Abstract
Objectives
Sexuality-related preferences have been understudied in contraceptive selection and uptake. Investigators endeavored to assess contraceptive preferences among patients selecting new methods at family planning clinics and to evaluate the degree to which two sexuality-related preferences are (a) valued and (b) associated with method selection.
Study design
Data were derived from the HER Salt Lake Contraceptive Initiative, a longitudinal cohort nested in a quasi-experimental, observational study enrolling 18–45-year-old patients at four family planning health centers in Salt Lake County. At the time of selecting the new method of their choice, participants reported the importance of nine factors in contraceptive method selection, including two sexuality-related preferences: a method's lack of impact on libido and its lack of sexual interruption. Analyses involved multinomial logistic regression with method selected as the outcome, sexuality-related factors as the main explanatory variables, and a range of controls and covariates.
Results
Among 2188 individuals seeking new contraceptive methods, the factors most frequently cited as quite or extremely important were safety (98%), effectiveness (94%), not interrupting sex (81%), not impacting libido (81%) and lack of side effects (80%). Less frequently cited factors included partner acceptability (46%), lack of hormones (39%), friend recommendation (29%) and alignment with religious beliefs (11%). Multivariate models documented no significant associations between sexual-related priorities and method selection.
Conclusions
Many contraceptive seekers rank sexual-related priorities alongside safety and efficacy as very important, but a range of methods align with people's sexual priorities.
Implications
Since patients endorse the importance of sexual-related contraceptive factors (impact on libido, impact on sexual interruption) alongside safety and efficacy, contraceptive research, counseling and care should attend to people's sexuality.
Keywords: Contraceptive preferences, Sexual-related priorities, Patient decision making, Women's sexuality
1. Introduction
Contraceptives improve both public health and individual lives [1,2], but many people use contraceptives inconsistently or not at all due to method dissatisfaction [3], and many stop using their methods after only several months [[4], [5], [6], [7]]. While not inherently negative, discontinuation can be indicative of less-than-ideal method selection due to availability, cost or other barriers. Discontinuation can also flag dissatisfaction with method characteristics or side effects. Researchers have yet to uncover the key characteristics of both current and in-development contraceptive products that affect contraceptive preferences, selection and satisfaction.
Growing research documents that patients have a variety of preferences beyond safety and efficacy that could influence method selection [8,9]. This team's earlier study of 188 intrauterine device (IUD) or implant users indicated that although methods' efficacy influenced contraceptive decision making, so did their potential sexual impacts [10]. When selecting their new method, these patients ranked factors of “doesn't reduce my libido” and “doesn't interrupt sex” just as highly as efficacy and more highly than all other criteria. However, few large-scale studies of this topic exist. We set out to address this gap with a study of over 2000 people seeking the full range of reversible contraceptive services at four family planning clinics.
We hypothesized that (1) contraceptive clients would value sexual-related factors in addition to more established factors such as efficacy and safety and (2) those who place strong value on sexual-related factors would be more likely to choose some methods over others even when controlling for other factors that influence method selection.
2. Methods
2.1. Overview
Data were derived from the HER Salt Lake Contraceptive Initiative, a longitudinal cohort study nested in a quasi-experimental, observational study [11]. Survey-arm recruitment and enrollment occurred from September 2015 to March 2017. Beginning in March 2016, out-of-pocket costs were removed for all reversible contraceptions. Individuals could enroll if they were between the ages of 18 and 45, spoke English or Spanish, were seeking a new contraceptive method at one of four participating family planning health centers in Salt Lake County, UT, and did not want to become pregnant for at least 1 year. This analysis includes only those enrolled during the 1 year of no-cost contraception provision to eliminate the influence of cost barriers on method selection and to reduce a potential source of variability among respondents without adding additional variables to our analyses.
The HER Salt Lake Contraceptive Initiative is registered at ClinicalTrials.Gov (NCT02734199). The University of Utah Institutional Review Board approved the larger project, and each participant provided informed consent to participate in the study. We created, administered and managed surveys through a secure Web-based research electronic data capture, or REDCap, hosted at the University of Utah [12]. Surveys were available in both English and Spanish and could be completed online or over the phone depending on patient preference. This analysis includes data collected during the baseline survey, for which participants received $20 gift cards for completing.
2.2. Procedures and measures
Following the consent process, participants completed baseline surveys online using a computer or tablet in a private area of the health center. This survey contained a variety of sociodemographic questions and baseline health and sexuality measures. Here, we focus on contraceptive preferences. Participants responded to the query, “How important are each of the following characteristics to you in deciding which birth control method to use?” Characteristics included: “it doesn't contain hormones,” “it is acceptable to my partner,” “it doesn't interrupt sex,” “it doesn't reduce my libido,” “it is in line with my religious beliefs,” “it is recommended by my friend(s),” “it is the most effective method,” “it doesn't have side effects” and “it is safe for me to use.” Response options were “not at all important,” “slightly important,” “quite important” and “extremely important.” The sexual-related preferences arose from prior qualitative [13,14], theoretical [15] and clinical pilot work [10] by members of this research team.
