Abstract
Trochanteric hip fractures may be fixed with either sliding hip screws or intramedullary devices. Current UK guidance is that intramedullary fixation should be used for AO/OTA 31A3 fractures but does not stipulate length of nail. We present a systematic review comparing short and long nails for these injuries in older patients.
Three studies were randomized, all with methodological concerns. None demonstrated a clinically significant difference in outcome.
There is no good evidence to support long over short intramedullary devices in this scenario. Evidence is required to demonstrate whether the potentially increased surgical risk confers any benefits in this group.
Keywords: Hip fracture, Intramedullary, Cephalomedullary, Fragility fracture, Osteoporosis
1. Introduction
Hip fractures are life-changing and frequently fatal or pre-terminal injuries occurring predominantly in older patients, in the context of deteriorating bone health and physiological reserve. Their impact on quality of life is profound and the goals of managing them centre on regaining as much function and quality of life as is possible; notwithstanding this, it has been demonstrated that patients experience a permanent decline in self-reported quality of life after hip fracture.1 A recent initiative in the United Kingdom (UK) to improve hip fracture care in the form of both national guidelines and quality standards and a registry with incentivization payments for compliance has led to reduced time to surgery, a higher proportion of patients being assessed pre-operatively by specialists in medicine for older people and an overall reduction in mortality.2 Overall hip fracture remains, however, an enormous burden on both patients and healthcare systems, with an estimated annual economic impact in excess of £1 bn.3
The approach to treatment is broadly based on replacement surgery for fractures occurring within the capsule of the hip joint and fixation of those outside it.4 The sliding hip screw (SHS) has been the standard of care for stable trochanteric fractures for more than two decades but intramedullary or cephalomedullary devices, originally used primarily in subtrochanteric femoral fractures, have seen increasing use in trochanteric fractures.5 Technical benefits of the implant include on-axis fixation, a provision of a buttress against further collapse when trochanteric comminution is a concern and a largely percutaneous technique.
Guidance in the UK remains to prefer sliding hip screw over intramedullary fixation for AO/OTA 31A1 and A2 fractures,4,6 as multiple clinical trials have failed to demonstrate a measurable benefit to patients from intramedullary fixation. Where there is clear guidance, however, is in the A3 fracture group which represents a highly unstable transverse or reverse oblique pattern biomechanically unsuited to off-axis fixation with the SHS.
In the context of increasing interest in intramedullary fixation, a number of manufacturers introduced shorter devices designed specifically for the fixation of more proximal fractures. These offer the benefits of an instrumentation system requiring no radiographically-guided stereotactic bolt placement at the distal end and offering the ability to introduce them without the use of flexible reamers in the femur and hence with a shorter operative time than their longer counterparts. The early generations of this device experienced high rates of failure with metallurgy, diameter, bow, distal locking bolt and distal taper all contributing to a high periprosthetic fracture rate. Subsequent generations have addressed these issues but, notwithstanding, many surgeons routinely prefer a longer variant to minimize exposure to these risks.
Whilst the logic of a longer device with significant distal fixation may be appealing, it should not be seen as a benign solution. It has recently been demonstrated that a significantly increased mortality exists in those patients undergoing intramedullary fixation over those with sliding hip screw fixation.7 Whilst the aetiology of this is not fully understood, and this work did not separate short and long nails, it must be taken into consideration that an operation that takes longer, involves more femoral instrumentation and thus may create more embolic phenomena and entail more, hidden blood loss may play its part in contributing to this difference.
Physiological insult is an important factor in hip fracture surgery – the patients are, by definition, frail and the key aim of surgery is to leave the patient recumbent for as short a time as possible. To this end, one of the key performance indicators in the NHFD report is the mobilization of the patient on the day after surgery, a target missed in one in five patients and with post-operative hypotension being one of the key causes cited in patients where this was not achieved.
Another challenging problem is that of post-operative confusion and delirium (POCD). A number of factors have been associated with this and anaesthetic techniques favouring spinal over general anaesthesia and using the lightest possible sedation have become popular. A recent retrospective, registry-based study in Canada reported a 6% increase in risk of POCD per additional half-hour of surgery in addition to that seen in association with general anaesthesia8 – in this context, it is again clear that shorter operations can confer patient benefit in this high-risk patient group. It has yet to be well-demonstrated whether there is a time benefit to either device.
