Abstract
Background/purpose
Pre-eruptive intracoronal resorption (PEIR) is usually detected accidently in radiographs. However, treatment modality is still not reported systematically. The current study aimed to conduct a systematic review of the treatment modality of PEIR case reports and to report a case on the preservation of a vital pulp with surgical exposure in permanent maxillary canine.
Materials and methods
We systematically searched case reports from PubMed/MEDLINE, EMBASE, and Web of science databases. The treatment modality, suspected etiology, and follow up periods were collected from each study and reviewed by two authors independently.
Results
The initial search identified 100 studies. After the title/abstract screening, 37 articles received a full-text reading; and finally, 24 articles (29 patients and 37 affected teeth) were selected for the final review. Among the 24 unerupted teeth, surgical opening and restoration treatment of PEIR was chosen as a high priority for treatment options (n = 9, 36%). Among the 13 erupted teeth, restoration was applied for the prevention such as developing in size and fracture (n = 4, 31%).
Conclusion
According to this systematic review, treatment modalities were based on the progressive nature of the lesion size and eruption state to establish the optimal approach for each patient. Clinicians should take into account the eruption status, lesion progression, the size of the lesion, and the degree of pulp involvement.
Keywords: Conservative approach, Pre-eruptive intracoronal resorption, Treatment protocol
Introduction
Pre-eruptive intracoronal resorption (PEIR) of the teeth is usually detected accidently in radiographs. Lesions are typically found in dentin of unerupted teeth and close to the dentinoenamel junction.1,2 The defect is generally located on the central or mesial portion of the crown. However, lesions sometimes involve the pulp and can cause symptoms such as swelling and pain.3,4 The prevalence of PEIR has been determined to be 2–8% by subject and 0.6–2% by tooth, primarily affecting the mandibular first premolar and second and third molars.5 Usually, a single tooth is affected in an individual,6 with nearly half of the lesions extending to more than two-thirds of the dentin thickness.7
Although this condition was first reported in 1941, the etiology of PEIR remains unclear because only a small number of studies have been conducted on it. No association was found between PEIR and sex, race, medical conditions, systemic factors, or fluoride supplementation.2,7 From a histological viewpoint of PEIR, multinucleated giant cells, osteoclasts, and chronic inflammatory cells have been described as related factors in some case reports. This evidence suggests that the process in PEIR involves resorption of calcified dental tissue.6,8
Regardless of suspected etiology, the clinician who discovers a radiolucency associated with an unerupted tooth is faced with a dilemma. Should the clinician wait until the tooth erupts to initiate treatment or intervene surgically to arrest this phenomenon? Or should the tooth be extracted surgically? There are many different treatment modalities of PEIR that depend on extent of the lesion at the time of discovery and anticipated eruption time of the affected tooth. The objective of this paper is to present a systematic review of treatment modalities of PEIR and to present a case report on vital pulp preservation in permanent dentition.
Materials and methods
We followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines for this systematic review.
Search strategy
A systematic search was conducted without limits, including studies published in or before July 2019. The authors independently searched PubMed/MEDLINE, Web of Science, and EMBASE. A combination of Medical Subject Heading (MeSH) and full-text search term were used: (“pre-eruptive” OR “intracoronal”) AND (“tooth resorption"[MeSH Terms] OR Tooth Resorption[Text Word] OR “radiolucency”) AND (“case reports"[Publication Type] OR “case reports"[All Fields]). Keywords in EMBASE were (‘pre-eruptive’ OR intracoronal) AND ‘tooth disease’ AND ‘case report.’ The search strategy in the Web of Science was (“pre-eruptive” OR “intracoronal”) AND (resorption) AND (case report).
Selection criteria
The studies were initially selected based on title and abstract according to the following inclusion criteria:
-
•
Case report related to PEIR
-
•
Published in English
Articles without an abstract or those without an adequate description were included for full-text evaluation. Eligibility was confirmed after evaluation of the full text based on previously defined exclusion criteria (i.e., duplicates, editorials, commentaries, retrospective study, and comparative study).
Screening process
The two reviewers (VNT Le and DW Lee) performed the search and selection process (finished on 30 July 2019). After initial screening of titles and abstracts, full-text articles were analyzed, and differences between the reviewers were resolved through discussion.
Results
Literature search
Electronic searches identified 100 publications (Fig. 1). The initial search yielded 39 available titles in PubMed/MEDLINE, 42 in EMBASE, and 19 in Web of Science. After eliminating duplicates, titles and abstracts were screened in the remaining 48 articles, resulting in exclusion of 11 articles. The full text of the remaining 37 articles was reviewed, and unrelated (n = 4) and retrospective studies (n = 9) were excluded. The remaining 24 articles (29 cases with 37 affected teeth) were included in our qualitative analyses.
Figure 1.
Flow diagram for identification of relevant studies.
Study characteristics
The main characteristics of all included studies are shown in Table 1. Included studies were published between 1988 and 2018, had range of patient age from 19 months to 14 years, with no sex predilection. All cases were diagnosed on radiographs, such as panoramic (n = 14, 48.3%),1,8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18 periapical (n = 8, 27.6%),3,4,6,19, 20, 21, 22 and bitewing (n = 7, 24.1%),8,23, 24, 25, 26, 27 with 24 unerupted teeth and 13 erupted teeth.
Table 1.
Study characteristics of the included studies.
| Case | Author (year) | Age /Sex |
Tooth | Diagnostic method | Eruption status | Treatment | Suspected etiology | Note (Histologic, impressive findings) | Follow-up |
|
|---|---|---|---|---|---|---|---|---|---|---|
| Period | Status | |||||||||
| 1 | Ilha et al.9 (2018) | 8 y Female |
#36 | Panoramic radiograph | Unerupted | Surgical exposure Restoration (GIC + Composite) |
NR | Delayed eruption of the affected tooth | 18 m | Asymptomatic |
| 2 | De Souza et al.1 (2017) | 10 y Male |
#35 | Panoramic radiograph | Unerupted | Monitoring eruption Restoration (Composite) |
Ectopic eruption | 12 m | Asymptomatic | |
| 3 | Schwimmer et al.3 (2017) | 19 m Female |
#74 | Periapical radiograph | Erupted | RCT | NR | 1w 7 m |
Good healing Asymptomatic |
|
| 4 | Manmontri et al.10 (2017) | 8 y 8 m | #37 | Panoramic radiograph | Unerupted | Monitoring (periodic intraoral and extraoral radiographs) | NR | Nine years of follow-up Supporting theory: progressive resorption of PEIR may cease or decelerate after tooth eruption |
2y3m 3y4m 6y4m |
Partially erupted Asymptomatic Completely erupted Asymptomatic No changes clinically or radiographically in the PEIR-affected tooth |
| 5 | Omar et al.23 (2015) | 11 y NR |
#37 | Bitewing | Unerupted | Surgical exposure MTA direct pulp capping + cotton pellets + IRM IRM and cotton pellets were removed + Composite |
NR | 8w 3m8w 3y3m8w |
Asymptomatic Normal root development Asymptomatic Normal root development Asymptomatic |
|
| 6 | Spierer and Fuks24 (2014) | 6 y Male |
#46 | Bitewing | Unerupted | Surgical exposure Restoration (Glass monomer lining + GIC) |
Minute gaps in enamel formation | Connective tissue, bone and granulation issue | 3w 3m3w 1 y |
Good healing Asymptomatic Normal root development Asymptomatic |
| 7 | Czarnecki et al.19 (2014) | 4 y 3 m Female |
#46 | Periapical radiograph | Unerupted | Surgical exposure Restoration (GC sealant) CHX rinse |
NR | 8w 2 m 20 m 30 m 35 m 44 m |
Asymptomatic Unremarkable No change size of the defect, caries-free |
|
| 8 | Brunet-Llobet et al.20 (2014) | 12 y Male |
