To the Editor:
An early and persistent trend of the coronavirus disease 2019 (COVID-19) pandemic has been the large number of deaths occurring among older adults and those living in long-term care (LTC) homes.1 Residents of LTC homes are at a disproportionately high risk of contracting severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) due to their congregant living environments, greater likelihood of being exposed to asymptomatic and pre-symptomatic care providers, and difficulty in effectively implementing infection prevention and control practices.2 , 3 Most LTC home residents are also older adults, for whom advanced age represents a strong risk factor for COVID-19 morbidity and mortality due to the higher prevalence of immunosenescence and chronic illnesses.4 Although the proportion of deaths occurring in LTC homes at an international level has been explored, population-specific mortality rates for LTC home residents and their comparison with rates for community-dwelling older,6 and younger persons have neither been calculated nor analyzed.5
Using publicly reported data on COVID-19 deaths for 12 Organization for Economic Co-operation and Development (OECD) member-countries (Belgium, Canada, Denmark, France, Germany, Ireland, Italy, Netherlands, Spain, Sweden, United Kingdom, and the United States), we calculated and compared the population-specific mortality rates and ratios for LTC home residents and community-dwelling older (age ≥65 years) and younger (age <65 years) persons. COVID-19 deaths data were collected directly from publicly available national health and epidemiological reports and were current as of July 24, 2020 (see Appendix 1 for methodology and data sources). COVID-19 deaths included both those reported as confirmed and probable, and those that occurred in LTC home and acute hospital settings.
We report a total of 361,161 COVID-19 deaths for the 12 countries, which accounted for 90% of deaths in all 37 OECD countries and 56% of all global deaths.7 Within the 12 countries, LTC home residents, community-dwelling older persons, and younger persons accounted for an average of 47.3%, 44.7%, and 8.0% of COVID-19 deaths and an average of 0.9%, 18.2%, and 80.9% of national populations, respectively.
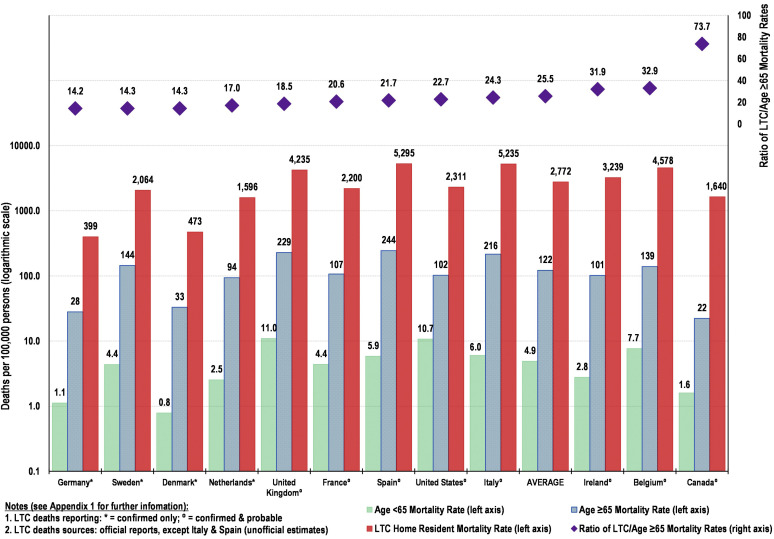
We calculate a 12-country average COVID-19 mortality rate of 2772 per 100,000 LTC home residents (range, 399 for Germany to 5295 for Spain) compared with 122 per 100,000 community-dwelling older persons (range, 22 for Canada to 244 for Spain), representing an average 24.2-fold higher rate of death (range, 14.2 for Germany to 73.7 for Canada). Even greater differences were observed when compared with COVID-19 mortality rates for community-dwelling younger persons, which averaged 4.9 per 100,000, representing a 644-fold higher rate of COVID-19 deaths among LTC home residents (range of 215 for the United States to 1165 for Ireland). (Figure 1 ).
Fig. 1.
COVID-19 mortality rates and ratios for LTC home residents and community-dwelling persons. Estimates for 12 OECD countries; deaths per 1000 of specific population.
Here we confirm a very high concentration of mortality of LTC home residents and report substantial variation among 12 OECD countries. Our results suggest that the level of community transmission, as reflected in the mortality rate for community-dwelling persons, and the level of policy response related to infection prevention and control practices in LTC homes and at the broader community level were important factors driving LTC home resident mortality rates.5 Reporting differences in our multinational data sources may limit some between country comparability, this includes: 1) four countries (Denmark, Germany, Netherlands and Sweden) reporting only confirmed LTC resident deaths, while the remaining eight report confirmed and probable deaths; 2) in the absence of official national estimates, we have used partial official or non-official figures to provide reasonable estimates of all LTC home resident deaths for Italy and Spain.
Countries, such as Denmark and Germany, that maintained relatively low levels of community transmission and acted early and aggressively to prevent the introduction and spread of COVID-19 into their LTC homes had the lowest LTC home resident mortality rates.8 These policy actions included the early restriction of nonessential visitors, enacting universal masking policies, improving LTC staffing levels, preventing care providers from working across multiple sites, implementing enhanced LTC infection control training and audit procedures, and widespread testing and isolation protocols for infected residents and asymptomatic contacts.1 , 9 , 10
In contrast, countries such as Spain and the United Kingdom, that had relatively high levels of community transmission and less robust LTC home–related policy responses, had the highest LTC home resident mortality rates. Other countries had mixed responses with uneven results. For instance, Canada promoted relatively forceful measures that were effective in limiting community transmission, but its LTC home–related responses were uneven and less robust for a system already characterized as being poorly staffed and funded at its baseline.11 This may explain why Canada particularly stands out, with the highest mortality ratio comparing LTC home residents with community-dwelling older persons (73.7 vs. the OECD 12-country average of 25.5), and why Canada's LTC home resident deaths accounted for such a high percentage of its overall deaths (78.4% vs. the OECD 12-country average of 47.3%).
As some countries are still grappling with their first waves of COVID-19 infections and others are starting to combat their second waves, understanding the factors that led to substantial mortality rates for LTC home residents in certain jurisdictions could help allow for the implementation of key policies and practices that could prevent introduction, transmission, and death from COVID-19 across all jurisdictions.
Appendix 1. Data Sources and Methodology
Population-specific mortality rates for the three population groups (community-dwelling younger persons age <65, community-dwelling older persons age ≥65 years and LTC residents) were calculated by dividing the COVID -19 deaths for each group (numerator) by their respective population (denominator).
Table 1 shows the calculated numerators and denominators for the three population groups for all 12 countries, which are the basis for the mortality rates presented in Figure 1.
 |
Population Estimates
-
•
Population estimates for total population and for groups age <65 and age ≥65 years were for 2020 and for the 10 European countries sourced from the European Centre for Disease Prevention and Control (ECDC): https://www.ecdc.europa.eu/sites/default/files/documents/covid-19-long-term-care-facilities-surveillance-guidance.pdf (Accessed July 24, 2020) and from the OECD for Canada and the USA https://stats.oecd.org/Index.aspx?DataSetCode=POPPROJ (Accessed July 24, 2020)
-
•
Population estimates for LTC residents were generally proxied by LTC home beds and for the 10 European countries sourced from the WHO (Europe): https://gateway.euro.who.int/en/indicators/hfa_491-5101-number-of-nursing-and-elderly-home-beds/visualizations/#id=19556&tab=table (accessed July 24, 2020); from the CDC for the USA https://www.cdc.gov/nchs/data/series/sr_03/sr03_43-508.pdf to include “Nursing Homes” and “Residential Care Community” beds (accessed July 24, 2020) and from Statistics Canada for Canada https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/dt-td/Rp-eng.cfm?TABID=2&Lang=E&APATH=3&DETAIL=0&DIM=0&FL=A&FREE=0&GC=0&GID=1234492&GK=0&GRP=1&PID=109537&PRID=10&PTYPE=109445&S=0&SHOWALL=0&SUB= 0&Temporal=2016&THEME=116&VID=0&VNAMEE=&VNAMEF=&D1=0&D2=0&D3=0&D4=0&D5=0&D6=0 to include residents in “Nursing homes”, “Residences for senior citizens” and mixes of both (accessed July 24, 2020).