In order to control for baseline sexual well-being in multivariate analyses, we included three measures of sexual functioning, sexual satisfaction and sex life ranking. An abridged, six-item version of the Female Sexual Function Index (FSFI-6) [16] measured desire, arousal, lubrication, orgasm and overall satisfaction [17]. The New Sexual Satisfaction Scale (NSSS) measured 20 items meant to identify psychological, partner-related and activity-focused components of sexuality [18]. Finally, to control for people's subjective assessments of their sex lives, we included a 0–100 visual analog scale that assessed respondents' rating of their current sex life. In all three measures, larger values are associated with higher levels of sexual well-being.
2.3. Analyses
At the time of study enrollment, the vast majority (99%) of our sample chose one of six methods: the contraceptive implant, copper IUD, levonorgestrel (LNg) IUD, combined oral contraceptives, vaginal ring and injectable contraception. Other method groups had insufficient sample sizes for method-specific analyses and are excluded from the present analysis.
We conducted all analyses using Stata version 15 [19]. Descriptive analyses documented percentages, means and standard deviations for control variables, covariates and outcomes both for the total sample and by contraceptive method group. χ2 tests and F tests assessed whether people selecting specific methods were significantly different from one another in terms of sociodemographic characteristics. χ2 tests also assessed whether the distribution of people's contraceptive preferences differed by method selected. Finally, we conducted multinominal logistic regressions with the selected method as the outcome and contraceptive factors as the main explanatory variables. The outcome in this regression was the average effect on probability of selecting each method in light of indicating that a contraceptive factor is “quite” or “extremely” important (vs. “somewhat” or “not at all” important). For controls and covariates, we used both sexual functioning and satisfaction measures (FSFI-6, NSSS, etc.) and sociodemographic factors.
3. Results
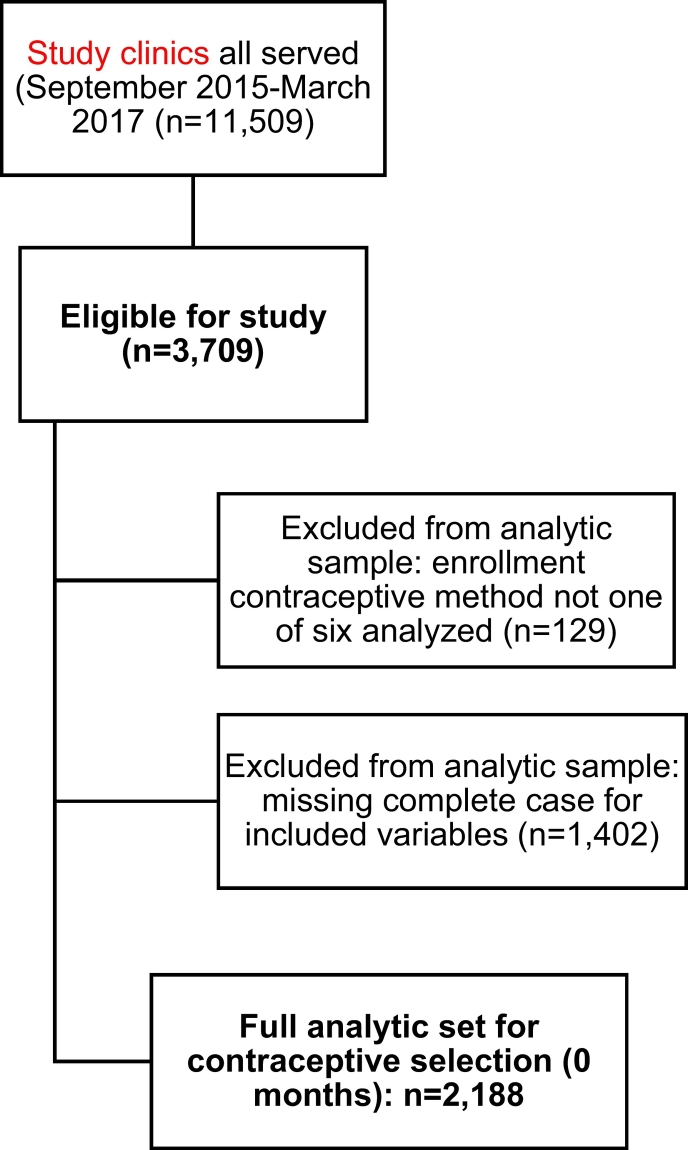
Of the 11,509 contraceptive patients served at four family planning clinics from September 2015 to March 2017, 4425 enrolled in the HER Salt Lake Study. Of these, 2188 were retained in our analytic sample; we excluded those who did not enroll during the no-cost intervention periods, who did not choose one of the six most-selected methods and who were missing data for included variables (Fig. 1).
