Abstract
Objective:
Depressive and anxiety symptoms co-occur with hazardous drinking among Latinxs. This secondary analysis of a clinical trial to reduce hazardous drinking (Motivational Interviewing adapted to address social stressors ([CAMI] vs. motivational interviewing [MI]) examined effects on anxiety/depressive symptoms. Discrimination and acculturation were examined as moderators.
Methods:
Latinx (n=296) hazardous drinkers (2+ occasions/month of heavy drinking; 4/5 drinks/occasion, females/males) were randomized to CAMI/MI. GEE analyzed how treatment condition and interactions were related to depressive and anxiety symptoms after controlling for covariates.
Results:
Baseline symptoms (anxiety, depression) exceeded clinical thresholds (Anxiety ≥ 8, M = 14.62, SD = 13.52; Depression ≥ 12, M = 18.78, SD = 12.57). CAMI showed significantly lower anxiety and depressive symptoms (6/12 months, respectively) than MI. CAMI with high baseline discrimination reported significantly less depression than MI (12 months).
Conclusions:
Explicitly addressing social stressors may be a beneficial adjunct to treatment for Latinx drinkers.
Keywords: alcohol, Latino/a, motivational interviewing, randomized controlled trial, depression
Latinxs are the largest and one of the fastest growing ethnic/racial minority groups in the United States (U.S. Census Bureau, 2017). Among Latinxs, the prevalence rates of anxiety and depressive symptoms and hazardous drinking are higher than the rates among non-Latinxs (Breslau, Schultz, Johnson, Peterson, & Davis, 2005; Hiott, Grzywacz, Arcury, & Quandt, 2006; Lee, Almedia, Colby, Tavares, & Rohsenow, 2016; Mendelson, Rehkopf, & Kubzansky, 2008; Sleath & Williams, 2004). Heavy alcohol use has been associated with double the risk of depressive symptomatology among community samples of Latinx men (Vasquez, Gonzalez-Guarda, & Santis, 2011).
The co-occurrence of psychological distress and heavy drinking has been associated with serious consequences for Latinxs, including higher rates of alcohol dependency and cirrhosis mortality. Data from the National Violent Death reporting system demonstrates that 40% of Latinxs tested positive for alcohol at the time of death by suicide, higher than non-Hispanic whites (34%), blacks (26%), or other racial/ethnic groups (28%) (Karch, Barker, & Strine, 2004). These consequences are part of the documented health disparities related to alcohol use for Latinxs (Chartier & Caetano, 2010; Keyes, Lui, & Cerda, 2011; Mulia, Ye, Greenfield, & Zemore, 2009; Torres, Romano, Voas, De La Rosa, & Lacey, 2014). To minimize these health disparities, it is important to address psychological symptoms of distress, such as elevated anxiety and depressive symptoms, and hazardous drinking before they progress to clinical disorders that require costly and intensive treatments. Addressing the factors associated with psychological distress among Latinxs might improve interventions.
Stress, or an “experience denoting adversity” (Keyes, Hatzenbuehler, & Hasin, 2011, p. 2), increases the risk for heavy drinking (APA, 2017) among racial/ethnic minorities (Keyes et al., 2011). Prolonged exposure to stress can create negative emotional states, which then increase coping responses to manage the stress, such as heavy drinking (Meyer, 2003). Minorities face additional, unique stressors related to their minority status, such as discrimination, stress related to migration and adaptation to a new country, feeling discriminated against, living in poverty, reduced access to economic opportunities, or exposure to crime (Cano et al., 2015; Cano et al., 2017; Nalven & Spillane, 2018; Ornelas & Perreira, 2011). These stressors have been associated with symptoms of depression and anxiety among Latinx heavy drinkers (Abraido-Lanza, Echeverria, & Florez, 2016; Lee et al., 2019).
Motivational Interviewing (MI) is an addiction counseling approach (Moyers & Martin, 2006; Carroll et al., 2006; Stewart, 2012) that helps individuals to resolve their ambivalence and increase motivation to change. MI has been widely applied to other health behaviors where people are ambivalent about change, including smoking cessation (Heckman, Egleston, & Hoffman, 2010), and diabetes self-management (Lundahl & Burke, 2009; Lundahl et al., 2013). MI has been successfully adapted for use with depression (Arkowitz & Burke, 2008; Keeley et al., 2016) with the presupposition that its focus on resolving ambivalence and increasing motivation are also key targets for change among depressed patients (Keeley et al., 2016). MI also has preliminary evidence supporting its efficacy in treating anxiety (Westra, Arkowitz, & Dozois, 2009); the MI focus on the therapeutic relationship may be particularly relevant to anxious people experiencing difficulties with interpersonal relationships (Westra, Arkowitz, & Dozois, 2009). MI is also presumed to have strong impact with marginalized individuals because it prioritizes autonomy and unique self-worth (Moyers & Martin, 2006), thus augmenting collaboration and engagement (Lee et al., 2019; Miller & Rose, 2009; Parsons, Lelutiu-Winberger, Bostko & Golub, 2014). Prior research has extended this idea by investigating whether a MI discussion that addressed sensitive topics/stressful experiences (i.e., experiences of discrimination) would encourage individuals to consider changes in their responses to the stressor (i.e., decrease drinking) (Lee et al., 2016). A meta-analysis of MI for various health outcomes revealed stronger effect sizes with different health outcomes for racial/ethnic minorities than non-minorities (Hettema, Steele, & Miller, 2005). Moreover, MI principles, such as collaboration, are consistent with Latinx cultural values like personalismo (overall preference for relationships with individuals rather than institutions) (Añez, Silva, Paris, & Bedregal, 2008). A MI that was culturally adapted for depressed Latinxs emphasized that cultural values that emerge in a social context: trabajar, luchar, and aprovechar (work, fight/struggle, to make the most of) were indicative of strength and resilience that can motivate people towards positive changes for themselves (Interian, Martinez, Rios, Krejci, & Guarnaccia., 2010). These authors documented improvements in medication adherence for those who received MI versus a brochure (Interian et al., 2010). These studies support MI’s potential efficacy in improving anxiety/depressive symptoms.
Our parent clinical trial of a cultural adaptation of MI ([CAMI], targeting stressors) compared to MI showed significant reductions in percent heavy drinking days and frequency of alcohol-related consequences through 12-month follow up when compared with baseline. CAMI participants with high self-reported discrimination and who were less acculturated (at baseline) reported significantly less frequent alcohol consequences than MI participants (Lee et al., 2019). In this secondary analysis, the goal was to explore whether the CAMI and MI might also have an effect on mental health symptoms. We examine this question first because of the co-occurrence of depression, anxiety, and hazardous drinking documented in clinical and general populations (Grant, Stinson, Dawson et al., 2004; Sullivan, Hasin & Grant, 2015). Second, CAMI was designed to specifically address stressors (e.g. acculturation and discrimination), so we hypothesized that this broader focus might improve depressive and/or anxiety symptoms among heavy drinkers. Minority Stress Theory hypothesizes that exposure to stressors (i.e., experiences of discrimination and marginalization) increases vulnerability to developing anxiety and depressive symptoms (Meyer, 2003). Given that the intervention provided opportunity to discuss these stressors, we might anticipate declines in participant depressive and anxiety symptoms.
We also examined potential treatment moderators because they indicate conditions under which treatments are most efficacious, and for whom (Kazdin 2007; Kraemer, Wilson, Fairburn, & Agras, 2002). These questions are particularly germane to tests of culturally adapted interventions. Acculturation has been found to moderate alcohol treatment outcomes; less acculturated Latinxs demonstrate a stronger treatment response to adapted MI (for alcohol use) than do more acculturated Latinxs (Carroll et al., 2009; Field & Caetano, 2010; Lee et al., 2019). A review of studies on culturally adapted cognitive behavior therapy for depression and anxiety (Griner & Smith, 2006; Hall, Ibaraki, Huang, Martin, & Sticer, 2016) similarly show that less acculturated individuals have stronger treatment response to culturally adapted interventions than more highly acculturated individuals. Accordingly, acculturation will be examined as a potential moderator of treatment effects on anxiety and depressive symptoms.
Discrimination was chosen as a moderator because it is an experience that contributes to minority stress (Abraido-Lanza, Echeverria, & Florez, 2016; Araújo Dawson & Panchandeswaran, 2010; Torres, Driscoll, & Voell, 2012). In the parent trial, among participants who experienced higher levels of discrimination at baseline, those who received CAMI reported significantly fewer adverse consequences related to alcohol use at 3 months follow-up compared to those who received MI (Lee et al., 2019). In this secondary analysis, we hypothesized that both conditions (CAMI, MI) would result in reduced anxiety/depressive symptoms and that CAMI participants would report significantly greater improvements in these symptoms compared to MI participants. Our second hypothesis was that acculturation and/or discrimination would moderate the relationship between treatment condition and depressive/anxiety symptoms at follow up.