COVID-19 Deaths
-
•COVID-19 deaths for the three population groups were sourced from publicly available national health and epidemiological reports:
-
○Deaths for community-dwelling persons age <65 were sourced directly from the corresponding epidemiological reports.
-
○Deaths for community-dwelling persons age ≥65 were generally calculated by subtracting reported LTC deaths (see below) from all age ≥65 deaths, sourced directly from the corresponding epidemiological reports.
-
○Deaths for LTC home residents were sourced directly as set out below.
-
○
-
•The following data-related notes and caveats apply:
-
○Choice of countries
-
▪Our objective is to provide a summary snapshot of mortality rates and ratios for LTC home residents in a manageable number of reasonably comparable countries that have been significantly affected by COVID-19. To maximize comparability, we applied the following criteria to select the 12 study countries: 1) country should be an OECD member-state; 2) country should report periodic and official LTC home resident deaths (alternatively, there should be other periodic sources that provide reasonable estimates); 3) country should have significant total national COVID-19 deaths, adjusted for population.
-
▪
-
○Definition and coverage of LTCs
-
▪There is significant variability in the definition and coverage of LTCs in the 12 study countries. We have endeavored to take these differences into account, including by focusing on mortality rates and carefully matching the numerator (LTC home resident deaths) with the denominator (LTC home residents). However, as noted above, because of inconsistency in the reporting of number of LTC home residents in the ten European countries, we have opted to use LTC home beds as a proxy for LTC home residents.
-
▪
-
○Location of LTC home resident deaths
-
▪Our objective is to include all LTC home resident deaths in our study. This includes deaths that occurred in LTC homes (“in-situ”) and in (acute) hospital and other/unknown settings (“hospital”). In this context, it is noteworthy that:
-
▪10 countries (Belgium, Canada, Denmark, France, Germany, Ireland, Netherlands, Sweden, UK and US) include hospital and in-situ LTC home resident deaths in official total national deaths. Belgium, France and UK report in-situ and hospital deaths separately, while Canada, Denmark, Germany, Ireland, Netherlands, Sweden and US do not separately report the location of death.
-
▪2 countries (Italy and Spain) include only hospital LTC home resident deaths in official national deaths totals. Further, such deaths are not reported separately from deaths of community-dwelling persons. For comparability with other countries, we 1) estimate additional “in-situ” deaths; and 2) estimate what proportion of official national deaths totals are indeed hospital LTC home resident deaths. Consequently, we adjust the official total national deaths to take into account our estimated additional “in situ” deaths. For specifics, please refer to Italy and Spain description below.
-
▪
-
○Confirmed only or confirmed and probable deaths
-
▪Countries have generally applied two broad approaches for accounting for deaths generally and in LTCs in particular: 1) a narrower approach (only confirmed deaths) or 2) a broader approach (confirmed and probable deaths). In our study:
-
•6 countries use the broader approach (Belgium, Canada, France, Ireland, UK and US);
-
•4 countries use the narrower approach (Denmark, Germany, Netherlands and Sweden);
-
•For the two countries (Italy and Spain) that include only hospital LTC home resident deaths in official national deaths totals, we have imposed the broader approach (see below).
-
•
-
▪
-
○Remaining data limitations
-
▪By choosing a limited number of reasonably comparable countries with high quality data collected over a two-day period (July 23 to 24) we have attempted to maximize the comparability of the data to provide a solid basis for our comparative analysis. Nevertheless, data limitations remain, including as described above. Of particular note are the following:
-
•We note that the four countries that employ the narrower approach for accounting for deaths (Denmark, Germany, Netherlands and Sweden) have the lowest ratios of LTC/≥65 age mortality rates in Figure 1. While it is true that Germany and Denmark have relatively low mortality rates across all three population groups, that is not the case for Sweden and Netherlands. This suggests that some part of the lower LTC/≥65 age mortality rates across this group is driven by the narrower approach. This would be the case, for instance, if the proportion of probable deaths, if such deaths were to be accounted, was higher among LTC home residents than for community-dwelling ≥65 age persons. There is evidence that this was the case in the one study country, Belgium, that separately reported confirmed and probably cases: in its July 22 report (see below) it reported that 95% of all hospital deaths (including those of LTC home residents) were “confirmed”, compared to only 26% of deaths in LTC homes being “confirmed”, with the rest (5% and 74% being probable).
-
•In spite of the above-noted issues with LTC home residents data for Italy and Spain, we include them in the study given that these two countries had some of the highest official national deaths in the world, adjusted for population, and for which there were widespread media reports of large numbers of deaths of LTC home residents. We have endeavored to identify and use non-official partial and/or periodic sources that we believe provide reasonable estimates. Further, we carried out sensitivity and other comparative analysis to ensure that the resultant rates and ratios in Italy and Spain are consistent with those of other European countries that also had comparably high official national deaths totals (e.g. Belgium, France, Ireland, UK). Nevertheless, until the national governments of Italy and Spanish provide comprehensive official national deaths totals, these remain our unofficial estimates.
-
•
-
▪
-
○
-
•
Belgium: The COVID-19 – Bulletin Epidémiologique hebdomadaire du 26 juin 2020 by Sciensano reported “Maison de repos” and “Maisons de repos et de soins” (MR/MRS) resident deaths of 4,857 in MR/MRS (78%) and 1,377 in Hospitals and 13 unknown locations (together 22%) as of June 21 (http://covid-19.sciensano.be/sites/default/files/Covid19/COVID-19_Weekly%20report_20200626%20-%20FR_0.pdf (accessed October 6, 2020). The COVID-19 – Bulletin Epidémiologique du 22 Juillet 2020 by Sciensano reports 4,877 LTC residents deaths in MR/MRS http://covid-19.sciensano.be/sites/default/files/Covid19/COVID-19_Daily%20report_20200722%20-%20FR.pdf (Accessed July 23, 2020). Based on the above-noted, most recently-available 78%/22% in-situ/hospital ratio, we estimate 1,398 hospital deaths to July 22, for a total of 6,275 deaths for MR/MRS residents for that date.
-
•
Canada: The “National Institute on Aging (NIA) Long Term Care COVID-19 Tracker reports 6,981 deaths of LTC residents https://ltc-covid19-tracker.ca/ as of July 23 (accessed July 24, 2020)
-
•
Denmark. The Danish “Statens Serum Institut” in the “Overvågning af COVID-19” https://www.ssi.dk/sygdomme-beredskab-og-forskning/sygdomsovervaagning/c/covid19-overvaagning reports 215 deaths of nursing homes residents in Table 7.1 (Accessed July 23, 2020)
-
•
France: The COVID-19 Point épidémiologique hebdomadaire du 23juillet 2020 reports 14,126 deaths of EHPA residents (3,696 (26%) in hospitals and 10,430 (74%) in EHPAs https://www.santepubliquefrance.fr/content/download/269451/2684823 (accessed July 23, 2020).
-
•
Germany: The COVID-19 Daily Situation Report of the Robert Koch Institute 23/07/2020 – Updated Status for Germany” reports 3,606 deaths for residents of s36 IfSG facilities https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/2020-07-23-en.pdf?__blob=publicationFile (Accessed July 23, 2020)
-
•
Ireland: On June 15 the Department of Health’s “Nursing Homes - Summary paper provided to Special Committee on COVID-19 Response” https://assets.gov.ie/77340/b73b66ea-01d8-41da-ba01-4bd9dadd449e.pdf (Accessed July 24) noted that as of June 13 there were 943 deaths for nursing home residents, which at the time accounted for 55.3% of all national deaths (1,705). The national number had increased to 1,763 to July 23 and we estimated the number of additional nursing home deaths over that period to be 32 (55.3% of 58), for a total of 975 deaths for nursing home residents for that date.
