Abstract
Background: The burden of HIV/AIDS is ever increasing, affecting populations all over the world. Along with the disease, its effects and consequences on bone health are also on a rise. A commonly used drug in managing HIV, “Tenofovir” has been shown to affect bone health, specifically on prolonged usage. Osteomalacia and osteoporosis secondary to drug induced Fanconi syndrome and the disease itself, could lead to pathological/fragility fractures with trivial trauma. Case description: A 45 year old female on antiretroviral drugs (ART) for HIV, presented with right hip pain and inability to bear weight. She has had similar symptoms previously in the left hip which resolved after 6 weeks of limited weight bearing. Anteroposterior and lateral radiographs of pelvis with hips showed bilateral sub-trochanteric fractures; healed on the left side and displaced on the right side. The patient was managed with cessation of tenofovir and right side proximal femoral nail anti-rotation (PFNA). Patient was lost to follow up but had started to ambulate independently with a cane, by the end of 6 weeks, before she succumbed to systemic complications. Conclusion: Patients receiving antiretrovirals especially tenofovir should be regularly investigated for their renal impairment and bone health. Fixation of pathological fractures and early mobilization are important to prevent prolonged bed immobilization and associated complications in these immunocompromised patients.
Keywords: Tenofovir, fragility fractures, fanconi syndrome, hip fractures, PFNA, sub-trochanteric fracture, osteoporosis
Introduction
With the advent of antiretroviral drugs therapy (ART), there is significant increase in life expectancy and reduction in associated morbidity and mortality in patients infected with human immunodeficiency virus (HIV) [1,2]. However, the long-term use of ART has several adverse effects like dyslipidemia, diabetes mellitus, and abnormalities related to bone metabolism [3,4]. Metabolic bone disorders in HIV patients are common, leading to premature osteoporosis and increased risk of fractures [5,6]. Although the mechanism for osteoporosis is not clearly understood and both HIV infection itself and the antiretroviral medications have been described as contributing factors for bone loss and associated fragility fractures [3,7]. Proximal femur is a common site for fragility fractures and we report a unique case of bilateral sub trochanteric (ST) femur fractures in a 45 years old HIV infected female on ART, with an objective to highlight the unlikely association of ART with such fractures. Additionally, we reviewed the literature to assess similar cases and their management.
Case report
A 45 year old HIV infected female presented to the outdoor patient department (OPD) of our institute with right hip pain following a trivial fall from her bed, 3 weeks back. She also had inability to bear weight on the right lower limb. Patient’s HIV infection was well controlled with normal range of CD4+ counts and viral load of 40 copies HIV RNA/mL. Patient was on regular ART since April 2014. She was initially put on Zidovudine 300 mg BD, Lamivudine 300 mg OD and Efavirenz 600 mg OD for four months, after which she developed Zidovudine induced anemia. In August 2014, Zidovudine was replaced with Tenofovir 300 mg OD along with Lamivudine and Efavirenz. Patient tolerated the doses of the ART well for approximately 5 years, until she was admitted for pain and inability to bear weight on her right hip. On probing she also gave history of left hip pain which started about 3 months before the pain in the right side and subsided on its own after one and a half months of limited weight bearing on the left side, before resuming full weight bearing. She had been taking calcium and vitamin D supplements with subcutaneous injection of Teriparatide for 2 months, for osteoporosis. Bilateral hip examination revealed tenderness over right proximal thigh without any gross deformity. Radiographs showed right ST femur fracture and a healed left ST fracture of the femur (Figure 1A, 1B). Laboratory findings revealed anaemia (Hemoglobin-9 g/dl), hypophosphatemia (1.3 mg/dL), hypokalemia (2.7 mmol/L), hyperchloremia (110 mmol), mild hypocalcemia (7.9 mg/dL), and an elevated alkaline phosphatase level (375 U/L); indicating drug induced Fanconi syndrome. Her ART was modified and Tenofovir was switched with Abacavir 600 mg OD after admission.
Figure 1.
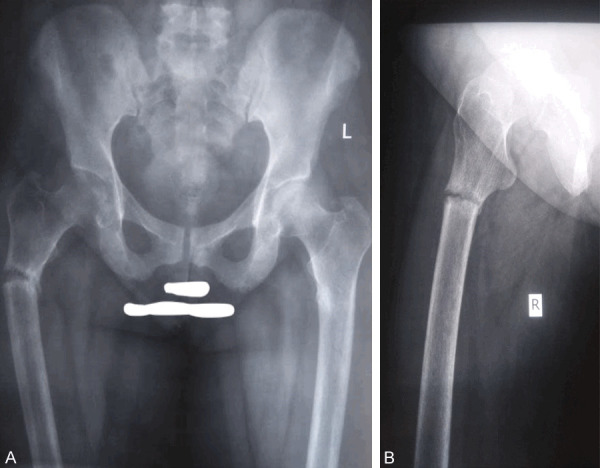
A. Pre-operative anteroposterior radiograph of Bilateral hip with femur. B. Pre-operative lateral view of right hip with femur.
Closed reduction and internal fixation for right ST femur fracture, with intramedullary proximal femoral nail anti rotation (PFNA) was done (Figure 2A-D). The left sided fracture had healed clinically and radiologically, and hence no intervention was done. Post-operative period was uneventful and patient was mobilized in wheel chair and discharged after 2 days. Bone mineral density (BMD) test of the patient gave a T-score of -3.0 at lumber spine and -2.7 at hip. Patient followed up after 2 weeks of surgery for wound inspection and suture removal. She was relatively pain free and could stand with axillary crutches. The patient’s general condition subsequently deteriorated, and she developed renal failure. She was lost to follow up and we could not assess her fracture union. 2 months later her husband informed us that she had expired due to renal complications and sepsis. She had started to walk independently with aid of a cane, by the end of 6 weeks post-operatively without pain, before succumbing to the systemic complications.
Figure 2.
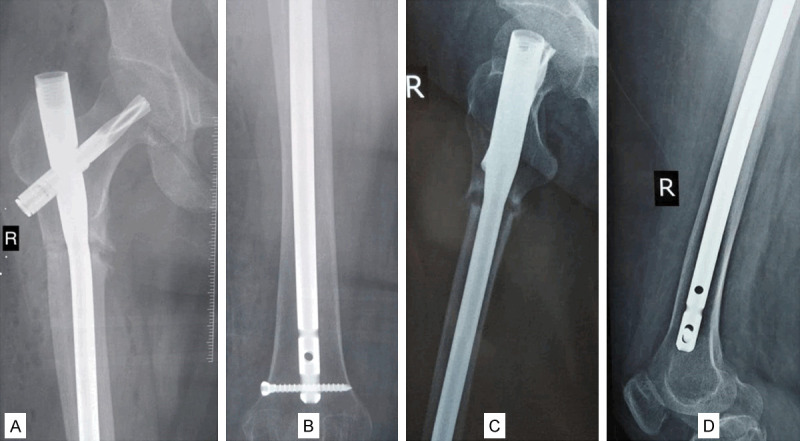
A. Post-operative anteroposterior radiograph of right hip with femur; B. Post-operative anteroposterior radiograph of right distal femur; C. Post-operative lateral radiograph of right hip with femur; D. Post-operative lateral radiograph of right distal femur.
Discussion
HIV infected patients can develop premature osteoporosis leading to 3.7 times increased risk of fractures than non-HIV patients [3,5]. HIV infection is associated with decreased BMD mediated by increased bone turnover and osteoclastic activity [8]. In addition to the HIV infection per se, adverse reactions associated with the commonly prescribed antiretroviral medications also contribute to this increased risk of fractures.
A literature search for the fractures of hip in patients on antiretroviral drugs was done electronically through PubMed, Scopus and Embase databases on 2nd May, 2020, using applicable Key words (Table 1). 6 studies have described fragility fractures around the hip joint in patients on ART (Table 2) [9-14].
Table 1.
Search results with key words
| Database | Results |
|---|---|
| PubMed | 48 |
| ((((((“anti retroviral agents”[Pharmacological Action] OR “anti-retroviral agents”[MeSH Terms]) OR (“antiretroviral”[All Fields] AND “agents”[All Fields])) OR “antiretroviral agents”[All Fields]) OR “antiretroviral”[All Fields]) OR “antiretrovirally”[All Fields]) OR “antiretrovirals”[All Fields]) AND ((((((“therapeutics”[MeSH Terms] OR “therapeutics”[All Fields]) OR “therapies”[All Fields]) OR “therapy”[MeSH Subheading]) OR “therapy”[All Fields]) OR “therapy s”[All Fields]) OR “therapys”[All Fields]) AND (((((((((“fractur”[All Fields] OR “fractural”[All Fields]) OR “fracture s”[All Fields]) OR “fractures, bone”[MeSH Terms]) OR (“fractures”[All Fields] AND “bone”[All Fields])) OR “bone fractures”[All Fields]) OR “fracture”[All Fields]) OR “fractured”[All Fields]) OR “fractures”[All Fields]) OR “fracturing”[All Fields]) AND (“hiv”[MeSH Terms] OR “hiv”[All Fields]) AND ((“hip fractures”[MeSH Terms] OR (“hip”[All Fields] AND “fractures”[All Fields])) OR “hip fractures”[All Fields]) | |
| Embase | 46 |
| ‘antiretroviral agent fracture hiv hip fractures’ OR (antiretroviral AND (‘agent’/exp OR agent) AND (‘fracture’/exp OR fracture) AND (‘hiv’/exp OR hiv) AND (‘hip’/exp OR hip) AND (‘fractures’/exp OR fractures)) | |
| Scopus | 28 |
| (antiretroviral AND therapy AND hip AND fracture AND HIV) |
Table 2.
Relevant literature review (Pubmed, Embase & Scopus)
| SL. NO. | AUTHOR | YEAR | NO. OF PATIENTS | AGE | SEX | SIDE | DIAGNOSIS | ART DRUGS | SURGERY | FOLLOW UP | CONCLUSION |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Rebelledo | 2011 | 1 | 54 | T | Bilateral | Right Basicervical neck fracture | Tenofovir, lamivudine/zidovudine, tenofovir discontinued and started on lopinavir/ritonavir | Right sided TFN, left sided TFN, teriparatide | 4, 6 week and 2 years | Fracture healed uneventfully |
| Left intertrochanteric fracture with HIV | |||||||||||
| 2 | Chaganty | 2019 | 1 | 35 | M | Bilateral | Bilateral femoral neck fracture with HIV | Zidovudine, Lamivudin | Left sided valgus osteotomy and DHS fixation | 6 months | HIV and retroviral drugs can lead to unrecognized stress fractures |
| 3 | Marco | 2017 | 1 | 14 | F | Bilateral | Femoral neck fracture with HIV | Abacavir, kaletra, tenofovir | CRIF with locking plates | 8 weeks, 10 weeks | Antiretroviral drugs may cause unrecognized fractures due to side effects |
| 4 | Brim | 2007 | 1 | 45 | F | Right | Femoral neck fracture with HIV | Nelfinavir plus lamivudine and zidovudine, later lopinavir/ritonavir, tenofovir, and didanosine | Right hip hemiarthroplasty | Monthly follow ups | Tenofovir induced Fanconi syndrome and fractures |
| 5 | Moon | 2018 | 1 | 51 | M | Bilateral | Left Femoral neck fracture and right Intertrochanteric femur fracture with Chronic HBV | Adefovir and tenofovir | Left THR and right sided CRIF with cephalomedullary nail | 3 months and 12 months | Orthopaedic surgeons should consider the possibility of hypophosphatemic osteomalacia if patients receiving antiviral drug |
| 6 | You Sung Suh | 2017 | 1 | 45 | M | Right | Right I/T femur fracture | Lamivudine and tenofovir | Right sided cephalomedullary nail | NA | Regularly renal toxicity and bone metabolism in patients on tenofovir for early diagnosis before its progression to pathologic fractures |
Rebelledo [10] described bilateral pathological hip fractures; neck of femur (NOF) fracture on the right and intertrochanteric (IT) on the left side, in a 54 years old patient with HIV infection on ART. Both the fractures were fixed with Trochanteric fixation nails (TFN) and they united uneventfully.
Bilateral NOF fractures in patients on ART were described by Changanty [14] and Marco [13] in their respective reports and they concluded that HIV and ART can lead to unrecognised stress fractures.
Moon [12] described a case of left NOF and right IT femur fractures in a 51 year old male, on antiviral medications (Adefovir and Tenofovir). They concluded that possibility of hypophosphatemic osteomalacia should be considered in patients receiving these drugs.
2 studies reported unilateral hip fractures; Brim [12] described a 45 year old female who was HIV positive and was on ART. She was diagnosed with right NOF fracture and she underwent hemiarthroplasty. Her fracture was termed a result of Tenofovir induced Fanconi syndrome and subsequent osteoporosis, similar to the mechanism which induced the fractures in the present case (Figure 3). Similarly, a 45 year old male who developed right IT femur fragility fracture was reported by Yousungsuh [11]. The patient was on Tenofovir with Lamivudine and the authors concluded that the renal toxicity and bone metabolism disorder due to these drugs should be regularly screened for, to avoid such fragility fractures.
Figure 3.
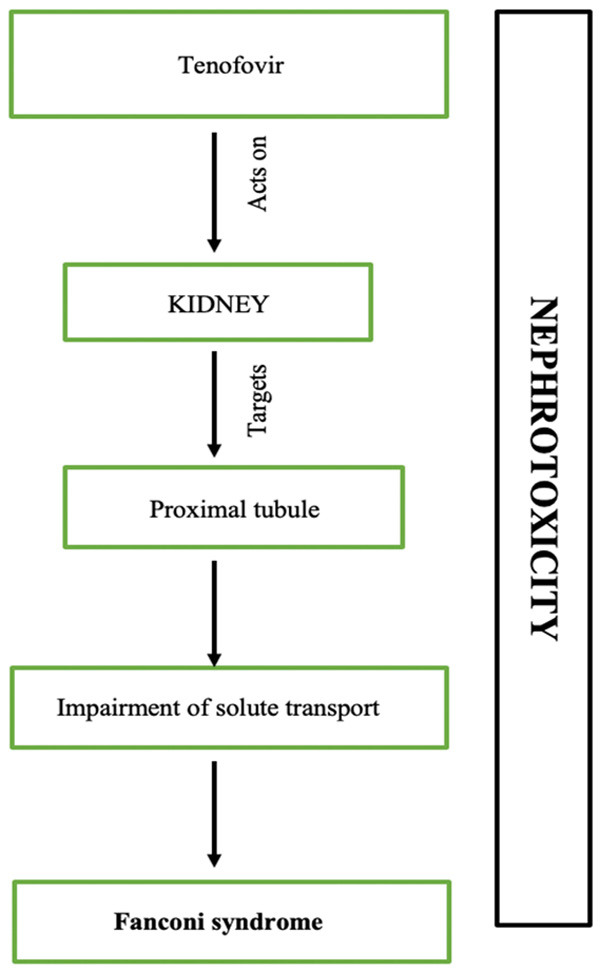
Pathogenesis of Fanconi syndrome in patients on Tenofovir.
