Abstract
BACKGROUND
Performance of electrocardiographic (ECG) criteria for echocardiographically diagnosed left ventricular hypertrophy (LVH) in Chinese hypertensive patients is not well known. We investigated the accuracy of various ECG criteria for the diagnosis of the echocardiographic LVH according to the new cutoff values of left ventricular mass (LVM) index (>115 g/m2 for men and >95 g/m2 for women) in Chinese hypertensive patients.
METHODS
Our study included 702 consecutive hypertensive inpatients including 92 (13.1%) concentric and 121 (17.2%) eccentric LVH on standard echocardiography. Diagnostic accuracy of 7 ECG criteria was evaluated by calculating sensitivity and specificity and by using the receiver operating characteristic curves.
RESULTS
The ECG criteria for the detection of the echocardiographically defined LVH had a sensitivity of 15%–31.9% and specificity of 91.6%–99.2% overall, 20.7%–43.5% and 91.6%–99.2% concentric, and 7.4%–23.1% and 91.6%–99.2% eccentric. ECG diagnosis of LVH defined as the positive diagnosis of any of 4 ECG criteria including Sokolow–Lyon voltage, Cornell voltage, Cornell product, and RavL voltage had a sensitivity of 54% and specificity of 86.3% overall, 71.7% and 86.3% concentric, and 40.5% and 86.3% eccentric. After adjustment for confounding factors, various ECG criteria were significantly correlated with LVM, with standardized β coefficients from 0.20 to 0.39 (P < 0.001) and the highest coefficient for the Cornell product criterion.
CONCLUSIONS
All ECG LVH indexes had low sensitivity and high specificity in Chinese hypertensive patients. Combination of 4 or all ECG criteria might improve sensitivity without any loss of specificity.
Keywords: blood pressure, diagnosis, echocardiography, electrocardiography, hypertension, left ventricular hypertrophy
Left ventricular hypertrophy (LVH) is common in patients with hypertension, and is associated with the risk of cardiovascular mortality and morbidity.1–3 Both electrocardiography (ECG) and echocardiography can be used for the diagnosis of LVH. Echocardiography has high sensitivity but limited availability and high technical requirement. In contrast, ECG is low cost and reproducible but has low sensitivity.4–7 ECG is a routine test for LVH detection in patients with hypertension in all major hypertension guidelines.8–11 It is recommended to every single hypertensive patient and especially suitable for LVH screening.
Several ECG criteria, such as the Sokolow–Lyon index, Cornell voltage or Cornell voltage duration product, and RavL, are available to assess LVH.9 Most of previous studies have been conducted in Caucasians,12–14 and the diagnostic performance of ECG criteria for Asians especially Chinese remains under investigation.15 A few previous studies of small sample size evaluated correlation between ECG criteria and LVH diagnosed with the old echocardiographic left ventricular mass index (LVMI) cutoff values (>125 g/m2 for men and >120 g/m2 for women) and showed inconsistent sensitivity and specificity in the Chinese population.16,17 Recent hypertension guidelines reduced the LVMI cutoff values of echocardiographic LVH diagnostic criteria to >115 g/m2 for men and >95 g/m2 for women.8–11 In the present study, we aimed to assess the accuracy of these ECG criteria for the diagnosis of the newly defined echocardiographic LVH including both concentric and eccentric patterns in Chinese adult hypertensive patients.
METHODS
Study population
Our retrospective cross-sectional study included a total of 702 adult hypertensive patients, who admitted in the hypertension inpatient ward in Ruijin Hospital, Shanghai, China from December 2016 to November 2017. All these patients were at least 18 years old and had undergone a 12-lead standard ECG and 2-dimensionally guided M-mode echocardiography. The study protocol was approved by the ethics committee of Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China. All patients gave informed written consent.
Exclusion criteria included valvular heart disease, previous myocardial infarction, left or right bundle branch block, pre-excitation syndrome, atrial fibrillation or flutter, hypertrophic cardiomyopathy, and pacemaker implantation. Patients with chronic kidney disease or diabetes mellitus were not excluded.