Fig. 1.
Flowchart of inclusion criteria for analytic sample; new contraceptive clients visiting family planning clinics in Salt Lake County; March 2016 to March 2017.
In terms of method profile, 28% of participants selected LNg IUDs, 21% selected implants, 20% pills, 15% copper IUDs, 11% injectables and 5% vaginal rings (Table 1). In terms of sociodemographic characteristics, one in three participants (34%) identified as people of color (18% Hispanic nonwhite, 16% non-Hispanic nonwhite), 39% had a high school diploma or less, and 39% reported household incomes that were at or below the federal poverty level. The majority were either cohabiting or in a committed relationship with their partner (50%) or married (12%). Approximately three quarters (71%) identified as “exclusively heterosexual”; the remaining 29% claimed another sexual identity. Study participants' mean age was 25. While some factors (age, household size) were significantly associated with method selected, none of the sexual function or satisfaction measures were significantly associated — meaning that baseline sexuality profiles did not appear to influence method selection.
Table 1.
Participant characteristics and criteria for choosing a new contraceptive method, by method selected; new contraceptive clients visiting family planning clinics in Salt Lake County; March 2016 to March 2017; N = 2188
| Totala | LNg IUD | Implant | Combined oral contraceptives | Copper IUD | 3-month injectable | Vaginal ring | p value | |
|---|---|---|---|---|---|---|---|---|
| Method selected, n (%) | 2188 (100.0) | 607 (27.7) | 468 (21.4) | 428 (19.6) | 330 (15.1) | 247 (11.3) | 108 (4.9) | |
| Highest level of education completed (%) | p <.001 | |||||||
| Did not complete high school | 4.7 | 4.3 | 5.3 | 4.7 | 3.0 | 6.1 | 6.5 | |
| HS or GED diploma | 34.1 | 29.7 | 35.5 | 37.6 | 23.6 | 50.2 | 33.3 | |
| Some associate, vocational, technical training or college | 43.3 | 44.8 | 44.2 | 41.4 | 47.9 | 36.4 | 39.8 | |
| Completed 4-year college + | 18.0 | 21.3 | 15.0 | 16.4 | 24.5 | 7.3 | 30.4 | |
| Race and ethnicity (%) | p <.001 | |||||||
| Non-Hispanic white | 66.1 | 73.5 | 62.0 | 64.0 | 69.7 | 57.1 | 61.1 | |
| Hispanic nonwhite | 17.9 | 12.7 | 22.9 | 20.3 | 13.6 | 23.5 | 16.7 | |
| Nonwhite, non-Hispanic other | 16.0 | 13.8 | 15.2 | 15.7 | 16.7 | 19.4 | 22.2 | |
| Current student status (%) | p <.05 | |||||||
| Not a student | 65.6 | 65.7 | 62.6 | 64.7 | 67.0 | 66.4 | 75.0 | |
| Part-time student | 12.0 | 9.4 | 13.7 | 15.9 | 9.7 | 11.3 | 12.0 | |
| Full-time student | 22.4 | 24.9 | 23.7 | 19.4 | 23.3 | 22.3 | 13.0 | |
| Current employment (%) | p = .09 | |||||||
| Unemployed | 12.6 | 10.5 | 13.3 | 15.0 | 9.4 | 16.6 | 13.0 | |
| Working full time | 46.6 | 45.6 | 46.6 | 50.0 | 48.8 | 40.9 | 45.4 | |
| Working part time | 19.5 | 20.4 | 20.5 | 18.9 | 18.5 | 17.4 | 20.4 | |
| Student | 15.2 | 15.8 | 15.0 | 12.6 | 16.7 | 16.2 | 15.7 | |
| Other | 6.1 | 7.6 | 4.7 | 3.5 | 6.7 | 8.9 | 5.6 | |
| Poverty category (%) | p <.001 | |||||||
| At or below poverty level | 39.2 | 35.9 | 39.5 | 40.7 | 32.7 | 55.9 | 32.4 | |
| 101%–200% above poverty level | 28.3 | 28.0 | 26.7 | 32.5 | 29.7 | 23.5 | 27.8 | |
| 201%–300% above poverty level | 20.8 | 21.6 | 20.9 | 19.9 | 22.4 | 17.4 | 23.2 | |
| 301% plus over poverty level | 11.6 | 14.5 | 12.8 | 7.0 | 15.2 | 3.2 | 16.7 | |
| % Reporting unstable housing | 0.9 | 0.7 | 0.9 | 1.2 | 0.3 | 2.0 | 0.0 | p = .24 |
| Relationship status (%) | p = .76 | |||||||
| Married | 12.0 | 13.5 | 13.0 | 10.8 | 11.5 | 10.9 | 7.4 | |
| Cohabiting or committed relationship | 49.5 | 50.1 | 50.0 | 46.7 | 50.9 | 50.6 | 49.1 | |
| Single | 13.3 | 12.9 | 13.9 | 14.5 | 12.1 | 13.4 | 12.0 | |
| Othera | 25.2 | 23.6 | 23.1 | 28.0 | 25.5 | 25.1 | 31.5 | |
| Religion (%) | p = .12 | |||||||
| Not religious | 61.3 | 62.4 | 62.6 | 56.3 | 64.5 | 59.4 | 60.0 | |
| Christian (Protestant or Catholic) | 18.0 | 16.7 | 17.2 | 22.3 | 13.1 | 22.8 | 20.0 | |
| Mormon | 10.5 | 11.0 | 10.4 | 10.7 | 12.2 | 7.8 | 6.0 | |
| Jewish | 0.4 | 0.5 | 0.0 | 0.0 | 0.6 | 1.1 | 1.0 | |
| Muslim | 0.3 | 0.5 | 0.0 | 0.3 | 0.3 | 0.0 | 0.0 | |
| Other | 5.2 | 3.9 | 5.6 | 5.0 | 5.3 | 5.6 | 11.0 | |
| Don't know/prefer not to answer | 4.5 | 5.0 | 4.4 | 5.5 | 4.1 | 3.3 | 2.0 | |
| Heterosexualborientation (%) | 70.5 | 69.2 | 70.9 | 72.9 | 65.5 | 74.1 | 73.2 | p = .18 |
| Age in years,(SD) | 24.9 ± 5.4 | 25.8 ± 5.9 | 23.6 ± 4.5 | 24.1 ± 4.8 | 26.3 ± 5.7 | 24.4 ± 5.4 | 26.6 ± 5.7 | p <.001 |
| Household size,(SD) | 2.5 ± 1.6 | 2.5 ± 1.6 | 2.6 ± 1.6 | 2.5 ± 1.6 | 2.3 ± 1.5 | 2.8 ± 1.9 | 2.3 ± 1.5 | p <.01 |
| On a scale of 1 to 100, how might you rank your sex life right now?(SD) (0–100 scale with 100 being “The best possible”) | 69.6 ± 23.5 | 70.1 ± 22.8 | 69.7 ± 24.1 | 69.2 ± 24.3 | 69.9 ± 22.8 | 69.0 ± 24.6 | 67.5 ± 21.9 | p = .91 |
| FSFI-6(SD) (scale 0–30) | 21.6 ± 6.9 | 21.5 ± 7.1 | 21.3 ± 6.9 | 21.5 ± 7.1 | 22.4 ± 6.6 | 21.6 ± 6.8 | 21.5 ± 6.8 | p = .38 |
| NSSS(SD) (scale 0–80) | 51.0 ± 20.8 | 51.0 ± 20.9 | 51.0 ± 21.1 | 50.8 ± 21.8 | 52.2 ± 19.3 | 50.7 ± 21.0 | 48.9 ± 18.6 | p = .81 |
Data presented are for complete cases, and percentages indicate the column proportion for the specific variable. Descriptive data are presented on the nonimputed original dataset.
Some columns may add to slightly less than or greater than 100% due to rounding adjustments.
Other category includes actively dating, divorced or separated, widowed and other.
Other category includes any category besides “exclusively heterosexual.”
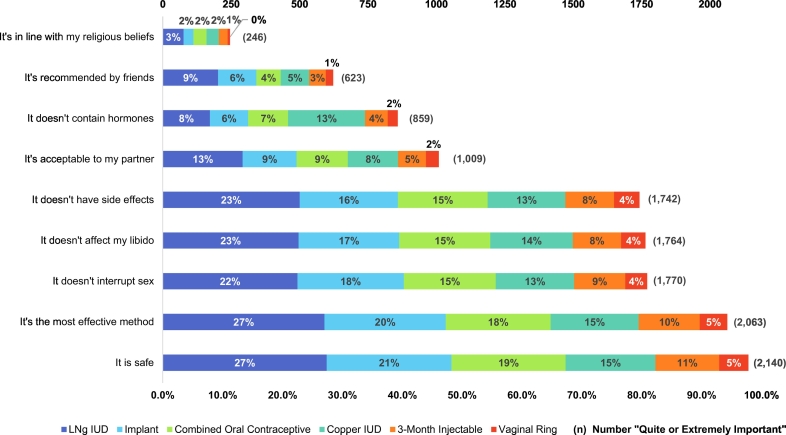
Fig. 2 presents the percent of participants stating that each contraceptive characteristic was either “quite” or “extremely” important to them in deciding which method to use. The contraceptive factors most frequently cited as “quite” or “extremely” important were safety (98%), effectiveness (94%), not interrupting sex (81%), not impacting libido (81%) and lack of side effects (80%). Less frequently cited factors included partner acceptability (46%), lack of hormones (39%), friend recommendation (29%) and alignment with religious beliefs (11%).
Fig. 2.
Quite” or “extremely important” reasons for contraceptive selection, by method selected; new contraceptive clients visiting family planning clinics in Salt Lake County; 2016–2017; N = 2188
We observed slight but significant differences across methods, including within the two sexual-related items. In terms of libido (χ2 p <.001), copper IUD users were proportionally more likely than others to say that not affecting libido was quite or extremely important to them (91% vs. for 72% of injectable users or 78% of pill users, for example) (χ2 p <.01). Copper IUD users were also the most likely to report that a method's lack of sexual interruption was quite or extremely important to them (87% compared to 74% of vaginal ring users and 76% of injectable users, for example; χ2 p <.01). More notable method differences emerged in some non-sexual-related preferences. For example, a far greater proportion of copper IUD users (85%) reported that a method's absence of hormones was quite or extremely important than people choosing other methods (such as 28% of LNg IUD selectors or 34% of pill selectors; χ2 p <.001). In terms of efficacy, over 97% of both types of IUD users and 95% of implant users said efficacy was quite or extremely important compared to 90% of pill users and injectable users and 94% of ring selectors (χ2 p <.001). In other words, efficacy was very important to the overwhelming majority of family planning patients, but particularly so for those people choosing the most effective methods.
Finally, Table 2 presents multinominal logistic regression results with method selected as the outcome and contraceptive preferences as the main explanatory variables. The coefficients in this table represent the average effect of indicating that a contraceptive factor is “quite” or “extremely” important on the probability of selecting each method. Positive numbers indicate that valuing that particular characteristic led to increased probability of selecting that particular method; negative effect sizes represent decreased probabilities of selecting that method. Coefficients range from 0 to 1 or 0 to − 1, with zero equal to no effect and 1 or − 1 the largest possible effect. We consider marginal effect sizes above .01 or below −.01 to be consequential because they reflect a full-unit increase or decrease in the probability of selecting a specific contraceptive method.
Table 2.
Average effect on probability of choosing a new contraceptive method, by method selected; new contraceptive clients visiting family planning clinics in Salt Lake County; March 2016 to March 2017; N = 2188
| Reasons for choosing a new birth control method, “quite or extremely important” relative to “somewhat or not at all important” | LNg IUD |
Implant |
Combined oral contraceptives |
Copper IUD |
3-month injectable |
Vaginal ring |
|---|---|---|---|---|---|---|
| Average effect of choosing “quite or extremely important” on the probability of selecting a method (CI) | ||||||
| It's safe | −.006 | −.079 | .054 | .061 | −.061 | .031 |
| (−.183 to .171) | (−.242 to .084) | (−.047 to .155) | (−.058 to .181) | (−.162 to .039) | (−.008 to .070) | |
| It's the most effective method | .154 | .038 | −.177 | .027 | −.025 | −.017 |
| (.092–.216) | (−.036 to .111) | (−.270 to −.084) | (−.048 to .102) | (−.087 to .037) | (−.065 to .032) | |
| It doesn't interrupt sex | −.038 | .060 | −.004 | .012 | −.001 | −.029 |
| (−.095 to .019) | (.014–.106) | (−.050 to .043) | (−.032 to .056) | (−.038 to .037) | (−.064 to .005) | |
| It doesn't reduce my libido | −.007 | −.013 | −.006 | .031 | −.014 | .009 |
| (−.062 to .048) | (−.064 to .038) | (−.055 to .043) | (−.014 to .076) | (−.053 to .025) | (−.015 to .035) | |
| It doesn't have side effects | .054 | −.007 | −.003 | −.049 | −.013 | .018 |
| (.009–.098) | (−.051 to .037) | (−.045 to .040) | (−.093 to −.004) | (−.048 to .022) | (−.003 to .038) | |
| It is acceptable to my partner | .037 | −.033 | .002 | .006 | −.017 | .005 |
| (−.005 to .079) | (−.072 to .006) | (−.036 to .040) | (−.024 to .036) | (−.047 to .013) | (−.016 to .025) | |
| It doesn't contain hormones | −.160 | −.080 | −.027 | .303 | −.022 | −.015 |
| (−.197 to −.123) | (−.062 to −.048) | (−.062 to .009) | (.267–.339) | (−.051 to .006) | (−.033 to .004) | |
| It's recommended by my friends | .076 | .035 | −.080 | −.013 | −.014 | −.004 |
| (.033–.120) | (−.006 to .076) | (−.116 to to −.045) | (−.042 to .016) | (−.045 to .016) | (−.025 to .018) | |
| It's in line with my religious beliefs | .037 | −.077 | .031 | −.016 | .033 | −.009 |
| (−.026 to .099) | (−.127 to −.026) | (−.030 to .093) | (−.054 to .022) | (−.015 to .082) | (−.038 to .021) | |
Underlined numbers represent significance at the p <.05 value or below.
