Dear Editor,
Governmental lockdown measures to prevent the uncontrolled spreading of the novel coronavirus diseases (COVID-19) are effective (Nussbaumer-Streit et al., 2020) but can decrease mental health (Brooks et al., 2020). For example, depression rates (measured with the PHQ-8 10-points cut-off) were 4% in 2014 and increased to 20% during the COVID-19 lockdown in Austria (Pieh et al., 2020). It is less known if depression changes when lockdown measures are lifted and who is at risk to still have depression after lockdown. Only one study addressed the question how mental health changes in vs. after quarantine (Brooks et al., 2020) but this previous study focused on anxiety and anger (Jeong et al., 2016). In the current study, we explored changes of depression in vs. after lockdown and whether stress and loneliness during the lockdown affect subsequent depression after the COVID-19 lockdown in Austria. Stress and loneliness were selected since they have been found to be associated with depression (Hammen, 2005; Heinrich and Gullone, 2006) and are relevant problems in times of COVID-19 (Holmes et al., 2020).
The Austrian lockdown started 16th of March 2020 (only five exceptions of the ban to enter public places: activities to avert an immediate danger to life, limb, or property; professional activity if home-office is not possible; errands to cover necessary basic needs; care and assistance for people in need of support; exercise outdoors alone and with pets / people living in the same household) and most restrictions ended between beginning of May and beginning of June 2020 (e. g., 1st of May: movement restrictions ended; 2nd of May: stores and shopping centers larger than 400m2, barbershops, beauty salons opened; 4th of May: senior year student returned to school; retirement homes allowed visitors; 15th of May: restaurants and bars opened, religious services allowed; 18th of May: school resumed for 6-14 years old; 29th of May: hotels, public swimming pools, zoos, other attractions opened, events up to 100 people allowed; 3rd of June: all age groups resumed school).
To investigate changes in depression in vs. after lockdown in Austrian adults, a repeated measures online survey was performed by Qualtrics with the first wave during the lockdown from 10th to 30th of April 2020 and the second wave after the lockdown from 11th to 22nd of June 2020. The study was approved by the ethics committee of the Danube University Krems, Austria. The first wave comprised 1,005 individuals (representative for age, gender, education, region) and 445 of them took part in the second wave. The 445 responders were analyzed in the present study. Of these 445 participants, 53.0% were female and most of them were 45-54 (24.5%), 55-64 (18.4%), or 35-44 (17.5%) years old. Depression was measured with the PHQ-9 (potential range: 0-27), stress with the PSS-10 (potential range: 0-40), and loneliness with the 11-item version of the De Jong Gierveld Scale (potential range: 0-11).
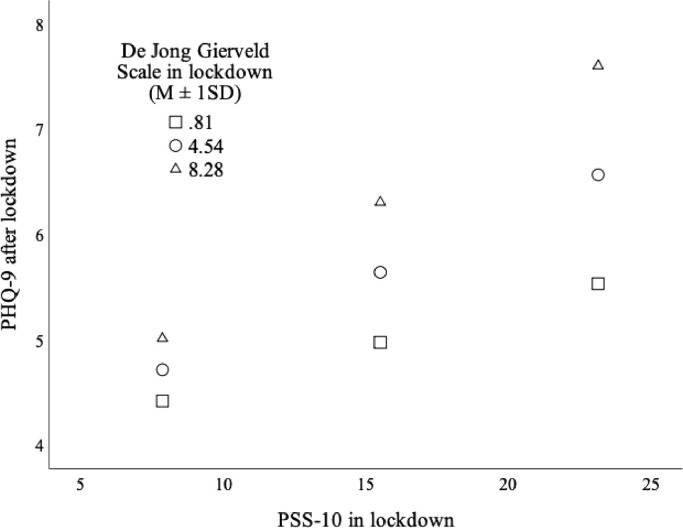
A t-test for dependent samples showed that PHQ-9 scale scores did not change in vs. after lockdown (in lockdown: M=5.76 (SD= 5.10); after lockdown: 5.83 (SD= 5.35); t(444)=-0.41; p=0.679). Yet, a McNemar test revealed that categories of depression severity (PHQ-9 scores dichotomized with the ≥10-points cut-off) changed significantly (p=0.027). More individuals changed from not depressed in lockdown to depressed after lockdown (n=39, 8.8%) as compared to from depressed in lockdown to not depressed after lockdown (n=21, 4.7%). These results imply that depression did not improve in the weeks after lifting lockdown measures and that additional factors besides lockdown measures might play a role in increased depression rates in times of COVID-19. To examine the role of stress and loneliness in lockdown on depression after lockdown, a moderation analysis was performed with PROCESS (model 1 with 10,000 bootstrap samples; predictor: PSS-10 scale in lockdown; outcome: PHQ-9 scale after lockdown; moderator: De Jong Gierveld Scale in lockdown; covariate: PHQ-9 scale in lockdown). Results of this model showed that there was an interaction effect of stress and loneliness in lockdown on depression after lockdown (F(1;440)=4.53; p=0.034). As visualized in Fig. 1 , higher stress combined with higher loneliness in lockdown had the most detrimental effect on depression after lockdown. The moderator value defining the Johnson–Neyman significance region was a De Jong Gierveld Scale score of 0.77 (% below: 16.40; % above 83.60). The results of this moderation analysis show that only those not experiencing loneliness (below 1-point on the De Jong Gierveld Scale) during the lockdown were protected from the effect of stress in lockdown on subsequent depression after lockdown. These results are in line with another current study highlighting the effect of loneliness on depression in times of COVID-19 (Palgi et al., 2020). Limitations of the present study are the rather low response rate and the lack of clinical interviews to assess depression.
Fig. 1.
Visualization of the effect of stress (PSS-10) in lockdown moderated by loneliness (De Jong Gierveld Scale) in lockdown on depression (PHQ-9) after lockdown when controlling for depression (PHQ-9) in lockdown.
Authors' contribution
T.P. drafted the manuscript, performed the statistical analyses, and contributed in study design; S.B. contributed in study design and revised the manuscript; C.P. contributed in study design and revised the manuscript
Funding
None
Declaration of Competing Interest
The authors have no conflict of interest to report.
Acknowledgements
None
References
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C. Stress and depression. Annu. Rev. Clin. Psychol. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- Heinrich L.M., Gullone E. The clinical significance of loneliness: a literature review. Clin. Psychol. Rev. 2006;26:695–718. doi: 10.1016/j.cpr.2006.04.002. [DOI] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., Worthman C.M., Yardley L., Cowan K., Cope C., Hotopf M., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeong H., Yim H.W., Song Y.J., Ki M., Min J.A., Cho J., Chae J.H. Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiol. Health. 2016;38 doi: 10.4178/epih.e2016048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nussbaumer-Streit B., Mayr V., Dobrescu A.I., Chapman A., Persad E., Klerings I., Wagner G., Siebert U., Christof C., Zachariah C., Gartlehner G. Quarantine alone or in combination with other public health measures to control COVID-19: a rapid review. Cochrane Database Syst. Rev. 2020;4 doi: 10.1002/14651858.CD013574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palgi Y., Shrira A., Ring L., Bodner E., Avidor S., Bergman Y., Cohen-Fridel S., Keisari S., Hoffman Y. The loneliness pandemic: loneliness and other concomitants of depression, anxiety and their comorbidity during the COVID-19 outbreak. J. Affect. Disord. 2020 doi: 10.1016/j.jad.2020.06.036. 2020accepted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pieh C., Budimir S., Probst T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J. Psychosom. Res. 2020 doi: 10.1016/j.jpsychores.2020.110186. accepted. [DOI] [PMC free article] [PubMed] [Google Scholar]