Abstract
Background
Surgical management of high-grade spondylolisthesis is not only challenging but also controversial, from in situ fusion to complete reduction. We report our results of a safe three-stage spinal procedure in a single surgical session with seven patients diagnosed high-grade spondylolisthesis.
Hypothesis
Posterior fixation combined with interbody fusion is effective on reduction, ossification and clinical outcomes in high-grade spondylolisthesis.
Patients and methods
This study is a retrospective review of patients who underwent surgery between 2016 and 2018. The surgical method involved specific installation for deformity reduction, pedicle screw fixation, correction of lumbosacral kyphosis with a specific distraction maneuver, wide decompression, gradual reduction of the deformity, and sometimes maintenance of the reduction with interbody fusion. Patients were checked out at 2, 6 and 12 months and yearly after the procedure. Clinical, radiological, Visual Analogic Scale (VAS) and Oswestry Disability Index (ODI) outcomes measures were collected.
Results
Seven patients with high-grade spondylolisthesis at L5-S1 (2 patients grade II, 4 patients grade IV and 1 patient grade V), with a median age of 37 years [17; 72] were included. Median follow-up was 24 months [12; 25 months]. All patients have a fused joint at 6 months except one. Median lumbosacral angle (LSA) improved from 76°[59; 85] to 94°[76; 104]. Meyerding grade of 2 cases was stable after surgery, 3 cases with loss of two ranks and 2 cases with loss of one rank. The radiological parameters showed statistically significant difference (p = 0.036) postoperatively. There was not deep infection. Medians VAS and ODI showed improved pain and disability scores.
Conclusion
This procedure allows correct reduction rate of high-grade spondylolisthesis with good clinic-radiologic outcomes. Though surgically demanding, it was safe and reproducible.
Level of evidence
IV, retrospective.
Keys words: High-grade spondylolisthesis, Reduction, Sciatalgia, Lumbosacral kyphosis, Trans-sacral, Pedicle screw
1. Introduction
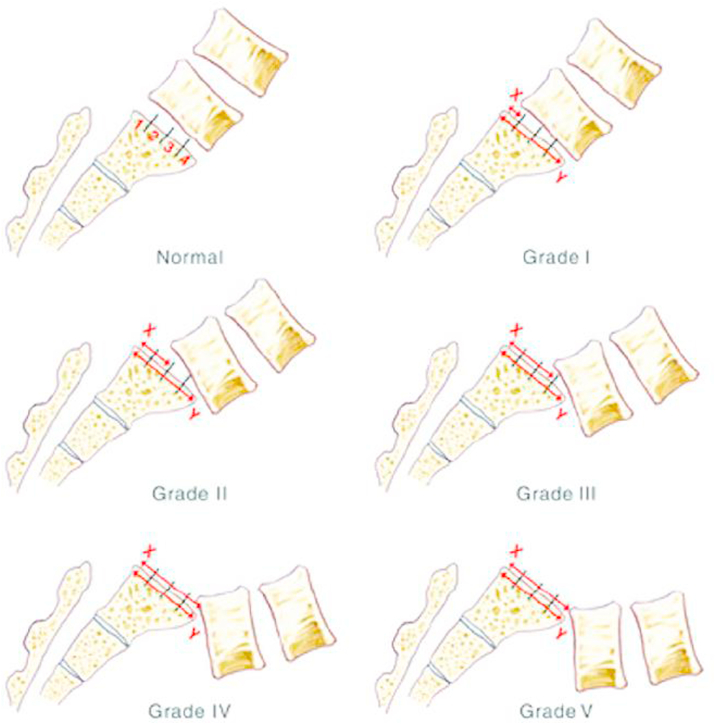
Spondylolisthesis refers to the anterior, posterior, or lateral translation of one vertebral segment compared with subjacent level. Measurement of spondylolisthesis is carried out with a grading system utilizing radiographic images. High-grade spondylolisthesis (Fig. 1) are cases with more than 50% displacement of one vertebra over the other (Meyerding displacement1 types 3 and 4 and spondylolisthesis). Wiltse2 classified spondylolisthesis based on the cause: degenerative, isthmic, traumatic, pathologic, congenital and iatrogenic.
Fig. 1.
Meyerding's classification for grading the degree of spondylolisthesis. Grade I, Grade II, Grade III, Grade IV, and normal vertebra with inferior body divided into quarters used to determine measurement of slip. Adapted from Meyerding (1932). Copyright 1932 by the American College of Surgeons. Reprinted with permission.
