Abstract
Objective
This study aimed to determine the effect of macro design in the primary stability of short and extra-short implants using resonance frequency analysis (RFA).
Material and methods
On an ex-vivo model using pig's ribs, we inserted 80 short and extra-short dental implants (20 implants per brand): Biohorizons®(B) 4.6 × 6mm; Intralock®(I) 4.75 × 6.5 mm; Straumann®(S) 4.1 × 4mm; and Tixos®(T) 5 × 5mm. Primary implant stability was measured using an RFA device. We compared mean ISQ values through ANOVA test.
Results
Mean ISQ values: B = 73.36 (±3.39); I = 75.13 (±3.88); S = 65.38 (±8.38); T = 72.13 (±11). B and I showed higher ISQ than S (p-value < 0.001). Short (I) showed higher ISQ than extra-short (B,S,T) implants (p-value = 0.001). Tapered (B,I) had higher ISQ than parallel (S,T) implants (p-value < 0.001). There was a moderate positive correlation between ISQ and length (r = 0.52), and a weak correlation with diameter (r = 0.33).
Discussion
The final result is a combination of implant design, length, and diameter. Tapered design (B and I) and larger implants (I) showed better primary stability in terms of ISQ values. This information could be beneficial at implant selection in a severely reabsorbed low-quality bone, privileging length (as long as it is safe), and conical walls design.
Keywords: Short implant, Extra short implant, Implant stability
1. Introduction
Sufficient bone volume (height and width) is necessary for predictable functional and esthetic results of dental implants. Tooth loss is always associate with bone volume resorption.1 The amount of bone loss could be up to 22% of the original volume during the first six months after extraction, being in the horizontal and vertical plane, compromising the implant placement surgery.1 Also, the vertical bone loss could expose anatomic structures (e.g., inferior alveolar nerve and vessels, maxillary sinus) to surgical damage during dental implant placement. Several bone augmentation surgical techniques have been proposed in the literature, adding monetary cost, longer treatment times, and morbidity to the patient.2
Short dental implants have proven to be a reliable and safe technique that can avoid these drawbacks with excellent survival rates comparable to standard size implants (risk difference of −0.02; 95%CI: -0.04-0.00, in favor of short implants).3 Among short implant literature, there are multiple designs proposed by different manufacturers making complicated their comparisons. Some classifications are available to classify them, particularly in terms of their length.4, 5, 6 For this article, we will use the classification proposed by Al-Johany et al.7 for diameter: extra narrow (<3 mm), narrow (≥3.0 mm to < 3.75 mm), standard (≥3.75 mm to < 5 mm) and wide (≥5.0 mm); for length: extra-short (≤6 mm), short (>6 mm to < 10 mm), standard (≥10 mm to < 13 mm), and long (≥13 mm).
There is consensus that implant stability plays a vital role in achieving osseointegration and is a prerequisite for immediate loading protocols.8 Primary stability definition is the absence of movement at the surgery time that is obtained by the friction between the implant and the bone walls.9 It depends on surgical factors (surgical technique and implant design), and patient factors (bone quality and quantity).10 Dental implant macro-design could affect primary stability, especially considering that short and extra-short implants could have less contact area during insertion in the bone. Design characteristics such as diameter, length, wall design (parallel, tapered), thread (v-shaped, square, buttress, reverse buttress, etc.), facial angle, and apex design can influence implant stability.11
Due to the variety of short implant designs, and their possible influence on primary stability, we aimed to determine the effect of macro-design in the primary stability of short and extra short implants using resonance frequency analysis (RFA).
2. Materials and methods
2.1. Sample
An experimental ex vivo study model was designed, using fresh commercially available pig ribs with three days since animal death. The rib has the advantage of having a cortical thickness homogeneity among samples, being classified as bone type 4, according to Lekholm and Zarb classification.12 An arbitrary sample size of 80 osteotomies was used, drilling up to 10 sites per rib.