Method
Sample and Participant Selection
Participants were recruited by community ads in an urban Northeast region. Participants self-identified as first or second-generation Latinx adults, 18-65 years of age, who met criteria for hazardous drinking ( ≥ 2 heavy drinking occasions/month of ≥ 4/5 drinks per occasion, females/males), National Institute on Alcohol Abuse and Alcoholism [NIAAA], 2006) and were not in alcohol treatment. Exclusion criteria were: active psychotic symptoms, evidence of cognitive impairment, and active drug use (4+ times in the month), excluding marijuana. The average participant age was 41 years (M = 41.10, SD = 12.23), and 63% was male. See Table 1 for descriptive information by condition.
Table 1.
Baseline Descriptives by Treatment Group (N = 296)
| Total (N = 296) | CAMI group (N = 149) | MI group (N = 147) | χ2 | p-value | ||||
|---|---|---|---|---|---|---|---|---|
| Variable | N | % | N | % | N | % | ||
| Gender | .07 | .79 | ||||||
| Male | 185 | 62.5% | 92 | 61.7% | 93 | 63.3% | ||
| Female | 111 | 37.5% | 57 | 38.3% | 54 | 36.7% | ||
| Employment status | .98 | .61 | ||||||
| Not employed | 180 | 60.8% | 87 | 58.4% | 93 | 63.3% | ||
| Part-time | 53 | 17.9% | 27 | 18.1% | 26 | 17.7% | ||
| Full-time | 63 | 21.1% | 35 | 23.5% | 28 | 19.0% | ||
| Place of Birth | .15 | .93 | ||||||
| US-born | 114 | 38.5% | 59 | 39.6% | 55 | 37.4% | ||
| Born in Puerto Rico | 79 | 26.7% | 39 | 26.2% | 40 | 27.2% | ||
| Born in Latin America | 103 | 34.8% | 51 | 34.2% | 52 | 35.4% | ||
| Variable | N | M (SD) | N | M (SD) | N | M (SD) | t | p-value |
| Age | 296 | 41.10 (12.23) | 149 | 41.22 (12.05) | 147 | 40.98 (12.46) | −.17 | .87 |
| Household Income | 295 | 2.53 (1.78) | 148 | 2.49 (1.67) | 147 | 2.56 (1.89) | .31 | .76 |
| Discrimination | 296 | 1.23 (1.02) | 149 | 1.25 (1.04) | 147 | 1.21 (1.00) | −.41 | .68 |
| Acculturation | 296 | 3.00 (.89) | 149 | 3.00 (.81) | 147 | 3.00 (.96) | −.05 | .96 |
| Anxiety (BAI) | ||||||||
| Baseline | 225 | 14.62 (13.52) | 118 | 14.19 (14.24) | 107 | 15.08 (12.72) | .49 | .62 |
| 3 months | 211 | 13.16 (12.11) | 103 | 10.80 (10.30) | 108 | 15.42 (13.28) | 2.81 | .005 |
| 6 months | 234 | 12.26 (12.84) | 119 | 10.30 (10.48) | 115 | 14.29 (14.66) | 2.40 | .008 |
| 12 months | 222 | 11.46 (12.42) | 109 | 10.35 (11.78) | 113 | 12.53 (12.98) | 1.31 | .19 |
| Depression (CES-D) | ||||||||
| Baseline | 296 | 18.78 (12.57) | 149 | 18.45 (12.53) | 147 | 19.12 (12.64) | .46 | .65 |
| 3 months | 242 | 18.31 (13.19) | 123 | 17.44 (11.86) | 119 | 19.20 (14.44) | 1.04 | .30 |
| 6 months | 234 | 17.27 (12.68) | 119 | 15.77 (11.44) | 115 | 18.84 (13.72) | 1.86 | .06 |
| 12 months | 222 | 16.76 (11.94) | 109 | 14.77 (10.89) | 113 | 18.68 (12.63) | 2.47 | .01 |
| Baseline Substance Use | ||||||||
| % Heavy Drinking Days | 296 | 38.99 (31.72) | 149 | 35.82 (29.54) | 147 | 42.20 (33.58) | 1.74 | .08 |
| # of Days Used Marijuana | 296 | 4.78 (9.46) | 149 | 4.21 (8.80) | 147 | 5.37 (10.09) | 1.05 | .29 |
| # of Days Used Other Drug | 293 | .37 (2.54) | 147 | .30 (1.46) | 146 | .44 (3.29) | .47 | .64 |
Note. Discrimination = Everyday Discrimination Scale; Acculturation = Short Acculturation Scale for Hispanics; BAI = Beck Anxiety Inventory; CES-D = Center for Epidemiologic Studies Depression Scale.
Percent heavy drinking days were reported from the prior 90 days. Number of days used marijuana and other drugs were reported from the prior 30 days.
Study Procedures
The study was approved by the University Institutional Review Board and the trial was registered with Clinical trials.gov, with identifier NCT (01996280). Latinxs who met criteria for heavy drinking responded to newspaper advertisements to participate in a health education study on the effects of alcohol on their health (Lee et al., 2019). A total of 624 Latinxs were screened to determine study eligibility (consumed 4/5 drinks/occasion, female or male, respectively) and a total of n=296 were enrolled (n=187 did not meet inclusion criteria, n=103 did not show up, n=38 not interested). At 6-months follow-up, there were n=234 participants (79%) who completed assessments, and at 12-months, there were n=222 who completed assessments (75%) (Figure 1). Data collection on baseline level of anxiety symptoms was started approximately one month after the RCT was launched. All questionnaires were translated and readily available to study staff who were all Spanish bilingual, prior to meeting participants.
Figure 1.
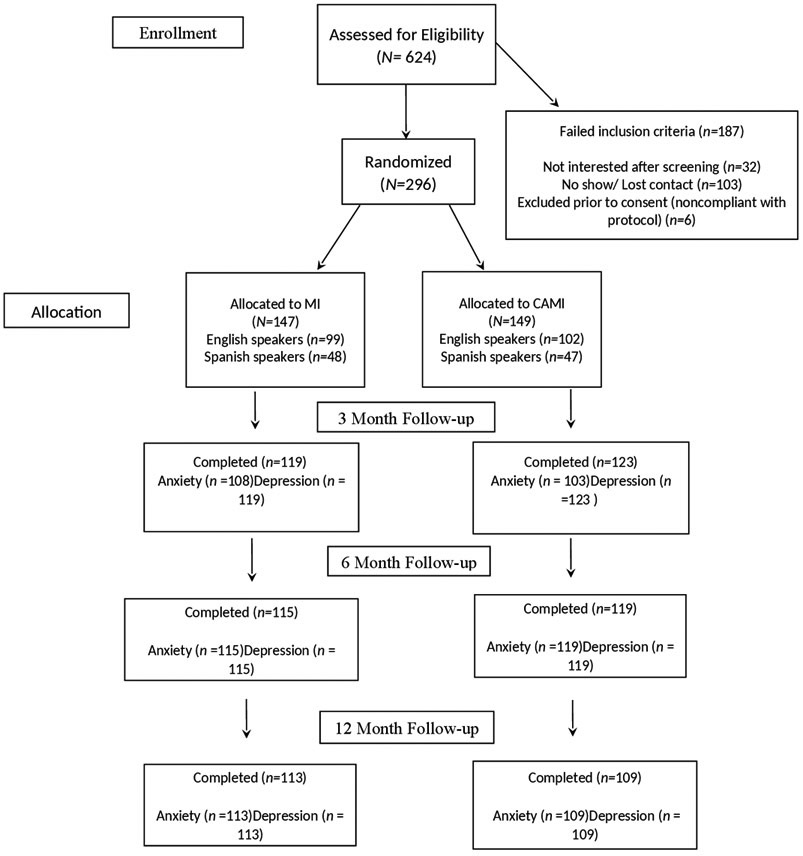
Consort Flow Diagram
All participants completed a baseline assessment and then received one of two intervention conditions (CAMI or MI). Approximately one-third (32%) of all participants received the intervention in Spanish. There were no differences in language delivery by condition (MI in Spanish, 32.7%; CAMI in Spanish, 31.5%). CAMI participants completed two measures (Acculturation Stress and Drinking Behavior Scale, selected items from the Hispanic Stress Inventory (Cervantes, Padilla, & Salgado de Snyder, 1991) that MI participants did not complete. These questions assessed stressors and a distinguishing characteristic of the CAMI was to focus on stressors. Thus, to minimize a “priming” influence (i.e., thinking about stress during baseline assessment) these measures were not administered to MI participants. Yet, if stressors were raised by MI participants, study therapists discussed them in a non-judgmental and curious way. They did not offer the study component on stressors that was designed for the CAMI condition. Follow-up assessments were conducted in person or by phone at 6 and 12 months.
Study Interventions
Both MI and CAMI were delivered in a single face-to-face session designed to last between 60 and 75 minutes. Other publications offer additional detail on the interventions (Lee et al., 2016; Lee et al., 2018). Both conditions were manualized treatments delivered by bilingual therapists.
Motivational interviewing (MI).
The MI included four major elements: (1) building rapport and asking about pros and cons of drinking, (2) discussing their values and goals, (3) exploring normative feedback about their drinking levels and consequences, and (4) collaboratively reviewing an alcohol-related change plan with ideas on how to involve the support of significant others. If participants referred to stressful experiences, these were discussed, but these were not elicited.
Culturally adapted MI (CAMI).
As part of the adaptation, therapists elicited and discussed client thoughts and feelings around the stressor. Specifically, the therapist was trained to elicit and to discuss stressors that had been assessed during the baseline, by asking, “You have told us that in the past, you have had thoughts of drinking in response to a stressor, such as: “Some people dislike me because I am Hispanic”; or “It bothers me that family members I am close to do not understand my new values”. It was hypothesized that by doing so, client self-exploration would generate new thoughts about ways to address their social stressors in healthier ways other than drinking. Using the MI Elicit-Provide-Elicit approach, after asking clients to reflect on a stressful event that led to heavy drinking, therapists elicited their client’s expectancies about how drinking would alleviate their mood, provided information about the physiological effects of drinking, and further discussed participant responses and thoughts about how to address their response to the stressful event in ways that did not involve drinking.
Treatment delivery supervision and training fidelity.
The eleven study therapists (5 female, 6 male) were all Master’s level graduate students (social work, psychology) who received 16 hours of training in MI (including role plays and demonstration of MI principles), and an additional 16 hours learning the manualized MI and CAMI. Training included practice of each component in Spanish and English, including forming reflections in Spanish. The MI study therapists met with the first author in supervision meetings weekly and reviewed audiotapes of their treatment sessions. An objective third-party rater system (Motivational Interviewing Treatment Integrity coding system [MITI; Moyers, Martin, Manuel, Miller, & Ernst, 2010]) was used to monitor treatment fidelity in Spanish and English. The MI trainer (first author) trained 5 Spanish bilingual members of the study team to code MI transcripts in Spanish and in English using the MITI. Sixty-six percent of all sessions were MITI coded using the MITI, exceeding the recommended 20% (Miller & Rollnick, 2014).
MITI data indicates that MI delivered in Spanish and in English, across all coders, met competency thresholds as established in the MITI (Moyers et al., 2010). MITI codes were lower in Spanish than in English, indicating that MI was delivered with greater treatment fidelity in English; this reflects that nearly all study therapists were not native-Spanish speakers (Empathy, Spanish (M=4.27, SD=.33), English (M=4.59, SD=.34), t (33) = 2.77, p = .009), evocation, Spanish, (M=4.34, SD=.38), English (M=4.69, SD=.09); t (33) = 2.4 p = .02), collaboration, Spanish (M=4.24, SD=.42); English (M=4.56, SD=.4); t (33) = 2.31 p = .03), autonomy/support, Spanish (M=4.22, SD=.43); English (M =4.52, SD=.32); t (33) = 2.36, p = .02). The inter-rater reliability was calculated using the intraclass correlation coefficient (ICC), a more conservative measure of inter-rater reliability than other measures because it accounts for differences between raters (Pierson et al., 2007). The MITI ICCs were: Empathy (.69), Evocation (.80), Collaboration (.33), and Autonomy/Support (.80). The MITI ICC for MI-Adherent behaviors was .81. Cichetti’s (1994) categorization system classifies .75-1.00 = excellent, .60-.74 = good, .40-.59 = fair, and below .40 = poor.
Measures
We only describe measures used in the current analyses.
Demographics.
Income was categorized into above and below the Federal Poverty Level for 2012 (United States Department of Health and Human Services (USDHHS; 2013)). To assess effects of U.S. residency, place of birth was categorized as: Foreign-born (born outside U.S. and Puerto Rico), Puerto-Rican Born, and U.S. Mainland Born.
Center for Epidemiologic Depression Scale (CES-D ; Radloff, 1977).
The CES-D assessed level of depressive symptoms at baseline and follow-ups. Items are scored on a four-point Likert scale (0 = none of the time, 3 = most or all of the time). Scores range from 0 to 60; higher scores indicate more severe depressive symptoms. The standard cutoff score indicating higher risk and the need to screen for clinical depression (including in studies that sampled Latinxs), is a score of ≥ 16 (Caetano, 1987; Lewinsohn, Seeley, Roberts, & Allen, 1997; Posner, Stewart, Marin, & Perez-Stable, 2001; Tsai, Pole, Levenson, & Munoz, 2003). Reliability for the entire sample was Cronbach’s α= 0.92 and for Spanish speaking (α= 0.92) and for English-speaking (α= 0.92) participants. The CES-D was collected at baseline (α = .91), 3 months (α = .93), 6 months (α = .92), and 12 months (α = .92).
Beck Anxiety Inventory (BAI; Beck, Epstein, Brown, & Steer, 1988).
The BAI assessed anxiety symptoms at baseline and follow-ups. Respondents are asked to identify how much they were bothered by each anxiety-related symptom during the previous month and the 21 items are rated on a four-point Likert scale (0 = not at all, 1 = mildly, but it didn’t bother me much, 2 = moderately, it wasn’t pleasant at times, 3 = severely, it bothered me a lot). The cutoff score indicating higher risk for anxiety disorders is ≥ 12 (Beck et al., 1988). The BAI is a widely-used measure of anxiety and is available in many languages, including English and Spanish. Beck et al. (1988) found a test-retest reliability of .75 and reported a high level of internal consistency (α = .92). Reliability for the entire sample was α = 0.95 and for Spanish speaking (α= 0.94) and for English-speaking (α= 0.94) participants. Among our sample, the internal consistency was excellent (α = 0.95). The BAI was collected at baseline (α = .94), 3 months (α = .93), 6 months (α = .95), and 12 months (α = .94).
Short Acculturation Scale for Hispanics (SASH; Marin, Sabogal, Marin, Otero-Sabogal, & Perez-Stable, 1987.
The SASH is a 12-item self-report measure that assesses acculturation across three domains: 1) language preference in different contexts (e.g., “In general, what language do you usually speak at home?”); 2) language preference in different media (e.g., In what language is the T.V. program you usually watch?”); and 3) ethnicity of social relations (e.g., Your close friends are…”). For the first two domains, item responses are: 1 = Only Spanish, 2 = More Spanish than English, 3 = Both equally, 4 = More English than Spanish, and 5 = Only English. For Ethnic/Social relations, response options are: 1 = All Latino/as, 2 = more Latino/as than Americans, 3 = About half and half, 4 = more Americans than Latino/as, 5 = All Americans). Higher total scores (sum of 12 items) for the entire scale reflect higher acculturation levels (Ellison, Jandorf, & Duhamel, 2011; Marin et al., 1987; Vella, Ontiveros, Zubia, & Bader, 2011). Reliability for the entire sample was Cronbach’s α= .92 and for the Spanish-speaking (α=.88) and for English-speaking (α=.83) participants. The SASH was collected at baseline.
Everyday Discrimination Scale (EDS; Williams, Yu, Jackson, & Anderson, 1997).
The EDS is a measure that asks participants to rate how often they experienced discrimination in the past 12 months with 4-point Likert scales (1 = never, 4 = often). Reliability for the entire sample was Cronbach’s α = 0.87 and for Spanish-speaking (α=.91) and for English-speaking (α=.85) participants. The EDS was collected at baseline (α = .87) and at 12 months (α = .88).
Data Analytic Strategy
IBM SPSS, Version 25.0 (IBM Corp., 2017) Statistics for PC was used for analyses. Variables were assessed for distributional assumptions of normality and for regression assumptions. Baseline differences on demographic characteristics, variables used as moderators, depression and anxiety symptoms were examined with t tests for continuous variables and with x 2 for dichotomous variables (Table 1). Correlations among study variables were used to evaluate whether there were issues with multicollinearity (r ≥ 90; Table 2). We tested whether the responses were missing completely at random (MCAR) using Little’s (1988) MCAR test in SPSS. Findings showed that the missing responses were MCAR and should not have an impact on the analysis, χ2 (241, N = 296) = 269.80, p = .10.
Table 2.
Correlation Matrix for Everyday Discrimination, Acculturation, Depression, Anxiety, Drinking Consequences, and Percent Heavy Drinking Days
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Discrimination | – | ||||||||||||||||
| 2 | Acculturation | .06 | – | |||||||||||||||
| 3 | Baseline CES-D | .46*** | −.09 | – | ||||||||||||||
| 4 | 3 months CES-D | .30*** | −.04 | .63*** | – | |||||||||||||
| 5 | 6 months CES-D | .32*** | .01 | .67*** | .74*** | – | ||||||||||||
| 6 | 12 months CES-D | .25*** | −.08 | .61*** | .60*** | .68*** | – | |||||||||||
| 7 | Baseline BAI | .40*** | −.02 | .72*** | .52*** | .54*** | .46*** | – | ||||||||||
| 8 | 3 months BAI | .20** | −.16* | .52*** | .70*** | .58*** | .52*** | .61*** | – | |||||||||
| 9 | 6 months BAI | .28*** | −.01 | .50*** | .58*** | .75*** | .55*** | .58*** | .71*** | – | ||||||||
| 10 | 12 months BAI | .21** | −.05 | .43*** | .44*** | .53*** | .68*** | .47*** | .61*** | .63*** | – | |||||||
| 11 | Baseline DrInC | .41*** | −.11 | .55*** | .35*** | .41*** | .30*** | .55*** | .41*** | .49*** | .33*** | – | ||||||
| 12 | 3 months DrInC | .32*** | −.10 | .44*** | .46*** | .49*** | .34*** | .44*** | .52*** | .57*** | .39*** | .79*** | – | |||||
| 13 | 6 months DrInC | .29*** | −.01 | .44*** | .42*** | .58*** | .37*** | .40*** | .46*** | .61*** | .41*** | .69*** | .83*** | – | ||||
| 14 | 12 months DrInC | .27*** | −.05 | .42*** | .34*** | .45*** | .47*** | .41*** | .41*** | .49*** | .58*** | .61*** | .67*** | .73*** | – | |||
| 15 | Baseline PHDD | .16** | −.04 | .25*** | .24*** | .32*** | .22** | .26*** | .17*** | .39*** | .43*** | .27*** | .44*** | .39*** | .39*** | – | ||
| 16 | 3 months PHDD | .14* | −.06 | .26*** | .26*** | .35*** | .26*** | .17* | .29*** | .36*** | .37*** | .36*** | .50*** | .49*** | .51*** | .59*** | – | |
| 17 | 6 months PHDD | .11*** | .03 | .27*** | .29*** | .39*** | .26*** | .20** | .31*** | .40*** | .32*** | .37*** | .43*** | .51*** | .50*** | .54*** | .77*** | – |
| 18 | 12 months PHDD | .17* | −.04 | .32*** | .25*** | .36*** | .28*** | .26*** | .27*** | .39*** | .35*** | .41*** | .46*** | .51*** | .59*** | .56*** | .73*** | .81*** |
Note. Discrimination = Everyday Discrimination Scale; Acculturation = Short Acculturation Scale for Hispanics; CES-D = Center for Epidemiologic Studies Depression Scale; BAI = Beck Anxiety Inventory; DrInC = Drinkers Inventory of Consequences; PHDD = Percent Heavy Drinking Days.
p<.05
p<.01
p<.001
Analyses of primary aims.
Two separate piecewise time-series generalized estimating equations (GEE; Liang & Zeger, 1986) models were used to examine whether levels of anxiety and depressive symptoms were significantly different between baseline assessment and each follow-up time point (3, 6, and 12 months). Treatment condition, discrimination, and acculturation were included as independent variables in the moderation models (Baron & Kenny, 1986) while controlling for variance attributable to demographic characteristics by covarying gender, place of birth, age, and income. GEE analyses examined the main effect of treatment condition (MI, CAMI), the piecewise effect of time (3, 6, and 12 months with baseline as the reference) and each two-way condition x time interaction (Table 3). Depressive symptom outcomes were analyzed with a GEE model with normal distribution and identity link function. Anxiety outcomes were examined using GEE models with a binomial distribution and logit link function. The Wald statistic was used for significance testing of model coefficients.
Table 3.
Analysis of Treatment Main Effects
| Anxiety Symptoms (BAI) | |||
|---|---|---|---|
| Independent variables | B(SE) | Wald | 95% CI |
| Intercept | 18.42(1.41)*** | 170.16 | [15.65, 21.19] |
| Male | −5.07(1.29)*** | 15.39 | [−7.60, −2.54] |
| Place of birth1 | |||
| Puerto Rican born | 2.58(1.44) | 3.19 | [−.25, 5.40] |
| Latin American born | −.12(1.35) | .01 | [−2.76, 2.53] |
| Age | 0.12(.05)** | 7.19 | [0.03, 0.21] |
| Income | −0.32(.20) | 2.53 | [−0.72, 0.08] |
| Acculturation | 1.50(.73)* | 4.27 | [.08, 2.92] |
| Discrimination | 3.62(.61)*** | 35.85 | [2.44, 4.78] |
| Treatment Main Effect | −3.30(.93)*** | 12.62 | [−5.12, −1.48] |
| 3 month follow up | −0.40(.72) | .32 | [−1.81, 1.00] |
| 6 month follow up | −1.33(.86) | 2.38 | [−3.02, 0.36] |
| 12 month follow up | −2.52(.72)*** | 12.32 | [−3.93, −1.11] |
| Depressive Symptoms (CES-D) | |||
| Independent variables | B(SE) | Wald | 95% CI |
| Male | −3.73(1.16)*** | 10.38 | [−6.00, −1.47] |
| Place of birth1 | |||
| Puerto Rican born | 1.28(1.00) | .67 | [−1.80, 4.37] |
| Latin American born | 0.93(1.40) | .44 | [−3.66, 1.81] |
| Age | 0.09(.05) | 3.71 | [−0.002, 0.18] |
| Income | −1.45(.29)*** | 24.70 | [−2.02, −0.88] |
| Acculturation | −0.74(.68) | 1.17 | [−2.07, 0.60] |
| Discrimination | 4.79(.60)*** | 63.03 | [3.61, 5.97] |
| Treatment Main Effect | −2.29(1.07)* | 4.63 | [−4.38, −0.20] |
| 3 month follow up | −0.07(.69) | .01 | [−1.43. 1.29] |
| 6 month follow up | −1.32(.66)* | 4.02 | [−2.61, −0.03] |
| 12 month follow up | −1.76(.71)* | 6.21 | [−3.15, −.38] |
Note. Discrimination = Everyday Discrimination Scale; Acculturation = Short Acculturation Scale for Hispanics; CES-D = Center for Epidemiologic Studies Depression Scale; BAI = Beck Anxiety Inventory.
Place of birth: US-born is the reference category.
p < .05
p < .01
p < .00
Moderation analyses.
GEE models were used to test the hypothesis that baseline acculturation and everyday discrimination would moderate the effects of treatment condition on anxiety and on depressive symptoms. When models were run with gender and place of birth as moderators they were insignificant. To the GEE models described above, the following terms were added: the main effect of the moderator, the three two-way interactions of Moderator x Each Time Point, the two-way interaction of Moderator x Condition, and the 3 three-way interactions of Moderator x Condition x Time (see Table 4). The moderators were continuous measures and centered prior to analysis. We describe the nature of the interactions in our moderation analyses by examining the models of condition effects on outcomes at three levels of the moderator: at the mean, 1 SD above the mean, and 1 SD below the mean (Figure 2).
Table 4.
GEE Moderation of Mental Health Outcomes Models1
| Moderator | ||||||
|---|---|---|---|---|---|---|
| Acculturation | Discrimination | |||||
| Dependent Variable Model Term |
B(SE) | Wald | 95% CI | B(SE) | Wald | 95% CI |
| Anxiety Symptoms (BAI) | ||||||
| Intercept | 2.79(.12)*** | 578.00 | [2.56, 3.02] | 2.79(.11)*** | 625.02 | [2.57, 3.01] |
| Condition X Mod. | −.07(.12) | .32 | [−.31, .17] | .004(.11) | .001 | [−.21, .22] |
| Condition X 3 Mo. | −.16(.12) | 1.63 | [−.40, .08] | −.18(.13) | 2.09 | [−.43, .06] |
| Condition X 6 Mo. | −.30(.13)* | 5.31 | [−.55, −.05] | −.28(.13)* | 4.28 | [−.54, −.02] |
| Condition X 12 Mo. | −.12(.15) | .65 | [−.40, .17] | −.10(.15) | .48 | [−.39, .19] |
| Moderator X 3 Mo. | −.13(.09) | 1.86 | [−.31, .06] | −.13(.07) | 3.05 | [−.27, .02] |
| Moderator X 6 Mo. | −.04(.10) | .18 | [−.23, .15] | −.06(.08) | .45 | [−.22, .11] |
| Moderator X 12 Mo. | −.03(.10) | .10 | [−.22, .16] | −.09(.08) | 1.10 | [−.25, .08] |
| Condition X Mod. X 3 Mo. | .09(.15) | .35 | [−.20, .37] | −.09(.12) | .51 | [−.32, .15] |
| Condition X Mod. X 6 Mo. | .16(.14) | 1.29 | [−.11, .43] | .02(.12) | .02 | [−.21, .25] |
| Condition X Mod. X 12 Mo. | .11(.14) | .60 | [−.17, .39] | −.07(.14) | .27 | [−.35, .20] |
| Moderator | ||||||
| Acculturation | Discrimination | |||||
| Dependent Variable Model Term |
B(SE) | Wald | 95% CI | B(SE) | Wald | 95% CI |
| Depressive Symptoms (CES-D) | ||||||
| Intercept | 3.04(.08)*** | 1637.85 | [2.90, 3.19] | 21.19(1.41)*** | 226.79 | [18.43, 23.95] |
| Condition X Mod. | −.04(.07) | .35 | [−.19, .10] | 1.67(1.29) | 1.67 | [−.86, 4.20] |
| Condition X 3 Mo | −.02(.08) | .05 | [−.18, .14] | −.44(1.38) | .10 | [−3.15, 2.27] |
| Condition X 6 Mo | −.12(.08) | 2.31 | [−.28, .04] | −2.08(1.29) | 2.57 | [−4.61, .461] |
| Condition X 12 Mo | −.18(.09)* | 4.31 | [−.35, −.01] | −2.94(1.36)* | 4.67 | [−5.60, −.27] |
| Moderator X 3 Mo. | .10(.06) | 3.13 | [−.01, .21] | −.63(1.03) | .37 | [−2.64, 1.39] |
| Moderator X 6 Mo. | .09(.06) | 2.40 | [−.02, .20] | .31(1.01) | .10 | [−1.67, 2.30] |
| Moderator X 12 Mo. | .04(.07) | .35 | [−.08, .17] | −.71(.97) | .53 | [−2.61, 1.19] |
| Condition X Mod. X 3 Mo. | −.04(.09) | .23 | [−.21, .13] | −1.29(1.31) | .96 | [−3.86, 1.29] |
| Condition X Mod. X 6 Mo. | .03(.08) | .17 | [−.13, .20] | −1.67(1.30) | 1.65 | [−4.22, .88] |
| Condition X Mod. X 12Mo. | −.06(.09) | .40 | [−.24, .13] | −2.60(1.37)* | 3.61 | [−5.27, .08] |
Gender, place of birth, household income, and age were controlled for in all models.
Note. Acculturation = Short Acculturation Scale for Hispanics; Discrimination = Everyday Discrimination Scale; BAI = Beck Anxiety Inventory. CES-D = Center for Epidemiologic Studies Depression Scale; Mo. = Month; Mod. = Moderator.
p < .05
p < .01
p < .001
Figure 2.
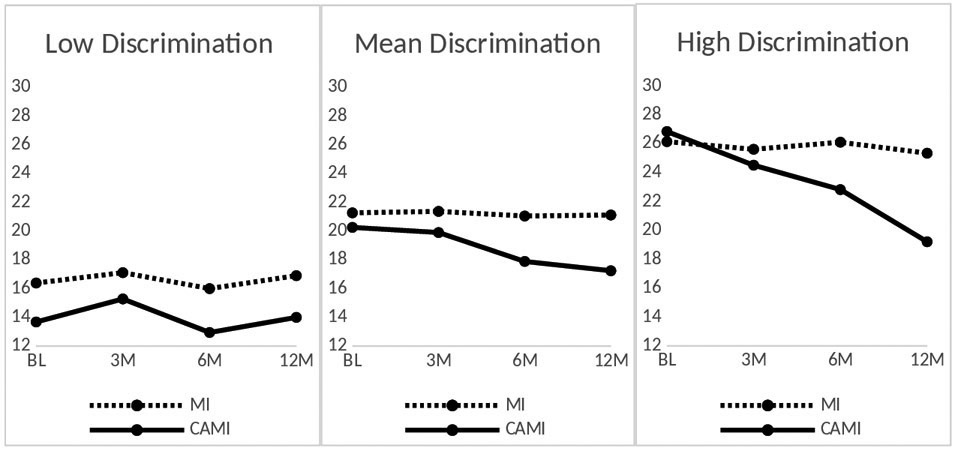
Moderation effects for Discrimination by Depressive Symptoms (CES-D) across 12 months. At higher levels of discrimination at baseline, CAMI participants had significantly lower CES-D scores compared to MI participants at 12 months.
Results
Sample Characteristics
Table 1 presents the baseline demographic characteristics, levels of anxiety and depressive symptoms at baseline and follow-up, and sample sizes. At baseline, there were no significant differences between MI and CAMI participants on: demographic characteristics; substance use (alcohol, marijuana, or other drug use days); covariates; or moderators, in t-tests or chi-squared tests. Forty-nine percent of the total sample (N=145) was Puerto Rican; 45% (n = 66) were mainland U.S. born and 54% (n = 79) were born in Puerto Rico. A comparison of the three birthplace groups revealed that U.S. mainland-born Latinxs (which included Puerto Ricans) had significantly higher levels of acculturation (M = 3.56, SD = .62) than Latinxs born in Puerto Rico (M = 2.65, SD = .89) or elsewhere in Latin America (M = 2.66, SD = .84), F (2,2) = 47.94, p < .001.
Table 2 presents the correlation matrix for the continuous variables in the study. Everyday Discrimination was significantly associated with greater anxiety and depression at all time points. Acculturation scores was not associated with anxiety or depression with the exception of acculturation being significantly correlated with anxiety at 3 months. None of the variables used in the same analyses had issues were multicollinear (r = ≥ .90, Tabachnick & Fidell, 2001).
Main Effects of Treatment
The primary outcomes measures were levels of anxiety and depressive symptoms. Table 3 presents the results for the study outcomes using piecewise time series GEE models evaluating the effect of Treatment Main Effect on levels of anxiety and depression at each time point when compared with baseline assessment after controlling for covariates. Table 4 presents the results of the moderator analyses when added to the main effects models.
Anxiety.
Both conditions showed significantly fewer levels of anxiety symptoms at 12 months compared with baseline after controlling for gender, place of birth, income, discrimination, acculturation, and age (Table 3). CAMI participants reported significantly fewer anxiety symptoms compared to MI participants at six months after controlling for gender, place of birth, income, discrimination, acculturation, and age (Table 4).
Depressive Symptoms.
Both conditions demonstrated significantly fewer levels of depressive symptoms at 6 and at 12 months compared with baseline after controlling for gender, place of birth, household income, discrimination, acculturation, and age (Table 3). CAMI participants reported significantly fewer depressive symptoms compared to MI participants at 12 months after controlling for gender, place of birth, income, discrimination, acculturation, and age (see Table 4).
Moderator effects
Acculturation.
Acculturation did not moderate treatment effects on depression or on anxiety symptoms at any follow-up time points (Table 4).
Everyday Discrimination.
Discrimination did not moderate treatment effects on anxiety at any time points (Table 4). At the 12 month follow-up, the three way interaction of Condition x Discrimination x Time was significant for level of depressive symptoms (Table 4). At higher levels of discrimination, those who received the CAMI had significantly lower levels of depressive symptoms at 12 months compared with those who received standard MI. Figure 2 illustrates the nature of the moderation effect of discrimination on level of depressive symptoms at three levels of the moderator: at the mean, 1 SD above and 1 SD below the mean.
Discussion
Our first hypothesis, that both conditions (CAMI, MI) would result in reduced anxiety/depressive symptoms, was supported. The observed reductions in symptoms of anxiety and depressive symptoms, from clinical to “normal” functioning levels, indicate a “clinically meaningful” result (Beutler & Moleiro, 2001). The baseline average levels of reported anxiety symptoms exceeded the cut points to screen for anxiety disorders (≥12, Beck et al., 1988) and the average level of reported depressive symptoms exceeded the established cut-points for risk of clinical depression (≥ 16, Radloff, 1977). While all participants declined over time on anxiety and depressive symptoms, only CAMI participants decreased from above clinical thresholds (baseline) to below clinical thresholds (12 months) for anxiety and depression. Similarly, improvements in depressive and anxiety symptoms over 6 months were observed among hazardous drinkers in a different clinical trial (Bahorik et al., 2016). These findings underscore the importance of addressing depressive and anxiety symptoms among heavy drinkers (Bahorik et al., 2016; Satre et al., 2016). Untreated depressive symptoms worsen the treatment prognosis for heavy drinkers (Karno & Longabaugh, 2003). Thus, interventions that address mental health symptoms among heavy drinkers are recommended (Bahorik et al., 2016; Satre et al., 2016). Similarly, it is advisable for providers to assess depressive symptoms among individuals with alcohol use disorders because depressive symptoms worsen alcohol treatment outcomes (Karno & Longabaugh, 2003).
Our hypothesis, that CAMI participants would have greater decreases in anxiety and depressive symptoms compared to MI participants, was supported. CAMI participants had significantly lower reported symptoms of anxiety at 6 months and significantly lower symptoms of depression at 12 months relative to MI participants. The main effect on anxiety attenuated after six months. Anxiety symptoms can be a naturally re-occurring response to the daily hassles of living adverse conditions characterized by poverty and unemployment. If this is the case, a booster session targeting symptoms of anxiety may be needed. Altogether, findings suggest that the intervention had additional benefits beyond the primary target (reduction of alcohol use and frequency of adverse consequences related to drinking (Lee et al., 2019). Effects on depressive symptoms lasted up to one year. It is possible that engaging in the CAMI interview helped participants to develop perspectives on their situation, or new skills that helped them to combat depressive symptoms longer-term. However, more investigation is needed to test this notion.
The improvements in mental health found by this investigation converges with a study that randomized psychiatry patients who drank heavily to receive three sessions of MI or a two-page brochure (Satre, et al., 2016). A secondary analysis found that symptoms of depression and anxiety decreased up to six-months among the psychiatry patients who drank heavily and who received MI (Bahorick, et al., 2016). Our findings contribute to the emerging literature on how people with depressive and anxiety symptoms may respond to treatments for alcohol use disorders (Bell, Orford, & Britton, 2015, Satre et al., 2016). Our study sampled more men than women (63%), in contrast to prior reports (Satre et al., 2016), followed participants beyond 6 months to one year, and used MI as an active treatment comparator.
Our second research hypothesis, that acculturation and discrimination would moderate the relationship between treatment condition and depressive/anxiety symptoms, was supported for discrimination only, in the case of depressive symptoms. Among those who reported high levels of discrimination, CAMI participants reported significantly fewer symptoms of depression than MI participants, up to one year following intervention. This treatment moderation effect suggests that the content of the CAMI intervention, which involved discussing social stressors like discrimination, in some way alleviated mental health symptoms. The decline over time in depressive symptoms suggests that talking about stressors in the context of the MI/CAMI confers mental health benefits.
The Causal Theory of Motivational Interviewing (Miller & Rose, 2009) posits that people are more likely to remember their own words. When people heard themselves linking how stressors affects their mood, it might have made this association more salient to them, or may have activated their awareness of an internal discrepancy between the challenging environment and how they would want to cope with it. Also, the CAMI - which prompted participants to discuss various stressful situations and how they responded to them – may have boosted self-efficacy in a culturally valued way. Asking participants to talk about their challenges and how they resolved them may be consistent with the observed Latino cultural value “aguantarse”, or the ability to withstand difficult situations (Añez et al., 2008) and with “poner de su parte”, or doing one’s best to improve circumstances (Interian et al., 2010). This striving and taking personal responsibility to cope with one’s problems is a source of pride (Interian et al., 2010) that might boost self-efficacy to change. Future interventions with Latinxs might be more impactful if they were strengths-based and focused on the cultural appreciation for personal resiliency in the face of adversity.
In contrast, discrimination did not moderate treatment effects on anxiety symptoms. The null finding is surprising given that depressive and anxiety symptoms shared 46-56% variance in common across time in this study (Table 2). A possible explanation is that we started measuring anxiety after the start of the clinical trial, so there were fewer participants in whom to analyze anxiety as an outcome. The finding that discrimination moderated treatment effects on depression but not on anxiety highlights the need for further research investigating within-group differences on discrimination, anxiety, depression, and hazardous drinking.
Acculturation did not moderate the relationship between treatment condition and depressive/anxiety symptoms. This finding contrasted with the parent clinical trial findings showing that acculturation was a treatment moderator for alcohol outcomes; CAMI was favored over MI specifically among less-acculturated participants (Lee et al., 2018). Why would acculturation be a treatment moderator for alcohol but not mental health outcomes? The null finding may be due to the fact that unidimensional measurement of acculturation as linguistic preference (for media, in social contexts), has been found to be an inconsistent predictor of other health outcomes (Abraido-Lanza, Armbrister, Florez, & Aguirre, 2006). Thus acculturation should be investigated more broadly than as a measure of linguistic preference in health outcome studies. Second, we may not see the effect for acculturation as hypothesized because our study sample includes U.S. born Latinxs who are significantly more acculturated. Other studies of acculturation and mental health have focused on less acculturated individuals (e.g., Interian et al., 2010, Griner et al., 2006). Our findings point to the need for further investigation on the relationship between acculturation and health risk behaviors across Latinx subgroups to improve the sensitivity of interventions.
Limitations include the fact that the study was conducted primarily with Latinxs in the Northeast, so results are of limited generalizability to Latinx communities in other parts of the country. Our study is also limited by our measurement of acculturation as linguistic preference. That said, our study supports the association of stressors (e.g., discrimination) to mental distress. Our study is consistent with the clinical applications of Minority Stress Theory (Meyer, 2003), by indicating that targeting such stressors during intervention might decrease mental health symptoms. Future studies should examine how changes in heavy drinking might impact changes in anxiety/depressive symptoms, as well as the interrelationships between symptoms over time, particularly among those with both anxiety and depression. Interventions that address underlying factors (i.e. stressful experiences) common to alcohol use, anxiety, and depression should also consider these dynamic, changing relationships. Given the nature of migration and settlement in the U.S., the relationship between anxiety and post-traumatic stress disorder among immigrant Latinxs is another important area of inquiry.
In sum, interventions that include discussion of the social context may contribute to improvements in psychological distress. Future interventions for populations who experience similar social stressors should address mental health symptoms because doing so may improve the impact of treatment on addictive behaviors. MI can be used to help people talk about stressors involved in immigration and their response to stressors. Resulting mental health benefits extended beyond alcohol outcomes alone.
Acknowledgments:
This study was supported by award numbers R01AA021136 and by T32 007459 from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) of the National Institutes of Health (NIH).
References
- Abraido-Lanza AF, Armbrister AN, Florez KR, & Aguirre AN (2006). Toward a theory-driven model of acculturation in public health resarch. American Journal of Public Health, 96 98), 1342–1346. Doi: 10.2015/AJPH.2005.064980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abraido-Lanza AF, Echeverria SE, & Florez KR (2016). Latino immigrants, acculturation, and health: Promising new directions in research. Annual Review of Public Health, 37, 219–236. Doi: 10.1146/annurev-publhealth-032315-021545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychological Association, APA Working Group on Stress and Health Disparities. (2017). Stress and health disparities: Contexts, mechanisms, and interventions among racial/ethnic minority and low-socioeconomic status populations. Retrieved from http://www.apa.org/pi/health-disparities/resources/stress-report.aspx.
- Añez LM, Silva MA, Paris M Jr., Bedregal LE (2008). Engaing Latinos through the integration of cultural values and motivational interviewing principles. Professional Psychology Research and Practice, 39(2), 153–159. doi: 10.1037/0735-7028.39.2.153 [DOI] [Google Scholar]
- Araújo Dawson B, & Panchanadeswaran S (2010). Discrimination and acculturative stress among first-generation Dominicans. Hispanic Journal of Behavioral Sciences, 32(2), 216–231. 10.1177/0739986310364750 [DOI] [Google Scholar]
- Arkowitz H , & Burke BL ( 2008). Motivational interviewing as an integrative framework for the treatment of depression In Arkowitz H , Westra HA , Miller WR , & Rollnick S (Eds.), Motivational interviewing in the treatment of psychological problems, (pp. 145–172). New York: Guilford. [Google Scholar]
- Bahorik AL, Leibowitz A, Sterling SA, Travis A, Weisner C, & Satre DD 92016). The role of hazardous drinking reductions in predicting depression and anxiety symptom improvement among psychiatry patients: A longitudinal study. Journal of Affective Disorders, 206, 169–173. 10.1916/j.jad.2016.07.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron RM, & Kenny DA (1986). The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173 – 1182. [DOI] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, & Steer RA (1988). An inventory for measuring clinical anxiety: psychometric properties. Journal of Consulting and Clinical Psychology, 56(6), 893–897. 10.1037/0022-006X.56.6.893 [DOI] [PubMed] [Google Scholar]
- Bell S, Orford J, Britton A (2015). Heavy drinking and mental health: an exploration of the dynamic 10-year longitudinal relationship in a prospective cohort of untreated heavy drinkers. Alcohol: Clinical and Experimental Research, 39, 688–696. doi: 10.111/acer.12681 [DOI] [PubMed] [Google Scholar]
- Beutler LE, & Moleiro C (2001). Clinical versus reliable and significant change. Clinical Psychology: Science and Practice, 8(4), 441–445. doi: 10.1093/clipsy.8.4.441 [DOI] [Google Scholar]
- Breslau N, Schultz LR, Johnson EO, Peterson EL, & Davis GC (2005). Smoking and the risk of suicidal behavior: a prospective study of a community sample. Archives of General Psychiatry, 62(3), 328–334. doi: 10.1001/archpsyc.62.3.328 [DOI] [PubMed] [Google Scholar]
- Brofenbrenner U (1994). Ecological models of human development. International Encyclopedia of Education, 3(2), p. 37–43. [Google Scholar]
- Caetano R (1987). Acculturation and drinking patterns among U.S. Hispanics. Addiction, 82(7), 789–799. 10.1111/j.1360-0443.1987.tb01546.x [DOI] [PubMed] [Google Scholar]
- Cano MA, de Dios MA, Castro Y, Vaughan EL, Castillo LG, Lorenzo-Blanco EI, Piña-Watson B, Berger Cardoso J, Ojeda L, Cruz RA, Correa-Fernandez V, Ibañez G, Afu R, & Modella LM (2015). Alcohol use severity and depressive symptoms among late adolescent Hispanics: Testing associations of acculturation and enculturation in a bicultural transaction model. Addictive Behaviors, 49, 278–82. doi: 10.1016/j.addbeh.2015.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cano MA, Sanchez M, Trepka MJ, Dillon FR, Sheehan DM, Rojas P, … de la Rosa M (2017). Immigration stress and alcohol use severity among recently immigrated Hispanic adults: Examining moderating effects of gender, immigration status, and social support. Journal of Clinical Psychology, 73(3), 294–307. doi: 10.1002/jclp.22330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Ball SA, Nich C, Martino S, Frankforter TL, Farentinos C, ... National Institute on Drug Abuse Clinical Trials Network. (2006). Motivational interviewing to improve treatment engagement and outcome in individuals seeking treatment for substance abuse: a multisite effectiveness study. Drug and Alcohol Dependence, 81(3), 301–12. https://dx.doi.org/10.1016%2Fj.drugalcdep.2005.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cervantes RC, Padilla AM, & Salgado de Snyder N (1991). The Hispanic Stress Inventory: A culturally relevant approach to psychosocial assessment. Psychological Assessment, 3, 438–447. 10.1037/1040-3590.3.3.438. [DOI] [Google Scholar]
- Cicchetti DV (1994). Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychological Assessment, 6(4), 284. [Google Scholar]
- Ellison J, Jandorf L, & Duhamel K (2011). Assessment of the Short Acculturation Scale for Hispanics among low-income, immigrant Hispanics. Journal of Cancer Education, 26(3), 478–83. doi: 10.1007/s13187-011-0233-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field C, & Caetano R (2010). The role of ethnic matching between patient and provider on the effectiveness of brief alcohol interventions with Hispanics. Alcoholism: Clinical and Experimental Research, 34(2), 262–271. 10.1111/j.1530-0277.2009.01089.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Kaplan K (2004). Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry 61 (8), 807–816. doi: 10.1001/archpsyc.61.8.807 [DOI] [PubMed] [Google Scholar]
- Griner D, & Smith TB (2006). Culturally adapted mental health intervention: A meta-analytic review. Psychotherapy: Theory, Research, Practice, Training, 43, 531–548. doi: 10.1037/0033-3204.43.4.531 [DOI] [PubMed] [Google Scholar]
- Hall GCN, Ibaraki AY, Huang ER, Marti CN, & Stice E (2016). A meta-analysis of cultural adaptations of psychological interventions. Behavior Therapy, 47(6), 993–1014. https://doi-org.ezproxy.neu.edu/10.1016/j.beth.2016.09.005 [DOI] [PubMed] [Google Scholar]
- Hasin DS, & Grant BF 92015). The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Waves 1 and 2: review and summary of findings. Social Psychiatry and Psychiatric Epidemiology, 50, 1609–1640. DOI 10.1007/s00127-015-1088-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckman CJ, Egleston BL, & Hoffman MT (2010). Efficacy of motivational interviewing for smoking cessation: a systemic review and meta-analysis. Tobacco Control, 19(5), 410–416. doi: 10.1136/tc.2009.033175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hettema J, Steele J, & Miller WR (2005). Motivational interviewing. Annual Review of Clinical Psychology, 1, 91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833 [DOI] [PubMed] [Google Scholar]
- Hiott A, Grzywacz JG, Arcury TA, & Quandt SA (2006). Gender differences in anxiety and depression among immigrant Latinos. Families, Systems, & Health, 24(2), 137–146. doi: 10.1037/1091-7527.24.2.137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp. [Google Scholar]
- Interian A, Martinez I, Rios LI, Krejci J, & Guarnaccia PJ (2010). Adaptation of a motivational interviewing intervention to improve antidepressant adherence among Latinos. Cultural Diversity and Ethnic Minority Psychology, 16(2), 215–225. DOI: 10.1037/a0016072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karno MP & Longabaugh R (2003). Patient depressive symptoms and therapist focus on emotional material: A new look at Project MATCH. Journal of Studies on Alcohol and Drugs, 64(5), 607. doi: 10.15288/jsa.2003.64.607 [DOI] [PubMed] [Google Scholar]
- Karch DL, Barker L, Strine TW (2006). Race/ethnicity, substance abuse, and mental illness among suicide victims in 13 US states: 2004 data from the National Violent Death Reporting System. Injury Prevention, 12 (Suppl II), ii22–ii27. doi: 10.1136/ip2006/013557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin AE (2007). Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology, 3, 1–27. 10.1146/annurev.clinpsy.3.022806.091432 [DOI] [PubMed] [Google Scholar]
- Keeley RD, Brody DS, Engel M, Burke BL Nordstrom K, Moralez E, Dickinson LM, & Emsermann C (2016). Motivational interviewing improves depression outcome in primary care: A cluster randomized trial. Journal of Consulting and Clinical Psychology, 84(11), 993–1007. doi: 10.1037/ccp0000124 [DOI] [PubMed] [Google Scholar]
- Keyes KM, Hatzenbuehler ML, & Hasin DS (2011). Stressful life experiences, alcohol consumption, and alcohol use disorders: the epidemiologic evidence for four main types of stressors. Psychopharmacology, 218(1), 1–17. doi: 10.1007/s00213-011-2236-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Liu XC, & Cerda M (2011). The role of race/ethnicity in alcohol-attributable injury in the United States. Epidemiologic Reviews, 34, 89–102. DOIL 10.1093/epirev/mxr018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, & Agras WS (2002). Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry, 59, 877–883. 10.1001/archpsyc.59.10.877 [DOI] [PubMed] [Google Scholar]
- Lee CS, Almeida J, Colby SM, Tavares T, & Rohsenow DJ (2016). Acculturation, hazardous drinking and depressive symptomatology among Hispanics enrolled in a clinical trial. Addiction Research and Theory, 24(1), 69–79. Doi: 10.3109/16066359.2015.1072517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee CS, Colby SM, Magill M, Almeida J, Tavares T, & Rohsenow DJ (2016). A randomized controlled trial of culturally adapted motivational interviewing for Hispanic heavy drinkers: Theory of adaptation and study protocol. Contemporary Clinical Trials, 50, 193–200. doi: 10.1016/j.cct.2016.08.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee CS, Colby SM, Rohsenow DJ, Martin R, Rosales R, McCallum TT, Falcon L, Almeida J, & Cortés DE (2019). A randomized controlled trial of motivational interviewing tailored for heavy drinking Latinxs. Journal of Consulting and Clinical Psychology, 87 (9), 815–830. 10.1037/ccp0000428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, Seeley JR, Roberts RE, & Allen NB (1997). Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychology of Aging, 12(2), 277–287. 10.1037/0882-7974.12.2.277 [DOI] [PubMed] [Google Scholar]
- Lewis-Fernández R, Morcillo C, Wang S, Duarte CS, Aggarwal NK, Sánchez-Lacay JA, & Blanco C (2016). Acculturation dimensions and 12-month mood and anxiety disorders across US Latino subgroups in the National Epidemiologic Survey of Alcohol and Related Conditions. Psychological Medicine, 46(9), 1987–2001. https://doi.org/10/1017/50033291760000763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang KY, & Zeger SL (1986). Longitudinal data analysis using generalized linear models. Biometrika, 73(1), 13–22. 10.1093/biomet/73.1.13 [DOI] [Google Scholar]
- Little RJA (1988). A test of missing completely at random for multivariate data with missing values. Journal of the American Statistical Association, 83(404), 1198–1202. doi: 10.2307/2290157 [DOI] [Google Scholar]
- Lundahl B, & Burke BL (2009). The effectiveness and applicability of motivational interviewing: a practice-friendly review of four meta-analyses. Journal of Clinical Psychology, 65(11), 1232–1245. doi: 10.1002/jclp.20638 [DOI] [PubMed] [Google Scholar]
- Lundahl B, Moleni T, Burke BL, Butters R, Tollefson D, Butler C, & Rollnick S (2013). Motivational interviewing in medical care settings: A systematic review and meta-analysis of randomized controlled trials. Patient Education and Counseling, 93(2), 157–168. doi: 10.1016/j.pec.2013.07.012 [DOI] [PubMed] [Google Scholar]
- Marin G, Sabogal F, Marin BV, Otero-Sabogal R, & Perez-Stable EJ (1987). Development of a short acculturation scale for Hispanics. Hispanic Journal of Behavioral Science, 9, 183–205. 10.1177/07399863870092005 [DOI] [Google Scholar]
- Mendelson T, Rehkopf DH, & Kubzansky LD, (2008). Depression among Latinos in the United States: A meta-analytic review. Journal of Consulting and Clinical Psychology, 76(3), 355–366. doi: 10.1037/0022-006X.76.3.355. [DOI] [PubMed] [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, & Rollnick S (2014). The effectiveness and ineffectiveness of complex behavioral interventions: Impact of treatment fidelity. Contemporary Clinical Trials, 37,234–241. 10.1016/j.cct.2014.01.005 [DOI] [PubMed] [Google Scholar]
- Miller WR, & Rose GS (2009). Motivational Interviewing in a Relational Context. American Psychologist, 64(5), 298–299. 10.1037/a0019487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyers TB, & Martin T (2006). Therapist influence on client language during motivational interviewing sessions. Journal of Substance Abuse Treatment, 30(3), 245–251. 10.1016/j.jsat.2005.12.003 [DOI] [PubMed] [Google Scholar]
- Moyers T, Martin T, Manuel J, Miller W, & Ernst D (2010). Revised Global Scales: Motivational Interviewing Treatment Integrity 3.1. 1 (MITI 3.1. 1). Unpublished manuscript, University of New Mexico, Albuquerque, New Mexico: Retrieved from https://casaa.unm.edu/download/miti3_1.pdf [Google Scholar]
- Mulia N, Ye Y, Greenfield TK, & Zemore SE (2009). Disparities in alcohol-related problems among white, black, and Hispanic American. Alcoholism: Clinical and Experimental Research, 33(4), 654–662. doi: 10.1111/j.1530-0277.2008.00880.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nalven T, & Spillane NS (2018). A Conceptual Framework for Understanding Alcohol Use Problems in Racial/Ethnic Minorities: The Role of Impulsivity and Stress In Braddon C (Ed.), Understanding Impulsive Behavior: Assessment, Influences and Gender Differences (pp. 99–120). New York, NU: Nova Science Publishers. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism [NIAAA] (2006). Why do adolescents drink, what are the risks, and how can underage drinking be prevented? Retrieved from https://pubs.niaaa.nih.gov/publications/AA67/AA67.htm.
- Ornelas IJ, & Perreira KM (2011). The role of migration in the development of depressive symptoms among Latino immigrant parents in the USA. Social Science & Medicine, 73(8), 1169–1177. doi: 10.1016/j.socscimed.2011.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Lelutiu-Weinberger C, Botsko M, & Golub SA (2014). A randomized controlled trial utilizing motivational interviewing to reduce HIV risk and drug use in young gay and bisexual men. Journal of Consulting and Clinical Psychology, 82(1), 9–18. 10.1037/a0035311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierson HM, Hayes SC, Gifford EV, Roget N, Padilla M, Bissett R, et al. (2007). An examination of the Motivational Interviewing Treatment Integrity Code. Journal of Substance Abuse Treatment, 32, 11–17. doi: 10.1016/j.jsat.2006.07.001. [DOI] [PubMed] [Google Scholar]
- Posner SF, Stewart AL, Marin G, & Perez-Stable EJ (2001). Factor variability of the Center for Epidemiological Studies Depression Scale (CES-D) among urban Latinos. Ethnicity and Health, 6(2), 137–144. doi: 10.1080/13557850120068469 [DOI] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. 10.1177/014662167700100306 [DOI] [Google Scholar]
- Satre DD, Travis A, Leibowitz A, Sterling SA, Lu Y, & Weisner C (2016). A randomized clinical trial of motivational interviewing to reduce alcohol and drug use among patients with depression. Journal of Consulting and Clinical Psychology, 84(7), 571–579. 10.1037/ccp00000096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sleath BL & Williams JW (2004) Hispanic ethnicity, language, and depression: Physician-patient communication and patient use of alternative treatments. International Journal of Psychiatry in Medicine 34(3), 235–246. 10.2190/VQU1-QYWT-XW6Y-4M14 [DOI] [PubMed] [Google Scholar]
- Stewart JS (2012). A critical appraisal of motivational interviewing within the field of alcohol misuse. Journal of Psychiatric and Mental Health Nursing, 19, 933–938. 10.1111/j.1365-2850.2012.01880.x [DOI] [PubMed] [Google Scholar]
- Sullivan LE, Fiellin DA, O’Connor PG (2005). The prevalence and impact of alcohol problems in major depression: a systematic review. American Journal of Medicine, 118, 330–341. 10.1016/j.amjmed.2005.01.007 [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, & Fidell LS (2001). Using Multivariate Statistics (4th ed.). Boston: Allyn & Bacon. [Google Scholar]
- Torres L, Driscoll MW, & Voell M (2012). Discrimination, acculturation, acculturative stress, and Latino psychological distress: A moderated mediational model. Cultural Diversity and Ethnic Minority Psychology, 18(1), 17–25. doi: 10.1037/a0026710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torres P, Romano E, Voas RB, de la Rosa M, & Lacey JH (2014). The relative risk of involvement in fatal crashes as a function of race/ethnicity and blood alcohol concentration. Journal of Safety Research, 48, 95–101. 10.1016/j.jsr.2013.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai JL, Pole N, Levenson RW, & Munoz RF (2003). The effects of depression on the emotional responses of Spanish-speaking Latinas. Cultural Diversity and Ethnic Minority Psychology, 9(1), 49–63. 10.1037/1099-9809.9.1.49 [DOI] [PubMed] [Google Scholar]
- United States Census Bureau. (2017). Facts for Features: Hispanic Heritage Month. Retrieved from https://www.census.gov/newsroom/facts.for.features/2017/hispanic-heritage.html.
- United States Department of Health and Human Services [USDHHS] (2013). 2013 poverty guidelines. Retrieved from https://aspe.hhs.gov/2013-poverty-guidelines.
- Vasquez EP, Gonzalez-Guarda RM, & De Santis JP (2011) Acculturation, depression, self-esteem, and substance abuse among Hispanic men. Issues in Mental Health Nursing, 32(2), 90–97. doi: 10.3109/01612840.2010.528169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vella CA, Ontiveros D, Zubia RY, & Bader JO (2011). Acculturation and metabolic syndrome risk factors in young Mexican and Mexican–American women. Journal of Immigrant and Minority Health, 13, 119–126. doi: 10.1007/s10903-009-9299-7 [DOI] [PubMed] [Google Scholar]
- Westra HA, Arkowitz H, & Dozois DJ (2009). Adding a motivational interviewing pretreatment to cognitive behavioral therapy for generalized anxiety disorder: A preliminary randomized controlled trial. Journal of Anxiety Disorders, 23(8), 1106–1117. doi: 10.1016/j.janxdis.2009.07.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Yu Y, Jackson JS, & Anderson NB (1997). Racial differences in physical and mental health: Socioeconomic status, stress, and discrimination. Journal of Health Psychology, 2(3), 335–351. doi: 10.1177/135910539700200305 [DOI] [PubMed] [Google Scholar]


