Abstract
Background
The COVID-19 pandemic disrupted the delivery of surgical services. The purpose of this communication was to report the impact of the pandemic on surgical training and learner well-being and to document adaptations made by surgery departments.
Study Design
A 37-item survey was distributed to educational leaders in general surgery and other surgical specialty training programs. It included both closed- and open-ended questions and the self-reported stages of GME during the COVID-19 pandemic, as defined by the ACGME. Statistical associations for items with stage were assessed using categorical analysis.
Results
The response rate was 21% (472 of 2,196). US stage distribution (n = 447) was as follows: stage 1, 22%; stage 2, 48%; and stage 3, 30%. Impact on clinical education significantly increased by stage, with severe reductions in nonemergency operations (73% and 86% vs 98%) and emergency operations (8% and 16% vs 34%). Variable effects were reported on minimal expected case numbers across all stages. Reductions were reported in outpatient experience (83%), in-hospital experience (70%), and outside rotations (57%). Increases in ICU rotations were reported with advancing stage (7% and 13% vs 37%). Severity of impact on didactic education increased with stage (14% and 30% vs 46%). Virtual conferences were adopted by 97% across all stages. Severity of impact on learner well-being increased by stage—physical safety (6% and 9% vs 31%), physical health (0% and 7% vs 17%), and emotional health (11% and 24% vs 42%). Regardless of stage, most but not all made adaptations to support trainees’ well-being.
Conclusions
The pandemic adversely impacted surgical training and the well-being of learners across all surgical specialties proportional to increasing ACGME stage. There is a need to develop education disaster plans to support technical competency and learner well-being. Careful assessment for program advancement will also be necessary. The experience during this pandemic shows that virtual learning and telemedicine will have a considerable impact on the future of surgical education.
Abbreviations and Acronyms: Academy, Academy of Master Surgeon Educators; ACS, American College of Surgeons; CR, chief resident; JR, junior resident; PD, program director; SI, sponsoring institution; SR, senior resident
Visual Abstract
Natural disasters, political upheavals, and pandemics can be extremely disruptive to medical education as a whole, and especially to training in procedural specialties, such as general surgery and other surgical specialties. In the US, this educational disruption was displayed in the aftermath of Hurricane Katrina in New Orleans in 2005; yet there was a paucity of literature on the educational consequences of that disaster. The experiences published described instances in which residency programs were able to sustain procedural exposure by redistributing residents to other areas of the state.1 Overall, the need for strong educational leadership and the presence of comprehensive recovery plans were the greatest lessons that emerged from the Katrina natural disaster.2
The COVID-19 pandemic has been inherently unique in that it affected our entire country and the global community. It impacted nearly all facets of daily life and work, including the need to drastically adjust healthcare systems, patient care, and healthcare delivery,3 as well as health sciences education.4 The need for medical professionals to rapidly respond to infection control and containment challenged by resource constraints, prioritization, and use has resulted in a drastic shift and reduction in hospital- and outpatient-associated clinical care across the country. This has called into question the breadth and scope of training and education of medical students, residents, and fellows across all medical disciplines, including the surgical specialties.5 , 6
Some argue that learners in procedural specialties might be at greatest risk to experience deficiency in training and skills acquisition.7 Accrediting and certifying entities have emphasized the need for continuously maintaining quality, and programs have pivoted to alternative approaches to maintain the integrity of surgical training.8 , 9 Virtual technology has emerged as an important tool for delivering both patient care and educational curricular content.10 Individual programs have shared strategies and practical tips focused on innovative education and training, the promotion of resident wellness,11 , 12 and creative interventions and flexibility necessary to successfully transition medical students and surgical residents to the next phase of their training.13 , 14
In response to the extensive and far-reaching challenges imposed on training programs and surgical educators during the COVID-19 pandemic, the American College of Surgeons’ (ACS) Division of Education, through the ACS Academy of Master Surgeon Educators (the Academy), appointed a Special Committee that would examine the impact of, and response to, the pandemic in domains of educational leadership, swift identification and communication of innovations in surgical education, and dissemination of best practices emerging from the disruption caused by the pandemic. Soon after the Special Committee was appointed in March 2020, it established specific priorities, including pursuit of a survey of key surgical educators on the ground (chairs, program directors, and other educators). The purpose was to understand how these leaders perceived the impact of the COVID-19 pandemic on surgical education at their institutions as it affected surgical trainees and faculty. Based on the results of the survey, the Special Committee aims to support surgical educators by communicating shared experiences, emerging trends and innovations, and best practices to sustain themselves and their learners throughout the course of COVID-19 pandemic. It is also hoped that the work of this Special Committee of the ACS Academy will help in preparing for future disasters and support transformation of surgical training once the pandemic is over.
Methods
The overarching goal of the ACS Division of Education and the Academy’s Special Committee was “to address challenges and opportunities relating to post-graduate surgical training during the COVID-19 pandemic.” The Special Committee developed an electronic survey using the Survey Monkey platform that was communicated to surgery chairs and program directors (PDs) and Academy members using available email distribution lists. All surgery chairs and PDs in the US and Canada were invited to participate. Individual participation was voluntary and the data were handled confidentially. The survey encompassed the surgical specialties related to general surgery (ie acute care, trauma, and burn; bariatric and minimally invasive; cardiothoracic, colorectal; critical care; endocrine; pediatric; surgical oncology; transplantation; and vascular surgery) and the following surgical specialties: neurologic surgery, obstetrics and gynecology, ophthalmology, oral and maxillofacial, orthopaedic, otolaryngology, plastic and reconstructive, and urologic surgery. The study was determined to be exempt by the American Institutes for Research IRB, Washington, DC.
The 37-item survey15 was distributed to general surgery and other surgical specialty programs on 3 occasions during a 6-week period (general surgery from April 24 to May 29, 2020) and an 8-week period (other surgical specialties from May 4 to June 26, 2020). The survey to general surgery and related specialties was sent via Listserv to the Association of Program Directors in Surgery; the Society of Surgical Chairs; and program directors in pediatric surgery, surgical oncology, and thoracic surgery with their approval. The survey was also sent via Listserv to associations with their approval representing the other surgical specialties listed in the acknowledgments. The survey was also sent to the Academy. Both closed- and open-ended questions were used to gather quantitative and qualitative information about the impact of the COVID-19 pandemic on surgical education and training. In addition, the 3-stage categorization of the pandemic’s impact on clinical care and education, as defined by ACGME “stage,” was used in analysis of the data obtained through this survey. Respondents reported the sponsoring institution’s (SI) ACGME stage as stage 1: business as usual; stage 2: increased but manageable clinical demand; or stage 3: crossing a threshold beyond which the increase in volume and/or severity of illness creates an extraordinary circumstance in which routine care education and delivery must be reconfigured to focus only on patient care.16
Data collected via the online survey were exported for statistical analyses using SAS, version 9.4 (SAS Institute). Given the variable email control of the majority of email distribution lists used, the ACGME 2018-2019 Data Book17 was used as a reference to determine the absolute number of training programs that served as a surrogate for the total number of possible chair and PD respondents to determine survey response rates.