Tenofovir, a retroviral drug which is a nucleotide reverse transcriptase inhibitor, prevents the action of reverse transcriptase required for HIV viral production [15]. It has been associated with development of Fanconi syndrome, which can lead to osteomalacia and pathological bone fractures [16-20]. Incidence of bilateral proximal femur fragility fractures in such a scenario although is very rare, with only 4 previously published cases reporting either neck or IT femur fractures. The present case is unique because both the fractures were present in the subtrochanteric region which has not been reported before, adding to its novelty.
Although the implants may vary but the principles of management of these fractures remain the same with requirement of early fixation and mobilisation. None of the reported cases were treated conservatively, although optimising the patient by reducing the viral load and correcting the metabolic parameters are equally important. Early mobilisation and reduced time on the bed are necessary for better quality of life and this also prevents dreaded complications like bed sores, deep vein thrombosis and venous thromboembolism. Although the union in the present case could not be established, these stress/fragility fractures tend to heal well.
Overall, the awareness of association of ART and fragility hip fractures is extremely important for early diagnosis and management. A multi-pronged collaborative approach by the orthopaedic surgeons and the nephrologists could reduce the associated morbidity and mortality.
Conclusion
HIV infected patients taking ART treatment are prone to renal complications with associated metabolic bone disorder, which can cause unsuspected fragility fractures. It is vital to switch to alternative safer drugs to prevent systemic complications. Such fractures around the hip joint need prompt diagnosis, reduced viral load, metabolic corrections, surgical fixation and early mobilisation, for optimal outcomes.
Acknowledgements
All the procedures performed involving the patients were in accordance with the highest ethical standards of the institution and was approved by the departmental review board. Informed consent from the participant/next of the kin was obtained for the study and publication.
Disclosure of conflict of interest
None.
References
- 1.Palella FJ Jr, Delaney KM, Moorman AC, Loveless MO, Fuhrer J, Satten GA, Aschman DJ, Holmberg SD. Investigators Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV outpatient study investigators. N Engl J Med. 1998;338:853–856. doi: 10.1056/NEJM199803263381301. [DOI] [PubMed] [Google Scholar]
- 2.Lau B, Gange SJ, Moore RD. Risk of non-AIDS-related mortality may exceed risk of AIDS-related mortality among individuals enrolling into care with CD41 counts greater than 200 cells/mm3 . J Acquir Immune Defic Syndr. 2007;44:179–187. doi: 10.1097/01.qai.0000247229.68246.c5. [DOI] [PubMed] [Google Scholar]
- 3.Brown TT, Qaqish RB. Antiretroviral therapy and the prevalence of osteopenia and osteoporosis: a meta-analytic review. AIDS. 2006;20:2165–2174. doi: 10.1097/QAD.0b013e32801022eb. [DOI] [PubMed] [Google Scholar]
- 4.Behrens G, Dejam A, Schmidt H, Balks HJ, Brabant G, Körner T, Stoll M, Schmidt RE. Impaired glucose tolerance, beta cell function and lipid metabolism in HIV patients under treatment with protease inhibitors. AIDS. 1999;13:F63–70. doi: 10.1097/00002030-199907090-00001. [DOI] [PubMed] [Google Scholar]
- 5.Prior J, Burdge D, Maan E, Milner R, Hankins C, Klein M, Walmsley S. Fragility fractures and bonemineral density in HIV positive women: a case-control population based study. Osteoporos Int. 2007;18:1345–1353. doi: 10.1007/s00198-007-0428-7. [DOI] [PubMed] [Google Scholar]
- 6.Triant VA, Brown TT, Lee H, Grinspoon SK. Fracture prevalence among human immunodeficiency virus (HIV)-infected versus non-HIV-infected patients in a large U.S. healthcare system. J Clin Endocrinol Metab. 2008;93:3499–3504. doi: 10.1210/jc.2008-0828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tebas P, Powderly WG, Claxton S, Marin D, Tantisiriwat W, Teitelbaum SL, Yarasheski KE. Accelerated bone mineral loss in HIV-infected patients receiving potent antiretroviral therapy. AIDS. 2000;14:F63–67. doi: 10.1097/00002030-200003100-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yin MT, McMahon DJ, Ferris DC, Zhang CA, Shu A, Staron R, Colon I, Laurence J, Dobkin JF, Hammer SM, Shane E. Low bone mass and high bone turnover in postmenopausal human immunodeficiency virus-infected women. J Clin Endocrinol Metab. 2010;95:620–629. doi: 10.1210/jc.2009-0708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moon NH, Shin WC, Do MU, Cho HJ, Suh KT. An uncommon case of bilateral pathologic hip fractures: antiviral drug-induced osteomalacia in a patient with hepatitis B. Hip Pelvis. 2018;30:109–114. doi: 10.5371/hp.2018.30.2.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rebolledo BJ, Unnanuntana A, Lane JM. Bilateral pathologic hip fractures associated with antiretroviral therapy: a case report. J Bone Joint Surg Am. 2011;93:e78. doi: 10.2106/JBJS.J.00885. [DOI] [PubMed] [Google Scholar]
- 11.Suh YS, Chun D, Choi SW, Lee H, Nho JH, Kwon SH. Pathologic femoral fracture due to tenofovir-induced fanconi syndrome in patient with chronic hepatitis B: a case report. Medicine (Baltimore) 2017;96:e8760. doi: 10.1097/MD.0000000000008760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brim NM, Cu-Uvin S, Hu SL, O’Bell JW. Bone disease and pathologic fractures in a patient with tenofovir-induced fanconi syndrome. AIDS Read. 2007;17:322–328. [PubMed] [Google Scholar]
- 13.Marco P, Cristian A, Isabel GM, Veronica V, Juan H. Bilateral hip fracture in adolescents with antiretroviral treatment. J Am Acad Orthop Surg Glob Res Rev. 2017;1:e005. doi: 10.5435/JAAOSGlobal-D-17-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chaganty SS, James D. Bilateral sequential femoral neck stress fractures in young adult with HIV infection on antiretroviral therapy: a case report. World J Orthop. 2019;10:247–254. doi: 10.5312/wjo.v10.i6.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fung HB, Stone EA, Piacenti FJ. Tenofovir disoproxil fumarate: a nucleotide reverse transcriptase inhibitor for the treatment of HIV infection. Clin Ther. 2002;24:1515–1548. doi: 10.1016/s0149-2918(02)80058-3. [DOI] [PubMed] [Google Scholar]
- 16.Verhelst D, Monge M, Meynard J. Fanconi’s syndrome and renal failure induced by tenofovir: a first case report. Am J Kidney Dis. 2002;40:1331–1333. doi: 10.1053/ajkd.2002.36924. [DOI] [PubMed] [Google Scholar]
- 17.Earle KE, Seneviratne T, Shaker J, Sboback D. Fanconi’s syndrome in HIV1 adults: report of three cases and literature review. J Bone Miner Res. 2004;19:714–721. doi: 10.1359/jbmr.2004.19.5.714. [DOI] [PubMed] [Google Scholar]
- 18.Clarke BL, Wynne AG, Wilson DM, Fitzpatrick LA. Osteomalacia associated with adult Fanconi’s syndrome: clinical and diagnostic features. Clin Endocrinol (Oxf) 1995;43:479–490. doi: 10.1111/j.1365-2265.1995.tb02621.x. [DOI] [PubMed] [Google Scholar]
- 19.Wanner DP, Tyndall A, Walker UA. Tenofovir-induced osteomalacia. Clin Exp Rheumatol. 2009;27:1001–1003. [PubMed] [Google Scholar]
- 20.Perrot S, Aslangul E, Szwebel T, Caillat-Vigneron N, Le Jeunne C. Bone pain due to fractures revealing osteomalacia related to tenofovir-induced proximal renal tubular dysfunction in a human immunodeficiency virus-infected patient. J Clin Rheumatol. 2009;15:72–74. doi: 10.1097/RHU.0b013e31819c20d8. [DOI] [PubMed] [Google Scholar]


