Abstract
Introduction
Small bowel lipomas are rarely encountered benign adipose growths found within the small intestine wall or mesentery. Limited up-to-date evidence exists regarding such lipomas. We aim to aid clinical decision-making and improve patient outcomes through this comprehensive review.
Methodology
The terms ‘small bowel,’ ‘small intestine,’ ‘jejunum’ and ‘ileum’ were combined with ‘lipoma.’ EMBASE, Medline and PubMed database searches were performed. All papers published in English from 01/01/2000-31/12/2019 were included. Simple statistical analysis (t-test, Anova) was performed.
Results
142 papers yielded 147 cases (adults = 138, pediatric = 9). Male = 88, female = 59 (average age = 49.9 years). Presenting symptoms: abdominal pain = 68.7%; nausea/vomiting = 35.3%, hematochezia/GI bleeding = 33.3%; anaemia = 10.9%; abdominal distension = 12.2%; constipation = 8.9%; weight loss = 7.5%. Mean preceding symptom length = 58.1 days (symptoms >1 year excluded (n = 9)). Diagnostic imaging utilised: abdominal X-Ray = 33.3%; endoscopy = 46.3%; CT = 78.2%; ultrasound = 23.8%. 124/137 (90.5%) required definitive surgical management (laparotomy = 89, laparoscopcic = 35). 9 patients were successfully managed endoscopically. Lipoma location: ileum = 59.9%, jejunum = 32%, mesentery = 4.8%. Maximal recorded lipoma size ranged 1.2–22 cm.
Mean maximum lipoma diameter and management strategy comparison: laparotomy 5.6 cm, laparoscopic = 4.4 cm, endoscopic = 3.7 cm, conservative = 4.5 cm. One-way Anova test, p value = 0.21. Average length of stay (LOS) was 7.4 days (range = 2–30). T-test p value = 0.13 when comparing management modalities and LOS. 4 complications, 0 mortality.
Conclusions
Important previously undocumented points are illustrated; a clearer symptom profile, diagnostic investigations utilised, size and site of lipomas, types and effectiveness of management modalities, associated morbidity and mortality. Open surgery remains the primary management. No statistically significant difference in LOS and lipoma size is demonstrated between management strategies. Endoscopic and laparoscopic techniques may reduce utilising invasive surgery in the future as skillset and availability improve.
Keywords: Lipoma, Small bowel, Small intestine, Jejunum, Ileum
Highlights
-
•
Up to date overview of symptomatic lipomas of the jejunum and ileum which no other paper has previously covered.
-
•
Highlights associated symptom profile, investigations, site and size of symptomatic lipomas, morbidity and mortality.
-
•
Evaluates the effectiveness of management strategies.
-
•
Offers a practical summary that may help guide other clinicians faced with similar presentations in the future.
1. Introduction
Little up to date evidence exists regarding lipomas of the small bowel other than anecdotal case reports. Much of the data quoted by these papers can be traced back to epidemiological studies carried out over 20 years ago. More recent studies relate to reviews of duodenal [1] and colonic [2] lipomas. However, no current systematic review exists pertaining to symptomatic lipomas of the ileum and jejunum, which for the purposes of this paper we shall refer to as small bowel lipomas.
Small bowel lipomas are rarely encountered benign adipose growths found within the wall or mesentery of the small intestine. Incidence of intestinal lipomas ranges from 0.035% to 4.4% [3]. Lipomas can arise throughout the gastrointestinal tract with the small bowel accounting for 25% [4]. These benign tumors arise from the sub mucosa of the small intestine in 90% of cases [5]. Small bowel lipomas are most commonly found incidentally with the majority of patients being asymptomatic.
Unlike more proximal and distal lesions that can be easily accessed and investigated with endoscopy, small bowel tumors represent a difficult diagnostic entity. The clinical picture is often not clear, with vague symptoms commonly reported.
This paper comprehensively reviews symptomatic small bowel lipomas, including demographics, clinical presentation, diagnostic investigations, management, pathology, length of stay and mortality. We hope clinicians managing such patients can draw on this paper to aid clinical decision-making and improve patient outcomes.
2. Methodology
The search terms ‘small bowel,’ ‘small intestine,’ ‘jejunum’ and ‘ileum’ were combined with ‘lipoma.’ Multiple database searches of EMBASE, Medline and PubMed were conducted. All papers published from January 01, 2000 to December 31, 2019 in English were included. Hand searches were also performed using Google Scholar with the same search terms. The first 50 hand search results were included for screening. The paper was registered with the International Prospective Register of Systematic Reviews, (PROSPERO) CRD42020172916.
Simple statistical analysis was preformed where appropriate. T-test was undertaken to compare length of stay between open and laparoscopic surgery patients. One-way Anova test was used for comparison of lipoma size between patients undergoing different management modalities (open surgery, laparoscopic surgery, endoscopic management).
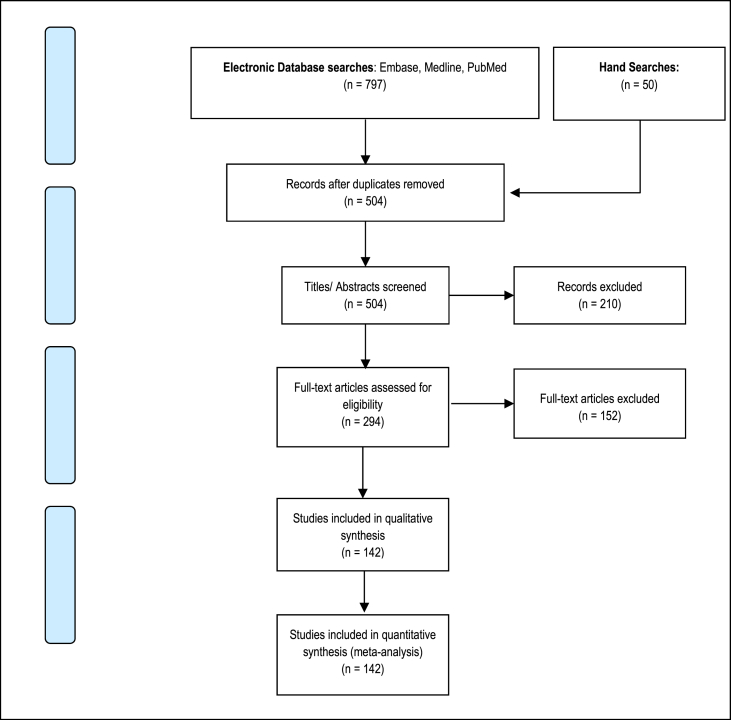
Two reviewers independently analysed the searches, abstracts and papers identified to reduce bias. The PRISMA [6] diagram (Fig. 1) demonstrates our search strategy. The selected papers were analysed for multiple outcomes relating to sex, age, presenting complaint, diagnostic modalities, management strategies, complications, mortality and length of stay. The AMSTAR 2 and PRISMA guidelines for assessing methodological quality in systematic reviews were followed [7].
Fig. 1.
Prisma diagram of database searches.
Of the 797 papers derived from database and hand searches, 504 titles/abstracts remained once duplicates had been removed. These were screened with a further 210 papers excluded because they were not relevant to the paper. Two independent reviewers then reviewed 294 full-text articles. A further 152 papers were excluded; 103/152 were either abstract only (full text not accessible or published), in a different language or not case specific; 18/152 related to duodenal lipomas; 5/152 were incidental lipomas in asymptomatic patients; the remaining 26/152 were unable to be accessed. Thus a total of 142 were included yielding a total of 147 cases.
All papers related to individual cases or case series. Given the observational nature of such reports and that no randomised control trials were included, reporter and publication bias was deemed to be low. No funding or other financial support was received in relation to this study.
3. Results
138 adults and 9 pediatric (age 0–16) cases were recorded. Average age was 49.9 (2–87) years. Male number (n) = 88, female n = 59, male:female ratio was 1.49:1. Average age was male = 49yrs, female = 51.4yrs (Table 1).
Table 1.
Results.
