Abstract
Background
The global COVID-19 pandemic has placed tremendous physical and mental strain on the US healthcare system. Studies examining the effects of outbreaks have demonstrated both an increased prevalence and long-term development of Post-Traumatic Stress Disorder (PTSD) symptoms in healthcare providers. We sought to assess the impact of the COVID-19 pandemic on the psychological well-being of medical providers, medical trainees, and administrators at a large academic center to identify stressors and moderators to guide future mental health and hospital-system interventions.
Methods
A 42-item survey examining specific stressors, grit, and resilience was widely distributed to physicians, residents, fellows, and administrators a large academic institution for departmental distribution. Survey results were analyzed using descriptive statistics, ANOVA, and multivariate linear regressions. A p-value <0.05 was considered statistically significant.
Results
A total of 785 participants completed the survey. The majority of respondents rated their stress to be significantly increased during the pandemic. Respondents’ fear of transmitting the virus to their family members was a significant stressor. Higher resilience was associated with lower stress, anxiety, fatigue, and sleep disturbances. Overall, respondents felt supported by their departments and institution and felt contingency plans and personal protective equipment were adequate.
Conclusions
Healthcare workers have increased resilience in the face of heightened stress during a pandemic. Higher resilience and grit were protective factors in managing personal and system-level stressors at the peak of the COVID-19 pandemic in our institution. Implementing an intervention designed to enhance healthcare workers’ resilience in response to the COVID-19 pandemic is warranted.
Background
The novel coronavirus SARS-CoV-2, which causes the disease COVID-19, was first identified in Wuhan, China in December of 2019 and declared a worldwide pandemic by the World Health Organization (WHO) on March 11, 2020.1 The first case of COVID-19 in the United States (US) was reported in mid-January of 2020 and quickly spread to affect all 50 states and the District of Columbia by mid-March.2 , 3 The rapid and widespread nature of this disease is unprecedented in recent history and has placed an enormous strain on the US healthcare system. Additionally, no US Food and Drug Administration (FDA) approved therapeutics or vaccines existed for the virus as of early 2020, conferring an increased daily risk of illness and death on frontline providers.4 Given the unprecedented nature of this pandemic, little is known about how this pandemic impacts the mental well-being of frontline providers.
Preliminary data from the COVID-19 experience in China has shown that frontline medical personnel had significantly higher levels of fear, anxiety, and depression compared to colleagues in lower-risk areas.5 Additionally, medical personnel had significantly higher levels of fear, anxiety, and depression when compared to hospital administration.5 Importantly, increased fear and anxiety are theorized to be psychological vulnerabilities that increase the risk of post-traumatic stress (PTS) symptoms or development of PTS disorder (PTSD).6
Publications assessing the impact of the 2003 severe acute respiratory syndrome (SARS) and the 2015 Middle East respiratory syndrome (MERS) outbreaks offer some guidance when considering the long-term impact of this pandemic on providers. Specifically, providers working in high risk locations such as the SARS wards were 2–3 times more likely to experience PTS symptoms.7 Similarly, providers who performed MERS-related tasks were more at risk for PTSD symptoms than providers who did not have MERS-related duties, an effect which persisted even after some time had passed.8 A review examining the psychological well-being of providers during viral outbreaks demonstrated that providers have higher instances of PTS symptoms and psychological stress when directly caring for infected patients, and that healthcare workers’ PTS symptoms were evident up to three years after the outbreak.9 Promisingly, there may be some psychological factors that safeguard against PTSD in healthcare workers: resilience and grit.
Resilience is considered to be a multidimensional psychological characteristic that enables individuals to thrive in the face of adversity, cope effectively with stress, and maintain stable psychological functioning.10 , 11 Characteristics of resilient people include viewing stressors as challenges to overcome, optimism, commitment, and adaptability to change.10 Resilience is an important trait of intensive care unit (ICU) nurses; compared to nurses diagnosed with PTSD, resilient ICU nurses had a more positive worldview, were cognitively flexible to remain optimistic and utilized positive reframing in response to trauma and stressors, and maintained better self-care habits.11 Additionally, highly resilient nurses had a significantly lower prevalence of burnout and PTSD.12 Among healthcare workers, resilience is clearly protective against the development of PTSD.
Similar to resilience, grit is a psychological characteristic that is defined by passion and perseverance to pursue long-term goals.13 , 14 Grit enables individuals to work strenuously toward challenges and to maintain both interest and effort over time despite adversity, failure, and plateaus in progress. Grit is predictive of better psychological health and lower burnout among surgery residents, and is a predictive factor for surgery residents at risk for attrition from residency.15 , 16 Research on the relationship between grit and resilience in emergency medical service (EMS) workers has also shown that grit is associated with lower PTSD symptoms, and while associated with factors of resilience (i.e., coping mechanisms), grit appears to be a distinct construct.17 Given the potential of frontline healthcare workers to experience significant stress during the COVID-19 pandemic, it is important to consider how resilience and grit may safeguard against these negative psychological factors.
Therefore, we sought to assess the impact of the COVID-19 pandemic on the psychological well-being of medical providers, medical trainees, and administrators as well as identify sources of stress. We examined how two psychological traits, specifically grit and resilience, moderate the impact of the pandemic on respondents’ psychological well-being. Knowledge of whether psychological traits moderate providers’ psychological well-being as well as identification of stressors can help guide future mental health and hospital system interventions moving forward.
Methods
Survey design
The 42-item survey was created by a multiprofessional team of medical education experts using the survey platform Qualtrics (Provo, UT) (Supplementary Figure 1). Indiana University (IU) Institutional Review Board approval was obtained. To assess grit, our team utilized the Short Grit Scale (Grit-S), which is an 8-item measure of perceived grit where users rate how much self-statements (e.g., “I am a hard worker”) reflect them on a 5-point Likert scale (1–5), and thus the sum of the answers can range from 8 to 40.18 Research on the validity evidence of the Grit-S found that this scale has strong internal consistency, is highly correlated with the original 12-item grit scale, has strong predictive validity, and has high test-retest reliability.18 Resilience was assessed with the 2-item version of the Connor-Davidson Resilience Scale (CD-RISC-2), which is a validated measure of a user’s resilience.19 Similar to the Grit-S, users rate their agreement with self-statements on a 5-point Likert scale (0–4), and thus the sum of the answers ranges from 0 to 8.
The remaining survey questions were designed to gauge current levels of various emotions including overall stress at the time of the survey, and change in stress due to COVID-19, as well as the impact of the pandemic on respondents’ nervousness/anxiety, fatigue, and sleep disturbances. Questions were designed regarding job and system-level stressors including concerns regarding salary, meeting productivity goals, institutional support, departmental support, contingency plans, the impact of the pandemic on their daily duties, the need for further training to properly care for patients, the perceived need for personal protective equipment (PPE), and perceived impact on clinical and didactic education. Finally, demographic data was collected including respondent’s department, position, exposure to COVID-19 patients, redeployment status, and whether they volunteered to be redeployed.
The survey was distributed on April 21, 2020 to the IU Vice Chairs of Education who subsequently sent the survey to their respective departments. The survey was also sent to administrators in the IU School of Medicine as well as presidents of individual IU Health system hospitals. The IU School of Medicine is the largest medical school in the United States encompassing nine campuses and seventeen hospitals in more than ten cities, thus the survey was widely distributed to participants across the state of Indiana.20 Faculty, administrators, fellows, and residents were considered for survey inclusion. Reminder emails were sent via the same method both one and two weeks after the survey opened. The survey remained available for a total of three weeks. Of note, the survey was open during the state of Indiana’s peak day of COVID-19 cases on April 26, 2020.21
Statistical analysis
Survey results were imported into Microsoft Excel (Redmond, WA) and respondents’ grit and resilience scores were calculated. Data was then imported into SPSS (Armonk, NY) for further statistical analysis. Mean ± standard deviation (SD) were calculated for continuous data, and total counts were tabulated for categorical data. Any missing data was addressed using the pairwise deletion method. Scores from the grit and resilience scales, along with all of the Likert (1–5) scale responses, were treated as continuous data. The decision to treat the Likert scale as a continuous variable was made due to the large sample size of our study (i.e., more than 10 observations per group), and to gain more robust and unbiased answers offered by a parametric analysis.22 , 23 Likert scale answers 1–5 were converted to a scale from −2 to +2 such that a positive value (+1 and + 2) represents a positive response (agree and strongly agree respectively), while a negative value (−1 and −2) represents a negative response (disagree and strongly disagree respectively). A Likert response of 0 corresponded to the statement “neither agree nor disagree”.
An ANOVA test was utilized to examine participant demographics. In order to identify how the COVID-19 pandemic affected faculty and trainees, we performed linear regression analyses for each dependent variable (questions regarding emotions and stressors) while accounting for confounders such as position (attendings, fellows, residents, administrators), whether they were involved in the care of COVID-19 patients (yes/no), whether they volunteered to be redeployed (yes/no), stress at the time of questionnaire completion, specialty (Internal Medicine, Pediatrics, Family Medicine, Emergency Medicine, Surgery, Obstetrics and Gynecology, Anesthesia, and Others), and grit and resilience scores. Attendings were the reference group for the position analyses while Internal Medicine respondents were the specialty reference group.
Free response answers to the final question, “Any further comments” were qualitatively analyzed for common themes. All statistical analyses were performed using SPSS; p-value <0.05 was considered statistically significant.
Results
A total of 785 participants completed the survey and the final analysis included 720 total eligible participants. 65 participants were excluded from the analysis as they did not classify themselves as an “attending physician”, “fellow”, “resident”, or “administrator”. All survey questions were answered by 97% of the participants. Nearly half of respondents volunteered to be redeployed and more than half were taking care of COVID-19 patients at the time of survey completion; further demographic details can be found in Table 1 .
Table 1.
Participant demographics. PGY, post graduate year; SD, standard deviation. ∗Fellowship years presented as median (range). Post-graduate years presented as median (range).
| Total N | Years of experience (N) |
Caring for COVID-19 patients |
Volunteered for redeployment |
|||||
|---|---|---|---|---|---|---|---|---|
| 0–4 | 5–9 | 10–14 | 15–19 | ≥20 | % of each category | |||
| Attendings | 403 | 92 | 81 | 65 | 62 | 103 | 76.9% | 58.1% |
| Fellows | 40 | 1.5 (1–5) ∗ | 70% | 30% | ||||
| Residents | 154 | 3.0 (1–7) | 76% | 50% | ||||
| Administrators | 65 | – | 9.2% | 7.7% | ||||
| Total | 662 | – | 69.6% | 49.6% | ||||
| Internal Medicine | 187 | 27 | 27 | 18 | 21 | 41 | 76.5% | 45.5% |
| Emergency Medicine | 12 | 3 | 1 | 2 | 0 | 0 | 100% | 33.3% |
| Family Medicine | 27 | 5 | 4 | 0 | 3 | 4 | 63% | 63% |
| Anesthesia | 102 | 13 | 15 | 13 | 12 | 17 | 95.1% | 73.5% |
| Obstetrics & Gynecology | 35 | 8 | 5 | 2 | 4 | 1 | 71.4% | 60% |
| Others | 43 | 4 | 0 | 3 | 2 | 2 | 74.4% | 27.9% |
| Pediatrics | 157 | 22 | 21 | 18 | 13 | 24 | 55.4% | 43.3% |
| School of Medicine | 6 | 0 | 1 | 1 | 1 | 1 | 33.3% | 50% |
| Surgery | 93 | 9 | 9 | 5 | 6 | 13 | 49.5% | 46.2% |
| Total | 662 | 91 | 83 | 62 | 62 | 103 | 69.6% | 49.6% |
Participants across all disciplines and specialties demonstrated equally high average grit and resilience scores (Table 2 ). Both grit and resilience were found to be independent of the participants’ position, specialty, and the stress of taking care of COVID-19 patients. However, resilience was found to have a strong negative association with the overall stress experienced the day of questionnaire completion (coefficient −0.122, p = 0.002).
Table 2.
Healthcare workers’ grit and resilience. Coef, Coefficient of the linear regression; Ref, reference; SD, standard deviation.
| Grit |
Resiliency |
|||||
|---|---|---|---|---|---|---|
| Mean ± SD | Coef | p-value | Mean ± SD | Coef | p-value | |
| Attendings | 31 ± 3.7 | ref | ref | 6.7 ± 1.2 | ref | ref |
| Fellows | 30.3 ± 3.2 | −0.044 | 0.286 | 6.5 ± 1.3 | −0.025 | 0.532 |
| Residents | 30.6 ± 3.3 | −0.057 | 0.170 | 6.7 ± 1.1 | −0.014 | 0.733 |
| Administrators | 31.3 ± 4.1 | 0.014 | 0.767 | 6.8 ± 1.4 | 0.055 | 0.235 |
| Total | 30.9 ± 3.6 | – | – | 6.7 ± 1.2 | – | – |
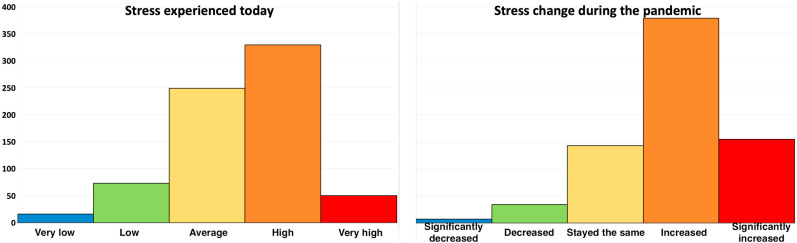
Most respondents (55.2%) agreed that the stress in all aspects of their lives was either high or very high at the time of questionnaire completion, and 76.7% agreed or strongly agreed that the COVID-19 pandemic had caused them additional stress (Fig. 1 ). More specifically, the multivariate analysis revealed that pandemic-induced stress was less prominent in the more resilient participants (coefficient = −0.106, p = 0.009), and those who volunteered to be redeployed (coefficient = −0.122, p = 0.003) even after adjusting for confounders such as taking care of COVID-19 patients. Additionally, respondents reported increased anxiety/nervousness, tiredness/exhaustion, and increased sleep disturbances or insomnia as a result of the pandemic. Interestingly, administrators reported more fatigue and insomnia than attendings. (Supplementary Table S1).
Fig. 1.
Respondents’ stress at the time of survey and stress change due to COVID-19 pandemic.
Multivariate analysis demonstrated that higher resilience (coefficient −0.106, p = 0.009) and willingness to volunteer (coefficient = −0.122, p = 0.003) were negatively associated with perceived stress. Similarly, resilience (coefficient = −0.191, p < 0.001) and willingness to volunteer (coefficient = −0.097, p = 0.018) were both negatively associated with anxiety. Participants who were taking care of COVID-19 patients were more likely to endorse fatigue (coefficient = 0.116, p = 0.010). More resilient participants reported less fatigue (coefficient = −0.104, p = 0.010) and insomnia (coefficient = −0.212, p < 0.001). Respondents from all specialties shared similar feelings regarding the aforementioned variables. However, we identified that even after adjusting for confounders such as caring for COVID-19 patients, the respondents from the Department of Surgery had less stress related to the pandemic (coefficient = −0.191, p < 0.001), less insomnia (coefficient = −0.109, p = 0.010), were less anxious (coefficient = −0.115, p = 0.006), and less fatigued (coefficient = −0.137, p = 0.001) than their colleagues. On the contrary, Obstetrics and Gynecology participants were more nervous (coefficient = 0.107, p = 0.007).
