Abstract
Background
Rapid naloxone administration is crucial in reversing an opioid overdose. We investigated whether equipping community members, including people who use opioids (PWUO), with a smartphone application enabling them to signal and respond to suspected overdose would support naloxone administration in advance of Emrgency Medical Services (EMS).
Methods
This observational cohort study of opioid overdose intervention used a dedicated smartphone app, UnityPhilly, activated by volunteers witnessing an overdose to signal other nearby volunteers in Philadelphia (March 2019 - February 2020). Alerted volunteers chose to respond, or declined to respond, or ignored/missed the alert. Witnessing volunteer was connected to 9-1-1 through a semi-automated telephone call. The primary outcome was layperson-initiated overdose reversal before EMS arrival, and a secondary outcome was hospital transfer. This study is registered with ClinicalTrials.gov, NCT03305497.
Findings
112 volunteers, including 57 PWUO and 55 community members, signaled 291 suspected opioid overdose alerts. 89 (30⸱6%) were false alarms. For 202 true alerts, the rate of layperson initiated naloxone use was 36⸱6% (74/202 cases). Most naloxone-use cases occurred in the street (58⸱11% (43/74)) and some in home settings (22⸱98% (17/74)). The first naloxone dose was provided by a nearby volunteer responding to the alert in 29⸱73% (22/74) of cases and by the signaling volunteer in 70⸱27% (52/74) of cases. Successful reversal was reported in 95⸱9% (71/74) of cases. Layperson intervention preceded EMS by 5 min or more in 59⸱5% of cases. Recovery without hospital transport was reported in 52⸱7% (39/74) of cases.
Interpretation
Our findings support the benefits of equipping community members, potentially witnessing suspected opioid overdose, with naloxone and an emergency response community smartphone app, alerting EMS and nearby laypersons to provide additional naloxone.
Funding
Funding provided by NIH through NIDA, grant number: 5R34DA044758.
Research in context.
Evidence before this study
A recognized remaining challenge in decreasing lethal opioid overdoses is ensuring naloxone reaches those in need at short notice. The time-sensitive nature of opioid overdose and its occurence in the community are two crucial characteristics in common with Out-of-hospital cardiac arrest (OHCA). Yet just last year OHCA has been characterised as a unique medical emergency given its unpredictable and time-sensitive nature, with “no other medical situation having such a vital reliance on the community”. We believe that one answer to the challenge of the former lies in reconsidering the latter. Recognizing this may open the door to new interventions and lower mortality. There has been an abundance of research on OHCA covering layperson CPR training, automatic external defibrillator (AED) placement and tracking, proximity-based volunteer notification, and integration with emergency services dispatch. Previous opioid overdose and drug policy studies have established the importance of making naloxone widely available in the community. The use of a smartphone-based layperson responder network to signal and respond to opioid overdose incidents has yet to be investigated.
Added value of this study
We report the first observational cohort study of community members equipped with naloxone and a smartphone application to signal and respond to opioid overdoses. We followed the cohort over one year in which they lived and/or worked in a neighborhood with high incidence of opioid overdose. We showed that laypersons, including people who use opioids (PWUO), can effectively signal and respond to overdose incidents to administer nasal naloxone in advance of EMS arrival. We observed 202 layperson-initiated overdose true alerts with a rate of layperson naloxone administration of 36⸱6% (74/202) and found that naloxone-based reversal was initiated over 5 min prior to EMS arrival in 59⸱6% of these cases. Without timely reversal, opioid overdose causes respiratory depression that may deteriorate into apnea, leading to anoxic injury. We observed layperson support behaviors, including contacting EMS and remaining with the victim until recovery, that are consistent with American Heart Association guidelines and strengthens the chain of survival that begins in the community.
Implications of all the available evidence
For opioid overdose, as for OHCA, layperson response is a key link in the “chain of survival”, the complex relationship between bystanders, emergency services, and hospitals. Locating a nearby volunteer with naloxone presents some unique challenges but is not inherently different than locating a nearby AED. It is time to recognize that opioid use disorder patients can benefit from similar forms of community support that we advance for OHCA. Creating and studying smartphone-based emergency response communities for naloxone provision can help address this important challenge.
Alt-text: Unlabelled box
1. Introduction
A crippling opioid epidemic continues to grip the United States [1, 2] where the drug overdose death rate was 20⸱7 per 100,000 in 20183. Philadelphia has the highest per capita overdose mortality rate among large U.S. cities, with 1150 deaths in 2019 and a death rate of over 60 per 100,000 [3, 4]. The use of naloxone hydrochloride (naloxone) an opioid receptor antagonist that displaces opioid drugs (e.g., heroin, fentanyl, or morphine) interferes with their respiratory depressant effects, thus reversing the immediate effects of opioid overdose, and has achieved widespread acceptance as part of initial emergency response [2, [5], [6], [7]]. American Medical Association (AMA) [8] and World Health Organization (WHO) [9] guidelines advocate making naloxone widely available “in the community” in the hope that distribution of naloxone to laypersons may reduce time to naloxone administration and thus reduce mortality in opioid overdose [10]. Naloxone access throughout Pennsylvania was increased through a standing order issued in 2015 [11]. While the availability of intranasal naloxone has greatly facilitated the administration of naloxone by laypersons, we are still faced with the challenge of ensuring naloxone can reach those who need it at short notice [2]. The aim of our study was to assess the feasibility of a smartphone-based layperson responder network for opioid overdose in Philadelphia, with the potential for volunteer responders to use intranasal naloxone to initiate overdose reversal in advance of Emergency Medical Services (EMS).
We observe that striking parallels for emergency healthcare delivery exist between opioid overdose in the community and out-of-hospital cardiac arrest (OHCA). Yet OHCA has been characterised as a unique medical emergency with time-sensitive characteristics and a reliance on the community found in no other medical situation [12]. This view is supported by decades of research into creating networks of layperson responders trained in cardiopulmonary resuscitation (CPR) and automated external defibrillator (AED) programs - recognized priorities for OHCA response [13]. Studies show that CPR and early defibrillation by a layperson, in advance of EMS, contributes to positive outcomes after OHCA [14, 15]. This has improved with the introduction of public-access AEDs, providing an infrastructure for citizen use, and the introduction and study of smartphone dispatch of nearby laypersons [15], [16], [17], [18], [19]. Nonetheless, the two key characteristics that make OHCA unique, time-sensitivity and reliance on community, dominate what we know of the opioid overdose care environment [1, 2, 5].