| Author | Year | Title | Journal | Age | Sex | Symptoms | Length of symptoms | Site of lipoma | Largest diameter (cm) | Emergency (Y/N) | Definitive management | Length of stay (days) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Abbasakoor et al. | 2010 | Midgut pain due to an intussuscepting terminal ileal lipoma: A case report | Journal of Medical Case Reports | 52 | F | Abdominal pain, constipation | 3 months | Ileum | 4 | N | Laparoscopic | 4 |
| Abdelmohsen et al. | 2019 | An ileo-ileal intussusception secondary to polypoid lipoma in a child, a case report and review of the literature | International Journal of Surgery Case Reports | 4 | M | Abdominal pain, vomiting | 24 h | Ileum | 4 | Y | Laparotomy | 7 |
| Ahmed et al. | 2004 | Acute abdomen from a Meckel lipoma | Journal of the Royal Society of Medicine | 28 | M | Abdominal pain, GI bleed, vomiting, diarrhoea | 24 h | Jejunum | 3 | Y | Laparotomy | Not stated |
| Ahmed et al. | 2018 | Submucosal Lipomas Causing Intussusception and Small Bowel Obstruction: A Case Report | Cureus Journal of Medical Science | 67 | M | Abdominal pain, nausea, vomiting, constipation | 5 days | Ileum | Not stated | Y | Laparoscopic | Not stated |
| Akagi et al. | 2008 | Adult intussusception caused by an intestinal lipoma: Report of a case | Journal of Nippon Medical School | 36 | M | Abdominal pain, nausea, vomiting, abdominal distension | 24 h | Ileum | 4 | Y | Laparotomy | 15 |
| Akimaru et al. | 2006 | Resection of over 290 polyps during emergency surgery for four intussusceptions with Peutz-Jeghers syndrome: Report of a case | Surgery Today | 41 | M | Abdominal pain, nausea | 12 h | Ileum | 2 | Y | Laparotomy | Not stated |
| Ako et al. | 2010 | Laparoscopic resection of ileal lipoma diagnosed by multidetector-row computed tomography | Surgical Laparoscopy, Endoscopy and Percutaneous Techniques | 43 | F | Abdominal pain, nausea | 6 h | Ileum | 2.4 | Y | Laparoscopic | 9 |
| Al-Radaideh et al. | 2018 | Adult intussusception: A 14-year retrospective study of clinical assessment and computed tomography diagnosis | Belgian Acta Gastro-Enterologica Belgica | 43 | F | Abdominal pain | Not stated | Jejunum | 13 | Y | Not stated | Not stated |
| Alsayegh et al. | 2019 | Mesenteric lipoma presenting as small bowel volvulus | Journal of Pediatric Surgery Case Reports | 4 | F | Abdominal pain, vomiting | Not stated | Mesentery | 7.6 | Y | Laparotomy | Not stated |
| Asaumi et al. | 2014 | Pediatric ileoileal intussusception with a lipoma lead point: a case report | Gastroenterology Report (Oxford Academic) | 7 | M | Abdominal pain | 3 days | Ileum | Not stated | Y | Laparotomy | 8 |
| Atila et al. | 2007 | Symptomatic intestinal lipomas requiring surgical interventions secondary to ileal intussusception and colonic obstruction: Report of two cases | Turkish National Journal of Trauma and Emergency Surger | 47 | F | Abdominal pain, nausea | 2 days | Ileum | 5 | Y | Laparotomy | Not stated |
| Bakker et al. | 2009 | Nausea caused by a jejunal lipoma | Clinical Gastroenterology and Hepatology | 57 | F | Nausea, vomiting, weight loss | 2 years | Jejunum | 10 | N | Laparotomy | Not stated |
| Balmadrid et al. | 2014 | Chronic iron deficiency anemia caused by small-bowel lipoma | Gastrointestinal Endoscopy | 64 | M | Fatigue, anaemia | 1 year | Ileum | 1.9 | N | Laparoscopic | Not stated |
| Bilgin et al. | 2012 | Ileocecal Intussusception due to a Lipoma in an Adult | Case Reports in Surgery | 39 | F | Abdominal pain | 24 h | Ileum | 2.5 | N | Laparotomy | 7 |
| Bosman et al. | 2014 | Ileocaecal intussusception due to submucosal lipoma in a pregnant woman | British Medical Journal Case Reports | 30 | F | Abdominal pain, nausea, vomiting | 2 days | Ileum | 1.5 | Y | Laparotomy | 5 |
| Chehade et al. | 2015 | Large ileocecal submucosal lipoma presenting as hematochezia, a case report and review of literature | International Journal of Surgery Case Reports | 42 | F | Abdominal pain, GI bleeding | 2 months | Ileocaecal valve | 4.5 | Y | Laparotomy | Not stated |
| Cherian et al. | 2004 | Small bowel volvulus due to giant mesenteric lipoma | Pediatric Surgery International | 14 | F | Abdominal pain, vomiting | 8 h | Mesentery | 16 | Y | Laparotomy | Not stated |
| Chou et al. | 2008 | Obscure gastrointestinal bleeding caused by small bowel lipoma | Internal Medicine | 57 | M | GI bleed | 5 days | Ileum | 3 | Y | Laparotomy | Not stated |
| Cuciureanu et al. | 2019 | Ulcerated intussuscepted jejunal lipoma-uncommon cause of obscure gastrointestinal bleeding: A case report | World Journal of Clinical Cases | 63 | M | Abdominal pain, nausea, anaemia | Not stated | Jejunum | 6 | Y | Laparotomy | 14 |
| Devillers et al. | 2016 | An atypical acute small-bowel obstruction | Diagnostic and Interventional Imaging | 54 | F | Abdominal pain, vomiting | 24 h | Mesentery | Not stated | Y | Laparotomy | Not stated |
| Di Saverio et al. | 2010 | Concomitant intestinal obstruction: a misleading diagnostic pitfall | British Medical Journal Case Reports | 78 | F | Constipation | 2 months | Ileum | 3 | Y | Laparotomy | 9 |
| Duijff et al. | 2007 | Intussusception in adults: report of four cases and review of the literature | Case Reports in Gastroenterology | 42 | M | Abdominal pain | Several months | Ileocaecal valve | 3 | Y | Laparotomy | 7 |
| Dultz et al. | 2009 | Ileocecal valve lipoma with refractory hemorrhage | Journal of the Society of Laparoendoscopic Surgeons | 77 | M | GI bleed | 2 days | Ileocaecal valve | 3.5 | Y | Laparoscopic | 5 |
| Ertem et al. | 2010 | Application of laparoscopy in the management of obscure gastrointestinal bleeding | Surgical Laparoscopy, Endoscopy and Percutaneous Techniques | 47 | M | GI bleed | Not stated | Jejunum | Not stated | Y | Laparoscopic | 7 |
| Eyselbergs et al. | 2014 | Ileocolic intussusception due to lipomatosis of the ileum: A common complication of a rare clinical entity | Journal of the Belgian Society of Radiology | 56 | M | Abdominal pain, GI bleeding | Not stated | Ileum | 2 | Y | Laparotomy | Not stated |
| Feo et al. | 2019 | A rare case of ileo-ileal intussusception due to a bleeding lipomatous mass treated by laparoscopic ileal resection | Italian annals of Surgery | 69 | M | GI bleed | 1 h | Ileum | 3 | Y | Laparoscopic | 3 |
| Ferrara et al. | 2012 | Laparoscopic resection of small bowel lipoma causing obscure gastrointestinal bleeding | Updates in Surgery | 78 | F | GI bleed | 1 h | Jejunum | 3 | Y | Laparoscopic | Not stated |
| Gao et al. | 2014 | Ileo-colonic intussusception secondary to small-bowel lipomatosis: A case report | World Journal of Gastroenterology | 52 | F | Abdominal pain | 21 days | Ileum | 5 | Y | Laparotomy | 30 |
| Garcia Zamora et al. | 2014 | Intestinal intussusception due to a lipoma in Meckel's diverticulum | Spanish Surgery | 50 | M | Abdominal pain, vomiting | 1 year | Meckel's diverticulum | 5 | N | Laparotomy | Not stated |
| Hanafiah et al. | 2019 | Adult entero-enteric intussusception secondary to lipoma | Clinical Case Reports | 35 | M | Abdominal pain, vomiting | Not stated | Ileum | 2 | Y | Laparotomy | Not stated |
| Hasab Allah et al. | 2013 | Percutaneous ultrasound-guided bowel wall core biopsy: A nonconventional way of diagnosis of gastrointestinal lesions | Surgical Endoscopy | 61 | F | Not stated | Not stated | Jejunum | 2 | Y | Not stated | Not stated |
| Honda et al. | 2012 | Enteroscopic and radiologic diagnoses, treatment, and prognoses of small-bowel tumors | Gastrointestinal Endoscopy | 61 | F | GI bleed | Not stated | Jejunum | Not stated | Y | Not stated | Not stated |
| 61 | M | GI bleed | Not stated | Jejunum | Not stated | Y | Endoscopic | Not stated | ||||
| 61 | M | GI bleed | Not stated | Jejunum | Not stated | Y | Endoscopic | Not stated | ||||
| Hou et al. | 2012 | Laparoscopic management of small-bowel intussusception in a 64-year-old female with ileal lipomas | World Journal of Gastrointestinal Surgery | 64 | F | Abdominal pain | 2 h | Ileum | Not stated | Y | Laparoscopic | 7 |
| Javia et al. | 2016 | Endoscopic resection of small-bowel submucosal nodule | Endoscopy | 67 | F | Evaluation after positive faecal immunochemical testing | Not stated | Ileum | 2 | N | Endoscopic | Not stated |
| Jayasundara et al. | 2016 | A case of gastroduodenal lipomatosis | Annals of the Royal College of Surgeons of England | 43 | F | Constipation, vomiting | 5 days | Jejunum | Not stated | Y | Laparotomy | 5 |
| Jiang et al. | 2015 | Submucosal Lipoma: a Rare Cause of Recurrent Intestinal Obstruction and Intestinal Intussusception | Journal of Gastrointestinal Surgery | 50 | M | Abdominal pain | 1 month | Ileum | 4 | N | Laparotomy | 8 |
| Jung et al. | 2007 | Intestinal chondrolipoma: uncommon cause of bowel obstruction | Journal of Pediatric Surgery | 11 | M | Abdominal pain, abdominal distension, vomiting. | 4 h | Jejunum | 7.5 | Y | Laparotomy | 7 |