#37 | Periapical radiograph | Unerupted | Extraction | NR | Inflamed myxomatous tissue, plump stellate fibroblast, hyalinized connective tissue, inflammatory cells, predominantly neutrophils, lymphocytes, and plasma cells | ||
| 9 | Wong and Khan11 (2014) | 12 y Female |
#37 | Panoramic radiograph | Unerupted | Extraction | NR | No evidence of pulpal inflammation | ||
| 10 | Ari12 (2014) | 12 y Male |
#35 | Panoramic radiograph | Erupted | RCT Restoration (Composite) |
NR | NR | ||
| 11 | Counihan and O'Connell8 (2012) | 10 y Female |
#45 | Panoramic radiograph | Unerupted | Monitoring eruption Restoration (indirect pulp cap + GIC + Composite) |
NR | Histological examination was inconclusive due to small sample size and contamination of the sample with oral bacteria | NR | |
| 12 | Counihan and O'Connell8 (2012) | 6 y Female |
#46 | Bitewing | Partially erupted | Monitoring eruption Conservative approach + monitoring annually |
NR | 5 y | Vital Asymptomatic No evidence of caries |
|
| 13 | Counihan and O'Connell8 (2012) | 12 y Female |
#37 | Panoramic radiograph | Partially erupted | Extraction | NR | Pulpal surface with osteoclast-like giant cells and granulation tissue | ||
| 14 | Hata et al.21 (2007) | 8 y 6 m 10 y 11 m |
#11 #42 #35 |
Periapical radiograph Periapical radiograph Periapical radiograph |
Erupting Erupted Unerupted |
Partial pulpotomy with calcium hydroxide + GIC Composite Gingivectomy Restoration (calcium hydroxide liner + Composite) Extraction of the primary second molar Restoration (calcium hydroxide liner + GIC) |
External resorption | Ps taken at age 11 years showed normal root formation | 2 m 3 y |
Asymptomatic Normal pulp vitality Normal periodontal tissue |
| 15 | Davidovich et al.13 (2005) | 11 y Female |
#37 | Panoramic radiograph | Unerupted | Surgical exposure Restoration (Glass monomer lining + GIC) Restoration removal Partial pulpotomy (calcium hydroxide + IRM + Amalgam) |
NR | The radiolucent area underneath the restoration | 1w 3m1w 9m1w |
Fibrin healing tissue Erupted, gingivitis Asymptomatic Normal appearance Continued root development |
| 16 | McEntire et al.25 (2005) | 9 y Female |
#35 | Bitewing | Unerupted | Monitoring Restoration (Composite) |
Ectopic positioning | 5 y | Asymptomatic | |
| 17 | Moskovitz and Holan26 (2004) | 6 y 2 m Female |
#47 | Bitewing | Partially erupted | Monitoring Restoration (Calcium hydroxide liner + IRM) |
A small aperture of the enamel surrounding the lesion | 5y8m 6y9m |
No increase in size of the radiolucent defect Asymptomatic |
|
| 18 | Dowling et al.4 (1999) | 11 y Female |
#33 | Periapical radiograph | Erupted | RCT Restoration (porcelain veneer) |
Idiopathic external resorption | Crown: granulation tissue Pulp: chronic inflammation |
NR | |
| 19 | Kupietzky27 (1999) | 12 y Male |
#35 | Bitewing | Erupted | Indirect pulp capping + Amalgam restoration Composite |
NR | Amalgam was removed | 8 m NR |
NR |
| 20 | Seow14 (1998) | 14 y Female |
#15 #26 #34 #35 #38 #45 #47 |
Panoramic radiograph | Unerupted | NR | A small or sealed external opening through which resorption cells had gained entry into the dentin during initial development of the tooth | NR | ||
| 21 | Savage et al.15 (1998) | 11 y Female |
27 | Panoramic radiograph | Erupted | Surgical extraction | Idiopathic external resorption | No evidence of dental caries A thin dentin bridge separated pulp from the resorption defect, pulpal response was minimal with very few inflammatory cells |
||
| 22 | McNamara et al.16 (1997) | 11 y Male |
#37 | Panoramic radiograph | Unerupted | Surgical extraction | External resorption | The extensive lesion was caused by external resorption | ||
