Abstract
Objective
Spondylolysis is 1 of the most common sources of low back pain in children and adolescents; however, there is still a great deal of confusion in regard to etiology, clinical presentation, and diagnostic imaging findings. It is imperative for clinicians to recognize that persistent low back pain is strongly indicative of spondylolysis, especially in high-performance athletes. This case series demonstrates a comprehensive diagnostic spectrum of spondylolysis and its treatment in 2 competitive adolescent cheerleaders.
Clinical Features
In case 1, a 12-year-old female competitive cheerleader presented with a gradual onset of subacute low back pain. Comprehensive clinical examination indicated imaging studies that identified bilateral L5 grade 1 stress reaction, consisting of neural arch bone marrow edema (BME). Treatment included spinal adjustments, rehabilitation, and myofascial therapy. In case 2, 15-year-old female competitive cheerleader presented with insidious chronic low back pain that was provocative with extension. Magnetic resonance imaging revealed a left L5 grade 1 pars interarticularis stress reaction. Computed tomography demonstrated right L5 pars grade 3 and left L5 healing spondylolysis. Treatment included spinal adjustments and rehabilitation exercises. She was also seen by a physical therapist who prescribed a lumbar spine flexion brace.
Intervention and Outcome
Diagnosis of BME and spondylolysis led to temporary cessation of cheerleading activities in cases 1 and 2. The individual in case 1 self-discharged with a list of rehabilitation exercises and was lost to follow-up. The individual in case 2 was able to return to sport pain free approximately 5 weeks after seeking treatment.
Conclusion
Spondylolysis is common in adolescent athletes, and the presence of BME precedes spondylolysis. Primary spine providers could consider this diagnosis in any adolescent, especially an athlete, who has persistent low back pain. Timely diagnosis will optimize treatment outcomes.
Key Indexing Terms: Spondylolysis, Adolescent, Magnetic Resonance Imaging, Tomography, Emission-Computed, Single-Photon, Manipulation, Spinal
Introduction
Spondylolysis is a common source of low back pain in the pediatric population.1,2 Spondylolysis is an osseous defect of the par interarticularis resulting from microtrauma caused by repetitive hyperextension and rotational loading of the spine.1,3, 4, 5, 6 The microtrauma subsequently provokes intraosseous bone marrow edema (BME) in the neural arch. The prevalence of spondylolysis has been reported as approximately 4.4% of children and adolescents.5,7, 8, 9 A higher prevalence of spondylolysis is present in competitive cheerleaders and gymnasts.9, 10, 11
Low back pain with extension is the most common clinical finding.3,12 The pain may start as a dull ache and gradually increase in intensity. Low back pain that persists beyond 2 weeks, and worsens with extension, should raise suspicion of spondylolysis.4 Imaging modalities commonly used to evaluate and diagnose spondylolysis may include lumbar spine radiography with oblique views, magnetic resonance imaging (MRI), and computed tomography (CT). Bone marrow edema is associated with many pathologies, but is known to precede spondylolysis. BME is now being recognized not only as a pain generator but also as being linked to worsening patient prognosis with certain disorders, including spondylolysis.6,13 Altered or increased mechanical stress to bone is a significant source of BME and pain.13 Single-photon emission CT (SPECT) or skeletal scintigraphy could also be used for the diagnosis of spondylolysis.14
Early diagnosis is key for treatment and quality outcomes. The goals of treatment are prevention of progression, healing of spondylolysis, and return to sport.1 This case series demonstrates the diagnostic and treatment spectrum of spondylolysis in 2 competitive adolescent cheerleaders, case 1 with subacute and case 2 with chronic spondylolysis. This case series emphasizes an MRI grading system for spondylolysis. Parents/Guardians of all patients provided consent to have the case information published in this case series.
Case Report: Methods and Results
Case 1
A 12-year-old female competitive cheerleader presented to our chiropractic teaching clinic with low and mid back pain that began gradually 3 weeks prior. She denied a history of acute trauma. Initially, she rated her low back pain at 3 out of 10, with 0 being absence of symptoms and 10 being very severe or unbearable. Her pain was dull and achy, with stiffness but no radiation. Her mid back pain was rated 2 out of 10 and was described as aching and stiff. Pain levels fluctuated with the extent of tumbling or cheering activity. Tumbling and back walkovers (extension) exacerbated her pain. Her medications included methylphenidate for attention-deficit/hyperactivity disorder. Her parents denied any additional relevant personal or family history.