Data provided a cross-sectional analysis of ACGME stage by respondent and institution, and for a subset of key items and sub-items that assessed overall impact (7 sub-items), adaptive steps (6 sub-items), clinical change (7 sub-items), operative volume (4 sub-items), and operative autonomy (4 sub-items). The impact on levels of learners was also reported. Responses were described using 5-level ordinal Likert-type scale ranging from 5 (extreme impact) to 1 (no impact), except for the binary (yes/no) clinical change items. Responses were dichotomized for analysis as severe impact (5 or 4 on the Likert-type scale) or moderate or less impact (3, 2, and 1 on the Likert-type scale). Learner levels were defined as fellows, chief residents (CRs), senior residents (SRs), and junior residents (JRs). ACGME stage, as described previously, was considered an ordinal variable. The location of the primary teaching institution was reported according to US Census regions and divisions.
To evaluate the association of stage with the analytic items, 2 types of analyses were conducted. First, correlational chi-square values were generated to explore the increase of 3-level stage with an increase in the 5-level Likert-type responses. Second, odds ratios with stage 3 (crossing a threshold) used as a reference were generated using logistic regression to compare stage 1 and stage 2 with stage 3.16 Region was considered as an adjustment variable, but was determined to be highly confounded with stage, and so is not presented here. Significance was defined as p ≤ 0.05.
In addition to quantitative questions, open-ended questions were used to gather information on institutional efforts to “innovate in surgical education” and "support the wellness of learners” during the pandemic. Open-ended responses were coded and analyzed by 2 experienced qualitative researchers and themes were identified.
Results
The overall survey response rate was 21% (472 of 2,196), calculated using a derived total survey estimate from members of the Association of Program Directors in Surgery and the other surgical specialties included in the 1,836 programs from the ACGME 2018-2019 Data Book, Society of Surgical Chairs (n = 187), and Academy members (n = 173). The final analytic dataset contained 472 responses and the total surveyed was determined to be 2,196 (Table 1 ).
Table 1.
Survey Response Rate by General Surgery or Other Surgical Specialties
| Category | Surveyed programs, n∗ | Responses, n | Response rate, % |
|---|---|---|---|
| General surgery and related specialty | |||
| Surgical oncology | 27 | 23 | 85 |
| Colorectal | 63 | 25 | 40 |
| General surgery† | 510 | 124 | 24 |
| Pediatric surgery | 50 | 19 | 38 |
| Cardiothoracic and vascular surgery‡ | 268 | 42 | 16 |
| Subtotal | 918 | 233 | 25 |
| Other surgical specialty | |||
| Ophthalmology | 123 | 65 | 53 |
| Neurologic surgery | 115 | 30 | 26 |
| Orthopaedic surgery | 185 | 42 | 23 |
| Obstetrics and gynecology | 282 | 59 | 21 |
| Other combined§ | 400 | 43 | 11 |
| Subtotal | 1,105 | 239 | 22 |
| Academy members|| | 173 | — | — |
| Total | 2,196 | 472 | 21 |
Academy, Academy of Master Surgeon Educators.
Number of surveyed programs determined from ACGME.17
General surgery programs surveyed include the 323 listed in the ACGME and 187 chairs in the Society of Surgical Chairs and the respondents include general surgery (n = 124), which includes adult general surgery (n = 50); acute care, trauma, burn, and critical care (n = 49); bariatric/minimally invasive (n = 13); endocrine (n = 8), and transplantation (n = 4).
General surgery specialties combined as response rates < 1 SD from the mean response rate.
Other surgical specialties combined as response rates < 1 SD from the mean response rate include oral maxillofacial surgery, otolaryngology, plastic and reconstructive surgery, urology, and not specified.
Academy members were surveyed with a response rate of 45% (73 of 173). The respondents are distributed across the general surgery and related specialties and the other surgical specialties.
The response rate estimates for those indicating general surgery specialties and other surgical specialties were 25% (n = 233 of 918) and 22% (n = 239 of 1,105), respectively, and the response rate for the Academy was 45% (78 of 173) (Table 1). The proportion of respondents indicating a primary role as chair was 36% (141 of 394) and as PD was 64% (253 of 394). Of the chairs, 36% (51 of 141) were from general surgery and 64% (90 of 141) from other surgical specialties. Of the PDs, 42% (107 of 241) were from general surgery specialties and 58% (134 of 241) from the other surgical specialties.
An initial analysis of the proportion of dichotomized severe impact responses from department chairs and PDs in programs with increasing ACGME stage found no significant differences according to their role or discipline and were therefore pooled for subsequent analyses.
Survey demographics
Characteristics of respondents and institutions
More than half of the respondents (54%) had more than 20 years of educational experience, 29% had 11 to 20 years of experience, and 17% had 10 years or fewer. Overwhelmingly, respondents indicated that their primary teaching hospitals were university or university-affiliated (89%) with a Level I trauma center (81%). Approximately two-thirds had a safety net designation (61%) and more than 500-bed capacity (65%). Almost 20% had an associated children’s hospital.
ACGME stage and regional distribution
Of the total sample of 472 respondents, 447 reported stage and US region. There were 15 respondents from other locations—9 from Canada and 6 from other locations outside the US—10 respondents skipped the question on location of primary institution and stage (Fig. 1 ). The proportions of stages in the US were as follows: stage 1 was 22% (98 of 447), stage 2 was 48% (214 of 447), and stage 3 was 30% (135 of 447). According to the ACGME, in June 2020 there were 151 SIs in 26 states with self-declared pandemic emergency status (stage 3). They represented 18% of the SIs, 31% of the accredited programs, and 33% of the residents and fellows in ACGME-accredited residency and fellowship programs in the US.18 The distribution in this survey was similar, with 30% (135 of 447) of respondents with accredited programs reporting an SI self-declared stage 3 status.
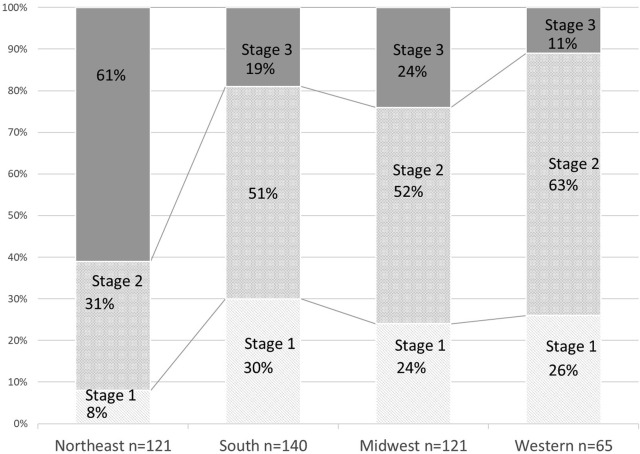
Figure 1.
