ABSTRACT
Background
Chronic undernutrition in children continues to be a global public health concern. Ethiopia has documented a significant decline in the prevalence of childhood stunting, a measure of chronic undernutrition, over the last 20 y.
Objectives
The aim of this research was to conduct a systematic assessment of the determinants that have driven child stunting reduction in Ethiopia from 2000 to 2016, focused on the national, community, household, and individual level.
Methods
This study employed both quantitative and qualitative methods. Specifically, a systematic literature review, retrospective quantitative data analysis using Demographic and Health Surveys from 2000–2016, qualitative data collection and analysis, and analyses of key nutrition-specific and -sensitive policies and programs were undertaken.
Results
National stunting prevalence improved from 51% in 2000 to 32% in 2016. Regional variations exist, as do pro-rich, pro-urban, and pro-educated inequalities. Child height-for-age z score (HAZ) decomposition explained >100% of predicted change in mean HAZ between 2000 and 2016, with key factors including increases in total consumable crop yield (32% of change), increased number of health workers (28%), reduction in open defecation (13%), parental education (10%), maternal nutrition (5%), economic improvement (4%), and reduced diarrhea incidence (4%). Policies and programs that were key to stunting decline focused on promoting rural agriculture to improve food security; decentralization of the health system, incorporating health extension workers to improve rural access to health services and reduce open defecation; multisectoral poverty reduction strategies; and a commitment to improving girls’ education. Interviews with national and regional stakeholders and mothers in communities presented improvements in health service access, women and girls’ education, improved agricultural production, and improved sanitation and child care practices as drivers of stunting reduction.
Conclusions
Ethiopia's stunting decline was driven by both nutrition-specific and -sensitive sectors, with particular focus on the agriculture sector, health care access, sanitation, and education.
Keywords: stunting, linear growth, children, nutrition, exemplar, Ethiopia, East Africa, mixed methods
Introduction
Chronic malnutrition in early childhood leads to stunting, which can affect the mental and physical development of the child, and can result in the intergenerational transfer of malnutrition along with poor birth outcomes in the next generation (1, 2). Stunting is a marker of inadequacy of the environment in which a child was born and raised, and it is associated with learning difficulties and barriers to community participation (3, 4). Because of this, stunting prevalence and severity is a good indicator to use for population assessment (4) and can be used to monitor the progress of children in a population over time. In 2018 there were 149 million stunted children globally, which represents nearly 22% of all children <5 y old (5).
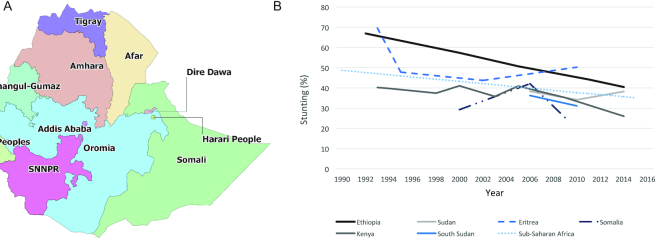
Ethiopia is a landlocked country located in Eastern Africa with a population of >108 million (Figure 1A). A predominantly agricultural country, >80% of Ethiopians live in rural areas (6, 7). Stunting prevalence in Ethiopia has been declining steadily since the early 1990s (Figure 1B). Compared with neighboring countries, Ethiopia's stunting decline was the steadiest and demonstrated the largest decline, although prevalence was not the lowest in the region. Ethiopia has consistently had a higher stunting prevalence than the regional average; however, the gap has been narrowing over time.
FIGURE 1.
Map of Ethiopia and regional under-5 stunting prevalence. (A) Ethiopia map. (B) The prevalence of under-5 stunting in Ethiopia and its neighboring countries in the East Africa region, 1990–2015. SNNPR, Southern Nations, Nationalities, and Peoples’ Region.
Ethiopia has a diverse terrain spanning plateaus, mountain ranges, and plains, with the highlands and lowlands divided by the Great East African Rift Valley (8). The highlands of Ethiopia are well-suited for settlement because they are dense in moist forests and wetlands. In these areas, there is opportunity for agricultural growth; however, the majority is rain-fed and thus dependent upon good and consistent weather (9). Ethiopia's lowlands, however, are warm and dry, resulting in a lack of biodiversity compared with other regions of the country (6). Arid or semi-arid areas cover ∼40% of the country where agricultural production can be low, which can lead to poor food availability and nutrition security (9).
Ethiopia regularly experiences climate shocks, which can dramatically affect malnutrition levels. In 2011–2012, a severe drought in the Horn of Africa peninsula affected 4.5 million people, and specifically the Afar, Somali, and Oromia regions of Ethiopia (10). The country is also highly susceptible to earthquakes, volcanic eruptions, and flooding due to the geologically active Great Rift Valley, which can result in food insecurity and water shortages, particularly among pastoral and agro-pastoral communities (8, 10, 11).
Ethiopia is composed of 14 major ethnic groups, with the Oromo and Amhara groups in the majority at 34% and 27%, respectively (8). Consequently, Oromia is the most populous administrative region, housing 37% of the population, followed by Amhara (23%) and the Southern Nations, Nationalities, and Peoples’ Region (SNNPR) (20%) (12, 13).
In 1990, the fertility rate in Ethiopia was 7.2 children/mother, which has since dropped to 4.2 in 2016 (14). The adolescent fertility rate has also plummeted from 118 births/1000 women aged 15–19 y in 1990 to 65 in 2016 (14). In 2000, 56% of Ethiopians lived on <$1.25/d, making it a country with one of the highest poverty rates in the world. By 2011, this figure had dropped to 31%, representing a remarkable decade of poverty reduction (15). Gross domestic product per capita in Ethiopia has risen from $652 in 1990 to $1730 in 2017, whereas the poverty headcount dropped from 67% in 1995 to 27% in 2015 (Supplemental Appendix 1). Literacy rates among all adults and adult females have been rising, reaching 39% and 29%, respectively, in 2007. The Gender Development Index, which rose from 0.74 in 2000 to 0.85 in 2017, indicates that the disparities between men and women have been decreasing over time (Supplemental Appendix 1). Access to improved water sources has risen from 25% in 2000 to 64% in 2016 and the practice of open defecation has fallen from 80% to 27% over the same time period (Supplemental Appendix 1).
Much literature exists on the reasons behind the stunting decline in Ethiopia, and findings point to several key drivers: parental education (16–33); health care interventions, such as delivery by a skilled birth attendant (SBA) (17, 34–36), antenatal care (16, 17, 26, 34, 37–44), and postnatal care (45, 46); improvements in water, sanitation, and hygiene (WASH), including access to improved water sources (21, 32, 37, 39, 40, 45, 47–58), reduced distance to fetch water (59), access to improved sanitation (17, 20, 21, 23, 27, 29, 39, 40, 45, 51, 60–63), and reductions in open defecation (19, 27); and child feeding indicators (19, 30, 37, 38, 60, 64–70) (Panel 1, Supplemental Appendix 2) (16–98, 99–118, 119–142). Although we found a wealth of national and subnational studies exploring factors related to stunting in Ethiopia, the overwhelming majority were cross-sectional in design which precludes causality.
Panel 1.
Systematic literature review of stunting determinants
Our literature review identified several basic determinants of child stunting in Ethiopia including ethnicity, economic development, governance, regional variation, climate and food shocks, wealth index, women's empowerment, and parental education. Ethnicity was found not to be associated with stunting risk (35), although religion was identified by 4 studies as associated with stunting; however, they found conflicting evidence based on which religion conferred greater risk (22, 71–73). One study suggests that economic development in Ethiopia was associated with improved nutritional status and stunting reductions (20), whereas another suggests that good governance was positively associated with stunting decline (21). Various studies have identified regional differences in stunting and some found that the northernmost regions Tigray, Amhara, and Afar were generally associated with increased stunting prevalence (16, 20, 21, 23, 74–78). Climate change, namely rainfall, drought, and temperature change, does predict some of the variation in child stunting in Ethiopia (18, 76), whereas the limited evidence of the impact of food shocks on stunting outcomes tends to show a lack of association (78, 79, 80). Increased wealth was found to be positively associated with HAZ and thus negatively associated with stunting in a large number of studies (16, 17, 19–21, 23–27, 29, 31, 34, 37, 38, 47, 60, 66, 77, 81, 82, 83, 96), whereas some found no association (30, 48, 64, 84, 85). Women's empowerment was difficult to quantify, and studies examining this variable suggested that the impact of proxies such as households being headed by women (23, 25, 30, 32, 47), women's autonomy (85), and mothers’ employment (26, 37, 48, 86) had conflicting or no association with HAZ in Ethiopia. Parental education has been shown to be positively associated with HAZ and negatively associated with stunting in the vast majority of both national (16–21) and subnational studies (22–27, 29–32, 96, 103), although some studies found no association (22, 34, 38, 47, 48, 59, 64, 82, 86).
Nutrition-specific and -sensitive programs identified in the literature were the Community-based Nutrition Program (CBNP), Productive Safety Net Program (PSNP), and the Targeted Supplementary Food Program (TSF). Two studies on the CBNP found that it was associated with increase in length-for-age z score and decrease in stunting (87, 88). The PSNP, however, was not found to have had an impact on stunting outcomes, although perhaps follow-up was not long enough to show these impacts (89–91). An evaluation of the TSF also showed no changes in child stunting outcomes, although there were differences between the intervention and control groups at baseline that render this finding uncertain (92).
Among the underlying causes of stunting, the literature suggests that immunization, skilled birth attendance, antenatal care, postnatal care, vitamin A supplementation, health care access and utilization, household environment, feeding practices, and food security were contributing factors. The majority of studies in our review found that childhood immunizations have a protective effect against stunting outcomes (28, 39, 40, 50, 93–95), although some found no association (23, 38, 45, 51, 97, 98). Health care interventions such as delivery by an SBA (17, 34–36), antenatal care (16, 17, 26, 34, 37–44), and postnatal care (45, 46) have been found to be associated with reduced stunting outcomes in most studies, although some found no association (16, 19, 22, 27, 30, 35, 42, 45, 49, 60, 64, 71, 86). Vitamin A supplementation is a promising initiative shown to be associated with a decreased risk of stunting, although variation in findings exists (40, 60, 61, 67, 99–102). Studies examining access, distance or time to a health facility typically found that these were not strongly related to stunting (17, 32, 33, 41, 52, 83, 100, 101, 104). There is substantial evidence in the literature that rural residence confers a higher likelihood of stunting than urban residence (18, 20, 22, 25, 28, 31, 37, 39, 48, 53, 72, 77, 80, 85, 105–107), although some studies found no association (16, 21, 23, 26, 27, 32, 34, 37, 46, 60, 64, 68, 109), whereas 1 found that rural-living children were protected (24). Improvements in WASH indicators such as access to improved water sources (21, 32, 37, 39, 40, 45, 47–58), distance to fetch water (59), access to improved sanitation (17, 20, 21, 23, 27, 29, 39, 40, 45, 51, 60–63), and open defecation (19, 27) have been generally found to be positively associated with stunting outcomes although some did find nonsignificant results (16, 17, 19, 20, 22, 23, 26, 27, 29, 30, 33, 34, 36–38, 45, 47, 49, 52, 60–62, 66, 75, 82, 93, 94, 101, 104, 108, 109, 119–126, 128). Hygiene was difficult to quantify, and this indicator was not found to be associated with stunting outcomes (19, 66, 75). Household crowding was examined in a large number of studies, of which the majority found no association with stunting, although some did find that smaller family size was associated with lower stunting (20, 23, 30, 32, 40, 41, 50, 51, 55, 63, 74, 80, 93, 102, 105, 106, 124–126, 128–132). A variety of breastfeeding practices were measured, and evidence of the association between breastfeeding and child growth in Ethiopia is mixed, although several studies did note a positive impact (19, 29, 36, 38, 40, 43–45, 49, 50, 52, 55, 56, 60, 63, 64, 69, 71, 75, 77, 79, 83, 85, 95–97, 101, 102, 105, 110, 111, 120, 124, 125, 127, 128, 132–143). Nearly all of the studies that explored the relation between stunting outcomes and complementary feeding found that it is significantly associated with child growth (58, 64, 100, 112, 119, 133, 134, 136, 139, 141). A number of studies examined the impact of food security on growth and most found that household food insecurity was negatively associated with HAZ, or positively associated with stunting (35, 47, 52, 75, 80, 113, 114, 131–134).
Immediate causes of stunting decline were identified as dietary intake, disease, maternal characteristics (age, height, BMI, and parity), and child characteristics (age, gender, birth weight, birth order, and number of children in the household). Studies highlighted the significance of improved dietary intake, dietary diversity, and consumption of multiple micronutrients, especially for children in early infancy (19, 30, 69, 70, 37, 38, 60, 64–68). Two studies examined the effect of disease on stunting and found no association (19, 85), although studies that looked at anemia found a dose–response relation between anemia severity and stunting risk (23, 27, 37). Diarrhea was also found to be an important risk factor for stunting outcomes (19, 38, 115), as was fever (27, 38, 78, 115); however, most studies treated ARI as an outcome with stunting as a significant predictor, not the other way around, which is an area for future research (60, 67, 69, 116). Literature showed that, generally, maternal age was not associated with stunting risk (20–23, 31, 34, 37, 85), but that mothers of shorter height (17, 19, 20, 31, 34, 37, 38, 47, 66, 85) or those with lower BMI were found to be more likely to have stunted children (19, 22, 23, 27, 28, 31, 37, 47, 60, 64), whereas increasing interpregnancy interval and fewer births are associated with a reduction in stunting outcomes (21, 23, 26, 31, 32, 37, 38, 96). With regard to child characteristics, studies emphasize that as child age increases, so do stunting outcomes (19, 20, 22–27, 29–32, 38, 47, 60, 64, 67, 69, 84, 86, 117, 118). In addition, under-5 boys were found to be more likely to be stunted than girls ( 19–23, 25, 27–29, 31, 37, 38, 47, 60, 64, 67, 69, 77, 84, 85, 118), whereas low-birth-weight children were at an increased risk of stunting outcomes (19, 22, 27, 37, 38, 59, 60, 64, 67, 85). A significant association was not found between birth order and stunting outcomes (16, 19, 22, 25–27, 34) but the majority of studies that looked at the number of children in households found that as the number of children under-5 in a household rises, stunting risk does as well (20, 21, 23, 47, 64, 85).
The aim of this research was to conduct a systematic assessment of the determinants that have driven stunting reduction in Ethiopia from 2000 to 2016, specifically on a national, community, household, and individual level. The 3 objectives included 1) to quantitatively examine determinants of stunting reduction in Ethiopia and to decompose long-term stunting change into relative contributions from key drivers; 2) to explore national- and community-level perspectives on the nutrition evolution (focused on progress in stunting) in Ethiopia and the major contributing factors behind it; and 3) to generate a systematic landscape of the major stunting-relevant policies and programs in Ethiopia, with a focus on both nutrition-specific and -sensitive initiatives.
Methods
Study design
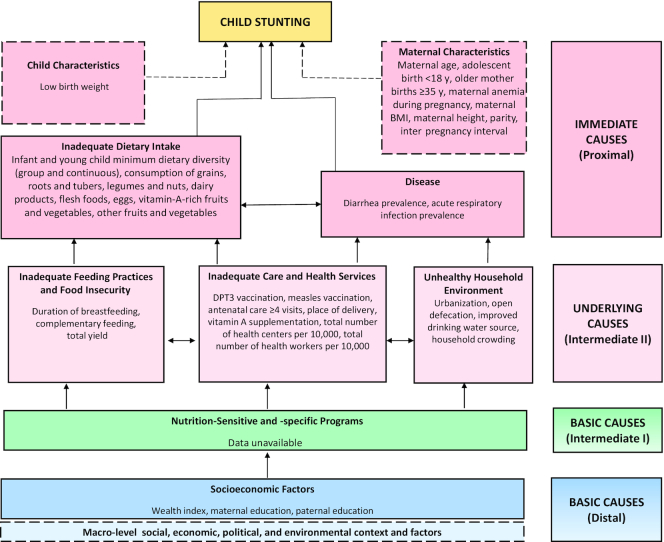
This study involved 4 methods of inquiry including a systematic literature review, retrospective quantitative data analysis, qualitative data collection and analysis, and policy and program analyses. The time period covered was from 2000 to 2016, at three 5-y intervals (2000–2005, 2005–2011, 2011–2016). A conceptual framework was adapted from the 1995 UNICEF Nutrition Framework and the 2008 Lancet Nutrition framework, and informs the quantitative and qualitative data analyses. This framework identifies the key distal-, intermediate-, and proximal-level factors that potentially contributed to Ethiopia's stunting decline (Figure 2). Ethics approval for the study, inclusive of primary data collection, was obtained through the University of Addis Ababa's research ethics process. Ethics approval for the broader stunting case study was also obtained through the Research Ethics Board at the Hospital for Sick Children (SickKids), in Toronto, Canada.
FIGURE 2.
Conceptual framework showing distal, intermediate, and proximal determinants of stunting in Ethiopia. Framework reflects only indicators that were measurable and available for quantitative analysis. Skilled birth attendance was omitted because estimates were not available for the first year of study, and were only available for the last 2 y studied (2011 and 2016). Flesh foods refers to meat, fish, poultry, and liver/organ meats. Data on early initiation of breastfeeding were also unavailable and were omitted. Other variables included in analyses were child age in months, child sex, child weight, and child height. DPT3, 3 doses of Diphtheria-tetanus-pertussis vaccine.
Systematic literature review
The systematic literature review resulted in 10,789 total articles being found, and consisted of a search for peer-reviewed literature, as well as gray literature, published between 1990 and 2019. Search terms used included “stunting” or “linear growth” or “linear growth stunting” or “HAZ” or “height” or “height-for-age” or “LAZ” or “length” or “length-for-age” or “undernutrition” or “malnutrition” or “nutr*” AND “child*” or “infan*” AND “Ethiopia*.” The initial database search found 10,789 records, and after duplicates were removed and records were screened, a total of 150 were included in our analysis, of which 5 were systematic reviews, 124 were quantitative analyses, and 21 were gray literature. More detailed information on the search terms, as well as the literature review flow diagram, can be found in Supplemental Appendix 2.
Quantitative methods
Data sources
The sources of data used for the quantitative analyses were 4 Demographic and Health Surveys (DHSs) from 2000, 2005, 2011, and 2016. Table 1 shows the sample size breakdown of under-5 children with available anthropometry data for these 4 surveys.
TABLE 1.
Sample size by survey based on the index child with valid anthropometric data
| Year of Demographic and Health Survey | ||||
|---|---|---|---|---|
| Age group | 2000 | 2005 | 2011 | 2016 |
| <5 y | 5975 | 2600 | 6561 | 6184 |
| <36 mo | 4623 | 1980 | 4998 | 4800 |
| 6–23 mo | 2470 | 1113 | 2615 | 2620 |
| ≥24 mo | 2697 | 1164 | 2978 | 2640 |
| <6 mo | 808 | 323 | 968 | 924 |
Outcomes and covariables
The main study outcomes included child height-for-age z score (HAZ) and stunting prevalence (HAZ < −2SD), as they were estimated from the WHO child growth standards (144). In line with Figure 2, covariables were selected as they were available in DHSs (individual/household variables) and the Agricultural Sample Survey conducted by Ethiopia's Central Statistical Agency (ecological variables at district level). We grouped potential stunting determinants hierarchically as distal, intermediate, and proximal factors that align with “basic causes,” “underlying causes,” and “immediate causes” in Figure 2.
Statistical analysis
Child HAZ kernel density plots were estimated for all survey years in order to examine population shifts in growth faltering over time. “Victora curves” or child HAZ-against-age plots were calculated using smoothed local polynomial regressions to enable examination of the growth faltering process from birth to 60 mo (145). We used piecewise linear splines to estimate the slopes and inflection points of the Victora curve growth trajectories (146). Equity analysis was conducted using standardized and well-established methods in order to study stunting prevalence disaggregated by wealth quintile, maternal education, area of residence (urban compared with rural), and child gender (147, 148). Wealth quintiles were derived using principal components analysis of household asset data. We also calculated the slope index of inequality (SII) and concentration index (CIX) in order to measure absolute and relative socioeconomic inequalities, respectively (147, 148). To assess the relative change (decline) in stunting prevalence of Ethiopia's districts, we calculated compound annual growth rates (CAGRs).
A series of stepwise linear regression models and hierarchical modeling were used to conduct 2 sets of multivariable analyses between HAZ and distal-, intermediate- and proximal-level variables as suggested in the literature (149). The DHS 2000–2016 rounds were assembled into a panel data set to conduct difference-in-difference (DID) analysis with time × covariable interaction terms to understand if a change in a proposed predictor of HAZ led to a change in HAZ over the studied time period (150). Regression-based Oaxaca–Blinder decomposition methods were used to decompose the change in mean child HAZ between 2000 and 2016 into the covariables that drove this change. Full methods details are included in Supplemental Appendix 3 and the methods article in this series (Akseer et al.). All analyses were conducted with Stata version 14.0 (StataCorp LLC) and accounted for survey design and weighting.
Policy and program review
Key nutrition-specific and nutrition-sensitive policies and programs in Ethiopia were incorporated into a timeline using an iterative approach. Literature was identified through a systematic approach in order to suggest a timeline which was then shared with expert stakeholders for them to corroborate and provide insight. Any additional policy/program documents suggested by stakeholders were added to the second iteration of the timeline, and the process was repeated until consensus was reached. Further, rating was done by stakeholders and research team members to evaluate the relative importance of the policies/programs to the observed reduction in stunting.
Qualitative methods
Qualitative research was conducted in 2019 using in-depth interviews with key informants at the national and community levels, and focus group discussions (FGDs) with mothers in communities. In-depth interviews were conducted with national stakeholders, including nutrition experts, representatives from multi- and bilateral international donor organizations, representatives of related ministries, and state agencies. Interviews with both national and community informants asked respondents to describe key nutrition-specific and -sensitive events in Ethiopia. National informant interviews also asked about successful factors and barriers to implementation. Community informant interviews with regional stakeholders, including teachers and health staff, explored how contextual factors such as changes in social and economic situations, access to key resources, and community-level changes to dietary intake affected child nutrition. FGDs with mothers who gave birth to children during 3 time periods (1987–1991; 1995–1999; 2011–2015) sought women's experiences, and perspectives regarding pregnancy, breastfeeding, child nutrition, and perceived drivers of change and general trends in children's nutrition. A total of 12 FGDs were conducted—with 3 age groups each in a rural and an urban area, in 4 districts of the SNNPR and Somali regions. Data generated in interviews and FGDs were analyzed using the UNICEF Nutrition Framework, the Lancet Nutrition framework, and the adapted framework for country case studies (Figure 2). These frameworks guided the qualitative analysis and interpretation of key determinants, contextual factors, and barriers and facilitators to nutrition-specific and -sensitive events. Responses from national- and community-level stakeholders were analyzed separately. Thematic analysis was used to explore key themes that emerged regarding stunting determinants. Full methods for qualitative data collection and analysis are available in Supplemental Appendix 4.
Results
Descriptive analyses
HAZ kernel density plots and Victora curves
Figure 3A displays the HAZ kernel density plot with the HAZ distribution for children <5 y of age. The HAZ distribution from 2000 flattened out and underwent a parallel rightward shift to 2005. In comparing the 2000 and 2005 curves, the 2005 curve has a heavier right tail, indicating that more Ethiopian children are reaching a higher HAZ. By 2011, the curve shifted rightward somewhat and reached a higher peak. This indicates that the entire population of under-5 children had seen nutritional gains. This trend persisted into 2016 where the curve shifted further rightward and reached a slightly higher peak. The 2016 curve shows that by this year, more children were reaching the improved mean HAZ, which was also closer to that of the international reference population; however, the curve did flatten out, thus indicating that inequality remained present and widened slightly.
FIGURE 3.
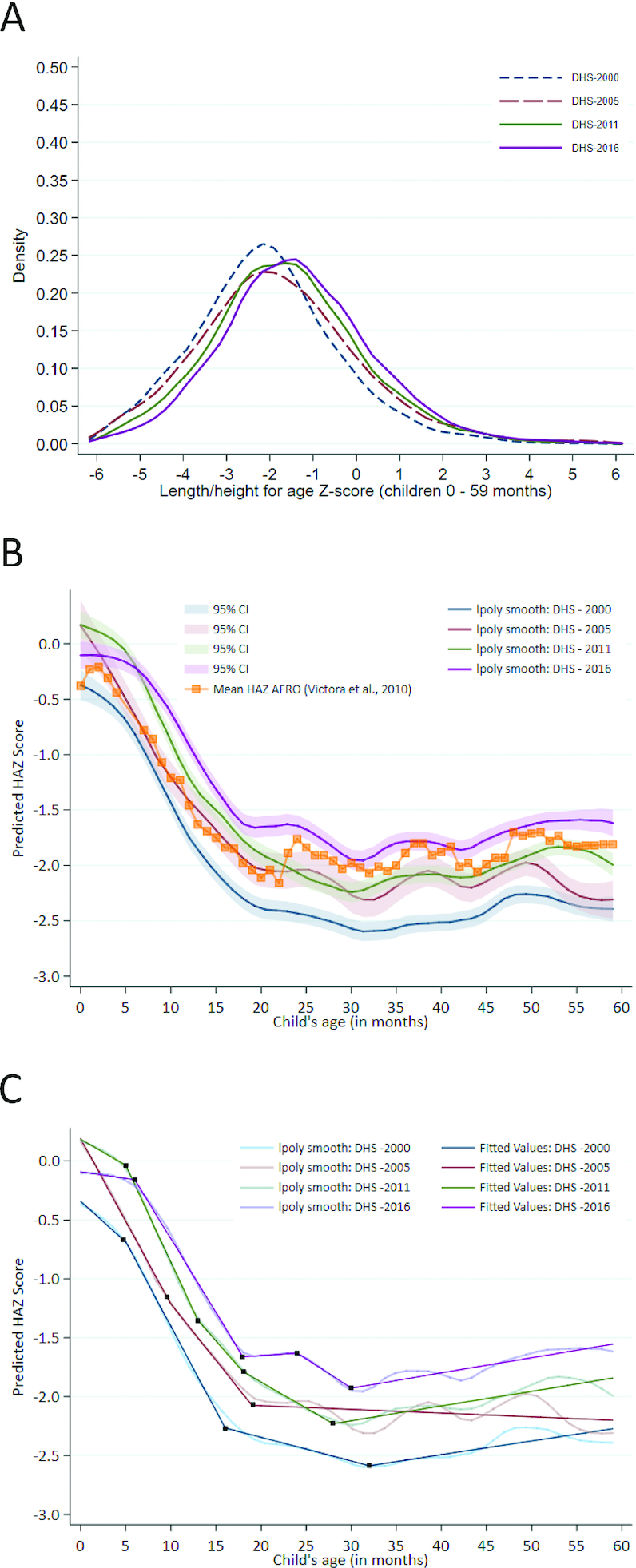
Distribution of HAZ scores and growth faltering among children under 5 y old. (A) Kernel density plot for HAZ distribution in children <5 y, DHS 2000, 2005, 2011, and 2016. (B) Victora curve using data from the 2000, 2005, 2011, and 2016 surveys among children <5 y, with 95% CIs (145). (C) Victora curve using data from the 2000, 2005, 2011, and 2016 surveys among children <5 y, with linear splines. DHS, Demographic and Health Survey; HAZ, height-for-age z score.
Figure 3B shows predicted child HAZ from smoothed local polynomial regressions plotted against child age for Ethiopian children for the 4 studied years, as well as an overlay of the growth faltering trends calculated from other countries in Africa. These curves allow for the examination of the growth faltering process from birth to 5 y of age.
Improvements in Ethiopian children's HAZ trajectory can be observed over the 16-y study period. The 2000 curve intercepts at the lowest point of all the years, suggesting that genetics and maternal nutrition throughout pregnancy may have been important markers of the child's size at birth. There was a decline in predicted HAZ in the first 6 mo of age, which may suggest that breastfeeding practices were inadequate, because this is the time in a child's development that exclusive breastfeeding is recommended to occur. A sharp decline can be observed during the growth faltering period between 6 and 24 mo of age. After 6 mo, food is being introduced to the child, and thus diet quality becomes a factor in their growth. The 2000 curve drops the lowest of all the curves during the growth faltering period, suggesting that children were consuming a poor diet and experienced unmet nutritional needs.
In 2016, the Victora curve intercepts just below the international reference population, which suggests that there had been improvements to maternal health or nutrition since 2000. The 2016 curve is markedly flatter in the first 6-mo period, indicating that infants were being breastfed and maintaining their growth during the first 6 mo of life. There remains a steep growth faltering period during which predicted HAZ declines sharply, although this decline does not reach 2011 levels. During the 16-y study period, it appears that improvements occurred in maternal health and nutrition, breastfeeding practices, and childhood nutrition.
The Victora curves were analyzed using piecewise linear regression to create linear splines which were fitted to the polynomial curves, with knots corresponding to major changes in the slope of the curve. These points suggest at which months in a child's development growth changes significantly. In 2000, the sharpest decline occurred between 5 and 16 mo of age at a rate of −0.14 SD/mo (Figure 3C; detailed coefficient estimates in Supplemental Appendix 5). By 2016, the period of greatest growth faltering was between 6 and 18 mo of age, at a slightly more moderate rate of −0.13 SD/mo. Despite fluctuations at 18 and 24 mo, the predicted HAZ in 2016 did not ever fall to stunted levels. Although the trajectories over time were similar, the absolute levels of HAZ were around half an SD higher in 2016 than in 2000.
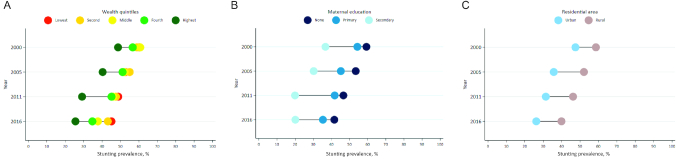
Equity analysis
Stunting prevalence in Ethiopia declined from 51% in 2000 to 32% in 2016, although declines were not uniform and geographic disparities were large. Stunting prevalence was highest in Amhara and lowest in Addis Ababa in all 4 y studied (Figure 4A). Declines in stunting prevalence were observed in all but 1 region, and the CAGR was lowest for Addis Ababa, followed by Somali and Gambela, indicating that stunting declined most in these regions (Figure 4B). By 2016, these were the 3 regions with the lowest stunting prevalence at 15%, 27%, and 23%, respectively. Stunting prevalence in Dire Dawa increased over the studied time period, and the next highest CAGR was in Benishangul-Gumaz, which had the most modest declines in stunting. Regional stunting prevalence for other years can be found in Supplemental Appendix 5.
FIGURE 4.
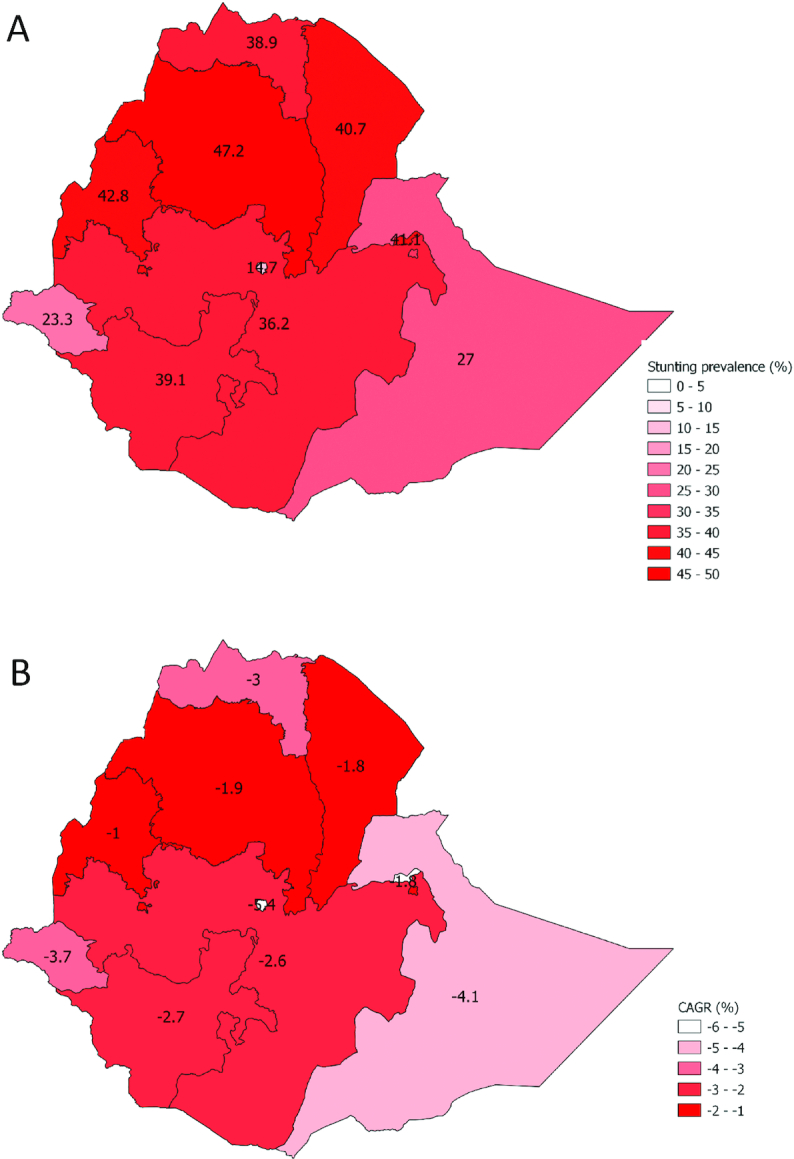
Subnational stunting estimates and rates of change in Ethiopia. (A) Subnational stunting estimates for children under-5 in Ethiopia, 2016. (B) Subnational stunting rates of change for children under-5 in Ethiopia. CAGR, compound annual growth rate; SNNPR, Southern Nations, Nationalities, and Peoples’ Region.
Stunting decline occurred across all wealth quintiles from 2000 to 2016; however, the gaps between rich and poor nearly doubled over this time period, because the wealthy experienced lower stunting prevalence and larger declines over time (Figure 5A). The SII and CIX plots show that both absolute and relative socioeconomic inequalities rose in Ethiopia (see Supplemental Appendix 5). Disaggregating by maternal education shows that mothers with higher levels of education had lower levels of stunting prevalence; however, the greatest stunting declines between 2000 and 2016 occurred among mothers with no or primary level of education (Figure 5B). Stunting prevalence was reduced for children living in both urban and rural areas. Slightly greater reductions occurred for children in urban areas, which also consistently experienced significantly lower stunting prevalence rates (Figure 5C). Supplemental Appendix 5 graphs disaggregation by child sex, and shows that boys consistently had a slightly higher stunting prevalence than girls, and that disparities between boys and girls widened over time.
FIGURE 5.
Stunting prevalence disaggregation by contextual factors. (A) Stunting prevalence disaggregated by wealth quintiles, 2000–2016. (B) Stunting prevalence disaggregated by maternal education, 2000–2016. (C) Stunting prevalence disaggregated by residential area, 2000–2016.
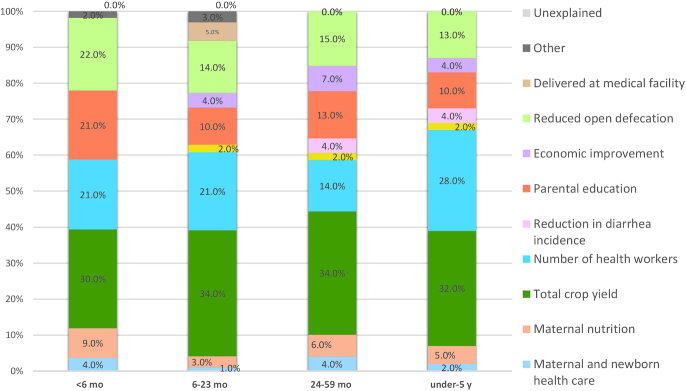
Multivariable analyses
Decomposition analysis reveals that the top 4 explanatory factors for stunting decline were the same across all 3 age groups (Figure 6). See Supplemental Appendix 5 for supporting analyses. The top explanatory factor was increased total agricultural yield (between 32% and 34%), followed by increased number of health workers (14%–28%). Reductions in open defecation (13%–15%) and parental education (10%–13%) were the third and fourth explanatory factors for all age groups. Economic improvement also explained HAZ increases for all age groups, whereas reduction in diarrhea incidence contributed to only the ≥2 y and under-5 age groups. Maternal and newborn health care was most impactful for the 6- to 23-mo age group (6%), because it included a measure of delivery in a health facility. Maternal nutrition and fertility were also impactful for all age groups, and they explained between 2% and 6% of HAZ change.
FIGURE 6.
Decomposing predicted changes in HAZ (i.e., percentage contribution of determinant domains) from 2000 to 2016. Parental education breakdown: children 6–23 mo: maternal: 3.3%, paternal: 3.8%; children 24–59 mo: maternal: 7.5%, paternal: 0%; children under-5: maternal: 4.6%, paternal: 3.6%. For the 6- to 23-mo age category, delivery in medical facility is included in maternal and newborn health care (6.7%). Other category includes child age, gender, and region for all age groups in addition to maternal age (0.5%) for the 6- to 23-mo age group. HAZ, height-for-age z score.
The DID analyses (Supplemental Appendix 5) showed that delivery in a medical facility, number of health workers, and maternal education each contributed to HAZ change between 2000 and 2016.
Policy and program review
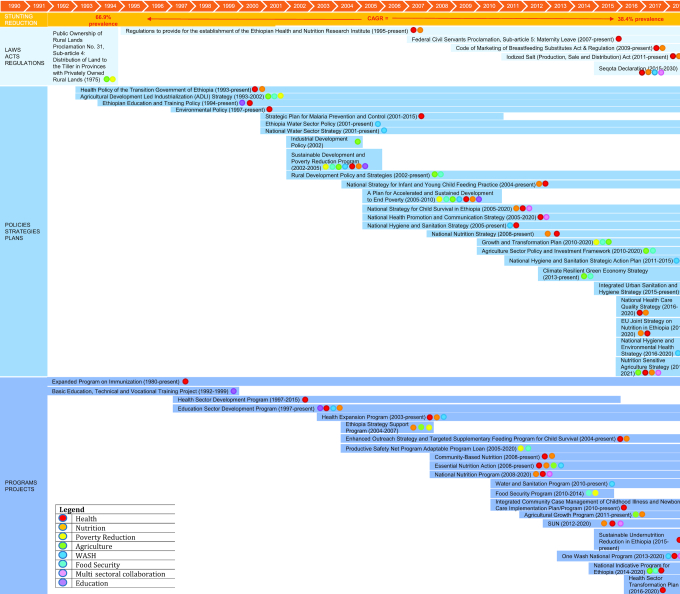
Figure 7 and Panel 2 show a timeline of Ethiopia's key nutrition-specific and -sensitive programs and policies (151–153, 154–178). Ethiopia has introduced broad national development plans, as well as focused policies and programs that worked to address malnutrition and improvements in a child's environment more generally. Significant investments in agriculture-related policies and programs led to the strengthening of ties between agriculture and industry, particularly in rural areas, as well as improvements to the agricultural labor force and proper land use. Health system–strengthening programs bolstered by the 1993 Health Policy of the Transition Government led to the expansion of primary care, increased vaccine coverage, and the introduction of community health extension workers (HEWs). Nutrition-sensitive programs and policies related to poverty reduction, the WASH sector, and expansion of primary education, particularly for girls, have also been significant in explaining stunting change. Supplemental Appendix 6 provides expanded information on each initiative.
FIGURE 7.
Overview of laws, policies, programs, and enablers 2000–2018 in Ethiopia. CAGR, compound annual growth rate; SUN, Scaling Up Nutrition Movement; WASH, water, sanitation, and hygiene.
Panel 2.
Program and policy review
After Emperor Selassie's overthrow in 1974 after pervasive socioeconomic issues and famine in 1973, the Provisional Military Administrative Council introduced Proclamation 31 in 1975. This proclamation allowed any individual willing to cultivate land to be given land not exceeding 10 hectares so as to promote equality and economic development (154, 155). Other agriculture-related policies include the Agriculture Development Led Industrialization strategy (1993–2002) which represents Ethiopia's overarching strategic framework for development. It focuses on strengthening ties between agriculture and industry in rural areas so that incomes for rural families may rise and the nation can achieve food self-sufficiency (156, 157). The Industrial Development Policy followed in 2002 and continued to work toward agriculture-led industrialization, export-led development, and labor-intensive industries (157, 158). Also in 2002, the Rural Development Policy was introduced to minimize the need for foreign aid by developing Ethiopia's market economy through initiatives such as strengthening the agricultural labor force, proper use of land, and directing agricultural development (157, 158).
The Sustainable Development and Poverty Reduction Program (SDPRP) was a 3-y program beginning in 2002 with an aim to reduce poverty in Ethiopia. It aims to achieve this through numerous initiatives such as a focus on agriculture, strengthening private-sector growth, increased exports, particularly of agricultural products, and investment in education (159). Its successor, A Plan for Accelerated and Sustained Development to End Poverty (PASDEP), aimed to work toward achievement of the Millennium Development Goals. PASDEP ended in 2010 and its scope was wide, and affected agriculture, health care, water, and child nutrition (160, 161). After PASDEP, the Growth and Transformation Plan (2010–2020) shares the goals of its predecessors in improving economic growth and ending poverty. This plan aims to quickly and equitably drive economic growth by focusing on agriculture, expanding infrastructure, empowering women, and ensuring good governance (162, 163).
Ethiopia introduced many health and nutrition-related policies and programs over the study period. The Expanded Program on Immunization began in 1980 and continues into the present. It aims to accomplish 90% coverage of all vaccines nationally by 2020. In 1993, after the end of the Derg government, the Health Policy of the Transition Government of Ethiopia was created with a focus on women and children, the rural population, the poor, minorities, and victims of disaster (179, 164–166). The Health Sector Development Program (HSDP) was introduced years later in 1997 and provided comprehensive, integrated, and cost-effective primary care (151, 169, 169). The National Strategy for Child Survival in Ethiopia was introduced in 2005 and will continue until 2020 with the goal to achieve universal high-quality health coverage for mothers and newborns in communities and health facilities (167, 168). This strategy utilizes the Health Extension Workers (HEWs) to reach communities. The HEP emanated from the HSDP in 2003 and introduced HEWs to improve equitable access to health care in rural areas, despite resource limitations. HEWs focus on 4 major components: family health, disease prevention and control, hygiene and environmental sanitation, and health education and communication (152, 170–173). The Enhanced Outreach Strategy and Targeted Supplementary Feeding Program (2004) and the National Nutritional Policy and Strategy (2008) both address child nutrition, and continue into the present (153, 166, 174, 175).
Reductions in open defecation were an important factor in stunting decline in Ethiopia, with numerous policies addressing this important issue. Ethiopia's Health Policy of the Transition Government, adopted in 1993, had a focus on sanitation and open defecation (176). The HSDP, adopted in 1997, emphasized environmental health and communicable disease prevention, ensuring a safe environment (151, 169). The HEP had a clear focus on reducing open defecation and teaching about latrines; in fact, 5 of the 16 domains were related to safe environment (152, 170–173). Poverty reduction programs including SDPRP and PASDEP both had a focus on WASH, and the latter specifically promoted the use of latrines through the HEW program (160, 161). The National Hygiene and Sanitation Strategy (2005) also emanated from the HSDP, and itself produced the National Hygiene and Sanitation Strategic Action Plan (2011) (177, 178).
Qualitative inquiry results
Across stakeholders, our qualitative analyses showed that health systems strengthening, improved access to health—and specifically reproductive, maternal, newborn, and child health—services, agriculture improvements and food security, breastfeeding promotion/improved knowledge of complementary feeding, disease prevention and management, social safety nets and poverty reduction programs, better access to education, and reductions in open defecation were named key drivers of child stunting reduction in Ethiopia. Full qualitative results can be found in Panel 3 and Supplemental Appendix 7.
Panel 3.
Qualitative inquiry results
National expert stakeholders
Interviews were conducted with 11 national key informants from various ministries in Ethiopia, and NGOs. Basic drivers of stunting decline as reported by national informants include increased urbanization, poverty reduction, improvements in education and women's empowerment, remittances and labor migration, and the decentralization and democratization process. This process helped regional states to improve agricultural productivity, infrastructure, and health services via a bottom-up process.
Nutrition-specific and -sensitive policies and programs discussed include programs related to community health, nutrition, poverty reduction, and health sector development. Barriers and facilitators of program and policy implementation were brought up, and key informants named the National Health Policy of 1993 as the primary guide for subsequent programs. Several key informants identified the HEP as the main driver of stunting decline in Ethiopia.
Underlying causes of stunting reduction discussed by national stakeholders include improvements to the household environment, food security and feeding practices, and access to health services. Improved sanitation and hygiene, specifically increased access to latrines, and major declines in open defecation were linked to the HEP:
“again thanks to the HEP a lot has been done regarding toilet utilization, especially in South and Tigray region there are open defecation free woredas.” (Ministry of Health representative)
Among the immediate causes of stunting decline are improvements in dietary intake, maternal characteristics such as fertility rate, and reductions in childhood illness such as malaria, vaccine-preventable diseases, and diarrhea.
Regional stakeholders
Regional stakeholders, including teachers and health staff (HEWs; maternal, newborn, and child health care workers; district health surveillance focal persons; and senior health center staff), were interviewed in depth across 2 regions and 4 districts. Basic drivers of stunting decline brought up by regional stakeholders include peace and security, improvements to education and women's empowerment, and poverty reduction.
A variety of nutrition-specific and -sensitive programs were discussed and implemented in community settings including the HEP, Mercy Corps, one WASH, ENGINE, PSNP, and the Pastoralist Community Development Program. The HEP was emphasized for resulting in substantial health and nutrition improvements.
Among the underlying causes of stunting reduction, interviewees discussed access to health services, WASH, and food security. The observed improvements in food security named by the regional stakeholders were related to increased agricultural production, as well as improved access to markets, availability of roads, and access to media.
Immediate causes of stunting reduction mentioned include dietary intake, infant and young child feeding, recommendations for optional breastfeeding and complementary feeding, increased contraceptive utilization, and declines in childhood communicable diseases including diarrhea, parasitic infection, typhus, and skin and eye infections. Key informants perceived limited access to animal source foods, but improved diversity of children's diets over time:
“Previously the dietary intake of people was poor. […] Children need different kinds of foods such as vegetables, fruits, rice, pasta, fish, and milk. Nowadays people consume various diets that is rich in many nutrients.” (Community informant, Somali region)
Mothers in communities
FGDs with mothers of children under-5 born during 3 time periods (1987–1991, 1995–1999, 2011–2015) were conducted in order to identify the factors that were salient in these time periods of substantial stunting decline. Poverty was mentioned as a concern by mothers of children in all 3 age groups in the Somali region; however, it was not brought up by mothers in SNNPR. Improvements in both boys’ and girls’ education, as well as improved infrastructure such as roads or housing, were brought up by mothers in both regions in the later years as distal drivers of stunting decline:
“Our view of girl education is not the same now and then. We used to think that a girl that goes out early to learn was a bad girl. […] Now we educate both genders equally.” (Mother FGD Aware, Somali, 1995–1999)
Neither mothers in the Somali region nor those in SNNPR brought up any nutrition-specific and -sensitive policies, likely because they were not prompted on these and they may not have been familiar with specific government initiatives. Mothers in Somali were concerned about drought and water shortage in all years, and the price of food in later years. Mothers in both regions brought up access to a safe water supply as concerning as well. Improved hygiene and sanitation, and health service access were mentioned by mothers in both regions in the latest group, whereas mothers in SNNPR in the latest group also spoke about improved crop production.
Immediate causes of stunting decline spoken about by mothers in both the Somali region and SNNPR in the later years include improved child vaccination, and a decreased concern about childhood illness because health services were readily available. Mothers in the SNNPR region also brought up improved access to fruits and vegetables and improved child care in later years.
Discussion
Summary
Our mixed-methods case study suggests a variety of contributors to under-5 stunting decline, including targeted nutrition-sensitive and -specific policies and programs, that led to improvements in underlying and immediate causes of child malnutrition. Key national investments in agriculture, sanitation, health, education, and poverty reduction have been essential to achieving these gains.
Numerous agriculture-focused policies allowed individuals to cultivate land, improve crop output, increase economic opportunities, and reduce food insecurity, particularly in rural areas. Health sector development policies combined with the proliferation of facilities and health workers in communities led to increased access to health services, improved knowledge through nutritional advice, and reductions in open defecation. This availability of health knowledge, combined with improved women's empowerment through increased girls’ schooling, allowed mothers to make more informed decisions around family planning and child feeding practices. Multisectoral poverty reduction programs contributed to economic improvement and affected agriculture, health care, water and sanitation, women's empowerment, and child nutrition.
Triangulating evidence from our qualitative analyses, quantitative analyses, policy review, and systematic literature review showed that the aforementioned themes recur as major contributors to stunting decline in Ethiopia. Underlying this was the government's push toward decentralization and democratization, with a focus on the country's large rural population to provide equitable services and reach development goals.
Study strengths and limitations
Our study has 5 key strengths. First, to our knowledge, it is the first systematic mixed-methods analysis of the major determinants of stunting in Ethiopia, using a multitude of research methods in order to draw a holistic picture of the country's stunting situation. Second, we used a comprehensive set of variables in order to explore a range of determinants at all levels of the conceptual framework. Third, our quantitative analyses incorporated a hierarchical modeling approach such that we were able to build appropriate modeling pathways between potential stunting determinants that adjusted for confounders and let us examine mediators. Fourth, our qualitative analyses captured diverse and multilevel perspectives, with 12 FGDs with mothers and interviews with both community and national stakeholders. This allowed for varied opinions on the tangible changes in socioeconomic status, local infrastructure, behavior, health, and nutrition over time. Finally, our study was the first to systematically compile all nutrition-relevant published and unpublished literature and policy analysis on Ethiopia to date.
Our study also had several limitations. First, our qualitative data collection, transcription, and analysis were conducted primarily in the local language, which may have contributed to points being lost in translation. Interviews and FGDs could have been affected by recall bias, especially for mothers of children born in the earliest time period (1987–1991). Second, our study uses Oaxaca–Blinder decomposition analysis and, as such, previously cited limitations of this method apply (17, 180, 181). Third, although we adjusted for confounding variables in our quantitative analyses, residual confounding may remain from unmeasured confounders or poorly estimated variables. Fourth, mapping of financial data pertaining to nutrition-specific and -sensitive initiatives in Ethiopia may be incomplete, because data were obtained from stakeholders and published literature only, and were scarce. Lastly, measures of certain variables such as food insecurity, intrauterine growth, and dietary intake for children under-5 were lacking, requiring the use of proxy variables where appropriate and available.
Existing evidence
This study of Ethiopia's stunting decline reveals a multidimensional story incorporating contextual factors in conjunction with targeted policies and programs that worked to improve the underlying and immediate causes of child malnutrition.
Stunting in Ethiopia declined by 18.5% points, with mean HAZ rising significantly between 2000 and 2016. Improvements in health, nutrition, and stunting were achieved in spite of ongoing ethnic clashes, conflicts with neighboring countries, the Ethiopian–Eritrean war, and climate shocks including major droughts in 2002–2003 and 2011 leading to a high level of food insecurity. Advances were achieved through reactive implementation of poverty alleviation strategies, including social protection and resettlement programs. In addition, agriculture-related policies and programs contributed to improved crop yields, reducing household food insecurity and bolstering economic improvements, especially among Ethiopia's rural population.
Our study identified several main drivers of stunting reduction, namely, improved agricultural production, health system strengthening and reforms, reductions in open defecation, poverty reduction, and improvements in education, all of which would not have been possible without strong government support and buy-in. Agriculture was a major contributing factor to improved child HAZ in Ethiopia, and has been a driving force behind the increased economic and social stability in the country. Beginning with the Public Ownership of Rural Lands Proclamation in 1975, and continuing with the Agricultural Development Led Industrialization Strategy (1993–2002), the Industrial Development Policy (2002), and the Rural Development Policy and Strategies (2002–present), the Ethiopian government has invested heavily in the agricultural sector. These investments appear to have paid off, because in 2018, the agricultural sector employed 60% of all employed women and 72% of employed men (182). The production of staple crops has risen steadily since 1990 across all regions, as has production of fruits, vegetables, and animal-source products (183, 184). Increased crop yield was the top explanatory factor in our decomposition analyses, and improved diet diversity and availability of fruits and vegetables were noted by both stakeholders and mothers. Although our literature review did not allow for definitive conclusions, there was evidence that HAZ change in Ethiopia could be explained in part by climate and food shocks (76, 78, 80), and that environmental disruptions are associated with lower HAZ.
Ethiopia's health system has undergone a number of reforms which resulted in marked improvements in health and reductions in stunting among children under-5. Health services were decentralized, allowing local governments to place emphasis on health service availability in rural communities and expand primary care provision. Policies and programs including the Expanded Plan on Immunization, the Health Policy of the Transition Government of Ethiopia, the Health Sector Development Program, and the Health Extension Program (HEP) served to spread the provision of community-based health services and expand preventative health interventions including immunization, WASH initiatives, and advice on nutrition and infant feeding practices (151, 164–166, 169–173, 176, 185). Our quantitative analysis showed that the total number of health workers and facilities increased, as did deliveries at a medical facility. Our decomposition analysis demonstrated that the increases in maternal and newborn health care and in the number of health workers positively contributed to increases in HAZ. This finding is corroborated by our qualitative research, wherein respondents consistently spoke about expansion of health facilities and increased coverage of basic health services as contributors to stunting decline. In addition, the literature indicates that skilled birth attendance and antenatal care are both negatively associated with stunting outcomes in Ethiopia.
Open defecation was identified by our decomposition analysis as the third most important factor in explaining HAZ change in children under-5, and reductions in diarrhea also contributed to this change. These improvements were likely linked to community-led sanitation programs that fell under the umbrella of the HEP. National and regional stakeholders identified these programs as the reason for increased construction of pit latrines and community engagement in healthy WASH practices taught by HEWs. Additional programs, including the National Hygiene and Sanitation Strategy and Action Plan and the Community-led Total Sanitation Program, aided in open defecation reduction and, ultimately, open defecation–free communities (186, 187). Interviews with mothers in Ethiopian communities corroborated these achievements, because mothers of children born in later years discussed improved hygiene and sanitation. Despite these achievements, safe water access remains an outstanding issue for many Ethiopians—a finding that was noted by interview respondents and highlighted by our quantitative data.
With support from the literature on the role of improved wealth on increased HAZ (16, 17, 19–29, 31, 34, 37, 47, 60, 77, 81, 82), our study found that poverty reduction and economic growth were key drivers of stunting reduction in Ethiopia. Ethiopia's economy grew significantly over the last 2 decades, and the country aims to reach lower middle income status by 2025 (188). National experts, community stakeholders, and mothers expressed in interviews that improvements in agricultural yield, employment opportunities, and government support programs drove these economic gains and were related to improvements in stunting. A national priority in Ethiopia, poverty reduction programs introduced by the government include the Sustainable Development and Poverty Reduction Program, the Plan for Accelerated and Sustained Development to End Poverty, and the Growth and Transformation Plan. Our decomposition analyses show that improvements in household wealth explained a portion of HAZ change for all age groups studied. However, equity analyses revealed that improvements did not occur uniformly, because stunting prevalence reduction favored the wealthy across all time periods, and both relative and absolute inequalities increased over time.
Finally, improvements in education have been a driver of stunting decline. The percentage of literate women rose between 2000 and 2016, as did the percentage of women with secondary or higher education. Our equity analyses provide some pathways by which child HAZ was associated with maternal education, namely that compared with mothers with no education, those with some education had increased rates of care seeking for diarrhea and acute respiratory infection (ARI), improved vaccination rates, greater piped water access, and reduced open defecation. Decomposing HAZ change in Ethiopia over the study period, we found that parental education accounted for a portion of the change observed. The literature supports our findings, because both maternal and paternal education have been found to be positively associated with HAZ (16–21, 23–26, 28, 30, 32, 103). National and regional stakeholders, as well as mothers in SNNPR and Somali, corroborated the improvements to education, particularly of girls and women, and the accompanying advances in child care and nutritional knowledge. Programs that have helped achieve these gains include the Ethiopian Education and Training Policy (189) and the Education Sector Development Program (190) which seek to ensure universal primary education, improved access, and, more recently, quality of education.
Remaining challenges and future research
Although stunting prevalence at the national level has declined substantially, regional variations remain. Certain regions, especially those in the north such as Amhara, continue to have a very high stunting prevalence. Dire Dawa in particular increased stunting prevalence over time; this may be due to persistent droughts, land shortages and degradation, shortage of water for irrigation, lack of political will for enhancing agricultural practices (191–193), lower levels of education and higher fertility (192), and generally poor economic indicators relative to other regions (192). Government must prioritize the extension of effective programs to Dire Dawa and other regions with high stunting to accelerate stunting reduction at the national level. Children from poorer households, in rural areas, and who have uneducated mothers continue to have disproportionately higher stunting prevalence. Future nutrition strategies should take on more targeted approaches that focus on these disadvantaged groups.
Child underweight, overweight, and wasting prevalence also declined over our study period, although not uniformly. Regional variations existed among these nutritional indicators as well, with Afar and Benishangul-Gumaz having a child underweight prevalence of 35% in 2016, whereas in Addis Ababa, only 5% of children were underweight. In 2016, Somali was the region with the highest wasting prevalence, at 23%, whereas overweight was highest in Addis Ababa at 7%. Whereas maternal short stature remained <5% over our study period, maternal anemia was persistently high, particularly in the Somali region at a staggering 60%. Maternal underweight also varied by region and was highest in Afar in 2016 at 38%, and lowest in Addis Ababa at 13%. These remain challenges and areas for future research as Ethiopia continues to work toward improving maternal and child nutrition.
Conclusion
Through political will, leadership, and prioritization of nutrition, this study of stunting decline in Ethiopia shows a multifactorial story of change. Nutrition-specific and -sensitive approaches focused on the agricultural sector to increase household food security and decrease poverty, the health sector to increase service utilization and health care access, and multisectoral efforts to improve access to sanitation and reduction in open defecation.
Supplementary Material
Acknowledgments
We sincerely thank the Technical Advisory Group for key oversight throughout the research process, including Zulfiqar Bhutta (The Hospital for Sick Children), Shawn Baker (Bill and Melinda Gates Foundation), Robert Black (Johns Hopkins University), Sue Horton (University of Waterloo), Joanne Katz (Johns Hopkins University), Purnima Menon (International Food Policy Research Institute), Meera Shekar (The World Bank), and Cesar Victora (Federal University of Pelotas). Special thanks to Goutham Kandru, Kevin Ho, Oliver Rothschild, and Niranjan Bose from Gates Ventures for funding support and overall technical/research support to the project. Acknowledgment also goes to students and research staff at the Centre for Global Child Health—Zahra Hussain, Argie Gingoyon, Kimberly D Charbonneau, Rachel Jardine, Ahalya Somaskandan, and Marianne Stefopulos—for research support throughout the case study.
The authors’ responsibilities were as follows—HT, NA, SHG, BSE, AM, MI, AA, EC, and SB: analysis; HT and NA: drafted the manuscript; NA and ZAB: designed the study; HT, NA, ZAB, SHG, EK, and BSE: critically revised the manuscript; ZAB: has primary responsibility for the final content; and all authors: contributed to interpretation of the data and read and approved the final manuscript. The authors report no conflicts of interest.
Notes
Funded by a grant to the Centre for Global Child Health from Gates Ventures. The funder had no role in the design, implementation, analysis, or interpretation of the data.
Supplemental Appendices 1–7 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/ajcn/.
Data described in the article, code book, and analytic code will be made available upon request pending application and approval.
AA to JW authors organized alphabetically.
Published in a supplement to the American Journal of Clinica lNutrition. The Guest Editor for this supplement was Mark Manary, and has no disclosures. Publication costs for this supplement were defrayed in part by the payment of page charges by Gates Ventures. The opinions expressed in this publication are those of the authors and are not attributable to the sponsors or the publisher, Editor, or Editorial Board of theAmerican Journal of Clinical Nutrition. The Supplement Coordinator for the supplement publication was Nadia Akseer, Gates Ventures/Hospital for Sick Children, Toronto, Canada. Supplement Coordinator disclosure: no conflicts to disclose. The Stunting Exemplars research Principal Investigator was Zulfiqar A Bhutta, Hospital for Sick Children, Toronto, Canada. Principal Investigator disclosure: no conflicts to disclose.
Abbreviations used: ARI, acute respiratory infection; CAGR, compound annual growth rate; CBNP, Community-based Nutrition Program; CIX, concentration index; DHS, Demographic and Health Survey; DID, difference-in-difference; FGD, focus group discussion; HAZ, height-for-age z score; HEP, Health Extension Program; HEW, health extension worker; HSDP, Health Sector Development Program; PASDEP, A Plan for Accelerated and Sustained Development to End Poverty; PSNP, Productive Safety Net Program; SBA, skilled birth attendant; SDPRP, The Sustainable Development and Poverty Reduction Program; SII, slope index of inequality; SNNPR, Southern Nations, Nationalities, and Peoples’ Region; TSF, Targeted Supplementary Food Program; WASH, water, sanitation, and hygiene.
Contributor Information
Hana Tasic, Centre for Global Child Health, Hospital for Sick Children, Toronto, Ontario, Canada.
Nadia Akseer, Centre for Global Child Health, Hospital for Sick Children, Toronto, Ontario, Canada; Dalla Lana School of Public Health, University of Toronto, Toronto, Ontario, Canada.
Seifu H Gebreyesus, Department of Nutrition and Dietetics, School of Public Health, Addis Ababa University, Addis Ababa, Ethiopia.
Anushka Ataullahjan, Centre for Global Child Health, Hospital for Sick Children, Toronto, Ontario, Canada.
Samanpreet Brar, Centre for Global Child Health, Hospital for Sick Children, Toronto, Ontario, Canada.
Erica Confreda, Centre for Global Child Health, Hospital for Sick Children, Toronto, Ontario, Canada.
Kaitlin Conway, Centre for Global Child Health, Hospital for Sick Children, Toronto, Ontario, Canada.
Bilal S Endris, Department of Nutrition and Dietetics, School of Public Health, Addis Ababa University, Addis Ababa, Ethiopia.
Muhammad Islam, Centre for Global Child Health, Hospital for Sick Children, Toronto, Ontario, Canada.
Emily Keats, Centre for Global Child Health, Hospital for Sick Children, Toronto, Ontario, Canada.
Afrah Mohammedsanni, Department of Nutrition and Dietetics, School of Public Health, Addis Ababa University, Addis Ababa, Ethiopia.
Jannah Wigle, Centre for Global Child Health, Hospital for Sick Children, Toronto, Ontario, Canada.
Zulfiqar A Bhutta, Centre for Global Child Health, Hospital for Sick Children, Toronto, Ontario, Canada; Dalla Lana School of Public Health, University of Toronto, Toronto, Ontario, Canada; Center of Excellence in Women and Child Health, The Aga Khan University, Karachi, Pakistan.
References
- 1. Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, De Onis M, Ezzati M, Grantham-McGregor S, Katz J, Martorell R et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382:427–51. [DOI] [PubMed] [Google Scholar]
- 2. Addo OY, Stein AD, Fall CHD, Gigante DP, Guntupalli AM, Horta BL, Kuzawa CW, Lee N, Norris SA, Osmond C et al. Parental childhood growth and offspring birthweight: pooled analyses from four birth cohorts in low and middle income countries. Am J Hum Biol. 2015;27:99–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sudfeld CR, Charles McCoy D, Danaei G, Fink G, Ezzati M, Andrews KG, Fawzi WW. Linear growth and child development in low- and middle-income countries: a meta-analysis. Pediatrics. 2015;135:e1266–75. [DOI] [PubMed] [Google Scholar]
- 4. Leroy JL, Frongillo EA. Perspective: what does stunting really mean? A critical review of the evidence. Adv Nutr. 2019;10:196–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. UNICEF Joint child malnutrition estimates: levels and trends. New York, NY: UNICEF; 2017. [Google Scholar]
- 6. Megistu A, Nagel P, Getahun A, Saber SA, Loader SP. Updated review of amphibian diversity, distribution and conservation in Ethiopia. Ethiop J Biol Sci. 2013;12:81–116. [Google Scholar]
- 7. World Bank Group Rural population (% of total population) – Ethiopia | data. [Internet] Open Data Washington (DC): World Bank; 2018; [cited 28 May 2019]. Available from: https://data.worldbank.org/indicator/SP.RUR.TOTL.ZS?locations=ET. [Google Scholar]
- 8. Central Intelligence Agency (CIA) Africa: Ethiopia – The World Factbook. [Internet] Washington (DC): CIA; 2019; [cited 28 May 2019]. Available from: https://www.cia.gov/library/Publications/the-world-factbook/geos/et.html. [Google Scholar]
- 9. Rajkumar AS, Gaukler C, Tilahun J. Combating malnutrition in Ethiopia: an evidence-based approach for sustained results. [Internet] Washington (DC): World Bank; 2011; [cited 28 May 2019] Available from: http://documents.worldbank.org/curated/en/456711468024616593/pdf/660480PUB0EPI10mbating0malnutrition.pdf. [Google Scholar]
- 10. World Bank Group World Bank Climate Change Knowledge Portal: Ethiopia: vulnerability. [Internet] Washington (DC): World Bank; 2019; [cited 4 June 2019]. Available from: https://climateknowledgeportal.worldbank.org/country/ethiopia/vulnerability. [Google Scholar]
- 11. Araya A, Stroosnijder L. Assessing drought risk and irrigation need in northern Ethiopia. Agric For Meteorol. 2011;151:425–36. [Google Scholar]
- 12. Ethiopia Office of the Population and Housing Census Commission Summary and statistical report of the 2007 Population and Housing Census: population size by age and sex. [Internet] Addis Ababa: Federal Democratic Republic of Ethiopia, Population Census Commission; 2008; [cited 28 May 2019]. Available from: https://www.worldcat.org/title/summary-and-statistical-report-of-the-2007-population-and-housing-census-population-size-by-age-and-sex/oclc/502444786. [Google Scholar]
- 13. Mesfin B. Ethiopia's role and foreign policy in the Horn of Africa. Int J Ethiop Stud. 2012;6:87–113. [Google Scholar]
- 14. World Bank Group Fertility rate, total (births per woman) – Ethiopia | data. [Internet]. Open data Washington (DC): The World Bank; 2018; [cited 7 March 2019]. Available from: https://data.worldbank.org/indicator/SP.DYN.TFRT.IN. [Google Scholar]
- 15. World Bank Group Ethiopia Poverty Assessment 2014. Washington (DC): World Bank; 2015. [Google Scholar]
- 16. Headey D. An analysis of trends and determinants of child undernutrition in Ethiopia, 2000–2011. [Internet] Washington (DC): International Food Policy Research Institute; 2014 [cited 7 March 2019]. Available from: http://ebrary.ifpri.org/utils/getfile/collection/p15738coll2/id/128896/filename/129107.pdf. [Google Scholar]
- 17. Headey D, Hoddinott J, Park S. Accounting for nutritional changes in six success stories: a regression-decomposition approach. Glob Food Sec. 2017;13:12–20. [Google Scholar]
- 18. Getahun Z, Urga K, Genebo T, Nigatu A. Review of the status of malnutrition and trends in Ethiopia. Ethiop J Health Dev. 2001;15:55–74. [Google Scholar]
- 19. Woodruff BA, Wirth JP, Bailes A, Matji J, Timmer A, Rohner F. Determinants of stunting reduction in Ethiopia 2000 – 2011. Matern Child Nutr. 2017;13:e12307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Biadgilign S, Shumetie A, Yesigat H. Does economic growth reduce childhood undernutrition in Ethiopia?. PLoS One. 2016;11:e0160050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Biadgilign S, Ayenew HY, Shumetie A, Chitekwe S, Tolla A, Haile D, Gebreyesus SH, Deribew A, Gebre B. Good governance, public health expenditures, urbanization and child undernutrition nexus in Ethiopia: an ecological analysis. BMC Health Serv Res. 2019;19:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Fantay Gebru K, Mekonnen Haileselassie W, Haftom Temesgen A, Oumer Seid A, Afework Mulugeta B. Determinants of stunting among under-five children in Ethiopia: a multilevel mixed-effects analysis of 2016 Ethiopian demographic and health survey data. BMC Pediatr. 2019;19:176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Haile D, Azage M, Mola T, Rainey R. Exploring spatial variations and factors associated with childhood stunting in Ethiopia: spatial and multilevel analysis. BMC Pediatr. 2016;16:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Tadesse M, Getabil F. Factors associated with stunting of under-five children in Ethiopia. Stat Appl. 2016;14:145–58. [Google Scholar]
- 25. Gurmu E, Etana D. Household structure and children's nutritional status in Ethiopia. Genus. 2013;69:113–30. [Google Scholar]
- 26. Woldemariam G, Genebo T. Determinants of the nutritional status of mothers and children in Ethiopia. [Internet] Calverton, MD: Measure DHS+; 2002; [cited 28 May 2019]. Available from: https://dhsprogram.com/pubs/pdf/FA39/02-nutrition.pdf. [Google Scholar]
- 27. Dessie ZB, Fentie M, Abebe Z, Ayele TA, Muchie KF. Maternal characteristics and nutritional status among 6–59 months of children in Ethiopia: further analysis of demographic and health survey. BMC Pediatr. 2019;19:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Zeleke BW, Rahman A. Prevalence and determinants of chronic malnutrition among under-5 children in Ethiopia. Int J Child Health Nutr. 2013;2:230–6. [Google Scholar]
- 29. Takele K, Zewotir T, Ndanguza D. Understanding correlates of child stunting in Ethiopia using generalized linear mixed models. BMC Public Health. 2019;19:626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rajkumar AS, Gaukler C, Tilahun T. Combating malnutrition in Ethiopia: an evidence-based approach for sustained results. Washington (DC): World Bank; 2012. [Google Scholar]
- 31. Farah AM, Endris BS, Gebreyesus SH. Maternal undernutrition as proxy indicators of their offspring's undernutrition: evidence from 2011 Ethiopia demographic and health survey. BMC Nutr. 2019;5:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Christiaensen L, Alderman H. Child malnutrition in Ethiopia: can maternal knowledge augment the role of income?. Washington (DC): World Bank; 2001. [Google Scholar]
- 33. Sohnesen TP, Ambel AA, Fisker P, Andrews C, Khan Q. Small area estimation of child undernutrition in Ethiopian woredas. PLoS One. 2017;12:e0175445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Buisman LR, Van de Poel E, O'Donnell O, van Doorslaer EKA. What explains the fall in child stunting in Sub-Saharan Africa?. SSM Popul Health. 2019;8:100384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hagos S, Hailemariam D, WoldeHanna T, Lindtjørn B. Spatial heterogeneity and risk factors for stunting among children under age five in Ethiopia: a Bayesian geo-statistical model. PLoS One. 2017;12:e0170785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Fikadu T, Assegid S, Dube L. Factors associated with stunting among children of age 24 to 59 months in Meskan district, Gurage Zone, South Ethiopia: a case-control study. BMC Public Health. 2014;14:800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Gebreegziabher T, Regassa N. Ethiopia's high childhood undernutrition explained: analysis of the prevalence and key correlates based on recent nationally representative data. Public Health Nutr. 2019;22:2099–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Suri D, Griffiths J, Ghosh S. Factors associated with stunting in Ethiopian children under 5: a comparison of DHS 2000, 2005 and 2011. FASEB J. 2014;28:620.6. [Google Scholar]
- 39. Abate KH, Belachew T. Chronic malnutrition among under five children of Ethiopia may not be economic. A systematic review and meta-analysis. Ethiop J Health Sci. 2019;29:265–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Tariku B, Mulugeta A, Tsadik M, Azene G. Prevalence and risk factors of child malnutrition in community based nutrition program implementing and nonimplementing districts from South East Amhara, Ethiopia. Open Access Libr J. 2014;1:e425. [Google Scholar]
- 41. Fentaw R, Bogale A, Abebaw D. Prevalence of child malnutrition in agro-pastoral households in Afar Regional State of Ethiopia. Nutr Res Pract. 2013;7:122–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Legesse Liben M, Abuhay T, Haile Y. Determinants of child malnutrition among agro pastorals in Northeastern Ethiopia: a cross-sectional study. Health Sci J. 2016;10:17. [Google Scholar]
- 43. Taye A, Wolde T, Seid A. Under-nutrition and related factors among children aged 6-59 months in Gida Ayana district, Oromiya Region, West Ethiopia: a community based quantitative study. J Nutr Food Sci. 2016;6:543. [Google Scholar]
- 44. Haile A, Amboma TA. Children's nutritional status and its determinants in small towns, Sebeta Hawas district, Oromia, Ethiopia. J Food Sci Nutr. 2018;1:33–47. [Google Scholar]
- 45. Shine S, Tadesse F, Shiferaw Z, Mideksa L, Seifu W. Prevalence and associated factors of stunting among 6-59 months children in pastoral community of Korahay Zone, Somali regional state, Ethiopia 2016. J Nutr Disorders Ther. 2017;7:208. [Google Scholar]
- 46. Agedew E, Chane T. Predictors of chronic under nutrition (stunting) among children aged 6-23 months in Kemba woreda, Southern Ethiopia: a community based cross-sectional study. J Nutr Food Sci. 2015;5:381. [Google Scholar]
- 47. Silva P. Environmental factors and children's malnutrition in Ethiopia. [Internet] Washington (DC): The World Bank Group; 2005 [cited 7 March 2019]. Available from:https://openknowledge.worldbank.org/handle/10986/8898. [Google Scholar]
- 48. Tesfaye M. Bayesian approach to identify predictors of children nutritional status in Ethiopia. Addis Ababa, Ethiopia: Addis Ababa University Institutional repository; 2009. [Google Scholar]
- 49. Kinfe M. Comparison of nutritional status of pre-school children among two agro ecologically different villages: the case of Ofla District, Southern Zone, Tigray, Ethiopia. Mekelle: Mekelle University, College of Health Sciences; 2013. [Google Scholar]
- 50. Batiro B, Demissie T, Halala Y, Anjulo AA. Determinants of stunting among children aged 6-59 months at Kindo Didaye woreda, Wolaita Zone, Southern Ethiopia: unmatched case control study. PLoS One. 2017;12:e0189106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Gemechu A. Determinants of nutritional status of children in Amhara Region. Addis Ababa: Addis Ababa University; 2000. [Google Scholar]
- 52. Jemal Z, Hassen K, Wakayo T. Household food insecurity and its association with nutritional status among preschool children in Gambella town, western Ethiopia. J Nutr Food Sci. 2016;6:566. [Google Scholar]
- 53. Yisak H, Gobena T, Mesfin F. Prevalence and risk factors for under nutrition among children under five at Haramaya district, Eastern Ethiopia. BMC Pediatr. 2015;15:212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Tadesse A. Nutritional status and associated factors among pastoralist children aged 6-23 months in Benna Tsemay woreda, South Omo Zone, Southern Ethiopia. Int J Nutr Food Sci. 2018;7:11–23. [Google Scholar]
- 55. Alemayehu M, Tinsae F, Haileslassie K, Seid O, Gebregziabher G, Yebyo H. Undernutrition status and associated factors in under-5 children, in Tigray, Northern Ethiopia. Nutrition. 2015;31:964–70. [DOI] [PubMed] [Google Scholar]
- 56. Hailemariam TW. Prevalence of underweight and its determinant factors of under two children in a rural area of Western Ethiopia. Food Sci Qual Manag. 2014;31:59–69. [Google Scholar]
- 57. Demissie S, Worku A. Magnitude and factors associated with malnutrition in children 6-59 months of age in pastoral community of Dollo Ado District. Sci J Public Health. 2013;1:175–83. [Google Scholar]
- 58. Zeray A, Kibret GD, Leshargie CT. Prevalence and associated factors of undernutrition among under-five children from model and non-model households in east Gojjam zone, Northwest Ethiopia: a comparative cross-sectional study. BMC Nutr. 2019;5:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Habtetsion M. Nutritional status of children among irrigation user and non user households in Hintalo Wajirat woreda, Tigray, Ethiopia: comparative cross sectional study. Mekelle: Mekelle University, College of Health Science; 2013. [Google Scholar]
- 60. Mohammed SH, Habtewold TD, Sileshi Tegegne B, Birhanu MM, Sissay TA, Larijani B, Esmaillzadeh A. Dietary and non-dietary determinants of linear growth status of infants and young children in Ethiopia: hierarchical regression analysis. PLoS One. 2019;14:e0209220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Derso T, Tariku A, Biks GA, Wassie MM. Stunting, wasting and associated factors among children aged 6–24 months in Dabat health and demographic surveillance system site: a community based cross-sectional study in Ethiopia. BMC Pediatr. 2017;17:96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Dearden KA, Schott W, Crookston BT, Humphries DL, Penny ME, Behrman JR, Young Lives Determinants and Consequences of Child Growth Project Team . Children with access to improved sanitation but not improved water are at lower risk of stunting compared to children without access: a cohort study in Ethiopia, India, Peru, and Vietnam. BMC Public Health. 2017;17:110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Tariku A, Woldie H, Fekadu A, Adane AA, Ferede AT, Yitayew S. Nearly half of preschool children are stunted in Dembia district, Northwest Ethiopia: a community based cross-sectional study. Arch Public Health. 2016;74:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Disha AD, Rawat R, Subandoro A, Menon P. Infant and young child feeding (IYCF) practices in Ethiopia and Zambia and their association with child nutrition: analysis of demographic and health survey data. Afr J Food Agric Nutr Dev. 2012;12:5895–914. [Google Scholar]
- 65. Jones AD, Ickes SB, Smith LE, Mbuya MNN, Chasekwa B, Heidkamp RA, Menon P, Zongrone AA, Stoltzfus RJ. World Health Organization infant and young child feeding indicators and their associations with child anthropometry: a synthesis of recent findings. Matern Child Nutr. 2014;10:1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Gibson RS, Yewelsew A, Hambidge KM, Arbide I, Teshome A, Stoecker BJ. Inadequate feeding practices and impaired growth among children from subsistence farming households in Sidama, Southern Ethiopia. Matern Child Nutr. 2009;5:260–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Mohammed SH, Esmaillzadeh A. The relationships among iron supplement use, Hb concentration and linear growth in young children: Ethiopian Demographic and Health Survey. Br J Nutr. 2017;118:730–6. [DOI] [PubMed] [Google Scholar]
- 68. Mohammed SH, Habtewold TD, Esmaillzadeh A. Household, maternal, and child related determinants of hemoglobin levels of Ethiopian children: hierarchical regression analysis. BMC Pediatr. 2019;19:113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Fentahun N, Belachew T, Lachat C. Determinants and morbidities of multiple anthropometric deficits in southwest rural Ethiopia. Nutrition. 2016;32:1243–9. [DOI] [PubMed] [Google Scholar]
- 70. Hoddinott J, Headey D, Dereje M. Cows, missing milk markets, and nutrition in rural Ethiopia. J Dev Stud. 2015;51:958–75. [Google Scholar]
- 71. Desalegn BB, Lambert C, Riedel S, Negese T, Biesalski HK. Feeding practices and undernutrition in 6–23-month-old children of Orthodox Christian mothers in rural Tigray, Ethiopia: longitudinal study. Nutrients. 2019;11:138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Tadele Wuneh M. Nutritional status and feeding practice of children 6–59 months old, Metekele Zone of Benishangul-Gumuz Region, Northwest Ethiopia. Sci J Clin Med. 2018;6:120. [Google Scholar]
- 73. Amare B, Moges B, Fantahun B, Tafess K, Woldeyohannes D, Yismaw G, Ayane T, Yabutani T, Mulu A, Ota F et al. Micronutrient levels and nutritional status of school children living in Northwest Ethiopia. Nutr J. 2012;11:108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Molla Birhanu M. Systematic reviews of prevalence and associated factors of under five malnutrition in Ethiopia: finding the evidence. Int J Nutr Food Sci. 2015;4:459. [Google Scholar]
- 75. Ngure FM, Humphrey JH, Menon P, Stoltzfus R. Environmental hygiene, food safety and growth in less than five year old children in Zimbabwe and Ethiopia. FASEB J. 2013;27:243.2.23038756 [Google Scholar]
- 76. Hagos S, Lunde T, Mariam DH, Woldehanna T, Lindtjørn B. Climate change, crop production and child under nutrition in Ethiopia; a longitudinal panel study. BMC Public Health. 2014;14:884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Hirvonen K, Headey D, Golan J, Hoddinott J. Changes in child under-nutrition in Ethiopia, 2000–16. In: Cheru F, Cramer C, Oqubay Aeditors. The Oxford handbook of the Ethiopian economy. New York: Oxford University Press; 2019. p. 398–411. [Google Scholar]
- 78. Wirth JP, Matji J, Woodruff BA, Chamois S, Getahun Z, White JM, Rohner F. Scale up of nutrition and health programs in Ethiopia and their overlap with reductions in child stunting. Matern Child Nutr. 2017;13:e12318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Tesfay GB, Abidoye B. Shocks in food availability and intra-household resources allocation: evidence on children nutrition outcomes in Ethiopia. Agric Food Econ. 2019;7:3. [Google Scholar]
- 80. Motbainor A, Worku A, Kumie A. Stunting is associated with food diversity while wasting with food insecurity among underfive children in East and West Gojjam Zones of Amhara Region, Ethiopia. PLoS One. 2015;10:e0133542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Ambel AA, Andrews C, Bakilana AM, Foster EM, Khan Q, Wang H. Examining changes in maternal and child health inequalities in Ethiopia. Int J Equity Health. 2017;16:152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Mohammed SH, Muhammad F, Pakzad R, Alizadeh S. Socioeconomic inequality in stunting among under-5 children in Ethiopia: a decomposition analysis. BMC Res Notes. 2019;12:184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Wirth JP, Rohner F, Petry N, Onyango AW, Matji J, Bailes A, de Onis M, Woodruff BA. Assessment of the WHO Stunting Framework using Ethiopia as a case study. Matern Child Nutr. 2017;13:e12310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Tessema M, De Groote H, Brouwer ID, Feskens EJM, Belachew T, Zerfu D, Belay A, Demelash Y, Gunaratna NS. Soil zinc is associated with serum zinc but not with linear growth of children in Ethiopia. Nutrients. 2019;11:221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Medhin G, Hanlon C, Dewey M, Alem A, Tesfaye F, Worku B, Tomlinson M, Prince M. Prevalence and predictors of undernutrition among infants aged six and twelve months in Butajira, Ethiopia: the P-MaMiE Birth Cohort. BMC Public Health. 2010;10:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Mekonnen AW. Prevalence of stunting and its associated factors among 6 – 59 months old children from Mersa Town, North Wollo Zone. Dessie: Wollo University, College of Medicine and Health Science; 2015. [Google Scholar]
- 87. White J, Mason J. Assessing the impact on child nutrition of the Ethiopia Community-based Nutrition Program. [Internet] New York: UNICEF; 2012; [cited 4 June 2019]. Available from: https://www.unicef.org/evaldatabase/files/Ethiopia_2013-057_CBN_Final_Report.pdf. [Google Scholar]
- 88. Kang Y, Kim S, Sisay S, Christian P. Effectiveness of a community-based nutrition programme to improve child growth in rural Ethiopia: a cluster randomized trial. Matern Child Nutr. 2017;13:e12349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Berhane G, Gilligan DO, Hoddinott J, Kumar N, Taffesse AS. Can social protection work in Africa? The impact of Ethiopia's Productive Safety Net Programme. Econ Dev Cult Change. 2014;63:1–26. [Google Scholar]
- 90. Porter C, Radhika G. Social protection for all ages? Impacts of Ethiopia's Productive Safety Net Program on child nutrition. Soc Sci Med. 2016;159:92–9. [DOI] [PubMed] [Google Scholar]
- 91. Gebrehiwot T, Castilla C. Do safety net transfers improve diets and reduce undernutrition? Evidence from rural Ethiopia. J Dev Stud. 2018;55:1947–66. [Google Scholar]
- 92. Skau J, Belachew T, Girma T, Woodruff BA. Outcome evaluation study of the Targeted Supplementary Food (TSF) program in Ethiopia. [Internet] Addis Ababa: World Food Programme, Ethiopia; 2009; [cited 4 June 2019]. Available from: https://www.alnap.org/help-library/outcome-evaluation-study-of-the-targeted-supplementary-food-tsf-program-in-ethiopia. [Google Scholar]
- 93. Ma'alin A, Birhanu D, Melaku S, Tolossa D, Mohammed Y, Gebremicheal K. Magnitude and factors associated with malnutrition in children 6–59 months of age in Shinille Woreda, Ethiopian Somali regional state: a cross-sectional study. BMC Nutr. 2016;2;44. [Google Scholar]
- 94. Gebre A, Reddy PS, Mulugeta A, Sedik Y, Kahssay M. Prevalence of malnutrition and associated factors among under-five children in pastoral communities of Afar Regional State, Northeast Ethiopia: a community-based cross-sectional study. J Nutr Metab. 2019;9187609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Mayer A-M. The causes of malnutrition in children under 3 in the Somali Region of Ethiopia related to household caring practices: preliminary report. London: Save the Children UK; 2007. [Google Scholar]
- 96. Megabiaw B, Rahman A. Prevalence and determinants of chronic malnutrition among under-5 children in Ethiopia. Int J Child Health Nutr. 2013;2:230–6. [Google Scholar]
- 97. Birhanu YW, Endris AY. Predictors of poor anthropometric status among children under two years of age in Gamo Gofa Zone, Southern Ethiopia, 2015; cross-sectional study. Epidemiology (Sunnyvale). 2015;5:209. [Google Scholar]
- 98. Genebo T, Girma W, Haider J, Demisse T. The association of children's nutritional status to maternal education in Zigbaboto, Guragie Zone, Ethiopia. Ethiop J Health Dev. 1999;13:55–61. [Google Scholar]
- 99. Semba RD, de Pee S, Sun K, Bloem MW, Raju VK. Coverage of the national vitamin A supplementation program in Ethiopia. J Trop Pediatr. 2008;54:141–4. [DOI] [PubMed] [Google Scholar]
- 100. Getaneh B, Kulkarni U, Yemane M, Mariam G. Assessment of the nutritional status and associated factors of orphans and vulnerable preschool children on care and support from nongovernmental organizations in Hawassa Town, Southern Ethiopia. Glob J Med Res. 2016;16:27–66. [Google Scholar]
- 101. Tariku A, Biks GA, Derso T, Wassie MM, Abebe SM. Stunting and its determinant factors among children aged 6–59 months in Ethiopia. Ital J Pediatr. 2017;43:112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Desalegn BB, Kinfe E, Fikre K, Bosha T. Stunting and its associated factors in under five years old children: the case of Hawassa University technology villages, Southern Ethiopia. IOSR J Environ Sci Toxicol Food Technol. 2016;10:25–31. [Google Scholar]
- 103. Sohnesen TP, Ambel A, Fisker P, Andrews C, Khan Q. Small area estimation of child malnutrition in Ethiopian woredas. [Internet] Policy Research Working Paper 7581 Washington (DC): World Bank; 2016; [cited 4 June 2019]. Available from: https://openknowledge.worldbank.org/bitstream/handle/10986/23924/Small0area0est0in0Ethiopian0woredas.pdf?sequence=1&isAllowed=y. [Google Scholar]
- 104. Headey D, Hirvonen K. Is exposure to poultry harmful to child nutrition? An observational analysis for rural Ethiopia. PLoS One. 2016;11:e0160590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Beyene TT. Predictors of nutritional status of children visiting health facilities in Jimma Zone, South West Ethiopia. Int J Adv Nurs Sci Pract. 2012;1:1–13. [Google Scholar]
- 106. Birhanu A, Mekonen S, Atenafu A, Abebaw D. Stunting and associated factors among children aged 6–59 months in Lasta woreda, North East Ethiopia, 2015: a community based cross sectional study design. J Fam Med. 2017;4:1112. [Google Scholar]
- 107. Tesfamariam K, Yilma D. Prevalence of stunting and its associated factors among children under 5 age in Holeta Town, West Shoa Zone, Oromia Region, Ethiopia, 2017. EC Nutrition. 2017;12:90–8. [Google Scholar]
- 108. Negash C, Whiting SJ, Henry CJ, Belachew T, Hailemariam TG. Association between maternal and child nutritional status in Hula, rural southern Ethiopia: a cross sectional study. PLoS One. 2015;10:e0142301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Mengistu K, Alemu K, Destaw B. Prevalence of malnutrition and associated factors among children aged 6-59 months at Hidabu Abote District, North Shewa, Oromia Regional State. J Nutr Disorders Ther. 2013;T1:001. [Google Scholar]
- 110. Alemayehu FR. Predictors of nutritional status and mortality of children in Southern Ethiopia. J Biol Agric Healthc. 2015;5:205–17. [Google Scholar]
- 111. Moges B, Feleke A, Meseret S, Doyore F. Magnitude of stunting and associated factors among 6-59 months old children in Hossana Town, Southern Ethiopia. J Clinic Res Bioeth. 2015;6:207. [Google Scholar]
- 112. Abdulahi A, Shab-Bidar S, Rezaei S, Djafarian K. Nutritional status of under five children in Ethiopia: a systematic review and meta-analysis. Ethiop J Health Sci. 2017;27:175–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Pelletier DL, Deneke K, Kidane Y, Haile B, Negussie F. The food-first bias and nutrition policy: lessons from Ethiopia. Food Policy. 1995;20:279–98. [DOI] [PubMed] [Google Scholar]
- 114. Ali D, Saha KK, Nguyen PH, Diressie MT, Ruel MT, Menon P, Rawat R. Household food insecurity is associated with higher child undernutrition in Bangladesh, Ethiopia, and Vietnam, but the effect is not mediated by child dietary diversity. J Nutr. 2013;143:2015–21. [DOI] [PubMed] [Google Scholar]
- 115. Lindtjorn B, Alemu T, Bjorvatn B. Nutritional-status and risk of infection among Ethiopian children. J Trop Pediatr. 1993;39:76–82. [DOI] [PubMed] [Google Scholar]
- 116. Amsalu ET, Akalu TY, Gelaye KA. Spatial distribution and determinants of acute respiratory infection among under-five children in Ethiopia: Ethiopian Demographic Health Survey 2016. PLoS One. 2019;14:e0215572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Alemu ZA, Ahmed AA, Yalew AW, Birhanu BS. Non random distribution of child undernutrition in Ethiopia: spatial analysis from the 2011 Ethiopia demographic and health survey. Int J Equity Health. 2016;15:198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Lindtjørn B, Alemu T. Year-to-year and seasonal variations in stunting among preschool children in Ethiopia. J Health Popul Nutr. 2002;20:326–33. [PubMed] [Google Scholar]
- 119. Mulugeta A, Hagos F, Kruseman G, Linderhof V, Stoecker B, Abraha Z, Yohannes M, Samuel GG. Child malnutrition in Tigray, northern Ethiopia. East Afr Med J. 2010;87:248–54. [DOI] [PubMed] [Google Scholar]
- 120. Kahsay A. Nutritional status of children (6-59 months) from food secure and food insecure households in rural communities of Saesie Tsaeda-Emba District, Tigray, North Ethiopia: comparative study. Int J Nutr Food Sci. 2015;4:51. [Google Scholar]
- 121. Wasihun AG, Dejene TA, Teferi M, Marugán J, Negash L, Yemane D, McGuigan KG. Risk factors for diarrhoea and malnutrition among children under the age of 5 years in the Tigray Region of Northern Ethiopia. PLoS One. 2018;13:e0207743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Malako BG, Asamoah BO, Tadesse M, Hussen R, Gebre MT. Stunting and anemia among children 6–23 months old in Damot Sore district, Southern Ethiopia. BMC Nutr. 2019;5:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Abera L, Dejene T, Laelago T. Prevalence of malnutrition and associated factors in children aged 6–59 months among rural dwellers of Damot Gale District, South Ethiopia: community based cross sectional study. Int J Equity Health. 2017;16:111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Kastro Dake S, Solomon FB, Bobe TM, Tekle HA, Tufa EG. Predictors of stunting among children 6–59 months of age in Sodo Zuria District, South Ethiopia: a community based cross-sectional study. BMC Nutr. 2019;5:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Yalew BM, Amsalu F, Bikes D. Prevalence and factors associated with stunting, underweight and wasting: a community based cross sectional study among children age 6-59 months at Lalibela Town, Northern Ethiopia. J Nutr Disorders Ther. 2014;4:147. [Google Scholar]
- 126. Berhanu G, Mekonnen S, Sisay M. Prevalence of stunting and associated factors among preschool children: a community based comparative cross sectional study in Ethiopia. BMC Nutr. 2018;4:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Assefa KM, Alemu K, Destaw B. Prevalence of malnutrition and associated factors among children aged 6–59 months at Hidabu Abote District, North Shewa, Oromia Regional State. Ann Nutr Metab. 2015;67(suppl 1):216–7. [Google Scholar]
- 128. Asfaw M, Wondaferash M, Taha M, Dube L. Prevalence of undernutrition and associated factors among children aged between six to fifty nine months in Bule Hora district, South Ethiopia. BMC Public Health. 2015;15:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Wondemeneh Tamiru M. Under nutrition and associated factors among under-five age children of Kunama ethnic groups in Tahtay Adiyabo woreda, Tigray Regional State, Ethiopia: community based study. Int J Nutr Food Sci. 2015;4:277. [Google Scholar]
- 130. Adeba A, Garoma S, Gemede HF, Garoma W. Prevalence of stunting and associated factors of children among 6-59 months age in Guto Gida District, East Wollega Zone, Oromia, Ethiopia. Food Science and Quality Management. 2014;; [cited 2019 Jul 10];29:. Available from:https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0195361. [Google Scholar]
- 131. Abate KH, Belachew T. Women's autonomy and men's involvement in child care and feeding as predictors of infant and young child anthropometric indices in coffee farming households of Jimma Zone, South West of Ethiopia. PLoS One. 2017;12:e0172885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Abate KH, Belachew T.. Care and not wealth is a predictor of wasting and stunting of “The Coffee Kids” of Jimma Zone, southwest Ethiopia. Nutr Health. 2017;23:193–202. [DOI] [PubMed] [Google Scholar]
- 133. Betebo B, Ejajo T, Alemseged F, Massa D. Household food insecurity and its association with nutritional status of children 6–59 months of age in East Badawacho District, South Ethiopia. J Environ Public Health. 2017:6373595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Fekadu Y, Mesfin A, Haile D, Stoecker BJ. Factors associated with nutritional status of infants and young children in Somali Region, Ethiopia: a cross- sectional study. BMC Public Health. 2015;15:846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Okike I, Jabbar MA, Gugsa A, Lema K. Household and environmental factors influencing anthropometric outcomes in preschool children in a rural Ethiopian community. Ecol Food Nutr. 2005;44:167–87. [Google Scholar]
- 136. Tessema M, Belachew T, Ersino G. Feeding patterns and stunting during early childhood in rural communities of Sidama, South Ethiopia. Pan Afr Med J. 2013;14:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Brhane G, Regassa N. Nutritional status of children under five years of age in Shire Indaselassie, North Ethiopia: examining the prevalence and risk factors. Kontakt. 2014;16:e161–70. [Google Scholar]
- 138. Darsene H, Geleto A, Gebeyehu A, Meseret S. Magnitude and predictors of undernutrition among children aged six to fifty nine months in Ethiopia: a cross sectional study. Arch Public Health. 2017;75:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Teshome B, Kogi-Makau W, Getahun Z, Taye G. Magnitude and determinants of stunting in children underfive years of age in food surplus region of Ethiopia: the case of West Gojam Zone. Ethiop J Health Dev. 2009;23:98–106. [Google Scholar]
- 140. Sako B, Leerlooijer JN, Lelisa A, Hailemariam A, Brouwer ID, Tucker Brown A, Osendarp SJM. Exploring barriers and enablers for scaling up a community‐based grain bank intervention for improved infant and young child feeding in Ethiopia: a qualitative process evaluation. Matern Child Nutr. 2018;14:e12551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Demilew YM, Abie DD. Undernutrition and associated factors among 24–36-month-old children in slum areas of Bahir Dar city, Ethiopia. Int J Gen Med. 2017;10:79–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Eshete H, Abebe Y, Loha E, Gebru T, Tesheme T. Nutritional status and effect of maternal employment among children aged 6–59 months in Wolayta Sodo Town, Southern Ethiopia: a cross-sectional study. Ethiop J Health Sci. 2017;27:155–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Abebe Z, Haki GD, Baye K. Health extension workers’ knowledge and knowledge-sharing effectiveness of optimal infant and young child feeding are associated with mothers’ knowledge and child stunting in rural Ethiopia. Food Nutr Bull. 2016;37:353–63. [DOI] [PubMed] [Google Scholar]
- 144. WHO, UNICEF WHO Child Growth Standards and the identification of severe acute malnutrition in infants and children: a joint statement. [Internet] Geneva, Switzerland and New York: WHO, UNICEF; 2009; [cited 10 July 2019]. Available from: www.who.int/childgrowth/standards. [PubMed] [Google Scholar]
- 145. Victora CG, de Onis M, Hallal PC, Blossner M, Shrimpton R. Worldwide timing of growth faltering: revisiting implications for interventions. Pediatrics. 2010;125:e473–80. [DOI] [PubMed] [Google Scholar]
- 146. UCLA Statistical Consulting Group How can I run a piecewise regression in Stata? Stata FAQ. [Internet] Los Angeles: UCLA Institute for Digital Research & Education; 2019; [cited 12 November 2019]. Available from: https://stats.idre.ucla.edu/stata/faq/how-can-i-run-a-piecewise-regression-in-stata/. [Google Scholar]
- 147. Barros AJD, Victora CG. Measuring coverage in MNCH: determining and interpreting inequalities in coverage of maternal, newborn, and child health interventions. PLoS Med. 2013;10:e1001390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Kakwani N, Wagstaff A, van Doorslaer E. Socioeconomic inequalities in health: measurement, computation, and statistical inference. J Econom. 1997;77:87–103. [Google Scholar]
- 149. Victora CG, Huttly SR, Fuchs SC, Olinto MT. The role of conceptual frameworks in epidemiological analysis: a hierarchical approach. Int J Epidemiol. 1997;26:224–7. [DOI] [PubMed] [Google Scholar]
- 150. Strumpf EC, Harper S, Kaufman JS. Fixed effects and difference-in-differences. Methods in Social Epidemiology. 2nd ed, Michael Oakes J, Kaufman JSeditors. San Francisco, CA: Jossey-Bass;2017. [Google Scholar]
- 151. Federal Ministry of Health. Health Sector Strategic Plan (HSDP-III) 2005/6–2009/10. Ethiopia: The Federal Democratic Republic of Ethiopia; 2005. [Google Scholar]
- 152. Federal Ministry of Health. Health Extension Progam in Ethiopia. Addis Ababa, Ethiopia: The Federal Democratic Republic of Ethiopia; 2007. [Google Scholar]
- 153. Negash S. Enhanced outreach strategy/ targeted supplementary feeding for child survival in Ethiopia (EOS/ TSF). Field Exchange. 2011;40:7–10. [Google Scholar]
- 154. The Provisional Military Administration Council A proclamation to provide for the public ownership of rural lands. Addis Ababa, Ethiopia: The Provisional Military Administration Council; 1975. [Google Scholar]
- 155. Abebe M. The March 1975 “Land to the Tiller” proclamation: dream or reality?. Am Res J Hist Cult. 2016;2:1–5. [Google Scholar]
- 156. Dube AK, Fawole WO, Govindasamy R, Ozkan B. Agricultural development led industrialization in Ethiopia: structural break analysis. Int J Agric For Life Sci. 2019;3:(1):193–201. [Google Scholar]
- 157. Agricultural Transformation Agency Ethiopian agriculture and strategies for growth. Addis Ababa, Ethiopia: Ethiopian Agricultural Transformation Agency; 2017. [Google Scholar]
- 158. Gebreeyesus M. Industrial policy and development in Ethiopia. In: Newman C, Page J, Rand J, Shimeles A, Söderbom M, Tarp Feditors. Manufacturing transformation: comparative studies of industrial development in Africa and emerging Asia. Oxford: Oxford University Press; 2016. p. 27–49. [Google Scholar]
- 159. Federal Democratic Republic of Ethiopia Ministry of Finance and Economic Development Ethiopia: Sustainable Development and Poverty Reduction Program. Ethiopia: The Federal Democratic Republic of Ethiopia; 2002. [Google Scholar]
- 160. Ministry of Finance and Economic Development (MoFED) Growth and Transformation Plan (GTP) 2010/11–2014/15 Draft. Ethiopia: The Federal Democratic Republic of Ethiopia; 2010. [Google Scholar]
- 161. Ministry of Finance and Economic Development (MoFED) Ethiopia: building on progress: a Plan for Accelerated and Sustained Development to End Poverty (PASDEP) (2005/06-2009/10): Volume I: main text. Addis Ababa, Ethiopia: MoFED; 2006. [Google Scholar]
- 162. IMF Growth and Transformation Plan (2010/11-2014/15). [Internet] Addis Ababa, Ethiopia: International Monetary Fund; 2010; [accessed 10 July 2019]. Available from: https://www.imf.org/external/pubs/ft/scr/2011/cr11305.pdf. [Google Scholar]
- 163. Federal Democratic Republic of Ethiopia Growth and Transformation Plan II (GTP II) (2015/16-2019/20)[Internet]. Addis Ababa, Ethiopia: National Planning Commission of The Federal Democratic Republic of Ethiopia; 2016; [accessed 10 July 2019]. Available from: http://extwprlegs1.fao.org/docs/pdf/eth169444.pdf. [Google Scholar]
- 164. Ethiopian Federal Ministry of Health Expanded Program on Immunisation (EPI). Strategy[Internet]. Addis Ababa, Ethiopia: The Federal Democratic Republic of Ethiopia; 2004; [accessed 10 July 2019]. Available from: https://www.who.int/countries/eth/areas/immunization/en/epi.pdf. [Google Scholar]
- 165. Ethiopian Federal Ministry of Health Ethiopian National Expanded Programme on Immunization: comprehensive multi-year plan 2016–2020[Internet]. Addis Ababa, Ethiopia: The Federal Democratic Republic of Ethiopia; 2015; [accessed 10 July 2019]. Available from: https://extranet.who.int/countryplanningcycles/sites/default/files/country_docs/Ethiopia/ethiop_cmyp_latest_revised_may_12_2015.pdf. [Google Scholar]
- 166. Central Statistical Agency of Ethiopia, ICF Ethiopia Demographic and Health Survey 2016. [Internet] Addis Ababa, Ethiopia and Rockville, MD: Central Statistical Agency of Ethiopia and ICF; 2017; [cited 28 May 2019]. Available from: https://dhsprogram.com/pubs/pdf/FR328/FR328.pdf. [Google Scholar]
- 167. Federal Health Department of the Federal Ministry of Health National Strategy for Child Survival[Internet]. Addis Ababa, Ethiopia: The Federal Democratic Republic of Ethiopia; 2005; [accessed 28 May 2019]. Available from: https://extranet.who.int/nutrition/gina/sites/default/files/ETH%202005%20National%20Strategy%20for%20Child%20Survival.pdf. [Google Scholar]
- 168. Maternal and Child Health Directorate of the Federal Ministry of Health. National Strategy for Newborn and Child Survival in Ethiopia 2015/16 - 2019/20 [Internet]. Addis Ababa, Ethiopia: The Federal Democratic Republic of Ethiopia; 2015; [accessed 28 May 2019]. Available from: https://www.healthynewbornnetwork.org/hnn-content/uploads/nationalstrategy-for-newborn-and-child-survival-in-ethiopia-201516-201920.pdf. [Google Scholar]
- 169. Federal Democratic Republic of Ethiopia Ministry of Health Health Sector Development Program-IV 2010/11-2014/15. [Internet] Addis Ababa, Ethiopia: The Federal Democratic Republic of Ethiopia; 2010; [accessed 28 May 2019]. Avabilable from: https://www.healthynewbornnetwork.org/hnn-content/uploads/HSDP-IV-Final-Draft-October-2010-2.pdf. [Google Scholar]
- 170. Sebhatu A. The implementation of Ethiopia's Health Extension Program: an overview [Internet]. Addis Ababa, Ethiopia: Partners for Population Development; 2008; [accessed 28 May 2019]. Available from: http://www.partners-popdev.org/wp-content/uploads/2017/11/ethiopiahep.pdf. [Google Scholar]
- 171. Wang H, Tesfaye R, Ramana GNV, Chekagn CT. Ethiopia Health Extension Program: an institutionalized community approach for universal health coverage. Washington (DC): World Bank; 2016. [Google Scholar]
- 172. Damtew ZA, Chekagn CT, Moges AS. The Health Extension Program of Ethiopia: strengthening the community health system. [Internet] Cambridge, MA: Harvard Health Policy Review; 2016 [accessed 28 May 2019]. Available from: http://www.hhpronline.org/articles/2016/12/17/the-health-extension-program-of-ethiopia. [Google Scholar]
- 173. Assefa Y, Gelaw YA, Hill PS, Taye BW, Van Damme W. Community health extension program of Ethiopia, 2003–2018: successes and challenges toward universal coverage for primary healthcare services. Global Health. 2019;15:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Federal Ministry of Health Integrating enhanced outreach strategy into Health Extension Programme Ethiopia, a transitional plan. Addis Ababa, Ethiopia: The Federal Democratic Republic of Ethiopia; 2010. [Google Scholar]
- 175. The Federal Ministry of Health of the Federal Democratic Republic of Ethiopia National Nutrition Strategy. Addis Ababa, Ethiopia: The Federal Democratic Republic of Ethiopia; 2008. [Google Scholar]
- 176. The Federal Democratic Republic of Ethiopia. Health Policy of the Transitional Government of Ethiopia. Addis Ababa, Ethiopia: The Federal Democratic Republic of Ethiopia; 1993; [accessed 28 May 2019]. Available from: https://www.mindbank.info/item/721. [Google Scholar]
- 177. Federal Democratic Republic of Ethiopia Ministry of Health National Hygiene and Sanitation Strategy [Internet]. Washington, DC, USA: World Bank Group; 2005; [accessed 28 May 2019]. Avaiable from: http://documents1.worldbank.org/curated/en/216221468023104331/pdf/463600WSP0Box31SanitationStrategyAF.pdf. [Google Scholar]
- 178. Federal Democratic Republic of Ethiopia Ministry of Health National Hygiene & Sanitation Strategic Action Plan for Rural, Per-Urban & Informal Settlements in Ethiopia, Part II. Addis Ababa, Ethiopia: Federal Democratic Republic of Ethiopia; 2011. [Google Scholar]
- 179. Federal Ministry of Health. National iCCM-CBNC Quality Improvement and Transition Plan July 2017-June 2019. Addis Ababa, Ethiopia: The Federal Democratic Republic of Ethiopia; 2017. [Google Scholar]
- 180. Headey D, Hoddinott J, Park S. Drivers of nutritional change in four South Asian countries: a dynamic observational analysis. Matern Child Nutr. 2016;12:210–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181. Alderman H, Headey D. The timing of growth faltering has important implications for observational analyses of the underlying determinants of nutrition outcomes. PLoS One. 2018;13:e0195904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. The World Bank Agriculture & rural development: Ethiopia. [Internet] World Development Indicators Washington (DC): World Bank; 2019 [cited 12 September 2019]. Available from: https://data.worldbank.org/topic/agriculture-and-rural-development?locations=ET&view=chart. [Google Scholar]
- 183. FAO Food balance sheets. [Internet] Rome, Italy: FAO; 2017; [cited 12 September 2019]. Available from: http://www.fao.org/faostat/en/#data/FBS. [Google Scholar]
- 184. The Federal Democratic Republic of Ethiopia Central Statistics Agency Area and production of major crops. Addis Ababa, Ethiopia: Federal Democratic Republic of Ethiopia; 2015. [Google Scholar]
- 185. Giday T, Asnake M, Wilder J. Ethiopia's HEP: Pathfinder International's Support 2003–2007 [Internet]. Ethiopia: Pathfinder International Ethiopia, USAID; 2008 [cited 21 August 2019]:1–8.. Available from: http://www2.pathfinder.org/site/DocServer/CBRHAs__HEWs_REVISED_REPRINT__2_.pdf?docID=11303. [Google Scholar]
- 186. Mehta L. Community-led total sanitation (CLTS) across the seas: experiences from Africa with a special emphasis on Ethiopia. [Internet] RiPPLE Working Paper; 2009 [accessed 21 August 2019]. Available from: https://www.ids.ac.uk/publications/community-led-total-sanitation-clts-across-the-seas-experiences-from-africa-with-a-special-emphasis-on-ethiopia/ [Google Scholar]
- 187. Sah S, Negussie A. Community Led Total Sanitation (CLTS): addressing the challenges of scale and sustainability in rural Africa [Internet]. Desalination. 2009;248(1–3):666–72. [cited 21 August 2019].. Available from: 10.1016/j.desal.2008.05.117. [DOI] [Google Scholar]
- 188. World Bank Ethiopia overview. [Internet] Washington (DC): World Bank; 2019; [cited 21 August 2019]. Available from: https://www.worldbank.org/en/country/ethiopia/overview. [Google Scholar]
- 189. Savadogo B, Bronselaer D. Basic Education, Technical and Vocational Training Project (EducationII): project completion report. Abidjan, Côte d’Ivoire: African Development Bank Group; 2004. [Google Scholar]
- 190. Federal Ministry of Health. Education Sector Development Program IV (2010/2011–2014/2015) Program Action Plan /PAP. Addis Ababa, Ethiopia: The Federal Democratic Republic of Ethiopia; 2010. [Google Scholar]
- 191. Bogale A, Shimelis A. Household level determinants of food insecurity in rural areas of dire dawa, eastern Ethiopia. African J Food Agric Nutr Dev. 2009;9:1914–26. [Google Scholar]
- 192. Feyissa D. Expectations and belonging in Dire Dawa: drivers, dynamics and challenges of rural to urban mobility [Internet]. Nairobi, Kenya: Rift Valley Institute; 2018 [cited 21 August 2019]. Available from: https://www.ecoi.net/en/file/local/1433517/1226_1527500554_expectations-and-belonging-in-dire-dawa-by-dereje-feyissa-rvi-2018.pdf. [Google Scholar]
- 193. United Nations Human Settlements Programme Ethiopia: Dire Dawa urban profile. Nairobi, Kenya: ;United Nations Human Settlements Programme (UN-HABITAT); 2008. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.