In sharp contrast to OHCA, evidence to inform management of suspected opioid overdose with intranasal naloxone is very limited [5], and the use of a smartphone-based layperson responder network to attend and intervene at opioid overdose incidents has not been investigated. Our objective is to assess such an intervention by observing actual response and naloxone administration rates by laypersons equipped with an emergency response app for opioid overdose, providing evidence in support of future studies paralleling those undertaken for OHCA.
2. Methods
2.1. Study design, population, and settings
We conducted a community-based observational cohort study [20, 21] in the Philadelphia neighborhood of Kensington, from March 2019 through February 2020. Kensington, where fentanyl, heroin, prescription opioids, and other illegal drugs are openly sold, has Philadelphia's highest concentration of overdose deaths [22]. Kensington is also home to Prevention Point Philadelphia, the only city-sanctioned syringe exchange program in Philadelphia, and one of only two in the state of Pennsylvania, and a primary distribution site for naloxone and other harm reduction services [23]. We selected Kensington due to its high number of overdoses, its population density, and the proximity of Prevention Point as a possible recruitment venue.
Volunteers were trained in recognizing opioid overdose, the use of intranasal naloxone, and use of a dedicated smartphone app to signal and/or respond to a suspected overdose alert. The app was activated by volunteers witnessing an overdose to signal other nearby volunteers. We looked for three possible scenarios when volunteers received an alert. Volunteers receiving an alert chose to respond and help, explicitly declined to respond, or missed/ignored the alert. The witnessing volunteer was connected to speak with 9-1-1 dispatch through a semi-automated telephone call. The primary outcome was layperson-initiated overdose reversal before the arrival of EMS/first responders. Our report follows STROBE guidelines [20].
2.2. The UnityPhilly emergency response community app
UnityPhilly is an Emergency Response Community (ERC) app designed to support laypersons in signaling and responding to opioid overdose incidents [24, 25]. The app SOS function enabled volunteers to signal an overdose incident with a single button press, initiating an automated alert to other nearby volunteer app users (Fig. 1a). For this study, ‘nearby’ was defined as within a 15 min estimated time of arrival (ETA) to the overdose site, calculated dynamically based on the participants’ declared transport mode (foot, car, etc.). Concurrent with sending the alert, a call was initiated from the signaler's smartphone to a dedicated PSAP (Public Safety Answering Point) phone number connecting to the Philadelphia Police EMS dispatch unit. Smartphone operating system constraints resulted in slightly different EMS call behavior for Android and Apple-based phones. On Android handsets calls were placed immediately when the SOS button was pressed. On Apple (IOS) handsets, a pop-up with the EMS phone number appeared requiring the caller to confirm the dial request.
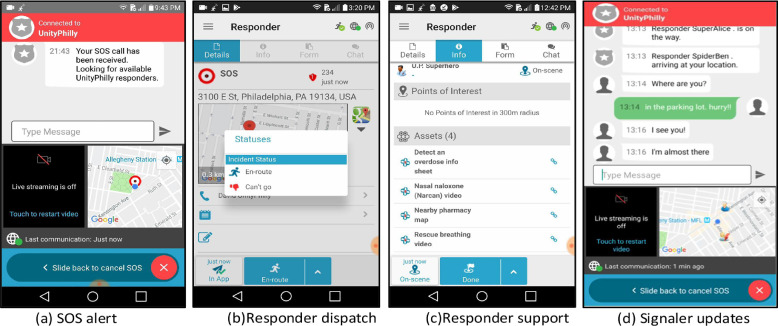
Fig. 1.
UnityPhilly Smartphone App Interface Screens. (a) SOS alert (b) Responder dispatch (c) Responder support (d) Signaler updates.
Volunteers receiving the alert enter the Responder module (Fig. 1b and c) enabling them to choose to respond or decline to respond to the alert; navigate to the overdose site; communicate with the signaler and other responding volunteers (Fig. 1d); and review salient overdose information including instruction for recognizing overdose, administering naloxone, and rescue breathing.
2.3. EMS notification and involvement
Philadelphia EMS is one of the busiest systems in the United States and uses a priority dispatch system [26]. Overdose/poisoning (unconscious, MPDS code 23D1) is considered a high priority (Delta) dispatch, immediately life threatening and very time sensitive [27].
A pre-trial version of the UnityPhilly app featured an automatic computer-generated voice call to EMS in which the system “spoke” to a human EMS dispatcher and provided the address+GPS coordinates, and a message that an opioid overdose had occurred - without any direct interaction between EMS dispatch and the human signaller. The text of the original message was “Hi, I am reporting an overdose incident that is happening now. This automated message was generated by the UnityPhilly app and will repeat twice. The overdose is occurring at {Street Address}, {City}. The GPS coordinates are {SOS location GPS x} and {SOS location GPS y}. Please send an ambulance with naloxone.” During pre-trial consultations with Philadelphia EMS, concerns for situational assessment and control were raised leading to an EMS request that this functionality be removed and that a direct person-to-person voice call be established. Therefore, we modified the app to comply with Philadelphia EMS requirements, which enabled a process whereby standard EMS caller interrogation protocols could be followed irrespective of the additional layperson support provided through the ERC app. These phone calls were initiated immediately and without delay when a participant, having encountered a suspected opioid overdose, pressed the SOS button.
We distinguish between false alarms as determined by EMS, and false alarms as determined by data analysts for our research. Under no circumstance did our system or participants make any determination that EMS should consider a call to be false, which was solely in the hands of EMS when they received a phone call. We do not report false alarms as determined by EMS. In analyzing our data, we observed many SOS alerts in which the signaller canceled the alert within 2 min or the signaller wrote a chat message to tell other participants that the alert was false. In these cases, and only in these cases, we treat those incidents as false for data analysis purposes. In no way did cancelation of an app alert or a cancelation chat message influence EMS response.