Upon physical examination, vital signs were within normal limits. Postural findings consisted of bilaterally rounded shoulders, mildly increased lumbar lordosis, and anterior head carriage. Orthopedic examination revealed a positive Yeoman test on the right and Thomas test bilaterally. Segmental dysfunction in the pelvis (right sacroiliac joint), lumbar (L1/L2), and thoracic spine (T12/L1 and T4/T5) was noted with associated muscular hypertonicity of the erector spinae and psoas muscles. Provocation of pain was re-created with active extension and demonstration of a back walkover. At rest, she experienced mild low back pain.
The patient was initially diagnosed with segmental dysfunction of the thoracic and lumbar spine and the pelvis. She was scheduled for treatment once a week for 1 month. The patient consistently responded to care. She indicated withdrawal of symptoms with each spinal adjustment, clinic rehabilitation exercises, and myofascial therapy. Orthopedic examinations were used as necessary with each episode of care, and positive responses resolved subsequent to the treatment.
Two weeks into the patient care plan, she participated in a 2-day cheering competition. After this competition, she started experiencing sharp pain in her low back, which radiated down the left leg, with occasional right leg radiation. A forward flexed posture relieved her radiating pain. Evaluation revealed a positive Bonnet test on the right and right S1 deep tendon reflex of +1; all other orthopedic and neurologic testing was within normal limits. Palpation demonstrated bilateral hamstring and piriformis tension and tenderness. The radiating symptoms into the patient's left leg were reproduced with palpation of the piriformis.
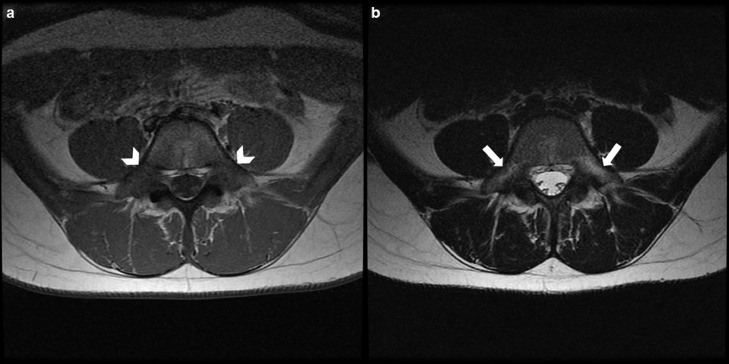
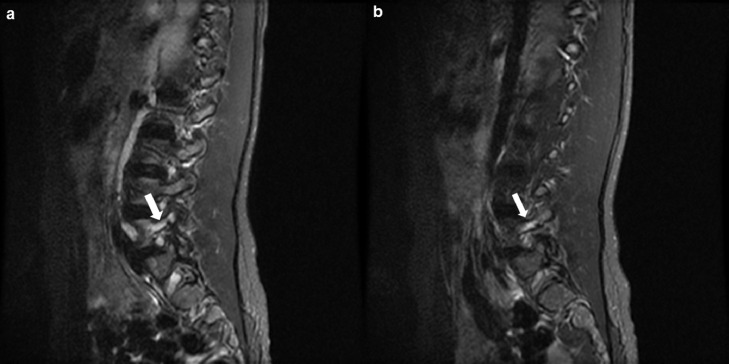
In light of her root signs, a 5-view lumbar spine series was obtained (not shown). No spondylolysis was identified. In addition, the examination revealed a type IV lumbosacral transitional segment and 6 non–rib-bearing lumbar vertebrae. Her differential diagnosis also included spondylolysis. A lumbar spine MRI was performed 1 week later. It demonstrated bilateral L5 pars interarticularis high signal intensity on T2-weighted imaging. There was corresponding low signal intensity on T1-weighted imaging in the axial plane (Fig 1A and 1B). High signal intensity was also identified on the STIR sequences of the left (Fig 2A) and the right (Fig 2B) L5 pars interarticularis. This finding was consistent with a grade 1 stress reaction demonstrating BME and associated stress injury.9 No fracture line was noted.
Fig 1.
Magnetic resonance imaging axial T1-weighted image demonstrated low signal intensity (white arrowheads) bilaterally at the L5 pars interarticularis (A). Axial T2-weighted image demonstrated high signal intensity (white arrows) at the L5 pars, which indicated bilateral grade 1 stress reactions, consisting of neural arch bone marrow edema (B).
Fig 2.
Magnetic resonance imaging left parasagittal STIR sequence demonstrated high signal intensity at the L5 pars interarticularis (A; white arrow). Right parasagittal STIR also demonstrated high signal intensity at the L5 pars (B; white arrow). This is consistent with a bilateral grade 1 stress reaction, demonstrating neural arch bone marrow edema.
Management recommendations included cessation of gym and cheer practice to permit healing of her L5 stress reaction. Chiropractic care was discontinued because the patient self-discharged, cheerleading activities were temporarily ceased, and rehabilitation exercises were recommended to be performed at home. The patient was lost to follow-up.
Case 2
A 15-year-old female competitive cheerleader presented to our chiropractic teaching clinic with insidious low back pain that began 1 and a half years earlier. An increase in low back pain occurred after participating in gymnastics and was provoked with jumping, running, and back walkovers. She denied any history of acute trauma or radiation with her low back complaint. Her pain was located at the lumbosacral junction, rating 3 out of 10 on the pain scale. The pain was described as a discomfort or ache.
Results of orthopedic and neurologic examinations were within normal limits. Provocation of pain occurred with active range of motion: flexion, returning to neutral with flexion, left rotation, and returning to neutral from right lateral bending. Passive and resisted range of motion were pain free and within normal limits. Segmental dysfunction was found in the pelvis (right sacroiliac joint) and lumbar (L4/L5) spine. Manual muscle testing revealed weakness of the hips in flexion at 30°. The patient and her parents denied any significant family history, aside from essential hypertension in maternal and paternal grandparents and her father with a history of essential hypertension and hypercholesterolemia.
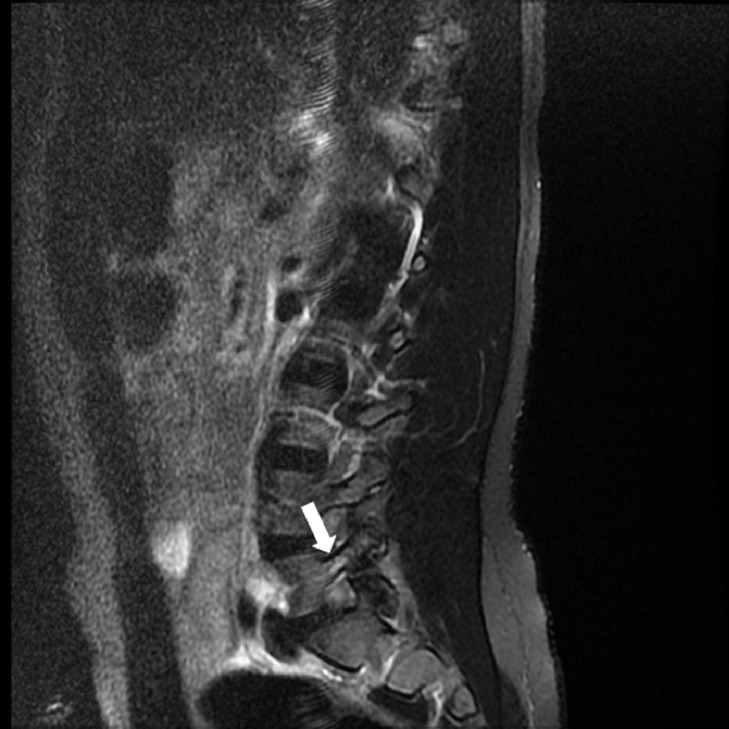
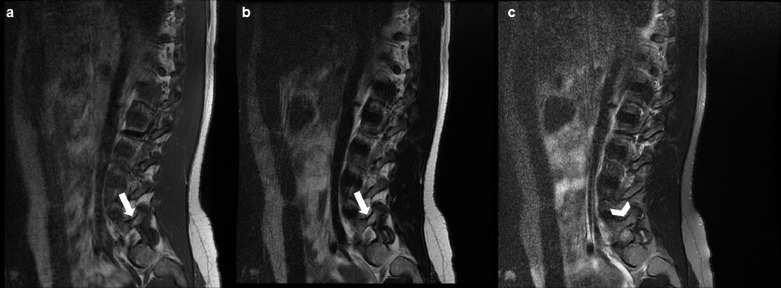
Outside imaging studies consisted of a lumbar MRI and CT, which were reviewed by the radiology department. An MRI was performed at her initial onset of low back pain, 1 and a half years earlier. The MRI revealed a low T1-weighted signal intensity and high signal intensity on fluid sequences within the left L5 pars interarticularis and neural arch (Fig 3). This finding was consistent with a grade 1 stress reaction, indicating active BME. There was high signal intensity noted in the right L5 pars interarticularis on T1- and T2-weighted sequences that was suppressed on the fat saturation. These findings indicated fatty marrow infiltration, likely in response to spondylolysis (Fig 4A-C). The MRI findings noted were consistent with L5 spondylolysis. A physical therapist prescribed a lumbar brace, directed the patient to limit repetitive activities, and referred her for rehabilitative care.
Fig 3.
Magnetic resonance imaging sagittal T2-weighted image demonstrated high signal intensity at the left L5 pars interarticularis (white arrow). There was corresponding low signal intensity on the T1-weighted image (not pictured). This indicated a grade 1 stress reaction with bone marrow edema.
Fig 4.
Magnetic resonance imaging right parasagittal T1-weighted (A) and T2-weighted (B) images demonstrated high signal intensity within the L5 pars interarticularis (white arrows). Right parasagittal T2-weighted image with fat suppression demonstrated that the high signal intensity was reduced on fat saturation, suggesting fatty marrow infiltration in response to the defect of the pars interarticularis (C; white arrowhead).
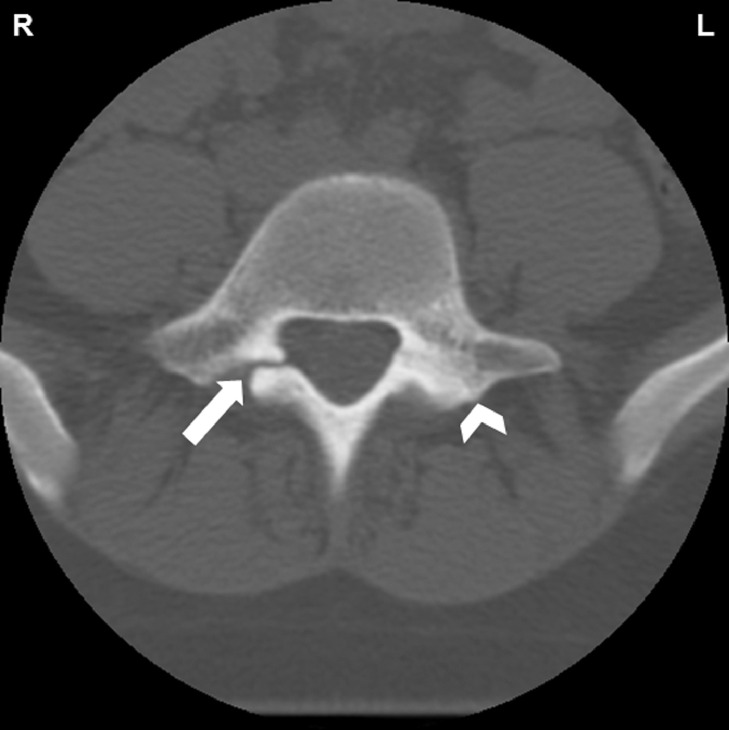
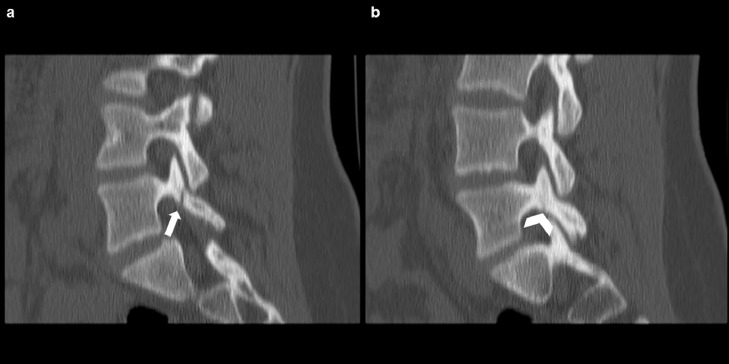
The patient continued to experience lumbar spine pain for another 8 months, and a CT examination was ordered. Axial images revealed a complete radiolucent defect of the right L5 pars interarticularis with adjacent smooth cortices and sclerosis (Fig 5). These findings correlate with a grade 3 stress fracture. In addition, there was remodeling and sclerosis without defect in the left L5 pars interarticularis (Fig 5). Sagittal CT reconstruction findings were consistent with an L5 right spondylolysis and a healing L5 left spondylolysis (Fig 6A and 6B). No spondylolisthesis was observed.
Fig 5.
Computed tomography reconstructed axial plane of the L5 vertebral body and posterior elements. Complete spondylolysis of the right pars interarticularis (white arrow) indicated a grade 3 complete active fracture. There was reactive sclerosis in the left pars (white arrowhead), which indicated healing of the spondylolysis.
Fig 6.
Computed tomography. Right parasagittal plane demonstrated a grade 3 complete spondylolysis (active fracture) of the L5 pars interarticularis (A; white arrow). Left parasagittal plane demonstrated healing of the spondylolysis in the L5 pars (B; white arrowhead).
A diagnosis of spondylolysis was obtained based on the clinical examination and the imaging studies. Additionally, the patient was diagnosed with segmental dysfunction of the lumbar spine, pelvis, and lower extremities. Treatment was scheduled for twice a week for 2 weeks and once a week for a duration of 4 weeks.
Treatment consisted of adjustments in the pelvis and lumbar spine along with myofascial therapy of associated areas (lumbar spine erector spinae, quadratus lumborum, and psoas). Clinical rehabilitative exercises were prescribed as needed.
One week after re-evaluation, she presented with low back pain on the left without radiation but had pain with extension. Pain that was provoked by lumbar extension was reduced following pelvic adjustments. Spinal adjustments, myofascial therapy, and exercises were continued, as they reduced pain and increased performance capability. In approximately 5 weeks, she was able to return to sport with no pain.
Discussion
Today, many cheerleaders have increased the level of performance in their sport. Not only do they perform basic cheering maneuvers, but they also perform gymnastic tumbling and partner stunts. The increase in difficulty and number of repetitive maneuvers has increased the prevalence of cheerleading injuries.15,16 Cheerleading and gymnastics are year-round sports that involve repetitive jumping and landing, which causes high skeletal stress and limited potential for healing. Competitive adolescent female athletes may be at greater risk of developing spondylolysis as a result of high-impact movement and training demands, cheering on harder surfaces, and effects of hormonal changes.11,16,17 Schroeder et al conclude that athletes have a higher prevalence of spondylolysis compared with nonathletes.18
Spondylolysis, a common cause of low back pain in children and adolescents (especially athletes), results from repetitive hyperextension and rotational stress placed upon the spine.1, 2, 3, 4,7,12,19,20 Isthmic spondylolysis most commonly involves the L5 pars interarticularis, often bilaterally.3,5,21 Spondylolysis in children and adolescents occur as a stress fracture at the caudal-ventral aspect of the pars due to tensile stresses being higher in the ventral aspect than the dorsal.20,22,23 Labelle et al24 determined that patients with L5 spondylolysis show significantly greater pelvic incidence and sacral slope, which appears to play a role in spondylolysis.25 Kim et al suggest that body mass index and adjacent disc and facet degeneration may be associated factors in the manifestation of symptomology in young adults with L5 spondylolysis, and that individuals with more severe L5-S1 disc degeneration are more likely to exhibit symptoms.26
The spectrum of spondylolysis and its progression from BME is a complex set of pathomechanical events. Dunn et al propose a 4-stage evolution of pars interarticularis fractures that has been described for MRI and is listed in Table 1.9 Initially, a stress reaction (pending spondylolysis) includes intraosseous edema with sclerosis of the pars, lamina, or pedicle without cortical disruption. This is the earliest stage, equivalent to a grade 1 stress reaction. The MRI in case 1 revealed a bilateral grade 1 stress reaction. The MRI in case 2 demonstrated a left L5 grade 1 stress reaction. Stress fractures (spondylolysis) include BME and incomplete disruption of cortical bone of the pars interarticularis. This is the intermediate stage, consistent with a grade 2 stress fracture. Grade 3 is the progression of the stress reaction, including a complete fracture and gap. The CT in case 2 demonstrated a right L5 grade 3 complete fracture. Nonunion, sclerosis, and absence of BME characterize the terminal stage, grade 4.6,9,12,14,19,22,27 This MRI grading system of pars interarticularis stress fractures correlates well with CT and SPECT. Diagnosis of a grade 2 (incomplete) or grade 3 (complete) acute pars interarticularis stress fracture is important, because fracture healing may be accomplished with appropriate clinical management.9 Regardless of the magnitude of pars involvement (stress reaction, spondylolysis, or spondylolisthesis), a correct diagnosis is imperative because misdiagnosis can lead to progression and permanent disability.11,12
Table 1.
MRI Grading System for Stress Fractures of the Pars Interarticularis9
| Grade | Description | MRI Features |
|---|---|---|
| 0 | Normal | Normal marrow signal Intact cortical margins |
| 1 | Stress reaction | Marrow edema Intact cortical margins |
| 2 | Incomplete fracture | Marrow edema Cortical fracture incompletely extends through pars |
| 3 | Complete active fracture | Marrow edema Fracture completely extends through pars |
| 4 | Fracture nonunion | No marrow edema Fracture completely extends through pars |
Common clinical presentation for spondylolysis includes mild to moderate low back pain, with occasional radiating pain into the buttock or posterior thigh.1,10,11 Antalgic gait may be sporadic in individuals with more acute symptoms.1,11 Low back pain may be reproduced by the standing single-legged hyperextension test.10,12
When spondylolysis is suspected, radiography of the lumbar spine, including obliques, is often the first imaging modality.1,3,14,27 Radiography is advantageous because it is inexpensive and provides a low dose of ionizing radiation in a susceptible pediatric population.14 However, radiography has no sensitivity for detecting BME in a grade 1 stress reaction.27 When radiography is negative, MRI should be the next step in the imaging examination.2,4,14 MRI has shown abnormal high signal intensity, representing BME, in the pars interarticularis of pending or acute spondylolysis. This finding was reported in case 1. Additionally, the use of ionizing radiation is avoided.1,2,9,14,20,27
Early detection and diagnosis of BME is enabled by MRI, which provides recognition of a pending spondylolysis before it progresses to a complete pars interarticularis stress fracture (spondylolysis).2,6,10 Primary spine care providers are often the first to evaluate adolescent patients with acute low back pain. In addition, office-based advanced imaging is not typically available. Therefore, stress reactions or spondylolysis may not be confirmed.2 Primary spine care providers should recognize that approximately 40% of pediatric patients presenting with low back pain persisting beyond 2 weeks will have a spondylolysis. For that reason, MRI should be an imaging consideration, especially in athletes with a history of acute or subacute low back pain.2,4
Options for advanced imaging in spondylolysis include CT, SPECT, and skeletal scintigraphy.1 Computed tomography is best at assessing skeletal morphology, cortical integrity, and occult fractures, and establishing the extent of healing in spondylolysis.4,14,21,27 A major disadvantage of CT is ionizing radiation, which is substantial in a vulnerable, still-growing population.21 Also, CT cannot demonstrate a stress reaction when one is present, or reliably distinguish between recent active fractures and chronic nonunion.9 SPECT can be useful in detecting spondylolysis in symptomatic athletes whose radiographic or scintigraphic examinations appear normal.11,27 The concern is the dose of ionizing radiation. Skeletal scintigraphy also involves a significant radiation dose, and furthermore displays low specificity. However, it is quite sensitive in the detection of spondylolysis and its phases of healing.14 A controversial study has suggested similar diagnostic accuracy of MRI to CT in the diagnosis of spondylolysis, although this view is not generally shared.21 Computed tomography, however, is widely regarded as the gold standard for accurate diagnosis of spondylolysis.9,21 Other studies have suggested that if further diagnostic certainty is required, MRI should be used early in the diagnosis and CT should be used in more persistent cases of low back pain, as in case 2.14,27
First-line treatment of spondylolysis is conservative care. Adolescent athletes usually respond well to conservative treatment.11 Chiropractic adjustments may be used in the absence of contraindications to provide pain relief.5 Symptomatic athletes should refrain from hyperextension activities and sports until they are pain free, which may take a few days to 6 months.4,10,11 The majority of spondylolysis patients respond to lumbar bracing, rest, rehabilitation, and gradual return to their sport.4,11,12,22 Rehabilitation exercises may include routine hamstring stretches to improve flexibility, which can influence daily lumbar spine movement and posture, along with abdominal core-strengthening exercises.5,28 Additionally, the following considerations would be advisable in cheerleading to reduce the incidence of spondylolysis: Practice should promote varied training routines in order to decrease the cumulative total of high-impact activities, avoid stunts and tumbling on hard surfaces, and use specific guidelines for execution of technically demanding skills.16,17
Indications for surgical management include patients not responding to conservative care after 6 months and those with continued progression of spondylolysis.1,11 Pars interarticularis repair methods have been used in an attempt to spare spinal motion segments and minimize spinal fusion.29 These surgical methods include direct pars repair with cortical screws and indirect pars repair with posterior wiring.29 Return to sport is approximately 6 months after the surgical intervention.29
The goal of treatment is prevention of progression, healing of spondylolysis, and return to sport.1 Return to sport is permitted once the athlete demonstrates a consistent reduction in the visual analog scale and an unremarkable physical examination and has completed rehabilitation.10
Conclusion
Spondylolysis is common in adolescent athletes, and BME precedes its development. Primary spine providers should contemplate this diagnosis in any adolescent, especially athletes, who have persistent low back pain. The use of appropriate diagnostic imaging will facilitate a timely and accurate diagnosis, ensuring complete and accelerated recovery.
Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
Contributorship Information
Concept development (provided idea for the research): A.N.R., N.W.K.
Design (planned the methods to generate the results): A.N.R., N.W.K.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): N.W.K.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): C.B.W.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): C.B.W.
Literature search (performed the literature search): A.N.R.
Writing (responsible for writing a substantive part of the manuscript): A.N.R.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): A.N.R., S.M.C., C.B.W., N.W.K.
Practical Applications.
-
•
Persistent low back in an adolescent, especially an athlete, may reflect increasing incidence of spondylolysis.
-
•
Early identification and classification of spondylolysis can lead to optimal outcomes.
-
•
Spinal adjustments, myofascial therapy, and rehabilitative exercises can lead to reduced pain and increased performance capability.
Alt-text: Unlabelled box
References
- 1.Herman MJ, Pizzutillo PD, Cavalier R. Spondylolysis and spondylolisthesis in the child and adolescent athlete. Orthop Clin North Am. 2003;34(3):461–467. doi: 10.1016/s0030-5898(03)00034-8. [DOI] [PubMed] [Google Scholar]
- 2.Nitta A, Sakai T, Goda Y, Takata Y, Higashino K, Sakamaki T, Sairyo K. Prevalence of symptomatic lumbar spondylolysis in pediatric patients. Orthopedics. 2016;39(3):e434–e437. doi: 10.3928/01477447-20160404-07. [DOI] [PubMed] [Google Scholar]
- 3.Leone A, Cianfoni A, Cerase A, Magarelli N, Bonomo L. Lumbar spondylolysis: a review. Skeletal Radiol. 2011;40(6):683–700. doi: 10.1007/s00256-010-0942-0. [DOI] [PubMed] [Google Scholar]
- 4.Lawrence KJ, Elser T, Stromberg R. Lumbar spondylolysis in the adolescent athlete. Phys Ther Sport. 2016;20:56–60. doi: 10.1016/j.ptsp.2016.04.003. [DOI] [PubMed] [Google Scholar]
- 5.Haun DW, Kettner NW. Spondylolysis and spondylolisthesis: a narrative review of etiology, diagnosis, and conservative management. J Chiropr Med. 2005;4(4):206–217. doi: 10.1016/S0899-3467(07)60153-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yochum TR, Rowe LJ. 3rd ed. Lippincott Williams & Wilkins; Philadelphia, PA: 2005. Yochum and Rowe's Essentials of Skeletal Radiology. [Google Scholar]
- 7.Tezuka F, Sairyo K, Sakai T, Dezawa A. Etiology of adult-onset stress fracture in the lumbar spine. Clin Spine Surg. 2017;30(3):E233–E238. doi: 10.1097/BSD.0000000000000162. [DOI] [PubMed] [Google Scholar]
- 8.Beutler WJ, Fredrickson BE, Murtland A, Sweeney CA, Grant WD, Baker D. The natural history of spondylolysis and spondylolisthesis: 45-year follow-up evaluation. Spine (Phila Pa 1976) 2003;28(10):1027–1035. doi: 10.1097/01.BRS.0000061992.98108.A0. [DOI] [PubMed] [Google Scholar]
- 9.Dunn AJ, Campbell RSD, Mayor PE, Rees D. Radiological findings and healing patterns of incomplete stress fractures of the pars interarticularis. Skeletal Radiol. 2008;37(5):443–450. doi: 10.1007/s00256-008-0449-0. [DOI] [PubMed] [Google Scholar]
- 10.Patel DR, Kinsella E. Evaluation and management of lower back pain in young athletes. Transl Pediatr. 2017;6(3):225–235. doi: 10.21037/tp.2017.06.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Motley G, Nyland J, Jacobs J, Caborn DNM. The pars interarticularis stress reaction, spondylolysis, and spondylolisthesis progression. J Athl Train. 1998;33(4):351–358. [PMC free article] [PubMed] [Google Scholar]
- 12.Ralston S, Weir M. Suspecting lumbar spondylolysis in adolescent low back pain. Clin Pediatr (Phila) 1998;37(5):287–293. doi: 10.1177/000992289803700502. [DOI] [PubMed] [Google Scholar]
- 13.Starr AM, Wessely MA, Albastaki U, Pierre-Jerome C, Kettner NW. Bone marrow edema: pathophysiology, differential diagnosis, and imaging. Acta Radiol. 2008;49(7):771–786. doi: 10.1080/02841850802161023. [DOI] [PubMed] [Google Scholar]
- 14.Tofte JN, CarlLee TL, Holte AJ, Sitton SE, Weinstein SL. Imaging pediatric spondylolysis: a systematic review. Spine (Phila Pa 1976) 2017;42(10):777–782. doi: 10.1097/BRS.0000000000001912. [DOI] [PubMed] [Google Scholar]
- 15.Shields BJ, Fernandez SA, Smith GA. Epidemiology of cheerleading stunt-related injuries in the United States. J Athl Train. 2009;44(6):586–594. doi: 10.4085/1062-6050-44.6.586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.LaBella CR, Mjaanes J, Council on Sports Medicine and Fitness Cheerleading injuries: epidemiology and recommendations for prevention. Pediatrics. 2012;130(5):966–971. doi: 10.1542/peds.2012-2480. [DOI] [PubMed] [Google Scholar]
- 17.Field AE, Gordon CM, Pierce LM, Ramappa A, Kocher MS. Prospective study of physical activity and risk of developing a stress fracture among preadolescent and adolescent girls. Arch Pediatr Adolesc Med. 2011;165(8):723–728. doi: 10.1001/archpediatrics.2011.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schroeder GD, LaBella CR, Mendoza M, Daley EL, Savage JW, Patel AA, Hsu WK. The role of intense athletic activity on structural lumbar abnormalities in adolescent patients with symptomatic low back pain. Eur Spine J. 2016;25(9):2842–2848. doi: 10.1007/s00586-016-4647-5. [DOI] [PubMed] [Google Scholar]
- 19.Sairyo K, Nagamachi A, Matsuura T. A review of the pathomechanism of forward slippage in pediatric spondylolysis: the Tokushima theory of growth plate slippage. J Med Invest. 2015;62(1.2):11–18. doi: 10.2152/jmi.62.11. [DOI] [PubMed] [Google Scholar]
- 20.Kaneko H, Murakami M, Nishizawa K. Prevalence and clinical features of sports-related lumbosacral stress injuries in the young. Arch Orthop Trauma Surg. 2017;137(5):685–691. doi: 10.1007/s00402-017-2686-y. [DOI] [PubMed] [Google Scholar]
- 21.Dhouib A, Tabard-Fougere A, Hanquinet S, Dayer R. Diagnostic accuracy of MR imaging for direct visualization of lumbar pars defect in children and young adults: a systematic review and meta-analysis. Eur Spine J. 2018;27(5):1058–1066. doi: 10.1007/s00586-017-5305-2. [DOI] [PubMed] [Google Scholar]
- 22.Sakai T, Tezuka F, Yamashita K, Takata Y, Higashino K, Nagamachi A, Sairyo K. Conservative treatment for bony healing in pediatric lumbar spondylolysis. Spine (Phila Pa 1976) 2017;42(12):E716–E720. doi: 10.1097/BRS.0000000000001931. [DOI] [PubMed] [Google Scholar]
- 23.Terai T, Sairyo K, Goel VK. Spondylolysis originates in the ventral aspect of the pars interarticularis: a clinical and biomechanical study. J Bone Joint Surg Br. 2010;92-B(8):1123–1127. doi: 10.1302/0301-620X.92B8.22883. [DOI] [PubMed] [Google Scholar]
- 24.Labelle H, Roussouly P, Berthonnaud É. Spondylolisthesis, pelvic incidence, and spinopelvic balance: a correlation study. Spine (Phila Pa 1976) 2004;29(18):2049–2054. doi: 10.1097/01.brs.0000138279.53439.cc. [DOI] [PubMed] [Google Scholar]
- 25.Hanke LF, Tuakli-Wosornu YA, Harrison JR, Moley PJ. The relationship between sacral slope and symptomatic isthmic spondylolysis in a cohort of high school athletes: a retrospective analysis. PM R. 2018;10(5):501–506. doi: 10.1016/j.pmrj.2017.09.012. [DOI] [PubMed] [Google Scholar]
- 26.Kim M-W, Lee KY, Lee S. Factors associated with the symptoms of young adults with L5 spondylolysis. Asian Spine J. 2018;12(3):476–483. doi: 10.4184/asj.2018.12.3.476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Viana SL, Viana MA, de CB, de Alencar ELC. Atypical, unusual, and misleading imaging presentations of spondylolysis. Skeletal Radiol. 2015;44(9):1253–1262. doi: 10.1007/s00256-015-2138-0. [DOI] [PubMed] [Google Scholar]
- 28.Yamazaki K, Kota S, Oikawa D, Suzuki Y. High defect stage, contralateral defects, and poor flexibility are negative predictive factors of bone union in pediatric and adolescent athletes with spondylolysis. J Med Invest. 2018;65(1.2):126–130. doi: 10.2152/jmi.65.126. [DOI] [PubMed] [Google Scholar]
- 29.Raudenbush BL, Chambers RC, Silverstein MP, Goodwin RC. Indirect pars repair for pediatric isthmic spondylolysis: a case series. J Spine Surg. 2017;3(3):387–391. doi: 10.21037/jss.2017.08.08. [DOI] [PMC free article] [PubMed] [Google Scholar]