ECG recording and criteria for the diagnosis of LVH
A 12-lead standard ECG was performed by trained technicians at rest in the supine position with the MedEx apparatus (MedEx Technology Ltd, Beijing, China) with a speed and voltage regulation of 25 mm/s and 1 mV/10 mm, respectively. Seven ECG LVH criteria were evaluated, including the Sokolow–Lyon voltage, Cornell voltage index, Cornell product, Gubner index, RavL voltage, Rv5 or Rv6 voltage, and Lewis voltage, as recommended by the American Heart Association guidelines.18
Echocardiography
Standard 2-dimensional (2D) echocardiography was performed at rest by an experienced research sonographer blinded to clinical information and ECG findings using the Philips IE33 device (Philips, Eindhoven, The Netherlands). Left ventricular end-diastolic diameter (LVEDd), diastolic posterior wall thickness (PWTd), and diastolic interventricular septum thickness (IVSTd) were imaged from a parasternal long-axis window at the level of the mitral chords using 2D-targeted M-mode echocardiography. Left ventricular mass (LVM) was calculated according to the American Society of Echocardiography-cube formula: LVM (g) = 0.8 × [1.04 × {(LVEDd + PWTd + IVSTd)3 − (LVEDd)3}] + 0.6. LVM was indexed for body surface area to obtain LVMI.19,20 LVH was defined as a LVMI >115 g/m2 in men and >95 g/m2 in women. The relative wall thickness (RWT) was calculated as the sum of anteroseptal and posterior wall thickness divided by LVEDd. LVH was classified according to RWT as concentric (RWT ≥0.42) and eccentric patterns (RWT <0.42).
Blood pressure measurement
Blood pressure was measured on the day of admission at the hypertension inpatient ward. An automated oscillometric electronic blood pressure monitor was used during the entire study period (Omron BP-1300, Omron Healthcare, Kyoto, Japan). Two consecutive readings were obtained with a 1-minute interval after at least 5 minutes rest in the seated position. These 2 blood pressure readings were averaged for statistical analysis.
Statistical analysis
Means (±SD) and proportions were compared by the Student t test and Fisher’s exact test, respectively. We also performed analysis of variance for comparisons between the 3 groups according to the echocardiographic LVH status. Diagnostic accuracy for each ECG criteria was evaluated by calculating sensitivity and specificity and by the receiver operating characteristic curves. We also performed multiple linear regression analyses to analyze the relationship between the 7 ECG indexes and LVM after adjustment for age, sex, body mass index, systolic and diastolic blood pressure, diabetes mellitus, and chronic kidney disease. We reported the standardized β coefficients for the 7 ECG indexes. P values <0.05 were considered to be statistically significant. Statistical analysis was performed using the SPSS software, version 17.0 (SPSS, Chicago, IL).
RESULTS
Clinical and echocardiographic characteristics of patients
The 702 study participants included 449 men (64%), and had a mean (±SD) age of 51.9 ± 15.2 years. The proportion of patients with echocardiographic LVH was 30.3% (n = 213), including 92 patients concentric and 121 patients eccentric. Table 1 shows the clinical characteristics of these patients with LVH and those with normal geometry (n = 489). The 3 groups significantly differed in most of the characteristics (P < 0.05), except for body mass index, body surface area, serum triglycerides, and fasting plasma glucose (P > 0.05). They also significantly differed in the use of all major classes of antihypertensive drugs (P < 0.001), except for angiotensin-converting enzyme inhibitors (P = 0.58).
Table 1.
Clinical characteristics of patients by echocardiographic left ventricular hypertrophy status
| Characteristic | No LVH (n = 489) | Concentric LVH (n = 92) | Eccentric LVH (n = 121) | P (ANOVA) |
|---|---|---|---|---|
| Age (years) | 50 ± 15 | 54 ± 14* | 57 ± 14* | <0.001 |
| Men (%) | 67% | 70%* | 51%* ,† | <0.001 |
| Body mass index (kg/m2) | 25 ± 3 | 26 ± 4 | 26 ± 3 | 0.11 |
| Body surface area (m2) | 1.82 ± 0.20 | 1.84 ± 0.20 | 1.78 ± 0.20 | 0.11 |
| Systolic blood pressure (mm Hg) | 154 ± 14 | 166 ± 13* | 157 ±16* | 0.002 |
| Diastolic blood pressure (mm Hg) | 90 ± 12 | 92 ± 17 | 86 ± 16* ,† | 0.001 |
| Heart rate (beats/minute) | 81 ± 12 | 79 ± 11 | 77 ± 11* | 0.002 |
| Serum creatinine concentration (µmol/l) | 76 ± 23 | 97 ± 50* | 81 ± 28† | <0.001 |
| Serum uric acid concentration (µmol/l) | 341 ± 88 | 364 ± 99* | 356 ± 99 | 0.04 |
| Serum total cholesterol (mmol/l) | 4.6 ± 0.9 | 4.7 ± 1.1 | 4.9 ± 1.4* | 0.02 |
| Serum triglycerides (mmol/l) | 1.7 ± 1.0 | 1.9 ± 1.1 | 2.0 ± 1.5 | 0.14 |
| Fasting plasma glucose (mmol/l) | 5.8 ± 1.5 | 5.7 ± 1.0 | 5.4 ± 1.1 | 0.12 |
| Use of antihypertensive drugs, n (%) | ||||
| Calcium-channel blockers | 369 (75%) | 88 (95%) | 104 (85%) | <0.001 |
| Angiotensin-converting enzyme inhibitors | 135 (27%) | 26 (28%) | 28 (23%) | 0.58 |
| Angiotensin receptor blockers | 146 (29%) | 37 (40%) | 80 (66%) | <0.001 |
| β-Blockers | 215 (43%) | 60 (65%) | 56 (46%) | <0.001 |
| α-Blockers | 117 (23%) | 50 (54%) | 42 (34%) | <0.001 |
| Diuretics | 132 (26%) | 47 (51%) | 57 (47%) | <0.001 |
Values are mean ± standard deviation. Abbreviations: ANOVA, analysis of variance; LVH, left ventricular hypertrophy.
*P < 0.05 vs. no LVH.
† P < 0.05 vs. concentric LVH.
Table 2 shows the echocardiographic measurements of left ventricular structure and function in the 3 groups of patients. Patients with concentric LVH had the greatest IVSTd, posterior wall thickness, RWT, LVM, and LVMI. Patients with eccentric LVH had the greatest left ventricular diastolic and systolic diameters and lowest left ventricular ejection fraction.
Table 2.
Left ventricular structure and function by echocardiographic left ventricular hypertrophy status
| No LVH (n = 489) | Concentric LVH (n = 92) | Eccentric LVH (n = 121) | P (ANOVA) | |
|---|---|---|---|---|
| Left ventricular diastolic diameter (mm) | 48.9 ± 3.7 | 51.8 ± 3.5* | 53.5 ± 4.5* ,† | <0.001 |
| Left ventricular systolic diameter (mm) | 31.2 ± 3.0 | 33.3 ± 3.5* | 34.7 ± 4.8* ,† | <0.001 |
| Interventricular septal wall thickness (mm) | 9.6 ± 1.0 | 12.3 ± 1.0* | 10.5 ± 1.2* ,† | <0.001 |
| Posterior wall thickness (mm) | 9.3 ± 0.8 | 11.9 ± 1.0* | 10.0 ± 1.0* ,† | <0.001 |
| Relative wall thickness | 0.38 ± 0.04 | 0.46 ± 0.03* | 0.37 ± 0.03† | <0.001 |
| Left ventricular mass (g) | 163 ± 31 | 252 ± 48* | 214 ± 54* ,† | <0.001 |
| Left ventricular mass index (g/m2) | 89 ± 12 | 137 ± 19* | 120 ± 20* ,† | <0.001 |
| Left ventricular ejection fraction (%) | 65.7 ± 3.7 | 64.6 ± 4.0* | 63.7 ± 6.3* | <0.001 |
Values are mean ± standard deviation. Abbreviations: ANOVA, analysis of variance; LVH, left ventricular hypertrophy.
*P < 0.05 vs. no LVH.
† P < 0.05 vs. concentric LVH.
Sensitivity and specificity of various ECG criteria
The cutoff values for these 7 ECG criteria and sensitivity and specificity of various ECG criteria for echocardiographic LVH are shown in Table 3. In general, all ECG criteria had low sensitivity (15%–31.9%) and high specificity (91.6%–99.2%), especially for eccentric LVH. Regardless of the LVH pattern, the Cornell product criterion had the highest sensitivity for the diagnosis of LVH (43.5% and 23.1% for concentric and eccentric LVH, respectively). ECG diagnosis of LVH according to any of the 4 ECG criteria including the Sokolow–Lyon voltage, Cornell voltage, Cornell product, and RavL voltage had similar sensitivity (54% vs. 56.8% for overall, 71.7% vs. 72.8% for concentric LVH, and 40.5% vs. 44.6% for eccentric LVH) and specificity (86.3% vs. 83.4%) as any of all 7 ECG criteria.