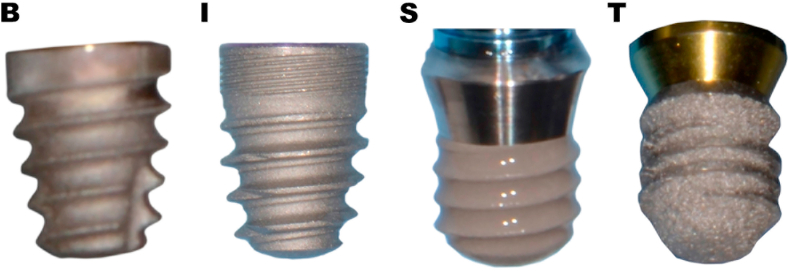
2.2. Implant description
Four different short and extra-short implants design were tested (see Fig. 1): Biohorizons® Tapered Short (B) 4.6 × 6 mm (Biohorizons®, Birmingham, Alabama, USA), Intralock® Intrahex (I) 4.75 × 6.5 mm (Intra-lock International, Boca-Raton, Florida, USA), Straumann® Tissue Level Standard Plus (S) 4.1 × 4 mm (Straumann AG, Basel, Switzerland), and Tixos® Short (T) 5 × 5mm (Leader Novaxa, Milan, Italy).
-
-
Biohorizons® (B) implants are made of Ti–6Al–4V ELI (Grade 23) alloy. Their surface is grit-blasted with a moderate roughness (0.72–1.34 μm), plus 1.8 mm of Laser-Lok® microchannels neck zone. The design is bone level, self-tapping, tapered, internal hexed connection, 15° bevel just before the implant platform, helical cutting flutes, deep aggressive reverse buttress threads, apex grove, and dome apex (Fig. 1B).
-
-
Intra-lock® (I) implants are made of Ti–6Al–4V ELI alloy. Their surface called Ossean™ is micro-blasted, presenting a nanometric scale texture within a micro-scale surface. The design is self-tapping, tapered, bone level, internal hexed connection with neck microchannels. The body configuration has Blossom® technology, which aims to continually cut through the bone with increased efficiency and minimal force across an integrated helical self-tapping configuration (Fig. 1I).
-
-
Straumann® (S) implants, in this particular case, are made of Roxolid® alloy (15% zirconia and 85% titanium). A sand-blasting and acid etching process, creates the surface roughness (0.5–3 μm), in combination with a chemical treatment that enhances hydrophilicity. This surface is called SLActive®. The design is tissue level with 1.8 mm of trans-mucosal neck, cylindrical design, with synOcta® internal connection similar to an indexed morse connection. It has 4 mm of implant body that is in touch with bone surface, with a continuous reverse buttress thread, with 0.8 mm pitch, and round apex (Fig. 1S).
-
-
Tixos® (T) implants are made of Ti–6Al–4V (Grade 5) alloy. They are produced by direct laser metal forming (3D printing technology), creating a relatively high porous surface (2–200 μm) with a compact core due to the incremental process. The design is bone level, cylindrical shape, and external hexed connection. It has a continuous reverse buttress thread, 0.9 mm pitch, and dome apex (Fig. 1T).
Fig. 1.
Four implant design used in this study.
B: Biohorizons® Tapered Short 4.6 × 6 mm; I: Intralock® Intrahex 4.75 × 6.5 mm; S: Straumann® Tissue Level Standard Plus 4.1 × 4 mm; T: Tixos® Short 5 × 5mm.
2.3. Preparation of osteotomies
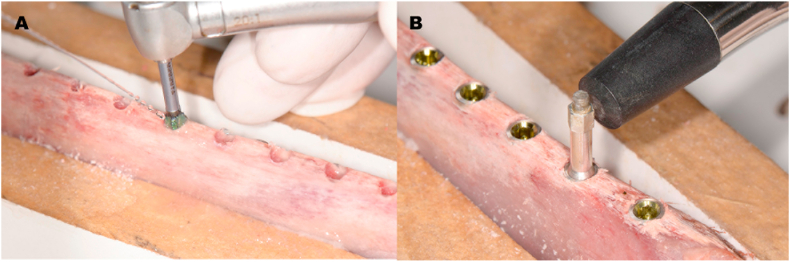
Using the manufacturer's recommended drilling procedure, a single experienced surgeon (RS) did all the osteotomies completing 20 per implant design (10 per rib) (Fig. 2).