2.4. Recruiting and enrollment
Rolling enrollment of participants (n = 112) occurred in Kensington between October 2018 and January 2020. Recruitment occurred via face-to-face screening at Prevention Point's drop-in center, Prevention Point's substance use disorder treatment van, street intercepts, and chain referrals from enrolled participants.
Inclusion requirements for participants were that they lived, worked, or used drugs within four zip codes around the Kensington neighborhood (19122, 19125, 19133, 19134); possessed a smartphone with a data plan; were willing to have location/movements tracked via an app; were willing to carry naloxone; and were aged 18 years or older. Sampling purposely targeted a mix of members of the Kensington community who used opioids non-medically in the past 30 days and those who reported no non-medical opioid use in the past 30 days.
At a research storefront in Kensington, study enrollment included: written informed consent; recording of contact information; structured baseline interview; app installation and training; and naloxone distribution and training. During informed consent, participants agreed to a baseline interview, monthly follow up interviews, and brief surveys following overdose incidents. Project staff installed the app on the participant's smartphone, followed by app training which included watching an animated training video explaining app use, and practicing using the app to send and receive alerts with project staff. The training video, which highlights the app's main functions, can be found in the online supplementary material. Naloxone training included recognizing signs of opioid overdose, practicing rescue breathing on a CPR dummy, and demonstrating how to administer intranasal naloxone. All participants received a kit containing two doses of intranasal naloxone (2 × 4 mg). Overdose prevention training was designed to be adaptive to the expertise of the participants and was delivered by trained staff interviewers. The curriculum included typical components of community-based opioid overdose prevention training, [28] such as an overview of opioids and risk factors for opioid overdose, opioid overdose recognition, and essential responses to an opioid overdose outlined by the American Heart Association [29]. Participants were provided with a hands-on opportunity to practice intranasal naloxone administration with a demo model and simulate rescue breathing using a manikin and face shield. At the end of the training, the participants answered review questions and received a naloxone kit including two doses of intranasal naloxone with instructions, disposable gloves, and a face shield. The session lasted 15–20 min for participants never trained in overdose prevention and 2–5 min for participants who needed refresher training. Participants received $25 in cash for the baseline interview and $5 for each completed follow up monthly interview or incident survey. No compensation was offered or given for usage of the app to signal or respond to overdose incidents.
The sample size for this observational feasibility study was determined by the sample sizes of other feasibility studies in the literature and resources provided by the grant mechanism for study staff and participant-related costs [30]. In this case, we determined that we had adequate resources for 112 participants: recruit, interview, and train in naloxone administration and app use; provide intranasal naloxone at recruitment and refills; provide participant incentives at baseline and for follow-up interviews; and track/retain during the 12 month follow up.
All study procedures were approved by the Drexel University Institutional Review Board, and registered with ClinicalTrials.gov (NCT03305497).
2.5. Layperson participation and dispatch
Participants were instructed to signal an SOS alert when they encountered a suspected opioid overdose, to administer naloxone if they had any, and to speak with 9-1-1 through a phone call initiated by the app. Location data from the volunteer's smartphone were transmitted to UnityPhilly servers which automatically checked for other nearby volunteers and sent dispatch alerts with the overdose location to the four closest. The system sent alerts to additional volunteers if an alerted volunteer did not acknowledge within 2 min. In this manner, additional volunteers were notified of the incident until either 4 had confirmed they were en-route, or there were no additional volunteers within the ETA radius.
Volunteer locations were automatically updated every 15 min by a message sent from the app to the server. Signalers in SOS mode were automatically informed when nearby volunteers were found, when volunteers indicated they were responding, and when a volunteer was arriving on scene (Fig. 1d).
2.6. Data collection
Three sources of data were collected and analyzed:
-
(1)
Structured baseline interview. The interview included structured questions focusing on demographics, history of witnessing or responding to drug overdoses, personal history of overdose, and drug use history.
-
(2)
App system data. All app activities were timestamped and logged on the system server. Activities examined in this analysis are: signaling an overdose by pressing the SOS button; receiving an alert based on location ETA; agreeing to respond to an alert by selecting “En-route”; declining to respond to an alert by selecting “Can't go”; and arriving on scene to the location of an overdose. The incident number, participant ID, and date and time was recorded for each activity. No activity data was retained on participant smartphones.
-
(3)
Incident survey data. Within 72 h following each suspected overdose incident alert, a Qualtrics-based incident survey was sent to study participants involved in the incident. Survey text included the date and time of the overdose incident to help trigger recollection. Incident involvement was defined as: (a) signaling the alert; (b) selecting “En-route” to accept a request to respond to an alert; or (c) selecting “Can't go” to decline a request to respond to an alert. The survey instrument polled respondents on the observed condition of the victim; naloxone administration; number of naloxone doses administered; arrival of EMS/police/fire responders; time lapsed between layperson arrival and EMS/police/fire arrival; observed victim recovery; and post-recovery actions.
2.7. Outcome measures
The primary outcome was the rate of layperson-initiated overdose reversal through administration of naloxone before the arrival of an ambulance or first responders. A secondary outcome was transfer of the overdose victim to a healthcare facility. All diagnosis and outcome measures are based on laypersons/nonmedical self-reports in the aforementioned incident survey data.
2.8. Statistical analysis
In keeping with accepted guidelines for reporting feasibility results, we mainly report descriptive statistics [20, 31]. Data were analyzed with IBM SPSS Statistics version 25. Baseline interview data were used to describe the participants by demographics, history of opioid misuse and treatment, history of personal and witnessed overdose, and history of overdose prevention training; these results were stratified by current opioid use (Table 1). App system data and incident surveys were used to assess study outcomes, including laypersons’ naloxone use, successful reversals, and hospital transfers (Table 2). All categorical variables were summarized with frequencies and percentages. Mean and standard deviation were computed for age, a variable with moderately skewed distribution. Medians and interquartile ranges (IQR) were calculated for count variables with highly skewed distribution, including the number of days in the study, the number of lifetime personal and witnessed overdoses, the number of lifetime naloxone administrations, and the number of naloxone doses administered at overdose events signaled by volunteers.
