Abstract
Sleep-related complaints are widely prevalent in those with Alcohol Dependence. Alcohol Dependence (AD) is not only associated with insomnia, but also with multiple sleep-related disorders as a growing body of literature has demonstrated.
This manuscript will review the various aspects of insomnia associated with AD. In addition, the association of AD with other sleep-related disorders will be briefly reviewed.
The association of AD with insomnia is bi-directional in nature. The etiopathogenesis of insomnia has demonstrated multiple associations and is an active focus of research. Treatment with cognitive behavioral therapy for insomnia is showing promise as an optimal intervention. In addition, AD may be associated with circadian abnormalities, short sleep duration, obstructive sleep apnea and sleep-related movement disorder.
The burgeoning knowledge on insomnia associated with moderate-to-severe alcohol use disorder has expanded our understanding of its underlying neurobiology, clinical features and treatment options.
Keywords: Alcohol, alcoholism, sleep, sleep initiation and maintenance disorders
Introduction
Moderate-to-severe Alcohol Use Disorder (or Alcohol Dependence [AD]) has been associated with a range of sleep-related disturbances. These disturbances may have direct ramifications on the underlying AD and on the overall health and social well-being of the individual. The last comprehensive review on this topic was published in March 2005 (Stein and Friedmann, 2005).
Over this past decade, knowledge in the field of sleep-related disorders has grown considerably with the evolution of sleep medicine and behavioral sleep medicine as independent sub-specialties, and improved comprehension of sleep disorders and their treatments. Another ramification of this growing body of knowledge is the revision in the diagnostic criteria for sleep disorders. These updated criteria are seen in the third edition of the International Classification of Sleep Disorders (ICSD-3) (AASM, 2014) and the fifth edition of the Diagnostic and Statistical Manual for Psychiatric disorders (DSM-5) (APA, 2013). In this manuscript we will adhere to the ICSD-3 classification for sleep disorders.
This exponential growth in information has also started to change the way we conceptualize and treat insomnia and other sleep-related disturbances associated with AD. It is with these facts in mind that we decided to review this growing body of knowledge. The primary aim of this manuscript is to review the literature related to insomnia associated with AD with a focus on its clinical manifestations, etiology and pathogenesis, and associated treatment interventions. The secondary aim of this manuscript is to briefly review literature on other sleep-related disorders associated with AD that sometimes present as insomnia.
Methods
The selection of manuscripts for this review was conducted in four steps. First, search terms were formulated to cover the effects of alcohol intoxication on sleep, the association of AD with various sleep-related disorders including insomnia, circadian rhythm sleep disorders, breathing-related sleep disorders, sleep-related movement disorders, and parasomnias. Second, appropriate search terms were applied to four different databases, namely Pubmed, Medline, Embase and Google Scholar in order to maximize retrieval of abstracts in the United States, European and other international databases. These searches were limited to human subjects, English language, and studies directly evaluating the relationships of alcohol use/disorder and sleep complaints/disorders. Wherever multiple studies were seen on the same topic, the largest studies and/or the most rigorous studies were evaluated. The dates of the literature were 1/1/1967 to 12/31/2015. Third, the references of the selected manuscripts were reviewed for additional manuscripts in our areas of interest. As a final step we also reviewed the last two literature reviews on this subject along with their references to extract additional manuscripts (Brower, 2001, Stein and Friedmann, 2005). A total of 135 manuscripts were reviewed for this manuscript. See Figure 1 for details. The primary author reviewed the articles and checked the tables for accuracy and consistency. Alcohol’s association with hypersomnia disorders was excluded from this review as it was considered beyond the scope of this current manuscript.
Figure 1.
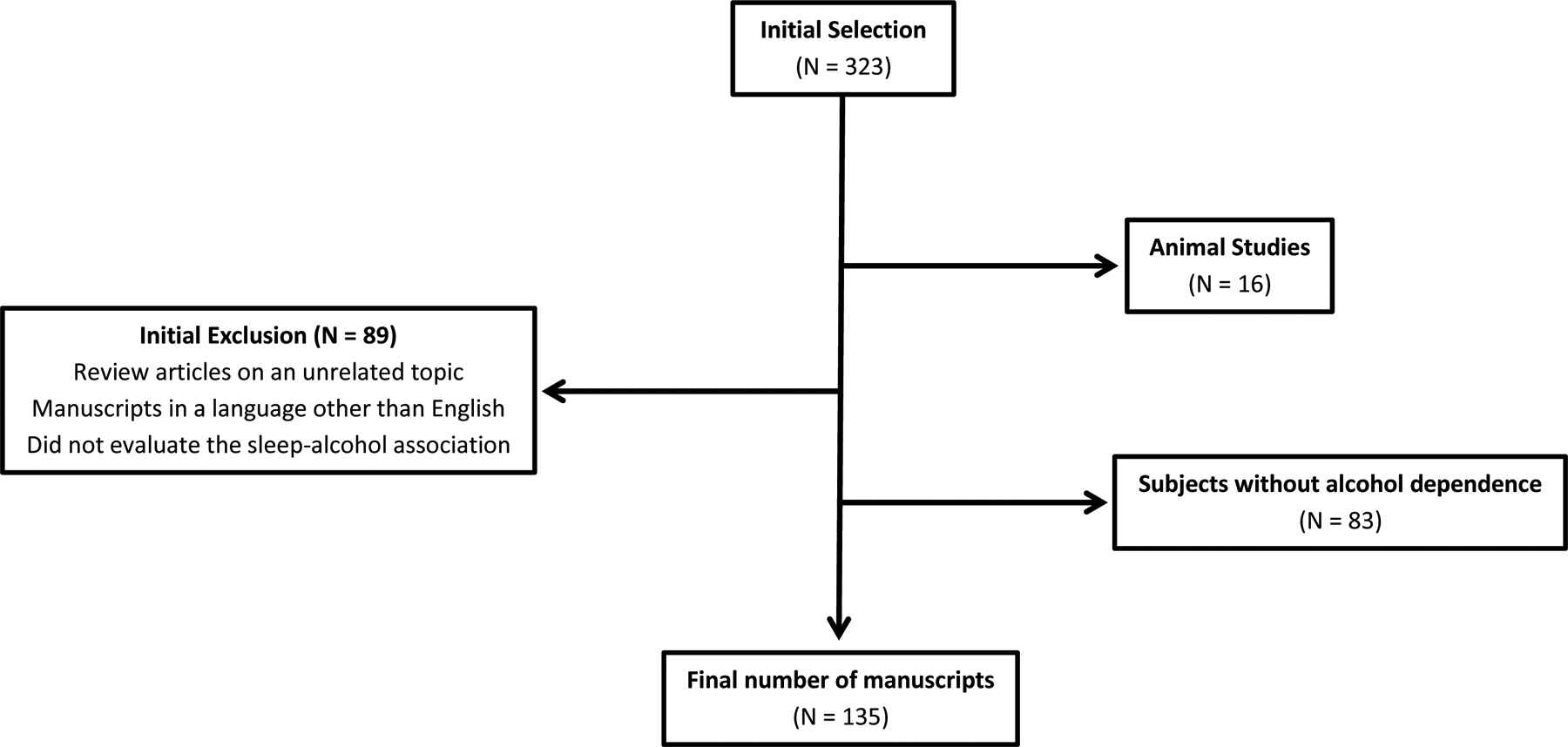
Manuscript selection process for the current review
Results
In healthy subjects, the time lag after lying in bed with the intention to sleep and actual sleep is referred to as sleep onset latency (SOL). Once an individual falls asleep, s/he alternates between two states of sleep - Non-Rapid Eye Movement Sleep (NREM) and Rapid Eye Movement Sleep (REM). NREM is characterized by a succession of stages traditionally called 1 – 4 (Rechtschaffen and Kales, 1968). Slow Wave Sleep (SWS) or deep sleep corresponds to stages 3 and 4 combined. These stages correspond to a progressive increase in the depth of NREM sleep, with an associated decrease in frequency and an increase in amplitude of the brain waves, as measured by sleep electroencephalography (EEG). Nocturnal monitoring of sleep EEG, breathing, and movements in the sleep lab is known as polysomnography (PSG). About 90 minutes after the onset of NREM sleep, a person enters into REM sleep characterized by a decrease in the EEG amplitude (height of the waves), mixed-frequency waves, rapid eye movements and loss of muscle tone (as reflected in a low chin electromyography tone (Iber et al., 2007, Siegel, 2017). Saw-tooth waves may also appear as a superimposed rhythm with a frequency of 2–3 Hz and triangular in shape with the appearance of teeth on a saw (Pearl et al., 2002, Berger et al., 1962). The timing and duration of each state and stage of sleep throughout the night is called sleep architecture. For further information on sleep-related variables see Table 1.
Table 1.