ACGME stage and regional distribution. Stage 1(n = 98 [22%]): business as usual; stage 2 (n = 214 [48%]): increasing but manageable; stage 3 (n = 135 [30%]): crossing the threshold. There were 447 respondents from the US. The graph shows the distribution of stage by region. There were 15 respondents from other locations—9 from Canada and 6 from other locations outside the US. In addition, 10 respondents skipped the question on location of primary institution and stage.
The numbers of respondents were the same in the Northeast and Midwest (n = 121 [27%] for each), were highest in the South (n = 140 [31%]), and lowest in the Western (n = 65 [15%]) regions of the US. As shown in Figure 1, reports of stage 3 were most frequent in the Northeast region; stage 1 was 8% (10 of 121), stage 2 was 31% (38 of 121), and stage 3 was 61% (73 of 121). As such, region was determined to be highly confounded with stage.
Impact of the COVID-19 pandemic on the education of surgical trainees
Clinical education
Importantly, the educational impact of the pandemic was considered to be the greatest on medical students (n = 461 [78%]) compared with surgical trainees (n = 462 [56%]) and faculty (n = 455 [40%]). This report specifically focuses on surgical trainees.
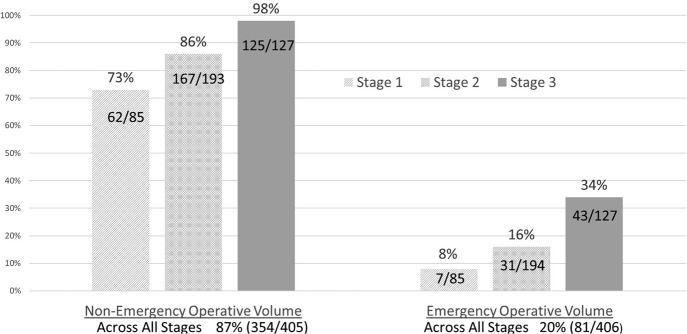
Emergency and elective operative volume
Not surprisingly, the volume of surgical procedures was severely reduced by the pandemic. Nonemergency operative experience was reported as being greatly reduced in 87% (354 of 405) across all stages. However, the reduction was significantly more severe with advancing stage (73% and 86% vs 98%). Emergency operative volume was affected less, but was reported to be reduced by 20% of the respondents and was also significantly associated with advancing stage (8% and 16% vs 34%) (Fig. 2 ).
Figure 2.
Proportion of respondents reporting severe reductions in nonemergency and emergency operative volume. Nonemergency operative volume, stage 1 vs stage 3: odds ratio (OR) 0.43; p < 0.0001; 95% CI, 0.010 to 0.189; stage 2 vs stage 3: OR 0.103; p = 0.0022; 95% CI, 0.024 to 0.441. Emergency operative volume, stage 1 vs stage 3: OR 0.175; p = 0.001; 95% CI, 0.075 to 0.413; stage 2 vs stage 3: OR 0.372; p = 0.0003; 95% CI, 0.218 to 0.632.
Minimal expected program operative requirements, autonomy, and remediation
Although a majority of respondents indicated that neither the program expectation for minimal operative requirements nor the progression to operative autonomy was severely affected, it is striking that minimal operative case expectations were reported as being severely impacted for trainees in the following categories: fellows (30%), CRs (30%), SRs (44%), and JRs (43%). These were not consistently related to stage (Table 2 ). In addition, there was a severe negative impact on expected progression of operative autonomy across all stages reported by 14% to 18% of respondents. These were unrelated to stage, with the exception of fellows in lower-stage programs, who were reported to be impacted less than those at stage 3 (Table 2).
Table 2.
Proportion of Respondents Reporting High Negative Impact on Program Expectations for Minimal Case Requirements and Expected Progression to Operative Autonomy
| Survey question | Total, % (n/N) |
Stage 1,∗ % (n/N) |
Stage 2,† % (n/N) |
Stage 3,‡ % (n/N) |
Stage 1 vs stage 3 |
Stage 2 vs stage 3 |
||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | |||||
| High negative impact on minimal case expectations | ||||||||
| Fellow | 30 (78/261) | 24 (12/49) | 20 (25/124) | 47 (41/88) | 0.610 (0.259–1.440) | 0.2593 | 0.392 (0.292–0.765) | 0.0060 |
| Chief resident | 30 (114/363) | 23 (21/64) | 28 (41/180) | 35 (42/119) | 0.933 (0.462–1.881) | 0.845 | 0.750 (0.4350–1.291) | 0.2989 |
| Senior resident | 44 (158/361) | 44 (29/66) | 40 (66/177) | 50 (59/118) | 1.009 (0.523–1.946) | 0.9796 | 0.829 (0.497–1.381) | 0.4710 |
| Junior resident | 43 (162/374) | 32 (24/74)) | 44 (79/181) | 50 (59/99) | 0.596 (0.308–1.153) | 0.1239 | 0.977 (0.588–1.623) | 0.9293 |
| High negative impact on expected progression to operative autonomy | ||||||||
| Fellow | 16 (50/322) | 14 (9/64) | 13 (20/153) | 18 (21/105) | 0.467 (0.234–0.931) | 0.0306 | 0.507 (0.299–0.859) | 0.0115 |
| Chief resident | 14 (43/381) | 13 (10/76) | 13 (23/183) | 16 (20/122) | 0.799 (0.324–1.970) | 0.6261 | 0.735 (0.361–1.495) | 0.3948 |
| Senior resident | 16 (59/378) | 10 (7/74) | 15 (27/181) | 20 (25/123) | 0.544 (0.210–1.411) | 0.2105 | 0.782 (0.401–1.527) | 0.4722 |
| Junior resident | 18 (89/381) | 18 (14/77) | 20 (35/180) | 23 (40/124) | 0.550 (0.257–1.177) | 0.1236 | 0.573 (0.321–1.023) | 0.0598 |
OR, odds ratio.
Stage 1, business as usual.
Stage 2, increasing but manageable.
Stage 3, crossing the threshold.
Respondents believed that remediation was necessary for some trainees: 18% (62 of 340) for fellows, 25% (93 of 377) for CRs, 47% (177 of 380) for SRs, and 53% (204 of 383) for JRs. The most frequent form of remediation considered was a change in rotation schedule primarily considered for 25% of SRs and JRs (each, n = 95 of 380) and less so for fellows at 8% (28 of 340) and CRs at 12% (47 of 377). Delaying graduation or progression to the next year was extremely rare, averaging < 2% (0.88% [3 of 278] for fellows, 1.3% [5 of 377] for CRs, 1.6% [6 of 380] for SRs, and 1.3% [5 of 383] for JRs). Nearly 70% (266 of 388) of respondents indicated that no extra steps were taken to develop technical competencies beyond the available clinical opportunities during the pandemic. This might have been related to a large proportion of the respondents (44% [180 of 405]) indicating that simulation centers were inaccessible during the pandemic.
Clinical assignments
Institutions adjusted clinical rotations to meet the clinical demands of the pandemic. It is not known whether this was done in consultation with the program. This was most evident in programs with advancing ACGME stage and included assignment of trainees to the emergency department (1% and 3% vs 14%), ICU rotations (7% and 13% vs 37%), and nonsurgical duties (11% and 14% vs 47%) and, to a lesser extent, reassigning faculty to nonsurgical duties (6% and 6% vs 33%). Reductions in outpatient experience were marked (74% and 84% vs 89%), as was in-hospital experience (58% and 75% vs 71%). Outside rotations were described by the respondents as severely reduced (40% and 56% vs 67%). This was more prevalent in other surgical specialties (63% [117 of 185]) compared with general surgery specialties (51% [92 of 182]) (Table 3 ).
Table 3.
Changes in Clinical Experience
| Change in clinical experience | Total, % (n/N) |
Stage 1,∗ % (n/N) |
Stage 2,† % (n/N) |
Stage 3,‡ % (n/N) |
Stage 1 vs stage 3 |
Stage 2 vs stage 3 |
||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | |||||
| Trainee increase in emergency department experience | 6 (27/462) | 1 (1/102) | 3 (7/219) | 14 (19/141) | 0.072 (0.009–0.595) | 0.0145 | 0.218 (0.078–0.609) | 0.0036 |
| Trainee increase in ICU experience | 19 (88/462) | 7 (7/102) | 13 (29/219) | 37 (52/141) | 0.272 (0.111–0.672) | 0.0047 | 0.466 (0.260–0.834) | 0.012 |
| Trainee reassigned to nonsurgical work | 24 (93/392) | 11 (9/82) | 14 (25/185) | 47 (59/125) | 0.138 (0.063–0.300) | < 0.0001 | 0.175 (0.101–0.303) | < 0.0001 |
| Faculty assigned to nonsurgical work | 15 (58/393) | 6 (5/82) | 6 (11/185) | 33 (42/126) | 0.130 (0.049–0.345) | < 0.0001 | 0.126 (0.062–0.258) | < 0.0001 |
| Reduced outpatient experience | 83 (384/462) | 74 (75/102) | 84 (184/219) | 89 (125/141) | 0.394 (0.183–0.847) | 0.0171 | 0.736 (0.365–1.483) | 0.398 |
| Reduced hospital inpatient experience | 70 (324/462) | 58 (59/102) | 75 (165/219) | 71 (100/141) | 0.538 (0.294–0.985) | 0.0446 | 1.126 (0.664–1.910) | 0.6587 |
| Reduction in outside rotation | 57 (207/365) | 40 (29/72) | 56 (98/174) | 67 (80/119) | 0.329 (0.179–0.603) | 0.0003 | 0.629 (0.387–1022) | 0.0613 |
OR, odds ratio.
Stage 1, business as usual.
Stage 2, increasing but manageable.
Stage 3, crossing the threshold.
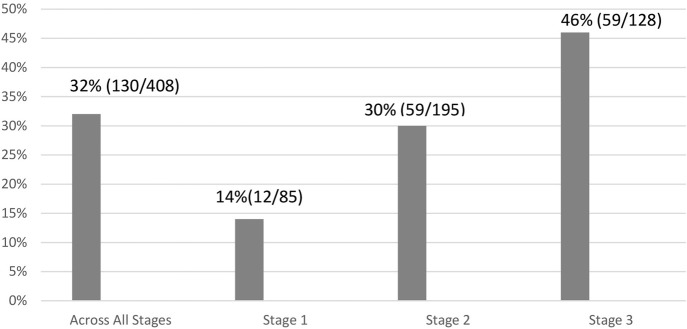
Didactic education
Nearly one-third of all respondents reported severe challenges in didactic education, with some activities suspended and many switched to a virtual format. Reports of high impact on didactic education were significantly more frequent with advancing stage—14% for stage 1, 30% for stage 2, and 46% for stage 3 (Fig. 3 ). Of general surgical specialties, 37% (75 of 204) reported severe challenges in didactic education compared with 27% (55 of 207) in other surgical specialties. Nearly all of those responding about educational innovation (n = 407) adopted virtual conferences (97%) and many had used virtual interviews (43%) and virtual oral examinations (33%); 45% recorded lectures for future use and 40% provided training for telemedicine. The most frequent use of virtual formats was journal club (74% [305 of 410]), grand rounds (73% [298 of 408]), research conferences (71% [291 of 410]), morbidity and mortality conferences (70% [294 of 404]), and tumor boards (62% [252 of 407]). Suspension of programs was noted as follows: visiting professors, 61% (249 of 409); simulation training, 53% (217 of 407); grand rounds, 21% (87 of 408); morbidity and mortality conferences, research conferences, and journal clubs, each 18% (72 of 404); and teaching rounds, 17% (70 of 409). Many of those responding about technical problems (n = 405) reported issues with the virtual platforms. The most frequent problems reported were general technical issues (47%) and bandwidth (25%). There were fewer concerns about privacy issues (10%), faculty resistance (11%), learner resistance (6%), and attendance (14%).
Figure 3.
Severe impact on didactic education by ACGME stage. Stage 1: business as usual; stage 2: increasing but manageable; stage 3: crossing the threshold. Stage 1 vs stage 3: OR 0.192; p < 0.0001; 95% CI, 0.095 to 0.388; stage 2 vs stage 3: OR 0.507; p = 0.0041; 95% CI, 0.319 to 0.806.
Quality of education
Despite the clinical and didactic educational challenges that resulted from the pandemic, the respondents indicated that they were able to continue to address the major ACGME competencies by the use of national curricula—core knowledge (92% [358 of 388]), problem solving (64% [247 of 388]), professionalism (53% [204 of 388]), communication (49% [189 of 388]), and technical skills (32% [122 of 388]). Surgical trainees’ end-of-rotation evaluations (n = 404) were conducted in the usual manner in 54% (218 of 404). Evaluations were expanded to include pandemic-specific concerns in 19% (76 of 404) of programs. The respondents were able to continue assessment of the ACGME competencies because evaluations were reported as being infrequently suspended (13% [51 of 404]) or reduced (29% [18 of 404]), and the ability to maintain formative assessments was reported by 55% (221 of 403). However, the survey did not assess the overall quality of the evaluations.
Qualitative analysis of educational impact
Several themes emerged from the qualitative analysis, as shown in Table 4 . Strategies being used included pivoting to online conferences; use of national programs and curricula; use of simulation, laboratories, and robotics; adjustment of exposure to clinical work; modified schedules; and virtual mentoring and testing.
Table 4.