Table 1.
Sociodemographic, drug use and overdose profile of study participants.
| Categories | Variables | Total N = 112 | Community Members (CM) n = 55 | People Who Use Opioids (PWUO)n = 57 |
|---|---|---|---|---|
| % (n) | % (n) | % (n) | ||
| Demographics | Age (years) Mean (SD) Range |
38.9 (10.2) 21–69 |
41.9 (11.5) 22–69 |
36.1 (7.9) 21–54 |
| Gender identity Men Women Transgender or Genderqueer/Non-binary |
48.2 (54) 50.9 (57) 0.9 (1) |
41.8 (23) 56.4 (31) 1.8 (1) |
54.4(31) 45.6 (26) 0 |
|
| Race Non-Hispanic White Hispanic or Latino Non-Hispanic Black Non-Hispanic American Indian or Native American Non-Hispanic Asian or Asian American |
67.9 (76) 21.4 (24) 8.0 (9) 1.8 (2) 0.9 (1) |
61.8 (34) 27.3 (15) 9.1 (5) 0 1.8 (1) |
73.7 (42) 15.8 (9) 7.0 (4) 3.5 (2) 0 |
|
| Employment, full- or part-time | 35.7 (40) | 52.7 (29) | 19.3 (11) | |
| Neighborhood of residence: Kensington | 64.3 (72) | 58.2 (32) | 70.2 (40) | |
| Homelessness, past 30 days | 29.5 (33) | 16.4 (9) | 42.1 (24) | |
| History of opioid misuse and treatment | Lifetime misuse of opioids1 30-day misuse of opioids1 Lifetime medication-assisted treatment (MAT)2 |
72.3 (81) 50.9 (57) 50.9 (57) |
43.6 (24) 0 27.3 (15) |
100.0 (57) 100.0 (57) 73.7 (42) |
| Lifetime personal and witnessed opioid overdose | Prevalence of witnessed overdose Frequency of witnessed overdose, median (IQR)3 |
95.5 (107) 10.0 (5.0–20.0) |
90.9 (50) 10.0 (4.0–20.0) |
100.0 (57) 10.0 (5.0–20.0) |
| Prevalence of personal overdose Frequency of personal overdose, median (IQR)4 |
53.6 (60) 0.5 (0–3.0) |
27.3 (15) 0 (0–0) |
78.9 (45) 2.0 (1.0–3.5) |
|
| Lifetime naloxone training and use | Training in naloxone use Frequency of giving naloxone to a person who experienced an opioid overdose, median (IQR)5 |
86.6 (97) 4.0 (2.0–11.0) |
85.5 (47) 3.0 (2.0–10.0) |
87.7 (50) 6.0 (2.0–11.0) |
IQR=Interquartile Range.
Includes heroin, fentanyl, and prescription opioids.
Includes treatment with methadone, buprenorphine/naloxone, or vivitrol.
Total n = 106, CM=53, PWUO=53.
Total n = 104, CM=53, PWUO=51.
Total n = 107, CM=50, PWUO=57.
Table 2.
Primary and secondary outcomes.
| Outcomes | Result | % (n) |
|---|---|---|
| Primary outcome: volunteer-initiated suspected overdose alert (n = 202) | At least one dose of naloxone administered | 36.63 (74) |
| No naloxone administered | 63.37(128) | |
| Nasal naloxone administration cases (n = 74) | Successful reversal | 95.95 (71) |
| On-scene death | 1.35 (1) | |
| Outcome unreported | 2.70 (2) | |
| Role of volunteer providing naloxone (n = 74) | Signaled alert and gave 1st dose | 70.27 (52) |
| Responded to alert with 1st dose | 29.73 (22) | |
| Responded to alert with 2nd dose | 5.41 (4) | |
| EMS/First-responder arrival (n = 74) | Already there | 0 (0) |
| Within 5 min | 32.43(24) | |
| 5–10 min after | 45.95 (34) | |
| 11–15 min after | 10.81 (8) | |
| 16–20 min after | 2.70 (2) | |
| More than 20 min | 0 (0) | |
| EMS arrival unreported | 8.11 (6) | |
| Secondary outcome: Transport to a healthcare facility (n = 74) | Yes | 45.95 (34) |
| No | 52.70 (39) | |
| Hospital transport unreported | 1.35 (1) | |
| Overdose Environment(n = 74) | On the street | 58.11 (43) |
| In their home | 16.22 (12) | |
| In a vehicle | 6.76 (5) | |
| In a business | 8.11 (6) | |
| In someone else's home | 6.76 (5) | |
| In an abandoned building | 1.35 (1) | |
| Somewhere else | 2.70 (2) | |
| Volunteer stayed with the victim until regained consciousness (n = 74) | Yes | 89.19 (66) |
| No | 10.81 (8) |
2.9. Role of the funding source
Funding for this study was received from the National Institutes of Health (NIH) through the National Institute on Drug Abuse (NIDA). NIH and NIDA had no role in the study design, collection, analysis or interpretation of the data, nor in the writing of this report. All authors had full access to all data collected and used in this study. The corresponding author had the ultimate responsibility for the decision to submit the study for publication.
3. Results
3.1. Participant characteristics
The 112 participants were almost equally divided between people who use opioids (PWUO) (57) and community members (55). Table 1 presents baseline characteristics, opioid use and overdose history. Participant median number of days in the study was 237⸱5; (IQR:139⸱75–316⸱00; minimum: 15, maximum:366).
