Abstract
Background
Coronavirus disease 2019 (COVID-19) has become global pandemic and resulted in considerable morbidity and mortality since December 2019. Information on the incidence of myocardial injury remains scarce.
Methods
English-language databases (PubMed, Embase, Cochrane), Chinese-language databases (CNKI, VIP, WANFANG), and preprint platform were searched to identify studies that reported the myocardial injury data in COVID-19 patients. Random-effects meta-analyses were used to derive the pooled incidence and relative risks (RRs) of myocardial injury. Variations by disease severity were examined by subgroup analyses. Sensitivity analyses were performed to strengthen the results. Meta-regression was applied to explore the risk factors associated with myocardial injury.
Results
A total of 53 studies involving 7,679 patients were included. The pooled incidence of myocardial injury was 21% [95% confidence interval (CI), 17–25%; I2, 96.5%]. The highest incidence of myocardial injury was found in non-survivors (66%; 95 CI%, 54–78%; I2, 85.7%), followed by severe patients (43%; 95 CI%, 33–53%; I2, 93.0%) and non-severe patients (11%; 95 CI%, 7–15%; I2, 95.2%). Higher risk of myocardial injury was detected in severe patients than non-severe patients (RR, 5.74; 95% CI, 3.74–8.79; I2, 86.8%). All the sensitivity analyses confirmed the robustness of primacy results.
Conclusions
This meta-analysis showed that myocardial injury occurred in 21% of COVID-19 patients. An elevated rate was observed in non-survivors (66%) and severe patients (43%). Severe patients had a 4.74-fold increase in the risk of myocardial injury than non-severe patients. Aggressive strategy may be considered for COVID-19 patients at high risk of myocardial injury.
Keywords: Severe acute respiratory syndrome coronavirus 2 (SAR-CoV-2), coronavirus disease 2019 (COVID-19), myocardial injury, incidence, meta-analysis
Introduction
Since December 2019, coronavirus disease 2019 (COVID-19) caused by the newly discovered severe acute respiratory syndrome coronavirus 2 (SAR-CoV-2) has been recognized as a major public health issue due to rapidly global pandemic, resulting in 7,823,289 confirmed infections and 431,541 deaths worldwide by 15 June 2020 (1). Previous studies have described the main findings of clinical and epidemiological characteristics in COVID-19 patients (2-4). With the increase of confirmed cases and the accumulation of clinical data, the cardiovascular manifestations caused by COVID-19 has raised concern. Myocardial injury, defined as elevated levels of troponin or creatine kinase isoenzyme (CK-MB) regardless of new abnormalities in electrocardiography and echocardiography, have been reported with the rate of 7.2% in the initial COVID-19 study (4). Two recent studies presented 19.7% to 27.8% of patients with COVID-19 had acute myocardial injury (5,6). Obviously, incidence of myocardial injury in this viral infection remains uncertain. The pathophysiology of COVID-associated myocardial injury have not well established but likely involve the direct damage to cardiomyocytes, systemic inflammation, myocardial interstitial fibrosis, interferon mediated immune response, exaggerated cytokine response, in addition to coronary plaque destabilization, and hypoxia (7). Apart from COVID-19 itself, there are other factors associated with myocardial injury in these patients, which include cardiovascular risk factors (smoking, hypertension, obesity, physical inactivity, advanced age), severe forms of the disease and medications such as hydroxychloroquine or chloroquine (7-9). Currently published meta-analyses have reported that more myocardial injury happened in severe COVID-19 patients, which was subsequently associated with deteriorative outcomes [mortality and need for intensive care unit (ICU) care] (10-12). Nevertheless, no study until now have given a full picture for myocardial injury incidence in patients with COVID-19. The present study therefore summarized all available evidence for a comprehensive and rigorous systematic review focused on myocardial injury incidence in COVID-19. In addition, to state the case-fatality rate related to cardiac injury, variations of myocardial injury incidence were also examined by disease severity (non-survivors, severe patients, and non-severe patients). We present the following article in accordance with the PRISMA reporting checklist (available at http://dx.doi.org/10.21037/cdt-20-535).
Methods
This systematic review and meta-analysis was established according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement. The authors declare that all supporting data are available within the article and in the Supplementary file.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The ethical approval and consent are not required because no patient-level data is involved for this systematic review and meta-analysis.
Data sources and searches
Relevant studies were identified by performing English-language searches of PubMed, Embase, Cochrane Library databases (through April 24, 2020) as well as Chinese-language searches of China National Knowledge Infrastructure (CNKI), China Science and Technology Journal Database (VIP), WANFANG databases (through April 23, 2020) using the search terms related to COVID-19. The full search strategy is outlined in Table S1. Preprint articles were retrieved from the websites of MedRxiv (https://www.medrxiv.org), BioRxiv (https://www.biorxiv.org), and SSRN (https://www.ssrn.com) (through April 24, 2020). Manual search was also conducted by screening the reference lists of inclusive studies and relevant meta-analysis.
Study selection and outcomes
Studies of any types [case series study, cross-sectional study, case control study, cohort study, or randomized controlled trial (RCT)] were eligible for inclusion if they included SARS-CoV-2 infected adult patients; reported the qualitative data of cardiac specific biomarkers (troponin or CKMB); or reported the data of myocardial injury with detailed definition. Studies were excluded if they did not report defined myocardial injury indexes or published in meta-analysis or case report. Because of the difficulty to estimate the potentially repetitive patients, all the studies met the inclusion criteria were available for meta-analysis. Two authors (ZG and CZ) independently reviewed each title and abstract, and assessed full texts of retrieved studies, with any disagreements being resolved via consultation with a third author (JP). The primary outcomes of this study were the incidence of myocardial injury in COVID-19 and corresponding relative risk (RR) in comparison between severe and non-severe patients. COVID-19 patients was the laboratory diagnosis using real time reverse transcription-polymerase chain reaction (RT-PCR) assay or clinical diagnosis based on the Guidance for COVID-19 (7th edition) released by the National Health Commission of China. Myocardial injury was defined as serum levels of troponin or CK-MB above the 99th percentile upper reference limit, regardless of new abnormalities in electrocardiography and echocardiography. Severe patients were judged according to the Guidance for COVID-19 (7th edition) released by the National Health Commission of China (13).
Data extraction and quality assessment
Two authors (ZG and CZ) independently extracted the data using a priori designed form: which included study characteristics (study name, study source, regions, detailed hospital), patient characteristics (included period, illness severity, diagnosis standard for COVID-19, myocardial injury definition and its cut-off value), clinical characteristics (age, gender, smoking, and the comorbidities of hypertension, diabetes, cardiovascular disease (CVD), cerebrovascular disease, chronic pulmonary disease, chronic kidney disease, liver disease, and cancer), and data on cardiac injury (occurrence number and total number). The methodological quality of included RCTs was evaluated according to Cochrane Collaboration Risk of Bias Tool (14). The methodological quality of each included observational studies was assessed according to the Newcastle-Ottawa Scale (NOS) (15). To fit in our study design, the NOS was modified with totally 8 scores and the following 6 dimensions: representative of the sample; ascertainment of the exposure; ascertainment of the outcome; ascertainment of the outcome for quality control; control for factors of age and gender; and control for factors related to myocardial injury. A study can be awarded a maximum of 1 point for the first 4 dimensions and a maximum of 2 points for the last 2 dimensions (control for factors of age and gender: 1 point for age and 1 point for sex; control for factors related to myocardial injury: 1 point for reporting 1 or 2 comorbidities and 2 points for reporting ≥3 comorbidities). The total scores of ≥5 points represented a relatively good quality.
Data synthesis and statistical analysis
A random-effects (DerSimonian and Laird method) meta-analysis was used to calculate the pooled incidence of myocardial injury with 95% confidence intervals (95% CIs). Likewise, RRs of myocardial injury comparing severe with non-severe patients was performed. Heterogeneity among studies was assessed using the Cochran Q test and I2 index, with I2 >50% representing considerable heterogeneity (16). Subgroup analysis was conducted by the severity of illness (non-survivors, severe patients, and non-severe patients). The interaction analysis (P for interaction) using Cochran’s Q test were applied to evaluate the risk difference of different illness severity (17). Interaction is referred to as effect modification, which investigates whether the effect of intervention in the primacy outcome varied between the subgroup such as disease severity. A leave-1-out sensitivity analysis for each meta-analysis was applied to explore whether a single study had an excessive influence on myocardial injury incidence. To strengthen the robustness of the results, further serial sensitivity analyses were conducted by including studies that real time RT-PCR assay was performed using a SARS-CoV-2 nucleic acid detection, or studies that used troponin or electrocardiography or echocardiography as definition of myocardial injury, or excluding studies that involved potentially repetitive patients in the same hospital with period within range of other studies; or excluding studies that sample size were <50. To address the potential risk factors associated with myocardial injury, all preexisting cardiovascular risk factors or established diseases will be taken into consideration in the meta-regression. As a rule, at least 25% data points should be available for each variable in univariable meta-regression. The presence of publication bias was evaluated qualitatively by funnel plots and quantitatively by Begg’s test and Egger’s test when more than 10 studies were available in a single analysis (18). Trim and fill method was used to deal with the publication bias. The trim and fill method requires no assumptions about the mechanism that lead to publication bias, provides an estimate of the number of missing studies, and also provides an estimated intervention effect to adjust the publication bias. Data were analyzed using Stata version 13.0 (StataCorp., College Station, TX, USA).
Results
Study selection and study characteristics
As outlined in Figure 1, initial search identified 5,449 records from English-language databases, 7,023 from Chinese-language databases, and 3,401 from preprint platform; 1,509 duplicates were removed and 14,077 records were excluded by screening titles and abstracts; the remaining 287 full-text articles were reviewed and 234 articles were excluded with the following reasons: studies were irrelevant (n=94), studies did not report outcome of myocardial injury (n=103), studies were meta-analyses, and studies was repetitive with other database (n=7). Finally, 53 studies involving 7,679 COVID-19 patients were included, with 24 from English-language databases, 10 from Chinese-language databases, and 19 from preprint platform. Among them, 21 studies (39%) were cross-sectional studies, 16 (30%) were case-series studies, 14 (26%) were case-control studies, and 2 (5%) were cohort studies. Twenty-eight studies (53%) were conducted in Hubei, 22 (41%) in regions outside Hubei, 2 (4%) in both Hubei and other regions, and 1 in New York (Table S2). The majority of studies (48/53, 91%) used RT-PCR method for confirming COVID-19. The remaining 5 studies used RT-PCR method or clinical diagnosis definition for confirming COVID-19. Thirty-three studies (62%) used troponin, 11 (21%) applied troponin or electrocardiography or echocardiography, and the remaining 9 (17%) employed CK-MB as cardiac injury definition (Table S3). The number of included COVID-19 patients varied from 8 to 1,327. The mean age was 54 years and the percentage of male was 54.1%. Other detailed information on comorbidities is summarized in Table S4.