Themes That Emerged Related to Education Innovations Implemented in Response to the Pandemic
| Theme | Sample responses |
|---|---|
| Pivot to online conferences/didactics | Implementation of virtual surgical conferences; enhanced daily didactic sessions (virtual); online morbidity and mortality conferences, journal club, tumor board, and grand rounds |
| Use of national programs/curriculum | Use of nationally available curricula to a much greater extent; city-wide shared lecture/educational sessions; virtual score curriculum; using national OB/GYN curriculum; national webinars on surgical training; collaboration with other institutions on virtual meetings |
| Simulation/laboratories/robotics | Increased use of wet laboratory for technical surgery practice; developed take-home simulation kits for certain procedures; structured individual trainee sessions in fundamentals of laparoscopic surgery simulation; boot camp remotely including simulation at home; live video of wet laboratory monitored remotely by an attending; increased use of surgical simulators to keep from getting "rusty" |
| Continued exposure to clinical work | Virtual clinical rounding; more involvement in the ICU rotations; increased experience with remote consultation; live streaming of operating room cases with residents able to ask questions; telehealth participation by residents in pre- and postoperative care |
| Scheduling | Modified rotations to give more cases to residents with fewer cases; created teams of residents that would work in clinic at same time so that there was less likelihood of all the residents being exposed; moved some residents to our suburban locations; dynamic scheduling to maximize surgical exposure; improved planning of staffing with rotating key individuals; modified schedule to mirror weekends: teams get work done and sign out to a call team who stays |
| Virtual mentoring/mock-orals/examinations | Virtual mock oral examination that allowed us to use examiners from other institutions; virtual interviews for residents and fellows; virtual oral board preparations |
Impact of the COVID-19 pandemic on surgical trainee health and wellness
We assessed the perceptions of the educational leaders on surgical trainee well-being and not the opinions of the trainees. Sixty-one percent of respondents reported that surgical trainees were involved with the treatment of patients with COVID-19, 30% reported that trainees were not caring for these patients, and 9% were uncertain. Across all stages, respondents reported a severe impact on trainees’ physical safety in 15%, physical health in 9%, and emotional health in 27%. These numbers increased with advancing stage: physical safety, 6% and 9% vs 31%; physical health, 0% and 7% vs 17%; and emotional health, 11% and 24% vs 42% (Table 5 ).
Table 5.
Frequency of Severe Impact on Trainee Health and Institutional Adaptations Occurring to a Great Extent
| Survey parameter | Total, % (n/N) |
Stage 1,∗ % (n/N) |
Stage 2,† % (n/N) |
Stage 3,‡ % (n/N) |
Stage 1 vs stage 3 |
Stage 2 vs stage 3 |
||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | |||||
| Learner health | ||||||||
| Physical health | 9 (35/406) | 0 (0/85) | 7 (13/194) | 17 (22/127) | NR§ | — | 0.343 (0.166–0.709) | 0.0039 |
| Emotional health | 27 (109/404) | 11 (9/83) | 24 (47/194) | 42 (53/127) | 0.170 (0.078–0.369) | < 0.0001 | 0.446 (0.276–0.723) | 0.0010 |
| Physical safety | 15 (62/403) | 6 (5/83) | 9 (18/193) | 31 (39/127) | 0.145 (0.054–0.385) | 0.0001 | 0.232 (0.126–0.429) | < 0.00001 |
| Institutional adaptation | ||||||||
| Coping assistance | 71 (287/406) | 60 (51/85) | 71 (137/193) | 77 (99/128) | 0.439 (0.241–0.800) | 0.0072 | 0.717 (0.427–1.203) | 0.2073 |
| Sensitivity to learners | 73 (295/407 | 59 (50/85) | 76 (148/194) | 76 (97/128) | 0.464 (0.258–0.834) | 0.0104 | 1.135 (0.674–1.911) | 0.6330 |
| Sensitivity to faculty | 58 (235/406) | 54 (46/85) | 56 (108/193) | 63 (81/128) | 0.684 (0.392–1.196) | 0.1827 | 0.737 (0.466–1.166) | 0.1923 |
| Additional safety measures | 86 (249/407) | 85 (72/85) | 84 (163/194) | 88 (124/128) | 0.680 (0.302–1.530) | 0.3513 | 0.646 (0.329–1.268) | 0.2041 |
OR, odds ratio; NR, no result.
Stage 1, business as usual.
Stage 2, increasing but manageable.
Stage 3, crossing the threshold.
Proportion of physical health stage 1 vs stage 3 cannot be determined by logistic regression.
Institutional adaptations reported as occurring to a great extent were significantly related to stage, including the provision of coping assistance to trainees (60% and 71% vs 77%) and increased sensitivity to learners (59% and 76% vs 76%). Respondents reported the adoption of safety measures (86%) and sensitivity to the needs of faculty (58%) occurred regardless of stage (Table 5).
Qualitative analysis of the impact on learner well-being
Several themes emerged as related to institutional initiatives to support the wellness of learners. These included program check-ins or huddles, accessing existing or institutional and national resources, and scheduling to reduce exposure to COVID-19 and allow more free time, enhanced communication, and additional amenities (Table 6 ).
Table 6.
Themes That Emerged Related to Institutional Efforts to Support the Wellness of Learners During the Pandemic
| Theme | Sample responses |
|---|---|
| Individual and program check-ins (instituted in response to COVID-19) | Daily PD calls during peak surge, weekly check-in Zoom meetings with hospital leaders that could directly answer questions, daily contact in some fashion through Zoom; open access to the DIO, PDs and APDs for any and all concerns, bidirectional conversations to provide support and solutions; PD at sign out virtually twice a day; weekly Zoom meeting with PDs, chair, residents to discuss issues and concerns, more frequent feedback and contact with mentors; buddy system (1 person on is paired with someone who was off); text check-ins with residents by PD and APD; PD weekly “fireside” chat with residents to address concerns, provide forum for open discussion; special wellness task force with weekly meetings |
| Use of existing institutional and national resources | Information for wellness opportunities (eg free virtual yoga, meditation); 24/7 availability for residents through Employee Assistance Program, weekly wellness webinars; virtual meet and greets, access to therapists, psychologists and psychiatrists, virtual wellness camps and meetings; wellness center 24/7 hotlines, wellness bulletins; increased wellness sessions, access to online resources; access to free wellness apps; department wellness committee; meditation rooms, increased access to counseling; mindfulness sessions, chaplain counseling; lists of resources and free items for healthcare providers |
| Scheduling | Reduced hospital time, more personal time; agreeable to a relaxed clinical schedule; can take a wellness day when needed, rotating groups of residents for 2 wk of educational time at home; increased time away from hospital, decreased shifts (no 24 h), increased number on team at a time; rotation of fellow with residents to give more time at home; ensuring scheduling is not overburdensome; created care teams to limit hours of exposure in hospital; rotational approach to clinical coverage with additional time out of clinic; time off after redeployments; minimizing COVID exposure and fear by offering "call team only" attendance with academic assignments on days "working from home"; protected time between scheduled shifts, rotating people between locations frequently so that they do not stay too long in any high-risk areas |
| Communication | Solid information flow; increased communication and reassurance; weekly town hall meetings and daily email updates to keep people informed; we are maintaining open lines of communication to the residents, ensuring that their voices are heard; daily communications; DIO town halls, wellness emails from hospital leadership; daily PD calls during peak surge, weekly check-in Zoom with hospital leaders that could directly answer questions, daily contact in some fashion through Zoom; sending large numbers of emails with supportive phrases; ongoing conversations regarding the impact of COVID-19 on institutions, programs, individuals; weekly GME town halls with infectious disease doctors explaining changes |
| Amenities (food, housing, childcare) | Providing additional childcare assistance; lots of food; hazard pay, transportation allowance, housing assistance; providing massages; free food and parking, sharing discounts from stores; lunch and dinner provided to all floor/ICUs, free haircuts by a barber, food in the resident lounges, housing for those concerned to go home if on a COVID floor, babysitting for those with childcare issues |
APD, associate program director; DIO, designated institutional officer; PD, program director.
