Highlights
-
•
Postcard reminders increased vaccination rates during preventive care visits.
-
•
Postcards may prime parents for provider recommendations.
-
•
Reminders may be most effective if combined with provider-targeted interventions.
Abbreviations: HPV, Human papillomavirus; CHIP, Children's Health Insurance Program; LV, Learner Verification
Keywords: Preventative care, Provider recommendation, Reminder, Vaccine, Human papillomavirus
Abstract
Parent-targeted reminders increase human papillomavirus (HPV) vaccination rates. Our postcard reminders increased HPV vaccine initiation (receipt of at least one dose) by 60% among girls, but not substantially among boys. To select a complementary intervention that would maximize the effect of reminders, we assessed the percentage increase in HPV vaccine initiation from reminders increasing preventive care visits or increasing the likelihood of vaccine receipt during preventive care.
We conducted a secondary analysis of the postcard reminders from a quasi-experimental, factorial designed, feasibility trial conducted in 2013–2014 among 2,470 11- to 17-year-old girls enrolled in Florida’s Medicaid or Children’s Health Insurance Programs. We used log-linear models and a 4-way decomposition method to estimate the mediating and interacting effects of preventive visits on the effect of postcards on HPV vaccination.
After receiving a preventive visit, 76% (269/356) of girls remained unvaccinated. Nearly half of the effect of postcards on HPV vaccination was mediated by preventive visits (44%; 95% CI = 9.2% to 78.0%). Postcards increased HPV vaccine initiation mainly by increasing the likelihood of HPV vaccine receipt during preventive visits (pure indirect effect = 32.3%; 95% CI = 1.5% to 63.1%), and also by increasing the occurrence of preventive visits (mediated interaction = 11.3%; 95% CI = 1.5 to 21.1).
Reminders likely increased vaccination rates during well visits by priming parents for HPV vaccine conversations with their child’s health care provider. Thus, reminder effectiveness may be increased if timed closely to preventive care visits and/or combined with interventions that improve provider recommendations.
Trial Registration: ClinicalTrials.gov, NCT04208269, Registered 23, December 2019 – Retrospectively registered, https://clinicaltrials.gov/ct2/show/NCT04208269.
1. Background
Each year in the United States (US), the human papillomavirus (HPV) vaccine could prevent approximately 32,100 cancer cases (Senkomago et al., 2019). Yet, in 2018, HPV vaccine coverage remained low (Walker et al., 2019). In 2018, HPV vaccine initiation rates (at least one of the two to three dose series) among 13- to 17-year-olds in Florida were below the national average (64% Florida versus 68% US) (Walker et al., 2019). Between 2012 and 2016, among all states, Florida had the second highest annual number of HPV-related cancers targeted by the vaccine (2,690) (Senkomago et al., 2019).
One evidence-based strategy to increase vaccination, endorsed by the Centers for Disease Control and Prevention's Community Guide, is sending reminder messages to alert parents of vaccines recommended for their children (Community Preventive Services Task Force, 2015). Reminder studies targeting immunization, including HPV vaccine initiation, primarily show moderate increases (summarized effect estimates of 8%) (Francis et al., 2017, Jacobson Vann et al., 2018). If reminders are combined with complementary interventions, it is possible to boost effects (Staras et al., 2015, McLean et al., 2017).
The most effective complementary interventions for reminders likely differ based on how reminders influence HPV vaccination. It is unclear, however, whether reminders increase vaccination rates by (1) increasing the percentage of teens receiving well visits or (2) increasing vaccine acceptance among teens who were already planning to have preventive care visits. For example, two studies provide conflicting evidence regarding the intermediate outcomes of vaccine reminders. (Szilagyi et al., 2011, O'Leary et al., 2015) In one study, vaccine reminders increased vaccination rates and lowered missed opportunities (i.e., clinic visits where vaccines are due, but not received), but did not change the percentage of teens receiving preventive care visits. (O'Leary et al., 2015) In another study, vaccine reminders accompanied by home visits, if necessary, increased immunization rates and preventive care visits. (Szilagyi et al., 2011) Neither of these studies conducted a formal analysis to compare the mediation of preventive visits on the effect of vaccination reminders.