Coefficients are for null hypothesis of no effect on predicted probability of method selection.
Results are reported as average effects on the probability of method selection using the margins postestimation command in Stata 15.
All models are multinomial logistic, include full sets of control and independent variables, and are run on complete case datasets. The dependent variable is a categorical variable to identify whether that method was selected vs. other methods. Control variables include the household size, percent of federal poverty level, relationship status, race, sexual orientation, employment status, student status, unstable housing conditions, education and age category.
Neither sexual-related preference was significantly associated with choosing some methods over others; other contraceptive preferences were more strongly associated. Individuals who felt it quite or extremely important that their method not contain hormones had a .303 increased probability of selecting the copper IUD (p <.001) and decreased probability of selecting an LNg IUD (effect =−.160, p <.001) or implant (effect =−.080, p <.001). Placing more value on efficacy was positively associated with uptake of LNg IUDs (effect =.154, p <.001) and negatively associated with uptake of pills (effect =−.177, p <.001). Relative importance of friend recommendation was positively associated with uptake of LNg IUDs (effect =.076, p <.001) and negatively associated with uptake of pills (effect =−.080, p <.001). Finally, people who highly valued alignment with their religious beliefs had a decreased probability of selecting implants (effect =−.077, p <.01).
4. Discussion
In this study of over 2000 contraceptive clients at the time of method selection, we found convincing evidence to support our first hypothesis: people value sexual-related factors in addition to more well-studied factors. While nearly all participants valued efficacy and safety in selecting their selection, a substantial majority also wanted their contraceptive method to work with, not against, their sex lives — in particular, by not reducing their libido and by not interrupting the sexual flow. Findings suggest that patient concerns about sexuality are an important part of contraceptive decision making — regardless of the method they end up choosing.
Other research suggests that many individuals strongly value sexual-related characteristics of contraceptives [9]. For example, in a study of family planning and abortion clinic patients, 68% of 1783 participants said it was “extremely important” that a “method doesn't detract from my sexual enjoyment” [8]. In their development of a contraceptive decision-making aid, Jamin et al. found that “effect on sexual pleasure,” “effect on intimacy/spontaneity/libido” and “level of sexual activity” emerged as key factors influencing contraceptive choice [20].
Despite the striking evidence that family planning patients in this study placed value on sexual-related characteristics, we were also struck by the lack of association between sexual priorities and method selection. Individuals who placed higher value on libido and sexual interruption characteristics did not unilaterally select particular methods over others. Findings suggest that a variety of methods can meet people's needs, sexually and otherwise. Moreover, there can be downsides, sexually and otherwise, to all available methods. In other words, patients should not be steered toward particular methods; they should be encouraged to select methods they believe will work for them sexually, whatever that entails.
A 2012 study found that, for 91% of women, no single method had all the features that an individual selected as “extremely important” [21]. Other nonsexual contraceptive preferences also lacked strong predictive relationships to specific method uptake. In other words, patients with the exact same contraceptive-characteristic preference profiles can select different methods for a variety of reasons, both measurable and nonmeasurable. That said, our findings also indicate that at least some people are making contraceptive choices consistent with their desires. For example, efficacy was very important to the overwhelming majority of family planning patients but particularly so for those people choosing the most effective methods.
Study findings underscore the importance of person-centered approaches to contraception. A variety of methods can meet individuals' contraceptive needs. We would caution against clinical protocols that direct all patients with certain preference profiles to one method over others, as well as guidelines that promote methods based on one characteristic alone (e.g., efficacy). Family planning patients hold a variety of contraceptive preferences and needs. Retaining and developing a “deep bench” or various contraceptive products are critical to meeting people's contraceptive needs.
Findings also have implications for contraceptive counseling. Sexual acceptability of contraceptive methods is rarely discussed during contraceptive counseling or clinical care visits, and researchers have underscored the need for more research on the intimate sexual contexts in and for which people make contraceptive decisions [22]. Given that many contraceptive-seeking patients rank sexuality as a strong priority alongside safety and efficacy, future efforts should better integrate sexuality into contraceptive education and selection.
