difference between trial arms in the 12-month EQ-5D-3L overall health utility score. Finally, we performed pre-specified sensitivity analyses for the CVD outcome (i) adjusting for age, sex, and type of index event, (ii) analysing patients as treated, (iii) analysing only patients that were treated per protocol, and (iv) excluding patients whose index event had been a TIA with an ABCD2 score of 3. We also performed pre-specified subgroup analyses according to sex, age (<70 vs. ≥70 years), type of index event, trial centre, and use of e-tool “MyStrokecard”.
2.6. Role of the funding source
The funders had no role in study design, data collection, data analysis, or writing of the report. PW and SKi had full access to all data in the study and had final responsibility for the decision to submit for publication.
3. Results
3.1. Patients
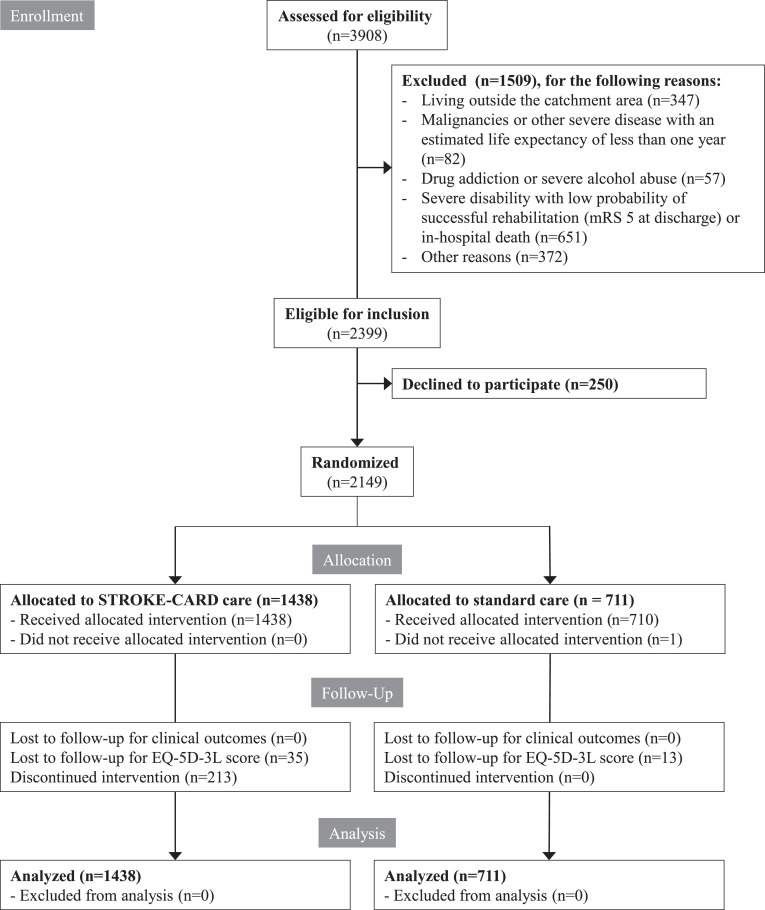
Trial enrolment began on 3 January 2014 and was completed on 31 December 2017; the last follow-up visit was on 15 January 2019. Of 3908 patients screened, 2399 were eligible for inclusion in the trial, of which 2149 patients participated (89.6%) (Figure 1). A total of 1438 patients were allocated STROKE-CARD care and 711 standard care. Follow-up for the composite CVD endpoint was complete. At the 12-month visit, the EQ-5D-3L overall health utility score was available for 2101 patients (97.8%) and the mRS score was available for 2117 patients (98.5%).
Fig. 1.
CONSORT diagram.
mRS denotes modified Rankin Scale. For the per-protocol and as treated analysis, patients were classified as having received STROKE-CARD care if they had attended the 3-month visits in person and/or had used the web-based patient portal during follow-up.
Mean age was 69 years (SD 14); 41% were women. As index event, 1791 patients (83%) had suffered an acute ischaemic stroke and 358 a TIA (17%). Patients with ischaemic stroke had a median National Institutes of Health stroke scale (NIHSS) score of 3 at hospital admission (IQR 1-6) and 14% had suffered a stroke prior to the index event. Patients with a TIA had a median ABCD2 score of 4 (IQR 3-5). Median duration of hospital stay was 9 days (IQR 6-13). Patients in both trial arms received the same medical attention as indicated by similar proportions of thrombolysis and thrombectomy, access to post-discharge rehabilitation, intake of preventive medication at discharge, and length of hospital stay (Table 1). Baseline characteristics were balanced between the trial arms (Table 1), but a few differed between patients enrolled at the two study centres (Supplementary Table 1).
Table 1.