In this systematic review we identify and summarize the results of studies comparing short and long intramedullary devices for the fixation of extracapsular fractures of the hip in patients aged over 60 years.
2. Methods
This systematic review complied with PRISMA guidelines and was registered with PROSPERO (128103).
2.1. Eligibility criteria
We included only randomized controlled trials and retrospective or prospective cohort studies, thereby analysing a minimum level III evidence. These studies compared long with short intramedullary fixation in patients aged 60 years or over with AO/OTA 31A1, 2 or 3 extracapsular hip fractures. To be included, each study had to report on at least one outcome measures from: quality of life (encompassing self-reported mobility); objective functional assessments of mobility; length of acute in-patient stay; change of residential status; duration of surgery; blood loss; post-operative venous thromboembolism; peri-prosthetic fracture; failure of fixation; death.
2.2. Search strategy
Embase, MEDLINE, Web of Science Core Collection and Google Scholar were queried to identify the widest possible list of potential studies for inclusion.9
Search strategy based on; (Intertrochanteric or pertrochanteric or extracapsular) and (intramedullary or cephalomedullary) and (long or short).
The timeframe of the search was not limited. The language was limited to English.
2.3. Study selection
Two independent reviewers identified eligible studies from the search in line with the eligibility criteria. Concordance review was then performed by a third reviewer.
2.4. Risk of bias assessment
Randomized studies were assessed using the RoB2 tool from the Cochrane Collaboration10 and non-randomized studies with the ROBINS-I tool.11
2.5. Data synthesis
This review focused on narrative synthesis, due to the diverse range of outcomes and small numbers of eligible studies.
3. Results
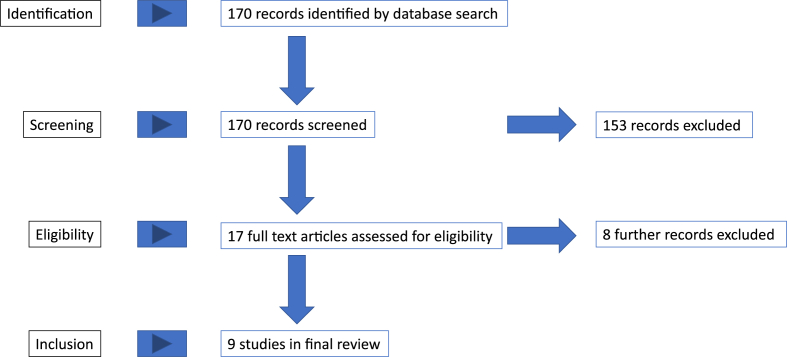
The results yielded by the literature search are outlined in Fig. 1.
Fig. 1.
Flowchart of studies in review.
4. Methodologies
Three studies, Okcu et al., Galanopoulos et al. and Shannon et al. had a randomized, controlled design. Okcu's work was planned as a pilot study and hence did not use a sample size calculation, whereas Shannon used a sample size appropriate to the outcome measure but not to the population on whom it was used, as it was informed by the MCID for other operations. Patients with dementia were also excluded. Galanopoulos et al. did not describe an a priori sample size calculation. All the randomized investigations were assessed to have some concerns over risk of bias.
Of the non-randomized studies, one involved prospective follow-up of non-randomized cohorts and the remainder retrospective review of clinical records. All of these studies were either at serious risk of bias or reported inadequate information to make a judgement.
4.1. Patients and fracture classification
All studies eligible for inclusion had broadly similar demographics in terms of age and sex. American Society of Anesthesiologists (ASA) score was only reported in two studies (Table 1). Many studies were excluded from our results due to inclusion of younger adults; of those included, Shannon et al. described an inclusion criterion of age >18 years but did not recruit anybody below 60 years of age.
Table 1.