Figure 1.
Flow diagram for the selection of eligible studies. CNKI, China National Knowledge Infrastructure; VIP, China Science and Technology Journal Database.
Study quality
All included studies satisfied the following risk bias items: representative of the sample; ascertainment of the exposure; ascertainment of the outcome; and control for factors of age and gender. Twenty-three studies (43%) defined the myocardial injury in the text (ascertainment of the outcome for quality control); 37 studies (70%) reported more than 3 comorbidities (2 points) and 11 studies (21%) reported 1 or 2 comorbidities (1 point). Eventually, all 53 studies were rated as relatively good quality (Table S5).
Incidence of myocardial injury
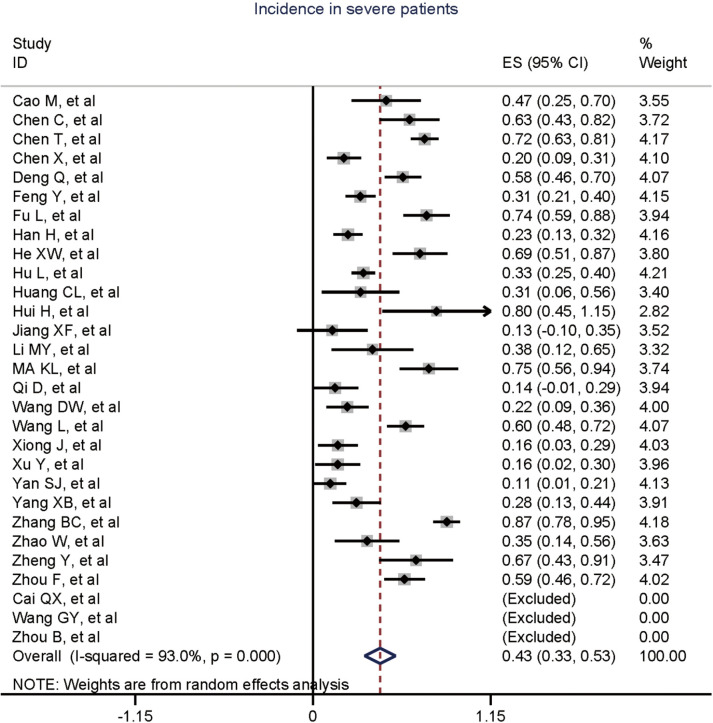
Figure 2 gives the full picture of myocardial injury incidence. The overall pooled incidence of myocardial injury was 21% (95% CI, 17–25%; I2, 96.5%; Figure S1). For severity of illness, the highest incidence of myocardial injury was found in non-survivors (66%; 95% CI, 54–78%; I2, 85.7%; Figure S2), followed by severe patients (43%; 95% CI, 33–53%; I2, 93.0%; Figure S3) and non-severe patients (11%; 95% CI, 7–15%; I2, 95.2%; Figure S4), with significant difference (Pinteraction <0.01). Sensitivity analyses by removing a single study at 1 time; or including studies that patients were detected with RT-PCR assay; or including studies that cases were defined as troponin; or excluding studies that involved potentially repetitive patients or sample size were <50 confirmed the robustness of primacy results (Table S6 and Figures S5,S6,S7,S8).
Figure 2.
Incidence of cardiac injury. No., number; 95% CI, 95% confidence interval; EKG, electrocardiography; Echo, echocardiography.
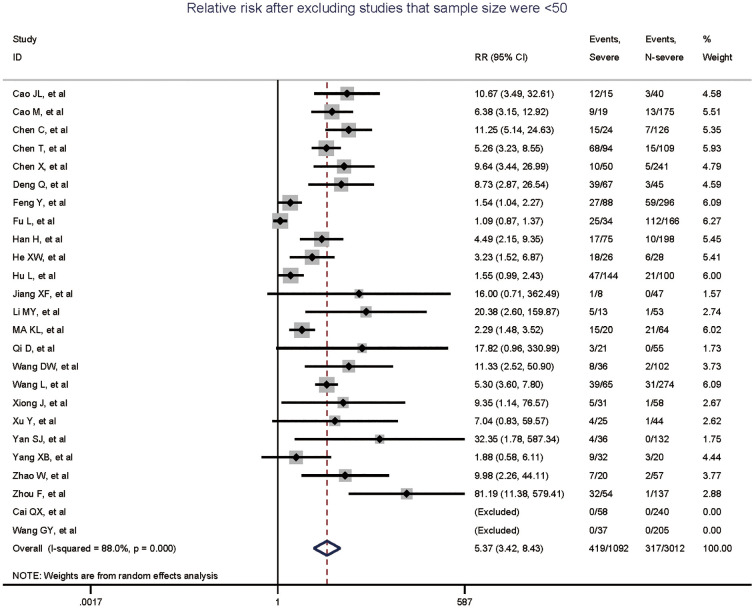
Comparison of myocardial injury risk with severe versus non-severe patients
Totally, 29 studies involving 4,233 patients were identified, and the incidence of myocardial injury was 39.3% in severe patients (445/1,133) compared with 10.4% (322/3,100) in non-severe patients (Figure 3), indicating that severe patients were associated with significantly higher risk of myocardial injury (RR, 5.74; 95% CI, 3.74–8.79; I2, 86.8%; Figure S9). Leave-1-out sensitivity analyses as well as further serial sensitivity analyses were in consistence with the primacy results (Figures S10,S11,S12,S13,S14). Meta-regression failed to detect any clinical characteristics and comorbidities to impact the primacy results (Table S7).
Figure 3.
Cardiac injury risk of severe patients versus non-severe patients. No., number; RR, relative risk; 95% CI, 95% confidence interval; EKG, electrocardiography; Echo, echocardiography.
Risk factors associated with myocardial injury
The association between various comorbidities and myocardial injury incidence is shown in Table S8. Eleven variables with more than 25% data points (age, gender, smoking, hypertension, diabetes, CVD, cerebrovascular disease, chronic pulmonary disease, chronic kidney disease, liver disease, and cancer) were assessed in univariable meta-regression. The results suggested that the incidence of myocardial injury were not associated with any of the above comorbidities.
Publication bias
The funnel plots for myocardial injury incidence in overall patients, in severe patients, and in non-severe patients were all asymmetrical on visual inspection, and the corresponding P values for the Egger’s test were <0.001, 0.972, and 0.004, respectively (Figure S15). The trim and fill method was applied to handle publication bias, resulting in 9% (95% CI, 5–14%) for incidence in overall patients and 4% (95% CI, 1–7%) for incidence in non-severe patients (Table S9). Because of limited study number in non-survivors (8 studies), funnel plot was not performed.
Discussion
Major findings and interpretations
This systematic review and meta-analysis firstly provided a comprehensive overview of myocardial injury incidence based on 53 retrospective studies involving 7,679 COVID-19 patients. The major findings were as follows: (I) the overall incidence of myocardial injury was 21%; (II) considering the severity of disease, myocardial injury incidence progressively increased in non-survivors (66%), severe patients (43%), and non-severe patients (11%); (III) severe patients had a 4.74-fold increased risk of myocardial injury compared with non-severe patients. Previous study found that COVID-19 patients who were admitted to the ICU had higher plasma levels of cytokines (3). As cytokine storm is one of the potential mechanisms underlying myocardial injury, it is predictable that incidence of myocardial injury might be high among non-survivors and severe patients.
Comparison with previous studies
Currently, several systematic reviews and meta-analyses have been conducted to assess the risk of myocardial injury among COVID-19 patients. The earliest one, which pooled 4 studies of 341 patients, showed that the values of troponin were significantly increased in severe patients than that in non-severe patients [standardized mean difference (SMD), 25.6 ng/L; 95% CI, 6.8–44.5 ng/L] (10). Although this is the first meta-analysis to assess the myocardial injury risk in COVID-19, the limitation of study number and sample size may influence the robustness of results. Another meta-analysis addressed this issue by merging 28 studies of 4,189 patients and found that myocardial injury biomarkers were higher in severe patients compared with less severe patients (SMD, 0.69; 95% CI, 0.48–0.89) (11). Notably, this study used a broadly definition of myocardial injury (the combination of troponin, CK-MB, NT-proBNP, and myoglobin), which inevitably led to the overestimation of myocardial injury risk. The recent meta-analysis involving 2,389 patients from 13 studies reported that myocardial injury was associated with higher mortality (RR, 7.95; 95% CI, 5.12–13.34) and need for ICU care (RR, 7.94; 95% CI, 1.51–41.78) (12). This study used a precise definition of myocardial injury (troponin above the 99th percentile upper reference limit, regardless of new abnormalities in electrocardiography and echocardiography), whereas risk factors of myocardial injury as well as visible publication bias seemingly not to be well addressed. Given the above limitations, the present meta-analysis restricted the definition of myocardial injury and included all available evidence to comprehensively estimate the incidence and potential risk factors of myocardial injury in COVID-19 patients.
Potential mechanism of myocardial injury
The mechanisms underlying myocardial injury have not well established but likely involve viral myocarditis, cytokine storm, microvascular thrombosis, and unmasked CVDs. Evidence from autopsies found that 35% of heart samples in SAR-CoV infected patients presented the viral genome, which raised the possibility of direct impair of cardiomyocytes by the virus (19). SAR-CoV-2 might share the same mechanism as the highly homologous with SAR-CoV. Nevertheless, a recent pathological study failed to demonstrate the presence of SAR-CoV-2 within myocardial tissue (20). Therefore, the question of whether the SAR-CoV-2 could directly damage the heart requires further scientific verification. Guo et al. found that plasma troponin levels had a significantly positive linear correlation with plasma high-sensitivity C-reactive protein (hs-CRP) levels, indicating that myocardial injury may be associated with inflammatory pathogenesis during the disease progress (5). Besides hs-CRP, other cytokines, including interleukin (IL)-2, IL-7, IL-10, IgG-included protein 10, monocyte chemoattractant protein-1, macrophage inflammatory protein 1-alpha, and tumors necrosis factor, were proved to be involved in the inflammatory response of COVID-19 (3). The activation of these inflammatory cytokines after infection might cause endothelial dysfunction, coronary plaque destabilization, microvascular dysfunction, and subsequently contribute to myocardial injury. Predictably, this marked inflammatory response could also lead to the development of disseminated intravascular coagulopathy (DIC) in critical patients. Tang et al. reported that coagulopathy was associated with high mortality and 71% of non-survivors met the criteria of DIC (21). As such, microvascular thrombosis of coronary vessels due to DIC is another potential mechanism that might contribute to myocardial injury. In addition, COVID-19 patients preexisting CVD and other comorbidities might be more likely to suffer from myocardial injury. Shi et al reported that approximately 30% and 60% of patients with myocardial injury had a history of coronary heart disease and hypertension, respectively, which were more prevalent than in those without myocardial injury (6). Although limited evidence exists for evaluating the association of myocardial injury with cardiovascular comorbidities, it is rational to presume that patients with underlying comorbidities are susceptible to myocardial injury through several mechanisms including virus-driven direct damage, systemic inflammatory response, coronary plaque destabilization, and hypoxia aggravation. Regrettably, we only obtained study-level information about comorbidities and failed to detect any risk factors associated with myocardial injury.