3.2. Overdose incidents
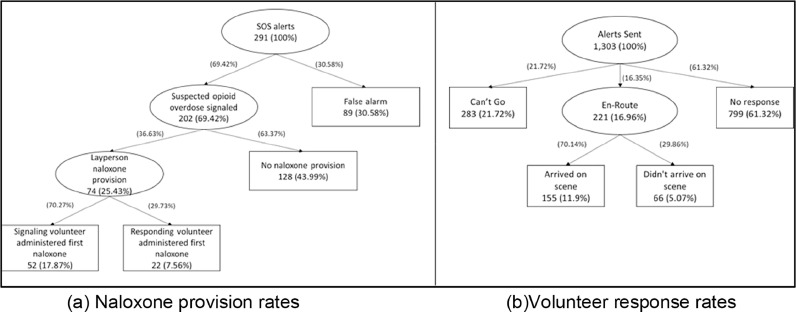
Participants signaled 291 suspected opioid overdose alerts during the 366 days of the study trial period (March 1, 2019 to February 29, 2020). 89 (30⸱58%) signaled events were determined to be false alarms, i.e., canceled by the signaler within 2 min of the alert being sent or the signaler entering an app chat message to the effect that this was a “false alarm”. Every signaled event initiated a phone call to EMS, irrespective of the alert being true or false, enabling EMS to execute their follow up protocol regardless of layperson responder engagement. In 74 (36⸱63%) of the remaining 202 cases, at least one dose of naloxone was administered by a layperson participating in the study. In the remaining 128 (63⸱37%) cases 9-1-1 was called but no naloxone administration or followup by laypersons was reported by incident survey respondents. The 291 alerts were signaled by a subset of 48⸱21% (54/112) of study participants. The number of alerts per signaler ranged from 1 to 52, the median (IQR) was 2 (1 to 4). 290 incident surveys were sent and 243 (83⸱79%) valid responses were received. Fig. 2 illustrates suspected opioid overdose case flow. Fig. 3 shows geographic distribution of naloxone-provision cases.
Fig. 2.
(a) Naloxone provision rates (b) Volunteer response rates.
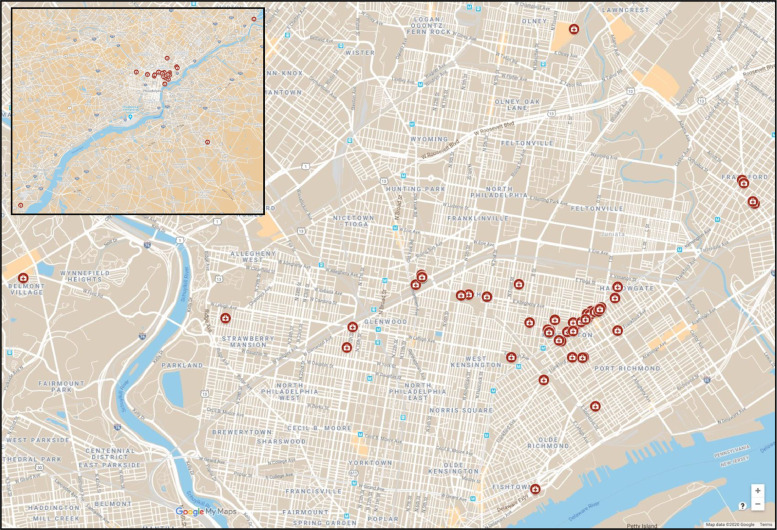
Fig. 3.
Map of Study Area Indicating Overdose Alert Locations. Signaled opioid overdose cases with naloxone-provision (n = 74), March 2019-February 2020. Inset: geographic outliers beyond core study area.
3.3. Outcomes
Across 74 naloxone-provision cases, 117 doses of nasal naloxone were administered by UnityPhilly volunteers, the median (IQR) of 1 dose (4 mg) per reversal was 1 (1 to 2). The first dose of naloxone was provided by a nearby volunteer responding to the alert in 29⸱73% (22/74) of cases and by the signaling volunteer in 70⸱27% (52/74) of cases. A successful reversal was reported in 95⸱95% (71/74) of cases. One on-scene death was reported (1⸱35%) and two intervention outcomes were unreported (2⸱70%). In just over half the cases the patient was reported recovered with no transport to a healthcare facility (52⸱70%). Table 2 summarizes outcomes.
3.4. First responder arrival
EMS arrival relative to the volunteer was reported in 68 naloxone-provision cases (in 6 cases EMS arrival was unreported) and measured in 5-min blocks ranging from ‘EMS already there’ to ‘more than 20 min after’. Volunteers reported EMS arrival: within 5 min 32⸱43% (24/74); 5–10 min after 45⸱95% (34/74); 11–15 min after 10⸱81% (8/74); 16–20 min after 2⸱70% (2/74). No volunteer reported ‘EMS already there’ or ‘more than 20 min after’. Volunteers reported staying with the overdose victim until they regained consciousness or EMS arrival in 89⸱19% (66/74) of cases.
3.5. Overdose environment
Volunteers reported observing the suspected overdose event on the street 58⸱11% (43/74), in their home 16⸱22% (12/74), in a vehicle 6⸱76% (5/74), in a business 8⸱11% (6/74), in someone else's home 6⸱76% (5/74), in an abandoned building 1⸱35% (1/74), and somewhere else 2⸱70% (2/74).
3.6. Volunteer response rates
A total of 1303 alert notifications were sent to volunteers during the study (Fig. 2b). Alerts were sent to available volunteers in 86⸱25% of suspected overdose cases (251/291). Non-notification was due to lack of signaler smartphone GPS/location data in 37⸱5% (15/40) of non-notification cases and due to no responders being within a 15 min ETA in 62⸱5% (25/40) of non-notification cases.
Of those contacted with an alert, 21⸱72% (283/1303) replied that they “Can't go”, 16⸱96% (221/1303) responded by indicating ‘En-route’, and 61⸱32% (799/1303) alerts were unanswered. Overall response rate based on alerts sent was 11⸱9% (155/1303). Of those who responded, 70⸱14% (155/221) arrived on scene. Of those who arrived on scene, 16⸱77% (26/155) provided naloxone. In 47⸱30% (35/74) of naloxone-provision cases a second volunteer arrived on scene, and in 18⸱92% (14/74) cases a third volunteer arrived.