Respondents’ fear of transmitting the virus to their family members was found to be a major source of stress (81.6%) which was further increased when taking care of COVID-19 patients (coefficient = 0.166, p < 0.001). However, most participants thought they had adequate PPE (56.8%) and did not need any additional training to feel safe when caring for COVID-19 patients (46.8%) (Supplementary Table S2). PPE adequacy was negatively correlated with level of stress due to the pandemic (r = −0.109, p = 0.007), while fear for family transmission was positively correlated (r = 0.240, p < 0.001). Residents were less satisfied with the PPE adequacy than the attendings (p = 0.001). Participants who volunteered to be redeployed were more likely to be satisfied with the available PPE (coefficient = 0.102, p = 0.015) and less likely to desire additional COVID-19 training (coefficient = 0.123, p = 0.002). All subspecialties reported similar fears regarding transmitting the virus to their family members. Satisfaction with the PPE adequacy was more common among Anesthesia (coefficient = 0.146, p = 0.001), Surgery (coefficient = 0.148, p = 0.001), and Pediatrics (coefficient = 0.104, p = 0.019) respondents. Finally, the desire for additional COVID-19 related training was more prevalent among Surgery (coefficient = 0.094, p = 0.025), Pediatrics (coefficient = 0.108, p = 0.011), and Obstetrics and Gynecology (coefficient = 0.159, p < 0.001) participants.
Most participants (64.8%) were concerned about work productivity, with attendings being the most concerned, and residents the least concerned. Similarly, 59.4% had concerns regarding salary cuts and furloughs, with the attendings again being more concerned than the residents. Only a small proportion of the sample size was concerned about academic promotion (33.5%), most of whom were fellows (Supplementary Table S3). Among subspecialties, no significant differences were observed regarding promotion and salary concerns. However, productivity concerns were more prominent among procedural specialties such as Surgery (coefficient = 0.101, p = 0.017) and Obstetrics and Gynecology (coefficient = 0.143, p < 0.001).
In general, most participants felt supported by both the hospital (56.4%) and their respective department (77.4%). Residents reported feeling less supported by hospital administration compared to attendings (coefficient = −0.203, p < 0.001). Most respondents felt satisfied with their department’s contingency plans (76.7%). Similarly, the institutional response to the pandemic was largely favorable (72.7%), with residents less satisfied than attendings (coefficient = −0.160, p < 0.001).
Eighty-seven participants provided a written response to the open-ended question “Any further comments?“. From those comments, six themes emerged (Table 3 ): (1) feelings of being supported; (2) concerns related to leadership; (3) dynamic experiences; (4) stress of undertaking higher risk; (5) concerns related to PPE; and (6) stress related to the unknown. The first theme reflected many respondents feeling supported by their institution, department, and team members providing statements such as, “Leadership … (has) done an outstanding job with updates and our nightly(,) now biweekly zoom meetings. I have found these incredibly valuable and they have helped me feel connected and informed. They have been honest, transparent and realistic.”
Table 3.
Identified themes from respondent comments with representative quotes.
| Theme | Respondent Comment |
|---|---|
| (1) Feelings of being supported |
“I have been incredibly impressed by how well-supported I have been … I am especially thankful for no pay cuts in salary since my husband is now unemployed.” “I have been inspired by the collective teamwork and dynamic responses throughout the (school of medicine) to adapt quickly and what I feel has been in the best interest of the patients, residents, faculty, staff on all levels …” |
| (2) Concerns related to leadership | “Shame on those sitting in their offices (without patient/co(−)worker contact taking no risk) suggest(ing) that I am not due an N95.” |
| (3) Dynamic experiences |
“One month ago I was actually more stressed. I feel things are better now that we have stay-at-home and PPE is better through acquisition and conservation. We are still in crisis mode.” “Trying to follow the policy guidance blanket across the whole hospital is challenging when the patient population I am caring for is impacted in a very different way.” |
| (4) Stress of undertaking higher risk | “… because I am young and otherwise healthy and relatively low risk for severe COVID-19 infection, this risk is certainly not zero. And while I feel some duty as a physician to help people, self-preservation is a very strong instinct to ignore …” |
| (5) Concerns related to PPE | “I feel responsible for the safety and wellbeing of our clinical team, yet the rigid PPE rules and removal of PPE from our site to place at other sites without ever learning about us or understanding us is unfathomable. The rules around PPE usage have been driven by PPE availability rather than protecting the worker … I lose sleep at night because of that.” |
| (6) Stress related to the unknown |
“The fear of the unknown with this virus and limited data that has come out has made our high standards in caring for our patients slip.” “I miss my family and don’t (feel) like there’s an end in sight, lots of feelings of helplessness and hopelessness. Feeling the impact of waning community support and protests.” |
The second theme, concerns related to leadership, reflected respondents’ stress related to decisions made by leadership not in direct contact with patients, faculty, fellows, or residents. Responses revealed many decisions challenged the respondent’s value system related to standards of patient care, policy regarding distribution of PPE, or lack of effective communication during a time of crisis. The third theme revealed that healthcare workers experiences are dynamic. Respondents reported they were more stressed initially, but their stress has decreased over time. The fourth theme, undertaking high risk, encompassed stress related to aerosolized procedures, exposing family to the virus, and feeling forced to come to work despite a pandemic. The fifth theme described that respondents felt PPE policy was based on availability rather than protection of healthcare providers. One respondent shared, “While I recognize that the PPE shortage is a nationwide issue, it feels very inauthentic for our institution to pretend our PPE is adequate … Reusing single use items is never best practice(s)”. This contrasted with the statistically significant data from the survey that showed respondents felt they had adequate PPE to safely care for patients. The final theme, stress related to the unknown, compiled a group of responses related to uncertainty of the future of medicine, schedule variabilities, and limited data about the virus during the peak of the pandemic. While not globally reflected in comments, respondents also shared concerns about the national government’s response to the pandemic, feeling impacted by protests in the community, and lack of consistent information about reopening society to the public.
Discussion
The results from our study confirm the general assumption that healthcare providers are experiencing higher levels of stress during the COVID-19 pandemic with greater than 76% of respondents identifying that COVID-19 had caused increased stress. Likewise, more than 55% of respondents had high or very high stress at the time of the survey. We found that the stress of providers caring for COVID-19 at our institution was compounded with concern for one’s own health and worries of exposing family members to COVID-19 as well as increased anxiety, insomnia, and fatigue. These findings are additionally concerning in light of the fact that fatigue has been linked to medical errors and resultant negative impact on patient outcomes.24
These findings should be discussed in conjunction with the institutional disease burden to gain a better understanding of the results. Testing limitations posed a challenge for providers during this time. Testing turnaround time was inconsistent, there was concern for test accuracy, and widespread testing was not yet available. A temporary COVID unit was constructed outside one of the hospitals for care of hospital overflow COVID patients, however inpatient ventilator use was only at 40% at the time of the survey. When the survey closed there were 114 confirmed cases and 122 suspected cases at our institution. In the state of Indiana, there were a total of 27,778 confirmed cases at survey closure. Also, at the time of survey 4015 team members had been tested for COVID with 413 positive test results. While case numbers do not demonstrate and overwhelming disease burden comparable to that of New York City, the stress identified was not due to the system being overwhelmed or lack of ventilators or intensive care unit beds but that providers were impacted negatively or highly stressed anyway.
Stressors at the system-level were immediately apparent in this survey. Attendings reported more stress related to potential salary cuts or furloughs as a result of the pandemic. These concerns were likely directly related to national recommendations to halt elective surgeries and procedures at the onset of the pandemic.25 In addition, graduating fellows, who expressed the greatest concern regarding jobs and promotion, are currently entering a difficult job market with record unemployment.26
Personal stressors were also readily apparent in this survey and included concerns about loss of professional identity, overall increased visceral responses to stress, and worry about transmission of COVID-19 to family members. We specifically identified fatigue and insomnia as symptoms associated with increased stress during the pandemic. To decrease negative effects during novel outbreaks on providers, Kisely et al. identified the need to provide sufficient time away from work and rest.9 It is reasonable to conclude that lack of time away from work for rest would exacerbate these symptoms in providers constantly exposed to stressors when caring for COVID-19 patients.
We hypothesized that the psychological factors of resilience and grit would positively impact the respondents in our survey. Our findings suggested that resilience was a critical factor given its significant association with lower perceived stress at the time of survey completion, lower stress due to the pandemic, and lower feelings of anxiety, fatigue, and insomnia. In light of these findings, it is apparent that resilience may be an important protective factor against deleterious psychological responses to the COVID-19 pandemic for frontline healthcare workers and administrators alike. The two questions on resilience included in our survey specifically inquire about respondents’ ability to adapt when changes occur and their tendency to bounce back after hardships. It is possible that more resilient individuals in the current study utilized more adaptive coping strategies to manage their stress related to the COVID-19 pandemic, and thus, experienced lower stress as a result.
We also found that higher resilience was associated with increased willingness of healthcare providers to volunteer to be re-deployed to a frontline service during the pandemic. Unlike those providers who experienced significant stress due to the unknown dangers of the COVID-19 pandemic, healthcare providers who are more resilient may perceive that they are capable to effectively manage unknown challenges or feel more capable to bounce back if faced with illness or hardship related to the pandemic.
Given the importance of resilience to safeguard against negative psychological effects from the COVID-19 pandemic, healthcare systems should look at enhancing resilience among their employees (i.e., frontline providers and administrators). There have been promising efforts to implement interventions with healthcare providers to increase their resilience. Mealer et al. developed a feasible and beneficial 12-week resilience training course for ICU nurses that taught key skills such as self-care topics, cognitive behavioral therapy, mindfulness-based stress reduction, expressive writing, and event-triggered counseling sessions.27 In another study, a resilience intervention consisting of cognitive reframing and structured relaxation training was implemented with Department of Medicine faculty.28 Compared to controls who did not receive resilience training, the resilience intervention group reported enhanced resilience and quality of life, as well as reduced stress and anxiety.28 Based on the available literature, implementing interventions to enhance healthcare workers’ resilience appears feasible and effective.
Respondents identified that the institutional and departmental leadership response to the pandemic has been positive and supportive. While the correlation may not be statistically significant, we can speculate that the collegial, team-focused culture at our institution contributes positively to the experience of being a healthcare provider in the face of a novel virus pandemic. We also found that grit was high at our institution across all disciplines and specialties (i.e., average grit score was 30.99 out of 40). It could also be speculated that high grit is a protective attribute and when combined with the team-centric focus at our institution, providers have remained more optimistic in light of increased stress as related to this pandemic.
This survey was a large volume study at a major academic center encompassing 17 hospitals. Nonetheless, there were some limitations that we would like to discuss. Although this survey included responses from a wide variety of departments, some departments had a disproportionately low number of responses relative to their size, such as the departments of Emergency Medicine and Family Medicine. This may have resulted in sampling bias for those specialties, which may have led to the compelling finding of Family Medicine (n = 20 of 785) as the only specialty to have a statistically significantly higher grit score as compared to all others. This variability in departmental response may have been due to the method of survey distribution, which also limited our ability to calculate a response rate for our survey as the number of providers receiving the survey is unknown. Other departmental initiatives may also have impacted our study as there were several other COVID-affiliated surveys circulated at the time of this survey which may have led to some degree of survey fatigue from potential respondents as well. This was especially true for our Emergency Medicine colleagues, who were all part of a departmental longitudinal survey, which explains their lower response rate. Despite this, we felt we received an adequate distribution of responses as Internal Medicine handled most COVID-related patient care and thus we had a strong sample of frontline workers. An additional limitation of this survey is that it was sent only to physicians and administrators. Future iterations of the survey have already been initiated and are currently being distributed to both Advanced Practice Providers and Medical Students.
Based on the results of this study, hospital leadership must be cognizant of the existence of PTSD risk factors amongst healthcare providers during a pandemic and develop ways to support healthcare providers moving forward. Mental skills are trainable psychological strategies designed to help individuals manage stress effectively and optimize performance.29 Our team has developed a novel, comprehensive mental skills curriculum (MSC) to systematically teach healthcare providers strategies such as goal setting, arousal and attention management techniques, and mental imagery, to enable them to manage their mental state effectively. We have obtained validity evidence that our curriculum can effectively enhance novices’ use of mental skills and surgical performance,30 reduce novices’ cognitive workload and stress during two validated stress tests,31 and maintain residents’ performance significantly better than controls under heightened stress.29 The IU Department of Surgery has made the commitment to implement this training at the resident level. In spite of this curriculum’s effectiveness to help trainees manage acute stress effectively, it is unclear whether it enhances providers’ resilience to manage more chronic or traumatic stress. Given the importance of resilience observed in the current study, it may be necessary to refine our curriculum to incorporate strategies to optimize providers’ resilience.
One potential technique to enhance providers’ resilience is mindfulness-based stress reduction (MBSR). Mindfulness is a type of meditation derived from Buddhism, that focuses on present, non-judgmental awareness of one’s thoughts, emotions, and behaviors.32 MBSR trains users to become mindful of maladaptive thought and emotional responses to events, and allows them the ability to intentionally implement more objective and productive thoughts that translate into feelings of increased control and agency over their responses to events, and reduced feelings of helplessness, depression, and anxiety. Among healthcare providers, MBSR has been shown to reduce stress and increase quality of life.32 In addition to a curricular module on mindfulness teaching learners to identify maladaptive stress coping strategies, we also plan to develop a module on resilience strategies. One strategy we plan to implement is developing meaning-based coping strategies through cognitive reframing. Cognitive reframing is a technique often implemented in cognitive behavioral therapy that aims to replace negative and maladaptive thoughts (e.g., ruminating on negatives, catastrophizing) with more objective and positive thoughts.33 In a study on healthcare providers’ stress coping strategies used when breaking bad news, researchers found that those providers who coped more effectively with breaking bad news to patients often utilized cognitive reframing to focus on their meaning as healthcare providers and providing the best care possible to their patients.34 Through a combination of adding MBSR and strategies like cognitive reframing to our existing MSC, we are hopeful that we can help providers recognize maladaptive or negative thought patterns and intentionally intervene with more objective and optimistic thought patterns. Accordingly, we plan to offer workshops to disseminate these skills to providers of all levels at our institution moving forward.
Conclusion
Our results from this large multidisciplinary survey confirm that healthcare providers are experiencing higher levels of stress during the COVID-19 pandemic. We have additionally shown that healthcare providers have high grit and resilience, and that resilience is protective against stress and other negative psychological factors resulting from this pandemic. Future research should evaluate the efficacy of mental skills and resilience training in frontline workers to reduce symptoms of PTSD in future times of global crisis.
Acknowledgements
Thank you to Drs. Paul M. Wallach, John D. Buckley, Ruben H. Hernandez, Anthony L. Shanks, Bobbi J. Byrne, and Sally A. Mitchell for their support of this project and assistance in survey distribution.
Footnotes
Supplementary Table S1.
| Total N | Years of experience (N) |
Taking care of COVID patients |
Volunteered for redeployment |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 0–4 | 5–9 | 10–14 | 15–19 | >20 | % of each category | % of each category | |||||
| Attendings | 403 | 92 | 81 | 65 | 62 | 103 | 76.9% | 58.1% | |||
| Fellows | 40 | 1.5 (1–5) ∗ | 70% | 30% | |||||||
| Residents | 154 | 3.0 (1–7) | 76% | 50% | |||||||
| Administrators | 65 | – | 9.2% | 7.7% | |||||||
| Total | 662 | – | 69.6% | 49.6% | |||||||
| Internal Medicine | 187 | 27 | 27 | 18 | 21 | 41 | 76.5% | 45.5% | |||
| Emergency Medicine | 12 | 3 | 1 | 2 | 0 | 0 | 100% | 33.3% | |||
| Family Medicine | 27 | 5 | 4 | 0 | 3 | 4 | 63% | 63% | |||
| Anesthesia | 102 | 13 | 15 | 13 | 12 | 17 | 95.1% | 73.5% | |||
| Obstetrics & Gynecology | 35 | 8 | 5 | 2 | 4 | 1 | 71.4% | 60% | |||
| Others | 43 | 4 | 0 | 3 | 2 | 2 | 74.4% | 27.9% | |||
| Pediatrics | 157 | 22 | 21 | 18 | 13 | 24 | 55.4% | 43.3% | |||
| School of Medicine | 6 | 0 | 1 | 1 | 1 | 1 | 33.3% | 50% | |||
| Surgery | 93 | 9 | 9 | 5 | 6 | 13 | 49.5% | 46.2% | |||
| Total | 662 | 91 | 83 | 62 | 62 | 103 | 69.6% | 49.6% | |||
Supplementary Table S2.
| Grit | Resiliency | |||||
|---|---|---|---|---|---|---|
| Mean ± SD | Coef | p-value | Mean ± SD | Coef | p-value | |
| Attendings | 31 ± 3.7 | ref | ref | 6.7 ± 1.2 | ref | ref |
| Fellows | 30.3 ± 3.2 | −0.044 | 0.286 | 6.5 ± 1.3 | −0.025 | 0.532 |
| Residents | 30.6 ± 3.3 | −0.057 | 0.170 | 6.7 ± 1.1 | −0.014 | 0.733 |
| Administrators | 31.3 ± 4.1 | 0.014 | 0.767 | 6.8 ± 1.4 | 0.055 | 0.235 |
| Total | 30.9 ± 3.6 | – | – | 6.7 ± 1.2 | – | – |
Supplementary Table S3.
| Productivity concern |
Promotion concern |
Salary concern |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Coef | p-value | Mean ± SD | Coef | p- value | Mean ± SD | Coef | p- value | |
| Attendings | 0.8 ± 1.1 | ref | ref | −0.2 ± 1.1 | ref | ref | 0.7 ± 1.1 | ref | ref |
| Fellows | 0.7 ± 1.3 | −0.27 | 0.491 | 0.5 ± 1.4 | 0.125 | 0.02 | 0.4 ± 1.4 | −0.075 | 0.058 |
| Residents | 0.3 ± 1.1 | −0.198 | <0.001 | 0.03 ± 1.2 | 0.073 | 0.067 | −0.1 ± 1.1 | −0.274 | <0.001 |
| Administrators | 0.7 ± 1.1 | −0.083 | 0.067 | 0.04 ± 1.0 | 0.047 | 0.308 | 0.8 ± 1.1 | 0.023 | 0.608 |
| Total | 0.6 ± 1.1 | – | – | −0.04 ± 1.1 | – | – | 0.6 ± 1.1 | – | – |
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.WHO Timeline - COVID-19 2020. https://www.who.int/news-room/detail/27-04-2020-who-timeline---covid-19
- 2.Previous U.S. 2020. COVID-19 Case Data.https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/previouscases.html [Google Scholar]
- 3.Geographic differences in COVID-19 cases, deaths, and incidence — United States. https://www.cdc.gov/mmwr/volumes/69/wr/mm6915e4.htm February 12–April 7, 2020. 2020. [DOI] [PMC free article] [PubMed]
- 4.Information for clinicians on investigational therapeutics for patients with COVID-19. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/therapeutic-options.html
- 5.Lu W., Wang H., Lin Y., Li L. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatr Res. 2020;288 doi: 10.1016/j.psychres.2020.112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elwood L.S., Hahn K.S., Olatunji B.O., Williams N.L. Cognitive vulnerabilities to the development of PTSD: a review of four vulnerabilities and the proposal of an integrative vulnerability model. Clin Psychol Rev. 2009;29:87–100. doi: 10.1016/j.cpr.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 7.Wu P., Fang Y., Guan Z. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatr. 2009;54:302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee S.M., Kang W.S., Cho A.R., Kim T., Park J.K. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr Psychiatr. 2018;87:123–127. doi: 10.1016/j.comppsych.2018.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kisely S., Warren N., McMahon L., Dalais C., Henry I., Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369 doi: 10.1136/bmj.m1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Connor K.M., Davidson J.R. Development of a new resilience scale: the connor-davidson resilience scale (CD-RISC) Depress Anxiety. 2003;18:76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- 11.Mealer M., Jones J., Moss M. A qualitative study of resilience and posttraumatic stress disorder in United States ICU nurses. Intensive Care Med. 2012;38:1445–1451. doi: 10.1007/s00134-012-2600-6. [DOI] [PubMed] [Google Scholar]
- 12.Mealer M., Jones J., Newman J., McFann K.K., Rothbaum B., Moss M. The presence of resilience is associated with a healthier psychological profile in intensive care unit (ICU) nurses: results of a national survey. Int J Nurs Stud. 2012;49:292–299. doi: 10.1016/j.ijnurstu.2011.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Duckworth A. Grit : The Power of Passion and Perseverance. First Scribner hardcover edition. Scribner; New York: 2016. [Google Scholar]
- 14.Duckworth A.L., Peterson C., Matthews M.D., Kelly D.R. Grit: perseverance and passion for long-term goals. J Pers Soc Psychol. 2007;92:1087–1101. doi: 10.1037/0022-3514.92.6.1087. [DOI] [PubMed] [Google Scholar]
- 15.Salles A., Cohen G.L., Mueller C.M. The relationship between grit and resident well-being. Am J Surg. 2014;207:251–254. doi: 10.1016/j.amjsurg.2013.09.006. [DOI] [PubMed] [Google Scholar]
- 16.Salles A., Lin D., Liebert C. Grit as a predictor of risk of attrition in surgical residency. Am J Surg. 2017;213:288–291. doi: 10.1016/j.amjsurg.2016.10.012. [DOI] [PubMed] [Google Scholar]
- 17.Musso M., Tatum D., Hamer D., Hammarlund R., Son L., McMahon P. The relationship between grit and resilience in emergency medical service personnel. Ochsner J. 2019;19:199–203. doi: 10.31486/toj.18.0144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Duckworth A.L., Quinn P.D. Development and validation of the short grit scale (grit-s) J Pers Assess. 2009;91:166–174. doi: 10.1080/00223890802634290. [DOI] [PubMed] [Google Scholar]
- 19.Vaishnavi S., Connor K., Davidson J.R. An abbreviated version of the Connor-Davidson Resilience Scale (CD-RISC), the CD-RISC2: psychometric properties and applications in psychopharmacological trials. Psychiatr Res. 2007;152:293–297. doi: 10.1016/j.psychres.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.About our system. https://iuhealth.org/about-our-system
- 21.Indiana’s novel coronavirus response. 2020. https://www.coronavirus.in.gov/
- 22.Jamieson S. Likert scales: how to (ab)use them. Med Educ. 2004;38:1217–1218. doi: 10.1111/j.1365-2929.2004.02012.x. [DOI] [PubMed] [Google Scholar]
- 23.Norman G. Likert scales, levels of measurement and the "laws" of statistics. Adv Health Sci Educ : Theor Pract. 2010;15:625–632. doi: 10.1007/s10459-010-9222-y. [DOI] [PubMed] [Google Scholar]
- 24.Tawfik D.S., Profit J., Morgenthaler T.I. Physician burnout, well-being, and work unit safety grades in relationship to reported medical errors. Mayo Clin Proc. 2018;93:1571–1580. doi: 10.1016/j.mayocp.2018.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.COVID-19: recommendations for management of elective surgical procedures. 2020. https://www.facs.org/covid-19/clinical-guidance/elective-surgery
- 26.Economic news release. 2020. https://www.bls.gov/news.release/empsit.nr0.htm
- 27.Mealer M., Conrad D., Evans J. Feasibility and acceptability of a resilience training program for intensive care unit nurses. Am J Crit Care. 2014;23:e97–e105. doi: 10.4037/ajcc2014747. [DOI] [PubMed] [Google Scholar]
- 28.Sood A., Prasad K., Schroeder D., Varkey P. Stress management and resilience training among Department of Medicine faculty: a pilot randomized clinical trial. J Gen Intern Med. 2011;26:858–861. doi: 10.1007/s11606-011-1640-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Anton N.E., Mizota T., Whiteside J.A., Myers E.M., Bean E.A., Stefanidis D. Mental skills training limits the decay in operative technical skill under stressful conditions: results of a multisite, randomized controlled study. Surgery. 2019;165:1059–1064. doi: 10.1016/j.surg.2019.01.011. [DOI] [PubMed] [Google Scholar]
- 30.Stefanidis D., Anton N.E., McRary G. Implementation results of a novel comprehensive mental skills curriculum during simulator training. Am J Surg. 2017;213:353–361. doi: 10.1016/j.amjsurg.2016.06.027. [DOI] [PubMed] [Google Scholar]
- 31.Anton N.E., Howley L.D., Pimentel M., Davis C.K., Brown C., Stefanidis D. Effectiveness of a mental skills curriculum to reduce novices’ stress. J Surg Res. 2016;206:199–205. doi: 10.1016/j.jss.2016.07.019. [DOI] [PubMed] [Google Scholar]
- 32.Shapiro S.L., Astin J.A., Bishop S.R., Cordova M. Mindfulness-based stress reduction for health care professionals: results from a randomized trial. Int J Stress Manag. 2005;12:164–176. [Google Scholar]
- 33.Robson J.P., Jr., Troutman-Jordan M. A concept analysis of cognitive reframing. J Theor Construct Test. 2014;18:55–60. [Google Scholar]
- 34.Shaw J.M., Brown R.F., Dunn S.M. A qualitative study of stress and coping responses in doctors breaking bad news. Patient Educ Counsel. 2013;91:243–248. doi: 10.1016/j.pec.2012.11.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.