Clinical consideration for myocardial injury
Given the high incidence of myocardial injury among COVID-19 patients, it might be reasonable to triage patients according to cardiovascular comorbidities and myocardial biomarkers. The majority of patients with a mildly elevated troponin can be followed with expectant management until recovery from acute viral syndrome. However, patients whom are hemodynamically and electrophysiologically unstable with marked elevations of troponin should launch earlier and more aggressive intervention strategies.
Strengths and limitations
Strengths of this study mainly include the systematic and rigorous approach to estimate the incidence of myocardial injury. We performed a comprehensive search of English-language databases, Chinese-language, and preprint platform; restricted the definition of myocardial injury; used the revised NOS tool to suitably assess the study quality; conducted the subgroup analyses by disease severity to explore for differences on myocardial injury incidence; performed serial sensitivity analyses to strengthen the robustness of results; applied meta-regression to explore the risk factors associated with myocardial injury; and employed trim and fill method to handle the potential publication bias. Certainly, several intrinsic limitations should be recognized in this study. Firstly, all included studies were retrospective and there were differences on diagnosis criterion for COVID-19 and definition of myocardial injury. To account for these issues, we have conducted sensitivity analyses by only including studies that patients were detected with RT-PCR assay or cases were defined as troponin. The results of sensitivity analyses were in line with the primacy results. Secondly, given the difficulty of performing echocardiography or cardiac magnetic resonance imaging under strict isolation, the exact prevalence and nature of myocardial injury in COVID-19 may difficult to be fully illuminating. Thus, in the present study, we used myocardial enzymology indexes as the definition of myocardial injury. Thirdly, we did not obtain patient-level information about comorbidities and concomitant medication for exploring the potential risk factors of myocardial injury. Also, all the included studies did not report the adjusted RRs related to cardiac injury, thus the pooled RRs from crude data may introduce certain bias. Fourthly, there was significant heterogeneity among included studies and the sources of heterogeneity could be partly explained by disease severity. Finally, we did not assess the clinical diagnosis (angina, myocardial infarction, etc.) associated with elevated myocardial enzymes as well as the dynamic change of troponin and the association between myocardial injury and mortality.
Conclusions
This meta-analysis showed that 21% of patients undergoing myocardial injury in the setting of COVID-19. Higher incidence of myocardial injury was observed in non-survivors (66%) and severe patients (43%). Severe patients had a 4.74-fold increased risk of myocardial injury compared to non-severe patients. Aggressive intervention strategy might be considered for COVID-19 patients at high risk of myocardial injury.
Acknowledgments
Funding: This study was supported by the Research Funds of Shanghai Health and Family Planning commission (20184Y0022), Cultivation fund of clinical research of Renji Hospital (PY2018-III-06), Clinical Pharmacy Innovation Research Institute of Shanghai Jiao Tong University School of Medicine (CXYJY2019ZD001, CXYJY2019QN004), and Program for Key but Weak Disciplines of Shanghai Municipal Commission of Health and Family Planning (2016ZB0304).
Supplementary
Incidence of myocardial injury in COVID-19: a pooled analysis of 7,679 patients from 53 studies.
Figure S1.
Overall incidence of cardiac injury.
Figure S2.
Incidence of cardiac injury in non-survivors.
Figure S3.
Incidence of cardiac injury in severe patients.
Figure S4.
Incidence of cardiac injury in non-severe patients.
Figure S5.
Incidence of cardiac injury in patients detected with RT-PCR method. RT-PCR, reverse transcription-polymerase chain reaction.
Figure S6.
Incidence of cardiac injury in cases defined as troponin.
Figure S7.
Incidence of cardiac injury after excluding potentially repetitive patients.
Figure S8.
Incidence of cardiac injury after excluding studies that sample size <50.
Figure S9.
RR of cardiac injury with severe vs. non-severe patients. RR, relative risk.
Figure S10.
Leave-1-out sensitivity analysis for RR of severe patients vs. non-severe patients. RR, relative risk.
Figure S11.
RR of cardiac injury with severe vs. non-severe patients (RT-PCR). RR, relative risk; RT-PCR, reverse transcription-polymerase chain reaction.
Figure S12.
RR of cardiac injury with severe vs. non-severe patients (troponin). RR, relative risk.
Figure S13.
RR of cardiac injury with severe vs. non-severe patients after excluding potentially repetitive patients. RR, relative risk.
Figure S14.
RR of cardiac injury with severe vs. non-severe patients after excluding studies that sample size <50. RR, relative risk.
Figure S15.

Publication bias on the incidence of cardiac injury [(A) overall; (B) severe patients; (C) non-severe patients].
Table S1. Search strategy used in April 24, 2020.
| Literature databases | Search items | Items found |
|---|---|---|
| PubMed | COVID-19[Title/Abstract] OR 2019-nCov[Title/Abstract] OR novel coronavirus[Title/Abstract] OR Wuhan coronavirus[Title/Abstract] OR Wuhan pneumonia [Title/Abstract] OR SARS-CoV-2[Title/Abstract] OR coronavirus 2019[Title/Abstract] | 5,110 |
| Embase | 'covid 19':ab,ti OR '2019 ncov':ab,ti OR 'novel coronavirus':ab,ti OR 'wuhan coronavirus':ab,ti OR 'wuhan pneumonia':ab,ti OR 'sars cov 2':ab,ti OR 'coronavirus 2019':ab,ti AND NOT ([embase]/lim AND [medline]/lim) | 271 |
| Cochrane | (COVID-19):ti,ab,kw OR (novel coronavirus):ti,ab,kw OR (Wuhan coronavirus):ti,ab,kw OR (Wuhan pneumonia):ti,ab,kw OR (SARS-CoV-2):ti,ab,kw OR (coronavirus 2019):ti,ab,kw | 68 |
| Overall | – | 2,188 |
| Duplication | – | 3,940 |
Table S2. Characteristics of the included studies.
| Study name | Study source | Study design | Country | Region | Hospital in detail |
|---|---|---|---|---|---|
| Ai et al. (22) | Preprint platform | Cross-sectional | China | Hubei | Xiangyang No. 1 People’s Hospital |
| Cai et al. (23) | English database | Cross-sectional | China | Hubei outside | Third People’s Hospital of Shenzhen |
| Cao et al. (24) | English database | Cross-sectional | China | Hubei | Zhongnan Hospital of Wuhan University |
| Cao et al. (25) | Preprint platform | Cross-sectional | China | Hubei outside | Shanghai Public Health Clinical Centre |
| Chen et al. (26) | Chinese database | Case-control | China | Hubei | Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology |
| Chen et al. (27) | English database | Case-control | China | Hubei | Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology |
| Chen et al. (2) | English database | Case-control | China | Hubei | Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology |
| Chen et al. (28) | Preprint platform | Cross-sectional | China | Hubei outside | The first Hospital of Changsha and Loudi Central Hospital |
| Deng et al. (29) | English database | Case-control | China | Hubei | Renmin Hospital of Wuhan University |
| Fan et al. (30) | Preprint platform | Cross-sectional | China | Hubei | Wuhan Jinyintan Hospital |
| Fang et al. (31) | Chinese database | Cross-sectional | China | Hubei outside | Anhui Provincial Hospital |
| Feng et al. (32) | Chinese database | Case-series | China | Hubei outside | The First Hospital of Lanzhou University |
| Feng et al. (33) | English database | Cross-sectional | China | Hubei and other regions | Wuhan Jinyintan Hospital, Shanghai Public Health Clinical Center, and Anhui Tongling People’s Hospital |
| Fu et al. (34) | English database | Case-control | China | Hubei | Union Hospital, Tongji Medical College, Huazhong University of Science and Technology |
| Fu et al. (35) | Preprint platform | Case-control | China | Hubei | Union Hospital, Tongji Medical College, Huazhong University of Science and Technology |
| Guo et al. (5) | English database | Case-control | China | Hubei | The Seventh Hospital of Wuhan |
| Han et al. (36) | English database | Cross-sectional | China | Hubei | Renmin Hospital of Wuhan University |
| He et al. (37) | Chinese database | Case-control | China | Hubei | Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology |
| Hong et al. (38) | Chinese database | Case-control | China | Hubei outside | The Fifth Affiliated Hospital of Sun Yat-sen University |
| Hu et al. (39) | English database | Cross-sectional | China | Hubei | Tianyou Hospital, Wuhan University of Science and Technology |
| Huang et al. (3) | English database | Case-series | China | Hubei | Wuhan Jinyintan Hospital |
| Huang et al. (40) | English database | Case-series | China | Hubei | Zhongnan Hospital of Wuhan University |
| Hui et al. (41) | English database | Case-series | China | Hubei outside | Beijing Youan Hospital |
| Jiang et al. (42) | Preprint platform | Case-series | China | Hubei outside | Wuxi Fifth People’s Hospital |
| Li et al. (43) | Chinese database | Case-control | China | Hubei outside | Guangzhou Eighth People’s Hospital |
| Li et al. (44) | Preprint platform | Case-series | China | Hubei | Renmin Hospital of Wuhan University |
| Liu et al. (45) | Preprint platform | Case-control | China | Hubei outside | Guangzhou Eighth People’s Hospital |
| Ma et al. (46) | English database | Cross-sectional | China | Hubei outside | Chongqing Yongchuan Hospital |
| Petrilli et al. (47) | Preprint platform | Cross-sectional | U.S.A. | New York | NYU Langone Health |
| Qi et al. (48) | Preprint platform | Cross-sectional | China | Hubei outside | Qianjiang Central Hospital of Chongqing, Chongqing Three Gorges Central Hospital, and Chongqing Public Health Medical Center |
| Qiu et al. (49) | Preprint platform | Cross-sectional | China | Hubei outside | The First People’s Hospital of Huaihua and the Central Hospital of Shaoyang |
| Shi et al. (10) | English database | Case-control | China | Hubei | Renmin Hospital of Wuhan University |
| Tian et al. (50) | Preprint platform | Cross-sectional | China | Hubei outside | The First Hospital of Jilin University, Changchun Infectious Disease Hospital and Siping Infectious Disease Hospital |
| Wang et al. (4) | English database | Cross-sectional | China | Hubei | Zhongnan Hospital of Wuhan University |
| Wang et al. (51) | English database | Cross-sectional | China | Hubei outside | The Second Xiangya Hospital of Central South University |
| Wang et al. (52) | English database | Cross-sectional | China | Hubei | Renmin Hospital of Wuhan University |
| Wang et al. (53) | Chinese database | Case-series | China | Hubei outside | Jinhua Municipal Central Hospital |
| Wu et al. (54) | English database | Cohort | China | Hubei | Wuhan Jinyintan Hospital |
| Wu et al. (55) | English database | Case-series | China | Hubei outside | The First People’s Hospital of Yancheng City, The Fifth People’s Hospital of Wuxi, The second People’s Hospital of Yancheng City |
| Xiong et al. (56) | Chinese database | Case-series | China | Hubei | Renmin Hospital of Wuhan University |
| Xu et al. (57) | Preprint platform | Case-control | China | Hubei outside | West China Second University Hospital, Sichuan University |
| Xu et al. (58) | Preprint platform | Case-series | China | Hubei and other regions | Zhongnan Hospital of Wuhan University, Chinese PLA General Hospital, Peking Union Medical College Hospital, and affiliated hospitals of Shanghai University of Medicine & Health Sciences |
| Yan et al. (59) | Preprint platform | Cross-sectional | China | Hubei outside | The Second Affiliated Hospital of Hainan Medical University |
| Yang et al. (60) | Chinese database | Case-series | China | Hubei outside | Nanjing Public Health Medical Center |
| Yang et al. (61) | English database | Cross-sectional | China | Hubei | Wuhan Jinyintan Hospital |
| Zhang et al. (62) | Preprint platform | Case-series | China | Hubei | Renmin Hospital of Wuhan University |
| Zhang et al. (63) | English database | Case-control | China | Hubei | Wuhan No. 1 Hospital |
| Zhang et al. (64) | Chinese database | Case-series | China | Hubei | Wuhan Huo Shen-Shan Hospital |
| Zhao et al. (65) | Preprint platform | Case-series | China | Hubei outside | Beijing Youan Hospital |
| Zheng et al. (66) | Preprint platform | Case-series | China | Hubei outside | The First Affiliated Hospital, College of Medicine, Zhejiang University |
| Zhou et al. (67) | English database | Case-series | China | Hubei | Union Hospital, Tongji Medical College, Huazhong University of Science and Technology |
| Zhou et al. (68) | English database | Cohort | China | Hubei | Wuhan Jinyintan Hospital and Wuhan Pulmonary Hospital |
| Zhou et al. (69) | Preprint platform | Cross-sectional | China | Hubei | Yichang Central People’s Hospital and Yichang Third People’s Hospital |
Table S3. Population, diagnosis, and cardiac injury definition of the included studies.