-
•
Italy: The Government of Italy has to date not reported figures for RSA resident deaths outside of hospitals. We used three sources to “triangulate” a reasonable estimate for total LTC Resident deaths: 1) On May 5 the Istituto Superiore di Sanità (ISS) in “Survey nazionale sul contagio COVID-19 nelle strutture residenziali e sociosanitarie - REPORT FINALE » https://www.epicentro.iss.it/coronavirus/pdf/sars-cov-2-survey-rsa-rapporto-finale.pdf (accessed July 23, 2020) reported the final results of a survey of RSAs, based on which we project about 11,400 confirmed and symptom-compatible RSA deaths to July 24; 2) the Milan ATS (regional health unit) released the COVID-19 results of their survey of RSAs under their jurisdiction “RSA Flusso Covid 19 REPORT AL 15/07/2020” to July 15 https://www.ats-milano.it/Portale/desktopmodules/dnn_gestionedocumenti/Images/download.png (accessed July 24, 2020), based on which we project about 12,400 RSA deaths nationally 3) on May 19 an online publication interviewed a lawyer that was pursuing class action against RSAs and noted that there had been 12,000 COVID-19-related deaths https://www.ildigitale.it/morti-nelle-rsa-per-covid-in-atto-una-class-action-legale/ (access July 24, 2020). Taking into account these projections we use an estimate of 12,250 deaths for LTC residents. Based on an assumed in-situ/hospital distribution of LTC deaths of 75%/25% (see France and UK average), we estimate that of these total LTC deaths, 3,063 were in hospitals. Such in-hospital deaths are already included in the national totals. However, the LTC in situ deaths are not included and hence we add 9,188 deaths to the Government of Italy total of deaths for July 24 of 35,097 for a revised national total of 44,285.
-
•
Netherlands: The “Epidemiologische situatie COVID-19 in Nederland: Rijksinstituut voor Volksgezondheid en Milieu – RIVM (21 juli 2020)” reports 2,841 deaths of LTC residents “verpleeghuizen” as of July 21 https://www.rivm.nl/sites/default/files/2020-07/COVID-19_WebSite_rapport_wekelijks_20200721_1135.pdf (Accessed July 23, 2020), confirmed https://coronadashboard.rijksoverheid.nl/ (Accessed July 23, 2020)
-
•
Spain: The Government of Spain has to date not reported figures for LTC resident deaths outside of hospitals. The Spanish national broadcaster (RTVE) has compiled the reports of LTC residents deaths submitted to the National Government by the regional health authorities, indicating 19,646 deaths (confirmed and suspected) of LTC residents as of July 24, 2020. https://www.rtve.es/noticias/20200523/radiografia-del-coronavirus-residencias-ancianos-espana/2011609.shtml (accessed July 24, 2020). Based on an assumed in-situ/hospital distribution of LTC deaths of 75%/25% (see France and UK average), we estimate that of these total LTC deaths, 4,912 were in hospitals. Such in-hospital deaths are already included in the national totals. However, the LTC in situ deaths are not included and hence we add 14,735 deaths to the Government of Spain total of deaths for July 24 of 28,432 for a revised national total of 43,167.
-
•
Sweden: the National Board of Health and Welfare “Socialstyrelsen” reports 2,425 deaths of LTC “Särskilt boende” residents aged 70+ as of July 20, 2020 https://www.socialstyrelsen.se/globalassets/1-globalt/covid-19-statistik/statistik-om-covid-19-bland-aldre-efter-boendeform/statistik-covid19-70-ar-och-aldre.xlsx (accessed July 23, 2020), to which we added 132 deaths for those aged 65-69 based on applying the same LTC/community proportion, for a total of 2,557 deaths.
-
•
United Kingdom: The Office of National Statistics (ONS) reported 15,122 deaths in England and Wales “care homes” to July 10 that mentioned COVID-19. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/datasets/weeklyprovisionalfiguresondeathsregistered inenglandandwales (Accessed July 24, 2020). The National Records of Scotland reported 1,950 deaths in “care homes” to July 137 https://www.nrscotland.gov.uk/covid19stats (accessed July 24, 2020). The Northern Ireland Statistics and Research Agency reported 347 in “care homes” to July 17 https://www.nisra.gov.uk/publications/weekly-deaths (accessed July 24, 2020). These three figures sum to a UK total of 17,419 in situ deaths. The ONS reports the distribution of in-situ/hospital deaths of “care home” residents of 24%/76% (see “Number of deaths in care homes notified to the Care Quality Commission, England” at https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/datasets/numberofdeathsincarehomesnotifiedtothecarequalitycommissioneng land (accessed July 24, 2020). Using a 25%/75% distribution to be consistent as France (see above), we estimate 5,806 resident deaths in hospitals, for a total of 23,225 deaths of care home residents.
-
•
United States: The Kaiser Family Foundation (KFF) has compiled the reports of LTC resident deaths published by State, regional and local agencies https://www.kff.org/health-costs/issue-brief/state-data-and-policy-actions-to-address-coronavirus/ (Accessed July 24, 2020) indicating 59,506 deaths of LTC residents in the 41 reporting states as of July 23. That total is equal to 44.0% of total deaths for those 41 reporting States. We applied that ratio to the deaths totals of the 9 States that had not reported (based on CDC data (total deaths as well) https://www.cdc.gov/covid-data-tracker/index.html#cases (Accessed July 24, 2020) and calculated an additional 1,891 deaths. Summing these two estimates, the national total is 61,397 deaths of LTC residents.
References
- 1.Ouslander J.G., Grabowski D.C. COVID-19 in nursing homes: Calming the perfect storm. https://doi.org/10.1111/jgs.16784 [Epub ahead of print]. J Am Geriatr Soc. [DOI] [PubMed]
- 2.McMichael T.M., Currie D.W., Clark S. Epidemiology of Covid-19 in a long-term care facility in King County, Washington. N Engl J Med. 2020;382:2005–2011. doi: 10.1056/NEJMoa2005412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goldberg S.A., Pu C.T., Thompson R.W. Asymptomatic spread of COVID-19 in 97 patients at a skilled nursing facility. J Am Med Dir Assoc. 2020;21:980–981. doi: 10.1016/j.jamda.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.D'Adamo H., Yoshikawa T., Ouslander J.G. Coronavirus disease 2019 in geriatrics and long-term care: The ABCDs of COVID-19. J Am Geriatr Soc. 2020;68:912–917. doi: 10.1111/jgs.16445. [DOI] [PubMed] [Google Scholar]
- 5.Canadian Institute for Health Information Pandemic experience in the long-term care sector: how does Canada compare with other countries? 2020. https://www.cihi.ca/sites/default/files/document/covid-19-rapid-response-long-term-care-snapshot-en.pdf Available at:
- 6.Comas-Herrera A, Zalakaín J, Litwin C, Hsu AT, Lemmon E, Henderson D and Fernández J-L (2020) Mortality associated with COVID-19 outbreaks in care homes: early international evidence. Article in LTCcovid.org, International Long-Term Care Policy Network, CPEC-LSE, 26 June 2020. Available at: https://ltccovid.org/wp-content/uploads/2020/06/Mortality-associated-with-COVID-among-people-who-use-long-term-care-26-June-1.pdf. Published 2020. Updated June 26, 2020. Accessed October 6, 2020.
- 7.Johns Hopkins University & Medicine The Johns Hopkins Coronavirus Resource Center. 2020. https://coronavirus.jhu.edu Available at:
- 8.Lorenz-Dant K. Germany and the COVID-19 long-term care situation. International Long Term Care Policy Network. LTC Responses to COVID-19 Web site. 2020. https://ltccovid.org/wp-content/uploads/2020/05/Germany_LTC_COVID-19–6-May-2020.pdf Available at:
- 9.Lester P.E., Holahan T., Siskind D., Healy E. Policy recommendations regarding skilled nursing facility management of Coronavirus 19 (COVID-19): Lessons from New York State. J Am Med Dir Assoc. 2020;21:888–892. doi: 10.1016/j.jamda.2020.05.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Institute on Ageing The NIA’s ‘iron ring’ guidance for protecting older Canadians in long-term care and congregate living settings. https://static1.squarespace.com/static/5c2fa7b03917eed9b5a436d8/t/5f0f4610bcc2c332db002e67/1594836496177/NIA+Iron+Ring+Guidance+Document+July+15_2020.pdf Available at:
- 11.Hsu A.T., Lane N., Sinha S.K. Understanding the impact of COVID-19 on residents of Canada’s long-term care homes – ongoing challenges and policy responses. International Long Term Care Policy Network. LTC Responses to COVID-19 Web site. 2020. https://ltccovid.org/wp-content/uploads/2020/06/LTCcovid-country-reports_Canada_June-4–2020–1.pdf Available at: