Abstract
Introduction
The COVID-19 pandemic has led to changes in NHS surgical service provision, including reduced elective surgical and endoscopic activity, with only essential emergency surgery being undertaken. This, combined with the government-imposed lockdown, may have impacted on patient attendance, severity of surgical disease, and outcomes. The aim of this study was to investigate a possible ‘lockdown’ effect on the volume and severity of surgical admissions and their outcomes.
Methods
Two separate cohorts of adult emergency general surgery inpatient admissions 30 days immediately before (February 16, 2020 to March 15, 2020), and after UK government advice (March 16, 2020 to April 15, 2020). Data were collected relating to patient characteristics, severity of disease, clinical outcomes, and compared between these groups.
Results
Following lockdown, a significant reduction in median daily admissions from 7 to 3 per day (p < 0.001) was observed. Post-lockdown patients were significantly older, frailer with higher inflammatory indices and rates of acute kidney injury, and also were significantly more likely to present with gastrointestinal cancer, obstruction, and perforation. Patients had significantly higher rates of Clavien-Dindo Grade ≥3 complications (p = 0.001), all cause 30-day mortality (8.5% vs. 2.9%, p = 0.028), but no significant difference was observed in operative 30-day mortality.
Conclusion
There appears to be a “lockdown” effect on general surgical admissions with a profound impact; fewer surgical admissions, more acutely unwell surgical patients, and an increase in all cause 30-day mortality. Patients should be advised to present promptly with gastrointestinal symptoms, and this should be reinforced for future lockdowns during the pandemic.
Keywords: COVID-19, Lockdown effect, Emergency surgery, Volume, Severity
1. Introduction
In early December 2019, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a novel coronavirus, emerged in the city of Wuhan, Hubei, China [1,2]. The first cases of this virus were detected in the United Kingdom (UK) on the January 31, 2020 [3], and since then over 275,000 patients have had confirmed infection and over 39,000 have died [4].
As part of the response to the pandemic, on March 16, 2020 the UK government advised that people with certain health conditions should ‘shield’ and avoid all contact with others. The remainder of the population were directly instructed to avoid all ‘non-essential’ travel unless to seek emergency medical care, or for one period of exercise, or to obtain necessary food [5]. From this time, the UK was in a period of ‘lockdown’ to mitigate the transmission of the virus. In an attempt to protect patients, surgeons and other staff from infection, the Intercollegiate Board of the Four Royal Colleges of Surgeons and the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) released initial guidance in March 2020 which advised surgeons to consider open surgery over laparoscopic surgery and to only operate in immediately lifesaving emergencies [6,7]. To maximise inpatient and critical care capacity for the pandemic, on the March 17, 2020 NHS England and NHS Improvement advised all trusts to postpone all non-urgent elective operations from the 15th of April at the latest [8], however many trusts implemented this instruction shortly after it was issued.
In response to government instructions, patients who normally attend with acute medical issues were therefore advised only to travel in a medical emergency [5]. Following this there was a decrease in hospital presentations, with one million less attendance at Accident and Emergency (A&E) in April 2020 (916,581) compared to February 2020 (1,969,691) [9]. Across multiple countries, healthcare systems and specialities there is increasing evidence of a significant reduction in attendance and delays in presentation which is resulting in poorer patient outcomes [[10], [11], [12], [13]]. A Spanish cohort [14] identified a 65.4% decrease in emergency surgical activity, a delay in presentation from symptom onset (from 42.1 to 70.8 h), and an increased proportion of presentations with non-deferrable emergency conditions, such as obstruction and incarcerated hernia. Consequently, patients requiring specialist care may either not present at all, or present with advanced disease due to their delayed presentation.
The aim of this study was to investigate the impact of the UK Government's ‘lockdown’ on the volume and severity of surgical admissions during the COVID-19 pandemic by evaluating changes in the aetiology of presentations, management approach and short-term outcomes for these patients. These observations may be utilised to inform future surgical practice during subsequent COVID-19 surges locally and may help to inform surgical decisions across the NHS.
2. Methods
2.1. Study design and participants
Two separate cohorts of adult emergency general surgery inpatient admissions immediately before and during the COVID-19 pandemic at a large University hospital in the North of England providing specialist services to a population of over 450,000 people) were included in this study. These cohorts were defined by admission 30 days prior to, or 30 days following, UK Government instruction regarding ‘non-essential’ travel on the March 16, 2020 [5] referred to as day 1 of the beginning of ‘lockdown’. Consecutive emergency admissions to the hospital in the 30 days prior to the lockdown (February 16, 2020 to March 15, 2020) were referred to as the historical cohort (pre-lockdown group) and this data was collected retrospectively. Those who were admitted from the March 16, 2020 to April 15, 2020 were the study cohort (post-lockdown group) with prospective data collection. The main inclusion criteria were any adult (≥16 years old) patients who were admitted for more than 24 h requiring specialist general surgical assessment and treatment or referred from another specialty requiring the same. Patients were excluded from the study if they were admitted and transferred to urological services, admitted for less than 24 h, or under 16 years of age. All patients were followed-up for 30 days following admission to obtain short-term outcomes. The study protocol was prospectively approved as an observational service evaluation by the Research and Development department at the Trust. This study has been reported in line with the STROCSS criteria [15].
2.2. Data collection
Included patients had their anonymised data extracted from prospectively maintained electronic medical records, TrakCare® (Intersystems, Cambridge, MA, USA) using a standardised data collection form. These included demographic, clinical, laboratory, treatment, and surgical outcomes. Data were collected retrospectively for the historical cohort, and prospectively for the study cohort. These were entered and maintained within an encrypted spreadsheet on a secure Trust computer.
Patient characteristics collected included patient age, gender, postcode, and ethnicity (classified as white or Black, Asian and Minority Ethnic (BAME)). Calculation of deprivation scores were achieved by conversion of postal codes to Index of Multiple Deprivations scores using a validated online conversion tool [16]. Clinical diagnoses and pre-existing co-morbidities were then converted to Charlson Scores using the weightings employed by the hospital standardised mortality ratio [17,18]. Patients’ COVID-19 status was obtained from SARS-CoV-2 RNA testing, and/or pathognomonic features on chest X-ray and computed tomography (CT) of chest. Of note, the first documented case of COVID-19 in the hospital was March 17, 2020.
Severity of patient presentation was accounted for by collecting:
-
-
The National Emergency Warning Score (NEWS), to evaluate for organ dysfunction [19].
-
-
Initial Biochemistry and Haematology blood investigation results including white cell count (WCC), C-reactive protein (CRP), lactate, presence of metabolic acidosis, acute kidney injury (AKI); and if diagnosed as pancreatitis, their Glasgow-Imrie Score [20].
-
-
National Emergency Laparotomy Audit Risk Prediction Score [21] (for patients who progressed to laparotomy)
-
-
Patient's imaging findings (including Hinchey grade [22] if diagnosed with diverticulitis).
Primary diagnoses were identified and documented to establish whether there were any changes to accepted best surgical practice. Documented management strategies were categorised into: conservative with or without antibiotic treatment (and duration), radiological interventions, and endoscopic or operative interventions. Operative interventions were categorised into minor, moderate, major or complex major according to grade of surgery [23,24]. Additionally, operations undertaken laparoscopically or open were evaluated.
The main outcomes for this observational study were aetiology and severity of surgical disease at presentation, initial management strategies instigated, length of stay in hospital and intensive care, unplanned readmission to hospital or intensive care, postoperative complications (defined by the Clavien-Dindo Classification [25]), and all-cause patient mortality within 30 days of admission and operative 30-day mortality.
2.3. Statistical analysis
The historical cohort were compared to the study cohort to assess for any difference in admissions, severity of presentation and outcomes for patients. Continuous variables are presented as mean (95% confidence interval) or median (interquartile range), depending on the normality of data distribution, and compared using the independent t-test or Mann–Whitney U test, as appropriate. Categorical variables are presented as frequency with percentages, and were analysed using Pearson's χ2 test and Fisher's exact test. The factors associated with 30-day mortality following admission were determined using a logistic regression model. Clinically relevant factors with p < 0.200 in the univariable models were entered into multivariable models. The multivariable models were built by inclusion of variables that achieved p < 0.050 and significant improvement of model fit (reduction in Akaike's Information Criterion ≥4). A p-value <0.05 was used to denote statistical significance. Missing data (0.1%) were excluded from analyses on a case-by-case basis. These data were collected in Excel® 2010 (Microsoft, Redmond, Washington, USA) and analyses were undertaken using SPSS® Statistics 25 (IBM Corp., Armonk, NY, USA).
3. Results
3.1. Patient characteristics
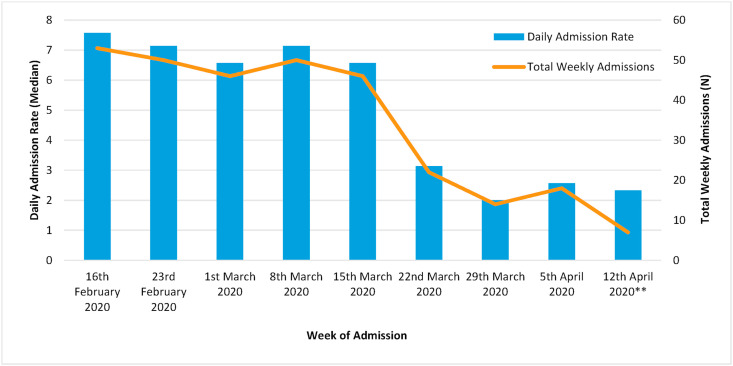
During the study period, 313 patients were admitted under the care of general surgery. There was a significant reduction in admissions following the Government's instruction on the March 16, 2020 (Fig. 1 ) from a median of 7 to 3 daily admissions (p < 0.001). Patients admitted during the post-lockdown period were found to be significantly more frail than those admitted in the pre-lockdown period (Table 1 ); they were older, had more co-morbidities (including hypertension, pre-existing lung disease, and chronic kidney disease), and had a poorer physiological function, as defined by the ASA score. Six patients were diagnosed with COVID-19 in the 30-days following their admission in the post-lockdown period.
Fig. 1.
Weekly changes in emergency admissions to general surgery over the course of the study period. Government advice dated March 16, 2020.
** Study censored on April 15, 2020.
Table 1.
Characteristics and clinical severity of patients admitted to general surgery during the COVID-19 pandemic, by study period.
| Patient Characteristics | Pre-Lockdown (n = 207) | Post-Lockdown (n = 106) | Overall (n = 313) | p-value |
|---|---|---|---|---|
| Age*‡ | 50.5 (47.8,53.1) | 57.5 (53.9,61.1) | 52.8 (50.7,55.0) | 0.002 |
| Gender | 0.687 | |||
| Male | 81 (39.1) | 39 (36.8) | 120 (38.3) | |
| Female | 126 (60.9) | 67 (63.2) | 193 (61.7) | |
| Ethnicity | 0.199 | |||
| White | 197 (95.2) | 104 (98.1) | 301 (96.2) | |
| BAME | 10 (4.8) | 2 (1.9) | 12 (3.8) | |
| Deprivation Quintile | 0.660 | |||
| 1 (Most) | 94 (45.4) | 49 (46.2) | 143 (45.7) | |
| 2 | 38 (18.4) | 22 (20.8) | 60 (19.2) | |
| 3 | 18 (8.7) | 13 (12.3) | 31 (9.9) | |
| 4 | 25 (12.1) | 10 (9.4) | 35 (11.2) | |
| 5 (Least) | 32 (15.5) | 12 (11.3) | 44 (14.1) | |
| Charlson Comorbidity Score*‡ | 3.8 (2.9,4.7) | 6.5 (5.1,7.9) | 4.7 (4.0,5.5) | 0.001 |
| Hypertensive | 33 (15.9) | 31 (29.2) | 64 (20.4) | 0.006 |
| Pre-existing Respiratory Disease | 28 (13.5) | 24 (22.6) | 52 (16.6) | 0.040 |
| Diabetes Mellitus | 26 (12.6) | 16 (15.1) | 42 (13.4) | 0.534 |
| Heart Failure | 11 (5.3) | 8 (7.5) | 19 (6.1) | 0.434 |
| Obesity (BMI >30) | 56 (27.1) | 35 (33.0) | 91 (29.1) | 0.271 |
| Chronic Kidney Disease | 8 (3.9) | 11 (10.4) | 19 (6.1) | 0.022 |
| ASA Classification | 0.073 | |||
| 1 | 21 (31.3) | 6 (16.7) | 27 (26.2) | |
| 2 | 33 (49.3) | 15 (41.7) | 48 (46.6) | |
| 3 | 9 (13.4) | 12 (33.3) | 21 (20.4) | |
| 4 | 4 (6.0) | 3 (8.3) | 7 (6.8) | |
| COVID-19 Diagnosis | 0 (0.0) | 6 (5.7) | 6 (1.9) | 0.001 |
| Clinical Condition | ||||
| NEWS Score (Admission)*‡ | 2.0 (1.7,2.2) | 1.9 (1.5,2.3) | 1.95 (1.7,2.2) | 0.814 |
| White Cell Count (Admission)*‡ | 11.5 (10.8,12.2) | 12.9 (11.8,14.1) | 12.0 (11.4,12.6) | 0.028 |
| C-Reactive Protein (Admission)*‡ | 58.4 (45.3,71.6) | 83.2 (61.5104.9) | 67.1 (55.6,78.5) | 0.042 |
| Acute Kidney Injury (Admission) | 15 (7.2) | 16 (15.1) | 31 (9.9) | 0.028 |
| Lactate (Admission)**† | 1.5 (1.0–2.0) | 1.5 (1.2–2.2) | 1.5 (1.1–2.0) | 0.122 |
| Acidosis (Admission) | 3 (7.1) | 7 (13.5) | 10 (10.6) | 0.323 |
| NELA Score**† | 4.9 (1.6–33.9) | 5.15 (3.0–14.9) | 4.9 (2.8–19.4) | 0.746 |
*values displayed are mean (95% c.i.) or **median (interquartile range). Percentages and proportions were derived by excluding missing data from the variable. χ2 test for difference, except ‡t-test or †Mann-Whitney U test. BAME, Black Asian and Minority Ethnic; BMI, Body Mass Index; ASA, American Society of Anesthesiologists; NEWS, National Early Warning Score; NELA, National Emergency Laparotomy Audit.
Patients were more unwell at admission in the post-lockdown period (Table 1); they had a significantly higher white cell count and CRP, as measures of inflammation, and significantly higher rates of AKI, as a measure of organ dysfunction through inadequate tissue perfusion. However, there was no difference in admission NEWS score or blood lactate, and there were no differences in NELA score for patients who subsequently underwent laparotomy. There was no significant difference in Hinchey score for patients admitted with diverticulitis (p = 0.162), nor in Glasgow-Imrie score for patients with pancreatitis (p = 0.762).
3.2. Changes in clinical presentation and management
There was a significant increase in presentations which would be considered higher risk and concomitant decrease in low risk admissions (Table 2 ). Patients were significantly more likely to present with GI cancer, GI obstruction, and GI perforation, and less likely to be admitted with non-specific abdominal pain and superficial infections or abscess.
Table 2.
Comparison of clinical diagnosis and management strategy for patients admitted to general surgery during the COVID-19 pandemic, by study period.
| Clinical Diagnosis | Pre-Lockdown (n = 207) | Post-Lockdown (n = 106) | Overall (n = 313) | p-value |
|---|---|---|---|---|
| Appendicitis | 14 (6.8) | 12 (11.3) | 26 (8.3) | 0.167 |
| Biliary Pathology | 32 (15.5) | 22 (20.8) | 54 (17.3) | 0.241 |
| Diverticular Disease | 9 (4.3) | 4 (3.8) | 13 (4.2) | 0.810 |
| Gastrointestinal Bleeding | 6 (2.9) | 0 (0.0) | 6 (1.9) | 0.100 |
| Gastrointestinal Cancer | 7 (3.4) | 9 (8.5) | 16 (5.1) | 0.048 |
| Gastrointestinal Perforation | 11 (5.3) | 12 (11.3) | 23 (7.3) | 0.033 |
| Hernia | 10 (4.8) | 2 (1.9) | 12 (3.8) | 0.350 |
| Inflammatory Bowel Disease/Colitis | 6 (2.9) | 6 (5.7) | 12 (3.8) | 0.231 |
| Ischaemic Bowel | 5 (2.4) | 4 (3.8) | 9 (2.9) | 0.496 |
| Non-Specific Abdominal Pain | 31 (15.0) | 8 (7.5) | 39 (12.5) | 0.041 |
| Non-Surgical Diagnosis | 20 (9.7) | 7 (6.6) | 27 (8.6) | 0.362 |
| Obstruction | 12 (5.8) | 18 (17.0) | 30 (9.6) | 0.001 |