Of 112 participants, 78 (69.64%) were sent at least one alert. In this group, 34 of 78 people or 43⸱59% confirmed they were en-route at least once. The number of “En-route” responses per person ranged from 1 to 29, the median (IQR) was 3⸱.5 (1 to 8⸱5). Additionally, 29/78 or 37⸱18% participants (of whom 27 have ever provided the “En-route” response) arrived at an overdose emergency scene at least once. In this subset, the onsite arrivals ranged from 1 to 20 with the median (IQR) of 3 (1 to 8).
4. Discussion
This observational cohort study assessed feasibility of laypersons signaling and responding to suspected opioid overdose emergencies when equipped with a dedicated smartphone app and naloxone. During the 52 week study, naloxone was administered at 74 overdose events (1⸱42 times per week on average), and was done more than 5 min in advance of EMS arrival in 59⸱46% of cases. Without timely reversal, opioid overdose causes respiratory depression that may deteriorate into apnea, leading to anoxic injury. Models have suggested that each minute of cerebral ischemia is associated with the loss of millions of neurons, billions of synapses, and miles of myelinated fibers [32]. In the minutes immediately following opioid overdose, 'time is brain.' Systematic reviews have demonstrated the ability of laypersons to effectively administer naloxone and shown the need for increasing access to naloxone in the community [28, 33].
Key elements for opioid overdose response as determined by the American Heart Association include: seeking help from emergency services, performing rescue breathing, administering naloxone, and staying with the victim until help arrives or the victim recovers [29]. Help seeking by community responders trained in overdose prevention and naloxone administration has been shown to be low, and in fact a pre-study assessment of intervention design found that respondents prefer not to communicate with EMS [25]. Lim et al. [34] who studied a decade (2007–2017) of 10,256 overdose events attended to by overdose education and naloxone distribution (OEND) program volunteers, found the percentage of overdoses where help seeking occurred reached a maximum of 50%, and concluded a need for targeted interventions that promote help seeking. Our study participants, whose app initiated calls to EMS in addition to alerting other volunteers, reported staying with the victim until EMS arrival in 89⸱19% of cases.
The UnityPhilly Emergency Response Community supported a two-tiered intervention approach. Every volunteer was able to act as a signaler, pressing the SOS button when encountering a suspected opioid overdose victim, but also able to act as a responder when receiving an overdose alert sent by another volunteer. Since adherence rates of carrying nasal naloxone are low [34], this approach enables a network of volunteers to leverage availability of naloxone from ERC members, when they encounter an overdose victim and have no naloxone on their person. In almost 30% of cases (22/74) the first dose of naloxone was provided by a nearby volunteer responding to the alert. However, even when the signaler has naloxone to initiate reversal, the second tier can arrive with additional naloxone doses, which are often needed [5]. Volunteer responders provided additional naloxone doses in 5⸱41% (4/74) of naloxone-provision cases.
It is important to differentiate between the rate of response to “alerts sent” (Fig. 2(b) and the rate of “layperson naloxone provision” (Fig. 2(a)). The former is measured as a percentage of response to all alerts that were sent by the system to nearby participants. The number of alerts sent and the radius (ETA) chosen are parameterized and can be studied to improve the response rate. For example, tightening the ETA radius will result in fewer alerts being sent, but may not reduce the actual response since most ‘no go’ decisions are due to distance/time as respondents feel someone else will get there faster. As reported, this was only 11⸱9% which can be considered low. We measured this to be able to compare with OHCA studies that seek to determine how many potential responders are needed to cover a given population and geography. However, the latter rate of “layperson naloxone provision” is measured as a percentage of incidents in which laypersons provided naloxone at a suspected opioid overdose which, as reported, was 25⸱43% - a rate with significant potential impact (rising to 36⸱63% if we exclude false alarms). This is a measure of incidents that actually received confirmed delivery of naloxone, irrespective of how many nearby laypersons had to be notified.
Consider that if there were 10 signaled SOS incidents, 100 people in the vicinity were notified (10 per incident), and single responders arrived with naloxone to 5 distinct incidents, the rate of response to “alerts sent” is only 5% (5/100), but the rate of “layperson naloxone provision” reaches 50% (5/10). One of the promising aspects of this type of layperson intervention is that a small increase in community engagement can result in a large increase in on-scene assistance, which we believe can be demonstrated with a larger-scale study.
The Kensington community environment is characterized by an open-air drug market [35, 36] and a significant proportion of study participants were homeless. While most incidents were reported as occurring on the street (58⸱11%), we observed a significant number of in-home overdose signaling (22⸱98%) indicating the relevance of this approach in providing at-home support for caregivers and family members of opioid users. Allowing entry of layperson responders into homes or businesses in this study was at the discretion of the person who signaled the SOS. Layperson responders in Pennsylvania are afforded certain legal protections through the ‘Good Samaritan’ provision of Act 139 [37].
There are no studies of app-based automatic dispatch of naloxone-carrying volunteers for opioid overdose with which to compare. While cognizant of the clinical and treatment distinctions between OHCA and opioid overdose, in the absence of existing relevant opioid overdose response studies, comparison with OHCA response studies offer some indication of the unrealized potential for layperson opioid overdose reversal. Our observed naloxone intervention rate (36⸱6%) exceeds both CPR and AED intervention rates reported for OHCA by Berglund et al. [18] The observed volunteer response rates of this study with 17% en-route to an incident and 70% of those dispatched arriving on scene, compares favorably with Brooks et al. [17] studies of volunteer response for OHCA using the PulsePoint app with rates of 23% and 70% respectively. Study volunteers who responded rarely or not at all to an overdose alert indicated the main factor for non-response was incident distance and a consideration that EMS or someone else will arrive faster. Subjects indicated that tightening the ETA radius would be effective in generating greater response rates. This should be examined in future studies. A future city-wide study is now being planned to test the scalability of the intervention. Aspects to be studied in addition to scalability include who might oversee the system if scalable, such as public health authorities, a city agency, or a non-profit. This study has examined an unmediated Emergency Response Community model in which layperson dispatch is concurrent with, yet independent from, EMS dispatch. Future research should also consider an integrated model in which EMS mediates layperson dispatch and directly supports the responses of community laypersons [38].