Characteristics of patients enrolled in the trial.
| Characteristics | STROKE-CARD care | Standard care | ||
|---|---|---|---|---|
| No. of patients | Mean ± SD, %, or median (IQR) | No. of patients | Mean ± SD, %, or median (IQR) | |
| Age (years) | 1438 | 69 ± 14 | 711 | 70 ± 13 |
| Female sex | 1438 | 41% | 711 | 41% |
| Index event | ||||
| Ischaemic stroke | 1438 | 82% | 711 | 86% |
| Recurrent stroke | 1180 | 14% | 611 | 15% |
| NIHSS score at hospital admission | 1180 | 3 (1-6) | 611 | 3 (1-6) |
| Intravenous thrombolysis | 1180 | 23% | 611 | 21% |
| Mechanical thrombectomy | 1180 | 5% | 611 | 5% |
| Discharge to rehabilitation centre | 1180 | 26% | 611 | 27% |
| TIA | 1438 | 18% | 711 | 14% |
| ABCD2 score | 258 | 4 (3-5) | 100 | 4 (4-5) |
| TOAST classification | ||||
| Large-artery atherosclerosis | 1438 | 22% | 711 | 17% |
| Cardiac embolism | 1438 | 26% | 711 | 27% |
| Small-artery occlusion | 1438 | 20% | 711 | 23% |
| Uncommon causes | 1438 | 4% | 711 | 5% |
| Undetermined causes | 1438 | 28% | 711 | 29% |
| Duration of hospital stay (days) | 1438 | 9 (6-13) | 711 | 9 (6-13) |
| Prior to index event | ||||
| Modified Rankin Scale | 1431 | 0 (0-0) | 698 | 0 (0-0) |
| Physical activity (min/week) | 749 | 373 (228-644) | 346 | 340 (228-644) |
| Smoking status | ||||
| Current smoker | 1438 | 24% | 711 | 23% |
| Ex-smoker | 1438 | 34% | 711 | 32% |
| Never smoker | 1438 | 42% | 711 | 45% |
| At hospital discharge | ||||
| Comorbidities | ||||
| Coronary heart disease | 1438 | 16% | 711 | 14% |
| Peripheral vascular disease | 1438 | 8% | 711 | 9% |
| Revascularisation procedures | 1438 | 18% | 711 | 18% |
| Hypertension | 1438 | 80% | 711 | 82% |
| Diabetes mellitus | 1438 | 21% | 711 | 20% |
| HbA1c (%) in patients with diabetes mellitus | 295 | 7.3 ± 1.6 | 142 | 7.4 ± 1.6 |
| Atrial fibrillation | 1438 | 24% | 711 | 26% |
| Intake of medication | ||||
| Lipid-lowering medication | 1438 | 81% | 711 | 81% |
| Oral anticoagulants or antiplatelet therapy | 1438 | 96% | 711 | 94% |
| Oral anticoagulants in patients with AF | 343 | 74% | 188 | 71% |
| Systolic blood pressure (mmHg) | 1407 | 134 ± 18 | 700 | 136 ± 18 |
| Diastolic blood pressure (mmHg) | 1407 | 77 ± 12 | 700 | 78 ± 12 |
| LDL cholesterol (mmol/L) | 1398 | 3.0 ± 1.0 | 705 | 3.0 ± 1.0 |
| Body mass index (kg/m2) | 1421 | 27 ± 5 | 702 | 26 ± 4 |
| Estimated GFR (mL/min/1.73m2) | 1438 | 71 ± 20 | 711 | 71 ± 20 |
| Modified Rankin Scale | 1438 | 1 (0-2) | 711 | 2 (0-2) |