To develop more effective complementary interventions to reminders, we aimed to increase understanding of how reminders interact with preventive care visits to increase HPV vaccination. Building on our published trial main effects where postcard reminders increased HPV vaccine initiation, (Staras et al., 2015) we decomposed the significant effect of postcards on HPV vaccination among girls into four components: (a) the effect of the postcards on HPV vaccination outside of preventive visits; (b) the effect of preventive visits on vaccination without postcards; (c) the effect of postcards increasing preventive visits; and (d) the effect of postcards increasing vaccination rates during preventive visits. The decomposition can aid selection of complementary interventions to boost reminder effectiveness. For example, if reminders act primarily by increasing preventive care visits, complementary interventions could focus on simplifying scheduling procedures. Alternatively, if reminders mainly increase parent receptivity to vaccination during visits, complementary interventions could focus on increasing the likelihood of provider HPV vaccine recommendations.
2. MATERIALS and METHODS
2.1. Study population
This study focuses on girls from our 2013 to 2014 multi-level, quasi-experimental trial of a centralized postcard campaign and an in-clinic application alerting providers of the parents’ intent to receive the HPV vaccine (Staras et al., 2015). The study focuses only on girls because postcards increased vaccination among girls, but not significantly among boys (Staras et al., 2015). Girls enrolled in the trial: (a) were 11 to 17 years old, (b) were enrolled in Florida Medicaid or Children's Health Insurance Program (CHIP) during June 2013, (c) had a residential zip code in the Medicaid and CHIP enrollment file from North Central Florida (The Dartmouth Atlas of Health Care, 2014); and (d) had a regular office visit claim between July 1, 2011 and August 1, 2013 (Centers for Medicare & Medicaid Services, 2013). Girls with HPV vaccine claims prior to August 1, 2013 (sample draw) were excluded. Florida’s program eligibility is based on the Federal Poverty level: Medicaid ≤ 133% and CHIP ≤ 210% (Centers for Medicare & Medicaid Services, 2016). Permission for this use of the claims and enrollment data was granted by the Florida Agency of Health Care Administration. The institutional review board at the University of Florida approved the project.
2.2. Study design
In the trial, parent-targeted postcards were individually randomly assigned within two strata based on history of attendance at a clinic participating in the application intervention (yes/no) and address (Gainesville or surrounding area) (Staras et al., 2015). We expect little influence of the stratification on the effect of postcards because: (a) the factorial design allows for assessing the postcard effects separately, (b) baseline HPV vaccine initiation rates were similar between stratum, and (c) the in-clinic app was only used by 8% of the adolescents who had an office visit during the study (Staras et al., 2015).
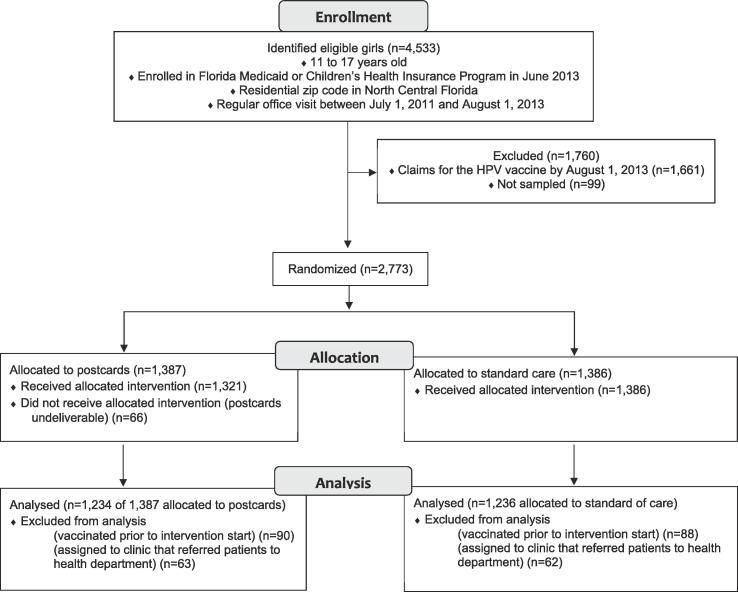
The trial analysis dataset included 2,470 girls (Fig. 1). Among the 2,773 girls randomized, the analysis dataset excluded the 178 girls who had HPV vaccine claims prior to the study start (reported or administered before the study start) and the 125 girls assigned to a specific participating clinic that later reported referring all Medicaid and CHIP enrollees to the health department for vaccines.
Fig. 1.
CONSORT Diagram of Study Design.
2.3. Postcard intervention
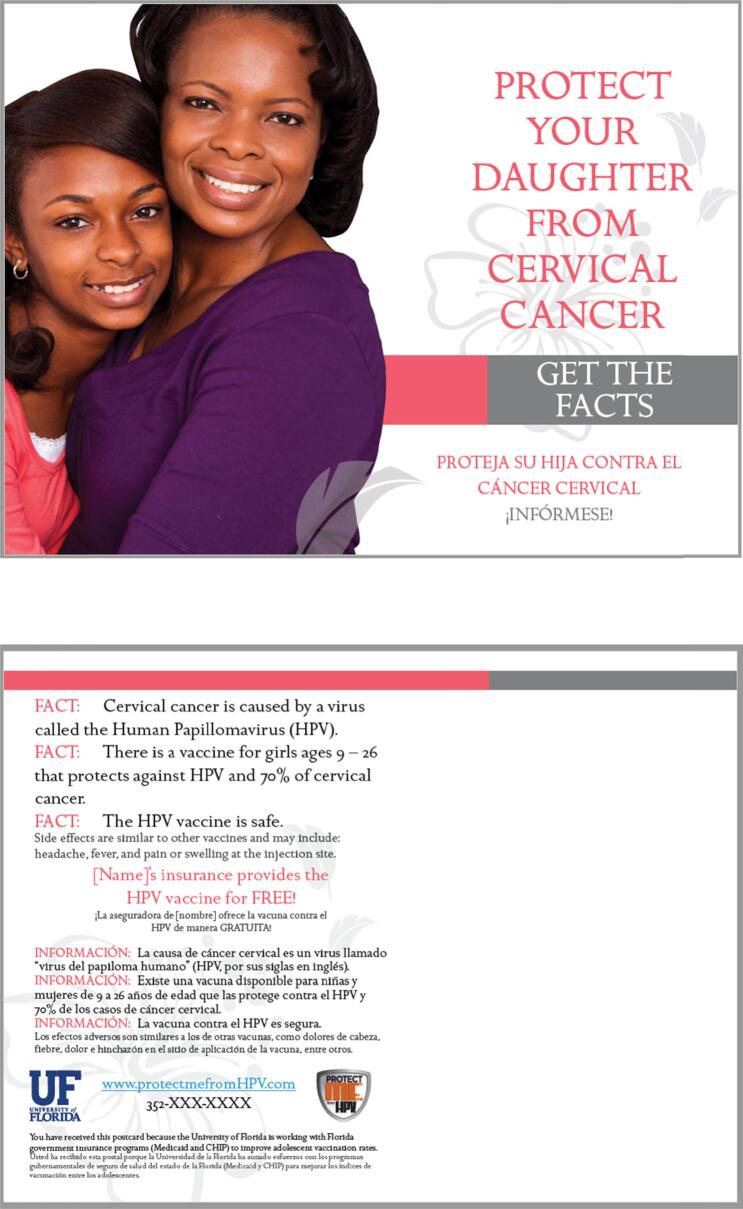
Guided by the Health Belief Model (Janz and Becker, 1984); we developed postcard reminders because 86% of parents of Florida Medicaid and CHIP enrollees reported preferring to receive health information about their child by mail (Staras et al., 2014). Postcards were developed by health behavior professionals in collaboration with a professional design company, and refined with parent focus groups using Learner Verification (LV) as an evaluation framework. (Doak et al., 1996)
When analyzing the focus groups, LV components were operationalized as follows: (1) attraction — the postcard is enticing to look at and images are consistent with subject tone and mood; (2) comprehension — recipients understand and could use the information; (3) persuasion — the postcard motivated specific action (in this case, discussing the HPV vaccine with the adolescent’s provider) by increasing benefits and decreasing barriers in the mind of the recipient; and (4) cultural acceptability — whether recipients feel excluded from or unintentionally offended by the message.