Table 3.
Sensitivity and specificity of various criteria for the diagnosis of echocardiographic left ventricular hypertrophy
| Criterion | Sensitivity (%) | Specificity (%) | Area under curve |
|---|---|---|---|
| Sokolow–Lyon voltage (mV) | |||
| Sv1 + Rv5 or Rv6 >3.5 | |||
| Total LVH | 26.8 | 91.6 | 0.64 |
| Concentric LVH | 38.0 | 91.6 | |
| Eccentric LVH | 18.2 | 91.6 | |
| Cornell voltage (mV) | |||
| RavL + Sv3 >2.8 (men); RavL + Sv3 >2.0 (women) | |||
| Total LVH | 21.1 | 96.5 | 0.67 |
| Concentric LVH | 29.3 | 96.5 | |
| Eccentric LVH | 14.9 | 96.5 | |
| Cornell product (mV ms) | |||
| Cornell voltage × QRS duration >0.244 | |||
| Total LVH | 31.9 | 96.3 | 0.68 |
| Concentric LVH | 43.5 | 96.3 | |
| Eccentric LVH | 23.1 | 96.3 | |
| Gubner voltage (mV) | |||
| RI + SIII >2.5 | |||
| Total LVH | 18.8 | 99.2 | 0.69 |
| Concentric LVH | 29.3 | 99.2 | |
| Eccentric LVH | 10.7 | 99.2 | |
| RavL voltage (mV) | |||
| RavL ≥1.1 | |||
| Total LVH | 20.2 | 98.0 | 0.69 |
| Concentric LVH | 27.2 | 98.0 | |
| Eccentric LVH | 14.9 | 98.0 | |
| Rv5 or Rv6 voltage (mV) | |||
| Rv5 or Rv6 >2.7 | |||
| Total LVH | 15.0 | 96.9 | 0.60 |
| Concentric LVH | 25.0 | 96.9 | |
| Eccentric LVH | 7.4 | 96.9 | |
| Lewis voltage (mV) | |||
| (RI + SIII) − (RIII + SI) >1.7 | |||
| Total LVH | 19.2 | 98.4 | 0.68 |
| Concentric LVH | 20.6 | 98.4 | |
| Eccentric LVH | 18.2 | 98.4 | |
| Four electrocardiographic criteriaa | |||
| Total LVH | 54.0 | 86.3 | |
| Concentric LVH | 71.7 | 86.3 | |
| Eccentric LVH | 40.5 | 86.3 | |
| All 7 electrocardiographic criteria | |||
| Total LVH | 56.8 | 83.4 | |
| Concentric LVH | 72.8 | 83.4 | |
| Eccentric LVH | 44.6 | 83.4 |
Abbreviation: LVH, left ventricular hypertrophy.
aThe Sokolow–Lyon voltage, Cornell voltage, Cornell product, and RavL voltage criteria.
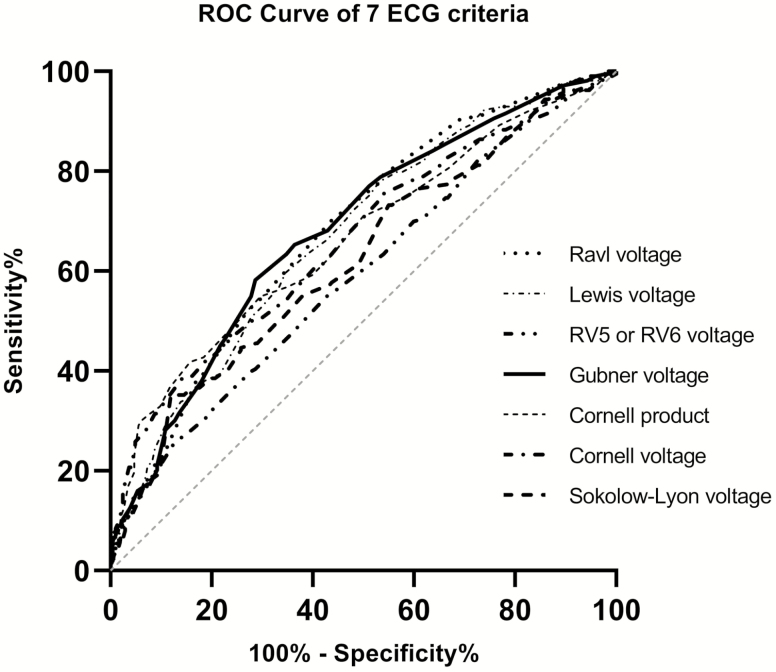
The receiver operating characteristic curve of various ECG criteria for LVH
Figure 1 shows the receiver operating characteristic curve comparison for the performance of all 7 ECG criteria. All 7 ECG criteria showed poor performance in the entire range of the receiver operating characteristic curve with an area under the curve of <0.70 (Table 3).