Terminologies used in sleep related assessments
| Term | Description |
|---|---|
| Time in Bed (TIB) | The total time spent in bed |
| Total Sleep Time (TST, min) | The total duration of sleep through the night |
| Sleep Efficiency (SE, %) | The percentage of time spent sleeping through the night, i.e. TST/TIB |
| NREM sleep | The initial part of sleep; consists of stages 1, 2 and slow wave sleep (SWS); quiet sleep; about 80% of sleep |
| Stage 1 (N1) sleep | Consists of slow eye movements, and waves with low amplitude and predominantly 4–7 Hz activity |
| Stage 2 (N2) sleep | The sleep stage characterized by the onset of sleep spindles and K complexes |
| Slow Wave (N3) Sleep (stages 3 & 4) | The presence of low frequency and high amplitude delta waves (0.5–2Hz) for ≥ 20% of the epoch |
| REM sleep | Sleep with low amplitude and mixed frequency waveforms, rapid eye movements and low muscle tone |
| Sleep Onset Latency (min) | Time from “lights out” until the onset of sleep |
| REM Onset Latency (min) | Interval of time from sleep onset to the appearance of the first epoch of REM sleep |
| Stage 1 % | The percentage of time in sleep that is spent in Stage 1 sleep, i.e. 100 X total Stage 1 sleep/TST; usually about 4–5% |
| Stage 2% | The percentage of time in sleep that is spent in Stage 2 sleep, i.e. 100 X total Stage 2 sleep/TST; usually about 45–55% |
| Slow Wave Sleep (SWS) % | The percentage of time in sleep that is spent in SWS sleep, i.e. 100 X total SWS sleep/TST; usually about 16–21% |
| REM % | The percentage of time in sleep that is spent in REM sleep, i.e. 100 X total REM sleep/TST; usually about 20–25% |
| Apnea Hypopnea Index (AHI, #/Hour) | The number of apneas and hypopneas through the night, i.e. total number of apneas and hypopneas/TST (in hours) |
| Periodic Limb Movement | Limb movements with an amplitude of ≥ 8 μV, lasting 0.5–10 seconds, 5–90 sec apart, and ≥ 4 in a row |
| Periodic Limb Movement Index (number/hour) | The number of periodic limb movements during sleep/TST. |
| Phase Advance | Shift of the sleep cycle to an earlier time during the 24-hour period |
| Phase Delay | Shift of the sleep cycle to a later time during the 24-hour period |
Information gathered from the following sources: 1) The AASM Manual for the scoring of Sleep and Associated Events, AASM, 2007; 2) http://www.sleepnet.com/definition.html (Updated for the scoring criteria replacing Stages 1–4 with N1–N3, from the American Academy of Sleep Medicine, 2012.)
In addition to the electrophysiologic mechanisms of sleep, Borbely and colleagues postulated a two-process model of sleep regulation (Borbely, 1982). In brief, this model posits that sleep is a function of two independent mechanisms, namely homeostatic sleep drive and circadian rhythmicity. The homeostatic mechanism is responsible for a build-up of the sleep drive with continued wakefulness through the day, whereas the circadian mechanism is responsible for maintenance of wakefulness and is influenced by zeitgebers such as ambient light and meal times. One or both mechanisms may be weakened or abnormal in insomnia. A mismatch between the normally synergistic circadian and homeostatic mechanisms may also lead to circadian rhythm sleep disorders.
Alcohol and its effect on sleep continuity in healthy subjects
The alcohol level in blood is determined by gender, weight, number of drinks consumed over a unit of time, and rate of metabolism. It is generally metabolized at a rate of 0.01 to 0.02 g% per hour (Arnedt et al., 2011b). When alcohol is consumed before bedtime, its effects on sleep architecture also differ based on the ascending or peak concentrations during the first 3–4 hours of the night (first half of the night) as compared to the descending phase of blood alcohol levels during the next 3–4 hours of sleep (second half of the night).
The effect of moderate and heavy alcohol on sleep in healthy adults has been investigated across multiple studies although most of these studies were limited with their small sample sizes. With moderate doses of alcohol (< 1 g/Kg), the only consistent PSG sleep finding has been decreased REM sleep duration (Williams et al., 1983, Miyata et al., 2004, Roehrs et al., 1991). Analysis of sleep across the first half of the night did not demonstrate any consistent changes in PSG sleep. In the second half of the night, the consistent finding was decreased REM sleep duration (Rundell et al., 1972, Miyata et al., 2004). Recently, Arnedt and colleagues conducted one of the largest studies of sleep in heavy drinking healthy adults. They demonstrated that alcohol at a dose of > 1 g/Kg, as compared with placebo, decreased SOL and sleep efficiency (SE; percentage of time in bed spent sleeping), and increased wake after sleep onset time (WASO). Alcohol’s effect on sleep architecture was to increase the percentage of slow wave sleep (SWS%), stage 2 sleep, and REM latency, and to decrease REM%. During the 1st half of the night, alcohol as compared to placebo, increased Total Sleep Time (TST) and SE, and decreased the number and duration of awakenings. But, during the 2nd half of the night, TST and SE were decreased, with an increased number and duration of awakenings (Arnedt et al., 2011b). Similar findings of sleep disruption have been demonstrated in late adolescence (Chan et al., 2013), although their EEG power spectra analysis after alcohol consumption demonstrated simultaneous increases in frontal delta and alpha powers during the earlier part of sleep, which may lead to sleep disturbance (Chan et al., 2015). Lastly, consumption of alcohol earlier in the evening and despite an undetectable breath alcohol level showed sleep to be superficial (subjectively) and with high frequency EEG activity (objectively), thus demonstrating an increased arousal within their sleep (Landolt et al., 1996).
In summary, moderate doses of alcohol may decrease the amount of REM sleep through the night. In doses mimicking heavy drinking, alcohol may initially improve sleep continuity during the first half of the night. But in the second half of the night, it may lead to fragmented sleep (more awakenings). Further, alcohol may continue to disturb sleep even after the breath alcohol concentration is undetectable.
Insomnia
Introduction.
Insomnia is the most investigated sleep disorder, although some of these studies have evaluated insomnia symptoms in lieu of it as a disorder. Insomnia disorder as defined by the ICSD-3 requires the presence of ≥ 1 of the following complaints: difficulty initiating sleep, difficulty maintaining sleep, or waking up earlier than desired. These symptoms are associated with ≥ 1 of the following impairments: fatigue or malaise, attention or memory problems, impairment of psychosocial functioning, mood disturbance, daytime sleepiness, behavioral problems, reduced motivation or energy, proneness for errors, and concern or dissatisfaction with sleep. These complaints must occur despite adequate opportunity and circumstances for sleep and are present for most nights of the week for ≥ 3 months (AASM, 2014). The criteria for insomnia disorder in DSM-5 are nearly identical.
Alcohol Dependence (AD)
Insomnia or sleep disturbance is widely prevalent in alcohol dependence. The prevalence estimates range from 36–91% (Mello and Mendelson, 1970, Brower et al., 2001b, Chaudhary et al., 2015, Baekeland et al., 1974, Cohn et al., 2003). Alcohol dependence may be categorized into different stages based on the temporal relationship with exposure to alcohol. Insomnia has been associated with all these stages and is briefly reviewed below, taking into account different populations, wherever applicable.
During Active Alcohol Use
A. Treatment Seeking AD subjects –
There is a limited body of literature on insomnia associated with active alcohol use in AD. These studies may be categorized based on their use of subjective or objective measures: a) Subjective measures. The prevalence rate of insomnia was 74% in a recent study that used the Insomnia Severity Index (Chaudhary et al., 2015). In one study, 30% of the subjects were actively drinking during treatment. They complained of increased sleep latency and fragmentation of their sleep (Skoloda et al., 1979). In another investigation, staff assessments in an inpatient rehabilitation unit demonstrated that those who continued to drink had sleep fragmentation and a reduction of their TST (Mello and Mendelson, 1970); b. Objective measures. PSG sleep studies in subjects with AD and alcohol consumption also found increased SOL and decreased TST, and sleep architectural changes including decreased REM sleep duration and increased REM sleep latency and SWS (Gross et al., 1973, Gross and Hastey, 1975). These findings contrast with another study where increased TST with alcohol consumption was seen (Allen et al., 1980).
B. Non-treatment seeking problem drinkers –
In a recent study of non-treatment seeking problem drinkers in the community (N = 295), Hartwell and colleagues used the Pittsburgh Sleep Quality Index (PSQI) (Hartwell et al., 2015) to demonstrate a 76% prevalence rate of sleep disturbance. They defined sleep disturbance using a PSQI total score > 5. In addition, they also used a 3-factor scoring model to evaluate insomnia; these factors consisted of sleep efficiency, perceived sleep quality and daily disturbances. This sleep disturbance was positively associated with alcohol problem severity.
C. Veterans –
In a chart review of Veterans with AD (N = 84), insomnia symptoms included increased SOL (72±67 minutes), and WASO time (82±13 minutes), and poor sleep quality in 63% of patients. These insomnia symptoms were prevalent for 75±123 months (Chakravorty et al., 2013). One of the strongest predictor of insomnia symptoms was the presence of psychiatric disorder (OR = 20.8).
In summary, the preponderance of studies report subjective and objective increase in sleep onset latency and sleep fragmentation with consequently decreased TST in actively drinking subjects with AD.
During Acute Withdrawal
The withdrawal phase after acute cessation of sustained alcohol use lasts about 1–2 weeks with a prevalence rate of sleep complaints that is variable. Steinig and colleagues demonstrated that 92% of inpatients with AD acutely withdrawing from alcohol had sleep disturbance (Steinig et al., 2011). In a study of Brazilian subjects undergoing inpatient alcohol detoxification (N = 58), subjective sleep disturbance was prevalent in all women (100%, 13/13) and most men, 88.9% (40/45) (Escobar-Cordoba et al., 2009). In another investigation involving subjects in a residential treatment program, the symptom of “inability to sleep” differed in prevalence across race and ethnicity. In this treatment-seeking sample of male patients, the prevalence was the lowest in Blacks (54%), highest in Whites (82%), and with an intermediate prevalence of 65% in Mexican-Americans males (Caetano et al., 1998).
These insomnia symptoms may improve with time as the detoxification progresses. Bokstrom and colleagues demonstrated a decrease in the mean ± S.D. insomnia scores from 1.3 ± 1.1 (N = 48) to 0.8 ± 1.0 (N = 13), p = 0.01 for days 0 versus 7 after last alcohol use during inpatient detoxification (Bokstrom and Balldin, 1992). In the general population, the prevalence rate of insomnia as a withdrawal symptom was 32% among alcohol-dependent individuals (Brower and Perron, 2010).
In patients with delirium tremens (DTs), a higher percentage of Stage 1 sleep with REM (stage 1 period with low voltage EEG with REM) was demonstrated (Greenberg and Pearlman, 1967). In this study, one of the subjects had nightmares of hallucinatory intensity during alcohol withdrawal and with 100% Stage 1-REM sleep. As DTs ended, recovery sleep set in as a response to sleep deprivation in most of these patients. However, a subset of patients may have fragmented sleep and disturbances of consciousness that predict a guarded prognosis for future episodes of DTs (Kotorii et al., 1982, Nakazawa et al., 1981).