Our study has a few limitations. First, it was a single-center observational trial to assess feasibility, and not powered to analyze efficacy or survival. Second, our survey data may be affected by recall bias. This includes baseline measures of prior drug use, prior overdose and overdose reversal experience; incident survey reporting of naloxone administration and overdose incident details; and EMS arrival time estimates. All incident-related data are based on the recollection and time sense of layperson responders who were under the psychological stress of attending an opioid overdose incident, and could not be objectively measured. Third, only 112 participants were recruited for an area covering four zip codes and a local population of 137,097 [39] such that response rates and relative arrival times may not be representative of response characteristics of a widely disseminated app with a different density of population and participants. Finally, the Kensington neighborhood of Philadelphia, where this study took place, is characterized by a highly active street-based drug scene, and relatively high levels of naloxone availability. Generalizability of results may depend on similar neighborhood characteristics.
In conclusion, the results of our study show that equipping laypersons with naloxone and an emergency response community app to signal suspected opioid overdose and alert other nearby volunteers to provide naloxone, can result in naloxone administration prior to EMS arrival and overdose reversal, potentially reducing mortality in opioid overdose. Our findings support further study of smartphone-based naloxone intervention to strengthen the chain of survival starting at the community level.
Funding
Funding provided by the National Institute on Drug Abuse (5R34DA044758).
Contributors
The study was designed by SL, DGS, AR, IY and GM. Data were obtained by JA, SL, AR, and DGS. All authors were involved in data analysis and the interpretation of results. All authors contributed sections of the manuscript which DGS combined to produce the final manuscript. All authors approved the final version.
Declaration of Interests
All authors report grants from NIH/NIDA during the course of this study.
Data sharing statement
Data are available upon reasonable request. Available data includes deidentified participant data, and location-less incident alert and response data. Data requests should be sent to info@unityphilly.org. The study protocol is registered and available online at https://clinicaltrials.gov/ct2/show/NCT03305497.
Acknowledgements
The authors thank our development partner team at Verint/Nowforce for helping to customize and support the UnityPhilly app. We thank our community partners, including Prevention Point Philadelphia, Esperanza, and Angels in Motion, as well as collaborators in the city of Philadelphia, including the Police Department and Fire/Emergency Medical Services.
Footnotes
Supplementary material associated with this article can be found, in the online version at doi:10.1016/j.eclinm.2020.100474.
Appendix. Supplementary materials
References
- 1.Murthy V.H. Ending the opioid epidemic - a call to action. N Engl J Med. 2016;375:2413–2415. doi: 10.1056/NEJMp1612578. [DOI] [PubMed] [Google Scholar]
- 2.Blanco C., Volkow N.D. Management of opioid use disorder in the USA: present status and future directions. Lancet. 2019;393:1760–1772. doi: 10.1016/S0140-6736(18)33078-2. [DOI] [PubMed] [Google Scholar]
- 3.Drug Overdose Deaths | Drug Overdose | CDC Injury Center. 2020; Published online March 19. https://www.cdc.gov/drugoverdose/data/statedeaths.html. (accessed March 21, 2020).
- 4.Whelan A.Philly's overdose deaths rose again in 2019, especially in black and Latino communities2020; published online May 13. https://www.inquirer.com/health/opioid-addiction/philadelphia-overdose-deaths-2019-rise-20200513.html. (accessed June 14, 2020).
- 5.Chou R., Korthuis P.T., McCarty D. Management of suspected opioid overdose with naloxone in out-of-hospital settings: a systematic review. Ann Intern Med. 2017;167:867–875. doi: 10.7326/M17-2224. [DOI] [PubMed] [Google Scholar]
- 6.Csete J., Kamarulzaman A., Kazatchkine M. Public health and international drug policy. Lancet. 2016;387:1427–1480. doi: 10.1016/S0140-6736(16)00619-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lankenau S.E., Wagner K.D., Silva K. Injection drug users trained by overdose prevention programs: responses to witnessed overdoses. J Community Health. 2012;38:133–141. doi: 10.1007/s10900-012-9591-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American Medical Association. National roadmap on state-level efforts to end the opioid epidemic. 2019. https://www.end-opioid-epidemic.org/wp-content/uploads/2019/09/AMA-Manatt-National-Roadmap-September-2019-FINAL.pdf. (accessed April 12, 2020).
- 9.World Health Organization. Community management of opioid overdose. 2015. https://www.ncbi.nlm.nih.gov/pubmed/25577941. (accessed March 21, 2020).
- 10.Walley A.Y., Xuan Z., Hackman H.H. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ. 2013;346:f174. doi: 10.1136/bmj.f174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gov.Wolf announces naloxone standing order. Gov. Wolf announces naloxone standing order. https://www.governor.pa.gov/naloxone-standing-order/. (accessed Dec 2, 2015).
- 12.The Lancet Out-of-hospital cardiac arrest: a unique medical emergency. Lancet. 2018;391:911. doi: 10.1016/S0140-6736(18)30552-X. [DOI] [PubMed] [Google Scholar]
- 13.Hazinski M.F., Nolan J.P., Aickin R. Part 1: executive summary: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2015;132:S2–39. doi: 10.1161/CIR.0000000000000270. [DOI] [PubMed] [Google Scholar]
- 14.Weisfeldt M.L., Sitlani C.M., Ornato J.P. Survival after application of automatic external defibrillators before arrival of the emergency medical system: evaluation in the resuscitation outcomes consortium population of 21 million. J Am Coll Cardiol. 2010;55:1713–1720. doi: 10.1016/j.jacc.2009.11.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ong M.E.H., Perkins G.D., Cariou A. Out-of-hospital cardiac arrest: prehospital management. Lancet. 2018;391:980–988. doi: 10.1016/S0140-6736(18)30316-7. [DOI] [PubMed] [Google Scholar]
- 16.Ringh M., Rosenqvist M., Hollenberg J. Mobile-phone dispatch of laypersons for CPR in out-of-hospital cardiac arrest. N Engl J Med. 2015;372:2316–2325. doi: 10.1056/NEJMoa1406038. [DOI] [PubMed] [Google Scholar]
- 17.Brooks S.C., Simmons G., Worthington H., Bobrow B.J., Morrison L.J. The PulsePoint respond mobile device application to crowdsource basic life support for patients with out-of-hospital cardiac arrest: challenges for optimal implementation. Resuscitation. 2016;98:20–26. doi: 10.1016/j.resuscitation.2015.09.392. [DOI] [PubMed] [Google Scholar]
- 18.Berglund E., Claesson A., Nordberg P. A smartphone application for dispatch of lay responders to out-of-hospital cardiac arrests. Resuscitation. 2018;126:160–165. doi: 10.1016/j.resuscitation.2018.01.039. [DOI] [PubMed] [Google Scholar]
- 19.Hatakeyama T., Nishiyama C., Shimamoto T. A smartphone application to reduce the time to automated external defibrillator delivery after a witnessed out-of-hospital cardiac arrest: a randomized simulation-based study. Simul Healthc. 2018;13:387–393. doi: 10.1097/SIH.0000000000000305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.von Elm E., Altman D.G., Egger M. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 21.Schmidt W.-.P. Randomised and non-randomised studies to estimate the effect of community-level public health interventions: definitions and methodological considerations. Emerg Themes Epidemiol. 2017;14:9. doi: 10.1186/s12982-017-0063-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eichel L, Pharis M, Poll shows impact of opioid crisis on philadelphians and their neighborhoods. https://www.pewtrusts.org/en/research-and-analysis/articles/2019/08/06/poll-shows-impact-of-opioid-crisis-on-philadelphians-and-their-neighborhoods. (accessed March 21, 2020).
- 23.Ruiz M.S., OʼRourke A., Allen S.T. Using interrupted time series analysis to measure the impact of legalized syringe exchange on HIV diagnoses in Baltimore and Philadelphia. J Acquir Immune Defic Syndr. 2019;82(Suppl 2):S148–S154. doi: 10.1097/QAI.0000000000002176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schwartz D.G., Bellou A., Garcia-Castrillo L., Muraro A., Papadopoulos N. Exploring mHealth participation for emergency response communities. Australas J Inf Syst. 2017;21 doi: 10.3127/ajis.v21i0.1378. [DOI] [Google Scholar]
- 25.Marcu G., Aizen R., Roth A.M., Lankenau S., Schwartz D.G. Acceptability of smartphone applications for facilitating layperson naloxone administration during opioid overdoses. Jamia Open. 2019 doi: 10.1093/jamiaopen/ooz068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mechem C.C., Yates C.A., Rush M.S., Alleyne A., Singleton H.J., Boyle T.L. Deployment of alternative response units in a high-volume, urban EMS system. Prehosp Emerg Care. 2020;24:378–384. doi: 10.1080/10903127.2019.1657212. [DOI] [PubMed] [Google Scholar]
- 27.Sporer K.A., Wilson K.G. How well do emergency medical dispatch codes predict prehospital medication administration in a diverse urban community? J Emerg Med. 2013;44 doi: 10.1016/j.jemermed.2012.02.086. 413–22.e3. [DOI] [PubMed] [Google Scholar]
- 28.Clark A.K., Wilder C.M., Winstanley E.L. A Systematic review of community opioid overdose prevention and naloxone distribution programs. J Addict Med. 2014;8:153–163. doi: 10.1097/ADM.0000000000000034. [DOI] [PubMed] [Google Scholar]
- 29.Neumar R.W., Shuster M., Callaway C.W. Part 1: executive summary: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:S315–S367. doi: 10.1161/CIR.0000000000000252. [DOI] [PubMed] [Google Scholar]
- 30.Billingham S.A.M., Whitehead A.L., Julious S.A. An audit of sample sizes for pilot and feasibility trials being undertaken in the United Kingdom registered in the United Kingdom clinical research network database. BMC Med Res Methodol. 2013;13:104. doi: 10.1186/1471-2288-13-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arain M., Campbell M.J., Cooper C.L., Lancaster G.A. What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Med Res Methodol. 2010;10:67. doi: 10.1186/1471-2288-10-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Saver J.L. Time is brain–quantified. Stroke. 2006;37:263–266. doi: 10.1161/01.STR.0000196957.55928.ab. [DOI] [PubMed] [Google Scholar]
- 33.Larney S., Tran L.T., Leung J. All-cause and cause-specific mortality among people using extramedical opioids: a systematic review and meta-analysis. JAMA Psychiatry. 2019 doi: 10.1001/jamapsychiatry.2019.4170. published online Dec 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lim J.K., Forman L.S., Ruiz S. Factors associated with help seeking by community responders trained in overdose prevention and naloxone administration in Massachusetts. Drug Alcohol Depend. 2019;204 doi: 10.1016/j.drugalcdep.2019.06.033. [DOI] [PubMed] [Google Scholar]
- 35.Bowles J.M., Lankenau S.E. I gotta go with modern technology, so I'm Gonna give'em the narcan’: the diffusion of innovations and an opioid overdose prevention program. Qual Health Res. 2019;29:345–356. doi: 10.1177/1049732318800289. [DOI] [PubMed] [Google Scholar]
- 36.Ataiants J., Roth A.M., Mazzella S., Lankenau S.E. Circumstances of overdose among street-involved, opioid-injecting women: drug, set, and setting. Int J Drug Policy. 2020;78 doi: 10.1016/j.drugpo.2020.102691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Get Naloxone. Pennsylvania department of drug and alcohol programs. www.ddap.pa.gov/overdose/pages/naloxone_reversal.aspx. (accessed June 7, 2020).
- 38.Khalemsky M., Schwartz D.G., Herbst R., Jaffe E. Motivation of emergency medical services volunteers: a study of organized Good Samaritans. Isr J Health Policy Res. 2020;9:11. doi: 10.1186/s13584-020-00370-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.U.S. Census Bureau. American community survey 5-year population estimates. 2017. https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=CF. (accessed March 26, 2020).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.