Impact of COVID-19 pandemic on institutional disaster planning
The majority of the 472 respondents surveyed were aware that an institutional disaster plan existed and were aware of its content (62%); however, 26% were made aware during the pandemic and 12% were left uncertain. Whether the plan included an education statement was uncertain for nearly half of respondents (46%), and either assuredly present (29%) or absent (22%) for the remainder of respondents. Seventy-nine percent of respondents believed their institutional disaster plan should include an educational statement in the future, although 11% did not believe it necessary and 10% were uncertain.
Discussion
The global COVID-19 pandemic has created unprecedented disruption to the delivery of surgical services throughout the US5, 6, 7 and internationally,19 with a profound effect on surgical training. The ACS Division of Education, through the Special Committee of the ACS Academy, has been assessing the short- and long-term impact of COVID-19 on learners in surgery and is developing new strategies and programs to address various challenges. As part of this effort, the survey that forms the basis of the current study included a sample of all surgical specialties, department chairs, PDs, and selected members of the Academy with the goal of taking a “snapshot” in time of the impact of the pandemic on surgical education and learner health. This study is unique in that it samples the “house of surgery” and, as such, the results might bring forth common strategies that can mitigate the impact of future pandemics or disasters on surgical training and learner well-being. In addition, to our knowledge, this is the first study to analyze the association between the severity of impact on surgical training and ACGME stage.
The survey results were stratified by geographic region and by self-declared SI ACGME pandemic stage on educational programs. Because the survey was administered in late April through June 2020, the impact of COVID-19 was greatest in the Northeast regions, which included the severe initial wave experienced in the New York tristate area. About one-third of the respondents indicated that their institutions were in stage 3 and had crossed the threshold, and nearly one-half of the respondents indicated their institutions were in stage 2, reflecting increased but manageable COVID-19-related clinical demand. Recent acceleration of the pandemic across the South and Western regions of the country occurred subsequent to the timeframe of the survey, and many of the adjustments to surgical education and training reported in those programs were likely more anticipatory than reactive.
Although the pandemic has substantially altered the educational experience of learners, most of the respondents indicated that the circumstances allowed for continued development of most of the ACGME core competencies, except technical skills. The normal rotation schedule at most institutions required considerable revision, including restrictions on rotations at outside institutions. Increases in ICU and nonsurgical experiences were particularly common in stage 3 programs and there was a trend that these were more common in general surgery specialties compared with the other surgical specialties. At stage 3 institutions, redeployment of trainees and, to a lesser extent, faculty to nonsurgical services was common. The outpatient experience for residents and fellows was severely impacted irrespective of institutional stage or surgical specialty. White and colleagues20 observed that the rapid adoption of telephone and video visits at many centers was independent of learner involvement and represented a loss of multiple face-to-face learning opportunities. Because video visits are likely to remain an important mechanism for outpatient patient care, there is an urgent need to share best practices to enhance resident participation.
The reduction of nonemergency operations substantially impacted the operative experience of trainees across all surgical specialties in an ACGME stage-dependent fashion. Reductions in operative experience have been noted in general surgery,20 as well as neurosurgery,21 , 22 ophthalmology,23 orthopaedic surgery,24 and otolaryngology.25 Alternatives to increase exposure to technical skills development include the use of simulation centers and cadaver laboratories, both of which had limited access during the pandemic.7 , 24
It is striking that three-quarters of stage 1 (“business as usual”) institutions still reported high-impact reductions, which is difficult to understand. This might be the result of the SI (as a whole) declaring itself as doing business as usual, despite the surgical programs within the institution struggling to provide clinical education. The decrease in surgical volume might have also been in preparation to free beds for a possible COVID-19 surge, which might or might not have materialized. It also might have reflected patient self-avoidance of elective procedures during the pandemic. Although the reasons might never be fully understood, it is important to note for future national disasters of this magnitude that the operative volume can be severely impacted in institutions that have not self-declared an emergency declaration.
Although many respondents indicated that progression to operative autonomy was not negatively affected, 14% to 18% perceived it was severely impacted. Concerns about the ability to achieve program expectations for case minimums for both residents and fellows across all surgical specialties were evident in half of the stage 3 programs and also, to a great extent, in lower stages (Table 2). The educators surveyed believed that remediation was necessary for many trainees, which seemed to be more of a concern for less experienced trainees—18% (62 of 340) for fellow, 25% (93 of 377) for CRs, 47% (177 of 380) for SRs, and 53% (204 of 383) for JRs. Contrarily, when general surgery CRs were surveyed in the study by Zheng and colleagues,5 they were found to be not as concerned about achieving minimal case numbers and were more concerned with the potential delay in board examinations and adequate preparation.
It is difficult to reconcile the discordance between the high impact on operative volume and expected case numbers and the lower impact on expected progression to operative autonomy. A goal of surgical training is the ability of the graduating resident or fellow to practice independently and case numbers do not necessarily predict readiness for independent practice. However, they are a surrogate for surgical experience and exposure. In situations in which institutional operative volume is severely reduced, such as the case in the pandemic, there is a clear opportunity to better address development of technical competence and operative autonomy through competency-based education models.
As highly impacted institutions gradually restore surgical volumes, PDs will likely need to find ways to adjust post-pandemic rotation schedules such that JRs and SRs can achieve case minimums during the course of a multiyear training program. It might be much harder for fellows and CRs to achieve adequate case volumes, depending on the timing of institutional disruption in the academic year. In the case of 1-year clinical fellowships, such as colorectal surgery, the pandemic could reduce operative experience by as much as 25%.
The survey was completed in the last quarter of the academic year. Although many respondents thought that remediation to provide more clinical experience and cases was not necessary, concern about readiness for fellowship training or to enter independent practice might be justified, and it might prove necessary for some individuals to extend their training or undergo additional proctoring as they transition to new positions. It remains the responsibility of individual PDs (supported by their clinical competency committees) to complete the summative evaluations that support decisions about progression to the next level of training or program completion and readiness for independent practice.
Although the pandemic introduced considerable challenges to didactic education, rapid innovation and transition to virtual (video) formats were evident irrespective of surgical specialty or institutional stage. Although some educational activities were suspended, a shift to video conferences was almost universally adopted. Nearly half of respondents reported technical problems with the transition. Video-based approaches were also adopted for oral examinations, interviews, and mentoring. Whether the use of video technology becomes the “new normal” remains to be seen, but anecdotal experiences strongly suggest this will be the case. The pandemic forced innovation in didactics, accelerating the implementation of distance/video-based virtual learning, which might ultimately prove to be more efficient and less disruptive to clinical workflows. Interestingly, increased participation in educational conferences, including morbidity and mortality conferences, has been observed.
According to the survey of educators, it was perceived that learner emotional health and sense of physical safety were more severely impacted at stage 3 institutions. It must be clear that residents and fellows were not surveyed in this study. However, this is consistent with surveys by other investigators of residents during the pandemic, which documented increased stress, burnout, and health concerns.26 , 27 Although there was a high proportion of institutional adaptations that included assistance with coping mechanisms and provision of safety measures beyond personal protective equipment, this was not universal even in stage 3 institutions. The sample in this study was disproportionately represented by academic health centers that have access to institutional wellness programs. Conversely, availability of such programs, including childcare, housing, and virtual mental health services, has been reported to be significantly less in independent programs.20 An opportunity for enhanced sensitivity to learners and faculty was evident, suggesting that the impact on provider wellness might have been underestimated. The pandemic has inflicted substantial and distressing morbidity and mortality on its victims and their caregivers, exacerbated by stringent visitor restriction policies. Many of the respondents represent safety net institutions in vulnerable communities that have been disproportionately impacted by COVID-19 against a pre-existent backdrop of disparities to access and care.
The results also indicated that although many institutions had effective disaster plans to responded effectively to clinical disruption, most institutions either had no provision for educational disruption or the respondents were unaware of such plans. The experience with the COVID-19 pandemic highlights the need for institutions to develop disaster plans that include disruption to educational programs that not only include the “rules of engagement” around clinical redeployment, but also the continuation of didactics and psychological counseling and other supportive infrastructure, including childcare, that are critical to sustain the wellness of learners. In previous disasters, such as Hurricanes Katrina and Sandy, or mass casualty events like the Boston Marathon bombing, the disruption was regional or local in nature; experience with the pandemic highlights the need to consider national and global disaster planning. Although the ACGME has sunset its “three stages” effective July 1, 2020 and is migrating to a binary approach to characterize GME operations during a pandemic with a nonemergency category and an emergency category,28 the results of this study support the linkage of future institutional planning an ACGME-like staging system. Also, we must call attention to the observation that lower-stage institutions had a substantial reduction in operative volume that could derail surgical training independent of an emergency declaration.
As the qualitative data illustrate, the response to the impact of the pandemic on the education of surgical trainees and their wellness was timely and might well change the future of surgical education and training. It is obvious that some of the changes in response to the pandemic might prove to be more effective and efficient than the old ways of training and supporting surgical learners. As illustrated, the use of technology to deliver virtual education is arguably just as successful as live conferences. Similarly, many of the efforts to support resident wellness can address the longstanding issue of burnout and better prepare us for future disasters. Perhaps most telling is the fact that the innovative training and wellness programs implemented are not new, extremely costly, or disruptive to patient care and hospital systems. In many cases, these resources existed but were not used.
The conclusion of this study must be interpreted in the context of its limitations. As with most surveys, the results might well be affected by response bias based on self-selection and the relatively low response rate. Because department chairs and PDs from the same institution might have completed the survey (and because there was no obvious difference between their responses as a group), there might be overweighting of some institutional experiences. Those most affected by the pandemic might have had increased motivation to participate in an assessment of its impact. University and university-affiliated programs represented nearly 90% of the responses, also indicating the possibility of response bias. The survey solicited opinion rather than actual institutional data, and it is possible that responses could be skewed to overestimate or underestimate the true impact. There was a variable response from each of the other surgical specialty groups outside of the general surgery specialties. Although there were no obvious differences among combined responses from other surgical specialties, the sample size was insufficient to draw meaningful comparisons between specialty groups (eg comparing obstetrics and gynecology with orthopaedic surgery).
Conclusions
As the surgical community increasingly digests the lessons learned during the COVID-19 pandemic, a number of conclusions are already clear. Few, if any, institutions were truly prepared to address the crisis in surgical training programs in the wake of the pandemic. There was a severe impact on surgical training across all surgical specialties and common themes have emerged.
Nonemergency operative experience was severely impacted, as were emergency case numbers, but to a lesser extent. Many perceived that some trainees did not achieve the expected training numbers and, as a result, there was a variable degree of the trainee achieving the expected progression of surgical skills to predetermined levels. As a result, there was the perception of the need for remediation for some surgical trainees, particularly those in more junior years. As such, during a crisis like the COVID-19 pandemic, it is even more important for individual PDs (supported by their clinical competency committees) to complete the summative evaluations that support decisions about progression to the next level of training or program completion or independent practice and to consider options for remediation when necessary. A real opportunity for surgical educators is to design and implement innovations that could help ensure continued development of optimal technical competence of surgical trainees during future pandemics or other global disasters.
The pandemic has forced innovation in clinical experiences and didactic learning, especially with respect to virtual learning and telemedicine, that has been generally well accepted and likely to become permanent. Opportunities are also evident for institutions to increase support for coping and learner safety. The ACGME staging system is associated with the severity of educational impact at each institution. Stage can be predictive of the impact of a future widespread national disaster and as such its consideration in disaster planning might permit a more graduated and individualized approach. Finally, institutional disaster plans should include statements about education that are reviewed by PDs and department chairs.
Author Contributions
Study conception and design: Ellison, Debas, Eberlein, Britt, Sachdeva
Acquisition of data: Nagler, Blair
Analysis and interpretation of data: Ellison, Spanknebel, Stain, Nagler, Farmer, Sloane
Drafting of manuscript: Ellison, Spanknebel, Stain, Shabahang, Matthews, Sloane
Critical revision: Spanknebel, Debas, Blair, Sachdeva
Acknowledgment
The authors wish to acknowledge Susan Newman, MPH, without whom we could not have completed the project. In addition, the authors wish to thank the following organizations that gave permission to circulate the survey to their members and their membership who completed the survey: Academic Orthopaedic Consortium, American Association of Oral and Maxillofacial Surgeons, American Council of Academic Plastic Surgeons, Association of Program Directors in Colon & Rectal Surgery, Association of Program Directors in Surgery, Association of Program Directors in Vascular Surgery, Association of Pediatric Surgery Training Program Directors, Association of University Professors in Ophthalmology, Council of University Chairs of Obstetrics and Gynecology & Council on Resident Education in Obstetrics and Gynecology, Otolaryngology Program Directors Association, Society of Academic Urologists, Society of Neurological Surgeons, Society of Surgical Chairs, Surgical Oncology Fellowship Committee for the Society of Surgical Oncology, and Thoracic Surgery Directors Association.