During Recovery From Alcohol Use
Early Recovery (2–8 weeks after detoxification) –
Some studies have reported a mild withdrawal syndrome persisting after the cessation of an acute withdrawal phase. This condition may be secondary to a hyperexcitable state of the central nervous system (Begleiter and Porjesz, 1979) and has been called protracted abstinence, protracted withdrawal phase, or late withdrawal symptoms (Heilig et al., 2010). Its main features include, mood disturbance, alcohol craving and sleep related disturbances, and they may persist for about 5 weeks (Alling et al., 1982).
Sleep problems are common during this phase and may be prevalent in about 65% of individuals during this phase (Brower et al., 2001a, Kolla et al., 2014). Subjective complaints in those with insomnia as compared to those without include longer SOL, increased WASO and lower sleep efficiency (Brower et al., 2001a, Conroy et al., 2006b). PSG sleep findings during the first 8 weeks of abstinence include increased SOL and stage 1 sleep and decreased TST and SWS % (Gillin et al., 1990b, Gillin et al., 1990a, Moeller et al., 1993, Le Bon et al., 1997, Brower et al., 2001a). REM sleep findings have been inconsistent during this phase with some studies reporting a decreased REM sleep latency and increased REM % (Gillin et al., 1990a, Williams and Rundell, 1981) whereas other studies did not (Gillin et al., 1990b, Le Bon et al., 1997). It is to be noted that individuals in early recovery may overestimate their subjective SOL but underestimate their WASO, as compared to their PSG estimated indices (Conroy et al., 2006b).
Those who relapse to alcohol use during treatment may have more disturbed sleep, as compared to abstainers (Brower, 2003, Currie et al., 2004, Conroy et al., 2006a, Smith et al., 2014). In contrast, two studies have failed to demonstrate such a relationship with subjective insomnia (Jakubczyk et al., 2013) (Feige et al., 2007) as measured by the Athens Insomnia Scale and PSQI, respectively; although the latter study demonstrated an association of relapse with increased sleep EEG β2 spectral power. It is possible that use of alcohol as a sleep aid rather than sleep disturbance is associated with relapse, as demonstrated in a recent study (Kolla et al., 2015).
Sustained Recovery (≥ 3 months beyond detoxification phase) –
Subjective and objective sleep related disturbances persist for up to 3 years into sobriety as demonstrated by cross-sectional and longitudinal studies. Subjective complaints of insomnia may persist up to 2 years into sobriety (Cohn et al., 2003, Wellman, 1954, Kissin, 1979). Longitudinal studies evaluating PSG sleep have demonstrated the presence of increased SOL and sleep fragmentation, a decreased TST, and, abnormalities in SWS and REM sleep stages. Although increased SOL reached normal levels by 5–9 months into recovery, sleep fragmentation persisted for 21 months and consequently TST was seen to normalize in ≤ 2 years (Adamson and Burdick, 1973, Williams and Rundell, 1981, Drummond et al., 1998). Slow wave sleep is decreased early in recovery and gradually normalizes over time and around 2 years of sobriety (Williams and Rundell, 1981, Imatoh et al., 1986, Drummond et al., 1998).
There is some inconsistency in the literature relating to REM sleep abnormalities during sustained recovery. In one study, REM sleep architecture demonstrated a reversal during early recovery, with the first REM sleep episode of the night being the longest, despite a lack of depressive disorder in these subjects. The REM sleep architecture normalized over time with continued recovery (Imatoh et al., 1986). This phenomenon may suggest a normalization of the acrophase of REM sleep with sobriety and may also account for increased REM % during early recovery. In a frequently cited study, decreased REM sleep latency and increased REM % was seen at 27 months into recovery (Drummond et al., 1998). These findings contrast with lack of REM sleep abnormalities reported in 2 other studies, as compared to healthy control subjects (Williams and Rundell, 1981, Schiavi et al., 1995). Discrepancies in REM sleep may reflect sample differences, duration of sobriety (where the REM sleep may have normalized over time) (Williams and Rundell, 1981), or an interaction between REM sleep architecture and a circadian disruption (Imatoh et al., 1986).
Other information on sleep in recovering alcoholics
Sleep Hygiene –
Poor sleep hygiene may perpetuate insomnia. Napping was common during recovery in one study resulting in longer WASO times, decreased TST and lower SE (Currie et al., 2003a).
Dreams and Nightmares –
Dreams and nightmares may lead to insomnia and sleep fragmentation. In a study of subjects with AD during acute alcohol detoxification, in addition to a poor sleep quality, only 21% had dreams about alcohol. Dream content was described as “strange, foreign” and as if “from another world”. As abstinence progressed, dreams became less strange and aggressive (Steinig et al., 2011). An unreplicated finding is that drinking-related dreams were positively associated with length of abstinence (Choi, 1973).
Epidemiology of Insomnia in Alcohol Dependence
There is a growing body of literature demonstrating a bidirectional relationship of insomnia with alcohol consumption and alcohol misuse.
Sleep problems and future alcohol use.
Retrospectively, subjects with AD reported the presence of insomnia prior to the onset of AD (Currie et al., 2003a). Sleep disturbance has been shown to predict subsequent alcohol consumption in adolescents and adults (Breslau et al., 1996, Wong et al., 2004, Wong et al., 2010, Wong et al., 2015, Ford and Kamerow, 1989, Weissman et al., 1997). This association may be secondary to subjects self-medicating their insomnia with alcohol (Kaneita et al., 2007, Ancoli-Israel and Roth, 1999, Johnson et al., 1998).
Does AD lead to Insomnia?
In a longitudinal Swedish study (N = 2602), having alcohol dependence (CAGE questionnaire total score of ≥ 2) was associated with subsequent insomnia symptoms (OR = 1.75, 95% CI: 1.2–2.5) (Janson et al., 2001). Similarly, respondents with chronic alcohol dependence (N = 248) during longitudinal follow-up, were more likely to report insomnia symptoms as compared to those who had remitted (N = 211) during the follow-up period (OR = 2.6, 95% CI: 1.1–6.0) (Crum et al., 2004).
What are the ramifications of insomnia in AD?
Prior cross-sectional and longitudinal studies have demonstrated the following associations with AD: a) Relapse to drinking (Brower, 2003, Currie et al., 2003b, Conroy et al., 2006a); b) Higher psychosocial problems related to the drinking, including recent employment problems, conflicts with others in their environment and with impulse control (Zhabenko et al., 2012, Chaudhary et al., 2013, Chaudhary et al., 2015); c) Decreased self-reported quality of life (Zhabenko et al., 2012, Cohn et al., 2003); d) Recent and lifetime suicidal ideation (Klimkiewicz et al., 2012, Chaudhary et al., 2015); and, e) Insufficient sleep duration (John et al., 2005). The recommended range of sleep duration to support optimal health in adults is 7–9 hours (Consensus Conference et al., 2015). Sleep duration ≤ 6 hours a night has been linked with an increased risk for mortality, injuries, cardio-metabolic and psychiatric problems as well as suicide in adults (Consensus Conference et al., 2015).
What are the risk factors for insomnia/Sleep problems?
Demographic and other covariates –
a) Age – Older age was associated with better subjective sleep quality in 2 studies (Chakravorty et al., 2013, Kolla et al., 2014), although it was inversely associated with objective PSG sleep continuity measures (Gillin et al., 1990b, Brower and Hall, 2001); b) relatively lower education (Zhabenko et al., 2012); c) marital/partner status – those who were single (Chakravorty et al., 2013, Perney et al., 2012); d) monetary problems (Zhabenko et al., 2012); e) severity of alcoholism (Brower et al., 2001a, Hartwell et al., 2015, Zhabenko et al., 2012); f) frequency of alcohol use (Zhabenko et al., 2012) although one study did not replicate this association (Currie et al., 2003a); and, g) a history of sexual or physical abuse (Zhabenko et al., 2012).
Family history of alcoholism –
children and adolescents of parents with AD have demonstrated lower delta power in their NREM sleep, greater power in the alpha frequencies in NREM and REM spectral PSG studies, and a shorter sleep duration (Tarokh and Carskadon, 2010, Dahl et al., 2003, Conroy et al., 2015, Schuckit and Bernstein, 1981).
Biomarkers of insomnia –
a few biomarkers that have been evaluated have included the following: a) Spectral PSG Studies. High frequency EEG activity in the beta and gamma range is increased in those with primary insomnia (Perlis et al., 2001a, Perlis et al., 2001b); b) Studies evaluating Autonomic Activity. Increased sympathetic activity with simultaneously decreased activity of the parasympathetic nervous system, especially during the first 4 hours of the night was seen in those with AD and sleep disturbance (Irwin et al., 2006, de Zambotti et al., 2014). A recent study has demonstrated that autonomic nervous system activity may improve with sustained recovery (de Zambotti et al., 2015); c) Cytokines. Cytokines such as Interleukins (IL) and Tumor Necrosis Factor (TNF) are humoral factors associated with sleep regulation (Krueger and Toth, 1994, Krueger et al., 1998). Studies in subjects with AD, as compared to controls, have demonstrated a decreased production of Interleukin (IL) - 6 in the early part of the night, suppression of the Il-6/IL-10 through the night, increased nocturnal levels along with greater increases in IL-6 and TNF-α levels with partial sleep deprivation (Redwine et al., 2003, Irwin and Miller, 2000). Etanercept, a TNF-α antagonist medication, has been shown to decrease the amount and % of REM sleep to a comparable level to age-comparable control subjects (Irwin et al., 2009). Thus, studies involving spectral sleep studies and autonomic activity suggest an increased arousal in sleep disturbance.
Genetic Studies.
There is an emerging interest in the associations between AD and circadian clock genes. In a Polish sample of individuals with AD (N = 285), PER3 4/4 homozygotes reported the highest insomnia scores, PER3 5/5 genotype the lowest, and the heterozygotes PER4/5 had an intermediate score (Brower et al., 2012).