| Other Relevant Surgical Pathology | 13 (6.3) | 4 (3.8) | 17 (5.4) | 0.354 |
| Pancreatitis | 13 (6.3) | 12 (11.3) | 25 (8.0) | 0.120 |
| Peptic Ulcer Disease | 17 (8.2) | 3 (2.8) | 20 (6.4) | 0.065 |
| Superficial Infection/Abscess | 25 (12.1) | 4 (3.8) | 29 (9.3) | 0.016 |
| Trauma | 4 (1.9) | 2 (1.9) | 6 (1.9) | 0.978 |
| Patient Management | ||||
| Imaging | 153 (73.9) | 93 (87.7) | 246 (78.6) | 0.005 |
| CT Scan | 89 (43.0) | 67 (63.2) | 156 (49.8) | 0.001 |
| Intravenous Antibiotic Therapy | 76 (36.7) | 68 (64.2) | 144 (46.0) | <0.001 |
| Duration of Intravenous Antibiotics (Days)**† | 3.0 (1.0–5.0) | 3.0 (2.7–5.0) | 3.0 (2.0–5.0) | 0.136 |
| Non-Interventional Management | 135 (65.2) | 66 (62.3) | 201 (64.2) | 0.723 |
| Endoscopic Intervention | 9 (4.3) | 4 (3.8) | 13 (4.2) | 0.810 |
| Radiological Intervention | 2 (1.0) | 6 (5.7) | 8 (2.6) | 0.020 |
| Operative Intervention | 67 (32.4) | 36 (34.0) | 103 (32.9) | 0.776 |
| Time to Intervention (Days)*‡ | 1.89 (1.22,2.57) | 1.73 (1.21,2.24) | 1.83 (1.37,2.30) | 0.693 |
| Operative Severity | 0.041 | |||
| Minor | 17 (25.4) | 4 (11.1) | 21 (20.4) | |
| Moderate | 35 (52.2) | 16 (44.4) | 51 (49.5) | |
| Major/Complex Major | 15 (22.4) | 16 (44.4) | 31 (30.1) | |
| Approach for Intra-peritoneal Operations | 0.023 | |||
| Laparoscopic | 25 (64.1) | 12 (40.0) | 37 (53.6) | |
| Open | 14 (35.9) | 18 (60.0) | 32 (46.4) |
*values displayed are mean (95% c.i.) or **median (interquartile range). Percentages and proportions were derived by excluding missing data from the variable. χ2 test for difference, except ‡t-test or †Mann-Whitney U test. CT, computed tomography.
In the group admitted following lockdown, a significantly higher proportion of patients were imaged following admission, from 43% to 63.2% (p = 0.001). Management strategies observed in the study group included radiological intervention in the form of percutaneous drainage being increasingly utilised, laparoscopic surgery was undertaken significantly less frequently than open surgery, and significantly less minor procedures were undertaken. On sub-analysis of patients who underwent laparotomy (15 in historical group and 16 in study group), there were no significant differences in patient demographics, aetiology, or baseline severity.
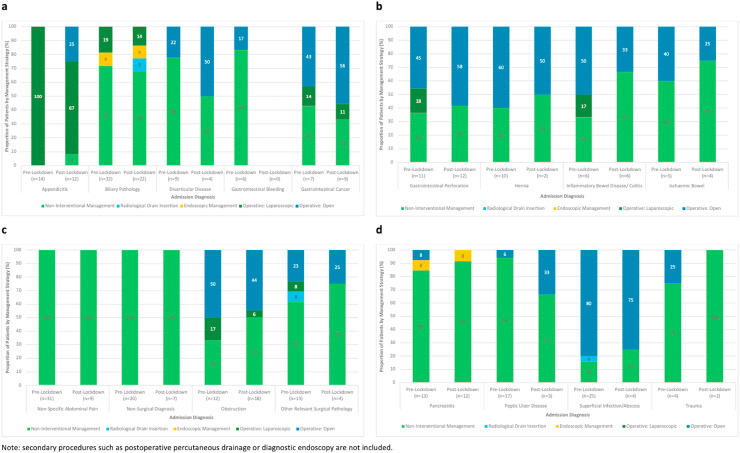
There were changes in the management approach to individual presenting conditions between the study groups (Fig. 2 ), however no statistically significant differences were found.
Fig. 2.
a–d: Primary management strategy for patients admitted to general surgery as an emergency, by surgical diagnosis and period of admission.
3.3. Clinical outcomes
Patients admitted post-lockdown had a significantly longer hospital stay (Table 3 ), and had higher rates of Clavien-Dindo Grade ≥3 complications (p = 0.001), even when mortality was excluded from complications (p = 0.025). All-cause 30-day mortality rates were significantly higher post-lockdown (8.5% vs. 2.9% prior, p = 0.028), but no differences was observed in operative 30-day mortality (1 (6.7%) vs. 2 (12.5%), p = 0.999). Of the 6 patients who were diagnosed with COVID-19 after admission, 2 had no surgery, 2 had a sub-total colectomy for bowel obstruction, 1 had a right hemi-colectomy for cancer, and 1 had a laparoscopic appendicectomy; all recovered and were discharged home without significant adverse outcome.
Table 3.
Comparison of clinical outcomes for patients admitted to general surgery during the COVID-19 pandemic, by study period.
| Outcome Measure | Pre-Lockdown (n = 207) | Post-Lockdown (n = 106) | Overall (n = 313) | p-value |
|---|---|---|---|---|
| Hospital Length of Stay*‡ | 4.3 (3.2,5.4) | 5.5 (4.4,6.6) | 4.7 (3.9,5.5) | <0.001 |
| Critical Care Admission | 12 (5.8) | 8 (7.5) | 20 (6.4) | 0.549 |
| Critical Care Length of Stay**† | 2.0 (1.0–3.0) | 2.5 (1.5–4.0) | 2.0 (1.0–3.0) | 0.545 |
| Unplanned Readmission to Hospital Within 30 days of Discharge | 9 (4.3) | 6 (5.7) | 15 (4.8) | 0.607 |
| Complications | ||||
| Clavien-Dindo Complication: ≥Grade III | 13 (6.3) | 19 (17.9) | 32 (10.2) | 0.001 |
| Clavien-Dindo Complication: ≥Grade III (excluding mortality) | 7 (3.4) | 10 (9.4) | 17 (5.4) | 0.025 |
| Mortality | ||||
| 30-day Mortality (Overall) | 6 (2.9) | 9 (8.5) | 15 (4.8) | 0.028 |
| 30-day Mortality (Laparotomy only) | 1 (6.3) | 2 (13.3) | 3 (10.3) | 0.999 |
*values displayed are mean (95% c.i.) or **median (interquartile range). Percentages and proportions were derived by excluding missing data from the variable. χ2 test or Fisher's exact test for difference, except ‡t-test or †Mann-Whitney U test.