| Kaczynski et al. | 2012 | Giant lipoma of the small bowel associated with perforated ileal diverticulum | British Medical Journal Case Reports | 38 | M | Abdominal pain, weight loss, nausea, vomiting, fever | 72 h | Ileum | 9 | Y | Laparotomy | 4 |
| Kakiuchi et al. | 2017 | A small intestine volvulus caused by strangulation of a mesenteric lipoma: a case report | Journal of Medical Case Reports | 67 | M | Abdominal pain, nausea, vomiting | Not stated | Ileum | 10 | Y | Laparoscopic | 6 |
| Kamaoui et al. | 2007 | Jejunojejunal intussusception secondary to a lipoma | French Radiology Sheets | 55 | M | Abdominal pain, anaemia, GI bleed | 3 months | Jejunum | 4 | Y | Laparotomy | 7 |
| Kane et al. | 2019 | Gastrointestinal hemorrhage caused by small intestinal benign tumors: 2 cases report | Pan African Medical Journal | 72 | M | Fatigue, GI bleed, anaemia | Not stated | Jejunum | Not stated | Y | Not stated | Not stated |
| 2019 | Gastrointestinal hemorrhage caused by small intestinal benign tumors: 2 cases report | Pan African Medical Journal | 68 | M | GI bleed, anaemia | Not stated | Ileum | Not stated | Y | Endoscopic | Not stated | |
| Kang et al. | 2014 | Resolution of intussusception after spontaneous expulsion of an ileal lipoma per rectum: A case report and literature review | World Journal of Surgical Oncology | 65 | F | Abdominal pain, nausea | 5 days | Not stated | 7 | Y | Conservative | Not stated |
| Karadeniz Cakmak et al. | 2007 | Lipoma within inverted Meckel's diverticulum as a cause of recurrent partial intestinal obstruction and hemorrhage: a case report and review of literature | World Journal of Gastroenterology | 47 | M | Abdominal pain, constipation, fatigue | 4 months | Meckel's diverticulum | 4 | Y | Laparotomy | 5 |
| Karthikeyan et al. | 2012 | Jejuno-jejunal intussusception secondary to small-bowel lipomatosis: a case report | South African Journal of Surgery | 60 | M | Abdominal pain, vomiting, abdominal distension | 3 days | Jejunum | Not stated | Y | Laparotomy | 10 |
| Katergiannakis et al. | 2004 | Jejunojenulal intussusception due to an intraluminal lipoma | Annals of Gastroenterology | 55 | M | Abdominal pain, GI bleeding, anaemia | 3 months | Jejunum | 4 | Y | Laparotomy | 7 |
| Kenkare et al. | 2010 | Macrodactylia fibrolipomatosis presenting as a small bowel obstruction | Southern Medical Journal | 69 | M | Abdominal pain, abdominal distension, vomiting | Not stated | Jejunum | 3.7 | Y | Laparotomy | Not stated |
| Kida et al. | 2017 | A unique case of massive gastrointestinal bleeding | SAGE Open Medical Case Reports | 67 | M | GI bleed, anaemia | Not stated | Jejunum | 4 | Y | Laparotomy | Not stated |
| Kim et al. | 2013 | A case of jejunal lipomatosis diagnosed with double-balloon enteroscopy | Journal of Gastroenterology and Hepatology Research | 50 | M | Abdominal pain | 3 months | Jejunum | Not stated | Y | Conservative | Not stated |
| Kim et al. | 2017 | Spontaneous peeled ileal giant lipoma caused by lower gastrointestinal bleeding A case report | Medicine (United States) | 82 | F | Abdominal pain, GI bleed | 7 days | Ileum | 3 | Y | Laparoscopic | 8 |
| Kiziltas et al. | 2009 | A remarkable intestinal lipoma case | Turkish Journal of Trauma and Emergency Surgery | 37 | F | Abdominal pain, nausea, vomiting, obstruction, anaemia | Not stated | Jejunum | 4 | Y | Laparotomy | Not stated |
| Komagata et al. | 2007 | Extensive lipomatosis of the small bowel and mesentery: CT and MRI findings | Journal of Medical Imaging and Radiation Oncology | 49 | F | Abdominal pain, abdominal distension | Long term | Ileum | 2 | Y | Conservative | Not stated |
| Konik et al. | 2018 | Complete small bowel obstruction without intussusception due to a submucosal lipoma | Journal of Surgical Case Reports | 53 | F | Abdominal pain, abdominal distension, nausea, vomiting | 1 day | Jejunum | 1.5 | Y | Laparotomy | 18 |
| Kraniotis et al. | 2016 | Giant ileocolic intussusception in an adult induced by a double ileal lipoma: a case report with pathologic correlation | Radiology Case Reports | 30 | M | Abdominal pain, nausea and vomiting | 3 days | Ileum | 3 | Y | Laparotomy | Not stated |
| Krasniqi et al. | 2011 | Compound double ileoileal and ileocecocolic intussusception caused by lipoma of the ileum in an adult patient: A case report | Journal of Medical Case Reports | 46 | M | Abdominal pain, nausea, vomiting | 4 months | Ileum | 3.5 | Y | Laparotomy | 30 |
| Krespis et al. | 2006 | Partial intestinal obstruction caused by a lipoma within a Meckel's diverticulum | Digestive and Liver Disease | 47 | M | Abdominal pain, fatigue, constipation, GI bleed | 4 months | Meckel's diverticulum | 5 | y | Laparotomy | 5 |
| Kroner et al. | 2015 | Endoscopic Mucosal Resection of Jejunal Polyps using Double-Balloon Enteroscopy | GE Portuguese Journal of Gastroenterology | 58 | F | GI bleed | Not stated | Jejunum | 2 | N | Endoscopic | Not stated |
| Kumar et al. | 2017 | Rare diagnosis of intestinal lipomatosis complicated by intussusception in an adult: A case report | International Journal of Surgery Case Reports | 47 | M | Abdominal pain | 5 days | Ileum | 3 | Y | Laparotomy | 5 |
| Kuzmich et al. | 2010 | Ileocolocolic intussusception secondary to a submucosal lipoma: an unusual cause of intermittent abdominal pain in a 62-year-old woman | Journal of Clinical Ultrasound | 62 | F | Abdominal pain, weight loss | 2 months | Ileum | 7 | Y | Laparotomy | Not stated |
| Lee et al. | 2010 | A case of small-bowel intussusception caused by intestinal lipomatosis: preoperative diagnosis and reduction of intussusception with double-balloon enteroscopy | Gastrointestinal Endoscopy | 48 | F | Abdominal pain, weight loss | 2 months | Jejunum | 5 | Y | Laparoscopic | Not stated |
| Lee et al. | 2017 | Ileocolic intussusception caused by a lipoma in an adult | World Journal of Clinical Cases | 29 | F | Abdominal pain, nausea, fever | 1 day | Ileum | 3.5 | Y | Laparoscopic | 8 |
| Li et al. | 2018 | Gastrointestinal hemorrhage caused by adult intussusception secondary to small intestinal tumors: Two case reports | Medicine (Baltimore) | 54 | M | GI bleed | 1 day | Ileum | 5 | Y | Laparoscopic | 5 |
| Lill et al. | 2007 | Multiple lipomatosis - A rare cause for small bowel intussusception | New Zealand Medical Journal | 39 | M | Abdominal pain | 3 months | Jejunum | 3 | Y | Laparotomy | Not stated |
| Lin et al. | 2007 | Laparoscopy-assisted resection of ileoileal intussusception caused by intestinal lipoma | Journal of Laparoendoscopic and Advanced Surgical Techniques | 31 | M | Anaemia, GI bleed | 1 year | Ileum | 4 | Y | Laparotomy | 8 |
| Lucas et al. | 2011 | Laparoscopic resection of a small bowel lipoma with incidental intussusception | Journal of the Society of Laparoendoscopic Surgeons | 73 | M | Anaemia, GI bleed | Not stated | Jejunum | 2.1 | Y | Laparoscopic | 3 |
| Manna et al. | 2017 | A rare cause of acute gastrointestinal hemorrhage: ileal lipoma Case report | Italian Annals of Surgery | 66 | M | Anaemia, GI bleed | Not stated | Ileum | Not stated | Y | Laparotomy | Not stated |
| Manouras et al. | 2007 | Lipoma induced jejunojejunal intussusception | World Journal of Gastroenterology | 55 | M | Abdominal pain, GI bleed | 3 months | Jejunum | 4 | Y | Laparotomy | 7 |
| Mazziotti et al. | 2006 | Macrodactylia fibrolipomatosis associated with multiple small-bowel lipomas | American Journal of Roentgenology | 57 | M | Abdominal pain, diarrhoea | 10 years | Jejunum | 4 | N | Not stated | Not stated |
| Mbaye et al. | 2017 | [Volvulus of the small intestine caused by mesenteric lipoma] | Pan African Medical Journal | 7 | F | Abdominal pain, vomiting | 6 days | Ileum | Not stated | Y | Laparotomy | Not stated |
| McCoubrey et al. | 2006 | Small bowel volvulus secondary to a mesenteric lipoma: A case report and review of the literature | Irish Journal of Medical Science | 40 | M | Abdominal pain, vomiting, constipation | 7 days | Mesentery | 16 | Y | Laparotomy | 8 |
| McKay | 2006 | Ileocecal intussusception in an adult: the laparoscopic approach | Journal of the Society of Laparoendoscopic Surgeons | 63 | M | Abdominal pain, nausea, GI bleed | 1 day | Ileoceacal valve | Not stated | Y | Laparotomy | 5 |
| Meshikhes et al. | 2005 | Adult intussusception caused by a lipoma in the small bowel: report of a case | Surgery Today | 55 | M | Abdominal pain, nausea, abdominal distension | Ileum | 6 | Y | Laparotomy | 5 | |
| Minaya Bravo et al. | 2012 | Ileocolic intussusception due to giant ileal lipoma: Review of literature and report of a case | International Journal of Surgery Case Reports | 75 | M | Abdominal pain, diarrhoea, vomiting | 3 months | Ileum | 5.5 | Y | Laparotomy | 9 |
| Morimoto et al. | 2010 | Peeling a giant ileal lipoma with endoscopic unroofing and submucosal dissection | World Journal of Gastroenterology | 62 | M | GI bleed | Not stated | Ileum | 5 | Y | Endoscopic | 7 |