A Conceptual Model for Insomnia in AD
Sleep and wakefulness are two parallel and competing processes. Sleep onset occurs when there are increased homeostatic (sleep-promoting) and decreased circadian (wake-promoting) drives (Borbely, 1982). From a general neurophysiological perspective, the onset and maintenance of sleep involves depolarizations of the thalamocortical neural circuits (Saper et al., 2010). The ‘sleep-wake switching system’ resides within the lateral hypothalamus, the ventrolateral preoptic area, and the median preoptic area. In contrast to generalized sleep activity across the brain, “local” sleep involves activities in certain neurons or neuronal assemblies leading to regional sleep-like neuronal activity patterns. These activities are then propagated to other brain regions via signaling systems. Insomnia results from a mismatch involving persistent activity in wake-promoting structures during NREM sleep, leading to simultaneous sleep and wake activity along with psychophysiological arousal (Buysse et al., 2011). From a clinical perspective, insomnia occurs in vulnerable patients with predisposing factors, such as having a family history of AD or certain genetic traits. Acute insomnia is triggered in them by stress promoting events (precipitating factors). This acute insomnia becomes persistent because of perpetuating factors such as reading in bed (Spielman et al., 1987) or drinking alcohol. Figure 2 presents a conceptual model for insomnia in AD during recovery.
Figure 2. A conceptual model of insomnia in alcohol dependence.
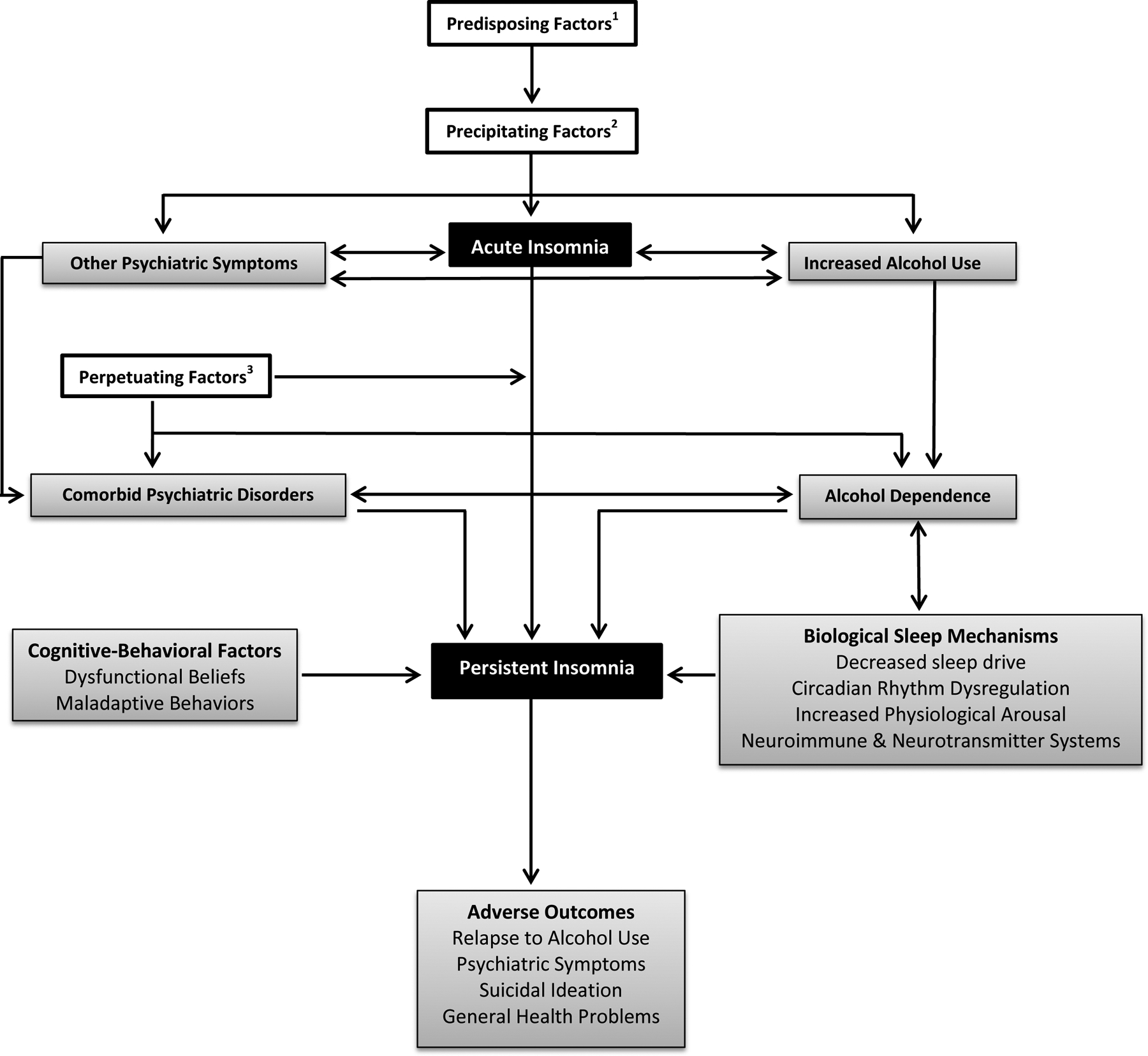
Legend: 1 Predisposing Factors: Familial AD, genetic (clock gene polymorphism), chronotype (evening type), childhood trauma, childhood sleep problems; 2 Precipitating Factors: Acute life events or psychosocial stressors; 3 Perpetuating Factors: Compensatory behaviors that are adopted by the individual in order to cope with the insomnia, but that actually reinforce the sleep problem. These factors can include the practice of non-sleep behaviors in the bedroom, staying in bed while awake, watching television or reading while in bed, and spending excessive amounts of time in bed (Spielman et al., 1987).
Treatments for Insomnia in AD
Despite the prevalence of insomnia in those with AD, it is not aggressively treated (Friedmann et al., 2003). We have summarized the pharmacologic and behavioral treatments for insomnia in AD in Table 2. These studies have been reviewed in more detail elsewhere (Brooks and Wallen, 2014, Brower, 2016, Kolla et al., 2011a). Medication treatments have demonstrated mixed efficacy. Trazodone was demonstrated to increase alcohol use in one randomized, placebo-controlled trial (Friedmann et al., 2008), although this finding was not replicated in an observational study (Kolla et al., 2011b). Similarly, Brower and colleagues did not demonstrate any superiority of gabapentin over placebo, although Mason and colleagues did report an improvement. In their study of non-treatment seeking patients with AD, Mason and colleagues demonstrated an improvement in sleep quality for those treated with gabapentin (1200 mg a day), as compared to placebo, and after 1 week of treatment, with a mean difference of – 2.38, p < 0.05 favoring gabapentin (Mason et al., 2009). In a follow up larger study, the authors replicated the finding of an improvement in sleep quality with gabapentin. It is to be noted that in this latter study, some of the subjects in the treatment arms did not meet criterion for sleep disturbance at baseline (Mason et al., 2014). In a randomized, placebo-controlled trial of heavy drinking subjects with AD (N = 224), quetiapine XR at a dose of 400 mg a day improved sleep quality, as compared to placebo (Litten et al., 2012). Behavioral treatments for insomnia have demonstrated consistent efficacy with moderate to large effect sizes, although these studies have small sample sizes and employed modified versions of CBT-I, such as CBTI-AD (Brooks and Wallen, 2014).
Table 2.
Pharmacologic and behavioral treatments for insomnia in alcohol dependence
| Authors | Selected for insomnia | N | RCT | Daily Dose, Treatment Duration | Primary Outcome Measure | Time Since Last Drink | Effect on Insomnia | Effect on Drinking |
|---|---|---|---|---|---|---|---|---|
| PHARMACOLOGIC | ||||||||
| Acamprosate | ||||||||
| (Staner et al., 2006) | No | 24 | Yes | 1998 mg/day; 23 days | PSG | 0 | ↓ | ↓ |
| (Perney et al., 2012) | Yes1 | 239 | Yes | 2–3 gm/day; 6 months | Short Sleep Index | ≤ 10 days | ↓ | ? ↓ |
| Agomelatine | ||||||||
| (Grosshans et al., 2014) | Yes | 9 | No | 25–50 mg/day; 6 wks | Sleep Quality | NA | ↓ | NA |
| Chlormethiazole | ||||||||
| (Gann et al., 2004) | No | 20 | Yes | Taper protocol; 5 days | PSG | 0 | ↑ | NA |
| Gabapentin | ||||||||
| (Karam-Hage and Brower, 2000) | Yes | 15 | No | Gabapentin 200 – 1500 mg; 4–6 wks | SPQ | 4 wks | ↓ | ↓ |
| (Karam-Hage and Brower, 2003) | Yes | 50 | No | Gabapentin (888±418 mg) or Trazodone (105±57 mg); 4–6 wks | SPQ | ≥ 4 wks | ↓ G > T | ↓ (Two subjects in each group) |
| (Malcolm et al., 2007) | No | 68 | Yes | Gabapentin/lorazepam taper | Insomnia questions2 | 0 | ↓ (G > L) | ∅ |
| (Brower et al., 2008) | Yes | 21 | Yes | 1500 mg; 6 wks | PSG | ≥ 1 week | ∅ | ↓ |
| Quetiapine XR | ||||||||
| (Chakravorty et al., 2014) | Yes | 20 | Yes | 400 mg; 8 wks | PSG | ≥ 1 month | ↓ | NA |
| Ramelteon | ||||||||
| (Brower et al., 2011) | Yes | 5 | No | 8 mg; 4 wks | ISI | 2–13 wks | ↓ | Lapse to HD (N=1) |
| Trazodone | ||||||||
| (Le Bon et al., 2003) | Yes | 18 | Yes | 150–200 mg; 4 wks | PSG | ≥ 2 wks | ↓ | NA |
| (Friedmann et al., 2008) | Yes | 173 | Yes | 50–150 mg; 12 wks | Sleep Quality | Day 3–5 post-detox | ↓ | ↑ |
| Triazolam | ||||||||
| (Fabre et al., 1977) | Yes | 12 | No | 0.5 – 1.0 mg; 28 days | Sleep diary & Q | 5–15 days | ↓ | ? ↓ |
| BEHAVIORAL | ||||||||
| Authors | Selected for insomnia | N | RCT | Treatment Duration | Primary Outcome Measure | Time Since Last Drink | Effect on Insomnia | Effect on Drinking |
| PR | ||||||||
| (Greeff and Conradie, 1998) | Yes | 22 | Yes | 2 wks | Quality of Sleep | ≥ 1 month in RTP | ↓ | NA |
| CBT-I | ||||||||
| (Currie et al., 2004) | Yes | 60 | Yes | 7 wks | Sleep diary | ≥ 1 month | ↓ | ∅ |
| (Arnedt et al., 2007) | Yes | 7 | No | 8 wks | Sleep diary | 27–433 days | ↓ | ↓ |
| (Arnedt et al., 2011a) | Yes | 17 | Yes | 8 wks | Sleep diary | 8–433 days | ↓ | ∅ |
Legend: Selection criteria = studies with sleep as the primary outcome;
this was the secondary aim of this manuscript, which is in itself a secondary analysis of data from a clinical trial;
insomnia questions from the CIWA (Clinical Institute Withdrawal Assessment Scale for Alcohol – Revised) and BDI (Beck Depression Inventory) questionnaires; N = number of subjects in the study; RCT = Randomized-controlled trial; SPQ = Sleep Problems Questionnaire; PSG = Polysomnography; G = Gabapentin; T = Trazodone; L = Lorazepam; wks = weeks; ISI = Insomnia Severity Index; RTP = Residential Treatment Program; Q = Questionnaire; HD = Heavy Drinking; ↑ = increased; ↓ = decreased; ? = unknown effect; NA = not applicable as not investigated; ∅ = no difference; day 3–5 post-detox = evaluated after 3–5 day detoxification protocol; PR = Progressive Relaxation (including muscle relaxation); CBT-I = Cognitive Behavioral Therapy for Insomnia.