Our survey instrument refrained from asking participants to rank their priorities relative to one another. Top priorities would likely be more significantly associated with method selection than observed here. Further, although we included nine contraceptive features in our assessment, patients could well have other, unobserved contraceptive preferences. Our item on libido was phrased in the negative (i.e., “doesn't reduce my libido”), which may have led a greater number of people to place importance on libido than if the item had been phrased neutrally (i.e., “doesn't affect my libido”). While the overwhelming majority of our sample selected one of six methods, analyses did not include other devices, most notably male condoms [23]. Although only 0.2% of patients selected condoms as their contraceptive method, condoms are a vital tool in the dual prevention of unwanted pregnancy and sexually transmitted infections [24].
In terms of generalizability of findings, it is likely that people in Utah overall differ meaningfully from the average U.S. resident seeking contraception. However, Salt Lake City has a more racially, socioeconomically and religiously diverse population than Utah overall [25]. For example, 26% of Salt Lake City inhabitants are people of color compared to 9% in Utah and 24% in the larger US [25]. Only 11% of respondents in our sample identified as Mormon, and 61% said they were not religious.
While efficacy and safety concerns matter in contraceptive selection, an overwhelming majority of contraceptive patients also value sexual-related contraceptive factors. A variety of methods can meet people's sexual needs, underscoring the importance of person-centered contraceptive development, counseling and care.
Acknowledgments
Acknowledgments
This analysis was funded by a National Institutes of Health (NIH) award (R01 HD095661) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Support for the HER Salt Lake Contraceptive Initiative comes from The Society of Family Planning Research Fund, The William and Flora Hewlett Foundation: Grant # 2018-7892, and an anonymous foundation. The following companies contributed contraceptive products for the project: Bayer Women's Healthcare: grant number 2015-025, Merck & Co. Inc: grant number 52689. and Teva Pharmaceuticals: grant number 20151027. The authors also acknowledge support from two NICHD Population Research Infrastructure grants (P2C HD047873 for University of Wisconsin; the Building Interdisciplinary Researchers in Women's Health K12 HD085852 for University of Utah). Study data were collected and managed using REDCap (Research Electronic Data Capture) hosted at the University of Utah; this service is supported by Center for Clinical and Translational Sciences grant 8UL1TR000105 (formerly UL1RR025764, National Center for Advancing Translational Sciences, NIH). Preliminary findings were presented at the Society of Family Planning's annual North American Forum on Family Planning, October 20–22, 2018, New Orleans. The authors thank the clinic staff at the four recruiting family planning clinics for their critical work in making the study a success. This content is solely the responsibility of the authors and does not necessarily represent the official view of any of the funding agencies or participating institutions, including the NIH, the University of Wisconsin-Madison, the University of Utah and the Planned Parenthood Federation of America, Inc.
Conflict of interest
The authors do not report any potential conflicts of interest. In this investigator-initiated project, research costs were covered by grants from federal agencies, private foundations and a research fund belonging to a professional family planning society. Some contraceptive products used in the study were donated by pharmaceutical companies. The family planning clinics, not the investigators, managed these contraceptive devices. All aspects of the study were investigator versus industry initiated. The authors take responsibility for the presentation and publication of the research findings, have been fully involved at all stages of publication and presentation development and are willing to take public responsibility for all aspects of the work.
Footnotes
Declarations of interest: none.
Clinical trials registration number: ClinicalTrials.gov, www.clinicaltrials.gov, NCT02734199.
Contributor Information
Jenny A. Higgins, Email: jenny.a.higgins@wisc.edu.
Kelsey Q. Wright, Email: kwright22@wisc.edu.
David K. Turok, Email: david.turok@hsc.utah.edu.
Jessica N. Sanders, Email: jessica.sanders@hsc.utah.edu.