Numbers are means and standard deviations, percentages or medians (IQR). Percentages may not total 100 because of rounding. There were no nominally significant differences between the two groups in baseline characteristics when correcting for multiple testing. To convert values for LDL cholesterol to mg/dL, multiply by 38.61. AF denotes atrial fibrillation, GFR glomerular filtration rate, HbA1c glycated haemoglobin, IQR interquartile range, LDL low-density lipoprotein, NIHSS National Institutes of Health Stroke Scale, SD standard deviation, and TIA transient ischaemic attack.
3.2. Co-primary outcomes
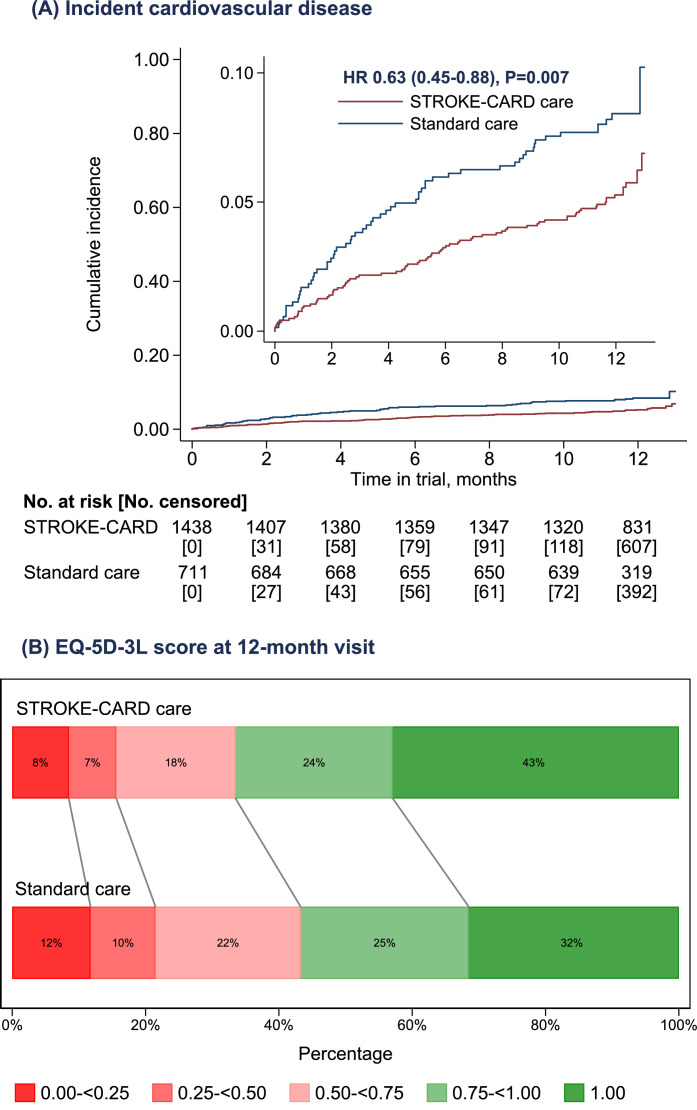
Over a median follow-up duration of 12.1 months (IQR 11.6-12.4), 137 major cardiovascular events occurred, including 95 nonfatal strokes (88 ischaemic, 7 haemorrhagic), 18 nonfatal myocardial infarctions, and 24 vascular deaths. 78 events occurred in patients allocated STROKE-CARD care (5.4%) and 59 in patients allocated standard care (8.3%) (Fig. 2A), corresponding to incidence rates per 1000 person-years of 57 (95% confidence interval [CI]: 45-71) and 89 (69-115). Compared with standard care, the hazard ratio (HR) for CVD with STROKE-CARD care was 0.63 (95% CI: 0.45-0.88; P =0.007). The number needed to treat to prevent one major CVD event in the first year after the stroke or TIA was 35 (95% CI: 19-154).
Fig. 2.
Effect of STROKE-CARD care on the co-primary outcomes.
Panel A shows the cumulative incidence of the composite cardiovascular disease endpoint; the inset shows the same data on an enlarged y axis. Panel B shows the distribution across categories of the EuroQol 5-Dimensions 3-Levels (EQ-5D-3L) health utility score at the 12-month visit. Higher EQ-5D-3L values indicate better health-related quality of life. HR denotes hazard ratio.
STROKE-CARD care also resulted in a better health-related quality of life after 12 months. The median EQ-5D-3L health utility score was 0.783 (IQR 0.687-1.000) in the STROKE-CARD care group and 0.779 (IQR 0.573-1.000) in the standard care group (P < 0.001). A score of 1.0 indicating absence of problems in all five EQ-5D-3L dimensions was achieved by 43% in the STROKE-CARD care group and 32% in the standard care group (relative risk 1.36; 95% CI: 1.20-1.54; P < 0.001) (Fig. 2B). A violin plot of the EQ-5D-3L overall health utility score at 12 months in the two groups is provided in Supplementary Figure 2.
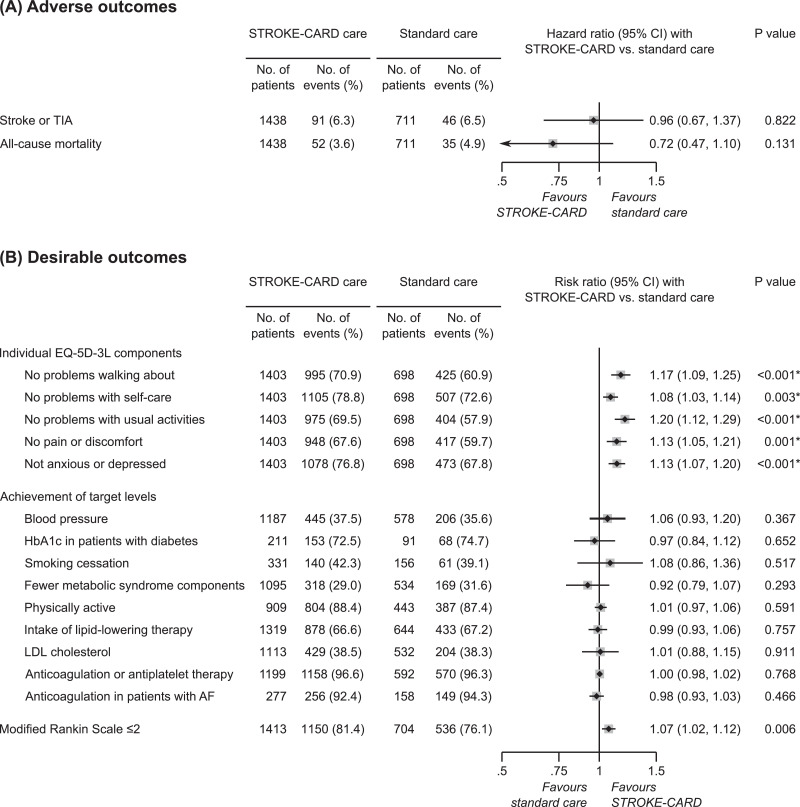
3.3. Pre-specified secondary outcomes
When comparing STROKE-CARD with standard care, the HR was 0.96 (95% CI: 0.67-1.37; P=0.822; 6.3 vs. 6.5% cumulative risk) for the composite outcome of stroke or TIA and 0.72 (0.47-1.10; P=0.131; 3.6 vs. 4.9% cumulative risk) for all-cause mortality (Fig. 3A and Supplementary Fig. 3).
Fig. 3.
Effect of STROKE-CARD care on the pre-specified secondary outcomes.
Panel A shows outcomes STROKE-CARD aimed to prevent; Panel B shows outcomes STROKE-CARD aimed to promote. *Indicates P values that met the pre-specified multiplicity-adjusted threshold for statistical significance. A single patient may have had multiple events and therefore may contribute information to more than one endpoint. AF denotes atrial fibrillation, CI confidence interval, EQ-5D-3L EuroQol 5-Dimensions 3-Levels, HbA1c glycated haemoglobin, LDL low-density lipoprotein, and TIA transient ischaemic attack.
Patients receiving STROKE-CARD care were less likely to have issues with walking about, self-care, performing usual activities, pain or discomfort, and anxiety or depression (Fig. 3B). Proportions of patients achieving target risk factor levels at 12 months did not differ significantly between trial arms (Fig. 3B). In the control group, the quality of risk factor control was not assessed prior to the 12-month visit.
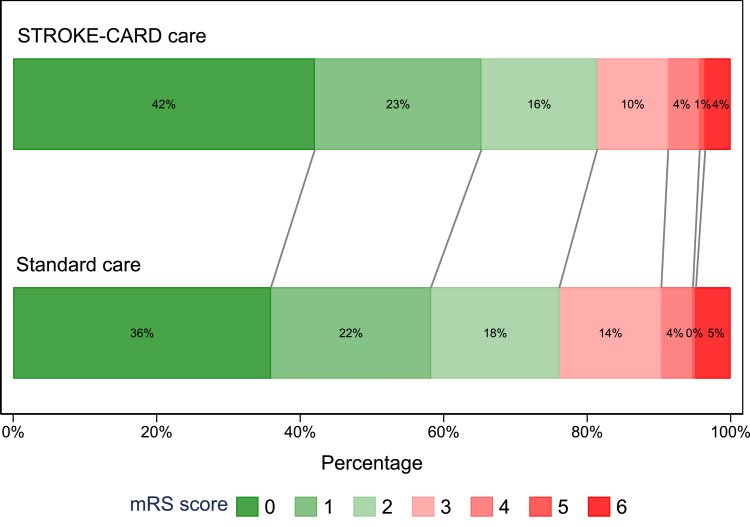
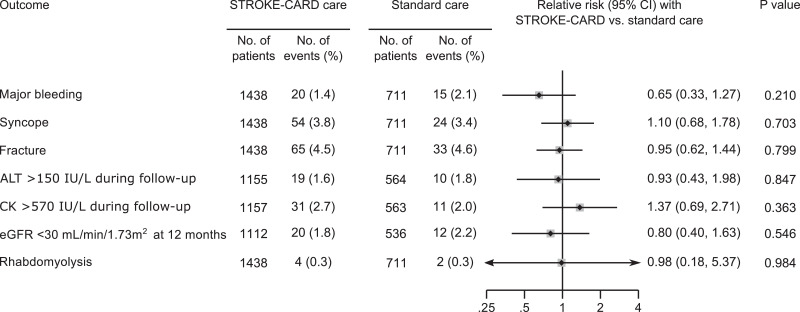
Functional independence 12 months after the index event (mRS ≤2) was achieved by 81.4% in the STROKE-CARD care group and 76.1% in the standard care group (relative risk, 1.07; 95% CI: 1.02-1.12; P = 0.006). The common odds ratio for a lower mRS score with STROKE-CARD care was 1.31 (95% CI: 1.12-1.55; P = 0.001) (Fig. 4) and remained significant when adjusting for age, sex, and mRS at discharge (1.19; 95% CI: 1.00-1.40; P = 0.044) and when excluding the 137 patients that experienced a major CVD event during follow-up (1.22; 95% CI: 1.03-1.44; P = 0.024). Finally, risk of potential side effects of intensified secondary prevention did not differ between trial arms (Fig. 5).
Fig. 4.
Functional outcome at 12 months assessed with the modified Rankin Scale.
The graph shows the distribution of scores for disability on the modified Rankin Scale (which range from 0 to 6, with higher scores indicating more severe disability) among patients in the standard care group versus patients in the STROKE-CARD care group. The numbers in the bar are percentages of patients who had each score; the percentages may not sum to 100% because of rounding. When analysing the shift of patients across all modified Rankin Scale categories at 12 months, the common odds ratio for a lower modified Rankin Scale score with STROKE-CARD care compared with standard care was 1.31 (95% confidence interval: 1.12-1.55; P = 0.001). mRS denotes modified Rankin Scale.
Fig. 5.
Effect of STROKE-CARD care on potential side effects of intensified secondary prevention.
For this analysis, the pre-specified threshold for statistical significance was P ≤ 0.05. A single patient may have had multiple events and therefore may contribute information to more than one endpoint. Relative risk refers to hazard ratios or risk ratios (dependent on the type of outcome). The analysis of laboratory parameters (ALT, CK, and eGFR) involved only data from the trial centre in Innsbruck. ALT denotes alanine aminotransferase, CI confidence interval, CK creatine kinase, and eGFR estimated glomerular filtration rate.
3.4. Pre-specified sensitivity analyses
We observed effects of STROKE-CARD care on the CVD outcome similar to the principal analysis when: (i) adjusting for age, sex, and type of index event (HR, 0.65; 95% CI: 0.46-0.91; P = 0.013); (ii) analysing patients as treated (HR, 0.64; 95% CI: 0.46-0.90 P = 0.010); (iii) analysing only patients that were treated per protocol (HR, 0.61; 95% CI: 0.43-0.87; P = 0.006); (iv) excluding patients whose index event had been a TIA with an ABCD2 score of 3; or (v) focusing the analysis on patient subgroups (Supplementary Figure 4). Sensitivity analyses for health-related quality of life after 12 months are provided in Supplementary Table 2.
3.5. Post-hoc explanatory analyses
Reflecting on the positive results, we got granular with the specific interventions delivered in the STROKE-CARD care group at the 3-month visit and provide numbers of patients targeted by these interventions in Supplementary Table 3. This analysis unravelled common refinements of cardiovascular prevention, high proportions of post-stroke complications, considerable demands for additional rehabilitation, and frequent warning signs of imminent CVD (4.6% of patients) within the first three months. Seven patients with new indications for carotid revascularisation were identified at the 3-month visit.
In exploratory analyses, the HR for CVD was 0.75 (95% CI: 0.50-1.12; P = 0.161) in patients with a mRS score of 0-2 at hospital discharge and 0.39 (0.21-0.75; P = 0.005) in patients with a mRS score of 3-4 (P for interaction=0.096). HRs for individual components of the composite CVD outcome were 0.81 (95% CI: 0.54-1.21; P = 0.297; 4.3 vs. 5.2% cumulative risk) for stroke, 0.32 (0.13-0.80; P = 0.014; 0.6 vs. 1.7% cumulative risk) for myocardial infarction, and 0.32 (0.16-0.66; P = 0.002; 0.9 vs. 2.7% cumulative risk) for vascular death. These findings should be interpreted with caution because the study was powered for the combined CVD endpoint.
4. Discussion
Management of stroke and TIA has improved tremendously over the past years with substantial advances in acute therapy, implementation of comprehensive pathways for stroke and TIA, and approval of novel effective preventive treatments. As a main unmet challenge, strategies of post-stroke care to maintain improved short-term patient outcome in the long run have to be developed and tested rigorously.
In our large-scale randomised controlled disease management trial among patients with ischaemic stroke or TIA, STROKE-CARD care reduced one-year cumulative incidence of CVD by about one third from 8.3% to 5.4% and ameliorated the patients’ health-related quality of life at 12 months (Fig. 2). Findings were consistent in pre-specified subgroups and confirmed in the per-protocol analysis (Supplementary Figure 4). Effect sizes tended to be higher in patients with non-minor stroke compared to TIA and minor stroke (P for interaction=0.096). Among secondary outcomes assessed at 12 months, we observed improvements in all individual dimensions of the EQ-5D-3L overall health-utility score and in one-year functional outcome, that each met the multiplicity-adjusted threshold for statistical significance (Fig. 3).
Only few previous trials of disease management programmes in stroke and TIA patients have focused on recurrent CVD. The SMART trial randomising 47 hospitals in China to a structured care programme or to usual care observed no effect on CVD outcomes after 12 months [20]. Limitations of this trial include a low uptake of the intervention, imbalance in baseline characteristics across trial arms, and its exclusive focus on risk factor control. In the DMP Stroke trial, rates for incident vascular events were lower in the intensified care group but statistical significance was not reached (HR 0.52; 95% CI: 0.24-1.17; P = 0.11) [21]. The recent large-scale INSPiRE-TMS trial randomised patients with acute minor stroke or TIA to an intensified secondary prevention programme or to conventional care and reported improved achievements of secondary prevention targets but no significant reduction in major vascular events [22]. Three disease management trials have addressed quality of life. Two reported null effects [23,24], whereas the TaCAS study observed pronounced effects of one or two simple post-discharge person-centred, self-management interventions on quality of life [25].
Importantly, the STROKE-CARD care programme entailed changes in the organisation of care, which can be achieved more easily than sustained changes in patient behaviour – the prime focus of most previous trials. STROKE-CARD care comprised a multifaceted 3-month intervention by the multidisciplinary stroke team. Individual measures in addition to counselling of patients and their care-givers are summarised in Supplementary Table 3 and included: (i) refinement of cardiovascular prevention strategies in order to achieve target levels or based on a reclassification of stroke aetiology [26,27] in no less than 43% of patients; (ii) systematic identification and treatment of post-stroke complications (exemplified in Supplementary Table 3, 19.9%-49.4%); (iii) standardised assessment of residual deficits and referral to additional rehabilitation in about one fifth of patients; and (iv) detection and management of warning signs of imminent CVD in 4.6% of patients.
These measures and respective achievements provide reasonable explanations for the improved health-related quality of life and functional outcome observed in our trial and provide also some clues for understanding the CVD benefit. First, the number of patients reporting CVD warning signs within the first three months after the index event was considerable and all were subjected to urgent pharmacological, endovascular, and surgical interventions. This procedure has likely prevented CVD events. STROKE-CARD care patients probably faced a reduced barrier to contact the hospital because the multidisciplinary stroke team formally extended its responsibility for them and offered a contact phone number. Second, there is good reason to assume that risk factor control was achieved earlier in the STROKE-CARD care group given the extra counselling during the web-portal introduction, the patients’ ambition to perform well at the 3-month visit, and the multiple refinements of CVD prevention performed as part of the 3-month visit. At the end of the follow-up, risk factor control was similar in both trial arms (Fig. 3B) and overall better than in previous real-world surveys in Europe [28], especially regarding the proportion of patients with atrial fibrillation taking anticoagulants (94.3%). Similar has been observed in the INSPiRE-TMS trial [22] and attributed to the facts that patients in both trial arms were managed by the same family doctors and trial inclusion per se enhances patient awareness. It is important to recognise that the inadvertent benefit in the control groups of INSPiRE-TMS and our trial may well have led to an underestimation of true effect sizes.
Our trial has several unique features and strengths. We report on a broad range of outcomes relevant in clinical practice, including major CVD events, health-related quality of life, and one-year functional outcome. Moreover, our study included patients with a broad spectrum of disease severities ranging from moderate-risk TIA to major ischaemic stroke and recruited near 90% of all eligible patients. Only patients unlikely to benefit from intensified secondary prevention were excluded, such as patients with assumed life expectancy of less than one year or permanent severe disability. Finally, full access to clinical records from the relevant hospitals and family doctors allowed complete and high-quality ascertainment of major cardiovascular outcomes, thereby reducing the potential for surveillance bias. One limitation of our trial is that it was conducted in a highly developed medical care system with advanced pathways for stroke care [13]. Although findings are not easily extrapolated to less developed systems of stroke care, the potential benefit of the intervention is presumably even higher. Moreover, block-randomisation is inferior to a standard randomisation procedure. However, the potential of selection bias is limited by the facts that the exact time and date of the stroke or TIA decided about patient allocation to the trial arms and about 90% of eligible patients consented to participate throughout the enrolment period. Importantly, patients in both trial arms received the same medical attention as indicated by similar proportions of thrombolysis and thrombectomy, access to post-discharge rehabilitation, intake of preventive medication at discharge, and length of hospital stay. Furthermore, uptake of the e-tool “MyStrokecard” was limited in this primarily elderly study population (regular use, 11.8%). While trial participants and study personnel were aware of the assigned treatment (open-label), clinical outcomes were adjudicated by a blinded endpoint committee using standardised diagnostic criteria. Finally, our study was limited to a 12-month follow-up. Thus, the sustainability of benefits over longer term remains to be determined.
In conclusion, STROKE-CARD care reduced CVD risk and improved health-related quality of life and functional outcome in patients with acute ischaemic stroke or TIA. Given the pragmatic intervention, STROKE-CARD care can easily be transferred into clinical routine. Our findings emphasise that optimal stroke care does not end with hospital discharge but should extend to a comprehensive 3-month reassessment performed by a multidisciplinary stroke team.
Funding
The Medical University of Innsbruck served as the sponsor of this study and received financial support from the university hospital (Tirol Kliniken), Tyrolean Health Insurance Company (TGKK), the Tyrol Health Care Funds (TGF), and unrestricted research grants from Boehringer Ingelheim, Nstim Services, and Sanofi. The study centre in Vienna additionally received a grant from Bayer Healthcare. LT and LS were supported by the Dr.-Johannes-and-Hertha-Tuba Foundation and a K-project grant from the Austrian Research Promotion Agency (“VASCage”, grant 843536). CB and SKi were supported by the excellence initiative VASCage (Centre for Promoting Vascular Health in the Ageing Community, project number 868624), an R&D K-Centre of the Austrian Research Promotion Agency (COMET program - Competence Centers for Excellent Technologies) funded by the Austrian Ministry for Transport, Innovation and Technology, the Austrian Ministry for Digital and Economic Affairs and the federal states Tyrol, Salzburg, and Vienna. The study sponsor and funders had no influence on the study design and clinical decisions, and no role in data analysis, interpretation, and publication.
The STROKE-CARD study group
Markus Anliker, Christian Boehme, Julia Ferrari, Martin Furtner, Andrea Griesmacher, Viktoria Hasibeder, Stefan Kiechl, Gerhard Klingenschmid, Michael Knoflach, Stefan Krebs, Clemens Lang, Wilfried Lang, Lukas Mayer, Anna Neuner, Raimund Pechlaner, Thomas Porpaczy, Gerhard Rumpold, Christoph Schmidauer, Gudrun Schoenherr, Lisa Seekircher, Martin Sojer, Christine Span, Lydia Thiemann, Thomas Toell, Lena Tschiderer, Marlies Wichtl, Johann Willeit, Karin Willeit, Peter Willeit.