Parents were attracted to postcards when the front reflected the seriousness of the topic using words like protect, cancer, HPV, and included images of an adolescent with their parent with serious looks on their faces. These collective words and images would motivate them to read the rest of the information, especially if their child’s name appeared on the back of the postcard. Parents were able to comprehend the messages measured by their ability to accurately rephrase the information in their own words. Parents perceived the final postcards as persuasive enough to potentially encourage a conversation with their adolescent’s health care provider about vaccination. To improve cultural acceptability, parents reiterated the importance of including images of individuals that reflect the socioeconomic status, race/ethnicity and family composition of their communities. An additional category that we called information sufficiency was uncovered during analysis. Parents wanted more information about HPV infection and vaccination added to the postcard and suggested adding a toll-free number or link to a website. Despite adding this information, parents still wanted more information.
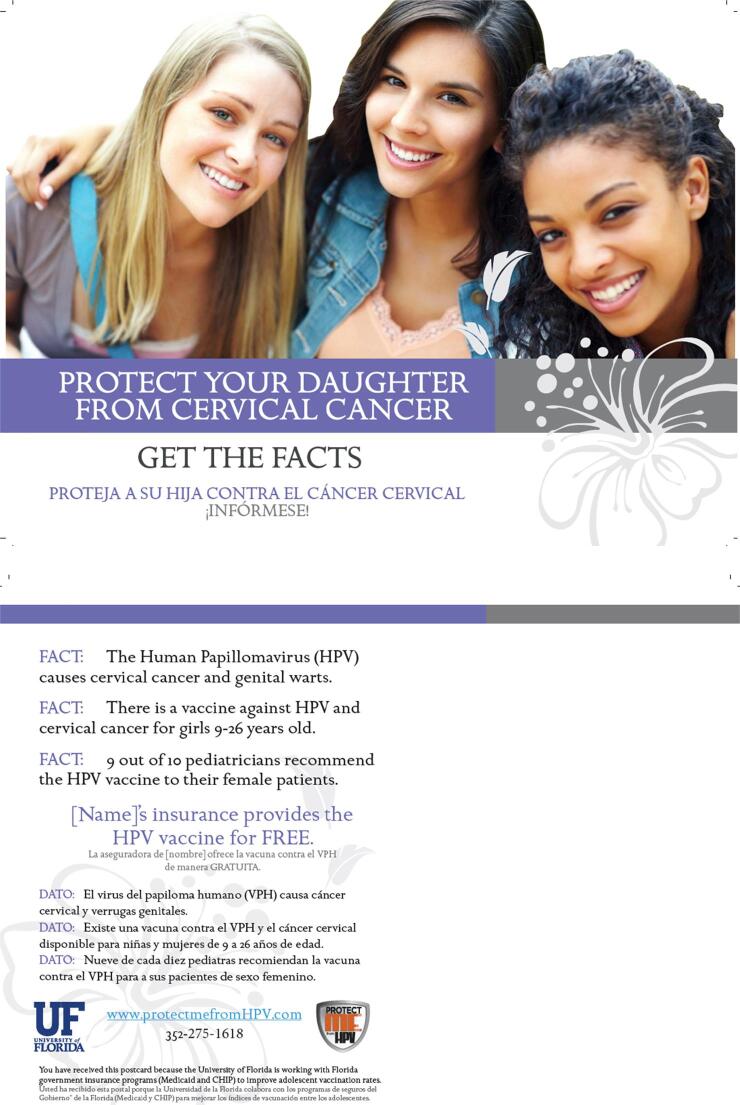
A series of two large, six-by-eight inch, full-color postcards were mailed to the parent or guardian of the 1,387 girls (Fig. 2, Fig. 3). Postcard text was in English and Spanish, used the child’s first name, and did not explicitly mention preventive visits. We obtained addresses from Florida Medicaid and CHIP enrollment files and updated addresses with the National Change of Address Database. Postcards were sent via first class mail with return service requested: one on August 19, 2013 and another on October 3, 2013. Postcards were sent to new addresses obtained from returned postcards (n = 2): undeliverable rates were 4.7% (n = 66) for both postcards and 2.5% (n = 35) for the second postcard.
Fig. 2.
First postcard mailed to parents of girls.
Fig. 3.
Second postcard mailed to parents of girls.
2.4. Outcomes
We examined how preventive visits mediated and interacted with the effect of postcards on HPV vaccine initiation. We defined preventive visits as any current procedural codes for Healthcare Effectiveness Data and Information Set well care and acute visits as any ambulatory procedural codes not including the well care set (including nurse only visits) (Centers for Medicare & Medicaid Services, 2013). While preventive care visits are only recommended once per year, the two randomized groups should have approximately similar percentages of girls due for preventive visits during the three-month study period. We measured HPV vaccine initiation as having at least one HPV vaccine claim during the study period (August 14, 2013 to November 15, 2013) reported in the claims by April 1, 2014.
2.5. Statistical analysis
We used log-linear models to assess the as assigned effect of postcards on: (a) receipt of a preventive care visits, (b) initiation of the HPV vaccine series during a preventive visit, and (c) initiation of the HPV vaccine series during an acute visit. In multivariable analyses, we adjusted for factors that may influence HPV vaccination and preventive visits: race/ethnicity, age in years as of August 14, 2013, and health program enrollment (Medicaid or CHIP) (Staras et al., 2010, Rand and Goldstein, 2014). Analyses restricted to adolescents with clinic visits were not adjusted for race/ethnicity due to small sample sizes within some racial/ethnic groups causing lack of convergence. As a sensitivity analysis, we adjusted the analyses for assignment to intervention or non-intervention clinics. While the factorial design enabled assessment of postcards independent of the clinic-level intervention, we conducted this analysis to account for any potential difference due to the clinic-level intervention.
We examined how preventive visits mediated and interacted with the effect of postcards on HPV vaccine initiation using a recently developed causal mediation analysis (VanderWeele, 2014). We decomposed the total effect of postcards on HPV vaccination initiation into four components: (a) the effect of the postcard without a preventive visit (i.e., controlled direct effect); (b) the additive interaction that operates only if preventive visits occur in the absence of postcards (i.e., reference interaction); (c) the additive interaction that operates only if post-cards have an effect on preventive visits (i.e., mediated interaction); and (d) the mediation effect of preventive visits (without interactions) (i.e., pure indirect effect). In partitioning these effects, we adjusted for race/ethnicity, age, and health program enrollment. All analyses were conducted with SAS software version 9.4 (SAS Institute, Inc., Cary, NC). Statistical significance was determined by p-values 0.05.
2.6. Ethics approval and consent to participate
Permission for this use of the claims and enrollment data was granted by the Florida Agency of Health Care Administration under a data use agreement. A waiver of consent was used to send postcards and evaluate claims. This study was approved by the University of Florida Institutional Review Board 01 (IRB 201200143).
3. Results
Random assignment of the postcard intervention resulted in well-balanced measured demographics (Mantel-Hanzel chi-square p-value > 0.2). The study population was racially and ethnically diverse with 49% non-Hispanic white, 26% non-Hispanic black, 15% Hispanic, and 10% from other racial/ethnic groups. Age was fairly evenly distributed with approximately between 10% and 16% in each one-year age group between 12- and 17-year-olds and 20% aged 11 years. The majority (80%) were enrolled in Florida Medicaid and 20% enrolled in CHIP.
For simplicity, only adjusted, main analyses are presented. We found similar estimates for unadjusted, adjusted analyses, and a sensitivity analysis adjusting for clinic intervention participation.
3.1. Postcards increased preventive care
During the three-month study, 14% of girls had a preventive care visit and 25% of girls had only an acute visit. Preventive care visits occurred 1.2 times as often among girls whose parents were mailed a postcard (16%) compared to girls whose parents were not mailed a postcard (13%): Adjusted Rate Ratio (ARR) = 1.2, 95% Confidence Interval (CI) = 1.0 to 1.5. We found no evidence of an effect of postcards on the percentage of girls with only acute visits (26% postcard versus 27% no postcard: ARR = 1.0, 95% CI = 0.9 to 1.1).
3.2. Vaccines were mainly initiated during preventive care
The majority (78%) of girls who initiated the HPV vaccine did so during a preventive visit. Among girls with preventive visits (n = 356), the rate of HPV vaccine initiation was similar regardless of whether parents were mailed postcards (27%) or not (22%; ARR = 1.3, 95% CI = 0.9 to 1.8). The frequency of HPV vaccine initiation during acute visits did not differ by postcard assignment (2.4% postcard versus 2.5% no postcard: ARR = 1.0, 95% CI = 0.4 to 2.6).