In summary, insomnia is prevalent across all stages of AD and may have psychosocial, addiction and psychiatric ramifications. “Although some encouraging results have been seen with gabapentin, quetiapine and CBT-I, these findings need to be replicated using adequately powered studies in individuals with insomnia comorbid with alcohol dependence”.
Alcohol Dependence and Insomnia Associated with Other Sleep Disorders
Other primary sleep disorders may occur more commonly with AD and present as insomnia in the clinical setting. These include obstructive sleep apnea (OSA), periodic limb movement disorder (PLMD), and delayed phase sleep disorder (DSPD). AD has also been linked with periodic limb movement disorder, circadian rhythm abnormalities, and obstructive sleep apnea, which are discussed below. There is a lack of evidence that alcohol consumption is a trigger for sleepwalking (Pressman et al., 2007), although it has been linked epidemiologically to night terrors, which is another parasomnia (Ohayon et al., 1999).
Alcohol Dependence and Period Limb Movement Disorder (PLMD).
The patient with PLMD may present with disturbed sleep and resultant impairment of functioning, which are not explained by another sleep/medical/neurologic/psychiatric disorder (AASM, 2014). It is diagnosed with polysomnography using a criterion of > 15 repetitive limb movements per hour of sleep in adults, mostly in the lower extremities. PLMD is associated with restless legs syndrome (Fulda, 2015) and may masquerade as insomnia.
Among those with AD, treatment-seeking subjects have been demonstrated to have a higher Periodic Limb Movement Index (PLMI) as compared to controls (Brower and Hall, 2001). A longitudinal study involving patients sober for 2–3 weeks after withdrawal, demonstrated higher baseline PLMI and PLMI with arousals versus healthy controls (Gann et al., 2002). At the 6-month follow-up, subjects with AD who relapsed had significantly higher PLMI and PLMI with arousals, than those who did not. Conversely, another study failed to find a difference in PLMI between those with AD in early recovery and controls (Le Bon et al., 1997). Magnesium supplementation had a mixed result on PLMs in an open-label trial of AD patients (Hornyak et al., 2004).
Alcohol and Circadian Rhythm Sleep-Wake Disorders.
Circadian rhythms are a manifestation of the activity of the primary endogenous pacemaker, the suprachiasmatic nucleus in the hypothalamus, upon which melatonin acts. Dim Light Melatonin Onset (DLMO) is a commonly used marker for evaluating the activity of the circadian pacemaker and for assessing the changes in circadian phase, i.e. delayed or advanced (Pandi-Perumal et al., 2007). The peak of the salivary melatonin curve occurs around 2AM in middle-aged males (Zhou et al., 2003). This peak may be blunted or delayed in those with AD (Kuhlwein et al., 2003). Consequently, AD subjects may be more likely to manifest a delayed phase type disorder, which may present as difficulty falling asleep.
Alcohol and Obstructive Sleep Apnea (OSA).
Alcohol use and AD have been associated with OSA in prior studies. Alcohol can impair normal breathing by impairing the normal arousal response to airway obstruction and by relaxing the upper airway musculature, leading to initiation or worsening of existing snoring, sleep-disordered breathing (SDB) and sleep fragmentation (Peppard et al., 2007, Vitiello, 1997, Sakurai et al., 2007).
In one study, subjects with AD in acute withdrawal demonstrated a higher intensity of respiratory events in their sleep (12.6 ± 12.3 events/hour), as compared to healthy controls (3.6 ± 3.4 events/hour) (Le Bon et al., 1997). In another study, a higher prevalence rate of SDB was seen in treatment-seeking patients with AD (41%), as compared to control subjects (23%). In this study, SDB was a significant contributor to sleep disturbance in a substantial proportion of male AD subjects above the age of 40 years (Aldrich et al., 1993). To the best of our knowledge, there is no data on the association of AD with central sleep apnea in the absence of other risk factors, such as comorbid congestive heart failure and opioid use.
Discussion
A growing body of literature has demonstrated an association between AD and sleep-related disorders. The preponderance of this literature is on insomnia. Insomnia is being increasingly evaluated as a disorder of inappropriate arousal during sleep associated with involvement of multiple underlying mechanisms, and downstream cognitive and behavioral manifestations. In addition, the role of circadian factors and sleep drive mechanisms in mediating and moderating insomnia are being recognized. The implications of this understanding have been the use of behavioral interventions for its treatment and the role of newer medications such as ramelteon, which may also have the ability to advance circadian phase (Richardson et al., 2008). In addition, AD is being increasingly implicated with insufficient sleep duration, obstructive sleep apnea, and periodic limb movement disorder.
One of the limitations associated with prior literature is assessment of insomnia symptoms rather than insomnia as a disorder in people with AD. This may stem from the difficulty in distinguishing alcohol-induced insomnia from other causes of insomnia. Other limitations include small sample sizes, use of different assessment instruments across studies, lack of PSG to rule out other alcohol-associated sleep disorders, and heterogeneous samples with and without insomnia in PSG or treatment studies of recovering AD patients. Future studies should investigate the underlying mechanisms of insomnia in AD, the role of pharmacologic and behavioral treatments of insomnia using PSG, and the relationships of AD with other sleep disorders such as parasomnias.
Supplementary Material
Acknowledgments
The study was supported by VA grant IK2CX000855 (S.C.). The content of this publication does not represent the views of the University of Pennsylvania, Department of Veterans Affairs, the United States Government, or any other institution. None of the authors report any actual or potential conflict of interest with this current manuscript.