Fig. 2.
Implant drilling procedure and ISQ measurement.
A: Biohorizons implant drilling process over pig's rib. B: ISQ measurement using Osstell ® ISQ.
2.4. Resonance frequency analysis (RFA)
RFA is a well-documented non-invasive implant stability measurement technique. It works through the continuous excitement of the implant using dynamic vibration analysis, showing ISQ values as stability measure.9 Measurements were done with a single RFA device (Osstell ISQ®, Integration Diagnostic, Gothenburg, Sweden). ISQ values came from four different directions per implant, simulating facial, palatal, mesial, and distal, using the average as a single value per implant (Fig. 2B).
2.5. Statistical analysis
Stata 14.2 (StataCorp LP. 2015, TX: StataCortp LP) software was used for the statistical analysis. For data description, we used central tendency and dispersion values. For normal distribution assessment, we performed the Shapiro-Wilk test. Differences between groups were evaluated through ANOVA and Sheffé post-hoc test. The significance level was set as p-value = 0.05. We also compared ISQ values of short (I) and extra-short implants (B, S, and T) using an unpaired t-test. Similarly, we compared tapered (B and I) and cylindrical (S and T) design using the same statistical test. Finally, we searched for possibles correlations between ISQ values, diameter, and length, using Pearson's correlation coefficient. Graphics were created with GraphPad Prism 8.2.1 software (San Diego, CA, USA).
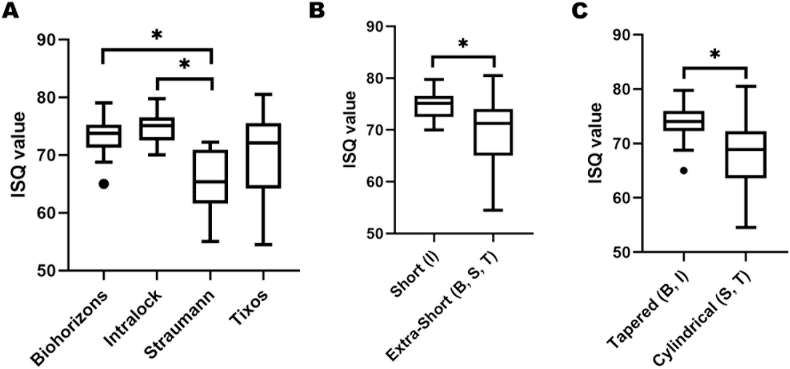
3. Results
ISQ values ranged between 54.5 and 80.5 N, with an average of 70.9 (±5.99) for all samples. The distribution was normal in each study group. Results by groups are present in Table 1 in terms of mean, standard deviation, minimum, and maximum values. ANOVA test showed differences between groups (p-value < 0.001) with homoscedasticity among groups. Post-hoc test showed statistical differences between B and S groups (p-value < 0.001) and between I and S groups (p-value < 0.001). This situation is present in the box plot shown in Fig. 3A.
Table 1.
Implant's primary stability description.
| Implant Design | Size (mm) | Mean (ISQ) | SD | Min | Max | N |
|---|---|---|---|---|---|---|
| Biohorizons (B) | 4.6 × 6 | 73.36 | 3.39 | 65 | 79 | 20 |
| Intralock (I) | 4.75 × 6.5 | 75.13 | 3.88 | 70 | 79.75 | 20 |
| Straumann (S) | 4.1 × 4 | 65.38 | 8.38 | 55 | 72.25 | 20 |
| Tixos (T) | 5 × 5 | 72.13 | 11 | 54.5 | 80.5 | 20 |
| Total | 70.92 | 5.997 | 54.5 | 80.5 | 80 |
SD: standard deviation.
Fig. 3.
Blox plots showing ISQ values per group.
A: Comparison between 4 implants (*p-value < 0.001). B: Comparison between short and extra-short implants (*p-value = 0.001). C: Comparison between tapered and cylindrical design (*p-value < 0.001).
When implants were grouped according to implant length, short implants (I) had an average ISQ of 74.51 (±2.42), while extra-short implants (B, S, and T) had 69.68 (±6.35). Short implants showed higher ISQ values compared to extra-short ones (p-value = 0.001) (Fig. 3B). When implants were grouped according to wall parallelism, tapered group (B and I) has an average ISQ of 73.95 (±2.95), while cylindric ones (S and T) had 67.94 (±6.71), also showing statistical difference (p-value < 0.001) (Fig. 3C).
A moderate positive correlation was found between ISQ values and implant length (Pearson r = 0.52). A weak positive correlation was observed between ISQ and implant diameter (r = 0.33).
4. Discussion
Resonance frequency analysis is a commonly used method to assess dental implant stability. If there is a direct relationship between ISQ values and insertion torque or bone-implant contact (BIC), it is still controversial. However, implant design characteristics clearly influence ISQ values.13 Since short implants have less length to anchor to the bone and achieve primary stability, implant diameter and design characteristics could gain importance for the selection of the indicated implant at the surgery. There is a wide range of ISQ values reported in the literature, recommending values above 65 for immediate loading.14 Most of the ISQ values obtained in our study were above this threshold, with an average ISQ of 70.9 (±5.99).
Short implant ISQ values are available in the dental literature. Rossi et al.15 used 40 Straumann® tissue level, cylindrical, extra-short implants (4.1 and 4.8 mm diameter x 6 mm length) on a 35 patients cohort finding an average ISQ of 70.2 (±9) at the surgical time in mostly bone type 1 (20%) and 2 (60%) (Leckholm & Zarb). Alonso et al.,16 using the same Straumann® implants (4.1 mm diameter), found an average ISQ of 63.68 (±8.79) for implants inserted on type 4 bone at surgery (12 cases). These findings were very close to our results (see Table 1). Zuffetti et al.17 using Biohorizons® tapered bone level implants (4.1 mm diameter x 6 or 7.5 mm length) on 254 clinical inserted implants, found an average ISQ of 58.7 (±8.01), making no specific description of the bone type or surgery zone. Since it was a multicenter retrospective clinical study, the standardization of surgical protocols and ISQ measurement may be difficult. This situation could have a detrimental effect on ISQ values since our results show higher average ISQ values for Biohorizons® short implants.
Until this review, ISQ data from Intralock® or Tixos® short implants could not be found. Nevertheless, there is data from other short implants. Benlidayi et al.18 used short and extra-short NucleOss® (Izmir, Turkey) implants, with a tapered design, aggressive reverse buttress thread, and internal connection. They used 86 implants on 37 patients (4.8, 5.5 and 6.2 mm diameter x 5, 6, and 7 mm length) with an average ISQ value of 71.2 (±9.2).
All data mentioned above shows that short and extra-short implants mostly have ISQ values compatible with immediate loading, at insertion surgery, showing agreement with our results.
Focusing deeper on the possible influence of implant macro-desing on ISQ values, we found that there was a positive correlation with ISQ (r = 0.52), where the highest ISQ was for the longest implant (I) and the smallest, for the shortest one (S) (see Table 1). This situation was also evident when we grouped short (I) and extra-short (B, S, and T) implants, with a significant statistical difference (see Fig. 3B). Some preclinical literature shows that increasing implant length improves primary stability, mainly were low-quality bone tissue is present.19,20 Clinical studies could not find a correlation between ISQ values and length. This situation could be due to the less controlled environment of the clinical scenario since cortical bone thickness, bone quality, and surgical technique could easily vary from case to case.21
If we focus on implant diameter, we found a weak positive correlation with ISQ values (r = 0.33). Some data supports that diameter might have a positive influence on ISQ values.22 Theoretically, an increased diameter leads to a higher BIC since the contact surface increases, but ISQ values do not always show this situation.20,23
Parallel (cylindrical) or conical (tapered) implant's wall configuration showed to influence ISQ values in our sample. This result matches with others in vitro studies in the literature since tapered implants could generate higher compressive strength in the surrounding bone tissue, achieving higher rigidity in the bone-implant interface.20,24
Bone characteristics are in close relation to ISQ values. Implants inserted into “corticalized” bone (type 1 or 2) have higher ISQ values than implants inserted thin cortical bone (type 3 or 4).25,26 We tried to limit this influence by using only one kind of bone sample (pig ribs) that resembles bone type 4. Other factors that could increase ISQ values are the under-preparation of implant bed or the use of osseodensification techniques.27,28 We did not apply these techniques during our study; instead, we used the manufacturer's recommended protocol for each implant, as a way for studying only implant's characteristics influence over ISQ values.