| Study | Population period | Population | Diagnosis standard | Definition | Cut-off value |
|---|---|---|---|---|---|
| Ai et al. (22) | NR–2020.2.9 | NR | RT-PCR | CK-MB | 24 U/L |
| Cai et al. (23) | 2020.1.11–2020.2.9 | Non-severe and severe patients | RT-PCR | CK-MB | NR |
| Cao et al. (24) | 2020.1.3–2020.2.1 | Survivors and non-survivors | RT-PCR | TNI | 26 pg/mL |
| Cao et al. (25) | 2020.1.20–2020.2.15 | Non-ICU and ICU patients | RT-PCR | TNI | 0.04 ng/mL |
| Chen et al. (26) | 2020.1.1–2020.2.29 | Non-severe and severe patients | RT-PCR | TNI | NR |
| Chen et al. (27) | 2019.12–2020.1.27 | Moderate and severe patients | RT-PCR | TNI or EKG or Echo | NR |
| Chen et al. (2) | 2020.1.13–2020.2.12 | Survivor and non-survivor patients | RT-PCR | TNI | 15.6 pg/mL |
| Chen et al. (28) | 2020.1.23–2020.2.14 | Mild, Moderate, and Severe (critical) patients | RT-PCR | CK-MB | 24 U/L |
| Deng et al. (29) | 2020.1.6–2020.2.20 | Non-severe and severe patients | RT-PCR | TNI | 0.04 ng/mL |
| Fan et al. (30) | 2019.12.30–2020.2.16 | Non-ICU and ICU patients | RT-PCR or clinical diagnosis | TNI | 10 U/L |
| Fang et al. (31) | 2020.1.22–2020.2.18 | Mild-moderate, severe, and critical patients | RT-PCR | TNI | 0.3 μg/L |
| Feng et al. (32) | 2020.1.23–2020.2.23 | NR | RT-PCR or clinical diagnosis | CK-MB | NR |
| Feng et al. (33) | 2020.1.1–2020.2.15 | Moderate, severe, and critical patients | RT-PCR | TNI | 0.04 ng/mL |
| Fu et al. (34) | 2020.1.1–2020.1.30 | Survivors and non-survivors | RT-PCR | TNI | NR |
| Fu et al. (35) | 2020.2.9–2020.3.17 | Good recovery and poor recovery patients | RT-PCR or clinical diagnosis | TNI | 26.2 ng/L |
| Guo et al. (5) | 2020.1.23–2020.2.23 | NR | RT-PCR | TNT | NR |
| Han et al. (36) | 2020.1.1–2020.2.18 | Mild, severe, and critical patients | RT-PCR | TNI | 0.04 ng/mL |
| He et al. (37) | 2020.2.3–2020.2.24 | Survivors and non-survivors | RT-PCR | TNI | 34.3 ng/L |
| Hong et al. (38) | 2020.1.17–2020.3.1 | NR | RT-PCR | TNI | NR |
| Hu et al. (39) | 2020.1.8–2020.2.20 | Non-severe, severe, and critical patients | RT-PCR or clinical diagnosis | TNI | 0.04 pg/mL |
| Huang et al. (3) | 2019.12.16–2020.1.2 | Non-ICU and ICU patients | RT-PCR | TNI or EKG or Echo | >28 pg/mL |
| Huang et al. (40) | 2019.12.21–2020.1.28 | NR | RT-PCR | TNI | NR |
| Hui et al. (41) | 2020.1.21–2020.2.3 | Mild, moderate, severe, and critical patients | RT-PCR | TNI | |
| Jiang et al. (42) | 2020.1.23–2020.2.16 | Non-severe and severe patients | RT-PCR | TNI or EKG or Echo | NR |
| Li et al. (43) | 2020.1.20–2020.2.10 | Mild, moderate, severe, and critical patients | RT-PCR | TNI | NR |
| Li et al. (44) | 2020.1.14–2020.2.13 | NR | RT-PCR | TNI | 0.04 ng/mL |
| Liu et al. (45) | 2020.1.10–2020.2.24 | NR | RT-PCR | TNI | 0.03 μg/L |
| Ma et al. (46) | 2020.1.21–2020.3.2 | Non-severe and severe patients | RT-PCR | TNI | 0.034 ng/mL |
| Petrilli et al. (47) | 2020.3.1–2020.4.2 | NR | RT-PCR | TNI | 0.1 ng/mL |
| Qi et al. (48) | 2020.1.19–2020.2.16 | Non-severe and severe patients | RT-PCR | TNT | 14 pg/mL |
| Qiu et al. (49) | 2020.1.22–2020.2.12 | Imported and Indigenous patients | RT-PCR | TNI or EKG or Echo | NR |
| Shi et al. (10) | 2020.1.20–2020.2.10 | NR | RT-PCR | TNI | 0.04 ng/mL |
| Tian et al. (50) | 2020.1.21–2020.3.5 | NR | RT-PCR | TNI | 1.5 ng/mL |
| Wang et al. (4) | 2020.1.1–2020.1.28 | Non-ICU and ICU patients | RT-PCR | TNI or EKG or Echo | 26.2 pg/mL |
| Wang et al. (51) | 2020.1.17–2020.2.20 | Non-severe and severe patients | RT-PCR | TNI | NR |
| Wang et al. (52) | 2020.1.1–2020.2.6 | Survivors and non-survivors | RT-PCR | TNI | 0.04 pg/ml |
| Wang et al. (53) | 2020.1.22–2020.2.7 | Non-severe and severe patients | RT-PCR | CK-MB | NR |
| Wu et al. (54) | 2019.12.25–2020.1.26 | without and with ARDS patients | RT-PCR | CK-MB | 24 U/L |
| Wu et al. (55) | 2020.1.22–2020.2.14 | Mild, moderate, severe, and critical patients | RT-PCR | CK-MB | 25 U/L |
| Xiong et al. (56) | 2020.1.17–2020.2.20 | Mild, moderate, severe, and critical patients | RT-PCR | TNI | NR |
| Xu et al. (57) | 2020.1.2–2020.2.14 | NR | RT-PCR | TNT | 28 pg/mL |
| Xu et al. (58) | 2020.2.7–2020.2.28 | Mild, severe, and critical patients | RT-PCR | TNI or EKG or Echo | 28 pg/ml |
| Yan et al. (59) | 2020.1.22–2020.3.14 | Non-severe and severe patients | RT-PCR | TNI or EKG or Echo | NR |
| Yang et al. (60) | 2020.1.23–NR | NR | RT-PCR | CK-MB | 4.87 g/mL |
| Yang et al. (61) | 2019.12.24–2020.1.26 | Survivors and non-survivors | RT-PCR | TNI | 28 pg/mL |
| Zhang et al. (62) | 2020.1.11–2020.2.10 | Non-survivors | RT-PCR | TNT | 0.04 pg/mL |
| Zhang et al. (63) | 2019.12.25–2020.2.15 | Survivors and non-survivors | RT-PCR | TNI | 0.026 μg/L |
| Zhang et al. (64) | 2020.2.4–NR | Non-severe and severe patients | RT-PCR | CK-MB | NR |
| Zhao et al. (65) | 2020.1.21–2020.2.8 | Non-severe and severe patients | RT-PCR | TNI | 0.05 ng/mL |
| Zheng et al. (66) | 2020.1.22–2020.3.5 | Noninvasive ventilation and invasive mechanical ventilation patients | RT-PCR | TNI or EKG or Echo | NR |
| Zhou et al. (67) | 2020.2.5–2020.2.13 | Non-severe and severe patients | RT-PCR | TNI | 26.2 ng/L |
| Zhou et al. (68) | 2019.12.29–2020.1.31 | Survivors and non-survivors | RT-PCR | TNI or EKG or Echo | 28 ng/mL |
| Zhou et al. (69) | 2020.1.17–2020.2.26 | Survivors | RT-PCR or clinical diagnosis | TNI or EKG or Echo | NR |
NR, not reported; RT-PCR, reverse transcription-polymerase chain reaction; CK-MB, creatine kinase isoenzyme; TNI, troponin I; ICU, intensive care unit; EKG, electrocardiography; Echo, echocardiography; ARDS, acute respiratory distress syndrome.