References
- AASM (2014) International Classification of Sleep Disorders - Third Edition, Darien, IL 60561. [Google Scholar]
- Adamson J, Burdick JA (1973) Sleep of dry alcoholics. Archives of general psychiatry 28:146–149. [DOI] [PubMed] [Google Scholar]
- Aldrich MS, Shipley JE, Tandon R, Kroll PD, Brower KJ (1993) Sleep-disordered breathing in alcoholics: association with age. Alcohol Clin Exp Res 17:1179–1183. [DOI] [PubMed] [Google Scholar]
- Allen RP, Wagman AM, Funderburk FR, Wells DT (1980) Slow wave sleep: a predictor of individual differences in response to drinking? Biol Psychiatry 15:345–348. [PubMed] [Google Scholar]
- Alling C, Balldin J, Bokstrom K, Gottfries CG, Karlsson I, Langstrom G (1982) Studies on duration of a late recovery period after chronic abuse of ethanol. A cross-sectional study of biochemical and psychiatric indicators. Acta Psychiatr Scand 66:384–397. [DOI] [PubMed] [Google Scholar]
- Ancoli-Israel S, Roth T (1999) Characteristics of insomnia in the United States: results of the 1991 National Sleep Foundation Survey. I. Sleep 22 Suppl 2:S347–353. [PubMed] [Google Scholar]
- APA (2013) Diagnostic and statistical manual of mental disorders : DSM-5. 5th ed., American Psychiatric Publishing, Washington, D.C. [Google Scholar]
- Arnedt JT, Conroy D, Rutt J, Aloia MS, Brower KJ, Armitage R (2007) An open trial of cognitive-behavioral treatment for insomnia comorbid with alcohol dependence. Sleep Med 8:176–180. [DOI] [PubMed] [Google Scholar]
- Arnedt JT, Conroy DA, Armitage R, Brower KJ (2011a) Cognitive-behavioral therapy for insomnia in alcohol dependent patients: a randomized controlled pilot trial. Behav Res Ther 49:227–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnedt JT, Rohsenow DJ, Almeida AB, Hunt SK, Gokhale M, Gottlieb DJ, Howland J (2011b) Sleep following alcohol intoxication in healthy, young adults: effects of sex and family history of alcoholism. Alcohol Clin Exp Res 35:870–878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baekeland F, Lundwall L, Shanahan TJ, Kissin B (1974) Clinical correlates of reported sleep disturbance in alcoholics. Q J Stud Alcohol 35:1230–1241. [PubMed] [Google Scholar]
- Begleiter H, Porjesz B (1979) Persistence of a “subacute withdrawal syndrome” following chronic ethanol intake. Drug Alcohol Depend 4:353–357. [DOI] [PubMed] [Google Scholar]
- Berger RJ, Olley P, Oswald I (1962) The EEG, eye movements and dreams of the blind. Q J Exp Psychol 14:183–186. [Google Scholar]
- Bokstrom K, Balldin J (1992) A rating scale for assessment of alcohol withdrawal psychopathology (AWIP). Alcoholism, clinical and experimental research 16:241–249. [DOI] [PubMed] [Google Scholar]
- Borbely AA (1982) A two process model of sleep regulation. Hum Neurobiol 1:195–204. [PubMed] [Google Scholar]
- Breslau N, Roth T, Rosenthal L, Andreski P (1996) Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry 39:411–418. [DOI] [PubMed] [Google Scholar]
- Brooks AT, Wallen GR (2014) Sleep Disturbances in Individuals with Alcohol-Related Disorders: A Review of Cognitive-Behavioral Therapy for Insomnia (CBT-I) and Associated Non-Pharmacological Therapies. Subst Abuse 8:55–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brower KJ (2001) Alcohol’s effects on sleep in alcoholics. Alcohol Res Health 25:110–125. [PMC free article] [PubMed] [Google Scholar]
- Brower KJ (2003) Insomnia, alcoholism and relapse. Sleep Med Rev 7:523–539. [DOI] [PubMed] [Google Scholar]
- Brower KJ (2016) Assessing and treating insomnia related to alcohol use disorders. Curr Addict Rep 3:98–108. [Google Scholar]
- Brower KJ, Aldrich MS, Robinson EA, Zucker RA, Greden JF (2001a) Insomnia, self-medication, and relapse to alcoholism. Am J Psychiatry 158:399–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brower KJ, Aldrich MS, Robinson EA, Zucker RA, Greden JF (2001b) Insomnia, self-medication, and relapse to alcoholism. Am J Psychiatry 158:399–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brower KJ, Conroy DA, Kurth ME, Anderson BJ, Stein MD (2011) Ramelteon and improved insomnia in alcohol-dependent patients: a case series. J Clin Sleep Med 7:274–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brower KJ, Hall JM (2001) Effects of age and alcoholism on sleep: a controlled study. J Stud Alcohol 62:335–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brower KJ, Myra Kim H, Strobbe S, Karam-Hage MA, Consens F, Zucker RA (2008) A randomized double-blind pilot trial of gabapentin versus placebo to treat alcohol dependence and comorbid insomnia. Alcohol Clin Exp Res 32:1429–1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brower KJ, Perron BE (2010) Prevalence and correlates of withdrawal-related insomnia among adults with alcohol dependence: results from a national survey. Am J Addict 19:238–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brower KJ, Wojnar M, Sliwerska E, Armitage R, Burmeister M (2012) PER3 polymorphism and insomnia severity in alcohol dependence. Sleep 35:571–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse DJ, Germain A, Hall M, Monk TH, Nofzinger EA (2011) A Neurobiological Model of Insomnia. Drug Discov Today Dis Models 8:129–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caetano R, Clark CL, Greenfield TK (1998) Prevalence, trends, and incidence of alcohol withdrawal symptoms: analysis of general population and clinical samples. Alcohol health and research world 22:73–79. [PMC free article] [PubMed] [Google Scholar]
- Chakravorty S, Grandner MA, Kranzler HR, Mavandadi S, Kling MA, Perlis ML, Oslin DW (2013) Insomnia in alcohol dependence: predictors of symptoms in a sample of veterans referred from primary care. Am J Addict 22:266–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakravorty S, Hanlon AL, Kuna ST, Ross RJ, Kampman KM, Witte LM, Perlis ML, Oslin DW (2014) The effects of quetiapine on sleep in recovering alcohol-dependent subjects: a pilot study. J Clin Psychopharmacol 34:350–354. [DOI] [PubMed] [Google Scholar]
- Chan JK, Trinder J, Andrewes HE, Colrain IM, Nicholas CL (2013) The acute effects of alcohol on sleep architecture in late adolescence. Alcohol Clin Exp Res 37:1720–1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan JK, Trinder J, Colrain IM, Nicholas CL (2015) The acute effects of alcohol on sleep electroencephalogram power spectra in late adolescence. Alcohol Clin Exp Res 39:291–299. [DOI] [PubMed] [Google Scholar]
- Chaudhary NS, Chakravorty S, Evenden JL, Sanuck N (2013) Insomnia severity is associated with decreased executive functioning in patients with suicidal ideation and drug abuse. The primary care companion to CNS disorders 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudhary NS, Kampman KM, Kranzler HR, Grandner MA, Debbarma S, Chakravorty S (2015) Insomnia in alcohol dependent subjects is associated with greater psychosocial problem severity. Addict Behav 50:165–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi SY (1973) Dreams as a prognostic factor in alcoholism. Am J Psychiatry 130:699–702. [DOI] [PubMed] [Google Scholar]
- Cohn TJ, Foster JH, Peters TJ (2003) Sequential studies of sleep disturbance and quality of life in abstaining alcoholics. Addict Biol 8:455–462. [DOI] [PubMed] [Google Scholar]
- Conroy DA, Hairston IS, Zucker RA, Heitzig MM (2015) Sleep Patterns in Children of Alcoholics and the Relationship with Parental Reports. Austin Journal of Sleep Disorders 2:01–09. [Google Scholar]
- Conroy DA, Todd Arnedt J, Brower KJ, Strobbe S, Consens F, Hoffmann R, Armitage R (2006) Perception of sleep in recovering alcohol-dependent patients with insomnia: relationship with future drinking. Alcohol Clin Exp Res 30:1992–1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Consensus Conference P, Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, Dinges DF, Gangwisch J, Grandner MA, Kushida C, Malhotra RK, Martin JL, Patel SR, Quan SF, Tasali E (2015) Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society on the Recommended Amount of Sleep for a Healthy Adult: Methodology and Discussion. J Clin Sleep Med 11:931–952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crum RM, Ford DE, Storr CL, Chan YF (2004) Association of sleep disturbance with chronicity and remission of alcohol dependence: data from a population-based prospective study. Alcohol Clin Exp Res 28:1533–1540. [DOI] [PubMed] [Google Scholar]
- Currie SR, Clark S, Hodgins DC, El-Guebaly N (2004) Randomized controlled trial of brief cognitive-behavioural interventions for insomnia in recovering alcoholics. Addiction 99:1121–1132. [DOI] [PubMed] [Google Scholar]
- Currie SR, Clark S, Rimac S, Malhotra S (2003a) Comprehensive assessment of insomnia in recovering alcoholics using daily sleep diaries and ambulatory monitoring. Alcohol Clin Exp Res 27:1262–1269. [DOI] [PubMed] [Google Scholar]
- Currie SR, Clark S, Rimac S, Malhotra S (2003b) Comprehensive assessment of insomnia in recovering alcoholics using daily sleep diaries and ambulatory monitoring. Alcohol Clin Exp Res 27:1262–1269. [DOI] [PubMed] [Google Scholar]
- Dahl RE, Williamson DE, Bertocci MA, Stolz MV, Ryan ND, Ehlers CL (2003) Spectral analyses of sleep EEG in depressed offspring of fathers with or without a positive history of alcohol abuse or dependence: a pilot study. Alcohol 30:193–200. [DOI] [PubMed] [Google Scholar]
- de Zambotti M, Baker FC, Sugarbaker DS, Nicholas CL, Trinder J, Colrain IM (2014) Poor autonomic nervous system functioning during sleep in recently detoxified alcohol-dependent men and women. Alcohol Clin Exp Res 38:1373–1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Zambotti M, Willoughby AR, Baker FC, Sugarbaker DS, Colrain IM (2015) Cardiac autonomic function during sleep: effects of alcohol dependence and evidence of partial recovery with abstinence. Alcohol 49:409–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drummond SP, Gillin JC, Smith TL, DeModena A (1998) The sleep of abstinent pure primary alcoholic patients: natural course and relationship to relapse. Alcohol Clin Exp Res 22:1796–1802. [PubMed] [Google Scholar]
- Escobar-Cordoba F, Avila-Cadavid JD, Cote-Menendez M (2009) Complaints of insomnia in hospitalized alcoholics. Revista brasileira de psiquiatria 31:261–264. [DOI] [PubMed] [Google Scholar]
- Fabre LF Jr., Gainey A, Kemple S, McLendon DM, Metzler CM (1977) Pilot open-label study of triazolam in the treatment of insomnia following alcohol withdrawal. J Stud Alcohol 38:2188–2192. [DOI] [PubMed] [Google Scholar]
- Feige B, Scaal S, Hornyak M, Gann H, Riemann D (2007) Sleep electroencephalographic spectral power after withdrawal from alcohol in alcohol-dependent patients. Alcohol Clin Exp Res 31:19–27. [DOI] [PubMed] [Google Scholar]
- Ford DE, Kamerow DB (1989) Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? Jama 262:1479–1484. [DOI] [PubMed] [Google Scholar]
- Friedmann PD, Herman DS, Freedman S, Lemon SC, Ramsey S, Stein MD (2003) Treatment of sleep disturbance in alcohol recovery: a national survey of addiction medicine physicians. J Addict Dis 22:91–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedmann PD, Rose JS, Swift R, Stout RL, Millman RP, Stein MD (2008) Trazodone for sleep disturbance after alcohol detoxification: a double-blind, placebo-controlled trial. Alcohol Clin Exp Res 32:1652–1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fulda S (2015) The Role of Periodic Limb Movements During Sleep in Restless Legs Syndrome: A Selective Update. Sleep Med Clin 10:241–248, xii. [DOI] [PubMed] [Google Scholar]
- Gann H, Feige B, Cloot O, Van Wasen H, Zinzgraf D, Hohagen F, Riemann D (2004) Polysomnography during withdrawal with clomethiazole or placebo in alcohol dependent patients--a double-blind and randomized study. Pharmacopsychiatry 37:228–235. [DOI] [PubMed] [Google Scholar]
- Gann H, Feige B, Fasihi S, van Calker D, Voderholzer U, Riemann D (2002) Periodic limb movements during sleep in alcohol dependent patients. Eur Arch Psychiatry Clin Neurosci 252:124–129. [DOI] [PubMed] [Google Scholar]
- Gillin JC, Smith TL, Irwin M, Kripke DF, Brown S, Schuckit M (1990a) Short REM latency in primary alcoholic patients with secondary depression. Am J Psychiatry 147:106–109. [DOI] [PubMed] [Google Scholar]
- Gillin JC, Smith TL, Irwin M, Kripke DF, Schuckit M (1990b) EEG sleep studies in “pure” primary alcoholism during subacute withdrawal: relationships to normal controls, age, and other clinical variables. Biol Psychiatry 27:477–488. [DOI] [PubMed] [Google Scholar]
- Greeff AP, Conradie WS (1998) Use of progressive relaxation training for chronic alcoholics with insomnia. Psychol Rep 82:407–412. [DOI] [PubMed] [Google Scholar]
- Greenberg R, Pearlman C (1967) Delirium tremens and dreaming. Am J Psychiatry 124:133–142. [DOI] [PubMed] [Google Scholar]
- Gross MM, Goodenough DR, Hastey J, Lewis E (1973) Experimental study of sleep in chronic alcoholics before, during, and after four days of heavy drinking with a nondrinking comparison. Ann N Y Acad Sci 215:254–265. [DOI] [PubMed] [Google Scholar]
- Gross MM, Hastey JM (1975) The relation between baseline slow wave sleep and the slow wave sleep response to alcohol in alcoholics. Adv Exp Med Biol 59:467–475. [DOI] [PubMed] [Google Scholar]
- Grosshans M, Mutschler J, Luderer M, Mann K, Kiefer F (2014) Agomelatine is effective in reducing insomnia in abstinent alcohol-dependent patients. Clin Neuropharmacol 37:6–8. [DOI] [PubMed] [Google Scholar]
- Hartwell EE, Bujarski S, Glasner-Edwards S, Ray LA (2015) The Association of Alcohol Severity and Sleep Quality in Problem Drinkers. Alcohol Alcohol 50:536–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heilig M, Egli M, Crabbe JC, Becker HC (2010) Acute withdrawal, protracted abstinence and negative affect in alcoholism: are they linked? Addict Biol 15:169–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hornyak M, Haas P, Veit J, Gann H, Riemann D (2004) Magnesium treatment of primary alcohol-dependent patients during subacute withdrawal: an open pilot study with polysomnography. Alcohol Clin Exp Res 28:1702–1709. [DOI] [PubMed] [Google Scholar]
- Iber C, Ancoli-Israel S, Chesson AL, Quan SF (2007) THe AASM Manual for the Scoring of Sleep and Associated Events, in Series THe AASM Manual for the Scoring of Sleep and Associated Events, WestChester, IL. [Google Scholar]
- Imatoh N, Nakazawa Y, Ohshima H, Ishibashi M, Yokoyama T (1986) Circadian rhythm of REM sleep of chronic alcoholics during alcohol withdrawal. Drug Alcohol Depend 18:77–85. [DOI] [PubMed] [Google Scholar]
- Irwin M, Miller C (2000) Decreased natural killer cell responses and altered interleukin-6 and interleukin-10 production in alcoholism: an interaction between alcohol dependence and African-American ethnicity. Alcohol Clin Exp Res 24:560–569. [PubMed] [Google Scholar]
- Irwin MR, Olmstead R, Valladares EM, Breen EC, Ehlers CL (2009) Tumor necrosis factor antagonism normalizes rapid eye movement sleep in alcohol dependence. Biol Psychiatry 66:191–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin MR, Valladares EM, Motivala S, Thayer JF, Ehlers CL (2006) Association between nocturnal vagal tone and sleep depth, sleep quality, and fatigue in alcohol dependence. Psychosom Med 68:159–166. [DOI] [PubMed] [Google Scholar]
- Jakubczyk A, Klimkiewicz A, Kopera M, Krasowska A, Wrzosek M, Matsumoto H, Burmeister M, Brower KJ, Wojnar M (2013) The CC genotype in the T102C HTR2A polymorphism predicts relapse in individuals after alcohol treatment. J Psychiatr Res 47:527–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janson C, Lindberg E, Gislason T, Elmasry A, Boman G (2001) Insomnia in men-a 10-year prospective population based study. Sleep 24:425–430. [DOI] [PubMed] [Google Scholar]
- John U, Meyer C, Rumpf HJ, Hapke U (2005) Relationships of psychiatric disorders with sleep duration in an adult general population sample. J Psychiatr Res 39:577–583. [DOI] [PubMed] [Google Scholar]
- Johnson EO, Roehrs T, Roth T, Breslau N (1998) Epidemiology of alcohol and medication as aids to sleep in early adulthood. Sleep 21:178–186. [DOI] [PubMed] [Google Scholar]
- Kaneita Y, Uchiyama M, Takemura S, Yokoyama E, Miyake T, Harano S, Asai T, Tsutsui T, Kaneko A, Nakamura H, Ohida T (2007) Use of alcohol and hypnotic medication as aids to sleep among the Japanese general population. Sleep medicine 8:723–732. [DOI] [PubMed] [Google Scholar]
- Karam-Hage M, Brower KJ (2000) Gabapentin treatment for insomnia associated with alcohol dependence. Am J Psychiatry 157:151. [DOI] [PubMed] [Google Scholar]
- Karam-Hage M, Brower KJ (2003) Open pilot study of gabapentin versus trazodone to treat insomnia in alcoholic outpatients. Psychiatry Clin Neurosci 57:542–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kissin B (1979) Biological investigations in alcohol research. J Stud Alcohol Suppl 8:146–181. [DOI] [PubMed] [Google Scholar]
- Klimkiewicz A, Bohnert AS, Jakubczyk A, Ilgen MA, Wojnar M, Brower K (2012) The association between insomnia and suicidal thoughts in adults treated for alcohol dependence in Poland. Drug Alcohol Depend 122:160–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolla BP, Mansukhani MP, Schneekloth T (2011a) Pharmacological treatment of insomnia in alcohol recovery: a systematic review. Alcohol Alcohol 46:578–585. [DOI] [PubMed] [Google Scholar]
- Kolla BP, Schneekloth T, Biernacka J, Mansukhani M, Geske J, Karpyak V, Hall-Flavin D, Louikianova L, Frye MA (2014) The course of sleep disturbances in early alcohol recovery: an observational cohort study. Am J Addict 23:21–26. [DOI] [PubMed] [Google Scholar]
- Kolla BP, Schneekloth T, Mansukhani MP, Biernacka JM, Hall-Flavin D, Karpyak V, Geske J, Frye MA (2015) The association between sleep disturbances and alcohol relapse: A 12-month observational cohort study. Am J Addict 24:362–367. [DOI] [PubMed] [Google Scholar]
- Kolla BP, Schneekloth TD, Biernacka JM, Frye MA, Mansukhani MP, Hall-Flavin DK, Karpyak VM, Loukianova LL, Lesnick TG, Mrazek D (2011b) Trazodone and alcohol relapse: a retrospective study following residential treatment. Am J Addict 20:525–529. [DOI] [PubMed] [Google Scholar]
- Kotorii T, Nakazawa Y, Yokoyama T, Ohkawa T, Sakurada H, Nonaka K, Dainoson K (1982) Terminal sleep following delirium tremens in chronic alcoholics--polysomnographic and behavioral study. Drug Alcohol Depend 10:125–134. [DOI] [PubMed] [Google Scholar]
- Krueger JM, Fang J, Hansen MK, Zhang J, Obal F Jr. (1998) Humoral Regulation of Sleep. News Physiol Sci 13:189–194. [DOI] [PubMed] [Google Scholar]
- Krueger JM, Toth LA (1994) Cytokines as regulators of sleep. Ann N Y Acad Sci 739:299–310. [DOI] [PubMed] [Google Scholar]
- Kuhlwein E, Hauger RL, Irwin MR (2003) Abnormal nocturnal melatonin secretion and disordered sleep in abstinent alcoholics. Biol Psychiatry 54:1437–1443. [DOI] [PubMed] [Google Scholar]
- Landolt HP, Roth C, Dijk DJ, Borbely AA (1996) Late-afternoon ethanol intake affects nocturnal sleep and the sleep EEG in middle-aged men. J Clin Psychopharmacol 16:428–436. [DOI] [PubMed] [Google Scholar]
- Le Bon O, Murphy JR, Staner L, Hoffmann G, Kormoss N, Kentos M, Dupont P, Lion K, Pelc I, Verbanck P (2003) Double-blind, placebo-controlled study of the efficacy of trazodone in alcohol post-withdrawal syndrome: polysomnographic and clinical evaluations. J Clin Psychopharmacol 23:377–383. [DOI] [PubMed] [Google Scholar]
- Le Bon O, Verbanck P, Hoffmann G, Murphy JR, Staner L, De Groote D, Mampunza S, Den Dulk A, Vacher C, Kornreich C, Pelc I (1997) Sleep in detoxified alcoholics: impairment of most standard sleep parameters and increased risk for sleep apnea, but not for myoclonias--a controlled study. J Stud Alcohol 58:30–36. [DOI] [PubMed] [Google Scholar]
- Litten RZ, Fertig JB, Falk DE, Ryan ML, Mattson ME, Collins JF, Murtaugh C, Ciraulo D, Green AI, Johnson B, Pettinati H, Swift R, Afshar M, Brunette MF, Tiouririne NA, Kampman K, Stout R (2012) A double-blind, placebo-controlled trial to assess the efficacy of quetiapine fumarate XR in very heavy-drinking alcohol-dependent patients. Alcohol Clin Exp Res 36:406–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malcolm R, Myrick LH, Veatch LM, Boyle E, Randall PK (2007) Self-reported sleep, sleepiness, and repeated alcohol withdrawals: a randomized, double blind, controlled comparison of lorazepam vs gabapentin. J Clin Sleep Med 3:24–32. [PubMed] [Google Scholar]
- Mason BJ, Light JM, Williams LD, Drobes DJ (2009) Proof-of-concept human laboratory study for protracted abstinence in alcohol dependence: effects of gabapentin. Addiction biology 14:73–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason BJ, Quello S, Goodell V, Shadan F, Kyle M, Begovic A (2014) Gabapentin treatment for alcohol dependence: a randomized clinical trial. JAMA Intern Med 174:70–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mello NK, Mendelson JH (1970) Behavioral studies of sleep patterns in alcoholics during intoxication and withdrawal. J Pharmacol Exp Ther 175:94–112. [PubMed] [Google Scholar]
- Miyata S, Noda A, Ito N, Atarashi M, Yasuma F, Morita S, Koike Y (2004) REM sleep is impaired by a small amount of alcohol in young women sensitive to alcohol. Intern Med 43:679–684. [DOI] [PubMed] [Google Scholar]
- Moeller FG, Gillin JC, Irwin M, Golshan S, Kripke DF, Schuckit M (1993) A comparison of sleep EEGs in patients with primary major depression and major depression secondary to alcoholism. J Affect Disord 27:39–42. [DOI] [PubMed] [Google Scholar]
- Nakazawa Y, Yokoyama T, Koga Y, Kotorii T, Ohkawa T, Sakurada H, Nonaka K, Dainoson K (1981) Polysomnographic study of terminal sleep following delirium tremens. Drug Alcohol Depend 8:111–117. [DOI] [PubMed] [Google Scholar]
- Ohayon MM, Guilleminault C, Priest RG (1999) Night terrors, sleepwalking, and confusional arousals in the general population: their frequency and relationship to other sleep and mental disorders. J Clin Psychiatry 60:268–276; quiz 277. [DOI] [PubMed] [Google Scholar]
- Pandi-Perumal SR, Smits M, Spence W, Srinivasan V, Cardinali DP, Lowe AD, Kayumov L (2007) Dim light melatonin onset (DLMO): a tool for the analysis of circadian phase in human sleep and chronobiological disorders. Prog Neuropsychopharmacol Biol Psychiatry 31:1–11. [DOI] [PubMed] [Google Scholar]
- Pearl PL, LaFleur BJ, Reigle SC, Rich AS, Freeman AA, McCutchen C, Sato S (2002) Sawtooth wave density analysis during REM sleep in normal volunteers. Sleep Med 3:255–258. [DOI] [PubMed] [Google Scholar]
- Peppard PE, Austin D, Brown RL (2007) Association of alcohol consumption and sleep disordered breathing in men and women. J Clin Sleep Med 3:265–270. [PMC free article] [PubMed] [Google Scholar]
- Perlis ML, Kehr EL, Smith MT, Andrews PJ, Orff H, Giles DE (2001a) Temporal and stagewise distribution of high frequency EEG activity in patients with primary and secondary insomnia and in good sleeper controls. J Sleep Res 10:93–104. [DOI] [PubMed] [Google Scholar]
- Perlis ML, Smith MT, Andrews PJ, Orff H, Giles DE (2001b) Beta/Gamma EEG activity in patients with primary and secondary insomnia and good sleeper controls. Sleep 24:110–117. [DOI] [PubMed] [Google Scholar]
- Perney P, Lehert P, Mason BJ (2012) Sleep disturbance in alcoholism: proposal of a simple measurement, and results from a 24-week randomized controlled study of alcohol-dependent patients assessing acamprosate efficacy. Alcohol Alcohol 47:133–139. [DOI] [PubMed] [Google Scholar]
- Pressman MR, Mahowald MW, Schenck CH, Bornemann MC (2007) Alcohol-induced sleepwalking or confusional arousal as a defense to criminal behavior: a review of scientific evidence, methods and forensic considerations. J Sleep Res 16:198–212. [DOI] [PubMed] [Google Scholar]
- Rechtschaffen A, Kales A (1968) A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects, UCLA Brain Information Service/Brain Research Institute, Los Angeles, CA 90024. [Google Scholar]
- Redwine L, Dang J, Hall M, Irwin M (2003) Disordered sleep, nocturnal cytokines, and immunity in alcoholics. Psychosom Med 65:75–85. [DOI] [PubMed] [Google Scholar]
- Richardson GS, Zee PC, Wang-Weigand S, Rodriguez L, Peng X (2008) Circadian phase-shifting effects of repeated ramelteon administration in healthy adults. J Clin Sleep Med 4:456–461. [PMC free article] [PubMed] [Google Scholar]
- Roehrs T, Yoon J, Roth T (1991) Nocturnal and next-day effects of ethanol and basal level of sleepiness. Human Psychopharmacology: Clinical and Experimental 6:307–311. [Google Scholar]
- Rundell OH, Lester BK, Griffiths WJ, Williams HL (1972) Alcohol and sleep in young adults. Psychopharmacologia 26:201–218. [DOI] [PubMed] [Google Scholar]
- Sakurai S, Cui R, Tanigawa T, Yamagishi K, Iso H (2007) Alcohol consumption before sleep is associated with severity of sleep-disordered breathing among professional Japanese truck drivers. Alcoholism: Clinical and Experimental Research 31:2053–2058. [DOI] [PubMed] [Google Scholar]
- Saper CB, Fuller PM, Pedersen NP, Lu J, Scammell TE (2010) Sleep state switching. Neuron 68:1023–1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schiavi RC, Stimmel BB, Mandeli J, White D (1995) Chronic alcoholism and male sexual function. Am J Psychiatry 152:1045–1051. [DOI] [PubMed] [Google Scholar]
- Schuckit MA, Bernstein LI (1981) Sleep time and drinking history: a hypothesis. Am J Psychiatry 138:528–530. [DOI] [PubMed] [Google Scholar]
- Siegel JE (2017) Rapid Eye Movement Sleep, in Principles and Practice of Sleep Medicine, Principles and Practice of Sleep Medicine (KRYGER M, ROTH T, DEMENT WC eds), pp 78–95, Elsevier, Philadelphia, PA 19103. [Google Scholar]
- Skoloda TE, Alterman AI, Gottheil E (1979) Sleep quality reported by drinking and non-drinking alcoholics, in Series Sleep quality reported by drinking and non-drinking alcoholics, Addiction Research and Treatment: Converging Trends. Proceedings of the First Annual Coatesville-Jefferson Conference on Addiction (GOTTHEIL EL MA, DRULEY KA, ALTERMAN AI ed, pp 102–112, Pergamon Press, Elmsford. [Google Scholar]
- Smith N, Hill R, Marshall J, Keaney F, Wanigaratne S (2014) Sleep related beliefs and their association with alcohol relapse following residential alcohol detoxification treatment. Behav Cogn Psychother 42:593–604. [DOI] [PubMed] [Google Scholar]
- Spielman AJ, Caruso LS, Glovinsky PB (1987) A behavioral perspective on insomnia treatment. Psychiatr Clin North Am 10:541–553. [PubMed] [Google Scholar]
- Staner L, Boeijinga P, Danel T, Gendre I, Muzet M, Landron F, Luthringer R (2006) Effects of acamprosate on sleep during alcohol withdrawal: A double-blind placebo-controlled polysomnographic study in alcohol-dependent subjects. Alcohol Clin Exp Res 30:1492–1499. [DOI] [PubMed] [Google Scholar]
- Stein MD, Friedmann PD (2005) Disturbed sleep and its relationship to alcohol use. Subst Abus 26:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinig J, Foraita R, Happe S, Heinze M (2011) Perception of sleep and dreams in alcohol-dependent patients during detoxication and abstinence. Alcohol Alcohol 46:143–147. [DOI] [PubMed] [Google Scholar]
- Tarokh L, Carskadon MA (2010) Sleep electroencephalogram in children with a parental history of alcohol abuse/dependence. Journal of sleep research 19:165–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitiello MV (1997) Sleep, alcohol and alcohol abuse. Addict Biol 2:151–158. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Greenwald S, Nino-Murcia G, Dement WC (1997) The morbidity of insomnia uncomplicated by psychiatric disorders. Gen Hosp Psychiatry 19:245–250. [DOI] [PubMed] [Google Scholar]
- Wellman M (1954) The late withdrawal symptoms of alcoholic addiction. Can Med Assoc J 70:526–529. [PMC free article] [PubMed] [Google Scholar]
- Williams DL, MacLean AW, Cairns J (1983) Dose-response effects of ethanol on the sleep of young women. J Stud Alcohol 44:515–523. [DOI] [PubMed] [Google Scholar]
- Williams HL, Rundell OH Jr. (1981) Altered sleep physiology in chronic alcoholics: reversal with abstinence. Alcohol Clin Exp Res 5:318–325. [DOI] [PubMed] [Google Scholar]
- Wong MM, Brower KJ, Fitzgerald HE, Zucker RA (2004) Sleep problems in early childhood and early onset of alcohol and other drug use in adolescence. Alcohol Clin Exp Res 28:578–587. [DOI] [PubMed] [Google Scholar]
- Wong MM, Brower KJ, Nigg JT, Zucker RA (2010) Childhood sleep problems, response inhibition, and alcohol and drug outcomes in adolescence and young adulthood. Alcohol Clin Exp Res 34:1033–1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong MM, Robertson GC, Dyson RB (2015) Prospective relationship between poor sleep and substance-related problems in a national sample of adolescents. Alcohol Clin Exp Res 39:355–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhabenko N, Wojnar M, Brower KJ (2012) Prevalence and correlates of insomnia in a polish sample of alcohol-dependent patients. Alcohol Clin Exp Res 36:1600–1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou JN, Liu RY, van Heerikhuize J, Hofman MA, Swaab DF (2003) Alterations in the circadian rhythm of salivary melatonin begin during middle-age. J Pineal Res 34:11–16. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