Most high-grade slips resulted from isthmic listhesis. It's recognized as a common cause of low back pain. In adult population, spondylolysis and isthmic spondylolisthesis prevalence is approximately 6%.3 Many environmental and activities-related factors are also thought to contribute to isthmic spondylolisthesis4: activities with hyperextension of the lower back lead to excessive stress on the pars interarticularis.5
The purpose of this study was to describe technique reduction and results for treatment of high-grade spondylolisthesis with a progressive, single-staged, posteriorly and without forced reduction, sometimes combined to trans-vertebral trans-sacral titanium strut, for restoration of lumbosacral alignment and analyzes functional and radiological outcomes.
2. Patients and methods
2.1. Patients and design
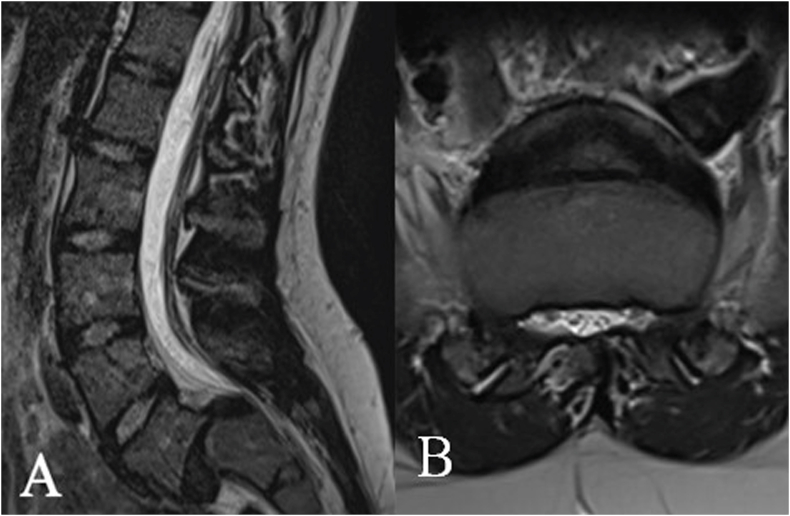
Seven consecutive adolescents and adults patients (median: 37 [17–72 years]) underwent surgery between 2016 and 2018. This retrospective study was performed in Reims University Hospital (France). Indications for surgical intervention in patients with high-grade spondylolisthesis include continued pain, progression of neurologic symptom, or progression of the slip (even if the slippage increasing during adulthood is uncommon3). All the cases had grade 3 or 4 (Fig. 2). Every patient is female.
Fig. 2.
(A) Sagittal and (B) axial MRI of lumbosacral spine in a patient with grade III spondylolisthesis.
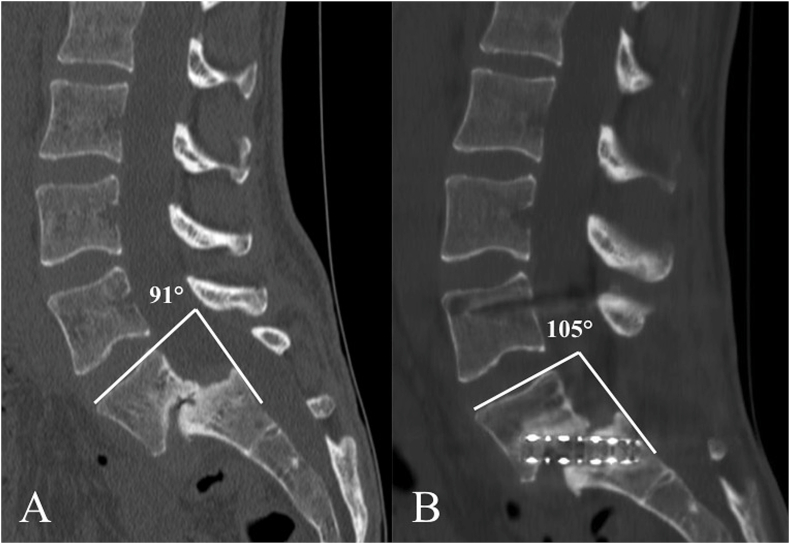
All the patients had lumbosacral spine radiographies antero-posterior, lateral views and flexion/extension views. All the patients had MRI studies. No urodynamic studies were conducted. The lumbosacral angle (LSA), according to Dubousset,6 were measured on radiographies using conventional techniques. LSA is the angle between L5 superior tray and posterior wall of S1 (Fig. 3).
Fig. 3.
(A) CT-scanner of a patient with grade 3, LSA of L5 measuring 91°. (B) The postoperative CT-scanner showing satisfactory reduction of the spondylolisthesis with the LSA corrected to 105°.