Declaration of Competing Interests
PW reports personal fees from Novartis Pharmaceuticals and non-financial support from Bayer, Daiichi Sankyo, and Sanofi outside the submitted work. TT reports non-financial support from Bayer and Pfizer outside the submitted work. CB reports non-financial support from EVER Pharma, Amgen, Medtronic, Daiichi Sankyo, and Bayer outside the submitted work. SKr reports non-financial support from Bayer and Pfizer outside the submitted work. LM reports non-financial support from Bayer and personal fees from Daiichi Sankyo, outside the submitted work. LS and LT report grants from VASCage (grant 843536) and the Dr.-Johannes-and-Hertha-Tuba Foundation during the conduct of the study, and non-financial support from Sanofi outside the submitted work. KW reports non-financial support from Bayer and Boehringer outside of the submitted work. GR is an owner of the intellectual property rights of the web-based patient portal for risk factor monitoring. JF reports non-financial support from Boehringer Ingelheim outside the submitted work. MK reports personal fees from Boehringer Ingelheim, Daiichi Sankyo, and Sanofi, and non-financial support from Pfizer. WL reports grants from Bayer during the conduct of the study, and personal fees from Amgen, Bayer, Boehringer, Daichii Sankyo, Medtronic, Pfizer, and Sanofi, and non-financial support from Bayer, Boehringer, and Pfizer, outside the submitted work. SKi reports grants from Tirol Kliniken, Tyrolean Health Insurance Company, Tyrol Health Care Funds, Boehringer, Nstim Services, Sanofi, and the Austrian Research Promotion Agency (FFG) during the conduct of the study, and personal fees from Amgen, Bayer, Boehringer, Pfizer, Medtronic, and Sanofi, and non-financial support from Boehringer outside the submitted work. JW reports grants from Tirol Kliniken, Tyrolean Health Insurance Company, Tyrol Health Care Funds, Boehringer, Nstim Services, and Sanofi during the conduct of the study, and personal fees from Amgen, Bayer, Boehringer, Daichii-Sankyo, Pfizer, Medtronic, and Sanofi, and non-financial support from Bayer and Boehringer, outside the submitted work. The other authors report no competing interests.
Author Contributions
PW wrote the analysis plan, was responsible for data management and cleaning, performed the statistical analysis, had access to all raw data, and drafted the manuscript. TT designed the study, recruited patients, collected patient data, performed follow-up ascertainment, and drafted the manuscript. CB recruited patients, collected patient data, performed follow-up ascertainment, and drafted the manuscript. SKr, LM, CL, and KW recruited patients, collected patient data, and performed follow-up ascertainment. LT and LS contributed to data management and cleaning. GR provided the web-based patient portal for risk factor monitoring. GS collected patient data and lead the team of neurological therapists. AG was responsible for the performance of the laboratory measurements at the University Hospital of Innsbruck. JF, MK, and WL designed the study and secured funding. SKi and JW designed the study, secured funding, and drafted the manuscript. All authors contributed to writing the final report and data interpretation and approved the version submitted.
Data statement
Anonymised patient data are available for use in independent scientific research to researchers upon reasonable request (peter.willeit@i-med.ac.at). Data will be provided following review and approval of a research proposal (including a statistical analysis plan) and completion of a data sharing agreement.
Acknowledgements
We thank the participants, the collaborating physicians, the nursing teams, the teams of stroke therapists, and other professionals that have helped conduct the trial (individual members of the teams are listed in the appendix).
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2020.100476.
Contributor Information
Peter Willeit, Email: peter.willeit@i-med.ac.at.
Stefan Kiechl, Email: stefan.kiechl@i-med.ac.at.
Appendix. Supplementary materials
References
- 1.GBD 2017 Causes of Death Collaborators Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1736–1788. doi: 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.GBD 2016 Causes of Death Collaborators Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1151–1210. doi: 10.1016/S0140-6736(17)32152-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Amarenco P, Lavallée PC, Monteiro Tavares L. Five-year risk of stroke after TIA or minor ischemic stroke. N Engl J Med. 2018;378:2182–2190. doi: 10.1056/NEJMoa1802712. [DOI] [PubMed] [Google Scholar]
- 4.Bergström L, Irewall A-L, Söderström L, Ögren J, Laurell K, Mooe T. One-year incidence, time trends, and predictors of recurrent ischemic stroke in sweden from 1998 to 2010: an observational study. Stroke. 2017;48:2046–2051. doi: 10.1161/STROKEAHA.117.016815. [DOI] [PubMed] [Google Scholar]
- 5.Samsa GP, Bian J, Lipscomb J, Matchar DB. Epidemiology of recurrent cerebral infarction: a medicare claims-based comparison of first and recurrent strokes on 2-year survival and cost. Stroke. 1999;30:338–349. doi: 10.1161/01.str.30.2.338. [DOI] [PubMed] [Google Scholar]
- 6.Boulanger M, Béjot Y, Rothwell PM, Touzé E. Long-term risk of myocardial infarction compared to recurrent stroke after transient ischemic attack and ischemic stroke: systematic review and meta-analysis. J Am Heart Assoc. 2018;7 doi: 10.1161/JAHA.117.007267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hackam DG, Spence JD. Combining multiple approaches for the secondary prevention of vascular events after stroke: a quantitative modeling study. Stroke. 2007;38:1881–1885. doi: 10.1161/STROKEAHA.106.475525. [DOI] [PubMed] [Google Scholar]
- 8.Chowdhury R, Khan H, Heydon E. Adherence to cardiovascular therapy: a meta-analysis of prevalence and clinical consequences. Eur Heart J. 2013;34:2940–2948. doi: 10.1093/eurheartj/eht295. [DOI] [PubMed] [Google Scholar]
- 9.Bridgwood B, Lager KE, Mistri AK, Khunti K, Wilson AD, Modi P. Interventions for improving modifiable risk factor control in the secondary prevention of stroke. Cochrane Database Syst Rev. 2018;5 doi: 10.1002/14651858.CD009103.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Toell T, Boehme C, Mayer L. Pragmatic trial of multifaceted intervention (STROKE-CARD care) to reduce cardiovascular risk and improve quality-of-life after ischaemic stroke and transient ischaemic attack -study protocol. BMC Neurol. 2018;18:187. doi: 10.1186/s12883-018-1185-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sacco RL, Kasner SE, Broderick JP. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American heart association/american stroke association. Stroke. 2013;44:2064–2089. doi: 10.1161/STR.0b013e318296aeca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johnston SC, Rothwell PM, Nguyen-Huynh MN. Validation and refinement of scores to predict very early stroke risk after transient ischaemic attack. Lancet. 2007;369:283–292. doi: 10.1016/S0140-6736(07)60150-0. [DOI] [PubMed] [Google Scholar]
- 13.Willeit J, Geley T, Schöch J. Thrombolysis and clinical outcome in patients with stroke after implementation of the Tyrol Stroke Pathway: a retrospective observational study. Lancet Neurol. 2015;14:48–56. doi: 10.1016/S1474-4422(14)70286-8. [DOI] [PubMed] [Google Scholar]
- 14.Mayer L, Ferrari J, Krebs S. ABCD3-I score and the risk of early or 3-month stroke recurrence in tissue- and time-based definitions of TIA and minor stroke. J Neurol. 2018;265:530–534. doi: 10.1007/s00415-017-8720-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thygesen K, Alpert JS, Jaffe AS. Fourth Universal Definition of Myocardial Infarction (2018) J Am Coll Cardiol. 2018;72:2231–2264. doi: 10.1016/j.jacc.2018.08.1038. [DOI] [PubMed] [Google Scholar]
- 16.Szende A, Janssen B, Cabases J, editors. Self-reported population health: an international perspective based on EQ-5D. Springer; Netherlands. Dordrecht: 2014. [PubMed] [Google Scholar]
- 17.Greiner W, Weijnen T, Nieuwenhuizen M. A single European currency for EQ-5D health states. Results from a six-country study. Eur J Health Econ. 2003;4:222–231. doi: 10.1007/s10198-003-0182-5. [DOI] [PubMed] [Google Scholar]
- 18.Dmitrienko A, D'Agostino RB. Multiplicity considerations in clinical trials. N Engl J Med. 2018;378:2115–2122. doi: 10.1056/NEJMra1709701. [DOI] [PubMed] [Google Scholar]
- 19.McNutt L-A, Wu C, Xue X, Hafner JP. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol. 2003;157:940–943. doi: 10.1093/aje/kwg074. [DOI] [PubMed] [Google Scholar]
- 20.Peng B, Ni J, Anderson CS. Implementation of a structured guideline-based program for the secondary prevention of ischemic stroke in China. Stroke. 2014;45:515–519. doi: 10.1161/STROKEAHA.113.001424. [DOI] [PubMed] [Google Scholar]
- 21.Fukuoka Y, Hosomi N, Hyakuta T. Effects of a Disease Management Program for Preventing Recurrent Ischemic Stroke. Stroke. 2019;50:705–712. doi: 10.1161/STROKEAHA.118.020888. [DOI] [PubMed] [Google Scholar]
- 22.Ahmadi M, Laumeier I, Ihl T. A support programme for secondary prevention in patients with transient ischaemic attack and minor stroke (INSPiRE-TMS): an open-label, randomised controlled trial. Lancet Neurol. 2019 doi: 10.1016/S1474-4422(19)30369-2. [DOI] [PubMed] [Google Scholar]
- 23.Barker-Collo S, Krishnamurthi R, Witt E. Improving adherence to secondary stroke prevention strategies through motivational interviewing: randomized controlled trial. Stroke. 2015;46:3451–3458. doi: 10.1161/STROKEAHA.115.011003. [DOI] [PubMed] [Google Scholar]
- 24.Boter H. Multicenter randomized controlled trial of an outreach nursing support program for recently discharged stroke patients. Stroke. 2004;35:2867–2872. doi: 10.1161/01.STR.0000147717.57531.e5. [DOI] [PubMed] [Google Scholar]
- 25.Fu VWY, Weatherall M, McPherson K. Taking Charge after Stroke: A randomized controlled trial of a person-centered, self-directed rehabilitation intervention. Int J Stroke. 2020 doi: 10.1177/1747493020915144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kamel H, Merkler AE, Iadecola C, Gupta A, Navi BB. Tailoring the approach to embolic stroke of undetermined source: a review. JAMA Neurol. 2019 doi: 10.1001/jamaneurol.2019.0591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Diener H-C. The cause of stroke matters for secondary prevention. Lancet Neurol. 2017;16:256–257. doi: 10.1016/S1474-4422(17)30057-1. [DOI] [PubMed] [Google Scholar]
- 28.Heuschmann PU, Kircher J, Nowe T. Control of main risk factors after ischaemic stroke across Europe: data from the stroke-specific module of the EUROASPIRE III survey. Eur J Cardiovasc Prev Rehabil. 2015;22:1354–1362. doi: 10.1177/2047487314546825. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.