| 23 | Seow and Hackley6 (1996) | 2 y 6 m Female |
#75 | Periapical radiograph | Erupted | Extraction | Localized developmental aberration of dentin | No dental caries No communication was noted between pulp and resorption area, pulp and outer surface, or resorption area and outer surface |
||
| 24 | Seow and Hackley6 (1996) | 11 y Female |
#47 | Periapical radiograph | Unerupted | Surgical exposure Restoration (calcium hydroxide liner + GIC) The tooth was re-covered with the mucosal flap for spontaneous eruption |
Communicating channels between exterior and resorptive areas | Normal dental follicle Uninflamed tissue Reduced enamel epithelium |
9 m 2 y 9 m |
Erupted Vital, intact restoration Normal root development Normal pulp vitality and occlusal function |
| 25 | Holan et al.17 (1994) | 12 y Male |
#43 | Panoramic radiograph | Erupting | Restoration (calcium hydroxide liner + composite) | Reduced enamel epithelium of the unerupted tooth (Invasion of the crown by vascular connective tissue) | 6 m | Normal root development Asymptomatic t |
|
| 26 | Holan et al.17 (1994) | 13 y Male |
#37 | Panoramic radiograph | Unerupted | Surgical exposure Restoration (calcium hydroxide liner + IRM) |
6 m 3 y 9 m |
Erupted Asymptomatic Asymptomatic Normal root development |
||
| 27 | Holan et al.17 (1994) | 11 y Female |
#45 | Bitewing | Erupted | Restoration (calcium hydroxide liner + composite) | 6 y | Asymptomatic | ||
| 28 | Ignelzi et al.18 (1990) | 12 y 9 m Male |
#47 | Panoramic radiograph | Unerupted | Surgical exposure Restoration (lining calcium hydroxide + Zinc oxide and eugenol) Suture Pulp therapy + stainless steel crown |
NR |
Eruption appeared imminent, and destruction to the crown was extensive |
2w 2 m 5 m 1 y 2 y 6 m |
Asymptomatic Good healing Asymptomatic Asymptomatic Asymptomatic Normal root development Asymptomatic Normal root development |
| 29 | Brooks22 (1988) | 10 y Female |
#45 | Periapical radiograph | Unerupted | Monitoring Restoration (lining calcium hydroxide + composite) |
NR | 1 m 6 m |
Erupted Apical root-end closure Asymptomatic |
|
Abbreviations: NR: Not reported, RCT: Root canal treatment, GIC: Glass ionomer cement, IRM: Intermediate restorative material (reinforced zinc oxide eugenol), MTA: Mineral trioxide aggregate.
Treatment modality and follow-up
Among the 24 unerupted teeth, the reviewed treatment options were surgical exposure and restoration due to large and developing lesions (n = 9, 36%),6,9,13,17, 18, 19,21,23,24 no reports (n = 7, 28%),14 monitoring and restoration due to small and static lesions (n = 4, 16%),1,8,22,25 extraction due to large lesion, unrecoverable residual, extensive pulpal involvement, or benefit of orthodontic treatment (n = 3, 16%),11,16,20 and observation due to small and static lesion without restoration (n = 1, 4%).10
Among the 13 erupted teeth, the reviewed treatment options were restoration due to prevention such as developing in size and fracture (n = 4, 30.7%),17,21,27 root canal therapy (n = 3, 23.1%),3,4,12 extraction due to an abscessed primary tooth, large lesion, or unrecoverable residuals (n = 3, 23.1%),6,8,15 monitoring and restoration due to prevention such as developing in the thickness of resorptive dentin and fracture (n = 1, 7.7%),26 surgical exposure and restoration due to large and developing lesions (n = 1, 7.7%),21 and observation due to small and static lesions (n = 1, 7.7%).8
Regarding conservative approaches (without extraction), the follow-up period ranged from 2 months to 6 years 9 months. With long-term follow-up, there was no apparent variation of prognoses regardless of approach.