Patients with spondylolisthesis especially presented low back pain due to spasm and hamstring tightness. Widening of the iliac wings, flattened buttocks, thoracolumbar hyperlordosis leading to absent waist line and exaggerated flank creases with lumbar sag were usual clinical findings. Limitation of straight leg rising was common but none of our patients presented a motor deficit. However in pre-operatory, all patients had sensory deficits at L5 or S1. All patients were serially assessed at 2, 6 and 12 months and yearly after surgery, with clinical examination including complete neurological status and analysis of symptoms, radiography, and grading of outcome measures Oswestry Disability Index (ODI)7 and Visual Analog Scale (VAS).
All the patients had posterior decompression, sacral osteotomy and posterolateral fusion. Some patients benefited from trans-vertebral trans-sacral strut across L5-S1 disc. This procedure was done along with our regular procedure.
Parameters to indicate fusion were clinical resolution of symptoms with a radiographically solid-appearing bone bridging anterior to the cages consistency in maintenance of lumbo-sacral measurements, and no evidence of instrumentation failure, loss of reduction, or pseudarthrosis at six months and one year.
2.2. Surgical technique: beginning and positioning
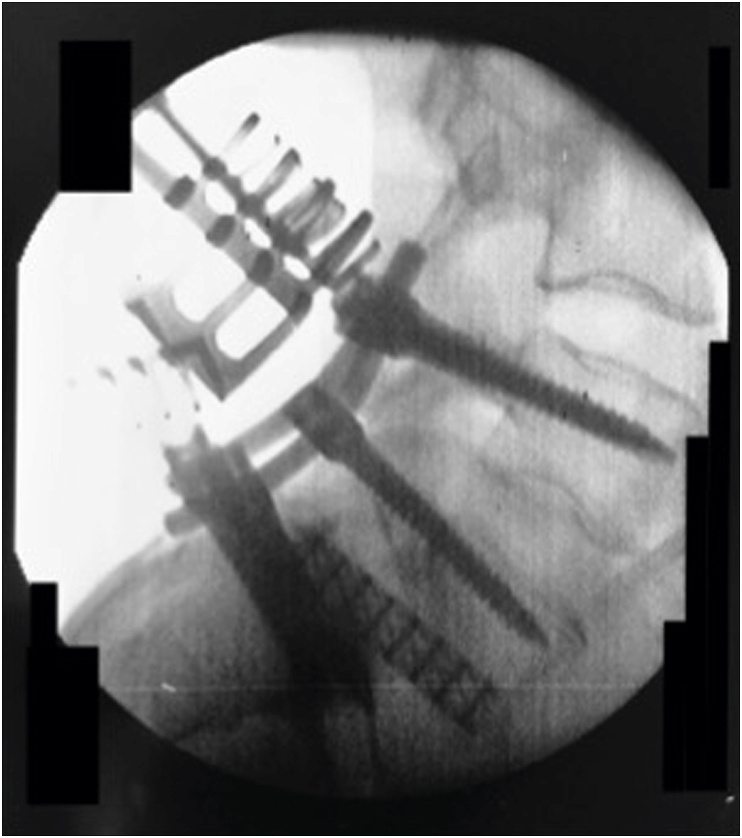
The technique is a modified version of that described by Shufflebarger et al.8 and Harms et al.9 After general anesthesia, the patient was positioned in ventral decubitus on the spine-operating table with all pressure points padded. The hips were positioned at maximum extension to help the initial positional reduction8. We used radiographs to check the amount of reduction (Fig. 4).
Fig. 4.
Intraoperative sagittal fluoroscopic image of pedicle screws for L4-L5-S1 fixation with rod construct, showing the strut titanium mesh across L5-S1 disc space and docking into the S1 body.
2.3. Surgical technique: exposure and instrumentation
A standard posterior midline lumbosacral approach was used to expose the spine depending on the grade of listhesis. Pedicle screws fixation was used in all cases with bicortical purchase of screws obtained in the sacrum. It was important to highlight the importance of using a bicortical purchase and monoaxial screws. Indeed, this was an integral part of the reduction process and helped to prevent the need for sacroiliac fixation. Sometimes we used temporary fixation of screws at L2-L3 to provide a long lever arm and a temporary prevent rod was placed to initiate the reduction. The rod was engaged and secured in the sacral screws to create a cantilever mechanism gradually fixed to the upper screw. Decompression with Gill laminectomy was performed at L5 with complete release of both L5 nerve roots.16
2.4. Surgical technique: procedure of reduction
An osteotomy of the dome-shaped sacrum was performed. A gentle reduction of L5 screw was next performed with control of the L5 nerve root: the reduction process would be done gradually. We used “persuaders” or tower reducers to reduce the screw to the rod. If we used a temporary rod on one side, this was replaced with permanent rod to bring the L5 body posterior reduction of the listhesis. Intraoperative radiographies were taken at every step of reduction, and the exchange of rods was done one at time to hold the reduction in position.