On multivariate logistic regression analysis (Table 4 ), significant predictors of 30-day mortality at admission were increasing number of co-morbidities, NEWS score, NELA score, blood lactate and the presence of AKI. Presentations with gastrointestinal perforation and ischaemic bowel were associated with significantly higher risk of 30-day mortality.
Table 4.
Multivariate logistic regression model of the significant factors associated with 30-day mortality in emergency general surgical admissions.
| Unadjusted |
Adjusted |
|||
|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Patient Characteristics | ||||
| Admission Period | ||||
| Pre-Lockdown | 1.00 | |||
| Post-Lockdown | 3.11 (1.08,9.00) | 0.036 | 1.20 (0.22,6.56) | 0.830 |
| Age | 1.07 (1.03,1.11) | 0.001 | 1.05 (0.98,1.12) | 0.206 |
| Gender | ||||
| Male | 1.00 | |||
| Female | 1.75 (0.55,5.64) | 0.346 | ||
| Ethnicity | ||||
| White | 1.00 | |||
| BAME | 0.00 (0.00,0.00) | 0.999 | ||
| Deprivation Quintile | ||||
| 1 (Most) | 1.00 | |||
| 2 | 0.23 (0.03,1.80) | 0.160 | ||
| 3 | 0.44 (0.06,3.60) | 0.446 | ||
| 4 | 0.39 (0.05,3.16) | 0.379 | ||
| 5 (Least) | 0.63 (0.13,3.01) | 0.565 | ||
| Charlson Comorbidity Score | 1.14 (1.07,1.21) | <0.001 | 1.19 (1.07,1.32) | 0.001 |
| Hypertensive | 2.76 (0.94,8.06) | 0.064 | 0.77 (0.11,5.24) | 0.786 |
| Pre-existing Respiratory Disease | 0.76 (0.17,3.49) | 0.727 | ||
| Diabetes Mellitus | 2.49 (0.75,8.21) | 0.135 | 1.73 (0.27,10.9) | 0.562 |
| Heart Failure | 4.41 (1.13,17.2) | 0.033 | 1.57 (0.15,16.2) | 0.707 |
| Obesity (BMI >30) | 0.36 (0.08,1.63) | 0.186 | ||
| Chronic Kidney Disease | 4.41 (1.13,17.2) | 0.033 | 0.24 (0.02,3.05) | 0.269 |
| ASA Classification | ||||
| 1 | 1.00 | |||
| 2 | 2.07 (0.37,11.6) | 0.408 | ||
| 3 | 13.8 (3.41,56.1) | <0.001 | 1.84 (0.09,37.5) | 0.693 |
| 4 | 16.6 (2.53,108) | 0.003 | 1.79 (0.43,2.48) | 0.464 |
| COVID-19 Diagnosis | 0.00 (0.00,0.00) | 0.999 | ||
| Clinical Condition | ||||
| NEWS Score (Admission) | 1.64 (1.32,2.05) | <0.001 | 1.80 (1.25,2.58) | 0.001 |
| White Cell Count (Admission) | 1.17 (1.08,1.28) | <0.001 | 0.99 (0.88,1.12) | 0.888 |
| C-Reactive Protein (Admission) | 1.01 (1.00,1.01) | <0.001 | 1.00 (1.00,1.01) | 0.171 |
| Acute Kidney Injury (Admission) | 9.99 (3.34,29.9) | <0.001 | 5.75 (1.25,26.44) | 0.025 |
| Lactate (Admission) | 1.85 (1.42,2.43) | <0.001 | 1.49 (1.07,2.08) | 0.017 |
| Acidosis (Admission) | 17.7 (4.36,71.8) | <0.001 | 1.77 (0.16,19.9) | 0.643 |
| NELA Score | 1.04 (1.00,1.09) | 0.067 | 1.03 (1.00,1.05) | 0.042 |
| Clinical Diagnosis | ||||
| Appendicitis | 0.00 (0.00,0.00) | 0.996 | ||
| Biliary Pathology | 0.73 (0.16,3.32) | 0.682 | ||
| Diverticular Disease | 1.70 (0.21,14.0) | 0.621 | ||
| Gastrointestinal Bleeding | 0.00 (0.00,0.00) | 0.999 | ||
| Gastrointestinal Cancer | 8.67 (2.41,31.2) | 0.001 | 7.04 (0.54,91.5) | 0.136 |
| Gastrointestinal Perforation | 21.6 (6.90,67.4) | <0.001 | 13.8 (2.75,69.7) | 0.001 |
| Hernia | 0.00 (0.00,0.00) | 0.997 | ||
| Inflammatory Bowel Disease/Colitis | 0.00 (0.00,0.00) | 0.998 | ||
| Obstruction | 0.66 (0.08,5.22) | 0.696 | ||
| Ischaemic Bowel | 12.2 (2.71,54.6) | 0.001 | 13.8 (1.27,150) | 0.031 |
| Non-Specific Abdominal Pain | 0.00 (0.00,0.00) | 0.998 | ||
| Non-Surgical Diagnosis | 1.68 (0.36,7.87) | 0.510 | ||
| Other Relevant Surgical Pathology | 0.00 (0.00,0.00) | 0.998 | ||
| Pancreatitis | 0.82 (0.10,6.47) | 0.847 | ||
| Peptic Ulcer Disease | 1.05 (0.13,8.41) | 0.964 | ||
| Superficial Infection/Abscess | 0.00 (0.00,0.00) | 0.997 | ||
| Trauma | 0.00 (0.00,0.00) | 0.997 | ||
| Patient Management | ||||
| Imaging | 0.00 (0.00,0.00) | 0.997 | ||
| Endoscopic Intervention | 1.70 (0.21,14.0) | 0.621 | ||
| Radiological Intervention | 2.97 (0.34,25.8) | 0.324 | ||
| Operative Intervention | 0.73 (0.23,2.35) | 0.599 | ||
| Operative Severity | ||||
| Minor | 1.00 | |||
| Moderate | 0.00 (0.00,0.00) | 0.997 | ||
| Major/Complex Major | 1.95 (0.520,7.36) | 0.321 | ||
| Operative Approach | ||||
| Laparoscopic | 1.00 | |||
| Open | 2.00 (0.53,7.51) | 0.304 | ||
OR = Odds ratio. 95% CI = 95% Confidence Interval. BAME, Black Asian and Minority Ethnic; BMI, Body Mass Index; ASA, American Society of Anesthesiologists; NEWS, National Early Warning Score; NELA, National Emergency Laparotomy Audit.
4. Discussion
To our knowledge, this study is the first to describe the impact of ‘lockdown’ on emergency general surgical admissions in the UK during the COVID-19 pandemic. We note a significant reduction in surgical admissions following lockdown, which reflects national and international findings [9,14,[26], [27], [28]], and the reasons for this are likely multifactorial. One reason for the reduction, may be the ‘gatekeeper’ effect, where the surgical team has managed patients without admission. The American and UK Surgical Colleges advised staff to minimise unnecessary admissions and manage conditions conservatively where possible, such as mild appendicitis or cholecystitis [6,29]. However, the ‘gatekeeper’ effect is likely to be minimal in this study as there were no significant differences in management of surgical patients before or after lockdown, and our findings are replicated in different surgical specialities and in different healthcare systems [14,27,28,30]. Any reported effect may also be mitigated by possible healthcare avoidance during the months preceding lockdown.
Patients admitted following lockdown were older, frailer and more acutely unwell. In the UK, patients who have high risk co-morbidities were advised to ‘shield’ and avoid all face-to-face contact [31]. We identified a higher proportion of patients admitted with multiple co-morbidities, and with higher risk medical co-morbidities – hypertension, pre-existing respiratory disease, and chronic kidney disease – which are predictive of poorer outcomes if diagnosed with COVID-19 [[32], [33], [34]]. Patients had higher biochemical markers of inflammation (WCC and CRP) and organ dysfunction (AKI) at admission. Whilst specific medical comorbidities did not predict 30-day mortality on logistic regression, evidence of organ dysfunction in this surgical cohort were independent predictors of mortality (increasing NEWS score, lactate, and the presence of acute kidney injury).
Changes in clinical presentations to surgical specialties have been noted in the literature [14,27], with evidence of a rise in some conditions deemed to be non-deferrable (such as bowel obstruction, incarcerated hernia or gross haematuria), and a reduction in less severe conditions, such as simple urinary tract infection. In this study, there was a significant reduction in non-specific abdominal pain and non-surgical admissions. The most frequently postulated reasons for this is hospital avoidance or reduced access to primary or secondary care [35,36]. A proportional increase in the use of CT imaging may have offered a more prompt diagnosis for clinicians and facilitated fewer unnecessary admissions. This increased use of CT is compatible with a recent Irish survey of surgeons, with 74% of responding surgeons using CT to diagnose appendicitis during the pandemic [37]. Worryingly, we report a significantly increased incidence of perforation and gastrointestinal cancer causing obstruction following lockdown by both raw number and also proportionately between cohorts, which may reflect delays in presentation, difficulties in accessing general practice for referral, or changes made to access cancer pathways during the pandemic [38].
There were significantly fewer minor procedures undertaken, such as abscess drainage, which parallels the reduction in low risk presentations. There were consequently a higher proportion of patients who underwent higher risk operations in the post-advice period. Despite recommendations from the American and UK Surgical Colleges [6,29] to move to open operations and reduce operative intervention, following lockdown we report no significant change in our operative practice, patient management or patient outcomes. There was a statistically higher rate of open operations in the post-advice period, which was largely driven by laparotomy and a small number of open appendicectomies. Interestingly, in the laparotomy population, there were no differences in any patient-related factors or outcomes between the study periods. In agreement with international findings [14,27], it is considered that this reflects a constancy of non-deferrable intra-abdominal emergencies that will appropriately attend irrespective of the prevailing lockdown. Unfortunately, there were significantly higher rates of major complications, even after excluding mortality. This is may be attributable to some extent to the higher proportion of patients presenting with perforations, cancer, and obstruction, and possibly due to more open surgery. Of the 4 reported patients who had emergency surgery with subsequent COVID-19 diagnosis, we found no deleterious effects of the virus on their recovery.
With the likelihood of further waves during the pandemic, it is critical to consider factors which influence mortality in this period. Older patients who have multiple co-morbidities and are admitted during lockdown are at higher risk of 30-day mortality. It is vital to be conscious of patients’ NEWS score, blood results and act on these at an early stage, such as ensuring AKI is prevented and promptly identified and treated where present. Early resuscitation, investigation and intervention as per guidelines [[39], [40], [41]] in these patients are essential, particularly if there are concerns of ischaemic bowel or perforations as these are significant predictors of mortality for emergency general surgical patients. It is important that patients attend promptly and receive the surgical care that they require, as delaying presentations to medical services may compromise their outcomes [10,14,27].
4.1. Strengths and limitations
This is the first UK study to consider predictive factors which may influence patient outcomes for surgical patients during the COVID-19 pandemic. We have undertaken prospective data collection and analysis of surgical patients during lockdown using a historical group as a comparator. This study has design limitations as a single centre service evaluation, and subsequently may not be representative of or generalisable to the wider UK population. Of particular note there were very few patients from black or minority ethnic communities in these cohorts. Furthermore, changes in rates of obstruction or GI cancer may reflect variation around the mean rather than genuine changes in presentation and larger multicentre studies may be able to evaluate this further.
5. Conclusion
This study has shown that a “lockdown” effect has had a wide-reaching impact on patients, with significantly fewer surgical admissions and surgical patients being admitted more acutely unwell. There has been a higher rate of complications and overall mortality for surgical patients during lockdown, but 30-day operative mortality has not significantly changed, which supports the use of accepted surgical techniques as employed in our practice. Early diagnosis, resuscitation and intervention with surgery is critical during the COVID-19 pandemic, especially for patients with GI obstruction or perforation, and patients should thus be strongly advised to seek early medical attention for gastrointestinal and abdominal symptoms during subsequent waves and “lockdowns” in this pandemic.
Ethical approval
Research and Development department at North Tees and Hartlepool NHS Foundation Trust. Registry not required as registered as service evaluation audit.
Sources of funding
Nil.
Trial registry number
-
1.
Name of the registry: Chinese Clinical Trial Registry (ChiCTR)
-
2.
Unique Identifying number or registration ID: ChiCTR2000034588
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked): http://www.chictr.org.cn/showprojen.aspx?proj=56245
Guarantor
Ross C McLean.
Kevin Jon Etherson.
Data statement
Patient data was collected following institutional approval, granted by the North Tees and Hartlepool NHS Foundation Trust in the North of England. We do not have permission to share this data.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Article category
Original article, observational study.
Originality
This work is not based on work submitted previously for publication or to a scientific meeting.
Financial Support
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
CRediT authorship contribution statement
Ross C. McLean: Conceptualization, Methodology, Validation, Formal analysis, Data curation, Writing - original draft, Supervision, Project administration. John Young: Methodology, Validation, Formal analysis, Data curation, Writing - original draft. Aya Musbahi: Conceptualization, Methodology, Validation, Writing - original draft, Supervision. Jing Xian Lee: Methodology, Validation, Formal analysis, Data curation, Writing - original draft. Hena Hidayat: Methodology, Validation, Formal analysis, Data curation, Writing - original draft. Nagi Abdalla: Validation, Formal analysis, Data curation, Writing - original draft. Sabyasachi Chowdhury: Validation, Formal analysis, Data curation, Writing - original draft. Elizabeth A. Baker: Conceptualization, Methodology, Writing - original draft. Kevin Jon Etherson: Conceptualization, Methodology, Validation, Writing - original draft, Supervision.
Declaration of competing interest
Nil.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijsu.2020.09.011.
Appendix A. Supplementary data
The following is/are the supplementary data to this article:
References
- 1.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., et al. Early transmission dynamics in wuhan, China, of novel coronavirus–infected pneumonia. N. Engl. J. Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., et al. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.U.G. Department of Health and Social Care . 2020. CMO Confirms Cases of Coronavirus in England.https://www.gov.uk/government/news/cmo-confirms-cases-of-coronavirus-in-england [Google Scholar]
- 4.U.G. Department of Health and Social Care . UK Gov; 2020. Coronavirus (COVID-19) in the UK.https://coronavirus.data.gov.uk (accessed June 3, 2020) [Google Scholar]
- 5.U.G. Prime . 2020. Minister's Office, 10 Downing Street and the Rt Hon Boris Johnson MP, PM Statement on Coronavirus: 16 March 2020.https://www.gov.uk/government/speeches/pm-statement-on-coronavirus-16-march-2020 [Google Scholar]
- 6.Intercollegiate Surgical Colleges . 2020. Updated General Surgery Guidance on COVID-19. [Google Scholar]
- 7.S. of A.G. and E. Surgeons . 2020. UPDATE TO SAGES RECOMMENDATIONS REGARDING SURGICAL RESPONSE TO COVID-19 CRISIS.https://www.sages.org/update-to-sages-recommendations-regarding-surgical-response-to-covid-19-crisis/ (accessed March 21, 2020) [Google Scholar]
- 8.Stevens S., Pritchard A. NHS Engl. NHS Improv; 2020. IMPORTANT AND URGENT – NEXT STEPS ON NHS RESPONSE TO COVID-19.https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/urgent-next-steps-on-nhs-response-to-covid-19-letter-simon-stevens.pdf [Google Scholar]
- 9.NHS England, A&E Attendances & Emergency Admission statistics . 2020. NHS and Independent Sector Organisations in England.https://www.england.nhs.uk/statistics/statistical-work-areas/ae-waiting-times-and-activity/ae-attendances-and-emergency-admissions-2020-21/ [Google Scholar]
- 10.Lazzerini M., Barbi E., Apicella A., Marchetti F., Cardinale F., Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc. Heal. 2020;4:e10–e11. doi: 10.1016/S2352-4642(20)30108-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Molica M., Mazzone C., Cordone I., Pasquale A., Niscola P., de Fabritiis P. SARS‐CoV‐2 infection anxieties and general population restrictions delay diagnosis and treatment of acute haematological malignancies. Br. J. Haematol. 2020:16785. doi: 10.1111/bjh.16785. bjh. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tam C.-C.F., Cheung K.-S., Lam S., Wong A., Yung A., Sze M., et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment–elevation myocardial infarction care in Hong Kong, China, circ. Cardiovasc. Qual. Outcomes. 2020;13 doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mantica G., Riccardi N., Terrone C., Gratarola A. Non-COVID-19 visits to emergency departments during the pandemic: the impact of fear. Publ. Health. 2020;183:40–41. doi: 10.1016/j.puhe.2020.04.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cano-Valderrama O., Morales X., Ferrigni C.J., Martín-Antona E., Turrado V., García A., et al. Reduction in emergency surgery activity during COVID-19 pandemic in three Spanish hospitals. Br. J. Surg. 2020 doi: 10.1002/bjs.11667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Agha R., Abdall-Razak A., Crossley E., Dowlut N., Iosifidis C., Mathew G., et al. STROCSS 2019 Guideline: strengthening the reporting of cohort studies in surgery. Int. J. Surg. 2019;72:156–165. doi: 10.1016/j.ijsu.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 16.Ministry of Housing Communities & local government. English indices of deprivation. 2019. http://imd-by-postcode.opendatacommunities.org/imd/2019 Postcode Lookup. (accessed 16 February 2020)
- 17.Quan H., Li B., Couris C.M., Fushimi K., Graham P., Hider P., et al. Updating and validating the charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am. J. Epidemiol. 2011;173:676–682. doi: 10.1093/aje/kwq433. [DOI] [PubMed] [Google Scholar]
- 18.NHS Digital Summary hospital-level mortality indicator. https://digital.nhs.uk/data-and-information/publications/ci-hub/summary-hospital-level-mortality-indicator-shmi (accessed 16 February 2020)
- 19.Royal College of Physicians (London) National early warning score (NEWS) 2 standardising the assessment of acute-illness severity in the NHS. https://www.rcplondon.ac.uk/projects/outputs/national-early-warning-score-news-2 (accessed 16 March 2020)
- 20.Blamey S.L., Imrie C.W., O'Neill J., Gilmour W.H., Carter D.C. Prognostic factors in acute pancreatitis. Gut. 1984;25:1340–1346. doi: 10.1136/gut.25.12.1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Royal College of Anaesthetists National emergency laparotomy audit (NELA) risk prediction tool. https://data.nela.org.uk (accessed 20 May 2020)
- 22.Hinchey E.J., Schaal P.G., Richard G.K. Treatment of perforated diverticular disease of the colon. Adv. Surg. 1978;12:85–109. [PubMed] [Google Scholar]
- 23.National Institute for Health and Clinical Excellence (NICE) Routine preoperative tests for elective surgery: recommendations for specific surgery grades (minor, intermediate, and major or complex) and ASA grades. NICE. 2016;45 https://www.nice.org.uk/guidance/ng45/chapter/recommendations#recommendations-for-specific-surgery-grades-minor-intermediate-and-major-or-complex-and-asa (accessed 16 March 2020) [Google Scholar]
- 24.NELA Project Team NELA HES algorithm – OPCS codes. https://www.nela.org.uk/download.php/?fn=NELA%20HES%20Algorithm%20OPCS%20(Oct%202017).pdf&mime=application (accessed 16 March 2020)
- 25.Dindo D., Demartines N., Clavien P.-A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. http://www.ncbi.nlm.nih.gov/pubmed/15273542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thornton J. Covid-19: A&E visits in England fall by 25% in week after lockdown. BMJ. 2020 doi: 10.1136/bmj.m1401. [DOI] [PubMed] [Google Scholar]
- 27.Novara G., Bartoletti R., Crestani A., De Nunzio C., Durante J., Gregori A., et al. Impact of COVID-19 pandemic on the urologic practice in the emergency departments in Italy. BJU Int. 2020 doi: 10.1111/bju.15107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Porreca A., Colicchia M., D'Agostino D., Amenta M., Corsaro A., Zaramella S., et al. Urology in the time of coronavirus: reduced access to urgent and emergent urological care during the coronavirus disease 2019 outbreak in Italy. Urol. Int. 2020:1–6. doi: 10.1159/000508512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.American College of Surgeons COVID-19 guidelines for triage of emergency general surgery patients. https://www.facs.org/covid-19/clinical-guidance/elective-case/emergency-surgery (accessed 20 March 2020)
- 30.Maniscalco P., Poggiali E., Quattrini F., Ciatti C., Magnacavallo A., Vercelli A., et al. Proximal femur fractures in COVID-19 emergency: the experience of two Orthopedics and Traumatology Departments in the first eight weeks of the Italian epidemic. Acta Biomed. 2020;91:89–96. doi: 10.23750/abm.v91i2.9636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.NHS Digital Coronavirus (COVID-19): shielded patients list. https://digital.nhs.uk/coronavirus/shielded-patient-list (accessed 23 April 2020)
- 32.Chen R., Liang W., Jiang M., Guan W., Zhan C., Wang T., et al. Risk factors of fatal outcome in hospitalized subjects with coronavirus disease 2019 from a nationwide analysis in China. Chest. 2020 doi: 10.1016/j.chest.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Long L., Zeng X., Zhang X., Xiao W., Guo E., Zhan W., et al. Short-term outcomes of coronavirus disease 2019 and risk factors for progression. Eur. Respir. J. 2020:2000990. doi: 10.1183/13993003.00990-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.NHS Digital Appointments in general practice. https://digital.nhs.uk/data-and-information/publications/statistical/appointments-in-general-practice (accessed 27 May 2020)
- 36.Charlesworth A., Watt T., Thorlby R. Heal. Found.; 2020. Early Insight into the Impacts of COVID-19 on Care for People with Long-Term Conditions. [Google Scholar]
- 37.Kelly M.E., Murphy E., Bolger J.C., Cahill R.A. Covid‐19 and the treatment of acute appendicitis in Ireland‐ A new era or short‐term pivot? Colorectal Dis. 2020:15141. doi: 10.1111/codi.15141. codi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.NHS England Clinical guide for the management of patients requiring endoscopy during the coronavirus pandemic. https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/04/C0076-Specialty-guide-for-endoscopy-and-coronavirus-v1-02April.pdf (accessed 16 May 2020)
- 39.Dellinger R.P., Levy M.M., Carlet J.M., Bion J., Parker M.M., Jaeschke R., et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock. Crit. Care Med. 2008;36:296–327. doi: 10.1097/01.CCM.0000298158.12101.41. 2008. [DOI] [PubMed] [Google Scholar]
- 40.Royal College of Surgeons of England . Royal College of Surgeons of England; London: 2011. Emergency Surgery: Standards for Unscheduled Surgical Care. [Google Scholar]
- 41.NELA Project Team Fifth patient report of the national emergency laparotomy audit ( NELA ) https://www.nela.org.uk/reports (accessed 16 May 2020)
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.