Table S4. Clinical characteristics of the included studies.
| Study | Number | Mean age (y) | Male (%) | Smoking (%) | Hypertension (%) | Diabetes (%) | CVD (%) | Cerebrovascular disease (%) | Chronic pulmonary disease (%) | Chronic kidney disease (%) | Liver disease (%) | Cancer (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ai et al. (22) | 102 | 50.38 | 51 | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Cai et al. (23) | 298 | 47 | 50 | NR | 12.8 | 6.4 | 3.7 | NR | NR | NR | 2.7 | 1.4 |
| Cao et al. (24) | 55 | 54 | 52 | NR | 27.5 | 10.8 | 4.9 | 5.9 | 9.8 | 3.9 | 2 | 3.9 |
| Cao et al. (25) | 194 | 50.1 | 51 | 5.6 | 21.2 | 7.6 | 6 | NR | NR | NR | 3 | 2 |
| Chen et al. (26) | 150 | 59 | 56 | NR | 32.6 | 13.3 | 7.33 | NR | NR | NR | NR | 2 |
| Chen et al. (27) | 21 | 56 | 81 | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Chen et al. (2) | 203 | 62 | 62 | 13.9 | 33.9 | 17.2 | 8.4 | 1.5 | 6.6 | 1.5 | 4.0 | 2.6 |
| Chen et al. (28) | 291 | 46 | 49.8 | NR | 13.4 | 7.6 | 4.1 | 2.7 | 3.4 | 0.7 | 5.2 | 0.7 |
| Deng et al. (29) | 112 | 65 | 50.9 | NR | 32.1 | 17 | 13.4 | NR | 3.6 | NR | NR | NR |
| Fan et al. (30) | 101 | 65.46 | 64 | NR | NR | NR | NR | NR | 4.95 | NR | NR | 4.95 |
| Fang et al. (31) | 79 | 45.1 | 57 | NR | 20.3 | 14.5 | 3.8 | 3.8 | 0 | 3.8 | 3.8 | 1.3 |
| Feng et al. (32) | 8 | 40 | 62.5 | NR | NR | 12.5 | NR | NR | NR | NR | NR | NR |
| Feng et al. (33) | 384 | 53 | 56.9 | 13.4 | 23.7 | 10.3 | 8 | 3.6 | 4.6 | 0.8 | NR | 2.5 |
| Fu et al. (34) | 200 | 49.5 | 52.35 | 50.5 | 68.5 | 8 | NR | 4 | NR | 4.5 | NR | |
| Fu et al. (35) | 50 | 64 | 54 | 20 | 20 | 24 | 22 | NR | 6 | 2 | 4 | NR |
| Guo et al. (5) | 187 | 58.5 | 48.7 | 9.6 | 32.6 | 15 | 15.5 | NR | 2.1 | 3.2 | NR | 7 |
| Han et al. (36) | 273 | 58.86 | 35.5 | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| He et al. (37) | 54 | 68.18 | 62.96 | NR | 44.4 | 24.07 | 14.81 | NR | 3.7 | NR | 40.74 | NR |
| Hong et al. (38) | 18 | 63.5 | 50 | NR | 38.9 | 27.8 | 11.1 | 5.5 | 11.1 | 5.5 | NR | 5.5 |
| Hu et al. (39) | 244 | 61 | 51.4 | 11.8 | 32.5 | 14.6 | NR | 2.2 | 10.9 | 2.2 | 1.5 | 1.5 |
| Huang et al. (3) | 41 | 49 | 73 | 7 | 15 | 20 | 15 | NR | 2 | NR | 2 | 2 |
| Huang et al. (40) | 15 | 56.24 | 41.2 | NR | 23.5 | 11.8 | 17.6 | NR | 8.8 | NR | 2.9 | 8.8 |
| Hui et al. (41) | 20 | 32.8 | 46.3 | NR | 14.63 | 4.88 | 9.76 | NR | NR | NR | NR | 2.44 |
| Jiang et al. (42) | 55 | 45 | 49.1 | NR | 30.9 | 16.4 | NR | 1.8 | NR | 1.8 | 3.6 | 3.6 |
| Li et al. (43) | 66 | 51 | 43.94 | NR | 15.15 | 7.58 | 15.15 | NR | NR | NR | NR | NR |
| Li et al. (44) | 15 | 71.88 | 40 | NR | 60 | 36 | 32 | 12 | 12 | 20 | 4 | 8 |
| Liu et al. (45) | 291 | 48.1 | 45.7 | NR | 18.5 | 7.6 | 5.1 | NR | NR | NR | NR | NR |
| Ma et al. (46) | 84 | 48 | 57.1 | 8.3 | 14.3 | 11.9 | 6 | 4.8 | 6 | 1.2 | 13.1 | 1.2 |
| Petrilli et al. (47) | 1,327 | 61.7 | 63.34 | 25.92 | 36.47 | 24.6 | 54.11 | NR | 10.24 | 9.86 | NR | 6.95 |
| Qi et al. (48) | 76 | 48 | 55.8 | 19.9 | 7.5 | 9.7 | NR | NR | 9.4 | NR | NR | NR |
| Qiu et al. (49) | 104 | 43 | 47.12 | 3.85 | 14.42 | 11.54 | 6.73 | NR | 0.96 | NR | NR | NR |
| Shi et al. (10) | 416 | 64 | 49.3 | NR | 30.5 | 14.4 | 10.6 | 5.3 | 2.9 | 3.4 | NR | 2.2 |
| Tian et al. (50) | 28 | 41 | 57.63 | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Wang et al. (4) | 138 | 56 | 54.3 | NR | 31.2 | 10.1 | 14.5 | 5.1 | 2.9 | 2.9 | 2.9 | 7.2 |
| Wang et al. (51) | 242 | 45 | 49.17 | 7.9 | 14.9 | 6.2 | 3.7 | 2.5 | 0.4 | NR | 5 | 0.8 |
| Wang et al. (52) | 339 | 69 | 49 | NR | 40.8 | 16 | 15.7 | 6.2 | 6.2 | 3.8 | 0.6 | 4.4 |
| Wang et al. (53) | 17 | 42.1 | 58.82 | NR | 11.76 | NR | NR | NR | NR | NR | NR | NR |
| Wu et al. (54) | 198 | 51 | 63.7 | NR | 19.4 | 10.9 | 4 | NR | 2.5 | 1 | 3.5 | 0.5 |
| Wu et al. (55) | 38 | 46.1 | 48.75 | NR | NR | NR | NR | NR | NR | 1.25 | 1.25 | 1.25 |
| Xiong et al. (56) | 89 | 53 | 46.07 | NR | 29.2 | 15.7 | NR | 6.7 | 5.6 | 3.4 | 1.1 | 12.3 |
| Xu et al. (57) | 53 | 48.21 | 52.83 | 11.32 | 15.09 | 15.09 | 11.32 | NR | 5.66 | NR | NR | NR |
| Xu et al. (58) | 69 | 57 | 50.7 | 7.2 | NR | NR | NR | NR | NR | NR | NR | NR |
| Yan et al. (59) | 168 | 51 | 51.8 | NR | 14.3 | 7.1 | 7.1 | NR | 6 | 0.6 | 3.6 | 1.2 |
| Yang et al. (60) | 57 | 37 | 50.9 | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Yang et al. (61) | 52 | 59.7 | 67 | 4 | NR | 17 | 10 | 13.5 | 8 | NR | NR | 4 |
| Zhang et al. (62) | 60 | 72.5 | 65.9 | NR | 56.1 | 18.3 | NR | 12.2 | 14.6 | 4.9 | 2.4 | 7.3 |
| Zhang et al. (63) | 48 | 64.03 | 54.5 | NR | 51.8 | 17.3 | 14.5 | 16.4 | NR | 8.2 | NR | NR |
| Zhang et al. (64) | 16 | 54 | 60 | 8 | 28 | 11 | 11 | 3 | 0 | 2 | 8 | NR |
| Zhao et al. (65) | 77 | 52 | 44.2 | NR | 20.8 | 7.8 | 11.7 | 2.6 | NR | 6.5 | NR | 5.2 |
| Zheng et al. (66) | 34 | 66 | 67.6 | NR | 64.7 | 23.5 | 11.8 | NR | 5.9 | 5.9 | 11.8 | NR |
| Zhou et al. (67) | 34 | 63 | 50 | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Zhou et al. (68) | 191 | 56 | 62 | 6 | 30 | 19 | 8 | NR | 3 | 1 | NR | 1 |
| Zhou et al. (69) | 197 | 55.94 | 50.3 | NR | NR | 9.1 | 24.4 | 4.6 | NR | 1.5 | NR | 1.5 |
CVD, cardiovascular disease; NR, not reported.
Table S5. Quality scores of the included studies.
| Study | Representativeness of the cases | Ascertainment of exposure | Ascertainment of outcome | Ascertainment of outcome (quality control)a | Control for factors of age and sexb | Control for factors related to cardiac injuryc | Total score |
|---|---|---|---|---|---|---|---|
| Ai et al. (22) | 1 | 1 | 1 | 0 | 2 | 0 | 5 |
| Cai et al. (23) | 1 | 1 | 1 | 1 | 2 | 2 | 8 |
| Cao et al. (24) | 1 | 1 | 1 | 0 | 2 | 2 | 7 |
| Cao et al. (25) | 1 | 1 | 1 | 0 | 2 | 2 | 7 |
| Chen et al. (26) | 1 | 1 | 1 | 1 | 2 | 2 | 8 |
| Chen et al. (27) | 1 | 1 | 1 | 1 | 2 | 1 | 7 |
| Chen et al. (2) | 1 | 1 | 1 | 0 | 2 | 2 | 7 |
| Chen et al. (28) | 1 | 1 | 1 | 0 | 2 | 2 | 7 |
| Deng et al. (29) | 1 | 1 | 1 | 0 | 2 | 2 | 7 |
| Fan et al. (30) | 1 | 1 | 1 | 0 | 2 | 1 | 6 |
| Fang et al. (31) | 1 | 1 | 1 | 0 | 2 | 2 | 7 |
| Feng et al. (32) | 1 | 1 | 1 | 0 | 2 | 0 | 5 |
| Feng et al. (33) | 1 | 1 | 1 | 0 | 2 | 2 | 7 |
| Fu et al. (34) | 1 | 1 | 1 | 1 | 2 | 2 | 8 |
| Fu et al. (35) | 1 | 1 | 1 | 0 | 2 | 2 | 7 |
| Guo et al. (5) | 1 | 1 | 1 | 1 | 2 | 2 | 8 |
| Han et al. (36) | 1 | 1 | 1 | 0 | 2 | 2 | 7 |
| He et al. (37) | 1 | 1 | 1 | 1 | 2 | 2 | 8 |
| Hong et al. (38) | 1 | 1 | 1 | 1 | 2 | 2 | 8 |
| Hu et al. (39) | 1 | 1 | 1 | 0 | 2 | 2 | 7 |
| Huang et al. (3) | 1 | 1 | 1 | 1 | 2 | 2 | 8 |
| Huang et al. (40) | 1 | 1 | 1 | 0 | 2 | 2 | 7 |
| Hui et al. (41) | 1 | 1 | 1 | 0 | 2 | 2 | 7 |
| Jiang et al. (42) | 1 | 1 | 1 | 1 | 2 | 2 | 8 |
| Li et al. (43) | 1 | 1 | 1 | 1 | 2 | 1 | 7 |
| Li et al. (44) | 1 | 1 | 1 | 0 | 2 | 2 | 7 |
| Liu et al. (45) | 1 | 1 | 1 | 1 | 2 | 2 | 8 |
| Ma et al. (46) | 1 | 1 | 1 | 0 | 2 | 1 | 6 |
| Petrilli et al. (47) | 1 | 1 | 1 | 0 | 2 | 2 | 7 |
| Qi et al. (48) | 1 | 1 | 1 | 0 | 2 | 2 | 7 |
| Qiu et al. (49) | 1 | 1 | 1 | 1 | 2 | 1 | 7 |
| Shi et al. (10) | 1 | 1 | 1 | 1 | 2 | 2 | 8 |
| Tian et al. (50) | 1 | 1 | 1 | 0 | 2 | 0 | 5 |
| Wang et al. (4) | 1 | 1 | 1 | 1 | 2 | 2 | 8 |
| Wang et al. (51) | 1 | 1 | 1 | 0 | 2 | 2 | 7 |
| Wang et al. (52) | 1 | 1 | 1 | 0 | 2 | 2 | 7 |
| Wang et al. (53) | 1 | 1 | 1 | 0 | 2 | 1 | 6 |
| Wu et al. (54) | 1 | 1 | 1 | 0 | 2 | 2 | 7 |
| Wu et al. (55) | 1 | 1 | 1 | 0 | 2 | 1 | 6 |
| Xiong et al. (56) | 1 | 1 | 1 | 0 | 2 | 1 | 6 |
| Xu et al. (57) | 1 | 1 | 1 | 1 | 2 | 2 | 8 |
| Xu et al. (58) | 1 | 1 | 1 | 1 | 2 | 1 | 7 |
| Yan et al. (59) | 1 | 1 | 1 | 1 | 2 | 2 | 8 |
| Yang et al. (60) | 1 | 1 | 1 | 0 | 2 | 0 | 5 |
| Yang et al. (61) | 1 | 1 | 1 | 1 | 2 | 1 | 7 |
| Zhang et al. (62) | 1 | 1 | 1 | 0 | 2 | 2 | 7 |
| Zhang et al. (63) | 1 | 1 | 1 | 1 | 2 | 2 | 8 |
| Zhang et al. (64) | 1 | 1 | 1 | 1 | 2 | 2 | 8 |
| Zhao et al. (65) | 1 | 1 | 1 | 0 | 2 | 2 | 7 |
| Zheng et al. (66) | 1 | 1 | 1 | 1 | 2 | 2 | 8 |
| Zhou et al. (67) | 1 | 1 | 1 | 0 | 2 | 0 | 5 |
| Zhou et al. (68) | 1 | 1 | 1 | 1 | 2 | 2 | 8 |
| Zhou et al. (69) | 1 | 1 | 1 | 1 | 2 | 1 | 7 |
a, one point for studies that reported the definition of cardiac injury; b, one point for age, and one point for sex, totally 2 points for this section; c, studies received 1 point for reporting 1 or 2 categories, received 2 points for reporting ≥3 categories related to cardiac injury (hypertension, diabetes, CVD, et al.). CVD, cardiovascular disease.
Table S6. Leave-1-out sensitivity analysis for cardiac injury incidence.
| Study omitted | Incidence (95% CI) | |||
|---|---|---|---|---|
| A. Overall | B. Non-severe patients | C. Severe patients | D. Non-survivors | |
| Ai et al. (22) | 0.21 (0.18–0.26) | |||
| Cai et al. (23) | 0.21 (0.17–0.25) | 0.11 (0.07–0.15) | 0.43 (0.33–0.53) | |
| Cao et al. (24) | 0.21 (0.17–0.25) | 0.65 (0.52–0.78) | ||
| Cao et al. (25) | 0.21 (0.17–0.25) | 0.11 (0.07–0.15) | 0.43 (0.33–0.54) | |
| Chen et al. (26) | 0.21 (0.17–0.25) | 0.11 (0.07–0.15) | 0.43 (0.33–0.53) | |
| Chen et al. (27) | 0.21 (0.17–0.25) | |||
| Chen et al. (2) | 0.21 (0.17–0.25) | 0.11 (0.07–0.15) | 0.42 (0.32–0.52) | 0.65 (0.51–0.80) |
| Chen et al. (28) | 0.22 (0.18–0.26) | 0.11 (0.07–0.16) | 0.44 (0.34–0.55) | |
| Deng et al. (29) | 0.21 (0.17–0.25) | 0.11 (0.07–0.15) | 0.43 (0.32–0.53) | |
| Fan et al. (30) | 0.20 (0.16–0.24) | |||
| Fang et al. (31) | 0.21 (0.17–0.25) | |||
| Feng et al. (32) | 0.21 (0.17–0.25) | |||
| Feng et al. (33) | 0.21 (0.17–0.25) | 0.10 (0.07–0.14) | 0.44 (0.34–0.55) | |
| Fu et al. (34) | 0.20 (0.16–0.24) | 0.07 (0.05–0.10) | 0.42 (0.32–0.52) | 0.65 (0.52–0.79) |
| Fu et al. (35) | 0.21 (0.17–0.25) | |||
| Guo et al. (5) | 0.21 (0.17–0.25) | |||
| Han et al. (36) | 0.21 (0.18–0.26) | 0.11 (0.07–0.15) | 0.44 (0.34–0.55) | |
| He et al. (37) | 0.21 (0.17–0.25) | 0.11 (0.07–0.14) | 0.42 (0.32–0.53) | 0.66 (0.53–0.79) |
| Hong et al. (38) | 0.21 (0.17–0.25) | |||
| Hu et al. (39) | 0.21 (0.17–0.25) | 0.10 (0.07–0.14) | 0.44 (0.33–0.55) | |
| Huang et al. (3) | 0.21 (0.17–0.25) | 0.11 (0.07–0.15) | 0.44 (0.34–0.54) | |
| Huang et al. (40) | 0.22 (0.18–0.26) | |||
| Hui et al. (41) | 0.21 (0.17–0.25) | 0.11 (0.07–0.15) | 0.42 (0.32–0.53) | |
| Jiang et al. (42) | 0.22 (0.18–0.26) | 0.11 (0.07–0.15) | 0.45 (0.34–0.55) | |
| Li et al. (43) | 0.22 (0.18–0.26) | 0.11 (0.07–0.15) | 0.44 (0.33–0.54) | |
| Li et al. (44) | 0.20 (0.17–0.24) | |||
| Liu et al. (45) | 0.22 (0.18–0.26) | |||
| Ma et al. (46) | 0.21 (0.17–0.25) | 0.10 (0.06–0.14) | 0.42 (0.32–0.52) | |
| Petrilli et al. (47) | 0.22 (0.17–0.26) | |||
| Qi et al. (48) | 0.22 (0.18–0.26) | 0.11 (0.07–0.15) | 0.45 (0.35–0.55) | |
| Qiu et al. (49) | 0.22 (0.18–0.26) | |||
| Shi et al. (10) | 0.21 (0.17–0.25) | |||
| Tian et al. (50) | 0.21 (0.17–0.25) | |||
| Wang et al. (4) | 0.22 (0.18–0.26) | 0.11 (0.07–0.15) | 0.44 (0.34–0.55) | |
| Wang et al. (51) | 0.21 (0.17–0.25) | 0.11 (0.07–0.15) | 0.43 (0.33–0.53) | |
| Wang et al. (52) | 0.21 (0.17–0.25) | 0.11 (0.07–0.15) | 0.43 (0.32–0.53) | 0.67 (0.54–0.81) |
| Wang et al. (53) | 0.21 (0.17–0.25) | |||
| Wu et al. (54) | 0.22 (0.18–0.26) | |||
| Wu et al. (55) | 0.21 (0.17–0.25) | |||
| Xiong et al. (56) | 0.22 (0.18–0.26) | 0.11 (0.07–0.15) | 0.45 (0.34–0.55) | |
| Xu et al. (57) | 0.21 (0.17–0.25) | |||
| Xu et al. (58) | 0.22 (0.18–0.26) | 0.11 (0.07–0.15) | 0.45 (0.34–0.55) | |
| Yan et al. (59) | 0.22 (0.18–0.26) | 0.11 (0.07–0.15) | 0.45 (0.35–0.55) | |
| Yang et al. (60) | 0.22 (0.18–0.26) | |||
| Yang et al. (61) | 0.21 (0.17–0.25) | 0.11 (0.07–0.15) | 0.44 (0.34–0.54) | 0.72 (0.63–0.80) |
| Zhang et al. (62) | 0.20 (0.16–0.23) | 0.41 (0.32–0.50) | 0.63 (0.51–0.75) | |
| Zhang et al. (63) | 0.21 (0.17–0.25) | |||
| Zhang et al. (64) | 0.21 (0.17–0.25) | |||
| Zhao et al. (65) | 0.21 (0.17–0.25) | 0.11 (0.07–0.15) | 0.44 (0.34–0.54) | |
| Zheng et al. (66) | 0.21 (0.17–0.25) | 0.11 (0.07–0.15) | 0.43 (0.32–0.53) | |
| Zhou et al. (67) | 0.21 (0.17–0.25) | 0.11 (0.07–0.15) | 0.43 (0.33–0.53) | |
| Zhou et al. (68) | 0.21 (0.17–0.25) | 0.12 (0.07–0.16) | 0.43 (0.32–0.53) | 0.67 (0.54–0.81) |
| Zhou et al. (69) | 0.21 (0.18–0.26) | 0.11 (0.07–0.15) | ||
CI, confidence interval.
Table S7. Meta-regression for RR of severe patients vs. non-severe patients.
| Variables | No. of reported studies | β coefficient (95% CI) | P value |
|---|---|---|---|
| Mean age | 26 | –0.0059 (–0.0275 to 0.0158) | 0.583 |
| Male | 27 | 0.0053 (–0.0173 to 0.0278) | 0.635 |
| Smoking | 11 | –0.0040 (–0.0124 to 0.0044) | 0.312 |
| Hypertension | 23 | –0.0060 (–0.0165 to 0.0045) | 0.249 |
| Diabetes | 24 | –0.0037 (–0.0090 to 0.0016) | 0.165 |
| CVD | 20 | 0.0090 (–0.0367 to 0.0546) | 0.685 |
| Cerebrovascular disease | 12 | 0.0135 (–0.0787 to 0.1058) | 0.750 |
| Chronic pulmonary disease | 18 | 0.0104 (–0.0585 to 0.0794) | 0.752 |
| Chronic kidney disease | 14 | 0.0315 (–0.1087 to 0.1717) | 0.633 |
| Liver disease | 15 | 0.0035 (–0.0173 to 0.0242) | 0.723 |
| Cancer | 18 | 0.0315 (–0.0890 to 0.1520) | 0.587 |
RR, relative risk; No., number; CI, confidence interval; CVD, cardiovascular disease.
Table S8. Univariable meta-regression for cardiac injury incidence.
| Population | Variables | No. of reported studies | β coefficient (95% CI) | P value |
|---|---|---|---|---|
| Overall | Mean age | 41 | –0.0062 (–0.0123 to –0.0002) | 0.054 |
| Male | 42 | –0.0026 (–0.0079 to 0.0027) | 0.322 | |
| Smoking | 14 | –0.0020 (–0.0053 to 0.0014) | 0.231 | |
| Hypertension | 33 | –0.0023 (–0.0055 to 0.0009) | 0.159 | |
| Diabetes | 35 | –0.0015 (–0.0035 to 0.0006) | 0.169 | |
| CVD | 32 | –0.0007 (–0.0039 to 0.0026) | 0.669 | |
| Cerebrovascular disease | 18 | –0.0030 (–0.0164 to 0.0105) | 0.646 | |
| Chronic pulmonary disease | 28 | –0.0034 (–0.0137 to 0.0069) | 0.504 | |
| Chronic kidney disease | 25 | –0.0020 (–0.0149 to 0.0109) | 0.754 | |
| Liver disease | 20 | –0.0019 (–0.0064 to 0.0103) | 0.632 | |
| Cancer | 28 | –0.0115 (–0.0318 to 0.0088) | 0.254 | |
| Non-survivors | Mean age | 7 | –0.0032 (–0.0165 to 0.0101) | 0.559 |
| Male | 8 | –0.0028 (–0.0150 to 0.0093) | 0.589 | |
| Smoking | 4 | 0.0002 (–0.0121 to 0.0125) | 0.961 | |
| Diabetes | 8 | 0.0005 (–0.0047 to 0.0057) | 0.832 | |
| CVD | 7 | 0.0017 (–0.0289 to 0.0322) | 0.895 | |
| Cerebrovascular disease | 5 | –0.0012 (–0.0250 to 0.0226) | 0.883 | |
| Chronic pulmonary disease | 8 | –0.0049 (–0.0218 to 0.0120) | 0.503 | |
| Chronic kidney disease | 5 | –0.0061 (–0.0737 to 0.0615) | 0.792 | |
| Liver disease | 6 | 0.0016 (–0.0084 to 0.0116) | 0.683 | |
| Cancer | 6 | –0.0073 (–0.0476 to 0.0329) | 0.639 | |
| Severe patients | Mean age | 22 | –0.0059 (–0.0130 to 0.0013) | 0.101 |
| Male | 23 | –0.0053 (–0.0133 to 0.0027) | 0.185 | |
| Smoking | 10 | –0.0006 (–0.0069 to 0.0056) | 0.820 | |
| Hypertension | 21 | –0.0028 (–0.0071 to 0.0015) | 0.195 | |
| Diabetes | 22 | –0.0007 (–0.0049 to 0.0036) | 0.749 | |
| CVD | 19 | 0.0013 (–0.0208 to 0.0234) | 0.904 | |
| Cerebrovascular disease | 11 | –0.0038 (–0.0194 to 0.0119) | 0.598 | |
| Chronic pulmonary disease | 17 | –0.0069 (–0.0202 to 0.0064) | 0.287 | |
| Chronic kidney disease | 13 | –0.0085 (–0.0482 to 0.0311) | 0.644 | |
| Liver disease | 14 | 0.0017 (–0.0059 to 0.0093) | 0.642 | |
| Cancer | 17 | –0.0102 (–0.0357 to 0.0153) | 0.407 | |
| Non-severe patients | Mean age | 11 | 0.0020 (–0.0203 to 0.0242) | 0.845 |
| Male | 12 | 0.0064 (–0.0177 to 0.0305) | 0.568 | |
| Smoking | 6 | –0.0030 (–0.0096 to 0.0037) | 0.283 | |
| Hypertension | 10 | –0.0045 (–0.0127 to 0.0036) | 0.233 | |
| Diabetes | 11 | –0.0025 (–0.0061 to 0.0010) | 0.142 | |
| CVD | 10 | 0.0096 (–0.0218 to 0.0411) | 0.500 | |
| Chronic pulmonary disease | 8 | 0.0270 (–0.0415 to 0.0956) | 0.372 | |
| Liver disease | 8 | 0.0066 (–0.0193 to 0.0325) | 0.555 | |
| Cancer | 9 | –0.0250 (–0.1880 to 0.1380) | 0.727 |
No., number; CI, confidence interval; CVD, cardiovascular disease.
Table S9. Trim and fill method to deal with publication bias.
| Population | Publication bias | Before trim and fill | After trim and fill | ||||
|---|---|---|---|---|---|---|---|
| P for Egger’s test | No. of studies | Incidence (95% CI) | No. of studies | Incidence (95% CI) | |||
| Overall | <0.001 | 50 | 0.21 (0.17–0.25) | 69 | 0.09 (0.05–0.14) | ||
| Non-severe patients | 0.004 | 23 | 0.11 (0.07–0.15) | 33 | 0.03 (0.01–0.07) | ||
No., number; CI, confidence interval.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The ethical approval and consent are not required because no patient-level data is involved for this systematic review and meta-analysis.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
Footnotes
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at http://dx.doi.org/10.21037/cdt-20-535
Peer Review File: Available at http://dx.doi.org/10.21037/cdt-20-535
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/cdt-20-535). The authors have no conflicts of interest to declare.
References
- 1.World Health Organization. Coronavirus disease 2019 (COVID-19) Situation Report-147. Available online: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200615-covid-19-sitrep-147.pdf?sfvrsn=2497a605_4
- 2.Chen T, Wu D, Chen H, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ 2020;368:m1091. 10.1136/bmj.m1091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497-506. 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020;323:1061-9. 10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guo T, Fan Y, Chen M, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020;5:1-8. 10.1001/jamacardio.2020.1017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shi S, Qin M, Shen B, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol 2020;5:802-10. 10.1001/jamacardio.2020.0950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Babapoor-Farrokhran S, Gill D, Walker J, et al. Myocardial injury and COVID-19: possible mechanisms. Life Sci 2020;253:117723. 10.1016/j.lfs.2020.117723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hendren NS, Drazner MH, Bozkurt B, et al. Description and proposed management of the acute COVID-19 cardiovascular syndrome. Circulation 2020;141:1903-14. 10.1161/CIRCULATIONAHA.120.047349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhong H, Wang Y, Zhang ZL, et al. Efficacy and safety of current therapeutic options for COVID-19 - lessons to be learnt from SARS and MERS epidemic: a systematic review and meta-analysis. Pharmacol Res 2020;157:104872. 10.1016/j.phrs.2020.104872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lippi G, Lavie CJ, Sanchis-Gomar F. Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): Evidence from a meta-analysis. Prog Cardiovasc Dis 2020;63:390-1. 10.1016/j.pcad.2020.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li JW, Han TW, Woodward M, et al. The impact of 2019 novel coronavirus on heart injury: A systemic review and Meta-analysis. Prog Cardiovasc Dis 2020. [Epub ahead of print]. 10.1016/j.pcad.2020.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Santoso A, Pranata R, Wibowo A, et al. Cardiac injury is associated with mortality and critically ill pneumonia in COVID-19: A meta-analysis. Am J Emerg Med 2020. [Epub ahead of print]. 10.1016/j.ajem.2020.04.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.China National Health Commission. Novel coronavirus diagnosis and treatment plan. seventh ed. 2020. Available online: http://www.gov.cn/zhengce/zhengceku/2020-03/04/content_5486705.htm
- 14.Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. Bmj 2011;343:d5928. 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25:603-5. 10.1007/s10654-010-9491-z [DOI] [PubMed] [Google Scholar]
- 16.Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gu ZC, Wei AH, Zhang C, et al. Risk of major gastrointestinal bleeding with new vs conventional oral anticoagulants: a systematic review and meta-analysis. Clin Gastroenterol Hepatol 2020;18:792-9.e61. 10.1016/j.cgh.2019.05.056 [DOI] [PubMed] [Google Scholar]
- 18.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 2009;62:e1-34. 10.1016/j.jclinepi.2009.06.006 [DOI] [PubMed] [Google Scholar]
- 19.Oudit GY, Kassiri Z, Jiang C, et al. SARS-coronavirus modulation of myocardial ACE2 expression and inflammation in patients with SARS. Eur J Clin Invest 2009;39:618-25. 10.1111/j.1365-2362.2009.02153.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med 2020;8:420-2. 10.1016/S2213-2600(20)30076-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tang N, Li D, Wang X, et al. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost 2020;18:844-7. 10.1111/jth.14768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ai J, Chen J, Wang Y, et al. The cross-sectional study of hospitalized coronavirus disease 2019 patients in Xiangyang, Hubei province. medRxiv 2020. doi: 10.1101/2020.02.19.20025023. [DOI]
- 23.Cai Q, Huang D, Ou P, et al. 2019-nCoV Pneumonia in a Normal Work Infectious Diseases Hospital Besides Hubei Province, China. The Lancet 2020. doi: . 10.2139/ssrn.3542163 [DOI] [Google Scholar]
- 24.Cao J, Tu WJ, Cheng W, et al. Clinical features and short-term outcomes of 102 patients with corona virus disease 2019 in Wuhan, China. Clin Infect Dis 2020;71:748-55. 10.1093/cid/ciaa243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cao M, Zhang D, Wang Y, et al. Clinical Features of Patients Infected with the 2019 Novel Coronavirus (COVID-19) in Shanghai, China. medRxiv 2020. doi: 10.1101/2020.03.04.20030395. [DOI]
- 26.Chen C, Chen C, Yan JT, et al. Analysis of myocardial injury in patients with COVID-19 and association between concomitant cardiovascular diseases and severity of COVID-19. Zhonghua Xin Xue Guan Bing Za Zhi 2020;48:E008. [DOI] [PubMed] [Google Scholar]
- 27.Chen G, Wu D, Guo W, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest 2020;130:2620-9. 10.1172/JCI137244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen X, Zheng F, Qing Y, et al. Epidemiological and clinical features of 291 cases with coronavirus disease 2019 in areas adjacent to Hubei, China: a double-center observational study. medRxiv 2020. doi: 10.1101/2020.03.03.20030353. [DOI]
- 29.Deng Q, Hu B, Zhang Y, et al. Suspected myocardial injury in patients with COVID-19: evidence from front-line clinical observation in Wuhan, China. Int J Cardiol 2020;311:116-21. 10.1016/j.ijcard.2020.03.087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen J, Fan H, Zhang L, et al. Retrospective Analysis of Clinical Features in 101 Death Cases with COVID-19. medRxiv 2020. doi: 10.1101/2020.03.09.20033068. [DOI]
- 31.Fang X, Mei q, Yang T, et al. Clinical characteristics and treatment strategies of 79 patients with COVID-19. Chinese Pharmacological Bulletin 2020;36:453-9. [Google Scholar]
- 32.Feng T, Yue H, Pu J, et al. Clinical characteristics of several patients with coronavirus disease 2019 in Lanzhou City. Journal of Xi'an Jiaotong University (Medical Sciences) 2020. [Epub ahead of print].
- 33.Feng Y, Ling Y, Bai T, et al. COVID-19 with different severities: a multicenter study of clinical features. Am J Respir Crit Care Med 2020;201:1380-8. 10.1164/rccm.202002-0445OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fu L, Fei J, Xiang H-X, et al. Influence factors of death risk among COVID-19 patients in Wuhan, China: a hospital-based case-cohort study. medRxiv 2020. doi: 10.1101/2020.03.13.20035329. [DOI]
- 35.Fu S, Fu X, Song Y, et al. Virologic and clinical characteristics for prognosis of severe COVID-19: a retrospective observational study in Wuhan, China. 2 medRxiv 2020. doi: 10.1101/2020.04.03.20051763. [DOI]
- 36.Han H, Xie L, Liu R, et al. Analysis of heart injury laboratory parameters in 273 COVID-19 patients in one hospital in Wuhan, China. J Med Virol 2020;92:819-23. 10.1002/jmv.25809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.He XW, Lai JS, Cheng J, et al. Impact of complicated myocardial injury on the clinical outcome of severe or critically ill COVID-19 patients. Zhonghua Xin Xue Guan Bing Za Zhi 2020;48:E011. [DOI] [PubMed] [Google Scholar]
- 38.Hong Z, Zheng X, Yang X, et al. Comparative analysis of the clinical characteristics of 18 severe/critical coronavirus disease 2019 patients with myocardial injury. Chin J Arterioscler 2020;28:290-5. [Google Scholar]
- 39.Hu L, Chen S, Fu Y, et al. Risk Factors Associated with Clinical Outcomes in 323 COVID-19 Patients in Wuhan, China. medRxiv 2020. doi: 10.1101/2020.03.25.20037721. [DOI] [PMC free article] [PubMed]
- 40.Huang Y, Tu M, Wang S, et al. Clinical characteristics of laboratory confirmed positive cases of SARS-CoV-2 infection in Wuhan, China: A retrospective single center analysis. Travel Med Infect Dis 2020. [Epub ahead of print]. 10.1016/j.tmaid.2020.101606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hui H, Zhang Y, Yang X, et al. Clinical and radiographic features of cardiac injury in patients with 2019 novel coronavirus pneumonia. medRxiv 2020. doi: 10.1101/2020.02.24.20027052. [DOI]
- 42.Jiang X, Tao J, Wu H, et al. Clinical features and management of severe COVID-19: a retrospective study in Wuxi, Jiangsu Province, China. medRxiv 2020. doi: 10.1101/2020.04.10.20060335. [DOI]
- 43.Li M, Lyu M, Li C, et al. Analysis on the cardiac features of patients with different clinical types of novel coronavirus disease 2019. Guangdong Medical Journal 2020;8:797-800. [Google Scholar]
- 44.Li X, Wang L, Yan S, et al. Clinical characteristics of 25 death cases infected with COVID-19 pneumonia: a retrospective review of medical records in a single medical center, Wuhan, China. medRxiv 2020. doi: 10.1101/2020.02.19.20025239. [DOI] [PMC free article] [PubMed]
- 45.Liu Y, Li J, liu D, et al. Clinical features and outcomes of 2019 novel coronavirus-infected patients with cardiac injury. medRxiv 2020. doi: 10.1101/2020.03.11.20030957. [DOI]
- 46.Ma KL, Liu ZH, Cao CF, et al. COVID-19 myocarditis and severity factors: an adult cohort study. medRxiv 2020. doi: 10.1101/2020.03.19.20034124. [DOI]
- 47.Petrilli CM, Jones SA, Yang J, et al. Factors associated with hospitalization and critical illness among 4,103 patients with COVID-19 disease in New York City. medRxiv 2020. doi: 10.1101/2020.04.08.20057794. [DOI]
- 48.Qi D, Yan X, Tang X, et al. Epidemiological and clinical features of 2019-nCoV acute respiratory disease cases in Chongqing municipality, China: a retrospective, descriptive, multiple-center study. medRxiv 2020. doi: 10.1101/2020.03.01.20029397. [DOI]
- 49.Qiu C, Xiao Q, Liao X, et al. Transmission and clinical characteristics of coronavirus disease 2019 in 104 outside-Wuhan patients, China. medRxiv 2020. doi: 10.1101/2020.03.04.20026005. [DOI] [PMC free article] [PubMed]
- 50.Tian S, Zhu X, Sun X, et al. Longitudinal analysis of laboratory findings during the process of recovery for patients with COVID-19. medRxiv 2020. doi: 10.1101/2020.04.04.20053280. [DOI]
- 51.Wang G, Wu C, Zhang Q, et al. Epidemiological and Clinical Features of Corona Virus Disease 2019 (COVID-19) in Changsha, China. The Lancet 2020. doi: . 10.2139/ssrn.3548770 [DOI] [Google Scholar]
- 52.Wang L, He W, Yu X, et al. Coronavirus disease 2019 in elderly patients: characteristics and prognostic factors based on 4-week follow-up. J Infect 2020;80:639-45. 10.1016/j.jinf.2020.03.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wang S, Peng W, Yu L, et al. Clinical analysis of 17 cases of coronavirus disease 2019. Zhejiang Medical Journal 2020;42:365-7. [Google Scholar]
- 54.Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med 2020;180:1-11. 10.1001/jamainternmed.2020.0994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wu J, Liu J, Zhao X, et al. Clinical characteristics of imported cases of COVID-19 in Jiangsu Province: a multicenter descriptive study. Clin Infect Dis 2020;71:706-12. 10.1093/cid/ciaa199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Xiong J, Jiang W, Zhou Q, et al. Clinical characteristics, treatment, and prognosis in 89 cases of COVID-2019. Medical Journal of Wuhan University 2020. doi: . 10.16016/j.1000-5404.202003236 [DOI] [Google Scholar]
- 57.Xu H, Hou K, Xu H, et al. Acute Myocardial Injury of Patients with Coronavirus Disease 2019. medRxiv 2020. doi: 10.1101/2020.03.05.20031591. [DOI]
- 58.Xu Y, Li Y, Zeng Q, et al. Clinical characteristics of SARS-CoV-2 pneumonia compared to controls in Chinese Han population. medRxiv 2020. doi: 10.1101/2020.03.08.20031658. [DOI]
- 59.Yan S, Song X, Lin F, et al. Clinical Characteristics of Coronavirus Disease 2019 in Hainan, China. medRxiv 2020. doi: 10.1101/2020.03.19.20038539. [DOI]
- 60.Yang K, Xiao L, Liu Y, et al. Epidemiological and clinical characteristics of coronavirus disease 2019 in nonepidemic areas: report of 57 cases. Journal of the third military medical university 2020;42:555-9.
- 61.Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 2020;8:475-81. 10.1016/S2213-2600(20)30079-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zhang B, Zhou X, Qiu Y, et al. Clinical characteristics of 82 death cases with COVID-19. medRxiv 2020. doi: 10.1101/2020.02.26.20028191. [DOI] [PMC free article] [PubMed]
- 63.Zhang F, Yang D, Li J, et al. Myocardial injury is associated with in-hospital mortality of confirmed or suspected COVID-19 in Wuhan, China: A single center retrospective cohort study. medRxiv 2020. doi: 10.1101/2020.03.21.20040121. [DOI]
- 64.Zhang Q, Yang Z, Li Y, et al. Coronary heart disease and its risk factors in COVID-19 patients with mild symptoms: clinical characteristics summary. Chinese Heart Journal 2020;32:119-23,127. [Google Scholar]
- 65.Zhao W, Yu S, Zha X, et al. Clinical characteristics and durations of hospitalized patients with COVID-19 in Beijing: a retrospective cohort study. medRxiv 2020. doi: 10.1101/2020.03.13.20035436. [DOI]
- 66.Zheng Y, Sun L, Xu M, et al. Clinical characteristics of 34 COVID-19 patients admitted to ICU in Hangzhou, China. medRxiv 2020. doi: 10.1101/2020.04.12.20062604. [DOI] [PMC free article] [PubMed]
- 67.Zhou B, She J, Wang Y, et al. The clinical characteristics of myocardial injury in severe and very severe patients with 2019 novel coronavirus disease. J Infect 2020;81:147-78. 10.1016/j.jinf.2020.03.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054-62. 10.1016/S0140-6736(20)30566-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zhou F, Yu X, Tong X, et al. Clinical features and outcomes of 197 adult discharged patients with COVID-19 in Yichang, Hubei. medRxiv 2020. doi: 10.1101/2020.03.26.20041426. [DOI]