Surface roughness has a role in implant stability, especially for achieving faster secondary stability.29 Regarding primary implant stability, there is data that shows that implant with a treated surface (improved roughness) shows higher insertion torque values than the machined implants.30 Nevertheless, RFA systems could not always quantify this effect, especially if all the implants have rough surfaces.31,32 For these reasons, we focused the discussion mainly on the macro-design instead of the micro-design of the short implants.
Finally, thread number, geometry, and configuration have an essential role in dental implant stability, since it can influence implant insertion through bone (e.g., self-tapping implants), and stress distribution.33 It is hard to analyze the particular influence of each factor, such as thread form (v, square, buttress, or reverse buttress shaped), depth, number, angle, lead, and pitch. Implant companies limit the information that gives to professionals since their products are protected by intellectual property. All the tested implants had reverse buttress thread, but the manufacturer did not give the specific pattern. Intralock® design named Blossom® had the more complex macroscopic configuration of the tested implants (see Fig. 1B), and it matches with the higher ISQ values under our experiment (Table 1).
Our four tested implants differed simultaneously on implant design, length, and diameter, making it difficult to understand the specific reason for the different ISQ values behavior. The final result is a combination of all those factors, indicating in our case, that tapered design (B and I) and larger length implants (I), shows better primary stability in terms of ISQ values. This information could be beneficial when the clinician needs to choose an implant for a severely reabsorbed low-quality bone, privileging length (as long as it is safe), and conical design.
5. Conclusion
Tapered wall configuration and larger size implants (6 and 6.5 mm) showed higher ISQ values than cylindric and shorter configurations on this ex vivo experiment using short and extra-short implants.
Ethics
The scientific board of the Faculty of Dentistry (Universidad de los Andes) approved the study protocol since no animal was harmed or euthanized during the study development.
Declaration of competing interest
There is no conflict of interest in this publication. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Contributor Information
Ramón Silva, Email: ramonsilva.barrios@gmail.com.
Pablo Villalón, Email: pablovillalone@gmail.com.
Felipe Cáceres, Email: fcaceres@uandes.cl, felipec.merino@gmail.com.
References
- 1.Tan W.L., Wong T.L.T., Wong M.C.M., Lang N.P. A systematic review of post-extractional alveolar hard and soft tissue dimensional changes in humans. Clin Oral Implants Res. 2012;23(s5):1–21. doi: 10.1111/j.1600-0501.2011.02375.x. [DOI] [PubMed] [Google Scholar]
- 2.Chiapasco M., Casentini P., Zaniboni M. Bone augmentation procedures in implant dentistry. Int J Oral Maxillofac Implants. 2009;24:237–259. [PubMed] [Google Scholar]
- 3.Uehara P.N., Matsubara V.H., Igai F., Sesma N., Mukai M.K., Araujo M.G. Short dental implants (≤7mm) versus longer implants in augmented bone area: a meta-analysis of randomized controlled trials. Open Dent J. 2018;12:354–365. doi: 10.2174/1874210601812010354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Renouard F., Nisand D. Impact of implant length and diameter on survival rates. Clin Oral Implants Res. 2006;17(S2):35–51. doi: 10.1111/j.1600-0501.2006.01349.x. [DOI] [PubMed] [Google Scholar]
- 5.Deporter D., Ogiso B., Sohn D.S., Ruljancich K., Pharoah M. Ultrashort sintered porous-surfaced dental implants used to replace posterior teeth. J Periodontol. 2008;79:1280–1286. doi: 10.1902/jop.2008.070496. [DOI] [PubMed] [Google Scholar]
- 6.Urdaneta R., Daher S., Leary J., Emanuel K M., Chuang S.-K. The survival of ultrashort locking-taper implants. Int J Oral Maxillofac Implants. 2012;27:644–654. [PubMed] [Google Scholar]
- 7.Al-Johany S.S., Al Amri M.D., Alsaeed S., Alalola B. Dental implant length and diameter: a proposed classification scheme. J Prosthodont. 2017;26(3):252–260. doi: 10.1111/jopr.12517. [DOI] [PubMed] [Google Scholar]
- 8.Al-Sabbagh M., Eldomiaty W., Khabbaz Y. Can osseointegration Be achieved without primary stability? Dent Clin. 2019;63(3):461–473. doi: 10.1016/j.cden.2019.02.001. [DOI] [PubMed] [Google Scholar]
- 9.Meredith N. Assessment of implant stability as a prognostic determinant. Int J Prosthodont. 1998;11(5):491–501. [PubMed] [Google Scholar]
- 10.Javed F., Ahmed H.B., Crespi R., Romanos G.E. Role of primary stability for successful osseointegration of dental implants: factors of influence and evaluation. Interv Med Appl Sci. 2013;5(4):162–167. doi: 10.1556/IMAS.5.2013.4.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Menicucci G., Pachiè E., Lorenzetti M., Migliaretti G., Carossa S. Comparison of primary stability of straight-walled and tapered implants using an insertion torque device. Int J Prosthodont. 2012;25(5):465–471. [PubMed] [Google Scholar]
- 12.Rastelli C., Falisi G., Gatto R. Implant stability in different techniques of surgical sites preparation: an in vitro study. Oral Implantol. 2014;7(2):33–39. [PMC free article] [PubMed] [Google Scholar]
- 13.Lages F.S., Oliveira D.W.D., Costa F.O. Relationship between implant stability measurements obtained by insertion torque and resonance frequency analysis: a systematic review. Clin Implant Dent Relat Res. 2018;20(1):26–33. doi: 10.1111/cid.12565. [DOI] [PubMed] [Google Scholar]
- 14.Bornstein MM, Hart CN, Halbritter SA, Morton D, Buser D. Early loading of nonsubmerged titanium implants with a chemically modified sand-blasted and acid-etched surface: 6-month results of a prospective case series study in the posterior mandible focusing on peri-implant crestal bone changes and implant stability quotient (ISQ) values. Clin Implant Dent Relat Res. 11(4):338-347. doi:10.1111/j.1708-8208.2009.00148.x. [DOI] [PubMed]
- 15.Rossi F, Lang NP, Ricci E, Ferraioli L, Marchetti C, Botticelli D. Early loading of 6-mm-short implants with a moderately rough surface supporting single crowns – a prospective 5-year cohort study. Clin Oral Implants Res. 26(4):471-477. doi:10.1111/clr.12409. [DOI] [PubMed]
- 16.Alonso F.R., Triches D.F., Mezzomo L.A.M., Teixeira E.R., Shinkai R.S.A. Primary and secondary stability of single short implants. J Craniofac Surg. 2018;29(6):e548–e551. doi: 10.1097/SCS.0000000000004567. [DOI] [PubMed] [Google Scholar]
- 17.Zuffetti F., Testarelli L., Bertani P., Vassilopoulos S., Testori T., Guarnieri R. A retrospective multicenter study on short implants with a laser-microgrooved collar (≤7.5 mm) in posterior edentulous areas: radiographic and clinical results up to 3 to 5 years. J Oral Maxillofac Surg. 2020;78(2):217–227. doi: 10.1016/j.joms.2019.08.007. [DOI] [PubMed] [Google Scholar]
- 18.Benlidayi M.E., Ucar Y., Tatli U. Short implants versus standard implants: midterm outcomes of a clinical study. Implant Dent. 2018;27(1):95. doi: 10.1097/ID.0000000000000710. [DOI] [PubMed] [Google Scholar]
- 19.Bataineh A.B., Al-Dakes A.M. The influence of length of implant on primary stability: an in vitro study using resonance frequency analysis. J Clin Exp Dent. 2017;9(1):e1–e6. doi: 10.4317/jced.53302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barikani H., Rashtak S., Akbari S., Fard M.K., Rokn A. The effect of shape, length and diameter of implants on primary stability based on resonance frequency analysis. Dent Res J. 2014;11(1):87. [PMC free article] [PubMed] [Google Scholar]