In some of our earlier cases, we performed posterolateral fusion and extended the fixation to L4. We used the Erisma™ (Clariance®, Chicago, USA) screws system at the lumbar and sacrum spine. The L5-S1 construct was compressed using a contoured rod on both sides to give the final reduction construct.
Finally in our later cases, trans-vertebral trans-sacral strut was used to maintain reduction and kyphosis correction. Laminectomy of S1 was then performed for exposure of the S1–S2 interspace. The dural sac was retracted toward the midline between the S1 nerve root and the S2 pedicle to reveal the entry site. Under fluoroscopic control, a guidewire was advanced from this entry point through S1 and across the lumbosacral disc space into the L5 vertebral body. A variable reamer was sequentially drilled over the guidewire to 1 mm less than the diameter of the titanium mesh (Pyramesh™, Medtronic®, Minneapolis, USA). The mesh was measured and cut, before driven into position across L5-S1 disc. It was beforehand filled with cancellous bone graft, or bone graft bank, or both. Only one strut was placed (Fig. 4). A total of 4 patients benefited from this procedure (57%).
This technique includes the correction of lumbosacral kyphosis with the distraction maneuver and gradual reduction of the deformity, which was followed by maintenance reduction with posterolateral and trans-vertebral trans-sacral strut.
3. Results
Seven patients with high-grade spondylolisthesis at L5-S1 were operated using this progressive reduction technique, representing 2 patients grade III (28%), 4 patients grade IV (57%) and one patient grade V (15%). All procedure was performed in a single operation using a posterior approach. The median age was 37 years old. All patients were upright on the second postoperative day.
The median follow-up was 24 months.12,25 Six months after surgery, 6 patients were pain free and able to stay home without disability. Only one patient presented persistent L5 sciatalgia. Even if, there was one patient with persistent pain, all of them maintained or improved their daily activities. All patients had good outcomes and returned to their full normal activities within 3 months after surgery. None patient developed deep or superficial infection.
Patients were advised to restrict forward bending and to avoid contact sports at least 3 months after surgery by the physiotherapists. Six patients had stiff corset after surgery (the other patient had elastic lumbosacral corset) for 6–8 weeks. The patient without caster after surgery was the older patient (72 years).
Only one patient (a young girl of 16 years old with grade IV spondylolisthesis) presented a low back pain at one year of follow-up. She had initially L4-L5-S1 arthrodesis with trans-sacral fixation strut. Radiographies and CT-scanner showed a lack of fusion and pseudarthrosis with a failure of trans-vertebral trans-sacral strut (Fig. 5). Fixation was revised after 18 months of follow-up: it was decided an extension of construct, with S2 screws and iliac screws implantation (Fig. 6). Since, her back pain decreased.
Fig. 5.
(A) Preoperative radiography of young girl patient with grade 4 spondylolisthesis. (B) CT-scanner and radiography showing satisfy reduction at 6 months of follow-up. (C) Beginning of back pain return at 12 months showing suspicion of pseudarthrosis. (D) Preoperative CT-scanner at 18 months of follow-up with pseudarthrosis and titanium mesh failure.
Fig. 6.
Postoperative radiographies after reoperation of patient with pseudarthrosis and titanium mesh failure: extension of construct, with S2 screws and iliac screws implantation.
Only one patient did not present a solid fusion at the 6 months follow-up visit. The radiographic parameter measured was the lumbosacral angle (LSA). The median preoperative degree of slip was 76°[59; 85] and reduced to 94°[76; 104], with the Meyerding grade of 2 cases stables after surgery, 3 cases with loss of two ranks and 2 cases with loss of one rank. The radiological parameters showed statistically significant difference (p = 0.002) postoperatively.
There was only one intraoperative complication with per operative bleeding and avoiding implementation of the trans-vertebral trans-sacral device. None of the patients needed an additional anterior procedure or vertebrectomy.
The mean Visual Analog Scale (VAS) showed improved pain scores, with improvement from a median of 8 cm6,8 to 1 cm [0; 3]. The modified Oswestry Disability Index (ODI) score showed significant improvement of function at latest follow-up (6 months) from median of 68%[54; 78] to 28%,25,35 even with only one case of pseudarthrosis without significant loss of reduction or real slip progression. The clinical parameters showed statistically significant difference (p < 0.05) postoperatively (Table 1).
Table 1.
Age of patients according to Meyerding grade pre/post surgery, LSA pre/post surgery, with/without corset, with/without Pyramesh™, pre/post ODI, pre/post VAS. The median of items is specified at the bottom line.
| P | A | Myd (pre) | Myd (post) | LSA (pre) | LSA (post) | Crst | Pyramesh™ | ODI (pre) | ODI (post) | VAS (pre) | VAS (post) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 47 | 3 | 2 | 76 | 77 | Y | N | 68 | 30 | 7 | 1 |
| 2 | 17 | 4 | 4 | 59 | 76 | Y | Y | 78 | 25 | 8 | 3 |
| 3 | 23 | 4 | 2 | 85 | 104 | Y | Y | 75 | 28 | 8 | 2 |
| 4 | 18 | 4 | 3 | 84 | 94 | Y | N | 54 | 35 | 7 | 1 |
| 5 | 72 | 3 | 2 | 82 | 97 | N | N | 58 | 25 | 6 | 0 |
| 6 | 37 | 4 | 2 | 70 | 102 | Y | Y | 71 | 30 | 8 | 1 |
| 7 | 37 | 3 | 3 | 71 | 87 | Y | Y | 56 | 26 | 8 | 0 |
| m | 37 | 3 | 2 | 76 | 94 | 68 | 28 | 8 | 1 |
Y: with, N: without, LSA: Lombosacral angle (°), m: median, ODI: Owestry Disability index (%), VAS: Visual Analogue Scale (cm), Crst: corset, P: Patient, Myd: Meyerding, A: Age.
4. Discussion
The goals of a reduction procedure are restoration of global spinal balance by correction of kyphosis at the lumbosacral junction. However, clinical symptoms and patient's requests are important. Patients with spondylolisthesis are likely to complain about symptoms that are mechanical, positional and mobility related in accordance with the cause. Patients with high-grade spondylolisthesis have generally collapse disc, with radicular symptoms from the resulting neuro-foraminal stenosis. The indications, and role for reduction of the spondylolisthesis, are extremely controversial, due to there currently being no widely accepted guidelines.10
Tsirikos and Garrido (2010) state treatment options depend on the age, remaining development, degree of spondylolisthesis, and severity of symptoms of the patient.10 Many surgical techniques have been suggested from simple laminectomy to complete reduction and fusion.11,12 However, lack of instrumentation result in apparition of pain and progression of the slippage, even if some studies gave a similar quality of life for surgical treatment of high-grade spondylolisthesis compared to the surgical preoperatively group.13 Moreover, new technique appeared with stabilization without reduction and trans-vertebral fusion.14 We used trans-vertebral trans-sacral L5-S1 cage in 4 patients. Interbody fusion using fibular struts placed across the L5-S1 disc space through the bodies of L5 and S1 has been described in high-grade isthmic spondylolisthesis.15,17 Lastly, posterior in-situ arthrodesis has also been described without laminectomy18 without good results in literature. Several techniques have been employed for surgical treatment including: posterior, posterolateral, and posterior interbody (PLIF).19 However, we must not forget some described cases of spondylolisthesis patients, which corrected spontaneously after surgery of concomitant scoliosis.20 Spontaneous fusion of L5 spondylolisthesis was uncommon.21
Moreover, the posterior arthrodesis was acceptable technique without additional anterior procedure. Some studies reported excellent correction of the deformity and good clinical outcome with posterior-only arthrodesis and reduction procedure.9,22 Excellent results were obtained with technique of decompression, distraction and reduction for posterior lumbar interbody fusion. In our case distraction was obtained using hook in the upper lumbar spine and reduction was done using long-headed pedicle screws. Ruf et al. even suggested L4 preservation of instrumental procedure in case of monosegmental fusion if L4/L5 segment was not primarily affected.9 Other studies described the same technique results with a wide decompression of the L5 nerve roots with laminectomy, distraction lumbar hooks, lumbosacral discectomy, anterior decortications and grafting, before placement of bilateral mesh cages packed with morselized bone autograft.8,23 Posterior compression helped to achieve kyphosis correction and to restore the load-sharing ability of the anterior column. Finally, we also sometimes used a trans-vertebral trans-sacral strut with titanium mesh, such as a modified Bohlman technique with fibular allograft.17,24
In studies, pseudarthrosis rates sometime could amount to 11% with an increased risk to 40% in case of spondylolisthesis.25 Thus the spondylolisthesis could progress in spite of successful posterior arthrodesis. As a reminder we had only one case of instrumentation failure and pseudarthrosis. Moreover, deformity progression is very common after in-situ fusion that increased this risk.18 Deformity was increased with larger initial slip angles, postsurgical immobilization, and use of Gill laminectomy technique8. Fusion without laminectomy was associated with neurological deficits (sometimes even cauda equina syndrome26), higher risk of proximal jonctionnal kyphosis (PJK) and higher risk of high-grade slips.27 Moreover, staged vertebrectomy (Gaines surgery28) with reduction and fusion, has shown significant complication rate like postoperative hematoma, retrograde ejaculation and also second look surgery for instrumentation failure or delayed union.29