| Mouaqit et al. | 2012 | Adult intussusceptions caused by a lipoma in the jejunum: report of a case and review of the literature | World Journal of Emergency Surgery | 35 | M | Abdominal pain, nausea | 4 months | Jejunum | 6 | y | Laparotomy | Not stated |
| Nakanishi et al. | 2019 | Laparoscopic-endoscopic cooperative surgery for ileal lipoma: A case report | Asian Journal of Endoscopic Surgery | 50 | M | GI bleed | Not stated | Ileum | 2.5 | N | Laparoscopic | Not stated |
| Noda et al. | 2016 | Successful endoscopic submucosal dissection of a large terminal ileal lipoma | Case Reports in Gastroenterology | 78 | F | Abdominal pain | 1 year | Ileum | 3 | N | Endoscopic | Not stated |
| Ooi et al. | 2015 | Bleeding ileal lipoma: An extremely rare presentation of anemia in adults | Journal of Gastroenterology and Hepatology (Australia) | 27 | M | GI bleed | 1 Week | Ileum | Not stated | Y | Laparotomy | Not stated |
| Oyen et al. | 2007 | Ileo-ileal intussusception secondary to a lipoma: A literature review | Belgian Acta Chirurgica Belgica | 54 | M | Not stated | Not stated | Ileum | Not stated | Y | Laparoscopic | Not stated |
| Pandya et al. | 2013 | Laparoscopic management of intussusception in an adult | Surgical Endoscopy and Other Interventional Techniques | 47 | F | Abdominal pain | 1 Month | Not stated | 3 | Y | Laparoscopic | Not stated |
| Papageorge et al. | 2018 | Pedunculated small bowel lipoma with heterotopic pancreas causing intussusception | Clinical Case Reports | 36 | M | Abdominal pain, abdominal distension | 4 months | Ileum | 6.5 | Y | Laparoscopic | Not stated |
| Parmar et al. | 2004 | Submucous lipoma of the ileocaecal valve presenting as cecal volvulus | International Journal of Clinical Practice | 53 | F | Abdominal pain | 1 Day | Ileocaecal valve | Not stated | y | Laparotomy | Not stated |
| Paya Llorente et al. | 2018 | Laparoscopic surgery for adult enterocolic intussusception: Case report and literature review | Gastroenterology Hepatology | 20 | M | Abdominal pain, GI bleed | 1 Day | Ileocaecal valve | 4.3 | Y | Laparoscopic | 7 |
| Pezzoli et al. | 2008 | Occult intestinal hemorrhage due to lipoma of the small bowel detected with the combined use of the new endoscopic techniques. A report of two cases | Digestive and Liver Disease | 64 | M | Anaemia | Not stated | Jejunum | 4 | Y | Not stated | Not stated |
| Rathore et al. | 2006 | Adult intussusception--a surgical dilemma | Journal of Ayub Medical College, Abbottabad | 65 | F | Abdominal pain, GI bleed | 8 months | Ileocaecal valve | Not stated | Y | Laparotomy | Not stated |
| 60 | F | Obstruction | Few days | Ileum | Not stated | Y | Laparotomy | Not stated | ||||
| Rattan et al. | 2013 | Small bowel lipomas may be a cause of significant obscure GI bleeding: Report of three cases identified by capsule endoscopy | Journal of Gastroenterology and Hepatology | 66 | M | Abdominal pain, GI bleed, anaemia | Not stated | Jejunum | 2.8 | Y | Laparoscopic | Not stated |
| 76 | F | GI bleed | Not stated | Jejunum | Not stated | Y | Not stated | Not stated | ||||
| Ross et al. | 2000 | Case 26: Jejunojejunal intussusception secondary to a lipoma | Radiology | 80 | M | Abdominal pain | Not stated | Jejunum | Not stated | Y | Not stated | Not stated |
| Safatle-Ribeiro et al. | 2016 | Obscure gastrointestinal bleeding caused by intestinal lipomatosis: double-balloon endoscopic and laparoscopic views | Endoscopy | 52 | M | Abdominal pain, GI bleed | 6 years | Jejunum | Not stated | Y | Laparoscopic | 3 |
| Saito et al. | 2013 | Laparoscopy-assisted resection of ileocecal intussusception caused by ileal pedunculated lipoma | International Journal of Surgery | 31 | M | GI bleed, anaemia | 1 year | Ileum | 4 | Y | Laparoscopic | 8 |
| Seow-En et al. | 2014 | Jejunojejunal intussusception secondary to submucosal lipoma resulting in a 5-year history of intermittent abdominal pain | British Medical Journal Case Reports | 44 | F | Abdominal pain, nausea | 5 years | Jejunum | 3 | Y | Laparoscopic | Not stated |
| Shah et al. | 2005 | Mesenteric lipoma leading to small gut strangulation and short syndrome | Journal of the College of Physicians and Surgeons Pakistan | 14 | M | Abdominal pain, vomiting | 1 day | Jejunum | 12 | Y | Laparotomy | Not stated |
| Sheehan et al. | 2000 | Intussusception in adults: A rare entity | Irish Journal of Medical Science | 53 | M | Abdominal distention, vomiting, diarrhoea. | 1 Week | Ileum | Not stated | Y | Laparotomy | Not stated |
| Sheen et al. | 2003 | A small bowel volvulus caused by a mesenteric lipoma: Report of a case | Surgery Today | 31 | M | Abdominal pain, nausea, vomiting | 2 days | Ileum | 10 | Y | Laparotomy | Not stated |
| Shenoy et al. | 2003 | Segmental jejunal lipomatosis - A rare cause of intestinal obstruction | Yonsei Medical Journal | 33 | M | Abdominal pain, abdominal distension | Not stated | Jejunum | Not stated | Y | Laparotomy | Not stated |
| Shiba et al. | 2009 | Preoperative Diagnosis of Adult Intussusception Caused by Small Bowel Lipoma | Case Reports in Gastroenterology | 33 | M | Abdominal pain | 2 weeks | Ileum | 4 | Y | Laparotomy | Not stated |
| Shimazaki et al. | 2015 | Laparoscopic management of an octogenarian adult intussusception caused by an ileal lipoma suspected preoperatively: A case report | World Journal of Surgical Oncology | 87 | M | Abdominal distention, vomiting | 2 weeks | Ileum | 4 | Y | Laparoscopic | 8 |
| Singh et al. | 2013 | Intussusception due to jejunal lipoma: A case report | Journal of International Medical Sciences Academy | 22 | M | Abdominal pain, nausea, vomiting | 5 days | Jejunum | 6 | Y | Laparotomy | 5 |
| Spada et al. | 2013 | Giant Lipoma as an Unusual Cause of Obscure Gastrointestinal Bleeding | Video Journal and Encyclopedia of GI Endoscopy | 62 | M | GI bleed | Not stated | Ileum | 3.6 | Y | Laparoscopic | Not stated |
| Spaventa-Ibarrola et al. | 2006 | Ileocecal valve lipoma. Case report and review of the literature | Spanish Surgery and Surgeons | 78 | F | Obstruction, abdominal distention, constipation | Not stated | Ileum | 2.5 | Y | Laparotomy | Not stated |
| Stancu et al. | 2016 | Ileo-colic intussusception by ileo-cecal valve lipoma - an infrequent ultrasonographic occurrence. A case report | Journal of Medical Ultrasound | 52 | F | Abdominal pain, weight loss, constipation | 1 month | Ileum | 5.5 | Y | Laparotomy | Not stated |
| Suairez Moreno et al. | 2010 | Multiple intestinal lipomatosis. Case report | Spanish Surgery and Surgeons | 51 | M | Abdominal pain, nausea | Not stated | Multiple | Not stated | N | Conservative | Not stated |
| Suga et al. | 2019 | Giant Mesenteric Lipoma Causing Small Bowel Volvulus: A Case Report | Ethiopian Journal of Health Sciences | 25 | M | Abdominal pain | 3 days | Jejunum | 15 | Y | Laparotomy | Not stated |
| Tayeh et al. | 2015 | Giant mesenteric lipoma: A case report and a review of the literature | Journal of Pediatric Surgery Case Reports | 2 | M | Abdominal distension | 1 year | Ileum | 22 | Y | Laparotomy | Not stated |
| Toya et al. | 2014 | Lipoma of the small intestine treated with endoscopic resection | Clinical Journal of Gastroenterology | 79 | M | GI bleed | Not stated | Jejunum | 3.5 | Y | Endoscopic | Not stated |
| Tse et al. | 2018 | Intermittent intussusception and microcytic anemia caused by a submucosal jejunal lipoma: A rare case report | Surgical Endoscopy and Other Interventional Techniques | 40 | M | Abdominal pain, anaemia, GI bleed | 3 weeks | Jejunum | 5.5 | Y | Laparoscopic | 2 |
| Tsushimi et al. | 2006 | Laparoscopic resection of an ileal lipoma: Report of a case | Surgery Today | 63 | F | Abdominal pain, vomiting | Not stated | Ileum | 2.5 | N | Laparoscopic | 15 |
| Turi et al. | 2004 | Lipoma of the Small Bowel - A Rare Cause of Abdominal Pain and Chronic Bloody Diarrhoea | German Journal of Gastroenterology | 40 | F | Abdominal pain, diarrhoea, weight loss | 6 weeks | Ileum | 2 | Y | Not stated | Not stated |
| Uyulmaz et al. | 2018 | Ileoileal intussusception in unspecific recurrent abdominal pain in adult: A case report | SAGE Open Medical Case Reports | 53 | F | Abdominal pain, diarrhoea, weight loss | 3 months | Ileum | 8 | Y | Laparoscopic | 8 |
| Vagholkar et al. | 2015 | Lipoma of the Small Intestine: A Cause for Intussusception in Adults | Case Reports in Surgery | 22 | M | Abdominal pain, vomiting | 2 days | Ileum | Not stated | Y | Laparotomy | Not stated |
| Vekic et al. | 2014 | Pedunculated obstructive lipoma of the ileocecal valve: a case report | Serbian Archives of Medicine | 67 | F | Abdominal pain, nausea, abdominal distension, vomiting, constipation | 3 days | Ileocaecal valve | 5 | Y | Laparotomy | 7 |
| Wan et al. | 2010 | Partial intestinal obstruction secondary to multiple lipomas within jejunal duplication cyst: A case report | World Journal of Gastroenterology | 68 | M | Abdominal distention, weight loss | 10 days | Jejunum | 3.2 | Y | Laparotomy | 7 |
| Wardi et al. | 2013 | Unusual cause of upper gastrointestinal bleeding | Journal of Medical Case Reports | 53 | M | GI bleed, anaemia | 6 months | Jejunum | 5 | Y | Laparotomy | Not stated |
| Watt et al. | 2012 | Mesenteric lipoma causing small bowel perforation: A case report and review of literature | Scottish Medical Journal | 72 | M | Abdominal pain | Not stated | Ileum | Not stated | Y | Laparotomy | Not stated |
| Wolko et al. | 2003 | Torsion of a giant mesenteric lipoma | Pediatric Radiology | 9 | M | Abdominal pain | 10 days | Ileum | Not stated | Y | Laparotomy | Not stated |
| Wu et al. | 2018 | Preoperative radiologic patent blue localization for intracorporeal laparoscopic resection of a terminal ileal submucosal lipoma: A case report | International Journal of Surgery Case Reports | 31 | F | Abdominal pain | Not stated | Ileum | 1.5 | Y | Laparoscopic | Not stated |
| Yagnik | 2018 | Giant ileocecal submucosal lipoma presenting with hematochezia | ANZ Journal of Surgery | 65 | M | GI bleed | 15 Days | Ileocaecal valve | 5 | Y | Laparotomy | Not stated |
| Yatagai et al. | 2016 | Obscure gastrointestinal bleeding caused by small intestinal lipoma: a case report | Journal of Medical Case Reports | 69 | M | GI bleed, anaemia | Not stated | Jejunum | 3.6 | Y | Laparoscopic | 9 |
| Yigitler et al. | 2007 | A rare cause of bleeding intestinal intussusception in adult: jejunal lipoma | Turkish Journal of Trauma and Emergency Surgery | 76 | M | Obstruction, GI bleed | Not stated | Jejunum | Not stated | N | Conservative | Not stated |
| Yoshimoto et al. | 2019 | Novel surgical approach without bowel resection for multiple gastrointestinal lipomatosis: A case report | International Journal of Surgery Case Reports | 47 | F | Obstruction | Not stated | Ileum | 4.3 | Y | Laparoscopic | Not stated |
| Zissin | 2004 | Enteroenteric intussusception secondary to a lipoma: CT diagnosis | Emergency Radiology | 20 | F | Abdominal pain, vomiting | 1 month | Ileum | 1.8 | Y | Laparotomy | Not stated |
| Gray et al. | 2001 | Small intestinal intussusception secondary to a submucosal lipoma | Archives of pathology and laboratory medicine | 64 | F | Abdominal pain | 9–12 months | Not stated | 3.5 | Y | Laparotomy | Not stated |
| Balamoun et al. | 2011 | Ileal lipoma-a rare cause of ileocolic intussusception in adults: case report and literature review | World Journal of Gastroenterology Surgery | 65 | M | Abdominal pain, vomiting | 3 days | Ileum | 1.2 | Y | Laparotomy | Not stated |
| Colovic et al. | 2000 | Mesenteric lipoma causing volvulus of the small intestine | Serbian Archives of Medicine | 77 | M | Abdominal pain, vomiting | 5 days | Mesentery | 18 | Y | Laparotomy | Not stated |
| Wong et al. | 2005 | Primary mesenteric lipoma causing closed loop bowel obstruction: a case report | The Kaoshiung Journal of Medical Sciences | 45 | F | Abdominal pain | Sudden onset | Ileum | 6.5 | Y | Laparotomy | Not stated |
| Aminian et al. | 2009 | Ileal intussusception secondary to both lipoma and angiolipoma: a case report | Cases Journal | 53 | F | Abdominal pain, nausea, diarrhoea | 4 months | Ileum | 1.5 | Y | Laparotomy | 7 |
| Lin et al. | 2007 | Laparoscopy-assisted resection of ileoileal intussusception caused by intestinal lipoma | Journal of Laparoendoscopic and Advanced Surgical Techniques | 47 | F | Abdominal pain, nausea, vomiting | 5 days | Ileum | 3 | Y | Laparotomy | 4 |
| Zografos et al. | 2005 | Small intestinal lipoma as a cause of massive gastrointestinal bleeding identified by intraoperative enteroscopy. A case report and review of the literature | Digestive diseases and Sciences | 82 | F | GI bleed | 2 days | Ileum | 2.5 | Y | Laparotomy | 9 |
| Park et al. | 2001 | Laparoscopic-assisted resection of ileal lipoma causing ileo-ileo-colic intussusception | Journal of Korean Medical Sciences | 39 | M | Abdominal pain | 2 years | Ileum | 4 | Y | Laparoscopic | 4 |
| Cha et al. | 2009 | Giant mesenteric lipoma as an unusual cause of abdominal pain: a case report and a review of the literature | Journal of Korean Medical Sciences | 29 | F | Abdominal pain, abdominal distension, constipation | 3 years | Mesentery | 19 | Y | Laparoscopic | Not stated |
| Charalambous et al. | 2012 | Jejunojejunal lipoma causing intussusception | Case Reports in Gastroenterology | 46 | M | Abdominal pain, GI bleed | 3 months | Jejunum | 4 | Y | Laparotomy | 7 |
| Jai et al. | 2008 | Jejunal lipoma with intermittent intussusception revealed by partial obstructive syndrome | The Saudi Journal of Gastroenterology | 37 | F | Abdominal pain | 3 years | Jejunum | 3 | Y | Laparotomy | Not stated |
| Chen et al. | 2008 | Severe adult ileosigmoid intussusception prolapsing from the rectum: A case report | Cases Journal | 36 | M | Abdominal pain, diarrhoea and rectal prolapse | 2 months | Ileocaecal valve | 9 | Y | Laparotomy | Not stated |
| Enyinnah et al. | 2013 | Mesenteric lipoma causing recurrent intestinal obstruction | Nigerian Journal of Clinical Practice | 29 | M | Abdominal pain, vomiting, constipation, abdominal mass | 10 years | Mesentery | 15 | Y | Laparotomy | Not stated |
| Innocent et al. | 2015 | Distal ileal stenosing subserosal lipoma: a case report | Nigerian Journal of Medicine | 38 | M | Obstruction | Not stated | Ileum | Not stated | Y | Laparotomy | 7 |
| Jiang et al. | 2015 | Pancreatic and Gastric Heterotopia with Associated Submucosal Lipoma Presenting as a 7-cm Obstructive Tumor of the Ileum: Resection with Double Balloon Enteroscopy | Case Reports in Gastroenterology | 38 | F | Abdominal pain, nausea, vomiting, GI bleed | 29 years | Ileum | 12.5 | Y | Endoscopic | Not stated |
| Kabawe et al. | 2019 | Jejunal intussusception in an adult due to multiple lipomas: a rare case report from Syria | Journal of Surgical Case Reports | 37 | M | Abdominal pain, vomiting, abdominal distension | 3 days | Jejunum | 4.5 | Y | Laparoscopic | 3 |
| Lee et al. | 2013 | Endoscopic treatment of a symptomatic ileal lipoma with recurrent ileocolic intussusceptions by using cap-assisted colonoscopy | Clinical Endoscopy | 73 | F | Abdominal pain, weight loss | 2 years | Ileum | 2.7 | Y | Endoscopic | Not stated |
| Molnar et al. | 2013 | Ileo-ceco-descendento-colic intussusception in adult - a case report | Romanian Journal of Surgery | 30 | F | Abdominal pain, nausea, vomiting, weight loss | 10 days | Ileum | 5 | Y | Laparotomy | 7 |
| Namikawa et al. | 2011 | Adult ileoileal intussusception induced by an ileal lipoma diagnosed preoperatively: report of a case and review of the literature | Surgery Today | 68 | F | Abdominal pain | Not stated | Ileum | 1.5 | Y | Laparotomy | 10 |
| Pinto et al. | 2018 | Jejunal Lipoma, an Uncommon Cause of Gastrointestinal Bleeding | Portuguese Journal of Gastroenterology | 46 | M | GI bleed, fatigue | Not stated | Jejunum | 7.5 | Y | Laparotomy | Not stated |
| Shpaner et al. | 2008 | Rectal bleeding caused by a large, partially obstructing lipoma of the terminal ileum | Clinical Gastroenterology and Hepatology | 38 | F | GI bleed, weight loss | 2 months | Ileum | 3.3 | Y | Laparoscopic | Not stated |
| Sueoka et al. | 2016 | A Case of Spontaneously Reduced Ileoileal Intussusception Caused by a Lipoma | Hiroshima Journal of Medical Sciences | 68 | F | Abdominal pain | Sudden onset | Ileum | 2.5 | Y | Laparotomy | Not stated |
| Yang et al. | 2017 | Torsion of a Giant Antimesenteric Lipoma of the Ileum: A Rare Cause of Acute Abdominal Pain | The American Journal of Case Reports | 67 | F | Abdominal pain, abdominal distension, nausea, vomiting | 1 week | Ileum | 12 | Y | Laparotomy | 7 |
GI = Gastrointestinal, M = Male, F = Female, Y = Yes, N = No.
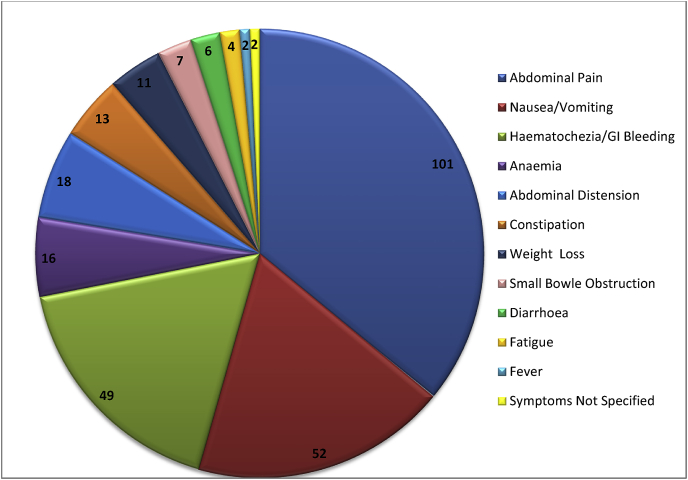
Presenting symptoms were reported as (Table 2): abdominal pain 101 (68.7%); nausea/vomiting 52 (35.3%), hematochezia/GI bleeding 49 (33.3%); anaemia 16 (10.9%); abdominal distension 18 (12.2%); constipation 13 (8.9%); weight loss 11 (7.5%); small bowel obstruction 7 (4.7%); diarrhoea 6 (4.1%); fatigue 4 (2.7%); fever 2 (1.4%); symptoms not specified 2 (1.4%).
Table 2.
Presenting symptom profile
All patients were symptomatic and 134/147 (91.2%) presented as emergencies. Duration of preceding symptoms varied from 1 h to 29 years and was recorded in 104/147 cases. Mean duration of preceding symptoms was 295 days and standard deviation (SD) = 1173. With symptoms greater than 1 year excluded (n = 9), mean preceding symptom length was 58.1 days (SD = 96.8).
Diagnostic imaging modalities were: abdominal X-Ray 49/147 (33.3%); endoscopy 68/147 (46.3%); CT 115/147 (78.2%); abdominal ultrasound 35/147 (23.8%); barium study 20/147 (13.6%); video capsule endoscopy (VCE) 13/147 (8.8%); MRI small bowel 4/147 (2.7%).
124/137 (90.5%) required definitive surgical management, either laparotomy (n = 89) or laparoscopic resection (n = 35). 8 laparotomies started as laparoscopic procedures and 1 as an attempted endoscopic resection. 13 patients were successfully managed non-operatively (9.5%); 9 with endoscopic resection (6.6%) and 4 conservatively (2.9%). In 10 cases the definitive management strategy was not stated (see Table 3).
Table 3.
Comparison of management strategies.
| Laparotomy | Laparoscopic | Endoscopic | Conservative | Not stated | |
|---|---|---|---|---|---|
| Initial Management | 80 | 43 | 10 | 4 | 10 |
| Definitive Management | 89 | 35 | 9 | 4 | 10 |
| Success (%) | NA | 81% | 90% | 100% | NA |
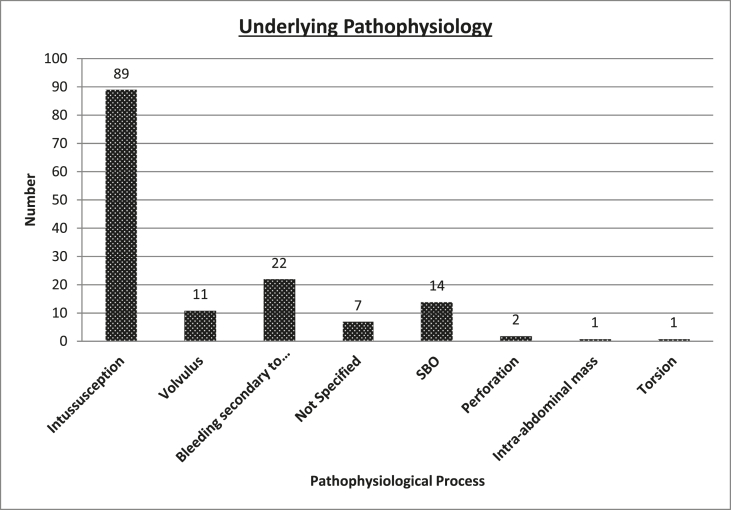
The underlying pathophysiology was intussusception 89 (60.5%); bleeding secondary to ulceration/necrosis 22 (15%); volvulus 11 (7.5%), small bowel obstruction 14 (9.5%); perforation 2 (1.4%); intra-abdominal mass 1 (0.7%); torsion 1 (0.7%) not specified 7 (4.8%). Fig. 2 highlights these results.
Fig. 2.
Underlying pathophysiology.
Location of lipoma was ileum (n = 88, 59.9%); jejunum (n = 47,32%); mesentery (n = 7, 4.8%); multiple (n-2, 1%) not specified (n = 3, 2%). The ileal cases can be further subdivided: ileum (n = 75; ileocaecal valve (n = 10); Meckel's diverticulum (n = 3).
Lipoma size was recorded in 115 cases and ranged from 1.2 to 22 cm at the greatest diameter. Mean size was 5.1 cm. When comparing mean lipoma size and successful management strategy, laparotomy = 5.6 cm, laparoscopic = 4.4 cm, endoscopically managed 3.7 cm, conservative 4.5 cm (Table 4. One-way Anova test was performed, the p value of 0.21 demonstrated no statistically significant difference between groups (laparotomy, laparoscopic and endoscopic).
Table 4.
Associations between management, lipoma size and length of stay.
| Definitive Management | Number | Average Size (cm) | Length of stay (days) |
|---|---|---|---|
| Laparotomy | 89 | 5.6 | 8.5 |
| Laparoscopic | 35 | 4.4 | 6.4 |
| Endoscopic | 9 | 3.7 | 7 |
| Conservative | 4 | 4.5 | not stated |
| Not stated | 10 | / | / |
| Overall | 147 | 5.1 | 7.4 |
Of the 147 cases, one report described the specimen as a chondrolipoma. All other cases were benign lipomas.
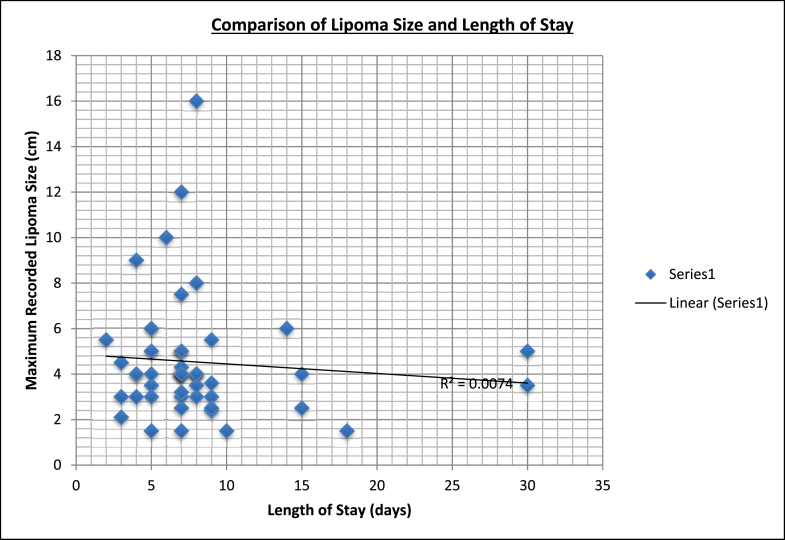
Average length of hospital stay (n = 68) was 7.4 (2–30) days. Interquartile range = 3 (Q3–Q1 (8-5)). Average length of stay was 8.5 days with open surgery and 6.4 days with laparoscopic surgery (Table 4). T-test was performed, analysing length of stay between laparotomy and laparoscopic management. A p value of 0.13 demonstrated no statistically significant difference in length of stay. Numbers did not permit comparison of length of stay with the other management modalities. Comparison of lipoma size and length of stay in the 52 cases where both variables were recorded is shown in Fig. 3. There was no significant correlation (R2 = 0.0074).
Fig. 3.
Comparison of lipoma size and length of stay.
4 complications were reported from the 135 cases: 2 surgical wound infections; multi-organ failure and PE; intraoperative laceration to muscular layer. No associated intraoperative or 30-day mortality was reported.
4. Discussion
Our data identify a male preponderance (60%) in those with symptomatic small bowel lipomas. Lipomas of the colon are reported as being more common in women [8], whereas those found in the oesophagus have a greater prevalence in men [9]. Gastrointestinal lipomas are most commonly found in patients aged 50–70 years [10,11]. Average patient age of this cohort (49.9 years) lies just outside this range (however this is comparable with other reported groups of patients with lipomas). Our data emphasise that lipomas may present at any age with both children and the elderly documented. Pediatric gastrointestinal lipomas are rarely encountered. Our study highlights 9 pediatric cases of symptomatic lipomas causing intussusception, volvulus, abdominal mass or obstruction.
Lipomas of the gastrointestinal tract have been extensively documented as causative factors in bleeding, intussusception, obstruction, volvulus and altered bowel habit. There is wide variation in presentation. (Our data highlights the breadth of presenting symptoms.) Abdominal pain was the most prevalent symptom, reported in 68% of patients, whilst nausea and/or vomiting and gastrointestinal bleeding were also commonly seen, in 35% and 34% of patients respectively. This is not surprising given that 60% of cases were related to intussusception.
Our results are consistent with data from other papers which identify chronic intermittent cramping abdominal pain associated with nonspecific signs of bowel obstruction including nausea, vomiting, gastrointestinal bleeding, constipation or abdominal distension as key symptoms associated with intussusception [12]. Lipomas accounts for 5% of all cases of intussusception in adults [13], the rest of which are mainly caused by malignant neoplasm [14].
The time course of presenting symptoms ranged from only a few hours to many years. Whilst there was considerable discrepancy in time course within our data, the mean of 58.1 days of preceding symptoms (when 9 results >1 year were excluded) serves as an indicator as to the most commonly encountered presentation. The wide variation may be explained by the fact that many patients had undergone semi-urgent/elective diagnostic investigations in the community prior to presenting as an emergency.
Gastrointestinal endoscopic investigations are viewed as the gold standard to investigate red flag symptoms of malignancy, bleeding, weight loss, on-going abdominal pain and anaemia [15]. Such symptoms are common to both gastrointestinal malignancy and symptomatic lipomas. However, endoscopic investigations are often negative in lipoma patients given the anatomical position of small bowel lipomas. Thus, delay in diagnosis and referral on for further investigations are likely outcomes.
It is not surprising that the majority of patients in our cohort underwent numerous investigations prior to definitive diagnosis and management. Negative endoscopic investigations were a recurrent theme in many. Given documented colonoscopy perforation rates of 0.016%–0.2% [16], are these patients being exposed to unnecessary risk of potential morbidity? This is pertinent, as radiological imaging is an effective diagnostic tool for lipomas. Nevertheless, malignancy is a differential diagnosis and CT alone may miss a small bowel cancer, diagnosis is only accurate in 55% of cases [17]. Thus, endoscopic work up is an important adjunct helping clinicians exclude other more common pathology despite associated risks.
As stated conventional endoscopic investigations such as colonoscopy and gastroscopy are negative in this cohort. However, double balloon enteroscopy (DBE) appears both an effective diagnostic and therapeutic modality enabling direct visualisation, biopsy and resection of small bowel lipomas in the appropriate setting. The ability to offer therapeutic treatment sets this option out from other diagnostic modalities such as video capsule endoscopy [18]. Nevertheless, DBE is an invasive procedure and is limited to specialist centres. Currently DBE does not appear to form part of standard diagnostic work in this patient cohort.
The sensitivity and specificity of ultrasound in the diagnosis of lipomas are reported as being 85.71% and 95.95% respectively by Rahmani et al. [19]. However, transabdominal ultrasonography is not accurate for detecting small bowel tumors; the reported sensitivity is low (26%) [20]. In contrast, CT and MRI both have high sensitivity in detecting gastrointestinal lipomas [21]. It therefore follows that the majority of patients underwent CT imaging (78%).
More lipomas were located in the ileum than jejunum (59.9%–32% respectively). Our data support previous reports that ileal lipomas are more prevalent than jejunal lipomas [22,23].
