Abstract
Schools in countries across the world are reopening as lockdown to slow progression of COVID-19 is eased. The UK government ordered school closures in England from March 20, 2020, later than the rest of Europe. A temporary and limited return for some year groups was trialled from June 2020. Teachers, school governors, the public and doctors have openly challenged the decision.
The UK government has struggled to provide enough detailed information to convince the public, teachers and health practitioners, that effective systems for protection, including test, trace and isolate, are in place to prevent and manage outbreaks in schools. Risks of infection on reopening to children, staff and families must be weighed against the harms of closure to children’s education and social development. The potential consequences, if the re-opening of schools is managed badly, is subsequent waves of COVID-19 infection leading to more deaths, further school closures and prolonged restrictions, losing any ground gained thus far. This article weighs the evidence for risks and benefits of reopening schools during the pandemic.
Keywords: School re-opening, Safety, COVID-19
What this study adds?
-
•
Consideration of risks and benefits of reopening schools in the UK including COVID-19 transmission, general wellbeing and academic development
-
•
Consideration of the quality and safety of school experience for children, parents and teachers on reopening
-
•
Suggestions for the way forward
Key messages
-
•
The competing demands of safety from infection, general wellbeing and education must be thoroughly considered and balanced in a pandemic school environment
-
•
Investment in schools and systems to enable implementation of safety measures including effective timely test, trace and isolate system minimises long-term harm from lost education and socialisation.
Schools in countries across the world are reopening as lockdown to slow progression of COVID-19 is eased. The UK government ordered school closures in England from March 20, 2020, later than the rest of Europe. The government announced a phased re-opening from the June 1, 2020 beginning with certain year groups identified as key transition years – children aged 4–6 years entering primary school, 10–11 years preparing to transition to secondary schools and, from June 15, 2020 some face-to-face contact for children aged 14–15 and 16–17 years due to take qualifying exams next year (https://www.gov.uk/government/publications/actions-for-educational-and-childcare-settings-to-prepare-for-wider-opening-from-1-june-2020/actions-for-education-and-childcare-settings-to-prepare-for-wider-opening-from-1-june-2020). Teachers, school governors, the public and doctors have openly challenged the decision [1,2].
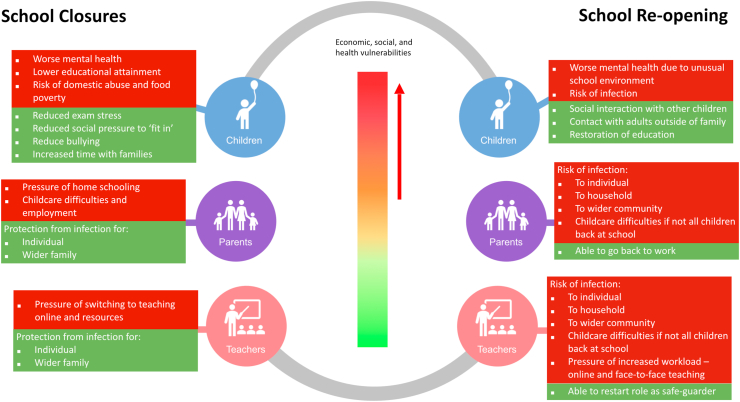
The UK government has struggled to provide enough detailed information to convince the public, teachers and health practitioners, that effective systems for protection, test, trace and isolate, are in place to prevent and manage outbreaks in schools [3]. Risks of infection on reopening to children, staff and families must be weighed against the harms of closure to children’s education and social development (see Fig. 1). The potential consequences, if the re-opening of schools is managed badly, is subsequent waves of COVID-19 infection leading to more deaths, further school closures and prolonged restrictions, thus losing any ground gained thus far. This article weighs the risks and benefits of reopening schools before the start of September 2020 by which time, all UK children had returned to school.
Fig. 1.
The risks (red) and benefits (green) of school closures and re-opening on children, parents and teachers. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
1. COVID-19 in children: How safe is it to reopen the box?
Person-to-person transmission is the main driver for the spread of COVID-19 [4] but there is scientific uncertainty and conflicting evidence around the extent to which children can transmit the virus to teachers, parents and other children from a few small studies.