3.3. Decomposition of the effect of postcards on HPV vaccination
The overall proportion of the effect of postcards on HPV vaccination mediated by preventive care was 44% (95% CI = 9.2% to 78.0%) (Table 1). The mediated interaction showed that 11.3% of the effect of postcards on HPV vaccination was due to increased preventive visits among those who received postcards (95% CI = 1.5% to 21.1%). The pure indirect effect showed 32.3% of the effect of postcards on HPV vaccination was from postcards increasing the influence of preventive visits on vaccination (95% CI = 1.5% to 63.1%). The increased influence of preventive visits on vaccination may be from parents being more receptive of provider recommendations for HPV vaccination after receiving postcards. A relatively small percentage (8.9%) of the total effect was attributed to postcards increasing HPV vaccination outside of preventive care (i.e., the controlled direct effect).
Table 1.
Percentages of the Total Effect of Postcards on HPV Vaccine Initiation Due to Mediation and Interaction with Preventive Visits.a
| Component | Excess Relative Likelihood of HPV Vaccine Initiation | 95% CI | Percentages Attributable | 95% CI |
|---|---|---|---|---|
| Controlled Direct Effect | 0.05 | (−0.18, 0.28) | 8.9% | (−29.9%, 47.7%) |
| Reference Interaction | 0.26 | (−0.02, 0.54) | 47.5% | (9.7%, 85.4%) |
| Mediated Interaction | 0.06 | (−0.03, 0.15) | 11.3% | (1.5%, 21.1%) |
| Pure Indirect Effect | 0.18 | (−0.01, 0.36) | 32.3% | (1.5%, 63.1%) |
| Total | 0.54 | (0.06, 1.02) | 100% |
Adjusted for age, race/ethnicity, and health program enrolment.
4. Discussion
Postcards mainly increased HPV vaccination within primary care visits, suggesting that postcards prime parents for providers’ recommendations. Yet, the low HPV vaccine initiation rates among girls with preventive visits, regardless of postcard assignment, suggest that raising vaccination rates will require more routine and stronger provider recommendations.
Multi-level interventions that simultaneously deploy reminders with a component targeting increasing provider recommendation frequency and strength may work synergistically to increase HPV vaccination. Evidence suggests that reminder effects can be boosted with provider-targeted interventions (Staras et al., 2015, McLean et al., 2017). Several strategies have shown effectiveness in increasing HPV vaccination by increasing provider recommendation strength and frequency such as a scripted announcement strategy, provider prompts, and education with performance feedback (Leung et al., 2019).
This study has two important limitations. First, consistent with all single-system immunization records (Hendrickson et al., 2015), the Medicaid and CHIP data likely have incomplete vaccination records. Because we randomized postcard assignment, the incompleteness in the vaccination records should be balanced across arms and have little influence on the results. Second, the postcards were sent in 2013 to parents in Northern Florida. In recent years, HPV vaccine initiation rates have increased, but remain low (Walker et al., 2019). Additionally, the Advisory Committee on Immunization Practices has modified guidelines since 2013. (Meites et al., 2016, Petrosky et al., 2015). When the series is started before age 15 years, the guidelines regarding our target population have reduced the number of needed doses from three to two (Meites et al., 2016) Finally, Gardasil 9 is now recommended in the US; thus, the postcards would need to be modified to state that 80% rather than 70% of cervical cancer could be prevented with the vaccine (Petrosky et al., 2015). Evidence-based campaigns are still needed, and directions for multi-level interventions are particularly relevant (Agurs-Collins et al., 2019).
This study has two important strengths. First, our design, an individually randomized trial, is the strongest possible to evaluate postcard effectiveness by controlling for unmeasured confounders including the percentage of girls due for preventive care and potential influence of the in-clinic application. Second, we used a centralized system to identify eligible families and send postcards; thereby reducing cost and improving scalability by reducing clinic burden (Dombkowski et al., 2012).
5. Conclusion
Postcard messages primarily increased HPV vaccination by increasing parents’ receptivity to providers’ HPV vaccine recommendations. Combining reminders with many of the efficacious provider-targeted interventions (e.g., Brewer’s announcement strategy) will likely produce stronger synergistic effects than combining reminders with increased preventive care access (Staras et al., 2015, McLean et al., 2017, Brewer et al., 2017). In particular, widespread provider use of the Centers for Disease Control and Prevention’s recommended bundling style of presenting all three adolescent vaccines the same day and same way may enhance the effectiveness of HPV vaccine reminders since parents will be primed to receive the effective provider recommendation during their child’s well visit (Centers for Disease Control and Prevention, 2019). Additionally, decreasing the time between vaccine reminders and preventive care appointments may maximize the priming effect of reminders. Multi-level interventions should consider including reminders as priming agents for parents combined with an intervention to increase provider recommendation frequency and strength.
6. Final disclosures
Availability of data and materials: The data that support the findings of this study are available from the Florida Agency for Health Care Administration but restrictions apply to the availability of these data, which were used under a data use agreement for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request with permission of the Florida Agency for Health Care Administration and a signed data use agreement.
Funding
Provided by the Society of Adolescent Health and Medicine under a grant received from Merck & Co, and from the University of Florida. All content is solely the responsibility of Grantee and the authors and does not necessarily represent the official views of the Society for Adolescent Health and Medicine.
CRediT authorship contribution statement
Stephanie A.S. Staras: Conceptualization, Methodology, Validation, Formal analysis, Resources, Writing - original draft, Writing - review & editing, Visualization, Supervision, Project administration, Funding acquisition. Susan T. Vadaparampil: Conceptualization, Funding acquisition, Formal analysis, Methodology, Writing - review & editing. Lindsay A. Thompson: Methodology, Writing - review & editing. Courtney Scherr: Formal analysis, Writing - review & editing. Matthew J. Gurka: Formal analysis, Visualization. Stephanie L. Filipp: Formal analysis. Elizabeth A. Shenkman: Resources, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We thank Shivani Desai, MPH for manuscript formatting assistance and our research assistants Kelli Nam and Rachel Lindor, who helped with coding. Postcard designs and graphics are the work of Syzygy Graphics.
References
- Senkomago V., Henley S.J., Thomas C.C., Mix J.M., Markowitz L.E., Saraiya M. Human papillomavirus-attributable cancers - united states, 2012–2016. MMWR Morb. Mortal. Wkly Rep. 2019;68(33):724–728. doi: 10.15585/mmwr.mm6833a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker T.Y., Elam-Evans L.D., Yankey D. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years - united states, 2018. MMWR Morb. Mortal. Wkly Rep. 2019;68(33):718–723. doi: 10.15585/mmwr.mm6833a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Community Preventive Services Task Force. Increasing appropriate vaccination: client reminder and recall systems. The Community Guide: Client Reminder and Recall Systems Web site. http://www.thecommunityguide.org/vaccines/RRclientreminder.html. Published 2015. Updated July 15, 2015. Accessed March 26, 2020.
- Francis D.B., Cates J.R., Wagner K.P.G., Zola T., Fitter J.E., Coyne-Beasley T. Communication technologies to improve HPV vaccination initiation and completion: a systematic review. Patient Educ. Couns. 2017;100(7):1280–1286. doi: 10.1016/j.pec.2017.02.004. [DOI] [PubMed] [Google Scholar]
- Jacobson Vann JC, Jacobson RM, Coyne-Beasley T, Asafu-Adjei JK, Szilagyi PG. Patient reminder and recall interventions to improve immunization rates. The Cochrane database of systematic reviews. 2018;1(1):Cd003941. [DOI] [PMC free article] [PubMed]
- Staras S.A.S., Vadaparampil S.T., Livingston M.D., Thompson L.A., Sanders A.H., Shenkman E.A. Increasing human papillomavirus vaccine initiation among publicly insured Florida adolescents. J. Adolesc. Health. 2015;56(5):S40–S46. doi: 10.1016/j.jadohealth.2014.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLean H.Q., VanWormer J.J., Chow B.D.W. Improving Human Papillomavirus Vaccine Use in an Integrated Health System: Impact of a Provider and Staff Intervention. J. Adolesc. Health. 2017;61(2):252–258. doi: 10.1016/j.jadohealth.2017.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szilagyi P.G., Humiston S.G., Gallivan S., Albertin C., Sandler M., Blumkin A. Effectiveness of a citywide patient immunization navigator program on improving adolescent immunizations and preventive care visit rates. Arch. Pediatr. Adolesc. Med. 2011;165(6):547–553. doi: 10.1001/archpediatrics.2011.73. [DOI] [PubMed] [Google Scholar]
- O'Leary S.T., Lee M., Lockhart S. Effectiveness and cost of bidirectional text messaging for adolescent vaccines and well care. Pediatr. 2015;136(5):e1220–1227. doi: 10.1542/peds.2015-1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Dartmouth Atlas of Health Care. Understanding of the efficiency and effectiveness of the health care system. http://www.dartmouthatlas.org/. Published 2014. Accessed March 26, 2020.
- Centers for Medicare & Medicaid Services. Core set of children’s health care quality measures for Medicaid and CHIP (Child Core Set): technical specifications and resource manual for federal fiscal year 2013 reporting. In. May 2013 ed.
- Centers for Medicare & Medicaid Services. Medicaid and CHIP eligibility levels. https://www.medicaid.gov/medicaid/program-information/medicaid-and-chip-eligibility-levels/index.html. Published 2016. Accessed March 26, 2020.
- Janz N.K., Becker M.H. The Health Belief Model: a decade later. Health Educ. Q. 1984;11(1):1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- Staras S.A.S., Vadaparampil S.T., Patel R.P., Shenkman E.A. Parent perceptions important for HPV vaccine initiation among low income adolescent girls. Vaccine. 2014;32(46):6163–6169. doi: 10.1016/j.vaccine.2014.08.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doak C.C., Doak L.G., Root J.H. 2 ed. Lippincott; Philadelphia: 1996. Teaching patients with low literacy skills. [Google Scholar]
- Staras S.A., Vadaparampil S.T., Haderxhanaj L.T., Shenkman E.A. Disparities in human papillomavirus vaccine series initiation among adolescent girls enrolled in Florida Medicaid programs, 2006–2008. J. Adolesc. Health. 2010;47(4):381–388. doi: 10.1016/j.jadohealth.2010.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rand CM, Goldstein NPN. Patterns of Primary Care Physician Visits for US Adolescents in 2014: Implications for Vaccination. Acad Pediatr. 2018;18(2, Supplement):S72-S78. [DOI] [PubMed]
- VanderWeele T.J. A unification of mediation and interaction: a 4-way decomposition. Epidemiology. 2014;25(5):749–761. doi: 10.1097/EDE.0000000000000121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung SOA, Akinwunmi B, Elias KM, Feldman S. Educating healthcare providers to increase Human Papillomavirus (HPV) vaccination rates: A Qualitative Systematic Review. Vaccine: X. 2019;3:100037. [DOI] [PMC free article] [PubMed]
- Hendrickson B.K., Panchanathan S.S., Petitti D. Evaluation of immunization data completeness within a large community health care system exchanging data with a state immunization information system. J. Public Health Manag. Pract. 2015;21(3):288–295. doi: 10.1097/PHH.0000000000000045. [DOI] [PubMed] [Google Scholar]
- Meites E., Kempe A., Markowitz L.E. Use of a 2-dose schedule for human papillomavirus vaccination - updated recommendations of the advisory committee on immunization practices. MMWR Morb. Mortal. Wkly Rep. 2016;65(49):1405–1408. doi: 10.15585/mmwr.mm6549a5. [DOI] [PubMed] [Google Scholar]
- Petrosky E., Bocchini J.A., Jr., Hariri S. Use of 9-valent human papillomavirus (HPV) vaccine: updated HPV vaccination recommendations of the advisory committee on immunization practices. MMWR Morb. Mortal. Wkly Rep. 2015;64(11):300–304. [PMC free article] [PubMed] [Google Scholar]
- Agurs-Collins T., Persky S., Paskett E.D. Designing and Assessing Multilevel Interventions to Improve Minority Health and Reduce Health Disparities. Am. J. Public Health. 2019;109(S1):S86–S93. doi: 10.2105/AJPH.2018.304730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dombkowski K.J., Cowan A.E., Harrington L.B., Allred N.J., Hudson E., Clark S.J. Feasibility of initiating and sustaining registry-based immunization recall in private practices. Acad. Pediatr. 2012;12(2):104–109. doi: 10.1016/j.acap.2012.01.002. [DOI] [PubMed] [Google Scholar]
- Brewer N.T., Hall M.E., Malo T.L., Gilkey M.B., Quinn B., Lathren C. Announcements Versus Conversations to Improve HPV Vaccination Coverage: A Randomized Trial. Pediatr. 2017;139(1) doi: 10.1542/peds.2016-1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Human Papillomavirus: Boosting Vaccination Rates. https://www.cdc.gov/hpv/hcp/boosting-vacc-rates.html. Published 2019. Updated March 19. Accessed August 5, 2020.