Anterior or staged posterior-anterior approaches exposed to intraoperative complications like iliac vein lesion and implants complications. Authors, like Vialle et al., considered in their study that the risk-reward ratio with a transperitoneal exposure was unacceptable, with complications of late infections.30 Recently, Mehdian et al., suggested good outcome with a three staged spinal procedure combined to anterior approach with a six years of duration, but the anterior approach increased the morbidity risk.31 Traditional ALIF and PLIF techniques were not possible in high-grade slips, due to the significant transitional and angular deformities. However, the addition of an interbody fusion helped to increase fusion rates and minimize progression of the postoperative slippage.32 Finally, the reduction complications include increased rates of hardware failure when posterior instrumentation is used alone without addition of anterior interbody fusion.33
After reduction, cast immobilization (6–12 weeks) followed by posterior or/and anterior fusion has been described with satisfactory results but loss of correction is observed on long-term follow-up.23,28 In this context, it has to be explained that the majority of patients had cast immobilization before surgery in our study.23
The process of achieved technique with shortest possible fusion allowed avoiding and reducing adjacent disc and degeneration. A better union is described with compression in the state of biomechanical lordosis. Intervertebral adjacent level disc degeneration has been reported in case of conventional surgical approaches, such as postero-lateral or interbody fusion and decompressive laminectomy. Adjacent-level disc degeneration was manifested by significantly increased bending efforts, axial stiffness and facet joint load and motion. Even if, in our study, it was an inactive spinal growth population, there was a progressive deformity risk.
Nowadays, the usual procedures are open techniques, but recent report showed reduction and fusion in mono-segmental case with intraoperative 3D navigation technique and high-dysplastic spondylolisthesis.22 Computer-assisted navigation system helps surgeons to select screws size, entry point and direction and for osteotomy realization. We used in our recent case trans-vertebral trans-sacral strut with titanium mesh (Pyramesh™, Medtronic®, Minneapolis, USA), thus, we didn't need a secondary anterior approach: it was certainly less invasive for the patient but we thought that we needed a pelvic fixation. Maybe we will use PEEK material in future cases.
Although we didn't use intraoperatively neuro-monitoring, our study reports no permanent neurological deficits in contrast of the series using others procedures and describing reduction in high-grade spondylolisthesis.34 The main complication of reduction of high-grade slips was the significant associated neurologic deficit, especially L5 nerve root injuries, ranged from 25 to 30% after reduction of high-grade slips.29,35,36 Probably that the complete exposure of both nerve roots and their visualization during reduction was a contributing factor toward fewer complications.
5. Conclusion
Treatment of high-grade spondylolisthesis has trended toward focusing on correct fusion of segmental lordosis and global sagittal balance. Surgical procedure using posterior fixation can optimize outcomes by increasing the ability for reduction and surface area for bone graft leading to successful fusion. Posterolateral or interbody fusion provide effective management of high-grades spondylolisthesis. We observed a restoration of global sagittal balance and correction of the lumbosacral kyphosis. Although, requiring experimented spine surgeon, the technique is safe, with a low rate of significant complication. This procedure may seem safe and reproducible. Long-term outcomes appear to be satisfying.
Fundings
We had no fundings for this study.
Declaration of competing interest
We have not links of interest.
Contributor Information
Maxime Rivollier, Email: mrivollier@chu-reims.fr.
Benoit Marlier, Email: bmarlier@chu-reims.fr.
Jean-Charles Kleiber, Email: jckleiber@chu-reims.fr.
Christophe Eap, Email: ceap@chu-reims.fr.
Claude-Fabien Litre, Email: flitre@chu-reims.fr.
References
- 1.Meyerding H. Spondylolisthesis: surgical treatment and results. Surg Gynecol Obstet. 1932;54:371–377. [Google Scholar]
- 2.Wiltse L.L. Spondylolisthesis. West J Med. 1975;122:152–153. [PMC free article] [PubMed] [Google Scholar]
- 3.Fredrickson B., Baker D., McHolick W. The natural history of spondylolysis and spondylolisthesis. J Bone Jt Surg. 1984;66:699–707. [PubMed] [Google Scholar]
- 4.He L.-C., Wang Y.-X.J., Gong J.-S. Prevalence and risk factors of lumbar spondylolisthesis in elderly Chinese men and women. Eur Radiol. 2014;24:441–448. doi: 10.1007/s00330-013-3041-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Micheli L.J., Wood R. Back pain in young athletes: significant differences from adults in causes and patterns. Arch Pediatr Adolesc Med. 1995;149:15–18. doi: 10.1001/archpedi.1995.02170130017004. [DOI] [PubMed] [Google Scholar]
- 6.Dubousset J. Treatment of spondylolysis and spondylolisthesis in children and adolescents. Clin Orthop. 1997:77–85. doi: 10.1097/00003086-199704000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Fairbank J.C. The Oswestry disability index. Spine. 2000;25 doi: 10.1097/00007632-200011150-00017. insights.ovid.com Available at: [DOI] [PubMed] [Google Scholar]
- 8.Shufflebarger H., Geck M. High-grade isthmic dysplastic spondylolisthesis: monosegmental surgical treatment. Spine. 2005;30 doi: 10.1097/01.brs.0000155583.55856.f9. Epub ahead of print March 1. [DOI] [PubMed] [Google Scholar]
- 9.Ruf M., Koch H., Melcher R. Anatomic reduction and monosegmental fusion in high-grade developmental spondylolisthesis. Spine. 2006;31:269–274. doi: 10.1097/01.brs.0000197204.91891.eb. [DOI] [PubMed] [Google Scholar]
- 10.Tsirikos A.I., Garrido E.G. Spondylolysis and spondylolisthesis in children and adolescents. J Bone Joint Surg Br. 2010;92:751–759. doi: 10.1302/0301-620X.92B6.23014. [DOI] [PubMed] [Google Scholar]
- 11.Hoel R.J., Brenner R.M., Polly D.W. The challenge of creating lordosis in high-grade dysplastic spondylolisthesis. Neurosurg Clin. 2018;29:375–387. doi: 10.1016/j.nec.2018.03.006. [DOI] [PubMed] [Google Scholar]
- 12.Guigui P., Ferrero E. Surgical treatment of degenerative spondylolisthesis. Orthop Traumatol Surg Res. 2017;103:S11–S20. doi: 10.1016/j.otsr.2016.06.022. [DOI] [PubMed] [Google Scholar]
- 13.Bourassa-Moreau E., Labelle H., Mac-Thiong J.-M. Radiological and clinical outcome of non surgical management for pediatric high grade spondylolisthesis. Stud Health Technol Inf. 2010;158:177–181. [PubMed] [Google Scholar]
- 14.Donnally C.J., Madhavan K., Butler A.J. A novel technique for stabilization of high-grade spondylolisthesis with transvertebral fusion without reduction. J Clin Neurosci Off J Neurosurg Soc Australas. 2019;60:170–175. doi: 10.1016/j.jocn.2018.11.001. [DOI] [PubMed] [Google Scholar]
- 15.Smith J., Deviren V., Berven S. Clinical outcome of trans-sacral interbody fusion after partial reduction for high-grade L5–S1 spondylolisthesis. Spine. 2001;26:2227–2234. doi: 10.1097/00007632-200110150-00014. [DOI] [PubMed] [Google Scholar]
- 16.Bohlman H., Cook S. One-stage decompression and posterolateral and interbody fusion for lumbosacral spondyloptosis through a posterior approach. Report of two cases. J Bone Jt Surg. 1982;64:415–418. [PubMed] [Google Scholar]
- 17.Hart R.A., Domes C.M., Goodwin B. High-grade spondylolisthesis treated using a modified Bohlman technique: results among multiple surgeons: clinical article. J Neurosurg Spine. 2014;20:523–530. doi: 10.3171/2014.1.SPINE12904. [DOI] [PubMed] [Google Scholar]
- 18.Poussa M., Schlenzka D., Seitsalo S. Surgical treatment of severe isthmic spondylolisthesis in adolescents. Reduction or fusion in situ. Spine. 1993;18:894–901. doi: 10.1097/00007632-199306000-00014. [DOI] [PubMed] [Google Scholar]
- 19.Molinari R.W., Bridwell K.H., Lenke L.G. Complications in the surgical treatment of pediatric high-grade, isthmic dysplastic spondylolisthesis. A comparison of three surgical approaches. Spine. 1999;24:1701–1711. doi: 10.1097/00007632-199908150-00012. [DOI] [PubMed] [Google Scholar]
- 20.Srivastava A., Bayley E., Boszczyk B.M. The management of high-grade spondylolisthesis and co-existent late-onset idiopathic scoliosis. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc. 2016;25:3027–3031. doi: 10.1007/s00586-014-3519-0. [DOI] [PubMed] [Google Scholar]
- 21.Di Martino A., Russo F., Denaro V. Spontaneous fusion of L5 spondyloptosis: should we learn from nature? Spine J Off J North Am Spine Soc. 2012;12:529. doi: 10.1016/j.spinee.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 22.Tian W., Han X.-G., Liu B. Posterior reduction and monosegmental fusion with intraoperative three-dimensional navigation system in the treatment of high-grade developmental spondylolisthesis. Chin Med J. 2015;128:865–870. doi: 10.4103/0366-6999.154278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grzegorzewski A., Kumar S. In situ posterolateral spine arthrodesis for grades III, IV, and V spondylolisthesis in children and adolescents. J Pediatr Orthop. 2000;20:506–511. [PubMed] [Google Scholar]
- 24.Sasso R., Shively K., Reilly T. Transvertebral transsacral strut grafting for high-grade isthmic spondylolisthesis L5-S1 with fibular allograft. J Spinal Disord Tech. 2008;21:328–333. doi: 10.1097/BSD.0b013e318149e7ea. [DOI] [PubMed] [Google Scholar]
- 25.Jaeger A., Giber D., Bastard C. Risk factors of instrumentation failure and pseudarthrosis after stand-alone L5-S1 anterior lumbar interbody fusion: a retrospective cohort study. J Neurosurg Spine. 2019:1–9. doi: 10.3171/2019.3.SPINE181476. [DOI] [PubMed] [Google Scholar]
- 26.Maurice H.D., Morley T.R. Cauda equina lesions following fusion in situ and decompressive laminectomy for severe spondylolisthesis: four case reports. Spine. 1989;14:214–216. doi: 10.1097/00007632-198902000-00012. [DOI] [PubMed] [Google Scholar]
- 27.Gill G.G. Long-term follow-up evaluation of a few patients with spondylolisthesis treated by excision of the loose lamina with decompression of the nerve roots without spinal fusion. Clin Orthop. 1984:215–219. [PubMed] [Google Scholar]
- 28.Gaines R.W. L5 vertebrectomy for the surgical treatment of spondyloptosis: thirty cases in 25 years. Spine. 2005;30:S66–S70. doi: 10.1097/01.brs.0000155577.19606.df. [DOI] [PubMed] [Google Scholar]
- 29.Lehmer S.M., Steffee A.D., Gaines R.W. Treatment of L5-S1 spondyloptosis by staged L5 resection with reduction and fusion of L4 onto S1 (Gaines procedure) Spine. 1994;19:1916–1925. doi: 10.1097/00007632-199409000-00010. [DOI] [PubMed] [Google Scholar]
- 30.Vialle R., Charosky S., Padovani J.-P. Surgical treatment of high-grade lumbosacral spondylolisthesis in childhood, adolescent and young adult by the “double-plate” technique: a past experience. Eur Spine J. 2006;15:1210–1218. doi: 10.1007/s00586-005-0051-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mehdian S., Arun R. A new three-stage spinal shortening procedure for reduction of severe adolescent isthmic spondylolisthesis: a case series with medium- to long-term follow-up. Spine. 2011;36 doi: 10.1097/BRS.0b013e3182158c1f. Epub ahead of print May 1. [DOI] [PubMed] [Google Scholar]
- 32.Hanson D., Bridwell K., Rhee J. Dowel fibular strut grafts for high-grade dysplastic isthmic spondylolisthesis. Spine. 2002;27 doi: 10.1097/00007632-200209150-00005. 1982–8. [DOI] [PubMed] [Google Scholar]
- 33.Boos N., Marchesi D., Zuber K. Treatment of severe spondylolisthesis by reduction and pedicular fixation: a 4–6-year follow-up study. Spine. 1993;18:1655. doi: 10.1097/00007632-199309000-00014. [DOI] [PubMed] [Google Scholar]
- 34.Schär R.T., Sutter M., Mannion A.F. Outcome of L5 radiculopathy after reduction and instrumented transforaminal lumbar interbody fusion of high-grade L5-S1 isthmic spondylolisthesis and the role of intraoperative neurophysiological monitoring. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc. 2017;26:679–690. doi: 10.1007/s00586-017-4964-3. [DOI] [PubMed] [Google Scholar]
- 35.Bradford D., Boachie-Adjei O. Treatment of severe spondylolisthesis by anterior and posterior reduction and stabilization. A long-term follow-up study. J Bone Jt Surg. 1990;72:1060–1066. [PubMed] [Google Scholar]
- 36.Hu S., Bradford D., Transfeldt E. Reduction of high-grade spondylolisthesis using edwards instrumentation. Spine. 1996;21:367–371. doi: 10.1097/00007632-199602010-00023. [DOI] [PubMed] [Google Scholar]