Manouras et al. state ‘lesions less than 1 cm are considered incapable of producing symptoms, while 75% of those greater than 4 cm are symptomatic’ [4]. Our data support this statement, with the average maximal diameter in symptomatic lipomas measuring 5.1 cm. No lipoma less than 1.2 cm was recorded within our dataset. When evaluating whether any association between maximum lipoma diameter and successful treatment modality exists our results suggest that larger lipomas are more likely to undergo surgery (surgically managed = 5.1 cm, endoscopically managed 3.7 cm, conservative 4.5 cm). Caution when interpreting such results should be taken given the small sample sizes of those managed conservatively and endoscopically.
No reports of surveillance relating to small bowel lipoma growth are reported. One may postulate that even incidentally found large (>2 cm) asymptomatic small bowel lipomas do not require routine follow up given the rarity of patients becoming symptomatic and very low associated risk of malignant transformation.
Various pathophysiological mechanisms are shown in Fig. 2. Some are related, with gastrointestinal bleeding occurring as a result of pressure necrosis and ulceration, and obstruction when a lipoma occludes the bowel lumen. Intussusception and volvulus are similarly capable of causing obstruction and bleeding. Intussusception was the most common pathophysiological mechanism within our cohort. Our data give an up to date review of ways in which lipomas give rise to pathology in these patients.
With few documented cases, no consensus on the management of symptomatic small bowel lipomas currently exists. Parallels can be drawn from the management of colonic lipomas where Nallamothu et al. advocate surgery as first line treatment in lipomas that are sessile, with limited peduncles, extension into muscularis propria/serosa, or when endoscopic resection has failed [8]. Surgery is also suggested as primary management for giant colonic lipomas (>4 cm). However, we suggest other strategies may sometimes have a role.
Conservative management alone was effective in 4 patients. Spontaneous expulsion of a 7 × 4.5 × 3.6 cm ileal lipoma resolved a patient's intussusception and negated the need for surgical intervention as described by Kang [24]. Kim et al. report a 50-year-old man who declined surgery after double balloon enteroscopy diagnosed multiple jejunal lipomatosis [25]. He was treated with analgesia and followed up regularly as an outpatient. Suarez et al. document a 51-year-old male found to have multiple submucosal lipomas in the stomach and small bowel [26]. His symptoms spontaneously settled without the need for any treatment. Nevertheless, these cases appear to be the exception within this cohort.
Endoscopic mucosal resection (as part of DBE) appears to have a limited role in the management of small bowel lipomas. Given the anatomical constraints and required expertise of such procedures this practice is not widespread and accounts for only a small portion of those managed. Nevertheless, successful procedures have been undertaken, as evidenced by our data. Noda et al. report endoscopic mucosal dissection of a 3 cm terminal ileal lipoma [27], whilst Morimoto used a combination of endoscopic snare and IT-knife to perform endomucosal dissection of a 5 cm ileal lipoma although this was complicated by a muscular and serosal layer laceration [28]. Javia reports a patient with a 2 cm terminal ileal lipoma which was excised using endoscopic snare [29]. A patient with a 2 cm lipoma underwent double-balloon-assisted jejunal endoscopic mucosal resection, as reported by Kröner et al. [30]. Such reports demonstrate that both jejunal and ileal lipomas may be managed by endoscopic measures. Only one reported case failed to remove the lipoma, citing the size (3 × 1.5 × 1.5 cm) and wide base as reasons for this. A subsequent laparotomy was required to treat the patient [31]. Careful case selection appears to be an important factor, with some authors stating risks of bleeding and perforation as contraindications to undertaking such procedures [32]. Of the 10 attempted endomucosal resections, 9 were published from 2012 onwards, indicating that this is an emerging area within endoscopy.
Our results show that surgery was the most utilised definitive management strategy. Both open and laparoscopic procedures were undertaken with preponderance for laparotomy as definitive management. Those patients requiring surgery primarily underwent bowel resection and primary anastomosis. Anatomical location determined whether resection was only small bowel or included a portion of large bowel. As Table 4 demonstrates, the average size of symptomatic lipoma resected laparoscopically was (1.2 cm) smaller than those removed via open surgery, however, the exact reasons for this is unclear. Patient selection is likely to a be a factor, with multiple aspects taken into consideration e.g. a surgeon's skillset/standard practice, a centres equipment, critical condition of a patient, degree of bowel obstruction, patient comorbidities and lipoma size. The high rate of surgical management may be attributable to the need to exclude alternative causes for each presentation such as malignancy and the limited practice of alternative management strategies [14,33].
Laparoscopic surgery was unsuccessful in 19% of cases attempted. Authors state a variety of reasons for converting to open surgery. Alsayegh et al. report the use of laparoscopy being diagnostic in a 4 year old before converting to a Pfannenstiel incision in order to resect a 6.7 × 7.6 × 4.4 cm lipoma of the mesentery causing volvulus [34]. Bilgin states that intraoperative adhesions in a case of adult intussusception secondary to a lipoma resulted in conversion [35]. The cost of laparoscopic staplers is highlighted as a factor by Lin for performing a laparoscopy-assisted extracorporeal resection and anastomosis of an intussuscepted segment [36]. Sheehan cites oedema and ischaemia following attempted laparoscopic reduction of an ileocolic intussusception [37].
Associated mortality (0%) and morbidity (2%) rates were low. Given that over 90% of patients underwent surgical intervention in a cohort where average age was almost 50 years, such values are encouraging. However, comparison of morbidity and mortality associated with similar pathologies suggests that complications may have been underreported or not documented. Mortality from adult intussusception increases from 8.7% for benign lesions to 52.4% for those with a malignant cause [38]. Although there are numerous documented cases of gastrointestinal lipomas associated with intussusception, very few report associated morbidity.
Crocetti et al. report an average length of stay in hospital of 5 and 7 days in patients with symptomatic colonic lipomas managed laparoscopically and with open surgery respectively [39]. In our cohort the average length of stay with symptomatic small bowel lipomas was 7.4 days. Open surgery was associated with a longer length of stay (8.5 days) when compared to laparoscopic management (6.4 days). These results are consistent with other reports of shorter hospital stays with laparoscopic management of small bowel obstruction [40].
We acknowledge that there are limitations associated with our study. The paper is based on only those cases documented in the literature. The true incidence of symptomatic lipomas is likely to be higher. Equally we take into account reporting bias. Sub-acute symptomatic patients are unlikely to require emergency intervention and equally will not be reported on. Nevertheless, based on the data collated and analysed we feel able to draw rational conclusions.
5. Conclusion
We provide a topical and current overview of symptomatic small bowel lipomas. Numerous reports exist of individual cases, referencing small observational studies dating back many decades, but little new data concerning this relatively unknown condition has been collated in recent years. Our study is up to date and practical, presenting new findings, helping provide a framework for classification and management.
A number of important and previously undocumented points are illustrated. A clearer symptom profile is described with most presenting as emergencies necessitating tailored patient care in a timely fashion. Computerised tomography appears to be the primary diagnostic investigation, helping delineate both lipoma and sequelae. Lipomas >1.2 cm may be symptomatic although larger lipomas appear more implicated. Open surgery remains the primary management modality, but smaller symptomatic lipomas may be targeted for laparoscopic surgery in appropriate settings. Laparoscopic surgery is associated with shorter hospitals stays. Endoscopic resection may be a practical first line management in carefully selected patients, although limited data currently exist. Such techniques may reduce the need for invasive surgery in future as skillset and availability improve. Morbidity and mortality rates appear low in this cohort of patients irrespective of lipoma size or management strategy.
We hope that this study offers an insight into the many different facets associated with symptomatic small bowel lipomas. This study adds to the scanty existing knowledge about symptomatic small bowel lipomas. It will inform clinicians and guide management in both the elective and emergency setting to help achieveoptimal patient outcomes.
Provenance and peer review
Not commissioned externally peer reviewed.
Funding
None.
Ethical approval
Not Applicable.
Consent
Not applicable.
Registration of research studies
1. Name of the registry: PROSPERO.
2. Unique Identifying number or registration ID: CRD42020172916.
3.Hyperlink to your specific registration (must be publicly accessible and will be checked): https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=172916
Author contribution
Nicholas Farkas : study design, data collection, data analysis, writing, editing
Joshua Wong : data collection, data analysis
Jordan Bethel : Data collection
Sherif Monib : Data collection, data analysis
Adam Frampton : Editing
Simon Thomson : writing, editing
Guarantor
Mr Nicholas Farkas
Mr Simon Thomson
Declaration of competing interest
No conflicts of interest.
Acknowledgements
We did not receive any funding.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2020.08.028.
.
Contributor Information
Nicholas Farkas, Email: nickfarkas@doctors.org.uk.
Joshua Wong, Email: joshua.wong3@nhs.net.
Jordan Bethel, Email: Jordan.bethel1@nhs.net.
Sherif Monib, Email: sherif.mmonib@gmail.com.
Adam Frampton, Email: a.frampton@imperial.ac.uk.
Simon Thomson, Email: Simon.thomson2@nhs.net.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Pei M.W., Hu M.R., Chen W Bin, Qin C. Diagnosis and treatment of duodenal lipoma: a systematic review and a case report. J Clin diagnostic Res. 2017;11(7):PE01. doi: 10.7860/JCDR/2017/27748.10322. JCDR Research & Publications Private Limited. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sapalidis K., Laskou S., Kosmidis C., Passos I., Mantalobas S., Michalopoulos N. vol. 7. SAGE Publications Sage UK; London, England: 2019. Symptomatic Colonic Lipomas: Report of Two Cases and a Review of the Literature. SAGE Open Med Case Reports. 2050313X19830477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Agrawal A., Singh K.J. Symptomatic intestinal lipomas: our experience. Med J. Armed Forces India. 2011;67(4):374–376. doi: 10.1016/S0377-1237(11)60090-7. https://pubmed.ncbi.nlm.nih.gov/27365853 [Internet]. 2011/10/22. Elsevier. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Manouras A., Lagoudianakis E.E., Dardamanis D., Tsekouras D.K., Markogiannakis H., Genetzakis M. Lipoma induced jejunojejunal intussusception. World J Gastroenterol WJG. 2007;13(26):3641. doi: 10.3748/wjg.v13.i26.3641. Baishideng Publishing Group Inc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Taylor A.J., Stewart E.T., Dodds W.J. Gastrointestinal lipomas: a radiologic and pathologic review. Am J Roentgenol. Am J Roentgen. Ray Soc. 1990;155(6):1205–1210. doi: 10.2214/ajr.155.6.2122666. [DOI] [PubMed] [Google Scholar]
- 6.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int. J. Surg. 2018;8(5):336–341. doi: 10.1016/j.ijsu.2010.02.007. Elsevier. [DOI] [PubMed] [Google Scholar]
- 7.Shea B.J., Reeves B.C., Wells G., Thuku M., Hamel C., Moran J. Amstar 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. bmj. Br. Med. J. 2017;358:j4008. doi: 10.1136/bmj.j4008. Publishing Group. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nallamothu G., Adler D.G. Large colonic lipomas. Gastroenterol. Hepatol. 2011;7:490–492. [PMC free article] [PubMed] [Google Scholar]
- 9.Ahmad A., Bruneton J. Lipomas of the digestive tract: general aspects and imaging. Cureus. 2014;6(9) [Google Scholar]
- 10.Ryan J., Martin J.E., Pollock D.J. Fatty tumours of the large intestine: a clinicopathological review of 13 cases. Br J Surg. 1989;76(8):793–796. doi: 10.1002/bjs.1800760809. Wiley Online Library. [DOI] [PubMed] [Google Scholar]
- 11.Michowitz M., Lazebnik N., Noy S., Lazebnik R. Lipoma of the colon. A report of 22 cases. Am. Surg. 1985;51(8):449–454. [PubMed] [Google Scholar]
- 12.Begos D.G., Sandor A., Modlin I.M. The diagnosis and management of adult intussusception. Am J Surg. 1997;173(2):88–94. doi: 10.1016/S0002-9610(96)00419-9. Elsevier. [DOI] [PubMed] [Google Scholar]
- 13.Azar T., Berger D.L. Adult intussusception. Ann Surg. United States. 1997 Aug;226(2):134–138. doi: 10.1097/00000658-199708000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chiang J., Lin Y. Tumor spectrum of adult intussusception. J Surg Oncol. 2008;98(6):444–447. doi: 10.1002/jso.21117. Wiley Online Library. [DOI] [PubMed] [Google Scholar]
- 15.Davila R.E., Rajan E., Adler D., Hirota W.K., Jacobson B.C., Leighton J.A. ASGE guideline: the role of endoscopy in the diagnosis, staging, and management of colorectal cancer. Gastrointest Endosc. 2005;61(1):1–7. doi: 10.1016/s0016-5107(04)02391-0. Elsevier. [DOI] [PubMed] [Google Scholar]
- 16.Lohsiriwat V. Colonoscopic perforation: incidence, risk factors, management and outcome. World J Gastroenterol. 2010;16(4):425–430. doi: 10.3748/wjg.v16.i4.425. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2811793/ [Internet]. The WJG Press and Baishideng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Han J.W., Hong S.N., Jang H.J., Jeon S.R., Cha J.M., Park S.J. Clinical efficacy of various diagnostic tests for small bowel tumors and clinical features of tumors missed by capsule endoscopy. In: Yen H.-H., editor. 2015. p. 623208. (Gastroenterol Res Pract [Internet]. Hindawi Publishing Corporation). 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saygili F., Saygili S.M., Oztas E. Examining the whole bowel, double balloon enteroscopy: indications, diagnostic yield and complications. World J Gastrointest Endosc. 2015;7(3):247–252. doi: 10.4253/wjge.v7.i3.247. https://pubmed.ncbi.nlm.nih.gov/25789095 [Internet]. Baishideng Publishing Group Inc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rahmani G., McCarthy P., Bergin D. vol. 6. SAGE Publications Sage UK; London, England: 2017. The Diagnostic Accuracy of Ultrasonography for Soft Tissue Lipomas: a Systematic Review. Acta Radiol Open. 6):2058460117716704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Masselli G., Casciani E., Polettini E., Laghi F., Gualdi G. Magnetic resonance imaging of small bowel neoplasms. Cancer Imaging. BioMed Central. 2013;13(1):92. doi: 10.1102/1470-7330.2013.0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Genchellac H., Demir M.K., Ozdemir H., Unlu E., Temizoz O. Computed tomographic and magnetic resonance imaging findings of asymptomatic intra-abdominal gastrointestinal system lipomas. J Comput Assist Tomogr. LWW. 2008;32(6):841–847. doi: 10.1097/RCT.0b013e318159a4b5. [DOI] [PubMed] [Google Scholar]
- 22.Ellis J.T., Windham S.W. Recurrent abdominal pains due to lipoma of ileum. AMA Arch Surg. Am. Med. Assoc. 1951;63(6):859–860. doi: 10.1001/archsurg.1951.01250040875018. [DOI] [PubMed] [Google Scholar]
- 23.Wilson J.M., Melvin D.B., Gray G., Thorbjarnarson B. Benign small bowel tumor. Ann Surg. Lippincott, Williams, and Wilkins. 1975;181(2):247. [PMC free article] [PubMed] [Google Scholar]
- 24.Kang B., Zhang Q., Shang D., Ni Q., Muhammad F., Hou L. Resolution of intussusception after spontaneous expulsion of an ileal lipoma per rectum: a case report and literature review. World J Surg Oncol. 2014;12(1):143. doi: 10.1186/1477-7819-12-143. Springer. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim Hyung-Keun, Cho Young-Seok, Kim Sung-Soo, Lee Su-Yeon, Kim Seung-Kyoung, Kim Eun-Sun, Yun-Ji Kim H.-S.C. A case of jejunal lipomatosis diagnosed with double-balloon enteroscopy. J Gastroenterol Hepatol Res. 2013;2(1) [Google Scholar]
- 26.Suárez R.M.M., Hernández D.A.R., Madrazo M.N., Salazar C.R.L., Martínez R.G. Multiple intestinal lipomatosis. Case report. Cir Cir. 2010;78(2):163–165. [PubMed] [Google Scholar]
- 27.Noda H., Ogasawara N., Tamura Y., Kondo Y., Izawa S., Ebi M. Successful endoscopic submucosal dissection of a large terminal ileal lipoma. Case Rep Gastroenterol. 2016;10(3):506–511. doi: 10.1159/000448886. Karger Publishers. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Morimoto T., Fu K.-I., Konuma H., Izumi Y., Matsuyama S., Ogura K. Peeling a giant ileal lipoma with endoscopic unroofing and submucosal dissection. World J Gastroenterol WJG. 2010;16(13):1676. doi: 10.3748/wjg.v16.i13.1676. Baishideng Publishing Group Inc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Javia S.B., Singhal S. Endoscopic resection of small-bowel submucosal nodule. Endoscopy. © Georg Thieme Verlag KG. 2016;48(S 01) doi: 10.1055/s-0042-104190. E111–E111. [DOI] [PubMed] [Google Scholar]
- 30.Kröner P.T., Sancar A., Fry L.C., Neumann H., Mönkemüller K. Endoscopic mucosal resection of jejunal polyps using double-balloon enteroscopy. GE Port J Gastroenterol. 2015;22(4):137–142. doi: 10.1016/j.jpge.2015.04.005. Elsevier. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chou J.-W., Feng C.-L., Lai H.-C., Tsai C.-C., Chen S.-H., Hsu C.-H. Obscure gastrointestinal bleeding caused by small bowel lipoma. Intern Med. Jap. Soc. Internal Med. 2008;47(18):1601–1603. doi: 10.2169/internalmedicine.47.0963. [DOI] [PubMed] [Google Scholar]
- 32.Yatagai N., Ueyama H., Shibuya T., Haga K., Takahashi M., Nomura O. Obscure gastrointestinal bleeding caused by small intestinal lipoma: a case report. J Med Case Rep [Internet]. BioMed Central. 2016;10(1):226. doi: 10.1186/s13256-016-1014-4. https://pubmed.ncbi.nlm.nih.gov/27520963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leong C. Ileal volvulus and its association with carcinoid tumours. Aus. Medi. J. 2012;5(6):326–328. doi: 10.4066/AMJ.2012.1239. https://pubmed.ncbi.nlm.nih.gov/22848331 Australas Med J [Internet]. 2012/06/30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alsayegh R.O., Almutairi R., Taqi E., Alnaqi A. Mesenteric lipoma presenting as small bowel volvulus. J Pediatr Surg Case Reports. 2019:43. [Google Scholar]
- 35.Bilgin M., Toprak H., Ahmad I.C., Yardimci E., Kocakoc E. Ileocecal intussusception due to a lipoma in an adult. Case Rep Surg. 2012:684298. doi: 10.1155/2012/684298. https://pubmed.ncbi.nlm.nih.gov/22991683 [Internet]. 2012/09/09. Hindawi Publishing Corporation; 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lin M.-W., Chen K.-H., Lin H.-F., Chen H.-A., Wu J.-M., Huang S.-H. Laparoscopy-assisted resection of ileoileal intussusception caused by intestinal lipoma. J Laparoendosc Adv Surg Tech. Mary Ann Liebert, Inc. 2 Madison Avenue Larchmont, NY 10538 USA. 2007;17(6):789–792. doi: 10.1089/lap.2007.0035. [DOI] [PubMed] [Google Scholar]
- 37.Sheehan E., O'Sullivan G.C. Intussusception in adults: a rare entity. Ir. J. Med. Sci. 2000;2(169):150. doi: 10.1007/BF03166925. [DOI] [PubMed] [Google Scholar]
- 38.Paskauskas S., Pavalkis D. Adult intussusception. Lule G curr concepts colon disord rijeka. Croat InTech. 2012;1–22 [Google Scholar]
- 39.Crocetti D., Sapienza P., Sterpetti A.V., Paliotta A., De Gori A., Pedulla G. Surgery for symptomatic colon lipoma: a systematic review of the literature. Anticancer Res. Int. Ins. Anticancer Res. 2014;34(11):6271–6276. [PubMed] [Google Scholar]
- 40.Nordin A., Freedman J. Laparoscopic versus open surgical management of small bowel obstruction: an analysis of clinical outcomes. Surg Endosc. 2016;30(10):4454–4463. doi: 10.1007/s00464-016-4776-2. Springer. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.