Figure 1.
Receiver operating characteristic comparison of the area under the curves between various electrocardiographic criteria for the detection of left ventricular hypertrophy.
Relationship between various ECG criteria and LVM
After adjustment for age, sex, body mass index, systolic and diastolic blood pressure, diabetes mellitus, and chronic kidney disease, all 7 ECG criteria indexes were significantly associated with LVM (P < 0.001, Table 4). The Cornell product had the greatest standardized β coefficient among all 7 criteria indexes (β 0.39 vs. 0.20 to 0.38, P < 0.001).
Table 4.
Multiple linear regression analysis between left ventricular mass and various electrocardiographic criteria
| Electrocardiographic criteria | Left ventricular mass | |
|---|---|---|
| Standardized β coefficient | P | |
| Sokolow–Lyon voltage | 0.31 | <0.001 |
| Cornell voltage | 0.38 | <0.001 |
| Cornell product | 0.39 | <0.001 |
| Gubner voltage | 0.27 | <0.001 |
| Ravl voltage | 0.28 | <0.001 |
| Rv5 or Rv6 voltage | 0.20 | <0.001 |
| Lewis voltage | 0.23 | <0.001 |
Adjusted for gender, age, body mass index, systolic and diastolic blood pressure, diabetes mellitus, and chronic kidney disease.
DISCUSSION
Our key finding was that the ECG criteria had low sensitivity and high specificity in the diagnosis of the echocardiographic LVH, especially the eccentric pattern. Nonetheless, the use of any of the 4 ECG criteria including Sokolow–Lyon voltage, Cornell voltage, Cornell product, and RavL voltage or any of the 7 ECG criteria may improve the diagnostic sensitivity for LVH in Chinese hypertensive patients.
Although it is known that the ECG LVH criteria might be ethnic dependent, few studies explored this important issue, and no study has yet evaluated the performance of ECG criteria for the new echocardiographic LVH criteria in Asians. With the old echocardiographic LVH criteria for the diagnosis of LVH, several previous studies investigated the accuracy of ECG criteria in the detection of LVH in Asians.21–23 In 546 Chinese patients with hypertension, Xie et al. found that the Cornell voltage and product criteria had a higher sensitivity to detect echocardiographic LVH (28% and 36.6%, respectively).21 In 539 young army men in Taiwan, Su et al. found that the Cornell voltage and product criteria had better performance for the echocardiographic LVH than the Sokolow–Lyon criteria, with a sensitivity of 22.2%, 27.8%, and 8.3%, respectively.22 However, in 332 Korean patients seen in a cardiology department, Park et al. demonstrated that the Cornell product criterion was superior to the Sokolow–Lyon voltage criterion in women, but the opposite was true in men.23
The low sensitivity of ECG criteria in the detection of LVH is probably typical for the Chinese and other eastern Asian populations. Other reasons may also play a part. A straightforward explanation could be the change of the echocardiographic criteria for the diagnosis of LVH.8–11 In our study participants, the prevalence of echocardiographic LVH increased from the old to the new criteria by 80.5%. If the old echocardiographic criteria would be used, the diagnostic sensitivity of the Cornell product criteria did increase to 41.5% with a specificity of 95.5%.
Peguero et al. recently reported a new criterion of the amplitude of the deepest S wave (SD) in any single lead plus the S wave amplitude of lead V4, i.e., (SD + SV4).24 In 94 hypertensive patients, the new ECG criterion had a higher sensitivity (62%) in the detection of LVH defined according to the new echocardiographic criteria than all the other ECG criteria (up to 35%).24 In our present study, this new criteria, SD + SV4, also had a slightly higher sensitivity (44.6%) than the other criteria. However, it had much lower specificity (75.8%) and area under the curve (0.62).
Our findings on the slightly higher sensitivity of the Cornell product are in line with the results of several previous studies.21,22 The mechanisms for the difference remain unexplained. One possible explanation is that the Cornell voltage index includes a limb lead in addition to the precordial one, and hence is less dependent on the thickness of the chest wall.25 In addition, combining QRS voltage with duration will further increase the area under the QRS complex in comparison with either QRS voltage or duration alone. Thus, the Cornell product may reflect the presence and severity of hypertrophy more accurately than ECG scores that involve only QRS voltage or duration.
Our observation on the even poorer sensitivity for the detection of eccentric hypertrophy remains under investigation. A possible explanation could be that the enlarged chamber and thinner wall thickness of the left ventricle influence both voltage and conductance and hence ECG evaluations of the heart. Left ventricular dilatation in eccentric LVH could cause elongated distance of the intraventricular conductance pathways, which produces a stretching of the conduction system, and in turn reduces the power of conductivity.26 Eccentric LVH may have even worse prognosis and hence even greater need for screening. It is imperative to further delineate the ECG characteristics of this pattern of LVH.
Previous studies often focused on the diagnostic sensitivity and specificity of single ECG criterion.27–29 Our current study found that any of the 4 ECG criteria including the Sokolow–Lyon voltage, Cornell voltage, Cornell product, and RavL voltage had a relatively higher sensitivity than each ECG criterion alone, without apparent compromise in specificity. These 4 ECG criteria are most commonly used with convenient acquisition by ECG devices and recommended by the European hypertension guideline.9 If applied properly and widely, this combined 4 ECG criteria approach might improve LVH screen in patients with hypertension.
Our study should be interpreted within the context of its limitations. First, our study examined only 7 of the numerous ECG criteria. Second, our study was a single center one. Most of our patients were from Shanghai or the nearby eastern China provinces. Our study therefore might be less representative than a multicenter study. Nonetheless, the current study built the ground for future studies on possible new ECG LVH diagnostic criteria in the Chinese or Asian population.
In conclusion, if the same cutoff values would be used in Chinese, the ECG criteria had high specificity but low sensitivity for the diagnosis of LVH, regardless of the pattern of LVH. Any of the 4 ECG criteria including the Sokolow–Lyon voltage, Cornell voltage, Cornell product, and RavL voltage, instead of a single ECG criterion, may have to be considered for the diagnosis of LVH in Chinese hypertensive patients.
ACKNOWLEDGMENTS
We gratefully acknowledge the expert technical assistance of Jun-Wei Li, Bei-Wen Lv, Yu-Zhong Shi, Yi Zhou, and Yi-Ni Zhou (The Shanghai Institute of Hypertension, Shanghai, China).
FUNDING
This study was supported by a grant from Merck & Co., Ltd (VEAP ID 6337). The present research was also supported by grants from the National Natural Science Foundation of China (grant no. 91639203 and 81770455), Ministry of Science and Technology (2015AA020105-06 and 2018YFC1704902), and Commission of Health (2016YFC0900902), Beijing, China and from the Shanghai Commissions of Science and Technology (19DZ2340200), Education (Gaofeng Clinical Medicine Grant Support 20152503), and Health (grant no. 15GWZK0802, 2017BR025, 20184Y0329, and 201840064 and a special grant for “leading academics”), Shanghai, China.
DISCLOSURE
Dr Ji-Guang Wang reports receiving lecture and consulting fees from Bayer, MSD, Omron, Pfizer, Servier, and Takeda. Drs Yinghua An and Rui Bian are employees of Merck & Co., Ltd. The other authors declare no conflicts of interest.
REFERENCES
- 1. Kannel WB, Gordon T, Castelli WP, Margolis JR. Electrocardiographic left ventricular hypertrophy and risk of coronary heart disease. The Framingham study. Ann Intern Med 1970; 72:813–822. [DOI] [PubMed] [Google Scholar]
- 2. Kannel WB, Gordon T, Offutt D. Left ventricular hypertrophy by electrocardiogram. Prevalence, incidence, and mortality in the Framingham study. Ann Intern Med 1969; 71:89–105. [DOI] [PubMed] [Google Scholar]
- 3. Romhilt DW, Bove KE, Norris RJ, Conyers E, Conradi S, Rowlands DT, Scott RC. A critical appraisal of the electrocardiographic criteria for the diagnosis of left ventricular hypertrophy. Circulation 1969; 40:185–195. [DOI] [PubMed] [Google Scholar]
- 4. Leese PJ, Viera AJ, Hinderliter AL, Stearns SC. Cost-effectiveness of electrocardiography vs. electrocardiography plus limited echocardiography to diagnose LVH in young, newly identified, hypertensives. Am J Hypertens 2010; 23:592–598. [DOI] [PubMed] [Google Scholar]
- 5. Levy D, Labib SB, Anderson KM, Christiansen JC, Kannel WB, Castelli WP. Determinants of sensitivity and specificity of electrocardiographic criteria for left ventricular hypertrophy. Circulation 1990; 81:815–820. [DOI] [PubMed] [Google Scholar]
- 6. Pewsner D, Jüni P, Egger M, Battaglia M, Sundström J, Bachmann LM. Accuracy of electrocardiography in diagnosis of left ventricular hypertrophy in arterial hypertension: systematic review. BMJ 2007; 335:711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Devereux RB. Is the electrocardiogram still useful for detection of left ventricular hypertrophy? Circulation 1990; 81:1144–1146. [DOI] [PubMed] [Google Scholar]
- 8. Joint Committee for Guideline Revision. 2018 Chinese Guidelines for prevention and treatment of hypertension—a report of the revision committee of Chinese guidelines for prevention and treatment of hypertension. J Geriatr Cardiol 2019; 16:182–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement D, Coca A, De Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen S, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder R, Shlyakhto E, Tsioufis K, Aboyans V, Desormais I; List of authors/Task Force members 2018 Practice Guidelines for the management of arterial hypertension of the European Society of Hypertension and the European Society of Cardiology: ESH/ESC Task Force for the Management of Arterial Hypertension. J Hypertens 2018; 36:2284–2309. [DOI] [PubMed] [Google Scholar]
- 10. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018; 71:e13–e115. [DOI] [PubMed] [Google Scholar]
- 11. Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, Horio T, Hoshide S, Ikeda S, Ishimitsu T, Ito M, Ito S, Iwashima Y, Kai H, Kamide K, Kanno Y, Kashihara N, Kawano Y, Kikuchi T, Kitamura K, Kitazono T, Kohara K, Kudo M, Kumagai H, Matsumura K, Matsuura H, Miura K, Mukoyama M, Nakamura S, Ohkubo T, Ohya Y, Okura T, Rakugi H, Saitoh S, Shibata H, Shimosawa T, Suzuki H, Takahashi S, Tamura K, Tomiyama H, Tsuchihashi T, Ueda S, Uehara Y, Urata H, Hirawa N. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res 2019; 42:1235–1481. [DOI] [PubMed] [Google Scholar]
- 12. Casiglia E, Schiavon L, Tikhonoff V, Bascelli A, Martini B, Mazza A, Caffi S, D’Este D, Bagato F, Bolzon M, Guidotti F, Haxhi Nasto H, Saugo M, Guglielmi F, Pessina AC. Electrocardiographic criteria of left ventricular hypertrophy in general population. Eur J Epidemiol 2008; 23:261–271. [DOI] [PubMed] [Google Scholar]
- 13. Toepker M, Schlett CL, Bamberg F, Blankstein R, Brady TJ, Nagurney JT, Hoffmann U. Performance of electrocardiographic criteria for left ventricular hypertrophy as compared with cardiac computed tomography: from the Rule Out Myocardial Infarction Using Computer Assisted Tomography trial. J Hypertens 2010; 28:1959–1967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cuspidi C, Facchetti R, Bombelli M, Sala C, Grassi G, Mancia G. Accuracy and prognostic significance of electrocardiographic markers of left ventricular hypertrophy in a general population: findings from the Pressioni Arteriose Monitorate E Loro Associazioni population. J Hypertens 2014; 32:921–928. [DOI] [PubMed] [Google Scholar]
- 15. Spencer CG, Beevers DG, Lip GY. Ethnic differences in left ventricular size and the prevalence of left ventricular hypertrophy among hypertensive patients vary with electrocardiographic criteria. J Hum Hypertens 2004; 18:631–636. [DOI] [PubMed] [Google Scholar]
- 16. Liu G. Application value of electrocardiogram in diagnosis of left ventricular hypertrophy in hypertensive patients. Chin Med Rec 2014; 15:79 (Chinese). [Google Scholar]
- 17. He P. Value of different electrocardiographic criteria in diagnosing left ventricular hypertrophy in hypertensive population. Med Equipment 2019; 32:36–38 (Chinese). [Google Scholar]
- 18. Hancock EW, Deal BJ, Mirvis DM, Okin P, Kligfield P, Gettes LS, Bailey JJ, Childers R. AHA/ACCF/HRS Recommendations for the standardization and interpretation of the electrocardiogram. J Am Coll Cardiol 2009; 53:992–1002. [DOI] [PubMed] [Google Scholar]
- 19. Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 2015; 28:1–39.e14. [DOI] [PubMed] [Google Scholar]
- 20. Devereux RB, Reichek N. Echocardiographic determination of left ventricular mass in man. Anatomic validation of the method. Circulation 1977; 55:613–618. [DOI] [PubMed] [Google Scholar]
- 21. Xie L, Wang Z. Correlation between echocardiographic left ventricular mass index and electrocardiographic variables used in left ventricular hypertrophy criteria in Chinese hypertensive patients. Hellenic J Cardiol 2010; 51:391–401. [PubMed] [Google Scholar]
- 22. Su FY, Li YH, Lin YP, Lee CJ, Wang CH, Meng FC, Yu YS, Lin F, Wu HT, Lin GM. A comparison of Cornell and Sokolow-Lyon electrocardiographic criteria for left ventricular hypertrophy in a military male population in Taiwan: the cardiorespiratory fitness and hospitalization events in armed forces study. Cardiovasc Diagn Ther 2017; 7:244–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Park JK, Shin JH, Kim SH, Lim YH, Kim KS, Kim SG, Kim JH, Lim HG, Shin J. A comparison of Cornell and Sokolow-Lyon electrocardiographic criteria for left ventricular hypertrophy in Korean patients. Korean Circ J 2012; 42:606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Peguero JG, Lo Presti S, Perez J, Issa O, Brenes JC, Tolentino A. Electrocardiographic criteria for the diagnosis of left ventricular hypertrophy. J Am Coll Cardiol 2017; 69:1694–1703. [DOI] [PubMed] [Google Scholar]
- 25. Kinoshita N, Onishi S, Yamazaki H, Katsukawa F, Yamada K. Recognition of left ventricular hypertrophy in new recruits of professional sumo wrestling. J Sci Med Sport 2003; 6:379–386. [DOI] [PubMed] [Google Scholar]
- 26. Ishizawa K, Ishizawa K, Motomura M, Konishi T, Wakabayashi A. High reliability rates of spatial pattern analysis by vectorcardiogram in assessing the severity of eccentric left ventricular hypertrophy. Am Heart J 1976; 91:50–57. [DOI] [PubMed] [Google Scholar]
- 27. Devereux RB, Casale PN, Eisenberg RR, Miller DH, Kligfield P. Electrocardiographic detection of left ventricular hypertrophy using echocardiographic determination of left ventricular mass as the reference standard. Comparison of standard criteria, computer diagnosis and physician interpretation. J Am Coll Cardiol 1984; 3:82–87. [DOI] [PubMed] [Google Scholar]
- 28. Jaggy C, Perret F, Bovet P, van Melle G, Zerkiebel N, Madeleine G, Kappenberger L, Paccaud F. Performance of classic electrocardiographic criteria for left ventricular hypertrophy in an African population. Hypertension 2000; 36:54–61. [DOI] [PubMed] [Google Scholar]
- 29. Okin PM, Roman MJ, Devereux RB, Kligfield P. Electrocardiographic identification of increased left ventricular mass by simple voltage-duration products. J Am Coll Cardiol 1995; 25:417–423. [DOI] [PubMed] [Google Scholar]