Footnotes
Disclosure Information: Nothing to disclose.
Disclosure outside the scope of this work: Dr Ellison receives royalty payments for original contributions from McGraw-Hill Medical and Wolters Kluwer. All other authors have nothing to disclose.
References
- 1.Hoxsey R., Smith M., Miller J., Nolan T. Surviving disaster: assessment of obstetrics and gynecology training at Louisiana State University-New Orleans before and after Hurricane Katrina. Am J Med Sci. 2008;336:151–155. doi: 10.1097/MAJ.0b013e318180f635. [DOI] [PubMed] [Google Scholar]
- 2.Kahn M., Sachs B. Crises and turnaround management: lessons learned from recovery of New Orleans and Tulane University following Hurricane Katrina. Rambam Maimonides Med J. 2018;9(4) doi: 10.5041/RMMJ.10354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brindle ME, Gawande A. Managing COVID-19 in surgical systems. Ann Surg 272(1):e1–e2. [DOI] [PMC free article] [PubMed]
- 4.Calhoun K.E., Yale L.A., Whipple M.E. The impact of COVID-19 on medical student surgical education: implementing extreme pandemic response measures in a widely distributed surgical clerkship experience. Am J Surg. 2020;220:44–47. doi: 10.1016/j.amjsurg.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zheng J., Hundeyin M., He K. General surgery chief residents’ perspective on surgical education during the COVID-19 pandemic. Surgery. 2020;168:222–225. doi: 10.1016/j.surg.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adesoye T., Davis C.H., Del Calvo H. Optimization of surgical resident safety and education during the COVID-19 pandemic-lessons learned. J Surg Educ. 2020 Jul 1 doi: 10.1016/j.jsurg.2020.06.040. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Imielski, B. The detrimental effect of COVID-19 on subspecialty medical education. Surgery 68:218–219. [DOI] [PMC free article] [PubMed]
- 8.American Board of Surgery ABS statement on training requirements during COVID-19. http://www.absurgery.org/default.jsp?news_covid19_training Available at: Updated March 19, 2020. Accessed July 12, 2020.
- 9.ACGME. ACGME response to coronavirus (COVID-19) https://acgme.org/Newsroom/Newsroom-Details/ArticleID/10111/ACGME-Response-to-the-Coronavirus-COVID-19 Available at: Updated March 18, 2020. Accessed March 20, 2020.
- 10.Coe T.M., Jogerst K.M., Sell N.M. Practical techniques to adapt surgical resident education to the COVID-19 era. Ann Surg. 2020;72:e139–e141. doi: 10.1097/SLA.0000000000003993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Daodu O., Panda N., Lopushinsky S. COVID-19–considerations and implications for surgical learners. Ann Surg. 2020;272(1):e22–e23. doi: 10.1097/SLA.0000000000003927. [DOI] [PubMed] [Google Scholar]
- 12.Nobel T.B., Marin M., Divino C.M. Lessons in flexibility from a general surgery program at the epicenter of the pandemic in New York City. Surgery. 2020;168:11–13. doi: 10.1016/j.surg.2020.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nassar A.H., Zern N.K., McIntyre L.K. Emergency restructuring of a general surgery residency program during the coronavirus disease 2019 pandemic: the University of Washington experience. JAMA Surg. 2020;155:624–627. doi: 10.1001/jamasurg.2020.1219. [DOI] [PubMed] [Google Scholar]
- 14.Bryan D.S., Benjamin A.J., Schneider A.B. Nimble, together: a training program's response to the COVID-19 pandemic. Ann Surg. 2020;272:e142–e143. doi: 10.1097/SLA.0000000000003994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Academy of Master Surgeon Educators ACS Academy of Master Surgeon Educators: educational impact of COVID-19. https://www.surveymonkey.com/r/ACSAcademyCovid19Education Available at:
- 16.ACGME (Archived) Three Stages of GME During the COVID-19. https://acgme.org/COVID-19/-Archived-Three-Stages-of-GME-During-the-COVID-19-Pandemic Available at:
- 17.ACGME. Table A.4. In: Data Resource Book. Academic Year 2018-2019. Chicago, IL: ACGME; 2019:17–19. Available at: https://www.acgme.org/About-Us/Publications-and-Resources/Graduate-Medical-Education-Data-Resource-Book. Accessed July 20, 2020.
- 18.Nasca T.J. ACGME’s early adaptation to the COVID-19 pandemic: principles and lessons learned. J Grad Educ. 2020;12:375–378. doi: 10.4300/JGME-D-20-00302.1. https://www.jgme.org/doi/pdf/10.4300/JGME-D-20-00302.1 Available at: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.James H.K., Pattison G.T.R. Disruption to surgical training during Covid-19 in the United States, United Kingdom, Canada, and Australasia: a rapid review of impact and mitigation efforts. J Surg Educ. 2020 Jun 25 doi: 10.1016/j.jsurg.2020.06.020. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.White E.M., Shaughnessy M.P., Esposito A.C. Surgical education in the time of COVID: understanding the early response of surgical training programs to the novel coronavirus pandemic. J Surg Educ. 2020 Jul 25 doi: 10.1016/j.jsurg.2020.07.036. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khalafallah A.M., Jimenez A.E., Lee R.P. Impact of COVID-19 on an academic neurosurgery department: the Johns Hopkins experience. World Neurosurg. 2020;139:e877–e884. doi: 10.1016/j.wneu.2020.05.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pennington Z., Lubelski D., Khalafallah A.M. Letter to the editor "Changes to Neurosurgery Resident Education Since Onset of the COVID-19 Pandemic. World Neurosurg. 2020;139:734–740. doi: 10.1016/j.wneu.2020.05.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ferrara M., Romano V., Steel D.H. Reshaping ophthalmology training after COVID-19 pandemic. Eye. 2020 Jul 1 doi: 10.1038/s41433-020-1061-3. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stambough J.B., Curtin B.M., Gililland J.M. The past, present, and future of orthopedic education: lessons learned from the COVID-19 pandemic. J Arthroplasty. 2020;35(7S):S60–S64. doi: 10.1016/j.arth.2020.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guo T., Kiong K.L., Yao C.M.K.L. Impact of the COVID-19 pandemic on otolaryngology trainee education. Head Neck. 2020 Jul 15 doi: 10.1002/hed.26368. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Collins C., Mahuron K., Bongiovanni T. Stress and the surgical resident in the COVID-19 pandemic. J Surg Educ. 2020 Jul 25 doi: 10.1016/j.jsurg.2020.07.031. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aziz H., James T., Remulla D. Effect of COVID-19 on surgical training across the United States: a national survey of general surgery residents. J Surg Educ. 2020 Jul 30 doi: 10.1016/j.jsurg.2020.07.037. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.ACGME Sponsoring institution emergency categorization. https://acgme.org/COVID-19/Sponsoring-Institution-Emergency-Categorization Available at: