Herpetic gingivostomatitis (HGS) and herpetiform aphthous ulcerations (HAU, also known as herpetiform type recurrent aphthous stomatitis) are two oral diseases with different etiologies and oral manifestations.1, 2, 3, 4, 5 However, they are easily confused because the two disease names contain a similar adjective, herpetic or herpetiform.
There are two types of herpes simplex virus (HSV): type 1 HSV (HSV-1) and type 2 HSV (HSV-2). HSV-1 and HSV-2 have similar structure and disease mechanism but differ in antigenicity, anatomic site predilection and epidemiology.1 HSV-1 usually infects the oral, facial, and ocular areas as well as skin above the waist, but HSV-2 usually infects the genital zones and typically involves the genitalia and skin below the waist. The natural history of HSV infection includes primary infection, latency, and recurrent infection. Primary HSV-1 infection typically occurs at a young age, may be asymptomatic, and usually does not cause significant morbidity. After primary HSV-1 infection is established, the virus is taken up by sensory nerves, and transported to the associated sensory or, less frequently, autonomic ganglia where the virus remains in a latent state. The most common site of latency for HSV-1 is the trigeminal ganglion. The virus uses the axons of the sensory neurons to travel back and forth to the skin or mucosa. Recurrent (secondary) herpes infection occurs with reactivation of the virus. Old age, physical or emotional stress, fatigue, severe systemic disease, and malignancy have been associated with reactivation. Symptomatic recurrences often affect epithelium supplied by the sensory ganglion.1,2
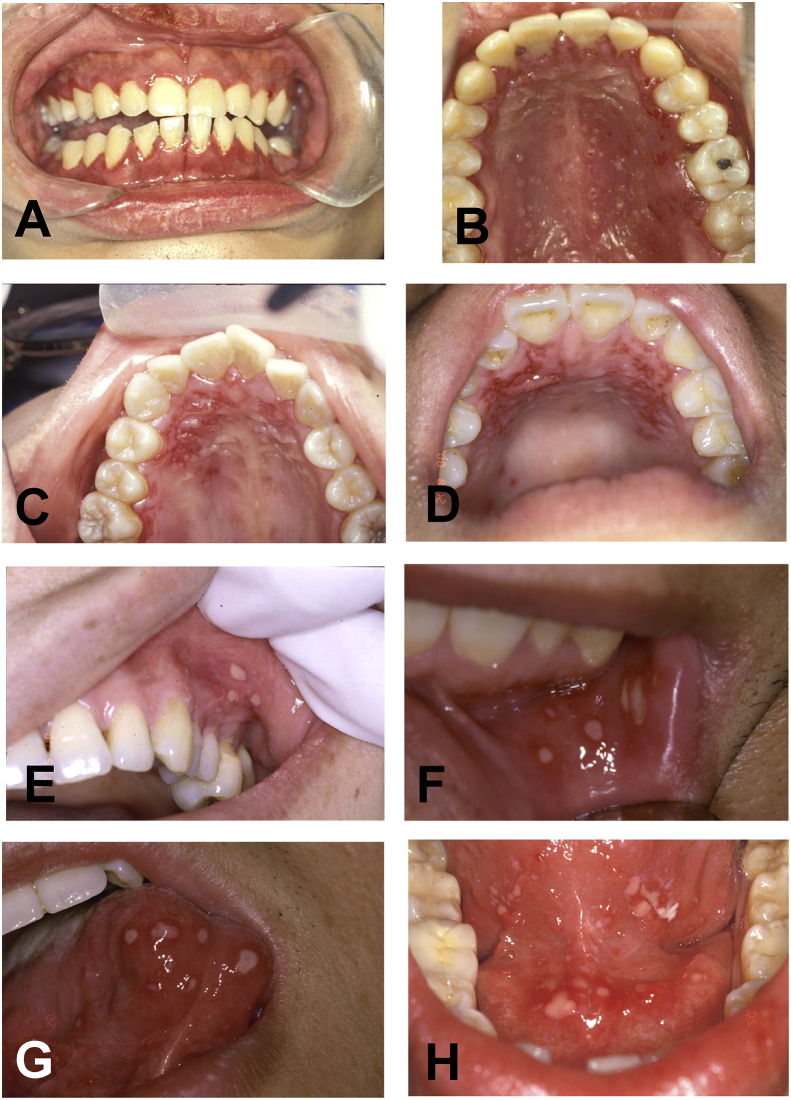
HGS is caused by HSV-1 infection. HGS can be divided into primary HGS (also known as acute HGS or primary herpes) and secondary HGS (also called as secondary herpes or recurrent herpes simplex infection). Primary HGS usually affects children between the ages of 6 months and 5 years, with the peak prevalence occurring between 2 and 3 years of age, but it may affect adults. The oral manifestations of primary HGS include multiple vesicles, erosions, and small or large ulcerations on both movable and attached oral mucosae (such as gingiva and hard palate).1,2 In all cases, the entire gingiva is enlarged, painful, and extremely erythematous (Fig. 1A and B). Mild primary HGS usually resolves within 5–7 days, but severe cases may last 2 weeks. Secondary HGS usually affect keratinized mucosa bound to bone (attached gingiva and hard palate).1 The lesions begin as small vesicles that rapidly collapse to form a cluster of erythematous macules or ulcerations especially on the focal areas of hard palate (Fig. 1C and D).