- 21.Degidi M, Daprile G, Piattelli A. Primary stability determination by means of insertion torque and RFA in a sample of 4,135 implants. Clin Implant Dent Relat Res. 14(4):501-507. doi:10.1111/j.1708-8208.2010.00302.x. [DOI] [PubMed]
- 22.Kessler-Liechti G., Zix J., Mericske-Stern R. Stability measurements of 1-stage implants in the edentulous mandible by means of resonance frequency analysis. Int J Oral Maxillofac Implants. 2008;23(2) [PubMed] [Google Scholar]
- 23.Farronato D., Manfredini M., Stocchero M., Caccia M., Azzi L., Farronato M. Influence of bone quality, drilling protocol, implant diameter/length on primary stability: an in vitro comparative study on insertion torque and resonance frequency analysis. J Oral Implantol. 2020;46(3):182–189. doi: 10.1563/aaid-joi-D-19-00145. [DOI] [PubMed] [Google Scholar]
- 24.Romanos G.E., Basha-Hijazi A., Gupta B., Ren Y.-F., Malmstrom H. Role of clinician's experience and implant design on implant stability. An ex vivo study in artificial soft bones. Clin Implant Dent Relat Res. 2014;16(2):166–171. doi: 10.1111/j.1708-8208.2012.00470.x. [DOI] [PubMed] [Google Scholar]
- 25.Fu M.-W., Fu E., Lin F.-G., Chang W.-J., Hsieh Y.-D., Shen E.-C. Correlation between resonance frequency analysis and bone quality assessments at dental implant recipient sites. Int J Oral Maxillofac Implants. 2017;32(1):180–187. doi: 10.11607/jomi.4684. [DOI] [PubMed] [Google Scholar]
- 26.Chávarri-Prado D., Brizuela-Velasco A., Diéguez-Pereira M. Influence of cortical bone and implant design in the primary stability of dental implants measured by two different devices of resonance frequency analysis: an in vitro study. J Clin Exp Dent. 2020;12(3):e242–e248. doi: 10.4317/jced.56014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Herrero-Climent M., Lemos B.F., Herrero-Climent F. Influence of implant design and under-preparation of the implant site on implant primary stability. An in vitro study. Int J Environ Res Publ Health. 2020;17(12):4436. doi: 10.3390/ijerph17124436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Huwais S. 2019. Enhancing Implant Stability with Osseodensification— a Case Report with 2-year Follow-Up Implant Practice US. Implant Practice US. Published February 16, 2015.https://www.implantpracticeus.com/case-studies/enhancing-implant-stability-osseodensification-case-report-2-year-follow/ [Google Scholar]
- 29.Elias C.N., Oshida Y., Lima J.H.C., Muller C.A. Relationship between surface properties (roughness, wettability and morphology) of titanium and dental implant removal torque. J Mech Behav Biomed Mater. 2008;1(3):234–242. doi: 10.1016/j.jmbbm.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 30.Dos Santos M.V., Elias C.N., Cavalcanti Lima J.H. The effects of superficial roughness and design on the primary stability of dental implants. Clin Implant Dent Relat Res. 2011;13(3):215–223. doi: 10.1111/j.1708-8208.2009.00202.x. [DOI] [PubMed] [Google Scholar]
- 31.Souza F.Á., Furtado T.S.M., Dayube U.R.C. Comparative in vivo study of alloy titanium implants with two different surfaces: biomechanical and SEM analysis. Clin Oral Invest. 2019;23(12):4383–4397. doi: 10.1007/s00784-019-02872-6. [DOI] [PubMed] [Google Scholar]
- 32.Javed F., Almas K., Crespi R., Romanos G.E. Implant surface morphology and primary stability: is there a connection? Implant Dent. 2011;20(1):40–46. doi: 10.1097/ID.0b013e31820867da. [DOI] [PubMed] [Google Scholar]
- 33.Steigenga J.T., Al-Shammari K.F., Nociti F.H., Misch C.E., Wang H.-L. Dental implant design and its relationship to long-term implant success. Implant Dent. 2003;12(4):306. doi: 10.1097/01.ID.0000091140.76130.A1. [DOI] [PubMed] [Google Scholar]