An Australian study showed that only two students were identified as secondary cases amongst 735 students and 128 members of staff identified as close contacts of 9 students and 9 members of COVID-19 positive staff from 15 schools [5]. There was no evidence of difference in rate of infection by age in China [6] and England [7] implying that children were as likely to be infected as adults but less likely to be symptomatic or develop severe disease [6]. Over 94% of 2135 children with confirmed or suspected COVID-19 in a Chinese cohort were asymptomatic or had mild to moderate symptoms [8] with better prognosis than adults [9]. A small proportion (5·2%) of children experience severe symptoms [8]. A meta-analysis of nine contact tracing studies concluded that children are half as likely as adults to catch COVID-19. However, the included studies were all considered low to medium quality, heterogeneous and included few children [10].
What has emerged is that COVID-19 remains a relatively benign illness for the majority of infected children. There have been 44 deaths from COVID-19 in children aged 0–19 years across the USA, England, Italy, Germany, Spain, France and Korea (0·117% of all deaths in this age group) during a three-month period to May 12, 2020 [11]. Although the risk of mortality from COVID-19 in children is low, concerns over the newly identified multisystem inflammatory syndrome in children must be taken seriously with responsible and transparent communication of risk and knowledge [12]. A recent study in the Bergamo province in Italy found a 30-fold increase in incidence of this inflammatory syndrome since the start of the epidemic [13]. The numbers were small with 19 cases identified in the five years prior to the epidemic and 10 in two months during the epidemic.
True infection and transmission rate cannot be accurately identified without mass testing. Children have been tested less frequently as they exhibit milder or no clinical symptoms [14,15]. A recent report (May 18, 2020) from Italy shows that 2% of 255,549 identified cases were in children aged 0–18 years [16]. Real-time monitoring to identify the daily number of new cases in all age groups and rate of transmission is needed to inform decisions at the local level. In children aged 10 years or younger, estimates from mathematical modelling in the UK on the risk of exposure to a contagious classmate show that risk of infection and death are low and get lower over time. Risk to children decreases by 90% if schools reopen on September 1, 2020 (risk of infection 0·15%) compared to reopening on June 1, 2020 (risk of infection 1·46%) [17]. However, there were no estimates of risk to teachers and families.
2. Effect of school closures on academic development
School closures disadvantage children’s educational and social development. Achievement gaps leave the poorest socioeconomic groups lagging behind their more affluent peers [18]. School narrows these gaps but the gap widens over the long summer holiday [19]. Evidence is limited regarding the impact of other types of school closures on learning loss. Progress has been made since 2011 in narrowing the attainment gap between children from lower socioeconomic backgrounds and their peers but a recent rapid evidence review suggests there is a danger that these school closures could reverse this progress, with the median estimate indicating the gap could widen by 36% [20]. In the UK, the period between Key stage 2 (aged 7–8 years) and Key stage 4 (aged 15–16 years) has been identified as a crucial time to ensure that higher-attaining students from lower socioeconomic backgrounds remain on the high achievement trajectory [21].
During the closure of schools, teacher support for learning has continued remotely, including, but not exclusively digitally. However, the quality of the learning experience will have varied. In a teacher survey on March 22, 2020, 6360 teachers responded to indicate that for state primary schools; 51% would be teaching using an online digital platform, with 49% using take-home physical worksheets or books. At state secondary, this was 82% and 19% respectively [22]. Worryingly, children from lower socioeconomic backgrounds were less likely to have online classes from their schools than their peers from higher socioeconomic backgrounds (~32% compared to ~43% for primary, ~40% compared to ~58% for secondary) [23]. This could be related to availability of technology at school and teacher confidence. Schools are in a difficult position balancing the needs of their students; the more extensive the home-learning resources provided for children, the more some may be left behind, and yet, not providing them, reveals the gaps between schools. Either way, children from lower socioeconomic backgrounds are disproportionately affected.
Alongside differences in what schools provide, children’s home circumstances and parents’ levels of engagement with home learning also vary. Those with poor academic and digital literacy, where parents are not fluent in English, and those with full-time jobs may struggle to keep up. This, combined with a lack of access to computers, books, learning space or other enriching opportunities create a home learning environment that is less conducive to learning [[24], [25], [26], [27]]. The UK government announced, in April, a plan to provide laptop computers to year 10 students from disadvantaged backgrounds [28], which are expected to be with schools shortly [29,30].