Figure 1.
Clinical photographs of herpetic gingivostomatitis (HGS) and herpetiform aphthous ulcerations (HAU). (A and B) Primary HGS in a 25-year-old male patient showing multiple vesicles, erosions, and small or large ulcerations on the whole maxillary and mandibular gingivae and parts of the hard palate. The entire gingiva is enlarged, painful, and extremely erythematous. (C and D) Secondary HGS in two adult male patients demonstrating a cluster of erythematous macules or ulcerations on the focal areas of hard palate. (E, F, G and H) HAU in four adult patients exhibiting groups of small ulcerations on the upper labial mucosa (E), lower labial mucosa (F), ventral tongue mucosa (G), and floor of mouth mucosa (H).
HAU is a specific type of recurrent aphthous stomatitis and it often presents with groups of several small-sized (1–3 mm in diameter) ulcerations on the movable or non-keratinized oral mucosae (such as upper and lower labial mucosae, buccal mucosa, ventral tongue mucosa, and floor of mouth mucosa) (Fig. 1E, F, G and H). HAU lesions often heal within 7–10 days.1, 2, 3, 4, 5
In summary, HGS usually affects keratinized or non-movable mucosae (gingiva and hard palate) but HAU often occurs on non-keratinized or movable mucosa (labial or buccal mucosa, ventral tongue mucosa, and floor of mouth mucosa), and this is the major difference between the two oral diseases.
Declaration of Competing Interest
The authors have no conflicts of interest relevant to this article.
References
- 1.Neville B.W., Damm D.D., Allen C.M., Chi A.C. Viral infections and allergies and immunologic diseases. In: Neville B.W., Damm D.D., Allen C.M., Chi A.C., editors. 4th ed. vols. 218–24. Elsevier; St Louis: 2016. pp. 303–308. (Oral and maxillofacial pathology). [Google Scholar]
- 2.Tovaru S., Parlatescu I., Tovaru M., Cionca L. Primary herpetic gingivostomatitis in children and adults. Quintessence Int. 2009;40:119–124. [PubMed] [Google Scholar]
- 3.Tappuni A.R., Kovacevic T., Shirlaw P.J., Challacombe S.J. Clinical assessment of disease severity in recurrent aphthous stomatitis. J Oral Pathol Med. 2013;42:635–641. doi: 10.1111/jop.12059. [DOI] [PubMed] [Google Scholar]
- 4.Chiang C.P., Chang J.Y.F., Sun A. Examination of serum hematinics and autoantibodies is important for treatment of recurrent aphthous stomatitis. J Formos Med Assoc. 2018;117:258–260. doi: 10.1016/j.jfma.2017.12.016. [DOI] [PubMed] [Google Scholar]
- 5.Chiang C.P., Chang J.Y.F., Wang Y.P., Wu Y.H., Wu Y.C., Sun A. Recurrent aphthous stomatitis - Etiology, serum autoantibodies, anemia, hematinic deficiencies, and management. J Formos Med Assoc. 2019;118:1279–1289. doi: 10.1016/j.jfma.2018.10.023. [DOI] [PubMed] [Google Scholar]