Suspected etiology
Most studies mentioned that the etiology seemed to remain unclear. Some etiologies were theorized as ectopic eruption,1,25 external resorption,4,6,14, 15, 16,21 and developmental abnormality of the tooth.17,24,26
Case report
A 9-year-10-month-old girl was referred to the Department of Pediatric Dentistry, Jeonbuk National University Dental Hospital, Jeonju, Jeonlabukdo, South Korea by a dentist at a local dental clinic, with a chief complaint of gingival swelling, bleeding, and pain when brushing or touching the right maxillary canine. Her past medical history was unremarkable. There was no known specific dental history (including trauma or infection of the maxilla and teeth). The patient did not have a family history of a genetic disorder.
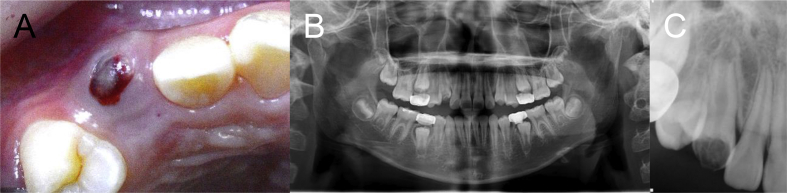
Intraorally, gingival swelling and bleeding were observed at the area of right maxillary canine. A clinical examination revealed an eruption hematoma. A panoramic radiograph revealed a delayed eruption of the right maxillary canine. Further periapical radiograph revealed a well circumscribed radiolucent lesion of two-thirds of the dentin thickness that extended over the dentinoenamel junction (Fig. 2). Given the position of lesion, clinical history radiographic examinations, and the features supported a diagnosis of a PEIR.
Figure 2.
During the first visit on #13. (A) Eruption hematoma. (B) Panoramic radiograph: a delayed eruption. (C) Periapical radiograph: a circumscribed radiolucent lesion.
For unerupted right maxillary canine, we made a treatment plan including surgical exposure and restoration.
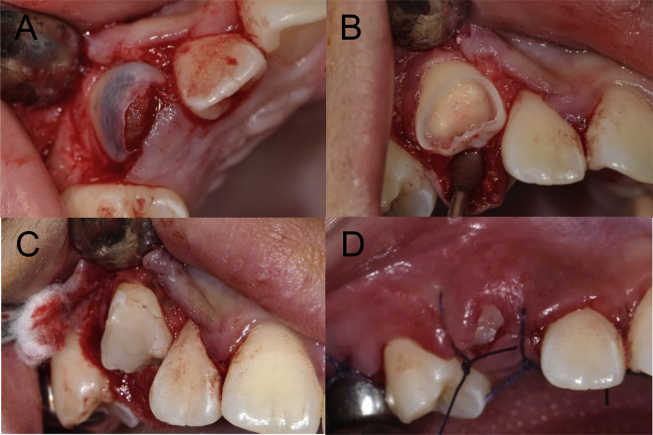
After the patient's parents agreed to the treatment plan, surgical opening was performed under local anesthesia. The cavity of the lesion showed a gray irregular and friable fragment of soft tissue without infected dentin (Fig. 3A). The dentin area inside the crown was resorbed by this tissue (Fig. 3B). After curettage of the tissue, no pulp exposure was found and the defect was restored by interim glass ionomer (Fig. 3C). A biopsy sample of the removed tissue was sent for histopathological examination, which revealed nonspecific chronic inflammation with hemorrhagic necrosis. This result supports distinction of PEIR from dental caries.
Figure 3.
Treatment of #13. (A) Surgical exposure of crown. (B) Tooth preparation. (C) Glass ionomer cement. (D) Surgical suture.
After nine months, the right maxillary canine remained asymptomatic. The tooth showed a negative response to percussion, physiological mobility, and normal response to hot and cold stimuli. A periapical radiograph revealed normal root development without infection. Therefore, resin restoration was performed to recover the appearance and function of the canine.
After the two years follow-up examination, the tooth was asymptomatic and completely erupted with normal root development. Occlusal adjustment was performed to ensure functional occlusion and restoration longevity (Fig. 4).
Figure 4.
Follow-up after treatment. One year follow-up: (A) intra-oral clinical photograph, (B) periapical radiograph. Two years follow-up: (C) intra-oral clinical photograph, (D) periapical radiograph, (E) panoramic radiograph.
Discussion
Overall, we found that no protocol is currently available for treatment of PEIR. Based on our systematic review, the majority of authors considered conservative therapy as a treatment of PEIR. In seven studies, extraction was performed because of large lesions,8,15,16,20 extensive pulpal involvement or benefit of orthodontic treatment,11 and abscessed primary tooth.6 Since early intervention was not performed in these cases,6,8,11,15,16,20 the lesion progressed, leading to extraction.
In this study, according to its progressive nature based on lesion size, PEIR lesions can be divided into two major types: static1,8,10,22,25,26 and developing.3,4,6,8,9,11, 12, 13,15, 16, 17, 18, 19, 20, 21,23,24,27 Most previous treatment plans were based on lesion size. For static cases, many authors chose the conservative option by monitoring without treatment until the tooth erupted1,8,22,25,26 since the lesion was asymptomatic and static. This group of authors suggested that the clinician should monitor development of the lesion through periodic radiographic examination. When a lesion increased in size, as in developing cases, treatment should be provided immediately to avoid the complication related to pulp as well as fracture.26,28
Clinically, not only the size of the PEIR lesion, but also the eruption state is critical for treatment planning.29 After initial detection of PEIR, the clinician can use periodic radiographic examinations to monitor the size of the lesion to create a restorative treatment plan.29 However, when eruption has occurred, restoration is indicated, as the lesion progresses rapidly and becomes symptomatic.6,8,15,16,20
Generally, PEIR of a developing and unerupted tooth have been discovered only through radiographic examination. This type of atypical resorption process is proceeded at a slow pace until the exposure of the crown to the oral cavity. However, once the tooth erupts through the gingiva, cariogenic microorganisms invade and progress into the dentin via the resorbed area, and the extensive size of the lesion makes it distinguishable.19,23 In our case report, permanent maxillary canine was unerupted. The swelling and inflammation of the gingival tissue implied that it was likely to be progressive due to penetration of bacteria externally. Therefore, we performed the treatment as soon as possible. We surgically exposed the right maxillary canine and restored with glass ionomer. This method of treatment is generally recommended for most cases as soon the lesion is diagnosed radiographically.6,9,17,21,23,24 Waiting until full emergence of the crown to achieve curettage may allow the resorption to extend to the pulp with complications from infection.
Our study is the first systematic review investigating the treatment modalities of PEIR. However, most case reports lack histological analyses of lesions, which supports the diagnosis of PEIR.1,3,6,8, 9, 10,12, 13, 14,16, 17, 18, 19,21,23, 24, 25 Although the etiology of each case is not clear, a review of treatment modalities helps to create a treatment plan for clinical management. The period of follow-up of included case reports is heterogeneous, from 2 months to 6 years 9 months. This leads to difficulty in evaluating the effect of treatment modalities by meta-analysis.
In conclusion, from the present systematic review, it can be concluded that surgical opening and restoration treatment are considered high priority (36%) as a treatment option for PEIR. Second, most treatment plan was based on progressive nature of the lesion size and eruption state to establish the optimal approach for each patient.
Declaration of Competing Interest
The authors declare no conflict of interest.
Acknowledgments
This work was supported by the Biomedical Research Institute, Jeonbuk National University Hospital.
References
- 1.De Souza N., Vaz A., Chalakkal P. Intracoronal radiolucency in an unerupted premolar: a rare occurrence. J Clin Diagn Res. 2017;11:ZD04–ZD5. doi: 10.7860/JCDR/2017/22791.9135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Seow W.K. Pre-eruptive intracoronal resorption as an entity of occult caries. Pediatr Dent. 2000;22:370–376. [PubMed] [Google Scholar]
- 3.Schwimmer Y., Zeltser R., Moskovitz M. Deep caries due to Pre-eruptive intracoronal resorption in a newly erupted primary molar. Int J Paediatr Dent. 2017;27:313–315. doi: 10.1111/ipd.12283. [DOI] [PubMed] [Google Scholar]
- 4.Dowling P.A., Fleming P., Corcoran F. A case report of pre-eruptive coronal resorption in a mandibular canine. Dent Update. 1999;26:444–445. doi: 10.12968/denu.1999.26.10.444. [DOI] [PubMed] [Google Scholar]
- 5.Zilberman U., Milevski I., Yegorov D., Smith P. A 3000 year old case of an unusual dental lesion: pre-eruptive intracoronal resorption. Arch Oral Biol. 2019;97:97–101. doi: 10.1016/j.archoralbio.2018.10.015. [DOI] [PubMed] [Google Scholar]
- 6.Seow W.K., Hackley D. Pre-eruptive resorption of dentin in the primary and permanent dentitions: case reports and literature review. Pediatr Dent. 1996;18:67–71. [PubMed] [Google Scholar]
- 7.Seow W.K., Lu P.C., McAllan L.H. Prevalence of pre-eruptive intracoronal dentin defects from panoramic radiographs. Pediatr Dent. 1999;21:332–339. [PubMed] [Google Scholar]
- 8.Counihan K.P., O'Connell A.C. Case report: pre-eruptive intra-coronal radiolucencies revisited. Eur Arch Paediatr Dent. 2012;13:221–226. doi: 10.1007/BF03262874. [DOI] [PubMed] [Google Scholar]
- 9.Ilha M.C., Kramer P.F., Ferreira S.H., Ruschel H.C. Pre-emptive intracoronal radiolucency in first permanent molar. Int J Clin Pediatr Dent. 2018;11:151–154. doi: 10.5005/jp-journals-10005-1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Manmontri C., Mahasantipiya P.M., Chompu-Inwai P. Preeruptive intracoronal radiolucencies: detection and nine years monitoring with a series of dental radiographs. Case Rep Dent. 2017;2017:6261407. doi: 10.1155/2017/6261407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wong L., Khan S. Occult caries or pre-eruptive intracoronal resorption? A chance finding on a radiograph. Pediatr Dent. 2014;36:429–432. [PubMed] [Google Scholar]
- 12.Ari T. Management of "hidden caries": a case of severe pre-eruptive intracoronal resorption. J Can Dent Assoc. 2014;80:e59. [PubMed] [Google Scholar]
- 13.Davidovich E., Kreiner B., Peretz B. Treatment of severe pre-eruptive intracoronal resorption of a permanent second molar. Pediatr Dent. 2005;27:74–77. [PubMed] [Google Scholar]
- 14.Seow W.K. Multiple pre-eruptive intracoronal radiolucent lesions in the permanent dentition: case report. Pediatr Dent. 1998;20:195–198. [PubMed] [Google Scholar]
- 15.Savage N.W., Gentner M., Symons A.L. Preeruptive intracoronal radiolucencies: review and report of case. ASDC (Am Soc Dent Child) J Dent Child. 1998;65:36–40. [PubMed] [Google Scholar]
- 16.McNamara C.M., Foley T., O'Sullivan V.R., Crowley N., McConnell R.J. External resorption presenting as an intracoronal radiolucent lesion in a pre-eruptive tooth. Oral Dis. 1997;3:199–201. doi: 10.1111/j.1601-0825.1997.tb00037.x. [DOI] [PubMed] [Google Scholar]
- 17.Holan G., Eidelman E., Mass E. Pre-eruptive coronal resorption of permanent teeth: report of three cases and their treatments. Pediatr Dent. 1994;16:373–377. [PubMed] [Google Scholar]
- 18.Ignelzi M.A., Jr., Fields H.W., White R.P., Bergenholtz G., Booth F.A. Intracoronal radiolucencies within unerupted teeth. Case report and review of literature. Oral Surg Oral Med Oral Pathol. 1990;70:214–220. doi: 10.1016/0030-4220(90)90122-9. [DOI] [PubMed] [Google Scholar]
- 19.Czarnecki G., Morrow M., Peters M., Hu J. Pre-eruptive intracoronal resorption of a permanent first molar. J Dent Child. 2014;81:151–155. [PMC free article] [PubMed] [Google Scholar]
- 20.Brunet-Llobet L., Lahor-Soler E., Miranda-Rius J. Oral pain due to severe pre-eruptive intracoronal resorption in permanent tooth. Eur J Paediatr Dent. 2014;15:332–334. [PubMed] [Google Scholar]
- 21.Hata H., Abe M., Mayanagi H. Multiple lesions of intracoronal resorption of permanent teeth in the developing dentition: a case report. Pediatr Dent. 2007;29:420–425. [PubMed] [Google Scholar]
- 22.Brooks J.K. Detection of intracoronal resorption in an unerupted developing premolar: report of case. J Am Dent Assoc. 1988;116:857–859. doi: 10.14219/jada.archive.1988.0294. [DOI] [PubMed] [Google Scholar]
- 23.Omar S., Choi J., Nelson B., Shin M., Chen J.W. Pre-eruptive intracoronal resorption (PEIR): literature review and case report. J Calif Dent Assoc. 2015;43:255–260. [PubMed] [Google Scholar]
- 24.Spierer W.A., Fuks A.B. Pre-eruptive intra-coronal resorption: controversies and treatment options. J Clin Pediatr Dent. 2014;38:326–328. doi: 10.17796/jcpd.38.4.dm7652634h12705v. [DOI] [PubMed] [Google Scholar]
- 25.McEntire J.F., Hermesch C.B., Wall B.S., Leonard D.L. Case report--pre-eruptive intracoronal resorption. Operat Dent. 2005;30:553–556. [PubMed] [Google Scholar]
- 26.Moskovitz M., Holan G. Pre-eruptive intracoronal radiolucent defect: a case of a nonprogressive lesion. J Dent Child. 2004;71:175–178. [PubMed] [Google Scholar]
- 27.Kupietzky A. Treatment of an undiagnosed pre-eruptive intra-coronal radiolucency. Pediatr Dent. 1999;21:369–372. [PubMed] [Google Scholar]
- 28.Wood P.F., Crozier D.S. Radiolucent lesions resembling caries in the dentine of permanent teeth. A report of sixteen cases. Aust Dent J. 1985;30:169–173. doi: 10.1111/j.1834-7819.1985.tb04128.x. [DOI] [PubMed] [Google Scholar]
- 29.Al-Batayneh O.B., AlJamal G.A., AlTawashi E.K. Pre-eruptive intracoronal dentine radiolucencies in the permanent dentition of Jordanian children. Eur Arch Paediatr Dent. 2014;15:229–236. doi: 10.1007/s40368-013-0104-x. [DOI] [PubMed] [Google Scholar]