3. Effect of school closures on children’s wellbeing
School closures can exacerbate food insecurity, particularly for children living in poverty. Four million children (30%) in the UK live in poverty [31]. Children eligible for free school meals continue to receive these if in school. Those not in school receive support in the form of meals, food parcels or vouchers but this is only applicable during the current coronavirus situation [32]. More than 3 million adults in Britain reported going hungry since the lockdown came into effect with food security worse in households with children compared to those without [33].
School closures during lockdown has meant home confinement, with no face-to-face social interaction with other children and adolescents outside of the immediate household, and restricted time outside of home. Approximately 1 in 10 children in Great Britain are likely to need treatment due to distress or social impairment from an underlying mental health disorder [34]. A survey of 1784 children in China after home confinement for a month found that 22·6% reported depressive symptoms [35], higher than previously identified (17·2%) [36].
Some children may have benefitted from school closures with experiencing less stress or pressure (particularly if bullied at school), receiving more attention from parents and spending quality time with their family. However, children in households under stress and children with additional needs are likely to experience adverse effects. Up to 40% of children receive special educational needs and disability support at some point across the child life course [37]. Social isolation, increased stress on parents and caregivers, uncertain access to food and housing, loss of financial income or support and worries about making ends meet may carry higher risks for child abuse [38]. This, combined with a lack of outside contact with teachers, healthcare professionals and social workers, raises the risk of missing opportunities to identify early signs of the need for safeguarding [39].
Schools in the UK have remained open for ‘vulnerable’ children but only 723,000 of the 2.3 million children in England with a vulnerable family background are estimated to be receiving statutory support and known to services [40]. The proportion of children known to be vulnerable attending school during lockdown has remained low (5% in early April to 14% in May) [41]. Calls to domestic abuse [42] and child support [43] helplines have increased during the lockdown.
4. School reopening in England: What considerations has the government made?
The Scientific Advisory Group for Emergencies (SAGE) compared insights from indicative modelling of seven scenarios for relaxing school closures to two baseline scenarios - schools remain closed (reproduction number Rt of 0) and schools are fully reopened (Rt of 1). The chosen option was to reopen for transition years before summer holidays which increases the modelled Rt to 0·21. This is less than the impact of all primary schools reopening but higher than the most effective strategy identified (alternating one or two weeks on and off with half the class in each staggered group). The potential effects of social distancing, hygiene, testing and other safety measures in school were not incorporated into the modelling but will play a role in informing infection rate in schools as well as wider contextual issues.
5. What have other countries done with regards to reopening of schools?
Most countries have implemented a phased reopening approach [44]. Others such as Italy, Spain, Portugal, California and parts of the UK (Scotland and Northern Ireland) opted for schools to remain closed until the new academic year. New Zealand and Israel have prioritised children with the greatest need such as those from vulnerable homes, younger children requiring adult supervision and children with learning difficulties. However, the success of such targeted approach may not be demonstrable in the UK as only 14% of ‘vulnerable’ children were in schools in May [41]. Germany and China have reopened schools for older children first prioritising those most able to comply with social distancing measures. Denmark has reopened primary schools and for older children due to take exams focusing on the urgency of educational need. There is insufficient scientific evidence to guide the decision to reopen schools for all or certain age groups. However, key influencing factors in most countries that have chosen to reopen schools are low daily number of coronavirus cases and high testing rates.
6. What is the quality of experience that children are returning to?
Schools will need to implement measures to maximise the safety of their staff and the children attending and so it is important to consider the experience that children return to in school. Measures to reduce contact include staggering drop-off and pick-up times, social distancing of parents outside school gates and not allowing parents to enter schools. Playtime may be limited with no tactile engagement or carpet time. The plan was for children to be separated into bubbles of 6–15 with interaction limited to within the bubble but these decisions will be made by staff rather than children who may have formed close friendships and want to interact with their friends. In practice, larger, year-group bubbles are likely for children in secondary schools (aged 11 years and above). Desks will need to be spaced further apart to enable social distancing where possible and children may have to spend most of the school day sat behind a desk [45] which will be new for children in the first year of primary school. Use of outdoor spaces is encouraged and other innovative strategies will need to be identified such as large spaces and phased re-entry to overcome space limitations as more year groups come back. Regular hand washing, or hand sanitisation where washing is not possible, and not allowing children to bring toys and books from school can limit contamination.