References
- 1.Sonfield A., Hasstedt K., Kavanaugh M.L., Anderson R. The Guttmacher Institute; New York: 2013. The social and economic benefits of women’s ability to determine whether and when to have children. [Google Scholar]
- 2.Kavanaugh M.L., Anderson R. The Guttmacher Institute; New York: 2013. Conception and beyond: the health benefits of services provided at family planning centers. [Google Scholar]
- 3.Severy L.J., Newcomer S. Critical issues in contraceptive and STI acceptability research. J Soc Issues. 2005;61:45–65. [Google Scholar]
- 4.Simmons R.G., Sanders J.N., Geist C., Gawron L., Myers K., Turok D.K. Predictors of contraceptive switching and discontinuation within the first six months of use among HER Salt Lake study participants. Am J Obstet Gynecol. 2018;220(4):376.e1–376.e12. doi: 10.1016/j.ajog.2018.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peipert J.F., Zhao Q., Allsworth J.E. Continuation and satisfaction of reversible contraception. Obstet Gynecol. 2011;117:1105–1113. doi: 10.1097/AOG.0b013e31821188ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Raine T.R., Foster-Rosales A., Upadhyay U.D. One-year contraceptive continuation and pregnancy in adolescent girls and women initiating hormonal contraceptives. Obstet Gynecol. 2011;117:363–371. doi: 10.1097/AOG.0b013e31820563d3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murphy P.A., Brixner D. Hormonal contraceptive discontinuation patterns according to formulation: investigation of associations in an administrative claims database. Contraception. 2008;77:257–263. doi: 10.1016/j.contraception.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 8.Jackson A.V., Karasek D., Dehlendorf C., Foster D.G. Racial and ethnic differences in women’s preferences for features of contraceptive methods. Contraception. 2016;93:406–411. doi: 10.1016/j.contraception.2015.12.010. [DOI] [PubMed] [Google Scholar]
- 9.Walker A.W., Stern L., Cipres D., Rodriguez A., Alvarez J., Seidman D. Do adolescent women’s contraceptive preferences predict method use and satisfaction? A survey of Northern California family planning clients. J Adolesc Health. 2019;64(5):640–647. doi: 10.1016/j.jadohealth.2018.10.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Higgins J.A., Sanders J.N., Palta M., Turok D.K. Women’s sexual function, satisfaction, and perceptions after starting long-acting reversible contraceptives. Obstet Gynecol. 2016;128:1143–1151. doi: 10.1097/AOG.0000000000001655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sanders J.N., Myers K., Gawron L.M., Simmons R.G., Turok D.K. Contraceptive method use during the community-wide HER Salt Lake Contraceptive Initiative. Am J Public Health. 2018;108:550–556. doi: 10.2105/AJPH.2017.304299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap) — a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Higgins J.A., Hirsch J.S. Pleasure, power, and inequality: incorporating sexuality into research on contraceptive use. Am J Public Health. 2008;98:1803–1813. doi: 10.2105/AJPH.2007.115790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Higgins J.A., Ryder K., Skarda G., Koepsel E., Bennett E.A. The sexual acceptability of intrauterine contraception: a qualitative study of young adult women. Perspect Sex Reprod Health. 2015;47:115–122. doi: 10.1363/47e4515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Higgins J.A., Smith N.K. The sexual acceptability of contraception: reviewing the literature and building a new concept. J Sex Res. 2016;53:417–456. doi: 10.1080/00224499.2015.1134425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Isidori A.M., Pozza C., Esposito K. Development and validation of a 6-item version of the female sexual function index (FSFI) as a diagnostic tool for female sexual dysfunction. J Sex Med. 2010;7:1139–1146. doi: 10.1111/j.1743-6109.2009.01635.x. [DOI] [PubMed] [Google Scholar]
- 17.Rosen R., Brown C., Heiman J. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26:191–208. doi: 10.1080/009262300278597. [DOI] [PubMed] [Google Scholar]
- 18.Stulhofer A., Busko V., Brouillard P. Development and bicultural validation of the new sexual satisfaction scale. J Sex Res. 2010;47:257–268. doi: 10.1080/00224490903100561. [DOI] [PubMed] [Google Scholar]
- 19.StataCorp . StataCorp LLC; College Station, TX: 2017. Stata statistical software: release 15. [Google Scholar]
- 20.Jamin C.G., Hausler G., Lobo Abascal P. Development and conceptual validation of a questionnaire to help contraceptive choice: CHLOE (Contraception: HeLping for wOmen’s choicE) Eur J Contracept Reprod Health Care. 2017;22:286–290. doi: 10.1080/13625187.2017.1364719. [DOI] [PubMed] [Google Scholar]
- 21.Lessard L.N., Karasek D., Ma S. Contraceptive features preferred by women at high risk of unintended pregnancy. Perspect Sex Reprod Health. 2012;44:194–200. doi: 10.1363/4419412. [DOI] [PubMed] [Google Scholar]
- 22.Dehlendorf C., Krajewski C., Borrero S. Contraceptive counseling: best practices to ensure quality communication and enable effective contraceptive use. Clin Obstet Gynecol. 2014;57:659–673. doi: 10.1097/GRF.0000000000000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Higgins J.A., Smith N.K., Sanders S.A. Dual method use at last sexual encounter: a nationally representative, episode-level analysis of US men and women. Contraception. 2014;90:399–406. doi: 10.1016/j.contraception.2014.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Higgins J.A., Cooper A.D. Dual use of condoms and contraceptives in the USA. Sex Health. 2012;9:73–80. doi: 10.1071/SH11004. [DOI] [PubMed] [Google Scholar]
- 25.United States Census Bureau. US census state and county quickfacts (https://www.census.gov/quickfacts/fact/table/saltlakecitycityutah,US/PST045218). 2018.