Eligible studies, showing sample characteristics, by group.
| Study | Country, year | Study design (level of evidence) | Device model (long/short) |
Sample size Long/Short |
OTA classification (31A1/2/3) | Length of follow-up (months) | ASA 3 or 4 | Age in yrs (range) | Gender M/F | Risk of bias | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Okcu G et al.12 | Turkey, | RCT (II) | PFNA/PFNA 240 mm | 18 | 15 | 0/0/33 | Long 1512, 13, 14, 15, 16, 17, 18, 19, 20 | N/A | Long 81 (73–89) | Long 4/14 | Some concerns |
| 2013 | Short 1412, 13, 14, 15, 16, 17, 18, 19, 20 (p = 0.153) |
Short 78 (67–95) (p = 0.255) |
Short 4/11 (p = 0.767) | ||||||||
| Kleweno C et al.13 | USA, 2014 |
Retrospective cohort (III) | Gamma 2,3, TFNA/Gamma 3, TFNA | 340 | 219 | 416 (A1+A2) /143 |
12–85 | 426 (75%) | 84 (65–102) | 155/404 | Some concerns |
| Li Z et al.14 | China, 2015 |
Retrospective cohort (III) | PFNA/PFNA | 59 | 97 | 45/71/40 (p = 0.210) | >12 | 29 (18.6%) | Long 74.8 ( ±8.15) | Long 20/39 | Serious risk |
| Short 76.8 ( ±6.5) (p = 0.1) |
Short 46/51 (p = 0.116) | ||||||||||
| Guo X et al.15 | China, 2015 |
Retrospective cohort (III) | Gamma 3/Gamma 3 180 mm | 76 | 102 | Long 26/50/0 | 12–24 | N/A | Long 78.9 ( ±8.8) | Long 43/33 | Serious risk |
| Short 47/55/0 (p = 0.037) | Short 82.7 ( ±9.9) (p = 0.003) |
Short 42/60 (p = 0.322) | |||||||||
| Raval P et al.16 | UK, 2016 |
Retrospective cohort (III) | PFNA/PFNA 240 mm | 40 | 40 | Long 9/24/7 | 12 | N/A | Long 76.1 ( ±8.7) | Long 13/27 | No info |
| Short 12/24/4 (p = 0.536) | Short 77.1 ( ±9.2) (p = 0.806) |
Short 11/29 (p = 0.625) | |||||||||
| Frisch N et al.17 | USA, 2017 |
Retrospective cohort (III) | InterTAN/InterTAN | 97 | 72 | 0/169 (A2+A3) | >8 | N/A | Long 76.3 ( ±15.2) | Long 30/67 | No info |
| Short 76.2 ( ±12.3) (p = 0.621) |
Short 18/54 (p = 0.501) | ||||||||||
| Galanopoulos I et al.18 | Greece, 2018 |
Randomized Prospective (II) | VeroNail TN/Affixus | 25 | 25 | All A2/3 | 24 | N/A | 80 (74–93) | 17/33 | Some concerns |
| Liu J et al.19 | USA, 2018 |
Retrospective cohort (III) | InterTAN, Natural, TFNA, T2 recon/InterTAN, Natural, TFNA, T2 recon | 565 | 334 | A1/A2/A3 | 3 | N/A | Long 78.1 | Long 106/228 | Serious risk |
| Short 80.1 (p = 0.0379) | Short 210/355 (p = 0.1064 | ||||||||||
| Shannon S et al.20 | USA, 2019 |
RCT (I) | TFNA, Gamma 3, Affixus/TFNA, Gamma 3, Affixus | 88 | 80 | Long 12/67/9 | 13.9 | N/A | Long 79 (76–82) | Long 25/63 | Some concerns |
| Short 13/61/6 (p = 0.23) | Short 82 (79–84) (p = 0.11) |
Short 20/60 (p = 0.72) | |||||||||
Fracture pattern was heterogeneous, with only one study by Ocku et al. focusing solely on the 31A3 subgroup. Guo et al. included no patients with A3 fractures whereas Frisch et al. and Galanopoulos et al. included no A1 fractures. All the other studies reported outcomes on all three subtypes.
4.2. Surgical factors
All studies reported significantly longer duration of surgery for long nails over short ones. Li, Guo, Raval, Frisch, Liu and Shannon reported higher estimated blood loss in long nail cases than in short nails, with only Li's report not finding this difference statistically significant. Guo, Raval and Liu reported higher transfusion rates in long nail cases, but this was only statistically significant in Guo's dataset.(Table 2).
Table 2.
Surgical characteristics, by group.
| Study | Duration of surgery (minutes) | Estimated blood loss (ml) | Patients requiring transfusion | Length of stay (days) |
|---|---|---|---|---|
| Okcu G et al. 2013 | Long 71.8 (57–94) | /// | /// | Long 4.92, 3, 4, 5, 6, 7, 8, 9 |
| Short 52.6 (34–65) | Short 5.42, 3, 4, 5, 6, 7, 8, 9, 10, 11 | |||
| (p < 001) | (p = 0.51) | |||
| Kleweno C et al. 2014 | Long 70 ( ±35) | /// | /// | /// |
| Short 51 ( ±22) | ||||
| (p < 0.001) | ||||
| Li Z et al. 2015 | Long 60.61 ( ±11.43) | Long 77.97 ( ±31.88) | /// | /// |
| Short 53.08 ( ±8.51) | Short 69.95 ( ±21.55) | |||
| (p < 0.05) | (p = 0.063) | |||
| Guo X et al. 2015 | Long 58.5 ( ±20.3) | Long 90.7 ( ±50.6) | Long 56.7% | Long 12.7 ( ±6.7) |
| Short 43.5 ( ±12.3) | Short 127.8 ( ±85.9) | Short 42.3% (p = 0.041) | Short 12.9 ( ±6.5) | |
| (p = 0.002) | (p = 0.004) | (p = 0.42) | ||
| Raval P et al. 2016 | Long 87 (55–119) | Long 341.7 ( ±191.8) | Long 8/40 | Long 10.9 ( ±4.8) |
| Short 58 (46–70) | Short 172 ( ±156.9) | Short 4/40 (p = 0.210) | Short 11.1 ( ±6.2) | |
| (p = 0.016) | (p = 0.042) | (p = 0.937) | ||
|
Frisch N et al. 2017 |
Long 82.6 ( ±26.4) | Long 208.1 ( ±116.9) | /// | /// |
| Short 63.8 ( ±20) | Short 161.4 ( ±122.4) | |||
| (p = 0.001) | (p = 0.002) | |||
| Galanopoulos I et al. 2018 | Long 54 (35–70) | /// | /// | /// |
| Short 41 (20–51) | ||||
| (p = 0.001) | ||||
| Liu J et al., 2018 | Long 157.0 ( ±50.5 | Long 226.2 ( ±211.8) | Long 330/565 (58.4%) | Long 6.8 |
| Short 139.7 ( ±35.8) | Short 185.5 ( ±168.3) | Short 179/334 (53.6%) | Short 7.2 (p = 0.338) | |
| (p=<0.0001) | (p = 0.0017) | (p = 0.16) @30 days | ||
| Shannon S et al. 2019 | Long 80 | Long 207 | /// | /// |
| Short 51 (p=<0.0001) | Short 70 (p=<0.001) |
4.3. Complications, length of stay and mortality
Data on re-operation were reported in six studies, with low numbers in both groups in all studies. Not all the studies reported indications for re-operation but where data were available, there was no significant difference in rates of infection, peri-prosthetic fracture, avascular necrosis or cut-out.
Of the four studies reporting length of stay, none showed a statistically significant difference between long and short nails (Table 3).
Table 3.
Post-operative surgical problems, by group.
| Study | Re-operation | Mortality | Delayed union/non-union/avascular necrosis | Infection | Peri-prosthetic fracture | Failure/cut-out |
|---|---|---|---|---|---|---|
| Okcu G et al. | Long 2/18 | Long 18.1% | /// | Long 1/18 | /// | Long 1/18 |
| 2013 | Short 0/15 (p = 0.41) | Short 16.6% | Short 1/15 | Short 0/15 | ||
| @1 year (p = 0.9) | ||||||
| Kleweno C et al. | Long 12/340 (3.5%) | 25% | /// | /// | Long 5/340 (1.5%) | Long 11/340 (3%) |
| 2014 | Short 7/219 (3.2%) | Overall @1 yr | Short 6/219 (2.7%) | Short 5/219 (2%) | ||
| Li Z et al. | Long 0/59 | /// | //// | /// | Incl. in reop but not subclassified | Incl. in reop not subclassified |
| 2015 | Short 3/97 | |||||
| (p=<0.05) | ||||||
| Guo X et al. | No absolute number given | 21/178 (11.8%) | Long 0/76 | Long 1/76 | Long 1/76 | Long 0/76 |
| 2015 | Short 1/102 Non-union (p=>0.05) | Short 1/102 (p=>0.05) | Short 1/102 (p=>0.05) | Short 1/102 (p=>0.05) | ||
| Raval P et al. | Long 2/40 | Long 5/40 (12.5%) | /// | Long 0 | Long 2/40 | Long 0/40 |
| 2016 | Short 1/40 (p = 0.556) | Short 3/40 (7.5%) | Short 0 | Short 0/40 | Short 1/40 | |
| (p = 0.456) | ||||||
| Frisch N et al. | /// | /// | /// | Long 3/97 | Long 0/97 | Long 6/97 |
| 2017 | Short 1/72 (p = 0.637) | Short 6/72 (p = 0.013) | Short 1/72 (p = 0.134) | |||
| Galanopoulos I et al. 2018 | /// | /// | Long 0/25 | /// | Long 0/25 | Long 1/25 |
| Short 0/25 | Short 1/25 | Short 0/25 | ||||
| Liu J et al. | 15 pts (90 days) | Long 30/565 (5.3%) | /// | Long 6/565 | Long 3/565 | Long 4/565 |
| 2018 | Short 23/334 (6.9%) | Short 1/334 (p=>0.05) | Short 2/334 (p = 0.7038) | Short 0/334 | ||
| (30 days, p = 0.3322) | ||||||
|
Shannon S et al. 2019 |
Long 8/88 | /// | Long 1/88 Delayed union | Long 2/88 | Long 2/88 | Long 2/88 |
| Short 5/80 (p = 0.72) | Short 0/80 | Short 1/80 | Short 2/80 (p = 1.0) | Short 3/80 (p = 0.67) |
Only four studies reported mortality, and one of these did not report by long versus short group. The results were heterogeneous.
4.4. Functional outcome
Three studies reported a Harris Hip Score, one of which went on to also report an SF-36 functional outcome. Only one study reported a statistically significant difference in HHS, but appropriately observed that whilst the difference was statistically significant, it did not cross the threshold of minimum clinically important difference (Table 4).
Table 4.
Patient-reported outcome measures, by group.
| Study | Harris Hip Score | Other |
|---|---|---|
| Okcu G et al. | Long 79 (59–92) | Parker Palmer Mobility Score |
| Long 5.5± 1.7 | ||
| Short 74 (61–88) | Short 5.2± 1.9 (p = 0.53) | |
| (p0.11) | ||
| Li Z et al. | Long 79.98 ( ±8.90) | |
| Short 76.16 ( ±10.84) | ||
| (p = 0.280) | ||
| Galanopoulos I et al. | Time for WB with single crutch | |
| Long 7.31 weeks (6–9 wks) | ||
| Short 7.85 weeks (6–9 wks) | ||
| Trendelenburg gait | ||
| @3 month - Long 7/25/Short 8/25 | ||
| @12 month - Long 3/25/Short 3/25 | ||
| Leg length discrepancy <1 cm | ||
| Long 2/25 | ||
| Short 3/25 | ||
| Shannon S et al. | Long 71 | SF-36all domains similar for both Short Nail and Long Nail cohorts (No statistically significant difference) |
| Short 76 | ||
| (p = 0.02) but not considered clinically important difference |
5. Discussion
In this systematic review we have identified and summarized the evidence from studies comparing short and long nails used for hip fractures. No robust evidence exists to demonstrate superiority of one over the other in this context.
Key to this evidence gap is the absence of a fully powered randomized clinical trial comparing these implants for fractures in patients over 60 years of age, and especially notable is deficit in evidence focused on the 31A3 fracture, the only one where there is clear guidance to use these implants. Okcu et al. performed a pilot study closest to this, but confined inclusion to reverse oblique patterns rather than including the transverse fractures which also form part of that group. The very low numbers per arm cannot permit much inference from the study, and the choice of Harris Hip Score as the functional outcome measure makes generalizability to the frail, elderly trauma population low. All the other studies either reported non-randomized cohorts or included a broader spectrum of fracture patterns than, under current standards of care, should be managed by SHS.
There exists a preponderance of evidence focusing on what is easily measured, such as failure and revision rates rather than what are increasingly evidently important parameters in hip fracture care such as patient- or carer-reported quality of life. Shannon et al. used the SF-36 instrument, with a power calculation predicated on the minimum clinically important difference for total knee replacement and tibial plateau fracture fixation.21, 22, 23 This study also excluded patients with dementia on the basis of inability to complete the PROM, thereby substantially reducing the generalizability of the findings to a population with a high burden of cognitive impairment. It has been demonstrated that the EuroQol 5-dimension instrument (EQ-5D) can be effectively completed by carers or relatives with a high degree of reliability and, given that its effect size in hip fracture is relatively well-understood and it already forms part of the core outcome set in the United Kingdom for hip fracture research, it would represent a much more appropriate choice of PROM.24,25
Most of the studies included in this review focused on surgical failure or patient death, but given both events are relatively rare, thousands of patients are needed in each arm to power a study capable of detecting a difference in these outcomes and hence minimal weight ought to be attached to the rates reported here. There is variable data on re-operation, with some studies not reporting it by group and minimal data on causes. We sought also to note rates of infection where possible, as this may be contributory in just the same way as mechanical factors.
The data on blood loss must be considered in the context of its estimated nature, especially when the surgical procedure is usually performed through a number of small incisions and most blood is lost into either the femur or the soft tissues surrounding it. That notwithstanding, there is a consistent picture of lower blood loss in short nails across all the studies reporting it, although this is not fully reflected in transfusion requirements. Given international variation in practice and availability of transfusion products, however, this may reflect clinical willingness to tolerate a significant blood loss rather than it being inconsequential.
The duration of surgery has also been shown to be shorter for short nails across all reported studies here. This is entirely logical given the reduced number and complexity of surgical steps and, in the absence of compelling evidence of superior functional outcomes from a longer device, and a strong body of evidence that prolonged surgery causes problems in this patient group, it may be that the time factor should be given more weight when we make our operative decisions. Equally, the quality of the data remains under question when reported from a number of studies which did not clearly define their surgical time in terms of start and finish in relation to surgical steps.
The risk of bias assessments reflect the wider methodological picture that many of the incorporated studies are retrospective in nature and often do not define outcomes or end-points. There is, therefore, often not enough information to judge a risk of bias but a key theme in all the non-randomized studies is the risk that implant was selected by some factor relating to fracture pattern or patient fitness for surgery, thereby introducing large selection bias. The retrospective nature of the reporting and the absence of an a priori plan also renders it nearly impossible to ascertain if reporting is selective as there is no means of knowing what data was available to researchers.
The strength of this review is that it provides evidence relevant to our practice as UK orthopaedic trauma surgeons by focusing on the older patient with an extracapsular fragility fracture of the hip, and highlights specifically where evidence can guide us in our implementation of NICE standards. The studies included in the review are all relatively recently published and a large proportion of them since the last systematic review was published in this area. This is also the first systematic review to be conducted with PROSPERO registration. Its key weakness is that it primarily reports a fairly limited and heterogeneous selection of lower-grade evidence and so must be interpreted in that context. As with all reviews, bibliographic error and exclusion through publication in another language remains a risk.
It bears re-iteration that this report addresses these fractures in older patients and, in younger patients with better bone quality, there may well be justification for a longer device to reflect the biomechanical environment, functional demand and risk: benefit ratio. Such a question would certainly be well worth addressing with an appropriate clinical trial – while these injuries are infinitely rarer in younger patients, the personal and societal cost of their mismanagement may well be heavy. Similarly, we stress the difference between an unstable extracapsular hip fracture and a subtrochanteric fracture and do not suggest this evidence base is generalizable to that injury.
In the older patient with an extracapsular hip fracture, however, there remains no evidence of the superiority of long intramedullary devices over shorter ones and, further, several surgical factors may well contribute to some of the adverse outcomes recently reported when using intramedullary devices in these situations. Given the commonplace use of long devices, we advocate that this evidence gap is urgently addressed to maximise the patient safety and functional gains being achieved under the best practice tariff.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We gratefully acknowledge the assistance of Mr. Tom Roper, Clinical Librarian, Brighton and Sussex NHS Library and Knowledge Service.
References
- 1.Griffin X.L., Fernandez M., Costa M.L. Recovery of health-related quality of life in a United Kingdom hip fracture population. The Warwick Hip Trauma Evaluation--a prospective cohort study. Bone Joint Lett J. 2015 Mar;97-B(3):372–382. doi: 10.1302/0301-620X.97B3.35738. [DOI] [PubMed] [Google Scholar]
- 2.Royal College of Physicians . 2018 Nov 14. National Hip Fracture Database (NHFD) Annual Report 2018; pp. 1–32. London. [Google Scholar]
- 3.Leal J., Gray A.M., Prieto-Alhambra D. Impact of hip fracture on hospital care costs: a population-based study. Osteoporos Int. 2015 Aug 19;27(2):549–558. doi: 10.1007/s00198-015-3277-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Clinical Guideline Centre . 2017 May 8. The Management of Hip Fracture in Adults; pp. 1–664. London. [Google Scholar]
- 5.Page P.R.J., Lord R., Jawad A. vol. 47. Injury. Elsevier Ltd; 2016 Jul 1. pp. 1525–1529. (Changing Trends in the Management of Intertrochanteric Hip Fractures – A Single Centre Experience). 7. [DOI] [PubMed] [Google Scholar]
- 6.OTA Classification, Outcomes. Database Committee The OTA fracture classification compendium - femur. J Orthop Trauma. 2018 Jan;32(Suppl 1):S33–S44. [Google Scholar]
- 7.Whitehouse M.R., Berstock J.R., Kelly M.B. Higher 30-day mortality associated with the use of intramedullary nails compared with sliding hip screws for the treatment of trochanteric hip fractures: a prospective national registry study. Bone Joint Lett J. 2019 Jan;101-B(1):83–91. doi: 10.1302/0301-620X.101B1.BJJ-2018-0601.R2. [DOI] [PubMed] [Google Scholar]
- 8.Ravi B., Pincus D., Choi S., Jenkinson R., Wasserstein D.N., Redelmeier D.A. Association of duration of surgery with postoperative delirium among patients receiving hip fracture repair. JAMA Netw Open. American Medical Association. 2019 Feb 22;2(2) doi: 10.1001/jamanetworkopen.2019.0111. 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bramer W.M., Rethlefsen M.L., Kleijnen J., Franco O.H. Optimal database combinations for literature searches in systematic reviews: a prospective exploratory study. Syst Rev. Systematic Reviews. 2017 Dec 4;6(1):1–12. doi: 10.1186/s13643-017-0644-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sterne J.A.C., Savovic J., Page M.J. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019 Aug 28;2:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 11.Sterne J.A., Hernán M.A., Reeves B.C. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016 Oct 12 doi: 10.1136/bmj.i4919. i4919–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Okcu G., Ozkayin N., Okta C., Topcu I., Aktuglu K. Which implant is better for treating reverse obliquity fractures of the proximal femur: a standard or long nail? Clin Orthop Relat Res. 2013 Sep;471(9):2768–2775. doi: 10.1007/s11999-013-2948-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kleweno C., Morgan J., Redshaw J. Short versus long cephalomedullary nails for the treatment of intertrochanteric hip fractures in patients older than 65 years. J Orthop Trauma. 2014 Jul;28(7):391–397. doi: 10.1097/BOT.0000000000000036. [DOI] [PubMed] [Google Scholar]
- 14.Li Z., Liu Y., Liang Y., Zhao C., Zhang Y. Short versus long intramedullary nails for the treatment of intertrochanteric hip fractures in patients older than 65 years. Int J Clin Exp Med. 2015;8(4):6299–6302. [PMC free article] [PubMed] [Google Scholar]
- 15.Guo X.-F., Zhang K.-M., Fu H.-B., Cao W., Dong Q. A comparative study of the therapeutic effect between long and short intramedullary nails in the treatment of intertrochanteric femur fractures in the elderly. Chin J Traumatol. Elsevier Ltd. 2015 Dec 1;18(6):332–335. doi: 10.1016/j.cjtee.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 16.Raval P., Ramasamy A., Raza H., Khan K., Awan N. Comparison of short vs long anti-rotation in treating trochanteric fractures. Malays Orthop J. 2016 Mar;10(1):22–28. doi: 10.5704/MOJ.1603.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Frisch N.B., Nahm N.J., Khalil J.G., Les C.M., Guthrie S.T., Charters M.A. Short versus long cephalomedullary nails for pertrochanteric hip fracture. Orthopedics. 2017 Mar 1;40(2):83–88. doi: 10.3928/01477447-20161116-01. [DOI] [PubMed] [Google Scholar]
- 18.Galanopoulos I.P., Mavrogenis A.F., Megaloikonomos P.D. Similar function and complications for patients with short versus long hip nailing for unstable pertrochanteric fractures. SICOT-J. 2018 Jun 15;4(7):23–25. doi: 10.1051/sicotj/2018023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu J., Frisch N.B., Mehran N., Qatu M., Guthrie S.T. Short-term medical complications following short versus long cephalomedullary nails. Orthopedics. 2018 Jul 16;41(5):e636–e642. doi: 10.3928/01477447-20180711-03. [DOI] [PubMed] [Google Scholar]
- 20.Shannon S.F., Yuan B.J., Cross W.W., III Short versus long cephalomedullary nails for pertrochanteric hip fractures. J Orthop Trauma. 2019 Oct;33(10):480–486. doi: 10.1097/BOT.0000000000001553. [DOI] [PubMed] [Google Scholar]
- 21.Dattani R., Slobogean G.P., O'Brien P.J. Psychometric analysis of measuring functional outcomes in tibial plateau fractures using the short form 36 (SF-36), short musculoskeletal function assessment (SMFA) and the Western ontario McMaster osteoarthritis (WOMAC) questionnaires. Injury. 2013 Jun 1;44(6):825–829. doi: 10.1016/j.injury.2012.10.020. Elsevier Ltd. [DOI] [PubMed] [Google Scholar]
- 22.Escobar A., Quintana J.M., Bilbao A., Aróstegui I., Lafuente I., Vidaurreta I. Responsiveness and clinically important differences for the WOMAC and SF-36 after total knee replacement. Osteoarthritis Cartilage. 2007 Mar;15(3):273–280. doi: 10.1016/j.joca.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 23.Shannon S.F., Yuan B.J., Cross W.W., III Short versus long cephalomedullary nails for pertrochanteric hip fractures. J Orthop Trauma. 2019 Jun:1–24. doi: 10.1097/BOT.0000000000001553. [DOI] [PubMed] [Google Scholar]
- 24.Parsons N., Griffin X.L., Achten J., Costa M.L. Outcome assessment after hip fracture is EQ-5D the answer? Bone and Joint Research. British Editorial Society of Bone and Joint Surgery. 2014;3(3):69–75. doi: 10.1302/2046-3758.33.2000250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Haywood K.L., Griffin X.L., Achten J., Costa M.L. Developing a core outcome set for hip fracture trials. Bone & Joint Journal. 2014 Aug;96-B(8):1016–1023. doi: 10.1302/0301-620X.96B8.33766. British Editorial Society of Bone and Joint Surgery. [DOI] [PubMed] [Google Scholar]