The use of personal protective equipment (PPE) are limited to staff in instances where it was previously used (in children whose care needs already involves the use of PPE) and if a child becomes unwell with COVID-19 symptoms while in school and needs care before they can return home [45]. The UK government has made the use of face coverings mandatory on public transport from June 15, 2020 [46] and in public spaces where social distancing measures are hard to follow [47]. Face coverings may have to be used in schools as a safety measure. The use of face coverings may limit the visual cues and engagement with the teachers that children may have experienced in the past, making for a less pleasant experience.
7. What worries parents and teachers?
There is significant fear and anxiety among teachers and parents around the risk of reopening schools [48,49]. The focus has been on the risk to children but schools could become a mode of intra- and inter-transmission for adults. The limited evidence and uncertainty around transmission from children means that some, if not all, concerns could be valid and thus safety measures need to be taken to mitigate the risk with communication of measures to reassure parents and teachers. Teachers need to be consulted in the decision making and implementation of measures at school level so that they feel confident and safe coming back. Responses to a recent online survey of 257,392 parents in England, Wales and Northern Ireland show that parents are concerned about their child not seeing friends and socialising (48%), missing out on learning from teachers (38%) and their child’s mental health (35%). However, 90% of parents do not want their children to return to school immediately after lockdown ends [50] reflecting concerns around risk of infection.
In addition to concern for children, parents with underlying conditions may be worried about exposure due to having to drop-off and pick-up their children from school. Similarly, teachers or other members of staff with underlying conditions who have either not been in work or have been in work for limited hours during the lockdown may be concerned about the risk to their own health. Infection fears, frustration, inadequate information, financial loss and stigma are psychological stressors of quarantine, the effects of which can be long-lasting [51]. Staff at schools should be supported and not pressured to be in work if their concerns cannot be alleviated through the implementation of safety measures. The approach to reopening schools will vary by school with consideration of the local context, for example, schools with higher representation of black and minority ethnic groups are based in more deprived areas where risks are likely to be greater. A system to monitor reasons for absences should be in place to ensure appropriate steps for quarantine of cases and contacts are taken.
8. What resources and long-term structures are needed to prevent and safely manage outbreaks?
The daily number of coronavirus cases in the UK (~2000) is significantly higher than in other countries that have chosen to reopen schools (<500–1000) [52]. Community transmission varies between areas so a local approach to school reopening balances demands of safety and educational need, but needs community testing to know where rates are low. Increased testing and effective contact tracing and isolation for infected individuals has been identified as the most effective measure to prevent a second wave on school reopening. In this modelling, prevention of a further infection wave would require testing at least 51% of symptomatic people, with tracing 40% of contacts, and isolation of symptomatic and positive cases [53]. Consultation with teachers, school leaders, unions, parents and members from the local Councils and the community ensuring ethnic diversity in representation alongside a monitoring system is needed to identify the way to make this work.
Surveillance by school staff is needed to detect symptomatic cases and to promptly isolate suspected cases, while testing is arranged. Schools are organised into small bubble groups and if one tests positive all staff and children in the bubble need to self-isolate for 14 days. Regular testing of teaching staff, children and their households offers a way to detect asymptomatic and pre-symptomatic cases but capacity is lacking [6,54]. Using simple methods of sample collection such as saliva samples is likely to facilitate this process and enhance its acceptability [55]. Responding ad hoc to symptomatic cases will not be efficient or effective. Staff and children living in a household where others have symptoms of COVID-19 infection should self-isolate.
Local Councils are responsible for co-ordinating the response to coronavirus arrangements by working with education settings to support schools and ensure there is sufficient capacity for the groups eligible to attend school or identify alternative options for provision [56]. The government needs to invest in coordination by local Councils with budgets that consider ‘area deprivation’ so that more funds are directed to more deprived areas of the country to enable them to support the safe reopening of schools. Long-term investment in schools to enable implementation of measures to maintain social distancing and changes to allow reorganisation of space and temporary use of alternative spaces also needs to be considered.
9. Conclusion
To avoid further disadvantaging education and social development, children have returned to school in September 2020 but there is a need to balance the competing demands of safety and education. Schools must be part of an effective and timely system of test, trace, isolate and support with virus transmission risk minimisation measures including face coverings and adequate ventilation considered and implemented. Complete transparency of the trade-offs in the face of scientific uncertainty needs to be communicated. This generation of school children will remember being locked down for years to come. Now that we have fully reopened Pandora’s Box, we must maximise the benefits as efforts to mitigate harms are likely to continue long into the future.
Author contributions
Concept (SS, RG, NAA), literature searches (NZ), writing original draft (NZ, KW-T) and reviewing and editing (all authors).
Funding statement
KW-T is supported by the National Institute for Health Research (NIHR) through the Southampton Biomedical Research Centre (BRC). SS is supported by the NIHR NW London Applied Research Collaboration and NIHR School for Public Health Research Programme and Imperial College London Biomedical Research Council. RG is supported by the NIHR through the Great Ormond Street BRC, the Children and Families Policy Research Unit, and Senior Investigator awards. RG receives funding from Health Data Research UK. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Nida Ziauddeen, Email: Nida.Ziauddeen@soton.ac.uk.
Nisreen A. Alwan, Email: N.A.Alwan@soton.ac.uk.
References
- 1.National Governance Association Patchwork picture emerges from BBC snapshot of primary school governors on further reopening. 2020. https://www.nga.org.uk/News/NGA-News/May-2020/Patchwork-picture-emerges-from-BBC-snapshot-of-pri.aspx Available from:
- 2.Independent SAGE Government failing to follow own school advice: review by independent sage. 2020. https://www.independentsage.org/government-failing-to-follow-own-school-advice-review-by-independent-sage/ Available from:
- 3.Department for Education Overview of scientific information on coronavirus (COVID-19) 2020 May. https://www.gov.uk/government/publications/overview-of-scientific-information-on-coronavirus-covid-19 Available from:
- 4.Chan J.F.-W., Yuan S., Kok K.-H., To K.K.-W., Chu H., Yang J., et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020 15;395(10223):514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Centre for Immunisation Research and Surveillance (NCIRS) COVID-19 in schools – the experience in NSW. NSW Government. 2020 Apr http://ncirs.org.au/sites/default/files/2020-04/NCIRS%20NSW%20Schools%20COVID_Summary_FINAL%20public_26%20April%202020.pdf Available from: [Google Scholar]
- 6.Bi Q., Wu Y., Mei S., Ye C., Zou X., Zhang Z., et al. Epidemiology and transmission of COVID-19 in 391 cases and 1286 of their close contacts in Shenzhen, China: a retrospective cohort study. Lancet Infect. Dis. 2020 Apr doi: 10.1016/S1473-3099(20)30287-5. S1473309920302875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Woodhill N. Coronavirus (COVID-19) infection survey pilot: England. 21 May 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/coronaviruscovid19infectionsurveypilot/england21may2020 [Internet]. Office for National Statistics; 2020 May. Available from:
- 8.Dong Y., Mo X., Hu Y., Qi X., Jiang F., Jiang Z., et al. Epidemiology of COVID-19 among children in China. Pediatrics. 2020 Mar 16 doi: 10.1542/peds.2020-0702. [DOI] [PubMed] [Google Scholar]
- 9.Ludvigsson J.F. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020 Jun;109(6):1088–1095. doi: 10.1111/apa.15270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Viner R.M., Mytton O.T., Bonell C., Melendez-Torres G.J., Ward J.L., Hudson L., et al. Susceptibility to and transmission of COVID-19 amongst children and adolescents compared with adults: a systematic review and meta-analysis. Public and Global Health. 2020 May doi: 10.1001/jamapediatrics.2020.4573. http://medrxiv.org/lookup/doi/10.1101/2020.05.20.20108126 [cited 2020 Jun 1]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bhopal S., Bagaria J., Bhopal R. Children’s mortality from COVID-19 compared with all-deaths and other relevant causes of death: epidemiological information for decision-making by parents, teachers, clinicians and policymakers. Publ. Health. 2020 May doi: 10.1016/j.puhe.2020.05.047. S0033350620302092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization Multisystem inflammatory syndrome in children and adolescents temporally related to COVID-19. 2020 May. https://www.who.int/news-room/commentaries/detail/multisystem-inflammatory-syndrome-in-children-and-adolescents-with-covid-19 Available from:
- 13.Verdoni L., Mazza A., Gervasoni A., Martelli L., Ruggeri M., Ciuffreda M., et al. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet. 2020 May doi: 10.1016/S0140-6736(20)31103-X. S014067362031103X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen Z.-M., Fu J.-F., Shu Q., Chen Y.-H., Hua C.-Z., Li F.-B., et al. Diagnosis and treatment recommendations for pediatric respiratory infection caused by the 2019 novel coronavirus. World J Pediatr. 2020 Feb 5 doi: 10.1007/s12519-020-00345-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zimmermann P., Curtis N. Coronavirus infections in children including COVID-19: an overview of the epidemiology, clinical features, diagnosis, treatment and prevention options in children. Pediatr. Infect. Dis. J. 2020;39(5):355–368. doi: 10.1097/INF.0000000000002660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.The COVID-19 task force of the department of infectious diseases and the IT service. Integrated surveillance of COVID-19 in Italy [internet]. Istituto superiore di Sanità. 2020 May. https://www.epicentro.iss.it/en/coronavirus/bollettino/Infografica_18maggio%20ENG.pdf Available from:
- 17.The Independent Scientific Advisory Group for Emergencies (SAGE) The independent SAGE report 2: should schools reopen? Interim findings and concerns - draft document for public discussion. http://www.independentsage.org/wp-content/uploads/2020/05/Independent-Sage-Brief-Report-on-Schools.pdf 22/05/2020; [cited 2020 May 22]. Available from:
- 18.Alexander K.L., Entwisle D.R., Olson L.S. Lasting consequences of the summer learning gap. Am. Socio. Rev. 2007 Apr;72(2):167–180. [Google Scholar]
- 19.Shinwell J., Defeyter M.A. Investigation of summer learning loss in the UK-implications for holiday club provision. Front Public Health. 2017;5:270. doi: 10.3389/fpubh.2017.00270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Education Endowment Foundation Best evidence on impact of school closures on the attainment gap. 2020. https://educationendowmentfoundation.org.uk/covid-19-resources/best-evidence-on-impact-of-school-closures-on-the-attainment-gap/ Available from:
- 21.Crawford C., Macmillan L., Vignoles A. Progress made by high-attaining children from disadvantaged backgrounds [internet]. London: social mobility and child poverty commission. 2014. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/324501/High_attainers_progress_report_final.pdf Available from:
- 22.Teacher Tapp What does distance learning look like in England? (And where will teachers’ kids be today?) 2020. https://teachertapp.co.uk/what-does-distance-learning-look-like-in-england-and-where-will-teachers-kids-be-today/ Available from:
- 23.Andrew A., Cattan S., Costa-Dias M., Farquharson C., Kraftman L., Krutikova S., et al. Institute for Fiscal Studies; 2020 May. Learning during the Lockdown: Real-Time Data on Children’s Experiences during Home Learning. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chowdry H., Crawford C., Dearden L., Joyce R., Sibieta L., Sylva K., et al. Poorer children’s educational attainment: how important are attitudes and behaviour? Joseph Rowntree Foundation. 2010 https://www.jrf.org.uk/report/poorer-children’s-educational-attainment-how-important-are-attitudes-and-behaviour Available from: [Google Scholar]
- 25.Shaw B., Baars S., Menzies L., Parameshwaran M., Allen R. Social Mobility Commission; London: 2017. Low Income Pupils’ Progress at Secondary School [Internet]https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/594363/Progress_at_Secondary_School_report_final.pdf Available from: [Google Scholar]
- 26.Dearden L., Sibieta L., Sylva K. The Socio-Economic Gradient in Early Child Outcomes: Evidence from the Millennium Cohort Study. LLCS. http://www.llcsjournal.org/index.php/llcs/article/view/140 [Internet]. 2011 Jan 31 [cited 2020 May 22];2(1). Available from:
- 27.Cullinane C., Montacute R. COVID-19 and social mobility impact brief #1: school shutdown. 04/2020. https://www.suttontrust.com/wp-content/uploads/2020/04/COVID-19-Impact-Brief-School-Shutdown.pdf The Sutton Trust; Available from:
- 28.Department for Education Get technology support for children and schools during coronavirus (COVID-19) 2020 Apr. https://www.gov.uk/guidance/get-help-with-technology-for-remote-education-during-coronavirus-covid-19 Available from:
- 29.Whittaker F. Coronavirus: majority of free laptops won’t be delivered until June. Schools Week [Internet] 2020 Apr 29. https://schoolsweek.co.uk/coronavirus-majority-of-free-laptops-wont-be-delivered-until-june/ Available from:
- 30.Department for Education Devices and 4G wireless routers data Ad-hoc Notice: laptops, tablets and 4G wireless routers for disadvantaged and vulnerable children: progress data [Internet] 2020 Jun. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/892510/Devices_and_4G_wireless_routers_data_ad_hoc_stats.pdf Available from:
- 31.Joseph Rowntree Foundation . 2020. UK poverty 2019/20. [Google Scholar]
- 32.Department for Education Providing free school meals during the coronavirus outbreak. 2020 May. https://www.gov.uk/government/publications/covid-19-free-school-meals-guidance/covid-19-free-school-meals-guidance-for-schools Available from:
- 33.The Food Foundation Three million people are going hungry just three weeks into lockdown new survey results released. 2020. https://foodfoundation.org.uk/wp-content/uploads/2020/04/Hunger-release-FINAL.pdf Available from:
- 34.Ford T., Goodman R., Meltzer H. The British child and adolescent mental health survey 1999: the prevalence of DSM-IV disorders. J. Am. Acad. Child Adolesc. Psychiatr. 2003 Oct;42(10):1203–1211. doi: 10.1097/00004583-200310000-00011. [DOI] [PubMed] [Google Scholar]
- 35.Xie X., Xue Q., Zhou Y., Zhu K., Liu Q., Zhang J., et al. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in hubei province, China. JAMA Pediatr. 2020 Apr 24 doi: 10.1001/jamapediatrics.2020.1619. https://jamanetwork.com/journals/jamapediatrics/fullarticle/2765196 [cited 2020 May 20]; Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xu D.-D., Rao W.-W., Cao X.-L., Wen S.-Y., An F.-R., Che W.-I., et al. Prevalence of depressive symptoms in primary school students in China: a systematic review and meta-analysis. J. Affect. Disord. 2020 May;268:20–27. doi: 10.1016/j.jad.2020.02.034. [DOI] [PubMed] [Google Scholar]
- 37.Jay M.A., Gilbert R. Special educational needs, social care and health. Arch. Dis. Child. 2020 Jan 22 doi: 10.1136/archdischild-2019-317985. archdischild-2019-317985. [DOI] [PubMed] [Google Scholar]
- 38.Rosenthal C.M., Thompson L.A. Child abuse awareness month during the coronavirus disease 2019 pandemic. JAMA Pediatr [Internet] 2020 Apr 24 doi: 10.1001/jamapediatrics.2020.1459. https://jamanetwork.com/journals/jamapediatrics/fullarticle/2765195 [cited 2020 May 22]; Available from: [DOI] [PubMed] [Google Scholar]
- 39.Green P. Risks to children and young people during covid-19 pandemic. BMJ. 2020 Apr 28:m1669. doi: 10.1136/bmj.m1669. [DOI] [PubMed] [Google Scholar]
- 40.Children’s Commissioner Childhood vulnerability in England 2019. 2019. https://www.childrenscommissioner.gov.uk/publication/childhood-vulnerability-in-england-2019/ [cited 2020 May 22]. Available from:
- 41.Department for Education Attendance in education and early years settings during the coronavirus outbreak. 2020. https://www.gov.uk/government/publications/coronavirus-covid-19-attendance-in-education-and-early-years-settings Available from:
- 42.Grierson J. UK domestic abuse helplines report surge in calls during lockdown. The Guardian. 2020 Sep 4 https://www.theguardian.com/society/2020/apr/09/uk-domestic-abuse-helplines-report-surge-in-calls-during-lockdown Available from: [Google Scholar]
- 43.Hennessy M. ‘Isolated at home with their tormentor’: childline experiences increase in calls since closure of schools. TheJournal. 2020 Mar 20 https://www.thejournal.ie/childline-calls-coronavirus-5053104-Mar2020/ Available from: [Google Scholar]
- 44.Coronavirus How lockdown is being lifted across Europe. BBC News. 2020 Mar 6 https://www.bbc.co.uk/news/explainers-52575313 Available from: [Google Scholar]
- 45.Department for Education Coronavirus (COVID-19): implementing protective measures in education and childcare settings. 2020 Jan. https://www.gov.uk/government/publications/coronavirus-covid-19-implementing-protective-measures-in-education-and-childcare-settings/coronavirus-covid-19-implementing-protective-measures-in-education-and-childcare-settings Available from:
- 46.Department for Transport Face coverings to become mandatory on public transport. 2020. https://www.gov.uk/government/news/face-coverings-to-become-mandatory-on-public-transport Available from:
- 47.Department of Health and Social Care Public advised to cover faces in enclosed spaces. 2020. https://www.gov.uk/government/news/public-advised-to-cover-faces-in-enclosed-spaces [cited 2020 May 22]. Available from:
- 48.Connolly K., Willsher K. European schools get ready to reopen despite concern about pupils spreading Covid-19. The Guardian. 2020 Jan 5 https://www.theguardian.com/world/2020/may/01/children-as-likely-to-spread-coronavirus-as-adults-says-scientist Available from: [Google Scholar]
- 49.Obordo R. ‘Rushed and premature’: parents reveal fears over schools reopening amid Covid-19 crisis The Guardian. https://www.theguardian.com/education/2020/may/15/rushed-and-premature-parents-reveal-fears-over-schools-reopening-amid-covid-19-crisis Available from:
- 50.Parentkind Major new Parentkind research - over a quarter of a million parents have a say on school closures and coronavirus fears. 2020. https://www.parentkind.org.uk/News/Major-new-Parentkind-research---over-a-quarter-of-a-million-parents-have-a-say-on-school-closures-and-coronavirus-fears [cited 2020 May 22]. Available from:
- 51.Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020 Mar;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.John Hopkins Coronavirus Resource Center New cases of COVID-19 in world countries. 2020. https://coronavirus.jhu.edu/data/new-cases Available from:
- 53.Panovska-Griffiths J., Kerr C., Stuart R.M., Mistry D., Klein D., Viner R.M., et al. Determining the optimal strategy for reopening schools, work and society in the UK: balancing earlier opening and the impact of test and trace strategies with the risk of occurrence of a secondary COVID-19 pandemic wave. Infect. Dis. (except HIV/AIDS) 2020 Jun http://medrxiv.org/lookup/doi/10.1101/2020.06.01.20100461 [cited 2020 Jun 16]. Available from: [Google Scholar]
- 54.Peto J., Alwan N.A., Godfrey K.M., Burgess R.A., Hunter D.J., Riboli E., et al. Universal weekly testing as the UK COVID-19 lockdown exit strategy. Lancet. 2020 May;395(10234):1420–1421. doi: 10.1016/S0140-6736(20)30936-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wyllie A.L., Fournier J., Casanovas-Massana A., Campbell M., Tokuyama M., Vijayakumar P., et al. Saliva is more sensitive for SARS-CoV-2 detection in COVID-19 patients than nasopharyngeal swabs. Infectious Diseases (except HIV/AIDS) 2020 Apr http://medrxiv.org/lookup/doi/10.1101/2020.04.16.20067835 [cited 2020 May 22]. Available from: [Google Scholar]
- 56.Department for Education Actions for schools during the coronavirus outbreak. 2020 May. https://www.gov.uk/government/publications/covid-19-school-closures/guidance-for-schools-about-temporarily-closing#what-arrangements-should-schools-and-local-authorities-maintain-throughout-the-remainder-of-may [cited 2020 May 22]. Available from: